Abstract
Purpose
Human dirofilariasis cases have increased in Europe for the last few decades. We document an autochthonous case of dirofilariasis infection in the subconjunctival space of a 60-year-old Spanish man.
Observations
The patient presented with pain in his right eye, which was diagnosed as epi-scleritis. In spite of the treatment administered, no improvement was reported. An external exam showed conjunctival congestion on the temporal part of the right eye bulbar conjunctiva. The anterior chamber showed no flare or cells in both eyes and dilated fundus exam was normal. Nevertheless, a long whitish vermiform mobile mass was detected under the conjunctiva in the temporal part of the right eye. The worm was surgically removed and diagnosed morphologically and also molecularly as Dirofilaria repens. This species uses dogs and wild canids as definitive hosts and principal reservoirs, while mosquito species are transmitters. Humans act as accidental hosts, and clinical manifestations depend on the location of the worm in the organs and tissues.
Conclusions and importance
The correct diagnosis and control of subcutaneous/ocular dirofilariasis by D. repens require several professionals under the One Health approach to deal with this zoonotic disease, which poses a serious public health problem, at least in the Mediterranean Basin.
Keywords: Dirofilaria repens, Subconjunctival dirofilariasis, Human infection
1. Introduction
Dirofilariasis is a zoonotic infection caused by filarioid nematodes of the genus Dirofilaria (Spirurida, Onchocercidae). Among the different species, D. repens uses dogs and wild canids as definitive hosts and principal reservoirs, and mosquito species as vectors. Humans act as accidental hosts and, in most cases, a single worm develops, without microfilaremia.1 Herein, we report an autochthonous subconjunctival case of D. repens infection treated at the Ophthalmology Service of Hospital General Universitario de Castellón, Castellón, Spain.
2. Case report
A 60-year-old man from Nules (Castellón, Spain) attended the emergency unit of Hospital General Universitario de Castellón, complaining of a pain in his right eye which he had suffered for a week. Initially, the patient had consulted his general practitioner a week before because of red-eye but without discharge. He was diagnosed with epi-scleritis. Following treatment with dexamethasone eye drops, no improvement was reported. After the standard practice, we carried out a full exploration of the patient. Best-corrected visual acuity was 20/20 in both eyes. An external exam showed conjunctival congestion on the temporal part of right eye bulbar conjunctiva. Following slit-lamp examination, the anterior chamber showed no flare or cells in both eyes, although there was a long whitish vermiform mobile mass under the conjunctiva in the temporal part of the right eye. Dilated fundus exam was normal. Emergency surgery was performed under local anesthesia. A small conjunctival incision was made using Westcott scissors to expose the worm. The entire parasite was removed while alive (Fig. 1A). The translucent parasite was stored in physiological saline and sent to the Microbiology Unit of Hospital General Universitario de Castellón, and afterwards to the Department of Parasitology of University of Valencia for identification. Thereafter, we referred the patient to the internist for further examination to ensure there were no other worms in the rest of the body. The patient had no history of similar episodes in the past, living in the countryside with different animals. He had no history of international travel. Within one month, the excision site healed uneventfully, without recurrences.
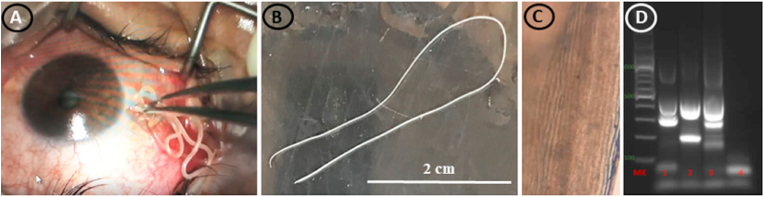
Fig. 1.
(A) Worm of Dirofilaria repens removed from the subconjunctiva of the patient eye; (B) entire worm isolated in the present case; (C) aspect of the ridges of the cuticle under an optical microscope; (D) Multiplex PCR amplification of the DNA extracted from the worm surgically removed from the patient. Lane 1: sample obtained from the worm removed from the patient; lane 2: D. immitis positive control (500 pb and 204 pb); lane 3: D. repens positive control (500 pb and 327 pb); lane 4: negative control. MK: molecular marker, 100–1000 pb.
The worm was morphologically identified as an immature female worm, thin, cylindrical, white, 0,470 mm thick and about 110 mm in length (Fig. 1B). Anterior end was rounded and of greater diameter (213 μm) than the posterior end (163 μm), with 105 μm tail. Under the microscope, after clarification with Lactophenol, the outer surface of the nematode's cuticle was found with external longitudinal cuticular ridges (Fig. 1C). Some features prompted us to consider a filariform appearance, assigning it as Dirofilaria repens. Since other nematodes could be implicated in the parasitism of the eye, and to reaffirm the morphological diagnosis, the worm was sent to Laboratory of Parasitology of University of Salamanca in order to be molecularly processed. Crude DNA preparations were obtained from the isolated worm following the instructions of the Nucleospin® Tissue Kit (Macherey-Nagel). Then, the extracted DNA was resuspended in 15 μl of PCR-grade water and amplified by multiplex PCR according to the protocol described by2 with minor modifications. The results showed a pattern of bands compatible with D. repens (Fig. 1D).
