Abstract
Background:
Scientific research increasingly focuses on visual symptoms of people with Parkinson’s disease (PD). However, this mostly involves functional measures, whereas self-reported data are equally important for guiding clinical care.
Objective:
This review provides an overview of the nature and prevalence of self-reported visual complaints by people with PD, compared to healthy controls.
Methods:
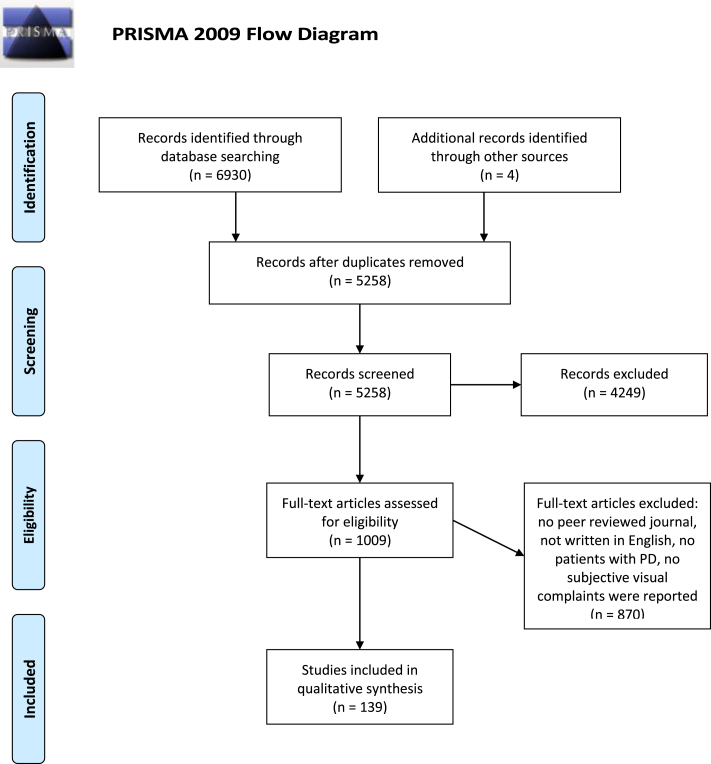
A systematic literature search was performed. Studies from three databases (PubMed, PsycInfo, and Web of Science) were screened for eligibility. Only studies that reported results of visual self-reports in people with idiopathic PD were included.
Results:
One hundred and thirty-nine eligible articles were analyzed. Visual complaints ranged from function-related complaints (e.g., blurred vision, double vision, increased sensitivity to light or changes in contrast sensitivity) to activity-related complaints (e.g., difficulty reading, reaching, or driving). Visual complaints were more prevalent in people with PD compared to healthy controls. The presence of visual complaints leads to a reduced quality of life (QoL). Increased prevalence and severity of visual complaints in people with PD are related to longer disease duration, higher disease severity, and off-state.
Conclusion:
A large proportion of people with PD have visual complaints, which negatively affect QoL. Complaints are diverse in nature, and specific and active questioning by clinicians is advised to foster timely recognition, acknowledgement, and management of these complaints.
Keywords: Activities of daily living, Parkinson’s disease, quality of life, self report, systematic review, vision disorders
INTRODUCTION
Parkinson’s disease (PD) is a neurodegenerative disorder characterized by a number of well-known motor and non-motor symptoms, including visual problems [1–5]. During recent years, visual symptoms in PD have received increasing attention in the literature. In clinical practice however, these symptoms are still underrecognized. Visual symptoms are less conspicuous than motor symptoms, and may therefore be overlooked [6, 7]. However, visual symptoms have a substantial impact on the daily lives of people with PD and may already occur in the early and prodromal stages of the disease [1, 4, 8]. Consequently, several studies state the importance of tools to improve the recognition, diagnostic accuracy, and management of non-motor symptoms, including visual symptoms, in clinical practice [2, 9–11].
To date, most tools used to assess visual symptoms are quantitative tests of visual functions. These measurements, in most cases part of an ophthalmological assessment, objectify functions and impairments, such as visual acuity and visual field loss. In contrast, few studies include self-report data, asking people to reflect on their own visual functioning. It is acknowledged that both functional and self-reported data are required to obtain a clear picture of the impact of PD on individuals [9], which is necessary to guide care and rehabilitation [12, 13].
Despite the importance of self-reported data, no reviews have been published on this topic so far. Therefore, this paper presents a systematic review on self-reported visual complaints in PD, compared to healthy controls.
METHODS
Literature search
A literature search was performed according to the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [14]. The search encompassed the scientific databases PsycInfo, PubMed, and Web of Science (Core Collection) and was performed on literature up to the date of February 5, 2021. The search terms are presented in Table 1. Two complementary searches were performed. The first one focused on subjective dysfunction in general, since the current review was part of a project that also examined self-reported cognitive complaints of people with PD. The second search addressed self-reported visual complaints specifically.
Table 1.
Search terms for literature search
| Search 1 | Terms used in all databases | MeSH and thesaurus terms used in PubMed or PsycInfo |
| First criterion | parkinson*a | PubMed: “Parkinson Disease”; PsycInfo: “Parkinson’s Disease” |
| Second criterion | “self report”, complaint*, “subjective assessment*”, “subjective measure*”, “subjective problem*”, “subjective dysfunction*”, “subjective deficit*”, “subjective impairment*”, “subjective symptom*”, “report a problem”, “report problem*”, “report a dysfunction”, “report dysfunction*”, “report a deficit”, “report deficit*”, “report an impairment”, “report impairment*”, “report a symptom”, “report symptom*”, “reports a problem”, “reports problem*”, “reports a dysfunction”, “reports dysfunction*”, “reports a deficit”, “reports deficit*”, “reports an impairment”, “reports impairment*”, “reports a symptom”, “reports symptom*”, “reported a problem”, “reported problem*”, “reported a dysfunction”, “reported dysfunction*”, “reported a deficit”, “reported deficit*”, “reported an impairment”, “reported impairment*”, “reported a symptom”, “reported symptom*”, “perceive a problem”, “perceive problem*”, “perceive a dysfunction”, “perceive dysfunction*”, “perceive a deficit”, “perceive deficit*”, “perceive an impairment”, “perceive impairment*”, “perceive a symptom”, “perceive symptom*”, “perceives a problem”, “perceives problem*”, “perceives a dysfunction”, “perceives dysfunction*”, “perceives a deficit”, “perceives deficit*”, “perceives an impairment”, “perceives impairment*”, “perceives a symptom”, “perceives symptom*”, “perceived a problem”, “perceived problem*”, “perceived a dysfunction”, “perceived dysfunction*”, “perceived a deficit”, “perceived deficit*”, “perceived an impairment”, “perceived impairment*”, “perceived a symptom”, “perceived symptom*”, “experience a problem”, “experience problem*”, “experience a dysfunction”, “experience dysfunction*”, “experience a deficit”, “experience deficit*”, “experience an impairment”, “experience impairment*”, “experience a symptom”, “experience symptom*”, “experiences a problem”, “experiences problem*”, “experiences a dysfunction”, “experiences dysfunction*”, “experiences a deficit”, “experiences deficit*”, “experiences an impairment”, “experiences impairment*”, “experiences a symptom”, “experiences symptom*”, “experienced a problem”, “experienced problem*”, “experienced a dysfunction”, “experienced dysfunction*”, “experienced a deficit”, “experienced deficit*”, “experienced an impairment”, “experienced impairment*”, “experienced a symptom”, “experienced symptom*”b | Pubmed: “Self Report”; PsycInfo: “Self Report”, “Self-Report” |
| Search 2 | Terms used in all databases | MeSH and thesaurus terms used in PubMed or PsycInfo |
| First criterion | parkinson*a | PubMed: “Parkinson Disease”; PsycInfo: “Parkinson’s Disease” |
| Second criterion | questionnaire*, scale*, survey*, inventor*, interview*b | PubMed: “Surveys and Questionnaires”, “Interview, Psychological”; PsycInfo: Questionnaires, Interviews, Surveys, Inventories |
| Third criterion | seeing OR eyesight OR sight OR ophthalmologic* OR “visual perception” OR “visual acuity” OR “visual field*” OR diplopia OR “double vision” OR “depth perception” OR “color vision” OR “colour vision” OR “color perception” OR “colour perception” OR “contrast sensitivity” OR “visual contrast” OR “brightness perception” OR “light sensitivity” OR “sensitive to light” OR “sensitivity to light” OR “oversensitive to light” OR “oversensitivity to light” OR photophobia OR photosensitivity OR glare OR “dark adaptation” OR “visual overload” OR “problems reading” OR “reading problem*” OR “difficulty reading” OR “reading difficult*” OR “painful eyes” OR “dry eyes” OR “eyelid opening” OR blink* OR “facial recognition” OR “face recognition” OR “face perception” OR “object recognition” OR “object perception” OR “figure perception” OR “form perception” OR “shape perception” OR “motion perception” OR “space perception” OR “spatial perception” OR “spatial orientation” OR “spatial disorientation” OR afterimage* OR “visual discrimination” OR “figure ground discrimination” OR “nonmotor symptom*” OR “non-motor symptom*” OR “autonomic dysfunction*” OR “autonomic symptom*” OR “autonomous dysfunction” OR “autonomous symptom*”b | PubMed: “Visual Perception”, “Vision disorders”, “Vision screening”, “Depth Perception”, “Color vision”; PsycInfo: “Visual perception”, “Vision disorders”, “Diplopia”, “Depth perception”, “Color perception”, “Brightness perception”, “Dark adaptation”, “Face perception”, “Visual acuity”, “Visual contrast”, “Visual discrimination”, “Visual field”, “Figure ground discrimination” |
aTerm should be present in title or abstract, bOne of the terms should be present in the content of the paper.
Eligibility criteria
Only papers fulfilling the following criteria were included: written in English, published in peer-reviewed academic journals, including human participants with idiopathic PD, including a self-report measure for visual functioning, and data (i.e., prevalence) of this measure for the group of people with PD or a comparison (i.e., prevalence or score) with healthy controls. Visual self-report measures were defined as items, subscales or total scores representing an individual’s reflection on their own visual functioning, performance of visual activities or vision-related quality of life (QoL). We made the assumption that a self-report measure was filled out by the patient, unless otherwise stated. Longitudinal or intervention studies were included if relevant baseline measures were presented. Review articles and case reports were excluded, as well as meeting abstracts and letters to editors. Since visual hallucinations in PD are widely recognized and extensively studied [15], these were not incorporated in this review.
Literature extraction
Figure 1 shows the PRISMA outline of papers identified through the literature search. Articles were first screened by title and abstract, and when they seemed relevant, reviewed by the full text. In addition to the database search, reference lists of included papers were screened according to the predefined inclusion criteria. Two authors (IvdL and FH) and a research assistant (EV) systematically judged the eligibility of articles and discussed this in case of doubt. In case uncertainty remained, a third author (GdH) was involved until consensus was reached.
Fig. 1.
PRISMA flow diagram of systematic literature search [14].
Analysis
Relevant results were extracted from included papers. Results were categorized per complaint. Complaints were divided amongst three categories: function-related complaints, activity-related complaints, and vision-related QoL. Results were ordered based on the number of studies investigating each complaint. Based on this systematic categorization, a descriptive table was included (Table 2). If data on subgroups of PD were reported (e.g., tremor dominant versus akinetic-rigidity subtypes, or young versus late onset PD), but no total prevalence, it was calculated by the authors. The weighted prevalence of a complaint was calculated for studies using the same method to assess the complaint. Relationships of self-reported visual complaints with demographics and disease-related variables were gathered in an additional table (Table 3).
Table 2.
