Abstract
Background
The purpose of this study was to evaluate the age-related change in pelvic sagittal inclination in the standing position after total hip arthroplasty (THA). This study hypothesized that the rate of progression of posterior tilt is not constant.
Material and methods
We measured sacral slope and pelvic tilt in 36 patients who were followed up for more than 10 years after unilateral primary THA.
Results
The posterior pelvic tilt in the standing position progressed significantly in the first year after THA and then progressed slowly. However, there was a tendency to accelerate again for those older than 75 years. Posterior pelvic tilt tended to progress rapidly after surgery in patients with femoral neck fractures and subchondral fractures of the femoral head.
Conclusions
In patients older than 75 years and those with fragility fractures, postoperative pelvic tilt in the standing position tends to be greater, suggesting that the use of a large head or dual mobility system should be considered.
Keywords: Total hip arthroplasty, Posterior pelvic tilt, Standing position, Rate of progression, Spinopelvic harmony
Background
In the field of total hip arthroplasty (THA), the influence of hip-spine relationships has recently attracted attention [[1], [2], [3]]. The placement of an acetabular component based on the hip-spine relationship has been recommended [1,2,4]. However, these recommendations are based on the condition at the time of surgery and do not consider long-term changes.
Previous studies [5,6] have suggested that pelvic sagittal inclination in the standing position after THA increases posteriorly over time. Pelvic reclination of 10° will lead to functional anteversion of the acetabular cup of approximately 7° [7] and increase the risk of anterior dislocation. Ideally, the degree and risk of future pelvic inclination should be predicted preoperatively, and a surgical plan to account for it should be developed [[6], [8], [9], [10], [11]].
In patients undergoing long-term follow-up after THA, posterior pelvic tilt (PT) in the standing position progresses slowly in some cases, while in others, it progresses rapidly in the early postoperative period. In other cases, posterior PT progresses slowly initially but then more rapidly after a period of time. In this study, age-related changes in pelvic sagittal inclination were evaluated based on the hypothesis that the rate of progression of posterior PT in the standing position after THA is not constant.
Material and methods
This study was approved by the author’s institutional review board, and informed consent was obtained from all patients.