3. Discussion
Dirofilaria repens causes both canine and feline subcutaneous dirofilariasis, although it is also able to cause human subcutaenous/ocular dirofilariasis. The transmission of this nematode takes place through a mosquito vector with species belonging to different genera, i.e. Anopheles, Aedes, Culex and Coquillettidia,3 which have been detected in the autonomous region of Valencia, particularly in Castellon province.4
This species is an endemic nematode of southern Europe (Italy, Spain, France, and Greece), and particularly of the Mediterranean Basin.1,5 However, D. repens prevalence is higher in humans than that of others species of Dirofilaria, possibly due to the easy detection of subcutaneous nodules and sub- and conjunctival infections.6 In any case, this endemic disease is gradually spreading to West-Central (Germany, Austria, Poland, and Hungary), Balkan (Serbia, Croatia, and Bulgaria), Eastern (Slovakia, Romania, Ukraine, Rostov region, and in various territories of Russia), Baltic (Lithuania and Latvia) and the Nordic (Finland) European countries3,7,8
During D. repens migration, and from a clinical point of view, different body areas and tissues have been reported to be affected, with the symptoms usually being limited to edema, local irritation, erythema and pruritus, or presenting with no symptoms at all. When reaching the eye, the worm can be observed through the subconjunctiva, although it is able to migrate in the intra-, peri-, or retro-ocular space. Dirofilaria can cause lid and lacrimal gland swelling, uveitis, glaucoma, epi-scleritis, and intraocular dirofilariasis.1,3
The diagnosis of this zoonotic filariasis is based on the microscopic identification of the worm in a histological section of a biopsy or the extraction of the worm from the lesion. Serological diagnosis does not usually make sufficient interspecific discrimination. Molecular techniques are a complementary tool, particularly in those cases where the host's immune response may alter the parasite morphology, or where the parasite's microhabitat may lead to specific confusion.9,10
The best treatment option in this type of filariasis is the surgical removal of the worm, as pharmacological treatments are usually not necessary. Measures to control this infection are focused on dogs and humans as well as mosquitoes.
In summary, multidisciplinary collaboration among entomologists, parasitologists, veterinarians, clinicians and public health experts, under the One Health approach, is needed in order to deal with this public health issue caused by D. repens infection, which is relevant, above all, in the Mediterranean Basin.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Funding source
None.
Ethical approval
Approval was not required.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
None.
References
- 1.Simón F., Siles-Lucas M., Morchón R., et al. Human and animal dirofilariasis: the emergence of a zoonotic mosaic. Clin Microbiol Rev. 2012;25:507–544. doi: 10.1128/CMR.00012-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gioia G., Lecová L., Genchi M., Ferri E., Genchi C., Mortarino M. Highly sensitive multiplex PCR for simultaneous detection and discrimination of Dirofilaria immitis and Dirofilaria repens in canine peripheral blood. Vet Parasitol. 2010;172:160–163. doi: 10.1016/j.vetpar.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 3.Capelli G., Genchi C., Baneth G., et al. Recent advances on Dirofilaria repens in dogs and humans in Europe. Parasites Vectors. 2018;11:663. doi: 10.1186/s13071-018-3205-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bueno-Marí R., Bernués-Bañeres A., Jiménez-Peydró R. Updated checklist and distribution maps of mosquitoes (Diptera: Culicidae) of Spain. Eur Mosq Bull. 2012;30:91–126. [Google Scholar]
- 5.Tahir D., Davoust B., Parola P. Vector-borne nematode diseases in pets and humans in the Mediterranean Basin: an update. Vet World. 2019;12:1630–1643. doi: 10.14202/vetworld.2019.1630-1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muro A., Genchi C., Cordero M., Simón F. Dirofilariasis humana en la Unión Europea. Parasitol Today. 1999;15:386–389. doi: 10.1016/s0169-4758(99)01496-9. [DOI] [PubMed] [Google Scholar]
- 7.Genchi C., Kramer L. Subcutaneous dirofilariosis (Dirofilaria repens): an infection spreading throughout the old world. Parasites Vectors. 2017;10:517. doi: 10.1186/s13071-017-2434-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alsarraf M., Levytska V., Mierzejewska E.J., et al. Emerging risk of Dirofilaria spp. infection in Northeastern Europe: high prevalence of Dirofilaria repens in sled dog kennels from the Baltic countries. Sci Rep. 2021;11:1068. doi: 10.1038/s41598-020-80208-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foissac M., Million M., Mary C., et al. Subcutaneous infection with Dirofilaria immitis nematode in human. Fr. Emerg. Infect. Dis. 2013;19(1):171–172. doi: 10.3201/eid1901.120281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benzaquen M., Brajon D., Delord M., et al. Cutaneous and pulmonary dirofilariasis due to Dirofilaria repens. Br J Dermatol. 2015;173:788–791. doi: 10.1111/bjd.13859. [DOI] [PubMed] [Google Scholar]