Overview of the prevalence of visual complaints in people with PD and the comparison to healthy controls
| Items covering complaint (N) | Criterion presence complaint | Studies (N) | PD patients (N) | Prevalence PD patients (%) | Controls (N) | Prevalence controls (%) | Studies PD > Controlsa (N) | Studies PD = Controls or PD < Controlsa (N) | |
| Function-related visual complaints | |||||||||
| Visual complaints in general | 17 | 2337 | 26.8 – 98 | 29344 | 16.1 – 31.6 | 6 | 0 | ||
| CIRS-G | 1 | ≥1 on a 0 (‘no problem’) – 4 (‘extremely severe’) scale | 1 [19] | 76 | 98 | N/A | N/A | N/A | N/A |
| VFQ-25 | 25 | At least one complaint | 3 [18, 25, 26] | 145 | 83.1 [25, 26] | 466 | 31.6 [25] | 3 | 0 |
| Direct asking of the patient according to ICF checklist | 2 | ≥1 (‘mild difficulty’) on a 0 – 4 scale | 1 [27] | 96 | 75.5b | N/A | N/A | N/A | N/A |
| Interview on autonomic dysfunction | 4 | N/A | 1 [20] | 26 | 67 | 27 | 22 | 1 | 0 |
| Questionnaire on visual complaints (20-item) | N/A | N/A | 1 [16] | 30 | 63.3 | 31 | 29.0 | 1 | 0 |
| PRO-PD | 1 | ≥5 on a 0 (‘lack of symptom’) – 100 (‘maximum severity’) scale | 1 [32] | 1031 | 58.0 | N/A | N/A | N/A | N/A |
| Self-report questionnaire (31-item) | N/A | At least one complaint | 1 [17] | 81 | 78c | N/A | N/A | N/A | N/A |
| Survey of Health, Ageing, and Retirement in Europe | 1 | ≥4 on a 1 (‘excellent’) – 5 (‘poor’) scale | 1 [21] | 191 | 46.1 | 28820 | 16.1 | 1 | 0 |
| Interview using a questionnaire on non-motor symptoms [30] | 1 | ‘yes’ | 2 [22, 30] | 76 | 46.1 | N/A | N/A | N/A | N/A |
| Symptom questionnaire | 1 | ‘yes’ | 1 [28] | 39 | 43.6 | N/A | N/A | N/A | N/A |
| Question: are you bothered due to vision-related problems? | 1 | N/A | 1 [23] | 295 | 41 | N/A | N/A | N/A | N/A |
| Structured interview | N/A | N/A | 1 [29] | 108 | 40.7 | N/A | N/A | N/A | N/A |
| Symptom index (20-item) | 1 | ‘yes’ | 1 [31] | 61 | 36.1 | N/A | N/A | N/A | N/A |
| Questions on visual complaints | N/A | N/A | 1 [24] | 82 | 26.8 | N/A | N/A | N/A | N/A |
| Double vision | 96 | 20994 | 7.7 – 53.1 | 1556 | 2.4 – 19.0 | 15 | 3 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 2 [118, 119] | 237 | 53.1 | 100 | 19.0 | 2 | 0 |
| Self-report questionnaire (31-item) | 1 | ‘sometimes’ or ‘often’ | 1 [17] | 81 | 38.0 | N/A | N/A | N/A | N/A |
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 22 | 250 | 3 | 1 | 0 |
| Questionnaire derived from VFQ-25 | N/A | N/A | 2 [25, 116] | 178 | 19.8 | 122 | 2.4 | 2 | 0 |
| Non-motor fluctuations questionnaire | 1 | N/A | 1 [159] | 11 | 18.2 | N/A | N/A | N/A | N/A |
| NMSQ | 1 | ≥1 (‘yes’) | 61 [33– 93] | 11511 | 13.9d | 690 | 3.5 [40, 47, 48, 56, 57, 59, 91, 92] | 6 [47, 48, 56, 57, 59, 91] | 2 [40, 92] |
| NMSS | 1 | ≥1 (‘mild’) on a 0 (‘none’) – 3 (‘severe’) scale | 24 [9, 41, 94– 115] | 7545 | 14.2 [9, 41, 94, 96– 107, 109– 115] | 363 | 2.4 94, 96] | 3 [95, 96, 108] | 1 [94] |
| Online symptom survey | 1 | ‘yes’ | 1 [160] | 432 | 12.7 | N/A | N/A | N/A | N/A |
| Questionnaire on visual complaints (20-item) | N/A | N/A | 1 [16] | 30 | 10.0 | 31 | 3.2 | 1 | 0 |
| Questions on visual complaints | N/A | N/A | 1 [24] | 82 | 9.8 | N/A | N/A | N/A | N/A |
| Questions on asthenopia | N/A | N/A | 1 [152] | 39 | 7.7 | N/A | N/A | N/A | N/A |
| Increased sensitivity to light | 27 | 6318 | 15.0 – 48 | 1480 | 0 – 28.3 | 13 | 2 | ||
| Interview on autonomic dysfunction | 1 | N/A | 1 [20] | 26 | 48 | N/A | N/A | N/A | N/A |
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 43 | 250 | 23 | 1 | 0 |
| ADS (autonomic dysfunction score) | 1 | N/A | 1 [140] | 21 | 38.1 | 27 | 0 | 1 | 0 |
| SCOPA-AUT | 1 | ≥1 (‘sometimes’) on a 0 (‘never’) – 3 (‘often’) scale | 19 [120– 138] | 5195 | 31.8 [120, 122, 124– 130, 132– 138] | 1044 | 28.3 [120, 128– 130, 132, 138] | 8 [120, 121, 123, 128– 130, 132, 138] | 1 [131] |
| COMPASS-31 | 5 | N/A | 1 [161] | 47 | 27.7 | N/A | N/A | N/A | N/A |
| Questionnaire derived from VFQ-25 | N/A | N/A | 1 [25] | 88 | 23.9 | 90 | 11.8 | 1 | 0 |
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 1 [119] | 53 | 15 | 31 | 3 | 1 | 0 |
| VAQ | 3 | N/A | 1 [142] | 25 | N/A | 23 | N/A | 0 | 1 |
| COMPASS | 7 | N/A | 1 [139] | 15 | N/A | 15 | N/A | 1 | 0 |
| Altered color vision | 9 | 1394 | 4.1 – 12.7 | 894 | 3 – 10 | 4 | 4 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 2 [118, 119] | 237 | 12.7 | 100 | 4.4 | 1 [118] | 1 [119] |
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 11 | 250 | 3 | 1 | 0 |
| Questions on visual complaints | N/A | N/A | 1 [24] | 82 | 6.1 | N/A | N/A | N/A | N/A |
| Interview on prodromal symptoms | 1 | ‘yes’ | 2 [141, 143] | 145 | 4.1 | 145 | 10 | 0 | 2 |
| VFQ-25 | 1 | N/A | 2 [18, 26] | 57 | N/A | 376 | N/A | 2 | 0 |
| VAQ | 3 | N/A | 1 [142] | 25 | N/A | 23 | N/A | 0 | 1 |
| Painful/dry eyes | 9 | 1706 | 6.1 – 87.5 | 850 | 8 – 22.4 | 5 | 1 | ||
| Dry eye symptom assessment | ‘various’ | ≥2-3 times a week (‘occasionally’) | 1 [144] | 56 | 87.5 | 34 | 20.6 | 1 | 0 |
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 28 | 250 | 8 | 1 | 0 |
| Question on dry eye | 1 | N/A | 1 [162] | 43 | 44.2 | N/A | N/A | N/A | N/A |
| VFQ-25 | 2 | N/A | 3 [18, 25, 26] | 145 | 27.3 [25] | 466 | 22.4 [25] | 2 [18, 25] | 1 [26] |
| Online symptom survey (dry eyes) | 1 | ‘yes’ | 1 [160] | 432 | 25.7 | N/A | N/A | N/A | N/A |
| Questions on visual complaints | N/A | N/A | 1 [24] | 82 | 6.1 | N/A | N/A | N/A | N/A |
| OSDI | 12 | N/A | 1 [145] | 100 | N/A | 100 | N/A | 1 | 0 |
| Blurred vision | 6 | 1695 | 19.7 – 46 | 630 | 7.4 – 19.0 | 4 | 0 | ||
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 46 | 250 | 12 | 1 | 0 |
| Symptom questionnaire | 1 | ‘yes’ | 1 [146] | 181 | 36.2 | 263 | 19.0 | 1 | 0 |
| ADS (autonomic dysfunction score) | 1 | N/A | 1 [140] | 21 | 28.6 | 27 | 7.4 | 1 | 0 |
| Interview on visual symptoms | 1 | ‘yes’ | 1 [111] | 125 | 20 | N/A | N/A | N/A | N/A |
| Online symptom survey | 1 | ‘yes’ | 1 [160] | 432 | 19.7 | N/A | N/A | N/A | N/A |
| Questionnaire derived from VFQ-25 | N/A | N/A | 1 [25] | 88 | N/A | 90 | N/A | 1 | 0 |
| Changes in contrast sensitivity | 3 | 1157 | 8.8 – 27 | 319 | 10 – 13 | 2 | 0 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 1 [118] | 184 | 27 | 69 | 13 | 1 | 0 |
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 26 | 250 | 10 | 1 | 0 |
| Interview on visual symptoms | 1 | ‘yes’ | 1 [111] | 125 | 8.8 | N/A | N/A | N/A | N/A |
| Changes in size and shape perception | 3 | 982 | 3.7 – 19 | 281 | 5 – 13 | 2 | 0 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 1 [119] | 53 | 19g | 31 | 13 | 1 | 0 |
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 17 | 250 | 5 | 1 | 0 |
| Questions on visual complaints | N/A | N/A | 1 [24] | 82 | 3.7 | N/A | N/A | N/A | N/A |
| Changes in depth perception | 3 | 926 | 17 – 26 | 304 | 2 – 6 | 3 | 1 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 1 [119] | 53 | 26 | 31 | 6 | 1 | 0 |
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 17 | 250 | 2 | 1 | 0 |
| VAQ | 3 | N/A | 1 [142] | 25 | N/A | 23 | N/A | 1e | 1f |
| Reduced peripheral vision | 3 | 82 | N/A | 399 | N/A | 3 | 1 | ||
| VFQ-25 | 1 | N/A | 2 [18, 26] | 57 | N/A | 376 | N/A | 2 | 0 |
| VAQ | 5 | N/A | 1 [142] | 25 | N/A | 23 | N/A | 1e | 1f |
| Difficulty estimating spatial relations | 3 | 390 | 6.4 – 50 | 69 | 28 | 1 | 0 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 1 [118] | 184 | 50 | 69 | 28 | 1 | 0 |
| Self-report questionnaire (31-item) | 1 | ‘sometimes’ or ‘often’ | 1 [17] | 81 | 45.0 | N/A | N/A | N/A | N/A |
| Interview on visual symptoms | 1 | ‘yes’ | 1 [111] | 125 | 6.4 | N/A | N/A | N/A | N/A |
| Visual field impairment | 2 | 930 | 6.1 – 9 | 250 | 2 | 1 | 0 | ||
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 9 | 250 | 2 | 1 | 0 |
| Questions on visual complaints | N/A | N/A | 1 [24] | 82 | 6.1 | N/A | N/A | N/A | N/A |
| Watery eyes | 2 | 930 | 26.8 – 31 | 250 | 15 | 1 | 0 | ||
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 31 | 250 | 15 | 1 | 0 |
| Questions on visual complaints | N/A | N/A | 1 [24] | 82 | 26.8 | N/A | N/A | N/A | N/A |
| Changes in motion perception | 2 | 237 | 23.7 | 100 | 3 | 2 | 0 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 2 [118, 119] | 237 | 23.7 | 100 | 3 | 2 | 0 |
| Reduced night vision | 2 | 869 | 16 – 47.6 | 277 | 3 – 18.5 | 2 | 0 | ||
| ADS (autonomic dysfunction score) | 1 | N/A | 1 [140] | 21 | 47.6 | 27 | 18.5 | 1 | 0 |
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 16 | 250 | 3 | 1 | 0 |
| Reduced light/dark adaptation | 2 | 873 | 27 | 273 | 11 | 2 | 1 | ||
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 27 | 250 | 11 | 1 | 0 |
| VAQ | 4 | N/A | 1 [142] | 25 | N/A | 23 | N/A | 1e | 1f |
| Floaters | 2 | 178 | N/A | 122 | N/A | 0 | 2 | ||
| Questionnaire derived from VFQ-25 | N/A | N/A | 2 [25, 116] | 178 | N/A | 122 | N/A | 0 | 2 |
| Misjudge objects | 2 | 178 | N/A | 122 | N/A | 2 | 0 | ||
| Questionnaire derived from VFQ-25 | N/A | N/A | 2 [25, 116] | 178 | N/A | 122 | N/A | 2 | 0 |
| Asthenopia (ocular fatigue) | 1 | 39 | 43.6 | 39 | 5.1 | 1 | 0 | ||
| Questions on asthenopia | N/A | Presence of visual discomfort, diplopia, blurred vision or headache when reading | 1 [152] | 39 | 43.6 | 39 | 5.1 | 1 | 0 |
| Hard to follow quick movements with the eyes | 1 | 848 | 25 | 250 | 4 | 1 | 0 | ||
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 25 | 250 | 4 | 1 | 0 |
| Need to turn head to side to see peripheral objects | 1 | 53 | 43 | 31 | 14 | 1 | 0 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 1 [119] | 53 | 43 | 31 | 14 | 1 | 0 |
| Mucus/slime or particles in eyes or eyelids | 1 | 848 | 20 | 250 | 6 | 1 | 0 | ||
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 20 | 250 | 6 | 1 | 0 |
| Reduced acuity/spatial vision | 1 | 25 | N/A | 23 | N/A | 1 | 1 | ||
| VAQ | 4 | N/A | 1 [142] | 25 | N/A | 23 | N/A | 1e | 1f |
| Reduced visual processing speed | 1 | 25 | N/A | 23 | N/A | 1 | 1 | ||
| VAQ | 6 | N/A | 1 [142] | 25 | N/A | 23 | N/A | 1e | 1f |
| Reduced visual search | 1 | 25 | N/A | 23 | N/A | 0 | 1 | ||
| VAQ | 5 | N/A | 1 [142] | 25 | N/A | 23 | N/A | 0 | 1 |
| Activity-related visual complaints | |||||||||
| Reading difficulties | 6 | 1176 | 18.3 – 42.0 | 403 | 5.6 – 9.7 | 4 | 0 | ||
| Self-report questionnaire (31-item) | N/A | N/A | 1 [17] | 81 | 42.0 | N/A | N/A | N/A | N/A |
| Questionnaire on visual complaints (20-item) | N/A | N/A | 1 [16] | 30 | 26.7 | 31 | 9.7 | 1 | 0 |
| Questions on asthenopia | N/A | N/A | 1 [152] | 39 | 23.1 | N/A | N/A | N/A | N/A |
| VIPD-Q | 1 | ≥2 (‘weekly’) on a 0 (‘never’) – 3 (‘daily’) scale | 1 [117] | 848 | 18.3h | 250 | 5.6h | 1 | 0 |
| Questionnaire derived from VFQ-25 | N/A | N/A | 2 [25, 116] | 178 | N/A | 122 | N/A | 2 | 0 |