Thirty-six patients were followed up for more than 10 years after unilateral primary THA in our department between February 2004 and October 2010. There were 2 men and 34 women with a mean age at surgery of 60.0 ± 10.8 years (range, 38-85 years). There were 29 patients with osteoarthritis, 1 patient each with idiopathic osteonecrosis of the femoral head, femoral neck fracture, or femoral head fracture, and 2 patients each with osteonecrosis of the femoral head after femoral neck fracture or subchondral fracture of the femoral head.
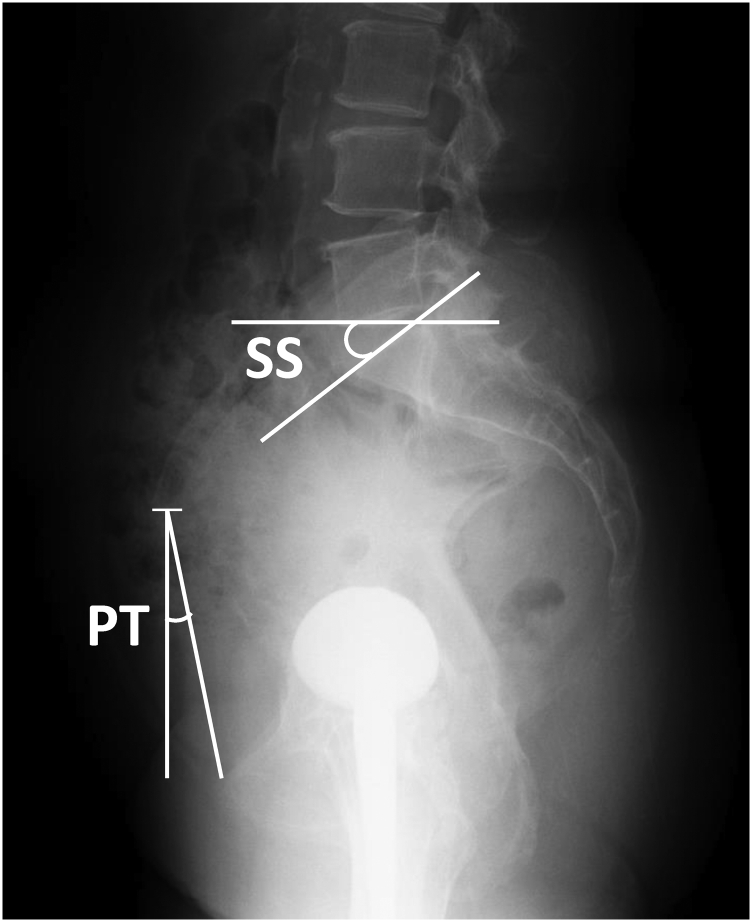
Preoperative sacral slope (SS) and PT in the supine and standing positions were measured to evaluate the difference in preoperative pelvic sagittal inclination between supine and standing postures. SS and PT in the standing position were measured using lateral spinopelvic radiographs. SS was defined as the angle formed by the S1 endplate and a horizontal line. PT was defined as the angle between the anatomic pelvic plane (APP) and the coronal plane [[12], [13], [14]]. The APP is defined by the plane connecting the anterior superior iliac spines and the most anterior aspect of the pubic tubercle. On imperfect lateral spinopelvic radiographs, the superior end of the APP intersects the horizontal midpoint between the left and right anterior superior iliac spines [2] (Fig. 1). SS and PT in the supine position were measured using a digitally reconstructed radiograph of the spinopelvic sagittal view of preoperative computed tomography.
Figure 1.
Measurement of pelvic sagittal inclination in the standing position. PT, pelvic tilt; SS, sacral slope.
Spinopelvic lateral radiographs in the standing position were taken at each follow-up time after THA. SS and PT in the standing position were measured to evaluate secular changes of pelvic sagittal inclination in the standing position. Posterior PT was defined by positive values, and anterior PT by negative values.
Data are expressed as mean ± standard deviation. Spearman's rank correlation coefficients and Wilcoxon signed-rank tests were used for postoperative evaluation of SS and PT. P values < .05 were considered significant. All statical analyses were performed using Statcel, the Useful Addin Forms on Excel-4th ed.
Results
The mean postoperative follow-up period was 11.8 ± 2.0 years (range, 10-16 years).
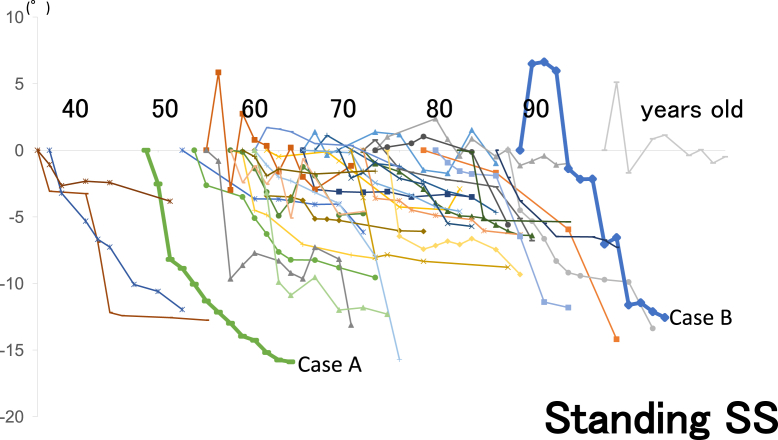
The mean changes of SS and PT in the standing position before THA and the last observation were −7.4° ± 4.5° (−15.9° to 1.0°) and −9.5° ± 5.4° (−21.7° to 0.6°), respectively. Posterior PT in the standing position progressed significantly in the first year after THA (mean change of SS = −3.2° ± 3.3°/y and mean change of PT = −5.0° ± 4.0°/y) and then more slowly (mean change of SS = −0.41° ± 0.40°/y and mean change of PT = −0.42° ± 0.41°/y) (P = .0.018). There was a clear positive correlation between SS and PT in the standing position (P = .0035) (Figure 2, Figure 3).
Figure 2.
Postoperative changes of pelvic sagittal inclination in the standing position after THA. The preoperative value is used as the reference (0°). Standing PT, pelvic tilt in standing position; Standing SS, sacral slope in the standing position. There was a clear positive correlation between SS and PT in the standing position. P = .0035, Spearman’s rank correlation coefficient.
Figure 3.
A 60-year-old woman at the time of surgery with unilateral dysplastic hip arthropathy. The posterior pelvic tilt in the standing position progressed significantly in the first 3 months after THA and remained at a constant angle thereafter. By the age of 73 years, 13 years after surgery, the posterior pelvic tilt in the standing position was 3.5° in SS and 5° in PT. (a) Change of SS in the standing position. (b) Anteroposterior (AP) radiographs of the pelvis in the standing position. (c) Lateral spinopelvic radiographs in the standing position. Line, S1 endplate line; dotted line, anatomical pelvic plane (APP).
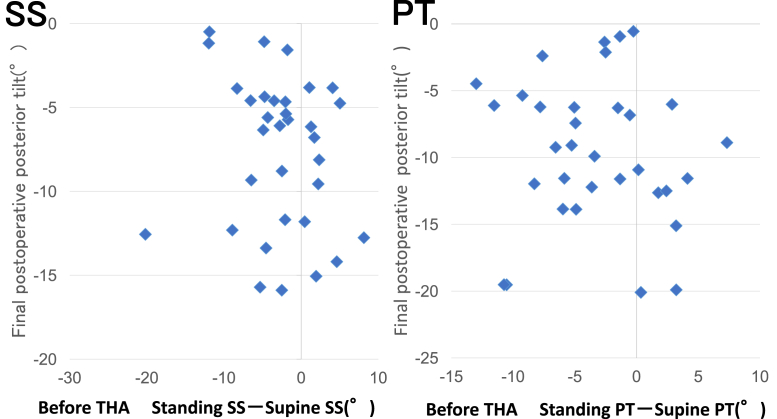
There was no clear correlation between the change in posture from standing to supine positions before surgery and the degree of posterior tilt progression after surgery (Fig. 4).
Figure 4.
Scattergram of preoperative postural changes and postoperative final posterior tilt. There was no clear correlation between preoperative postural changes and the degree of posterior tilt progression after surgery. Standing PT, pelvic tilt in the standing position; Supine PT, pelvic tilt in the supine position; Standing SS, sacral slope in the standing position; Supine SS, sacral slope in the supine position. P = .16 (SS), P = .36 (PT), Spearman’s rank correlation coefficient.
When postoperative changes of pelvic sagittal inclination in the standing position after THA were examined based on the age at surgery, there was a tendency for posterior tilt to progress at an accelerated rate in patients older than 75 years (Fig. 5).
Figure 5.
Postoperative changes in pelvic sagittal inclination in the standing position over time. The preoperative value is used as the reference (0°). There was a tendency for the posterior pelvic tilt to progress at an accelerated rate in patients older than 75 years. The posterior pelvic tilt progresses at an accelerated rate in the cases with femoral neck fracture (case A) and fragility fracture of the femoral head (case B).