| Near activities | 5 | 1875 | 34.5 – 44.3 | 114558 | 9.7 – 25.5 | 5 | 0 | ||
| Survey of Health, Ageing, and Retirement in Europe | 1 | ≥4 on a 1 (‘excellent’) – 5 (‘poor’) scale | 1 [21] | 1438 | 44.3 | 113802 | 25.5 | 1 | 0 |
| CISS | 14 | ≥21 | 2 [147, 148] | 380 | 34.5 | 380 | 9.7 | 2 | 0 |
| VFQ-25 | 3 | N/A | 2 [18, 26] | 57 | N/A | 376 | N/A | 2 | 0 |
| Difficulty/freezing in narrow spaces | 4 | 415 | 67.3 | 222 | 1.6 | 4 | 0 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 2 [118, 119] | 237 | 67.3i | 100 | 1.6i | 2 | 0 |
| Questionnaire derived from VFQ-25 | N/A | N/A | 2 [25, 116] | 178 | N/A | 122 | N/A | 2 | 0 |
| Distance activities | 3 | 1495 | 38.6 | 114178 | 15.0 | 3 | 0 | ||
| Survey of Health, Ageing, and Retirement in Europe | 1 | ≥4 on a 1 (‘excellent’) – 5 (‘poor’) scale | 1 [21] | 1438 | 38.6 | 113802 | 15.0 | 1 | 0 |
| VFQ-25 | 3 | N/A | 2 [18, 26] | 57 | N/A | 376 | N/A | 2 | 0 |
| Driving | 3 | 94 | 21.6 | 355 | 2.7 | 3 | 0 | ||
| VFQ-25 | 2 | N/A | 2 [18, 26] | 57 | N/A | 318 | N/A | 2 | 0 |
| Self-report driving questionnaire derived from Charlton et al. (2006) [163] | N/A | ‘very difficult’ in low visibility conditions | 1 [149] | 37 | 21.6 | 37 | 2.7 | 1 | 0 |
| Difficulty reaching for objects | 1 | 184 | 46 | 69 | 3 | 1 | 0 | ||
| Questionnaire on changes in vision | 1 | ‘sometimes’ or ‘often’ | 1 [118] | 184 | 46 | 69 | 3 | 1 | 0 |
| Problems with visual ADLs | 1 | 25 | N/A | 23 | N/A | 1 | 1 | ||
| VAQ | 33 | N/A | 1 [142] | 25 | N/A | 23 | N/A | 1e | 1f |
| Vision-related QoL | |||||||||
| Vision-specific social functioning | 2 | 57 | N/A | 376 | N/A | 2 | 0 | ||
| VFQ-25 | 2 | N/A | 2 [18, 26] | 57 | N/A | 376 | N/A | 2 | 0 |
| Vision-specific role difficulties | 2 | 57 | N/A | 376 | N/A | 1 | 1 | ||
| VFQ-25 | 2 | N/A | 2 [18, 26] | 57 | N/A | 376 | N/A | 1 [18] | 1 [26] |
| Vision-specific dependency | 2 | 57 | N/A | 376 | N/A | 2 | 0 | ||
| VFQ-25 | 3 | N/A | 2 [18, 26] | 57 | N/A | 376 | N/A | 2 | 0 |
| Vision-specific mental health | 2 | 57 | N/A | 376 | N/A | 2 | 0 | ||
| VFQ-25 | 4 | N/A | 2 [18, 26] | 57 | N/A | 376 | N/A | 2 | 0 |
Per complaint, each self-report measure used to describe this complaint is presented individually, along with the number of visual items it includes and the criterion that must be fulfilled for people to belong to the group with visual complaints. Weighted averages (prevalence of visual complaints) are presented for each complaint. References to the studies are placed in brackets []. ADLs, activities of daily living; CIRS-G, Cumulative Illness Rating Scale-Geriatric; CISS, Convergence Insufficiency Symptom Survey; COMPASS, Composite Autonomic Symptom Score; ICF, International Classification of Functioning; N, number/population size; N/A, not available; NMSQ, Non-Motor Symptoms Questionnaire, NMSS = Non-Motor Symptom Scale, OSDI = Ocular Surface Disease Index, PD = Parkinson’s disease, PRO-PD = Patient Reported outcomes in Parkinson’s Disease; QoL, quality of life; SCOPA-AUT, SCales for Outcomes in PArkinson’s disease– autonomic dysfunction; VAQ, Visual Activities Questionnaire; VFQ-25, Visual Function Questionnaire (25-item); VIPD-Q, Visual Impairment in Parkinson’s Disease Questionnaire. a Difference in score or prevalence between the groups, b Weighted prevalence of complaints on the ICF functions ‘seeing functions’ (72.9%) and ‘difficulty with watching’ (78.2%), c Items that may to some extent have arisen from motor symptoms (e.g., bumping into objects and freezing in narrow spaces) were included in the analysis. Prevalence was 57% after removing these items, dKhedr et al. (2012) [90] & Khedr et al. (2013) [55], and Giorelli et al. (2014) [65] & Giorelli et al. (2014) [66] used the same group of people with PD and reported the same results. For this reason, results of only one of these studies was reported, e Results only account for the non-tremor group (N = 12), f Results only account for the tremor group (N = 13), g Weighted prevalence of complaints on size (17%) and shape perception (21%), h Weighted prevalence of reading related complaints: ‘letters disappear while reading’ (20% in patients and 5% in controls) and ‘read better with one eye closed’ (17% in patients and 6% in controls), iWeighted prevalence of the complaints freezing (60% in patients and 3% in controls) and difficulty at doorways (56% in patients and 3% in controls) [119].
Table 3.
Relationship of demographic and disease-related variables with visual complaints
| Visual complaint | Significant positive relationship | Significant negative relationship | No significant relationship | |
| Demographic or disease-related variable | ||||
| 1. Age | Studies (N) | 1 | 0 | 3 |
| Double vision | 0 | 0 | 2 [66, 111] | |
| Increased sensitivity to light | 0 | 0 | 1 [122] | |
| Reduced visual health status | 1 [26] | 0 | 0 | |
| 2. Gender (+men > women) | Studies (N) | 1 | 0 | 12 |
| Visual complaints in general | 0 | 0 | 1 [117] | |
| Double vision | 0 | 0 | 10 [34, 50, 66, 67, 72, 75, 97, 103, 105, 111 | |
| Increased sensitivity to light | 0 | 0 | 1 [122] | |
| Altered color vision | 1 [17] | 0 | 0 | |
| Difficulty estimating spatial relations | 1 [17]a | 0 | 0 | |
| 3. Education | Studies (N) | 0 | 0 | 1 |
| Double vision | 0 | 0 | 1 [111] | |
| 4. Disease duration | Studies (N) | 6 | 0 | 3 |
| Visual complaints in general | 2 [32, 117] | 0 | 1 [17] | |
| Double vision | 3 [101, 111, 116] | 0 | 1 [17] | |
| Increased sensitivity to light | 1 [137] | 0 | 1 [122] | |
| Altered color vision | 0 | 0 | 1 [17] | |
| Difficulty estimating spatial relations | 0 | 0 | 1 [17] | |
| Asthenopia | 0 | 0 | 1 [152] | |
| 5. Disease severity | Studies (N) | 12 | 0 | 6 |
| Visual complaints in general | 0 | 0 | 1 [17] | |
| Double vision | 5 [52, 59, 110, 111, 116] | 2 [17, 66] | ||
| Increased sensitivity to light | 4 [120, 132, 138, 151]b | 4 [122, 131, 133, 151]c | ||
| Altered color vision | 0 | 1 [17] | ||
| Difficulty estimating spatial relations | 0 | 1 [17] | ||
| Asthenopia | 1 [152] | 0 | 0 | |
| Reduced visual health status | 2 [18, 26] | 0 | 0 | |
| Bumping into objects | 0 | 0 | 1 [17] | |
| 6. Motor fluctuations | Studies (N) | 2 | 0 | 0 |
| Double vision | 2 [104, 111] | 0 | 0 | |
| 7. Dominant symptom (+PIGD > tremor dominant) | Studies (N) | 2 | 0 | 7 |
| Double vision | 1 [36] | 0 | 6 [50, 55, 66, 81, 93, 96] | |
| Increased sensitivity to light | 0 | 0 | 1 [142] | |
| Altered color vision | 0 | 0 | 1 [142] | |
| Changes in depth perception | 1 [142] | 0 | 0 | |
| Reduced peripheral vision | 0 | 0 | 1 [142] | |
| Reduced light/dark adaptation | 1 [142] | 0 | 0 | |
| Reduced acuity/spatial vision | 0 | 0 | 1 [142] | |
| Reduced visual processing speed | 0 | 0 | 1 [142] | |
| Reduced visual search | 0 | 0 | 1 [142] | |
| Problems with visual ADLs | 1 [142] | 0 | 0 | |
| 8. Dyskinesia | Studies (N) | 1 | 0 | 0 |
| Double vision | 1 [104] | 0 | 0 | |
| 9. Left vs. right onset PD | Studies (N) | 0 | 0 | 1 |
| Double vision | 0 | 0 | 1 [81] | |
| 10. Young vs. late onset PD (+late onset > young onset) | Studies (N) | 2 | 0 | 2 |
| Double vision | 2 [70, 103]d | 0 | 2 [77, 79] | |
| 11. Idiopathic PD vs. gene-related parkinsonism (LRRK2 [33], G2385R [161] and PARKIN [79]; +idiopathic PD > gene-related parkinsonism) | Studies (N) | 1 | 0 | 3 |
| Double vision | 1 [79]e | 0 | 2 [33, 79]fg | |
| Increased sensitivity to light | 0 | 0 | 1 [161] | |
| 12. Camptocormia | Studies (N) | 1 | 0 | 1 |
| Double vision | 1 [114] | 0 | 1 [113] | |
| Medical or surgical treatment | ||||
| 13. LEDD | Studies (N) | 1 | 1 | 5 |
| Double vision | 0 | 1 [111] | 1 [54, 59, 82, 94] | |
| Reduced visual health status | 1 [26] | 0 | 0 | |
| Increased sensitivity to light | 0 | 0 | 1 [132] | |
| 14. Off vs. on state (+off state > on state) | Studies (N) | 3 | 0 | 0 |
| Visual complaints in general | 1 [30] | 0 | 0 | |
| Double vision | 1 [111] | 0 | 0 | |
| Problems focusing | 1 [119] | 0 | 0 | |
| 15. Specific medical treatment (Pergolide and Benzhexol [119], and Rotigotine [87, 164]) | Studies (N) | 1 | 0 | 2 |
| Double vision | 0 | 0 | 2 [87, 164] | |
| Adverse visual effects | 1 [119]h | 0 | 0 | |
| 16. DBS (subthalamic nucleus) | Studies (N) | 0 | 2 | 0 |
| Double vision | 0 | 2 [22, 61] | 0 | |
| Other variables | ||||
| 17. QoL and ADL | Studies (N) | 0 | 5 | 1 |
| Visual complaints in general | 0 | 1 [117] | 0 | |
| Double vision | 0 | 1 [118] | 0 | |
| Increased sensitivity to light | 0 | 3 [122, 137, 151] | 1 [125] | |
| 18. Consultation of medical doctor for eye problem | Studies (N) | 1 | 0 | 1 |
| Bumping into objects | 1 [17] | 0 | 0 | |
| Dry eyes | 0 | 0 | 1 [162] | |
Supplementary Table 2 provides an overview of investigated relationships per complaint. >, first group reported more visual complaints than second group; ADL, activities of daily living; DBS, Deep Brain Stimulation; LEDD, Levodopa Equivalent Daily Dose; N, number of studies; PIGD, postural instability and gait disorder; QoL, quality of life. aSide of onset influenced the relationship of gender with difficulty estimating spatial relations; the difference between males and females was bigger (and significant) for the left onset group than right onset group (not significant), bDisease severity measured by Hoehn & Yahr classification and Clinical Impression of Severity Index for Parkinson’s Disease (CISI-PD) [151], cDisease severity measured by Cumulative Illness Rating Scale – Geriatrics (CIRS-G) [151], dOnly significant when adjusted for disease duration and dopaminergic treatment duration and dose [70], eResult accounts for a group of patients with late onset PD [79], fResult accounts for a group of patients with young onset PD [79], gNot significant when adjusted for age, gender, disease duration, disease severity, dopamine agonist, and levodopa [33], hMore colorful dreams were reported after using Pergolide, and relaxation of the eye muscles and blurry vision after using Benzhexol [119].
RESULTS
The search procedure resulted in 139 relevant articles. Table 2 presents the prevalence of visual complaints reported by people with PD and the comparison with healthy controls. One hundred and thirty-one studies investigated the prevalence of visual complaints in people with PD. Some studies reported on more than one complaint, resulting in 185 prevalence numbers. Forty-four studies compared the presence of visual complaints between people with PD and healthy controls. Some studies reported group differences for multiple complaints, resulting in 122 numbers on group comparisons. Of these, 102 (83.6%) indicated that people with PD reported more complaints than healthy controls, whilst 20 (16.4%) found either no difference between these groups or reported healthy controls to experience more complaints than people with PD.