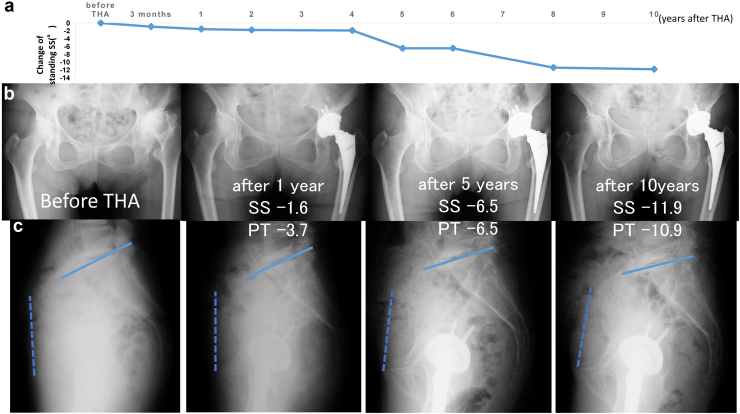
In the 12 patients aged 76 years or older (range, 77-95 years) at the last observation, the mean change of SS in standing position over the first year postoperatively was −1.8° ± 2.1° (−6.5° to −0.4°). The mean change between surgery and when they reached 75 years of age was −2.6° ± 2.7° (−7.5° to −0.5°). The mean change between surgery and the last observation was −8.0° ± 4.3° (−14.2° to −1.0°) (Fig. 6). To evaluate the average annual change in tilt, 3 phases were defined: phase 1, from preoperative stage to 1 year postoperatively; phase 2, from 1 year postoperatively to 75 years of age; and phase 3, from 75 years of age to the last observation. The mean annual change of SS in the standing position averaged −1.8° ± 2.1°/y (−6.5° to −0.4°) in phase 1; −0.2° ± 0.1°/y (−0.5° to 0) in phase 2; and −0.8° ± 0.5°/y (−1.7° to −0.1°) in phase 3 (Fig. 7). The annual change of the SS in the standing position was significantly greater in phase 1 (P = .012) and phase 3 (P = .015) than in phase 2. The posterior PT after THA progressed significantly in 2 phases, the early postoperative period and after the age of 75 years (Fig. 8).
Figure 6.
Longitudinal changes in pelvic sagittal inclination in the standing position (SS in the standing position) in patients older than 76 years at the last observation (N = 12). The preoperative value is used as the reference (0°). The average age at the last observation was 83 years.
Figure 7.
Annual change (acceleration) of posterior pelvic tilt in the standing position in patients older than 76 years at the last observation (N = 12). The average age at the last observation was 83 years. The annual change in the standing SS was significantly greater in phase 1 and phase 3 than in phase 2. ∗P < .05, ∗∗P = .272, Wilcoxon signed-rank test.
Figure 8.
A 71-year-old woman at the time of surgery with unilateral dysplastic hip arthropathy. Posterior pelvic tilt in the standing position progressed in the first year after THA and remained almost constant thereafter, but the posterior tilt rapidly progressed after 76 years of age, 5 years after surgery. By the age of 81 years, 10 years after surgery, the posterior pelvic tilt in the standing position was 11.9° in SS and 10.9° in PT. (a) Change of SS in the standing position. (b) AP radiographs of the pelvis in the standing position. (c) Lateral spinopelvic radiographs in the standing position. Line, S1 endplate line; dotted line, APP.
Posterior PT progressed rapidly after surgery in cases with femoral neck fracture or fragility fracture of the femoral head (Figure 5, Figure 9).
Figure 9.
A 78-year-old woman at the time of surgery with a fragility fracture of the femoral head. The pelvic sagittal inclination in the standing position temporarily tilted forward after THA, but the posterior pelvic tilt progressed drastically after 2 years. By the age of 89 years, 11 years after surgery, the posterior pelvic tilt in the standing position was 12.6° in SS and 16.0° in PT. (a) Change of SS in the standing position. (b) AP radiographs of the pelvis in the standing position. (c) Lateral spinopelvic radiographs in the standing position. Line, S1 endplate line; dotted line, APP.
Discussion
Previous studies [5,6] have suggested that pelvic sagittal inclination in the standing position after THA increases posteriorly over time. Suzuki et al. [6] reported that in 77 hips that underwent primary THA, age and a decrease in lumbo-lordotic angle were associated with the progression of posterior PT in the standing position over 5 years postoperatively. In addition, Kyo et al. [10] reported that in 124 patients who underwent primary THA, the mean change of pelvic sagittal inclination from the preoperative supine position to the standing position 1 year postoperatively was 9.5° posterior. The degree of posterior tilt was related to vertebral compression fractures, degenerative spondylolisthesis, and narrowing of the intervertebral disc space, indicating a relationship between posterior PT in the standing position and lumbar alignment.
On the other hand, it has been reported that spinopelvic alignment, so-called spinopelvic harmony, breaks down with age [15,16]. Yukawa et al. [17] reported in a cross-sectional study of healthy Asians that spinopelvic alignment begins to fail rapidly after the age of 70 years, and the pelvis begins to tilt posteriorly. Although there are no reports on differences in changes of spinopelvic alignment between normal subjects and those with hip deformities, in this study, the posterior PT after THA tended to progress significantly during 2 phases, the early postoperative period and after the age of 75 years. The latter phase generally coincided with the period when spinopelvic harmony is said to be disrupted. This suggests a relationship between the accelerating progression of posterior PT after 75 years of age and the disruption of spinopelvic harmony. It is difficult to prevent the progression of posterior PT after THA, and we believe that long-term systemic care after THA, including osteoporosis treatment and exercise therapy for postural maintenance, is important to prevent osteoporotic vertebral compression fractures and spinal deformities due to age-related degeneration, which have been suggested to be associated with the progression of posterior PT.
Miki et al. [9] reported that it is difficult to avoid edge loading and impingement when posterior PT increases by more than 20° postoperatively. Abdel [18] stated that the use of a dual mobility system is effective in patients with a high risk of postoperative dislocation due to spinal deformity. In this study, patients aged 75 years or older and patients with fragility fractures tended to have a greater postoperative progression of posterior PT, suggesting that the use of a large head or dual mobility system in THA should be considered.
The limitation of this study is that it does not include an evaluation of spinal alignment, such as lumbo-lordotic angle. The main reasons for this are that the L1 upper-end plate was not included in the imaging range of lateral spinopelvic radiographs in the standing position at each follow-up, and sagittal radiographs of the entire spine often were not taken at each follow-up, making it impossible to evaluate changes over time. However, the findings that posterior PT after THA tended to progress significantly in 2 phases, during early postoperative period and after the age of 75 years, are significant in terms of predicting changes in tilt with aging after THA. It is important to understand that preoperative planning and postoperative care must consider not only the patient's condition at the time of surgery but also long-term postoperative changes as the patient ages.
Conclusions
The rate of progression of posterior PT in the standing position after THA was not constant and tended to be faster in the early postoperative period and in patients older than 75 years. The postoperative progression of posterior PT tended to be greater in patients aged 75 years or older and in patients with fragility fractures, suggesting that the use of a large head or dual mobility system should be considered. To prevent osteoporotic vertebral compression fracture and degenerative spinal deformity, long-term systemic care after THA surgery, including osteoporosis treatment and exercise therapy to maintain posture, is important.
Conflicts of interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: T. Nakamura is in the speakers' bureau of or gave paid presentations for Zimmer Biomet, Kyocera, DePuy, and Smith & Nephew; is a paid consultant for Zimmer Biomet; and is a board member of the Japanese Hip Society. The other authors declare no potential conflicts of interests.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2022.03.021.