Function-related visual complaints
Visual complaints in general
Seventeen studies [16–32] reported on visual complaints in general. Six of these studies compared people with PD with a control group. In all cases, the prevalence of visual complaints was higher among patients than among controls [16, 18, 20, 21, 25, 26]. One study examined the number of complaints experienced. Three out of four patients (77.3%) experienced at least one complaint, and 43.2% experienced multiple visual complaints [25]. Only 31.6% of healthy controls reported a visual complaint [25].
Double vision
Sixty-one studies reported relevant results on double vision based on the Non-Motor Symptoms Questionnaire (NMSQ) [33–93] and 24 studies based on the Non-Motor Symptom Scale (NMSS) [9, 41, 94–115] (see Supplementary Figure 1). The prevalence ranged from 2.9% [72] to 23.5% [59] in studies with a sample size≥150. Studies with a smaller sample size (N < 150) showed a range from 0% [35, 40, 94] to 60.9% [45]. One study found that for most people with PD experiencing double vision (9.6% of total sample) complaints started after motor symptoms had manifested. Only a small proportion (1.8% of total sample) already experienced double vision before the onset of motor symptoms [71].
Most studies (15/18) on double vision showed a higher prevalence in people with PD compared to controls [16, 25, 47, 48, 56, 57, 59, 91, 95, 96, 108, 116–119]. One study reported prevalence numbers in more detail and showed that 16% of people with PD experienced double vision ‘often’, and 36% ‘sometimes’ [118].
Increased sensitivity to light
Nineteen studies included the SCales for Outcomes in PArkinson’s disease–autonomic dysfunction (SCOPA-AUT) [120] and reported relevant results for the item on oversensitivity to light in people with PD [120–138]. The prevalence ranged from 1.9% [130] to 61.0% [120] (see Supplementary Figure 2). Most studies (13/15) showed that the prevalence was higher in people with PD compared to controls [25, 117, 119–121, 123, 128–130, 132, 138–140].
Other light-related complaints were more prevalent in people with PD as well. People with PD had significantly more difficulty adapting to changing light conditions than controls (patients: 27% vs. controls: 11%) [117], and experienced reduced night vision more often (patients: 16%–47.6% vs. controls: 3%–18.5% [117, 140]).
Altered color vision
Prevalence of altered color vision did not significantly differ between people with PD and healthy controls in the majority of studies [18, 26, 118, 119, 141–143]. Three studies indicated a trend toward more complaints among people with PD [18, 26, 118]. Only one study found that significantly more people with PD (11%) reported the perception of colors to be more pale than controls did (3%) [117]. Another study found that 10% of people with PD perceived less color than before, while 5% perceived more color [118].
Painful, dry or watery eyes
Complaints related to painful, dry or watery eyes were more frequently reported by people with PD than by controls (5/6 studies [18, 25, 117, 144, 145]). Also, severity seems to differ. People with PD had ‘moderate dry eye disease’ and controls ‘mild dry eye disease’ [145]. It was reported that 28% of people with PD had a burning sensation or gritty feeling in their eyes, and only 8% of controls [117]. While some studies could not confirm significance [25, 26], painful eyes were present in 27.3% of people with PD compared to 22.4% of controls [25]. Watery eyes were more frequently reported by people with PD (26.8%–31%) than controls (15%) [24, 117].
Blurred vision
The prevalence of blurry vision was higher in people with PD compared to healthy controls (4/4 studies [25, 117, 140, 146]). Patients experiencing blurry vision indicated that their vision was worse in the dark and they needed more light to see clearly [119].
Changes in contrast sensitivity
Changes in contrast sensitivity were more often reported by people with PD compared to controls (2/2 studies [117, 118]). Roughly a quarter of people with PD (27%) reported changes in the perception of contrast (23% perceived less contrast, 4% perceived more contrast) [118]. People with PD (26%) reported more difficulty reading plain text on a colored or gray background compared to controls (10%) [117].
Changes in size, shape, or depth perception
People with PD reported more complaints regarding size, shape, or depth perception than controls [117, 119]. Seventeen percent of people with PD experienced difficulty with size, shape, and depth perception, compared to 2% (depth) – 5% (size/shape) of controls [117].
Peripheral vision
People with PD experienced significantly more limitations in peripheral vision (i.e., ‘noticing objects off to the side’) than controls [18, 26]. People with PD (43%) indicated to need to turn their head to the side to see peripheral objects more often than controls did (14%) [119].
Difficulty estimating spatial relations
Half of the patients (50%) reported misjudging spaces (5% ‘often’ and 45% ‘sometimes’), compared to 28% of controls [118]. Most people with PD (27%) indicated that spaces appear smaller, while 17% noted that spaces seem larger.
Visual field impairment
People with PD experienced visual field impairments more often (6.1% [24] – 9% [117]) than healthy controls (2% [117]).
Changes in motion perception
Changes in motion perception were reported by a significantly higher number of people with PD (19%–25%) than controls (3%) [118, 119]. Eight percent of people with PD had difficulties ‘often’, and 17% ‘sometimes’. Most people with PD perceived motion as faster (13%), while few perceived motion to be slower (4%). Others perceived motion to be less smooth (3%) [118]. In addition, people with PD had more difficulty following quick movements with their eyes (patients: 25% vs. controls: 4%) [117].
Activity-related visual complaints
Reading difficulties
People with PD reported more difficulty reading than controls (4/4 studies [16, 25, 116, 117]). While one study could not confirm significance, a higher prevalence was found in people with PD (26.7%) compared to controls (9.7%) [16]. Compared to controls, people with PD reported significantly more often that letters disappeared while reading (patients: 20% vs. controls: 5%) and that they had fewer reading difficulties when having one eye closed while reading (patients: 17% vs. controls: 6%) [117].
Near and distant visual activities
People with PD reported more problems with near (patients: 44.3% vs. controls: 25.5%) and distant visual activities (patients: 38.6% vs. controls: 15.0%) than controls [21]. All five studies confirmed this result [18, 21, 26, 147, 148]. Most individuals who had difficulty working nearby reported that their eyes felt tired or uncomfortable [147, 148]. In contrast, people with PD ‘often’ do not have trouble judging close (95%) or distant objects (87%), comparable to healthy controls, of which 96% and 99% did not have problems judging close or distant objects, respectively [118].
Difficulty/freezing in narrow spaces
People with PD had more difficulty in narrow spaces than controls (4/4 studies [25, 116, 118, 119]). Walking through narrow spaces was difficult for 70% of people with PD, compared to 1% of controls [118]. Eighteen percent of people with PD indicated to have difficulties ‘often’, and 52% ‘sometimes’. People with PD indicated to freeze (26%), bump (29%), feel uneasy (10%), or have other problems (3%) while walking through narrow spaces.
Freezing (patients: 60% vs. controls: 3%) and difficulty at doorways (patients: 56% vs. controls: 3%) was also significantly more common in people with PD compared to controls [119]. Half of the people with PD reported to bump into objects [17].
Driving
People with PD experienced more driving difficulties compared to controls (3/3 studies [18, 26, 149]). This could be attributed to poor vision, especially at night. Along with that, people with PD reported difficulties with reading maps or using navigational devices [17]. Besides finding driving more difficult in low visibility conditions (patients: 21.6% vs. controls: 2.7%), people with PD avoid these situations more frequently compared to controls (patients: 35.1% vs. controls: 5.4%) [149].
Difficulty reaching for objects
People with PD reported significantly more difficulty reaching for objects (46%) than controls (3%). Nine percent of people with PD had difficulties ‘often’, and 37% ‘sometimes’. Most patients indicated to not reach far enough (27%), while others reached too far (7%) or reached off to one side of the object (8%) [118].
Vision-related QoL
People with PD scored significantly worse than controls on vision-related QoL (Visual Function Questionnaire; VFQ [150]) [18, 26]. Social functioning and mental health are influenced, role difficulties exist, and people with PD are more dependent on others due to their visual problems. Except for role difficulties, vision-related QoL was influenced to a greater extent in people with PD than in controls.
Relationship of demographic or disease-related variables with visual complaints
Table 3 reports on the relationship of demographic and disease-related characteristics with self-reported visual complaints. Visual complaints did not relate to age (3/4 studies [66, 111, 122]) and gender (12/13 studies [34, 50, 66, 67, 72, 75, 97, 103, 105, 111, 117, 122]). Most studies did find a relationship with disease duration (6/9 studies [32, 101, 111, 116, 117, 137]) and severity (12/18 studies [18, 26, 52, 59, 110, 111, 116, 120, 132, 138, 151, 152]), indicating that visual complaints were more prevalent in patients with a longer disease duration and a more severe disease. Dominant symptoms of the disease (7/9 studies [50, 55, 66, 81, 93, 96, 142]), as well as side of onset (1/1 study [81]) did not relate to visual complaints.
A higher Levodopa Equivalent Daily Dose (LEDD) was not related to visual complaints (5/7 studies [54, 59, 82, 94, 132]), while patients did report more complaints during off-state (3/3 studies [30, 111, 119]). Some medicaments (i.e., Pergolide and Benzhexol) led to visual adverse effect (1/1 study [119]). Deep Brain Stimulation (DBS) was found to relieve double vision (2/2 studies [22, 61]).
The relationship of visual complaints with objectified visual disorders and non-motor symptoms was also investigated (see Supplementary Table 1). Double vision was related to abnormal ocular alignment and aberrant movements of the eyes [116]. Regarding painful or dry eyes, decreased tear production, abnormalities in Meibomian glands, and ocular surface problems could confirm the complaint [16, 145], but it was not related to decreased tear film break-up time or tear osmolarity [145]. Visual complaints were not related to cognitive functioning (3/4 studies [102, 111, 151]), but it did co-occur with psychotic symptoms (e.g., hallucinations; 3/3 studies [24, 111, 151]).
Visual complaints were found to negatively relate to the performance of activities of daily living (ADL) and QoL (5/6 studies [117, 118, 122, 137, 151]).
Supplementary Table 2 presents an overview of investigated relationships with demographic and disease-related variables per visual complaint (an aid for understanding Table 3 and Supplementary Table 1).
DISCUSSION
This systematic review aimed to provide an overview of the literature on self-reported visual complaints in people with PD. Visual complaints occur in a wide variety in people with PD. Moreover, there is a fundamental difference between people with PD and healthy controls. More than 80% of comparisons showed that visual complaints were more common in people with PD than in controls.
According to the literature found, the prevalence of visual complaints varies greatly. Nevertheless, we can conclude that visual complaints were more often present in people with PD than in controls. Visual complaints in general appear to occur in at least a quarter of people with PD, with prevalence ranging from 26.8%–98%. Other complaints with a relatively high prevalence are blurred vision (19.7%–46%), watery eyes (26.8%–31%), light-related complaints (reduced night vision (16%–47.6%) and light/dark adaptation (27%)), ocular fatigue (43.6%), and all activity related complaints (> 21.6%; i.e., reading, driving, reaching, near or distant activities, and difficulty/freezing in narrow spaces). Complaints that appear less prevalent are altered color vision (4.1%–12.7%), and visual field deficits (6.1%–9%).
Vision-related QoL in people with PD appears to be affected in a variety of ways. This is not surprising given that vision is essential in performing a wide variety of activities. Moreover, people with PD need their vision to compensate for their motor loss [6]. Therefore, vision loss may lead to even more difficulties in daily life.
Strengths and limitations
We conducted a systematic literature search and selected all articles that met the inclusion criteria. By involving at least three researchers in the process of data extraction, we sought to ensure reliable and standardized data extraction.
We aimed at providing a comprehensive overview of the literature on self-reported visual complaints in PD. The inclusion of lower quality studies may have biased the results. The prevalence of a complaint was sometimes determined by only few studies and small sample sizes (e.g., asthenopia prevalence was determined in 39 patients [152]). Moreover, the studies used different methods, response options and criteria to assess the complaints in patient groups with different disease characteristics. Therefore, the results presented should be interpreted with caution and results cannot be directly compared. For example, the two lowest rates of double vision are found in de novo PD patients [72, 94], which is in line with the reported increase of visual complaints with disease duration and severity (see Table 3). Also, it was not always clear in the phrasing of questions that problems were attributed to vision [17, 118, 119]. People might have involved other symptoms when answering the questions (i.e., reading difficulties were attributed to both visual problems and difficulties with concentration [17]). For the sake of transparency, we listed the (number of) references, the number of participants in whom a complaint was investigated, and the criterion on which the prevalence was based.
Some visual complaints are reported relatively often, while there are also complaints that are hardly ever reported. An important explanation for this is that former complaints are addressed in frequently used self-reports or questionnaires, while the latter are not. This does not mean that visual complaints not included in those instruments are less common or should be taken less seriously. The majority of 139 included studies (N = 85, 61.2%) reported double vision, an item in the NMSS and NMSQ. Similarly, oversensitivity to light constitutes an item in the SCOPA-AUT and was therefore reported in multiple studies (N = 19, 13.7%). Only 35 articles (25.2%) investigated visual complaints using other measures. For example, only few studies asked for experienced visual field loss or reduced contrast sensitivity, which might nevertheless be relevant in the light of known visual field and contrast sensitivity deficits in PD [4, 153]. To obtain a more complete picture of the prevalence, nature, and severity of visual complaints in people with PD and the characteristics of people who experience these complaints, future research should systematically examine a broad range of visual complaints in a large group of people with PD.
Clinical implications
Detection of visual complaints is necessary to prevent unnecessary limitations in QoL. With knowledge of the visual complaints a patient experiences, clinicians are able to select treatments based on the patient’s priorities [12, 154]. In addition, the use of self-report measures within rehabilitation may provide insight into the changes a patient is experiencing and can indicate when individual goals have been achieved [13].
Visual complaints may be an indication of a treatable underlying disorder, which requires assessment and treatment by an ophthalmologist. Complaints may also relate to underlying disorders that cannot be treated, in which case vision-related rehabilitation may be recommended. As an example, complaints of double vision may be caused by cataract, ptosis, or corneal surface abnormalities. These conditions may be treated with cataract extraction, surgery, or artificial tears, respectively. Another possible cause of double vision is convergence insufficiency, which may require prism glasses or advice on how to compensate while reading.
In some cases, objectified functional disorders may not fully reflect self-reported complaints. For example, even though color vision deficits are more common in people with PD compared to controls [155, 156], people with PD do not tend to report more complaints with regard to color vision. In this example, treatment seems irrelevant because patients do not suffer from the underlying disorder. Therefore, care should always be based on self-reported complaints as well.
Although the literature is scarce, visual complaints seem to be related to disease duration and severity. In addition, visual complaints might be influenced by certain types of treatment. Therefore, we suggest that people with PD should be questioned more frequently and more thoroughly about these complaints in clinical practice, especially in advanced disease stages or with medication changes.
The importance of active questioning is also evident from the fact that visual problems might not always be spontaneously reported to healthcare professionals [48, 49], given that people with PD and their family members are often unaware of the relationship between visual complaints and PD [50]. In addition, Martinez-Martin et al. (2007) argued that these complaints may not be recognized unless detected by a questionnaire [60]. Recently developed visual self-report questionnaires may be used to improve the visual care for people with PD [157, 158].
Conclusion
This overview illustrates that a substantial number of people with PD report complaints in a variety of visual domains. These complaints are related to disease duration and severity and may be influenced by medication use. Since visual complaints have a clear negative impact on QoL, attention to and management of these complaints is essential. Active questioning is advised for timely recognition and treatment of visual complaints.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by Stichting NOVUM, Amsterdam, The Netherlands, ZonMw grant 637005001 (Expertisefunctie Zintuiglijk Gehandicapten, Meerjarig deelsectorplan 2020-2022 Visueel).
Research support: E. Vooijs (BSc), Psychology student at the University of Groningen; K.C. Klaassen (MSc) and J.E.M. Meijerink (MSc), Patient-Res-earchers for the Dutch Parkinson’s Disease Association.
SUPPLEMENTARY MATERIAL
The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JPD-202324.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
REFERENCES
- [1]. Erro R, Santangelo G, Barone P, Vitale C (2015) Nonmotor symptoms in Parkinson’s disease: Classification and management. J Park Restless Legs Syndr 5, 1–10. [Google Scholar]
- [2]. Pfeiffer RF (2016) Non-motor symptoms in Parkinson’s disease. Parkinsonism Relat Disord 22(Suppl 1), S119–S122. [DOI] [PubMed] [Google Scholar]
- [3]. Armstrong RA (2015) Oculo-visual dysfunction in Parkinson’s disease. J Parkinsons Dis 5, 715–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Weil RS, Schrag AE, Warren JD, Crutch SJ, Lees AJ, Morris HR (2016) Visual dysfunction in Parkinson’s disease. Brain 139, 2827–2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Diederich NJ, Raman R, Leurgans S, Goetz CG (2002) Progressive worsening of spatial and chromatic processing deficits in Parkinson disease. Arch Neurol 59, 1249–1252. [DOI] [PubMed] [Google Scholar]
- [6]. Ekker MS, Janssen S, Seppi K, Poewe W, de Vries NM, Theelen T, Nonnekes J, Bloem BR (2017) Ocular and visual disorders in Parkinson’s disease: Common but frequently overlooked. Parkinsonism Relat Disord 40, 1–10. [DOI] [PubMed] [Google Scholar]
- [7]. Sauerbier A, Chaudhuri KR (2014) Non-motor symptoms: The core of multi-morbid Parkinson’s disease. Br J Hosp Med (Lond) 75, 18–24. [DOI] [PubMed] [Google Scholar]
- [8]. Armstrong RA (2008) Visual signs and symptoms of Parkinson’s disease. Clin Exp Optom 91, 129–138. [DOI] [PubMed] [Google Scholar]
- [9]. Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM, Chaudhuri KR (2011) The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov Disord 26, 399–406. [DOI] [PubMed] [Google Scholar]
- [10]. O’Sullivan SS, Williams DR, Gallagher DA, Massey LA, Silveira-Moriyama L, Lees AJ (2008) Nonmotor symptoms as presenting complaints in Parkinson’s disease: A clinicopathological study. Mov Disord 23, 101–106. [DOI] [PubMed] [Google Scholar]
- [11]. Shulman LM, Taback RL, Rabinstein AA, Weiner WJ (2002) Non-recognition of depression and other non-motor symptoms in Parkinson’s disease. Parkinsonism Relat Disord 8, 193–197. [DOI] [PubMed] [Google Scholar]
- [12]. Reddy P, Martinez-Martin P, Brown RG, Chaudhuri KR, Lin JP, Selway R, Forgacs I, Ashkan K, Samuel M (2014) Perceptions of symptoms and expectations of advanced therapy for Parkinson’s disease: Preliminary report of a Patient-Reported Outcome tool for Advanced Parkinson’s disease (PRO-APD). Health Qual Life Outcomes 12, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Vingerhoets G, Lannoo E, van der Linden C, Caemaert J, Vandewalle V, van den Abbeele D, Wolters M (1999) Changes in quality of life following unilateral pallidal stimulation in Parkinson’s disease. J Psychosom Res 46, 247–255. [DOI] [PubMed] [Google Scholar]
- [14]. Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, Atkins D, Barbour V, Barrowman N, Berlin JA, Clark J, Clarke M, Cook D, D’Amico R, Deeks JJ, Devereaux PJ, Dickersin K, Egger M, Ernst E, Gøtzsche PC, Grimshaw J, Guyatt G, Higgins J, Ioannidis JPA, Kleijnen J, Lang T, Magrini N, McNamee D, Moja L, Mulrow C, Napoli M, Oxman A, Pham B, Rennie D, Sampson M, Schulz KF, Shekelle PG, Tovey D, Tugwell P (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6, e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15]. Diederich NJ, Fénelon G, Stebbins G, Goetz CG (2009) Hallucinations in Parkinson disease. Nat Rev Neurol 5, 331–342. [DOI] [PubMed] [Google Scholar]
- [16]. Biousse V, Skibell BC, Watts RL, Loupe DN, Drews-Botsch C, Newman NJ (2004) Ophthalmologic features of Parkinson’s disease. Neurology 62, 177–180. [DOI] [PubMed] [Google Scholar]
- [17]. Davidsdottir S, Cronin-Golomb A, Lee A (2005) Visual and spatial symptoms in Parkinson’s disease. Vision Res 45, 1285–1296. [DOI] [PubMed] [Google Scholar]
- [18]. Almer Z, Klein KS, Marsh L, Gerstenhaber M, Repka MX (2012) Ocular motor and sensory function in Parkinson’s disease. Ophthalmology 119, 178–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19]. King LA, Priest KC, Nutt J, Chen Y, Chen Z, Melnick M HF (2014) Comorbidity and functional mobility in persons with Parkinson disease. Arch Phys Med Rehabil 95, 2152–2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Schmidt C, Herting B, Prieur S, Junghanns S, Schweitzer K, Reichmann H, Berg D, Ziemssen T (2008) Autonomic dysfunction in patients with progressive supranuclear palsy. Mov Disord 23, 2083–2089. [DOI] [PubMed] [Google Scholar]
- [21]. Hamedani AG, Willis AW (2020) Self-reported visual dysfunction in Parkinson disease: The Survey of Health, Ageing and Retirement in Europe. Eur J Neurol 27, 484–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22]. Kawaguchi M, Samura K, Miyagi Y, Okamoto T, Yamasaki R, Sakae N, Yoshida F, Iihara K (2020) The effects of chronic subthalamic stimulation on nonmotor symptoms in advanced Parkinson’s disease, revealed by an online questionnaire program. Acta Neurochir (Wien) 162, 247–255. [DOI] [PubMed] [Google Scholar]
- [23]. Aggarwal R, Goyal V, Pandey RM, Kumar N, Singh S, Shukla G, Behari M (2020) Development and validation of quality of life in Parkinson’s disease instrument. Ann Indian Acad Neurol 23, 59–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24]. Marques A, Beze S, Pereira B, Chassain C, Monneyron N, Delaby L, Lambert C, Fontaine M, Derost P, Debilly B, Rieu I, Lewis SJG, Chiambaretta F, Durif F (2020) Visual hallucinations and illusions in Parkinson’s disease: The role of ocular pathology. J Neurol 267, 2829–2841. [DOI] [PubMed] [Google Scholar]
- [25]. Urwyler P, Nef T, Killen A, Collerton D, Thomas A, Burn D, McKeith I, Mosimann UP (2014) Visual complaints and visual hallucinations in Parkinson’s disease. Parkinsonism Relat Disord 20, 318–322. [DOI] [PubMed] [Google Scholar]
- [26]. Brandt AU, Zimmermann HG, Oberwahrenbrock T, Isensee J, Müller T, Paul F (2018) Self-perception and determinants of color vision in Parkinson’s disease. J Neural Transm (Vienna) 125, 145–152. [DOI] [PubMed] [Google Scholar]
- [27]. Raggi A, Leonardi M, Ajovalasit D, Carella F, Soliveri P, Albanese A, Romito L (2011) Disability and profiles of functioning of patients with Parkinson’s disease described with ICF classification. Int J Rehabil Res 34, 141–150. [DOI] [PubMed] [Google Scholar]
- [28]. Abudi S, Ma RN (1997) Parkinson’s disease symptoms - patients’ perceptions. J Adv Nurs 25, 54–59. [DOI] [PubMed] [Google Scholar]
- [29]. Schenkman M, Cutson TM, Zhu CW, Whetten-Goldstein K (2002) A longitudinal evaluation of patients’ perceptions of Parkinson’s disease. Gerontologist 42, 790–798. [DOI] [PubMed] [Google Scholar]
- [30]. Witjas T, Kaphan E, Azulay JP, Blin O, Ceccaldi M (2002) Nonmotor fluctuations in Parkinson’s disease. Neurology 59, 408–413. [DOI] [PubMed] [Google Scholar]
- [31]. Whitson HE, Sanders LL, Pieper CF, Morey MC, Oddone EZ, Gold DT, Cohen HJ (2009) Correlation between symptoms and function in older adults with comorbidity. J Am Geriatr Soc 57, 676–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32]. Mischley LK, Lau RC, Weiss NS (2017) Use of a self-rating scale of the nature and severity of symptoms in Parkinson’s Disease (PRO-PD): Correlation with quality of life and existing scales of disease severity. NPJ Parkinsons Dis 3, 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33]. Li DW, Gu Z, Wang C, Ma J, Tang BS, Chen S Di, Chan P (2015) Non-motor symptoms in Chinese Parkinson’s disease patients with and without LRRK2 G2385R and R1628P variants. J Neural Transm (Vienna) 122, 661–667. [DOI] [PubMed] [Google Scholar]
- [34]. Durcan R, Wiblin L, Lawson RA, Khoo TK, Yarnall AJ, Duncan GW, Brooks DJ, Pavese N, Burn DJ (2019) Prevalence and duration of non-motor symptoms in prodromal Parkinson’s disease. Eur J Neurol 26, 979–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35]. Ragab OA, Elheneedy YA, Bahnasy WS (2019) Non-motor symptoms in newly diagnosed Parkinson’s disease patients. Egypt J Neurol Psychiatry Neurosurg 55, 1–7. [Google Scholar]