Appendix A. Supplementary data
References
- 1.Ike H., Dorr L.D., Trasolini N., et al. Spine-pelvis hip relationship in the functioning of a total hip replacement. J Bone Joint Surg Am. 2018;100:1606–1615. doi: 10.2106/JBJS.17.00403. [DOI] [PubMed] [Google Scholar]
- 2.Luthringer T.A., Vigdorchik J.M. A preoperative workup of a “Hip-Spine” total hip arthroplasty patient: a simplified approach to a complex problem. J Arthroplasty. 2019;34:S57–S70. doi: 10.1016/j.arth.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 3.Eftekhary N., Shimmin A., Lazennec J.Y., et al. A systematic approach to the hip-spine relationship and its applications to total hip arthroplasty. Bone Joint J. 2019;101-B:808–816. doi: 10.1302/0301-620X.101B7.BJJ-2018-1188.R1. [DOI] [PubMed] [Google Scholar]
- 4.Tezuka T., Heckmann N.D., Bodner R.J., et al. Functional safe zone is superior to the Lewinnek safe zone for total hip arthroplasty: why the Lewinnek safe zone is not always predictive of stability. J Arthroplasty. 2019;34:3–8. doi: 10.1016/j.arth.2018.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Tamura S., Nishihara S., Takao M., et al. Does pelvic sagittal inclination in the supine and standing positions change over 10 years of follow-up after total hip arthroplasty? J Arthroplasty. 2017;32:877–882. doi: 10.1016/j.arth.2016.08.035. [DOI] [PubMed] [Google Scholar]
- 6.Suzuki H., Inaba Y., Kobayashi N., et al. Postural and chronological change in pelvic tilt five years after total hip arthroplasty in patient with developmental dysplasia of the hip: a Three-dimensional analysis. J Arthroplasty. 2016;31:317–322. doi: 10.1016/j.arth.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 7.Lembeck B., Mueller O., Reize P., et al. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76(4):517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 8.Ishida T., Inaba Y., Kobayashi N., et al. Changes in pelvic tilt following total hip arthroplasty. J Orthop Sci. 2011;16:682–688. doi: 10.1007/s00776-011-0153-0. [DOI] [PubMed] [Google Scholar]
- 9.Miki H., Kyo T., Kuroda Y., et al. Risk of edge-loading and prosthesis impingement due to posterior pelvic tilting after total hip arthroplasty. Clin Biomech. 2014;29:607–613. doi: 10.1016/j.clinbiomech.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Kyo T., Nakahara I., Miki H. Factors predicting change in pelvic posterior tilt after THA. Orthopedics. 2013;36(6):753–759. doi: 10.3928/01477447-20130523-20. [DOI] [PubMed] [Google Scholar]
- 11.Tiberi J.V., Antoci V., Malchau H., et al. What is the fate of total hip arthroplasty (THA) acetabular component orientation when evaluated in the standing position? J Arthroplasty. 2015;30:1555–1560. doi: 10.1016/j.arth.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 12.DiGioia A.M., Hafez M.A., Jaramaz B., et al. Functional pelvic orientation measured from lateral standing and sitting radiographs. Clin Orthop Relat Res. 2006;453:272–276. doi: 10.1097/01.blo.0000238862.92356.45. [DOI] [PubMed] [Google Scholar]
- 13.Blondel B., Parratte S., Tropiano P., et al. Pelvic tilt measurement before and after total hip arthroplasty. Orthop Traumatol Surg Res. 2009;95:568–572. doi: 10.1016/j.otsr.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 14.Maratt J.D., Esposito C.I., McLawhorn A.S., et al. Pelvic tilt in patients undergoing total hip arthroplasty: when does it matter? J Arthroplasty. 2015;30:387–391. doi: 10.1016/j.arth.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwab F., Lafage V., Boyce R., et al. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine. 2006;31:E959–E967. doi: 10.1097/01.brs.0000248126.96737.0f. [DOI] [PubMed] [Google Scholar]
- 16.Schwab F., Patel A., Unger B., et al. Adult spinal deformity-Postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing aliment and planning corrective surgery. Spine. 2010;35(25):2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 17.Yukawa Y., Kato F., Suda K., et al. Sagittal spinal alignment in healthy subjects -Gender difference and changes with aging. J Spine Res. 2016;7:11–15. doi: 10.1007/s00586-016-4807-7. (in Japanese) [DOI] [PubMed] [Google Scholar]
- 18.Abdel M.P. Simplifying the hip-spine relationship for total hip arthroplasty : when do I use Dual-mobility and why does it work? J Arthroplasty. 2019;34:S74–S75. doi: 10.1016/j.arth.2019.01.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.