- [36]. Ba F, Obaid M, Wieler M, Camicioli R, Martin WRW (2015) Parkinson disease: The relationship between non-motor symptoms and motor phenotype. Can J Neurol Sci 43, 261–267. [DOI] [PubMed] [Google Scholar]
- [37]. Moccia M, Mollenhauer B, Erro R, Picillo M, Palladino R, Barone P (2015) Non-motor correlates of smoking habits in de novo Parkinson’s disease. J Parkinsons Dis 5, 913–924. [DOI] [PubMed] [Google Scholar]
- [38]. Erro R, Picillo M, Vitale C, Amboni M, Moccia M, Santangelo G, Pellecchia MT, Barone P (2016) The non-motor side of the honeymoon period of Parkinson’s disease and its relationship with quality of life: A 4-year longitudinal study. Eur J Neurol 23, 1673–1679. [DOI] [PubMed] [Google Scholar]
- [39]. Tanveer K, Attique I, Sadiq W, Ahmad A (2018) Non-motor symptoms in patients with Parkinson’s disease: A cross-sectional survey. Cureus 10, e3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40]. Aldaz T, Nigro P, Sánchez-Gómez A, Painous C, Planellas L, Santacruz P, Cámara A, Compta Y, Valldeoriola F, Martí MJ, Muñoz E (2019) Non-motor symptoms in Huntington’s disease: A comparative study with Parkinson’s disease. J Neurol 266, 1340–1350. [DOI] [PubMed] [Google Scholar]
- [41]. Salari M, Chitsaz A, Etemadifar M, Najafi MR, Mirmosayyeb O, Bemanalizadeh M, Panahi F, Mirzajani H (2017) Evaluation of non-motor symptoms and their impact on quality of life in patients with Parkinson’s disease, Isfahan, Iran. Iran J Neurol 16, 118–124. [PMC free article] [PubMed] [Google Scholar]
- [42]. Liu WM, Wu RM, Lin CH, Tai CH, Yu RL, Lin RJ (2015) The impact of nonmotor symptoms on quality of life in patients with Parkinson’s disease in Taiwan. Neuropsychiatr Dis Treat 11, 2865–2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43]. Duncan GW, Khoo TK, Yarnall AJ, O’Brien JT, Coleman SY, Brooks DJ, Barker RA, Burn DJ (2014) Health-related quality of life in early Parkinson’s disease: The impact of nonmotor symptoms. Mov Disord 29, 195–202. [DOI] [PubMed] [Google Scholar]
- [44]. Gan J, Zhou M, Chen W, Liu Z (2014) Non-motor symptoms in Chinese Parkinson’s disease patients. J Clin Neurosci 21, 751–754. [DOI] [PubMed] [Google Scholar]
- [45]. Lolekha P, Kulkantrakorn K (2014) Non-motor symptoms in Thai Parkinson’s disease patients: Prevalence, manifestation and health related quality of life. Neurol Asia 19, 163–170. [Google Scholar]
- [46]. Barone P, Antonini A, Colosimo C, Marconi R, Morgante L, Avarello TP, Bottacchi E, Cannas A, Ceravolo G, Ceravolo R, Cicarelli G, Gaglio RM, Giglia RM, Iemolo F, Manfredi M, Meco G, Nicoletti A, Pederzoli M, Petrone A, Pisani A, Pontieri FE, Quatrale R, Ramat S, Scala R, Volpe G, Zappulla S, Bentivoglio AR, Stocchi F, Trianni G, Del Dotto P; PRIAMO study group (2009) The PRIAMO study: A multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov Disord 24, 1641–1649. [DOI] [PubMed] [Google Scholar]
- [47]. Bostantjopoulou S, Katsarou Z, Karakasis C, Peitsidou E, Milioni D, Rossopoulos N (2013) Evaluation of non-motor symptoms in Parkinson’s disease: An underestimated necessity. Hippokratia 17, 214–219. [PMC free article] [PubMed] [Google Scholar]
- [48]. Chaudhuri KR, Martinez-Martin P, Schapira AH, Stocchi F, Sethi K, Odin P, Brown RG, Koller W, Barone P, MacPhee G, Kelly L, Rabey M, MacMahon D, Thomas S, Ondo W, Rye D, Forbes A, Tluk S, Dhawan V, Bowron A, Williams AJ, Olanow CW (2006) International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: The NMSQuest study. Mov Disord 21, 916–923. [DOI] [PubMed] [Google Scholar]
- [49]. Chaudhuri KR, Prieto-Jurcynska C, Naidu Y, Mitra T, Frades-Payo B, Tluk S, Ruessmann A, Odin P, Macphee G, Stocchi F, Ondo W, Sethi K, Schapira AH, Martinez Castrillo JC, Martinez-Martin P (2010) The nondeclaration of nonmotor symptoms of Parkinson’s disease to health care professionals: An international study using the nonmotor symptoms questionnaire. Mov Disord 25, 704–709. [DOI] [PubMed] [Google Scholar]
- [50]. Cheon SM, Ha MS, Park MJ, Kim JW (2008) Nonmotor symptoms of Parkinson’s disease: Prevalence and awareness of patients and families. Parkinsonism Relat Disord 14, 286–290. [DOI] [PubMed] [Google Scholar]
- [51]. Cosentino C, Nuñez Y, Torres L (2013) Frecuencia de síntomas no motores en Pacientes peruanos con enfermedad de Parkinson. Arq Neuropsiquiatr 71, 216–219.23588282 [Google Scholar]
- [52]. Crosiers D, Pickut B, Theuns J, Deyn PP, Van Broeckhoven C, Martinez-Martin P, Chaudhuri KR, Cras P (2012) Non-motor symptoms in a Flanders-Belgian population of 215 Parkinson’s disease patients as assessed by the non-motor symptoms questionnaire. Am J Neurodegener Dis 1, 160–167. [PMC free article] [PubMed] [Google Scholar]
- [53]. Erro R, Santangelo G, Picillo M, Vitale C, Amboni M, Longo K, Costagliola A, Pellecchia MT, Allocca R, De Rosa A, De Michele G, Santoro L, Barone P (2012) Link between non-motor symptoms and cognitive dysfunctions in de novo, drug-naive PD patients. J Neurol 259, 1808–1813. [DOI] [PubMed] [Google Scholar]
- [54]. Erro R, Picillo M, Vitale C, Amboni M, Moccia M, Longo K, Cozzolino A, Giordano F, De Rosa A, De Michele G, Pellecchia MT, Barone P (2013) Non-motor symptoms in early Parkinson’s disease: A 2-year follow-up study on previously untreated patients. J Neurol Neurosurg Psychiatry 84, 14–17. [DOI] [PubMed] [Google Scholar]
- [55]. Khedr EM, El Fetoh NA, Khalifa H, Ahmed MA, El Beh KM (2013) Prevalence of non motor features in a cohort of Parkinson’s disease patients. Clin Neurol Neurosurg 115, 673–677. [DOI] [PubMed] [Google Scholar]
- [56]. Mao CJ, Chen JP, Zhang XY, Chen Y, Li SJ, Li J, Xiong KP, Hu WD, Liu CF (2015) Parkinson’s disease patients with pain suffer from more severe non-motor symptoms. Neurol Sci 36, 263–268. [DOI] [PubMed] [Google Scholar]
- [57]. Khoo TK, Yarnall AJ, Duncan GW, Coleman S, O’Brien JT, Brooks DJ, Barker RA, Burn DJ (2013) The spectrum of nonmotor symptoms in early Parkinson disease. Neurology 80, 176–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58]. Li HJ, Zhang MF, Chen MX, Hu AL, Li Bin J, Zhang B, Liu W (2015) Validation of the nonmotor symptoms questionnaire for Parkinson’s disease: Results from a Chinese pilot study. Int J Neurosci 125, 929–935. [DOI] [PubMed] [Google Scholar]
- [59]. Zhang N, Liu W, Ye M, Cohen AD, Zhang Y (2015) The heterogeneity of non-motor symptoms of Parkinson’s disease. Neurol Sci 36, 577–584. [DOI] [PubMed] [Google Scholar]
- [60]. Martinez-Martin P, Schapira AH, Stocchi F, Sethi K, Odin P, MacPhee G, Brown RG, Naidu Y, Clayton L, Abe K, Tsuboi Y, MacMahon D, Barone P, Rabey M, Bonuccelli U, Forbes A, Breen K, Tluk S, Olanow CW, Thomas S, Rye D, Hand A, Williams AJ, Ondo W, Chaudhuri KR (2007) Prevalence of nonmotor symptoms in Parkinson’s disease in an international setting; study using nonmotor symptoms questionnaire in 545 patients. Mov Disord 22, 1623–1629. [DOI] [PubMed] [Google Scholar]
- [61]. Nazzaro JM, Pahwa R, Lyons KE (2011) The impact of bilateral subthalamic stimulation on non-motor symptoms of Parkinson’s disease. Parkinsonism Relat Disord 17, 606–609. [DOI] [PubMed] [Google Scholar]
- [62]. Raggi A, Leonardi M, Carella F, Soliveri P, Albanese A, Romito LM (2011) Impact of nonmotor symptoms on disability in patients with Parkinson’s disease. Int J Rehabil Res 34, 316–320. [DOI] [PubMed] [Google Scholar]
- [63]. Yu B, Xiao ZY, Li JZ, Yuan J, Yi-Ming L (2010) Study of an integrated non-motor symptoms questionnaire for Parkinson’s disease. Chin Med J (Engl) 123, 1436–1440. [PubMed] [Google Scholar]
- [64]. Rios Romenets S, Wolfson C, Galatas C, Pelletier A, Altman R, Wadup L, Postuma RB (2012) Validation of the non-motor symptoms questionnaire (NMS-Quest). Parkinsonism Relat Disord 18, 54–58. [DOI] [PubMed] [Google Scholar]
- [65]. Giorelli M, Bagnoli J, Consiglio L, Difazio P, Zizza D, Zimatore GB (2014) Change in non-motor symptoms in Parkinson’s disease and essential tremor patients: A one-year follow-up study. Tremor Other Hyperkinet Mov (N Y) 4, 216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66]. Giorelli M, Bagnoli J, Consiglio L, Lopane M, Bosco Zimatore G, Zizza D, Difazio P (2014) Do non-motor symptoms in Parkinson’s disease differ from essential tremor before initial diagnosis? A clinical and scintigraphic study. Parkinsonism Relat Disord 20, 17–21. [DOI] [PubMed] [Google Scholar]
- [67]. Sánchez-Martínez CM, Choreño-Parra JA, Placencia-Álvarez N, Nuñez-Orozco L, Guadarrama-Ortiz P (2019) Frequency and dynamics of non-motor symptoms presentation in Hispanic patients with Parkinson disease. Front Neurol 10, 1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68]. Vongvaivanich K, Nidhinandana S, Udommongkol C, Chairungsaris P, Chinvarun Y, Wongmek W, Suphakasem S, Suwantamee J, Sithinamsuwan P (2014) Non-motor symptoms in Thai patients with Parkinson’s disease studied at Phramongkutklao Hospital. J Med Assoc Thai 97, S159–S167. [PubMed] [Google Scholar]
- [69]. Sengul Y, Sengul HS, Sural MK, Bakim B, Forta H (2015) A comparison between rate of nonmotor symptom development in essential tremor and Parkinson’s disease. Acta Neurol Belg 115, 289–294. [DOI] [PubMed] [Google Scholar]
- [70]. Zhou MZ, Gan J, Wei YR, Ren XY, Chen W, Liu ZG (2013) The association between non-motor symptoms in Parkinson’s disease and age at onset. Clin Neurol Neurosurg 115, 2103–2107. [DOI] [PubMed] [Google Scholar]
- [71]. Zhang TM, Yu SY, Guo P, Du Y, Hu Y, Piao YS, Zuo LJ, Lian TH, Wang RD, Yu QJ, Jin Z, Zhang W (2016) Nonmotor symptoms in patients with Parkinson disease: A cross-sectional observational study. Medicine (Baltimore) 95, e5400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72]. Picillo M, Amboni M, Erro R, Longo K, Vitale C, Moccia M, Pierro A, Santangelo G, De Rosa A, De Michele G, Santoro L, Orefice G, Barone P, Pellecchia MT (2013) Gender differences in non-motor symptoms in early, drug naïve Parkinson’s disease. J Neurol 260, 2849–2855. [DOI] [PubMed] [Google Scholar]
- [73]. Wang G, Wan Y, Cheng Q, Xiao Q, Wang Y, Zhang J, Ma JF, Wang XJ, Zhou HY, Chen SD (2010) Malnutrition and associated factors in Chinese patients with Parkinson’s disease: Results from a pilot investigation. Parkinsonism Relat Disord 16, 119–123. [DOI] [PubMed] [Google Scholar]
- [74]. Cubo E, López Peña MJ, Diez-Feijo Varela E, Pérez Gil O, Garcia Gutierrez P, Araus González E, Prieto Tedejo R, Mariscal Pérez N, Armesto D (2014) Lack of association of morphologic and functional retinal changes with motor and non-motor symptoms severity in Parkinson’s disease. J Neural Transm (Vienna) 121, 139–145. [DOI] [PubMed] [Google Scholar]
- [75]. Mukhtar S, Imran R, Zaheer M, Tariq H (2018) Frequency of non-motor symptoms in Parkinson’s disease presenting to tertiary care centre in Pakistan: An observational, cross-sectional study. BMJ Open 8, e019172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76]. Rukmini Mridula K, Borgohain R, Jabeen SA, Padmaja G, Bandaru VS, Ankathi P, Kanikannan MA, Ali Khan MS (2015) Comparison of frequencies of non motor symptoms in Indian Parkinson’s disease patients on medical management versus deep brain stimulation: A case-control study. Iran J Neurol 14, 86–93. [PMC free article] [PubMed] [Google Scholar]
- [77]. Špica V, Pekmezović T, Svetel M, Kostić VS (2013) Prevalence of non-motor symptoms in young-onset versus late-onset Parkinson’s disease. J Neurol 260, 131–137. [DOI] [PubMed] [Google Scholar]
- [78]. Gulunay A, Cakmakli GY, Yon MI, Ulusoy EK, Karakoc M (2020) Frequency of non-motor symptoms and their impact on the quality of life in patients with Parkinson’s disease: A prospective descriptive case series. Psychogeriatrics 20, 206–211. [DOI] [PubMed] [Google Scholar]
- [79]. Kägi G, Klein C, Wood NW, Schneider SA, Pramstaller PP, Tadic V, Quinn NP, van de Warrenburg BP, Bhatia KP (2010) Nonmotor symptoms in Parkin gene-related Parkinsonism. Mov Disord 25, 1279–1284. [DOI] [PubMed] [Google Scholar]
- [80]. Erro R, Picillo M, Amboni M, Moccia M, Vitale C, Longo K, Pellecchia MT, Santangelo G, Martinez-Martin P, Ray Chaudhuri K, Barone P (2015) Nonmotor predictors for levodopa requirement in de novo patients with Parkinson’s disease. Mov Disord 30, 373–378. [DOI] [PubMed] [Google Scholar]
- [81]. Rodríguez-Violante M, Cervantes-Arriaga A, Villar-Velarde A, Corona T (2011) Relationship between the type and side of motor symptoms with the prevalence of non-motor symptoms in Parkinson’s disease. Neurologia 26, 319–324. [DOI] [PubMed] [Google Scholar]
- [82]. Picillo M, Erro R, Amboni M, Longo K, Vitale C, Moccia M, Pierro A, Scannapieco S, Santangelo G, Spina E, Orefice G, Barone P, Pellecchia MT (2014) Gender differences in non-motor symptoms in early Parkinson’s disease: A 2-years follow-up study on previously untreated patients. Parkinsonism Relat Disord 20, 850–854. [DOI] [PubMed] [Google Scholar]
- [83]. Guan X, Wang Y, Li Q, Wei M, Chen L, Cheng O (2018) Analysis of the clinical features of early Parkinson’s disease with comparatively integrated intestinal function. Neurol Sci 39, 1847–1856. [DOI] [PubMed] [Google Scholar]
- [84]. Mekawichai P, Kunadisorn S, Tungkasereerak C, Saetang S (2016) Non-motor symptoms in Thai Parkinson’s disease patients and the correlation with motor symptoms. Neurol Asia 21, 41–46. [Google Scholar]
- [85]. Neikrug AB, Avanzino JA, Liu L, Maglione JE, Natarajan L, Corey-Bloom J, Palmer BW, Loredo JS, Ancoli-Israel S (2014) Parkinson’s disease and REM sleep behavior disorder result in increased non-motor symptoms. Sleep Med 15, 959–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86]. Prell T, Schaller D, Perner C, Witte OW, Grosskreutz J (2020) Sicca symptoms in Parkinson’s disease: Association with other nonmotor symptoms and health-related quality of life. Parkinsons Dis 2020, 2958635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87]. Valldeoriola F, Salvador A, Gómez-Arguelles JM, Marey J, Moya M, Ayuga Á, Ramírez F (2018) The effects of transdermal rotigotine on nonmotor symptoms of Parkinson’s disease: A multicentre, observational, retrospective, postmarketing study. Int J Neurosci 128, 369–375. [DOI] [PubMed] [Google Scholar]
- [88]. Yu QJ, Yu SY, Zuo LJ, Lian TH, Hu Y, Wang RD, Piao YS, Guo P, Liu L, Jin Z, Li LX, Chan P, Chen Di S, Wang XM, Zhang W (2018) Parkinson disease with constipation: Clinical features and relevant factors. Sci Rep 8, 567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89]. Samart K (2018) Non-motor symptoms in Thai Parkinson’s disease patients: Prevalence and associated factors. Neurol Asia 23, 327–331. [Google Scholar]
- [90]. Khedr EM, Abo El Fetoh N, Khalifa H, Ahmed MA, El Beh KMA (2012) Prevalence of depression, anxiety, dementia and other non motor features of a large cohort of Egyptian Parkinson’s disease patients. Life Sci J 9, 509–518. [Google Scholar]
- [91]. Zhong LL, Song YQ, Cao H, Ju KJ, Yu L (2021) The non-motor symptoms of Parkinson’s disease of different motor types in early stage. Eur Rev Med Pharmacol Sci 21, 5745–5750. [DOI] [PubMed] [Google Scholar]
- [92]. Govorova T, Popova T, Tappakhov A, Andreev M (2019) Assessment of non-motor symptoms in essential tremor. Int J Biomed 9, 308–312. [Google Scholar]
- [93]. Ren J, Hua P, Pan C, Li Y, Zhang L, Zhang W, Xu P, Zhang M, Liu W (2020) Non-motor symptoms of the postural instability and gait difficulty subtype in de novo Parkinson’s disease patients: A cross-sectional study in a single center. Neuropsychiatr Dis Treat 16, 2605–2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94]. Kim HJ, Park SY, Cho YJ, Hong KS, Cho JY, Seo SY, Lee DH, Jeon BS (2009) Nonmotor symptoms in de novo Parkinson disease before and after dopaminergic treatment. J Neurol Sci 287, 200–204. [DOI] [PubMed] [Google Scholar]
- [95]. Kim J, Youn J, Shin H, Cho J (2013) Nonmotor symptoms in drug-induced parkinsonism and drug-naïve Parkinson disease. Can J Neurol Sci 40, 36–41. [DOI] [PubMed] [Google Scholar]
- [96]. Wu Y, Guo XY, Wei QQ, Ou RW, Song W, Cao B, Zhao B, Shang HF (2016) Non-motor symptoms and quality of life in tremor dominant vs postural instability gait disorder Parkinson’s disease patients. Acta Neurol Scand 133, 330–337. [DOI] [PubMed] [Google Scholar]
- [97]. Martinez-Martin P, Falup Pecurariu C, Odin P, van Hilten JJ, Antonini A, Rojo-Abuin JM, Borges V, Trenkwalder C, Aarsland D, Brooks DJ, Ray Chaudhuri K (2012) Gender-related differences in the burden of non-motor symptoms in Parkinson’s disease. J Neurol 259, 1639–1647. [DOI] [PubMed] [Google Scholar]
- [98]. Song W, Guo X, Chen K, Chen X, Cao B, Wei Q, Huang R, Zhao B, Wu Y, Shang HF (2014) The impact of non-motor symptoms on the health-related quality of life of Parkinson’s disease patients from Southwest China. Parkinsonism Relat Disord 20, 149–152. [DOI] [PubMed] [Google Scholar]
- [99]. Shalash AS, Hamid E, Elrassas HH, Bedair AS, Abushouk AI, Khamis M, Hashim M, Ahmed NS, Ashour S, Elbalkimy M (2018) Non-motor symptoms as predictors of quality of life in Egyptian patients with Parkinson’s disease: A cross-sectional study using a culturally adapted 39-item Parkinson’s disease questionnaire. Front Neurol 9, 357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100]. Ou R, Yang J, Cao B, Wei Q, Chen K, Chen X, Zhao B, Wu Y, Song W, Shang H (2016) Progression of non-motor symptoms in Parkinson’s disease among different age populations: A two-year follow-up study. J Neurol Sci 360, 72–77. [DOI] [PubMed] [Google Scholar]
- [101]. Guo X, Song W, Chen K, Chen X, Zheng Z, Cao B, Huang R, Zhao B, Wu Y, Shang HF (2013) Disease duration-related differences in non-motor symptoms: A study of 616 Chinese Parkinson’s disease patients. J Neurol Sci 330, 32–37. [DOI] [PubMed] [Google Scholar]
- [102]. Zhang SS, Ou RW, Chen XP, Yang J, Zhao B, Yuan XQ, Wei QQ, Cao B, Shang HF (2016) Correlative factors of cognitive dysfunction in PD patients: A cross-sectional study from Southwest China. Neurol Res 38, 434–440. [DOI] [PubMed] [Google Scholar]
- [103]. Guo X, Song W, Chen K, Chen XP, Zheng Z, Cao B, Huang R, Zhao B, Wu Y, Shang HF (2013) Gender and onset age-related features of non-motor symptoms of patients with Parkinson’s disease - a study from Southwest China. Parkinsonism Relat Disord 19, 961–965. [DOI] [PubMed] [Google Scholar]
- [104]. Santos-García D, de Deus Fonticoba T, Suárez Castro E, Aneiros Díaz A, McAfee D, Catalán MJ, Alonso-Frech F, Villanueva C, Jesús S, Mir P, Aguilar M, Pastor P, García Caldentey J, Esltelrich Peyret E, Planellas LL, Martí MJ, Caballol N, Hernández Vara J, Martí Andrés G, Cabo I, Ávila Rivera MA, López Manzanares L, Redondo N, Martinez-Martin P; COPPADIS Study Group McAfee D (2020) Non-motor symptom burden is strongly correlated to motor complications in patients with Parkinson’s disease. Eur J Neurol 27, 1210–1223. [DOI] [PubMed] [Google Scholar]
- [105]. Ravan A, Ahmad FM, Chabria S, Gadhari M, Sankhla CS (2015) Non-motor symptoms in an Indian cohort of Parkinson′s disease patients and correlation of progression of non-motor symptoms with motor worsening. Neurol India 63, 166–174. [DOI] [PubMed] [Google Scholar]
- [106]. Weerkamp NJ, Tissingh G, Poels PJ, Zuidema SU, Munneke M, Koopmans RT, Bloem BR (2013) Nonmotor symptoms in nursing home residents with Parkinson’s disease: Prevalence and effect on quality of life. J Am Geriatr Soc 61, 1714–1721. [DOI] [PubMed] [Google Scholar]
- [107]. Cho BH, Choi SM, Kim JT, Kim BC (2018) Association of coffee consumption and non-motor symptoms in drug-naïve, early-stage Parkinson’s disease. Parkinsonism Relat Disord 50, 42–47. [DOI] [PubMed] [Google Scholar]
- [108]. Santos García D, Jesús S, Aguilar M, Planellas LL, García Caldentey J, Caballol N, Legarda I, Hernández Vara J, Cabo I, López Manzanares L, González Aramburu I, Ávila Rivera MA, Catalán MJ, López Díaz L, Puente V, García Moreno JM, Borrué C, Solano Vila B; Álvarez Sauco M, Vela L, Escalante S, Cubo E, Carrillo Padilla F, Martínez Castrillo JC, Sánchez Alonso P, Alonso Losada MG, López Ariztegui N, Gastón I, Kulisevsky J, Menéndez González M, Seijo M, Rúiz Martínez J, Valero C, Kurtis M, de Fábregues-Boixar O, González Ardura J, Prieto Jurczynska C, Martinez-Martin P, Mir P; COPPADIS Study Group (2019) COPPADIS-2015 (COhort of Patients with PArkinson’s DIsease in Spain, 2015): An ongoing global Parkinson’s disease project about disease progression with more than 1000 subjects included. Results from the baseline evaluation. Eur J Neurol 26, 1399–1407. [DOI] [PubMed] [Google Scholar]
- [109]. Rosqvist K, Odin P, Hagell P, Iwarsson S, Nilsson MH, Storch A (2019) Dopaminergic effect on non-motor symptoms in late stage Parkinson’s disease. J Parkinsons Dis 9, 447–448. [DOI] [PubMed] [Google Scholar]
- [110]. Toyama M, Okuma Y, Yamamoto M, Kashihara K, Yoshida K, Saiki H, Maeda T, Tsuboi Y, Takahashi Y, Nakayama T (2020) Non-motor symptoms depending on motor severity in Japanese patients with Parkinson’s disease: A multicenter cross-sectional study. J Neurol Sci 412, 116641. [DOI] [PubMed] [Google Scholar]
- [111]. Schindlbeck KA, Schönfeld S, Naumann W, Friedrich DJ, Maier A, Rewitzer C, Klostermann F, Marzinzik F (2017) Characterization of diplopia in non-demented patients with Parkinson’s disease. Parkinsonism Relat Disord 45, 1–6. [DOI] [PubMed] [Google Scholar]
- [112]. Karri M, Ramasamy B, Kalidoss R (2020) Prevalence of non-motor symptoms in Parkinson’s disease and its impact on quality of life in tertiary care center in India. Ann Indian Acad Neurol 23, 270–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113]. Ou R, Guo X, Song W, Cao B, Wei Q, Shao N, Zhao B, Shang H (2014) Characteristics of non-motor symptoms in patients with Parkinson’s disease exhibiting camptocormia. Gait Posture 40, 447–450. [DOI] [PubMed] [Google Scholar]
- [114]. Ou R, Liu H, Hou Y, Song W, Cao B, Wei Q, Yuan X, Chen Y, Zhao B, Shang H (2018) Predictors of camptocormia in patients with Parkinson’s disease: A prospective study from southwest China. Parkinsonism Relat Disord 52, 69–75. [DOI] [PubMed] [Google Scholar]
- [115]. Santos-García D, de la Fuente-Fernández R (2013) Impact of non-motor symptoms on health-related and perceived quality of life in Parkinson’s disease. J Neurol Sci 332, 136–140. [DOI] [PubMed] [Google Scholar]
- [116]. Archibald NK, Clarke MP, Mosimann UP, Burn DJ (2011) Visual symptoms in Parkinson’s disease and Parkinson’s disease dementia. Mov Disord 26, 2387–2395. [DOI] [PubMed] [Google Scholar]
- [117]. Borm CDJM, Visser F, Werkmann M, de Graaf D, Putz D, Seppi K, Poewe W, Vlaar AMM, Hoyng C, Bloem BR, Theelen T, de Vries NM (2020) Seeing ophthalmologic problems in Parkinson disease: Results of a visual impairment questionnaire. Neurology 94, e1539–e1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118]. Lee A, Harris J (1999) Problems with perception of space in Parkinson’s disease: A questionnaire study. Neuroophthalmology 22, 1–15. [Google Scholar]
- [119]. McDowell SA, Harris JP (1997) Visual problems in Parkinson’s disease: A questionnaire survey. Behav Neurol 10, 77–81. [DOI] [PubMed] [Google Scholar]
- [120]. Visser M, Marinus J, Stiggelbout AM, van Hilten JJ (2004) Assessment of autonomic dysfunction in Parkinson’s disease: The SCOPA-AUT. Mov Disord 19, 1306–1312. [DOI] [PubMed] [Google Scholar]
- [121]. Bostantjopoulou S, Katsarou Z, Danglis I, Karakasis H, Milioni D (2016) Self-reported autonomic symptoms in Parkinson’s disease: Properties of the SCOPA-AUT scale. Hippokratia 20, 115–120. [PMC free article] [PubMed] [Google Scholar]
- [122]. Tomic S, Rajkovaca I, Pekic V, Salha T, Misevic S (2017) Impact of autonomic dysfunctions on the quality of life in Parkinson’s disease patients. Acta Neurol Belg 117, 207–211. [DOI] [PubMed] [Google Scholar]
- [123]. Mollenhauer B, Trautmann E, Sixel-Döring F, Wicke T, Ebentheuer J, Schaumburg M, Lang E, Focke NK, Kumar KR, Lohmann K, Klein C, Schlossmacher MG, Kohnen R, Friede T, Trenkwalder C (2013) Nonmotor and diagnostic findings in subjects with de novo Parkinson disease of the DeNoPa cohort. Neurology 81, 1226–1234. [DOI] [PubMed] [Google Scholar]
- [124]. Kim R, Jun JS (2019) Association of autonomic symptoms with presynaptic striatal dopamine depletion in drug-naive Parkinson’s disease: An analysis of the PPMI data. Auton Neurosci 216, 59–62. [DOI] [PubMed] [Google Scholar]
- [125]. Merola A, Romagnolo A, Rosso M, Suri R, Berndt Z, Maule S, Lopiano L, Espay AJ (2018) Autonomic dysfunction in Parkinson’s disease: A prospective cohort study. Mov Disord 33, 391–397. [DOI] [PubMed] [Google Scholar]
- [126]. Sklerov M, Shih CH, Browner N, Palma JA, Styner M, Dayan E (2020) Longitudinal change in autonomic symptoms predicts activities of daily living and depression in Parkinson’s disease. Clin Auton Res 30, 223–230. [DOI] [PubMed] [Google Scholar]
- [127]. van Deursen DN, van den Heuvel OA, Booij J, Berendse HW, Vriend C (2020) Autonomic failure in Parkinson’s disease is associated with striatal dopamine deficiencies. J Neurol 267, 1922–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [128]. Sprenger FS, Seppi K, Djamshidian A, Reiter E, Nocker M, Mair K, Göbel G, Poewe W (2015) Nonmotor symptoms in subjects without evidence of dopaminergic deficits. Mov Disord 30, 976–981. [DOI] [PubMed] [Google Scholar]
- [129]. Garg D, Srivastava AK, Jaryal AK, Rajan R, Singh A, Pandit AK, Vibha D, Shukla G, Garg A, Pandey RM, Prasad K (2020) Is there a difference in autonomic dysfunction between multiple system atrophy subtypes? Mov Disord Clin Pract 7, 405–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [130]. Stanković I, Petrović I, Pekmezović T, Marković V, Stojković T, Dragašević-Mišković N, Svetel M, Kostić V (2019) Longitudinal assessment of autonomic dysfunction in early Parkinson’s disease. Parkinsonism Relat Disord 66, 74–79. [DOI] [PubMed] [Google Scholar]
- [131]. Mantarova SG, Velcheva IV, Georgieva SO, Stambolieva KI (2013) Validation of the Bulgarian version of Scales for Outcomes in Parkinson’s Disease - Autonomic (SCOPA-AUT-BG). Folia Med (Plovdiv) 55, 56–62. [DOI] [PubMed] [Google Scholar]
- [132]. Verbaan D, Marinus J, Visser M, Van Rooden SM, Stiggelbout AM, Van Hilten JJ (2007) Patient-reported autonomic symptoms in Parkinson disease. Neurology 69, 333–341. [DOI] [PubMed] [Google Scholar]
- [133]. Malek N, Lawton MA, Grosset KA, Bajaj N, Barker RA, Burn DJ, Foltynie T, Hardy J, Morris HR, Williams NM, Ben-Shlomo Y, Wood NW, Grosset DG (2017) Autonomic dysfunction in early Parkinson’s disease: Results from the United Kingdom tracking Parkinson’s study. Mov Disord Clin Pract 4, 509–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [134]. Valentino F, Bartolotta TV, Cosentino G, Mastrilli S, Arnao V, Aridon P, Scurria S, Pavone A, Pavone C, D’Amelio M (2018) Urological dysfunctions in patients with Parkinson’s disease: Clues from clinical and non-invasive urological assessment. BMC Neurol 18, 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135]. Arnao V, Cinturino A, Valentino F, Perini V, Mastrilli S, Bellavia G, Savettieri G, Realmuto S, D’Amelio M (2015) In patient’s with Parkinson disease, autonomic symptoms are frequent and associated with other non-motor symptoms. Clin Auton Res 25, 301–307. [DOI] [PubMed] [Google Scholar]
- [136]. Kurtis MM, Rodriguez-Blazquez C, Martinez-Martin P; ELEP Group (2013) Relationship between sleep disorders and other non-motor symptoms in Parkinson’s disease. Parkinsonism Relat Disord 19, 1152–1155. [DOI] [PubMed] [Google Scholar]
- [137]. Tibar H, El Bayad K, Bouhouche A, Ait Ben Haddou EH, Benomar A, Yahyaoui M, Benazzouz A, Regragui W (2018) Non-motor symptoms of Parkinson’s disease and their impact on quality of life in a cohort of Moroccan patients. Front Neurol 9, 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138]. Damian A, Adler CH, Hentz JG, Shill HA, Caviness JN, Sabbagh MN, Evidente VG, Beach TG, Driver-Dunckley E (2012) Autonomic function, as self-reported on the SCOPA-autonomic questionnaire, is normal in essential tremor but not in Parkinson’s disease. Parkinsonism Relat Disord 18, 1089–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [139]. Frauscher B, Nomura T, Duerr S, Ehrmann L, Gschliesser V, Wenning GK, Wolf E, Inoue Y, Högl B, Poewe W (2012) Investigation of autonomic function in idiopathic REM sleep behavior disorder. J Neurol 259, 1056–1061. [DOI] [PubMed] [Google Scholar]
- [140]. Reimann M, Schmidt C, Herting B, Prieur S, Junghanns S, Schweitzer K, Globas C, Schoels L, Reichmann H, Berg D, Ziemssen T (2010) Comprehensive autonomic assessment does not differentiate between Parkinson’s disease, multiple system atrophy and progressive supranuclear palsy. J Neural Transm (Vienna) 117, 69–76. [DOI] [PubMed] [Google Scholar]
- [141]. Gaenslen A, Swid I, Liepelt-Scarfone I, Godau J, Berg D (2011) The patients’ perception of prodromal symptoms before the initial diagnosis of Parkinson’s disease. Mov Disord 26, 653–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [142]. Seichepine DR, Neargarder S, Miller IN, Riedel TM, Gilmore GC, Cronin-Golomb A (2011) Relation of Parkinson’s disease subtypes to visual activities of daily living. J Int Neuropsychol Soc 17, 841–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143]. Zimmermann M, Gaenslen A, Prahl K, Srulijes K, Hauser AK, Schulte C, Csoti I, Berg D, Brockmann K (2019) Patient’s perception: Shorter and more severe prodromal phase in GBA-associated PD. Eur J Neurol 26, 694–698. [DOI] [PubMed] [Google Scholar]
- [144]. Tamer C, Melek IM, Duman T, Öksüz H (2005) Tear film tests in Parkinson’s disease patients. Ophthalmology 112, 1795. [DOI] [PubMed] [Google Scholar]
- [145]. Nowacka B, Lubinski W, Honczarenko K, Potemkowski A, Safranow K (2014) Ophthalmological features of Parkinson disease. Med Sci Monit 20, 2243–2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [146]. Bulpitt CJ, Shaw K, Clifton P, Stern G, Davies JB, Reid JL (1985) The symptoms of patients treated for Parkinson’s disease. Clin Neuropharmacol 8, 175–183. [DOI] [PubMed] [Google Scholar]
- [147]. Law C, Chriqui E, Kergoat MJ, Leclerc BS, Panisset M, Irving EL, Postuma RB, Chouinard S, Kergoat H (2017) Prevalence of convergence insufficiency-type symptomatology in Parkinson’s disease. Can J Neurol Sci 44, 562–566. [DOI] [PubMed] [Google Scholar]
- [148]. Irving EL, Chriqui E, Law C, Kergoat MJ, Leclerc BS, Panisset M, Postuma R, Kergoat H (2017) Prevalence of convergence insufficiency in Parkinson’s disease. Mov Disord Clin Pract 4, 424–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [149]. Stolwyk RJ, Scally KA, Charlton JL, Bradshaw JL, Iansek R, Georgiou-Karistianis N (2015) Self-regulation of driving behavior in people with Parkinson disease. Cogn Behav Neurol 28, 80–91. [DOI] [PubMed] [Google Scholar]
- [150]. Mangione CM, Berry S, Spritzer K, Janz NK, Klein R, Owsley C, Lee PP (1998) Identifying the content area for the 51-item national eye institute visual function questionnaire: Results from focus groups with visually impaired persons. Arch Ophthalmol 116, 227–233. [DOI] [PubMed] [Google Scholar]
- [151]. Rodriguez-Blazquez C, Forjaz MJ, Frades-Payo B, de Pedro-Cuesta J, Martinez-Martin P; Longitudinal Parkinson’s Disease Patient Study, Estudio Longitudinal de Pacients con Enfermedad da Parkinson Group (2010) Independent validation of the scales for outcomes in Parkinson’s disease-autonomic (SCOPA-AUT). Eur J Neurol 17, 194–201. [DOI] [PubMed] [Google Scholar]
- [152]. Repka MX, Claro MC, Loupe DN, Reich SG (1996) Ocular motility in Parkinson’s disease. J Pediatr Ophthalmol Strabismus 33, 144–147. [DOI] [PubMed] [Google Scholar]
- [153]. Yenice O, Onal S, Midi I, Ozcan E, Temel A, I-Gunal D (2008) Visual field analysis in patients with Parkinson’s disease. Parkinsonism Relat Disord 14, 193–198. [DOI] [PubMed] [Google Scholar]
- [154]. Hobart JC, Freeman JA, Lamping DL (1996) Physician and patient-oriented outcomes in progressive neurological disease: Which to measure? Curr Opin Neurol 9, 441–444. [DOI] [PubMed] [Google Scholar]
- [155]. Piro A, Tagarelli A, Nicoletti G, Fletcher R, Quattrone A (2014) Color vision impairment in Parkinson’s disease. J Parkinsons Dis 4, 317–319. [DOI] [PubMed] [Google Scholar]
- [156]. Birch J, Kolle RU, Kunkel M, Paulus W, Upadhyay P (1998) Acquired colour deficiency in patients with Parkinson’s disease. Vision Res 38, 3421–3426. [DOI] [PubMed] [Google Scholar]
- [157]. Huizinga F, Heutink J, de Haan GA, van der Lijn I, van der Feen FE, Vrijling ACL, Melis-Dankers BJM, de Vries SM, Tucha O, Koerts J (2020) The development of the Screening of Visual Complaints questionnaire for patients with neurodegenerative disorders: Evaluation of psychometric features in a community sample. PLoS One 15, e0232232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158]. Borm CDJM, Werkmann M, Visser F, Peball M, Putz D, Seppi K, Poewe W, Notting IC, Vlaar A, Theelen T, Hoyng C, Bloem BR, de Vries NM (2019) Towards seeing the visual impairments in Parkinson’s disease: Protocol for a multicentre observational, cross-sectional study. BMC Neurol 19, 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [159]. Kleiner-Fisman G, Martine R, Lang AE, Stern MB (2011) Development of a non-motor fluctuation assessment instrument for Parkinson disease. Parkinsons Dis 2011, 292719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [160]. Mathur S, Mursaleen L, Stamford J, Dewitte S, Robledo I, Isaacs T (2017) Challenges of improving patient-centred care in Parkinson’s disease. J Parkinsons Dis 7, 163–174. [DOI] [PubMed] [Google Scholar]
- [161]. Yang J, Wang H, Yuan Y, Fan S, Li L, Jiang C, Mao C, Shi C, Xu Y (2021) Peripheral synucleinopathy in Parkinson disease with LRRK2 G2385R variants. Ann Clin Transl Neurol 8, 592–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [162]. Leclair-Visonneau L, Clairembault T, Volteau C, Chapelet G, Le Dily S, Vavasseur F, Coron E, Préterre C, Neunlist M, Péréon Y, Derkinderen P (2019) Colonic neuropathology is not associated with autonomic dysfunction in Parkinson’s disease. Parkinsonism Relat Disord 61, 224–247. [DOI] [PubMed] [Google Scholar]
- [163]. Charlton JL, Oxley J, Fildes B, Oxley P, Newstead S, Koppel S, O’Hare M (2006) Characteristics of older drivers who adopt self-regulatory driving behaviours. Transp Res Part F Traffic Psychol Behav 9, 363–373. [Google Scholar]
- [164]. Antonini A, Bauer L, Dohin E, Oertel WH, Rascol O, Reichmann H, Schmid M, Singh P, Tolosa E, Chaudhuri KR (2015) Effects of rotigotine transdermal patch in patients with Parkinson’s disease presenting with non-motor symptoms - results of a double-blind, randomized, placebo-controlled trial. Eur J Neurol 22, 1400–1407. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.