Abstract
Acute respiratory distress syndrome (ARDS) is a clinical syndrome characterized by several clinical features and pathological responses involving the respiratory system primarily. Infections (viral), sepsis, and massive transfusion are the commonest causes of ARDS during pregnancy. The majority of them recover with noninvasive ventilatory (NIV) support. NIV is safe in pregnancy provided the center is experienced and has a protocolized patient care pathway. Parturients requiring invasive mechanical ventilation are best managed in experienced centers. PaO2/FiO2 targets are higher in parturients compared to nonpregnant patients. Permissive hypercapnia is not a safe option in pregnancy. In severe ARDS with refractory hypoxemia, prone ventilation is a safe option. However, it has to be done in experienced centers. Venovenous ECMO is a safe alternative option in pregnant women with refractory hypoxemia, and delivery has been prolonged to a safe viable age on ECMO. The decision to deliver and the mode of delivery have to be a multidisciplinary decision; primary criterion is maternal survival. Postdelivery, establishing maternal bonding while in ventilatory support facilitates early weaning and minimizes lactation failure.
How to cite this article
Pandya ST, Krishna SJ. Acute Respiratory Distress Syndrome in Pregnancy. Indian J Crit Care Med 2021; 25(Suppl 3):S241–S247.
Keywords: ARDS, ECMO, NIV, Pregnancy, Prone, Ventilation
Introduction
Acute respiratory distress syndrome (ARDS) is a clinical syndrome characterized by several clinical features and pathological responses involving the respiratory system primarily. Fortunately, ARDS is relatively uncommon during pregnancy affecting 0.1–0.2% of all parturients. However, from most studies and our unit data (Figs 1 and 2), the lung is the commonest organ involved in patients admitted into the obstetric critical care unit. Further, our audit reported a 12% incidence of ventilatory support.
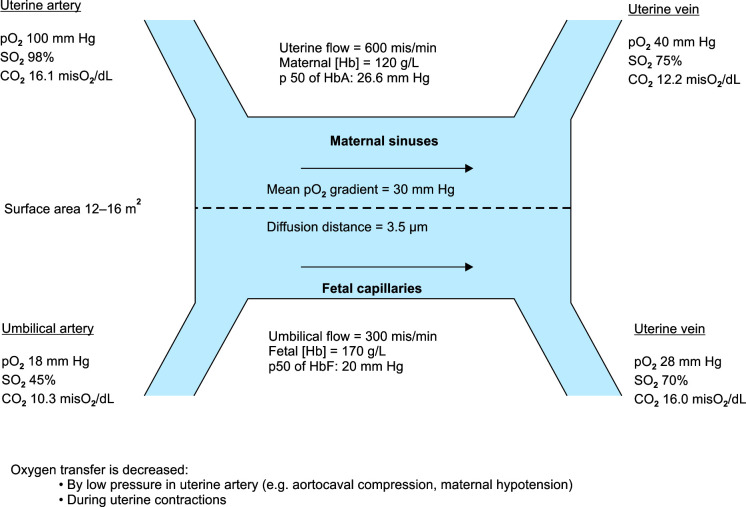
Fig. 1.
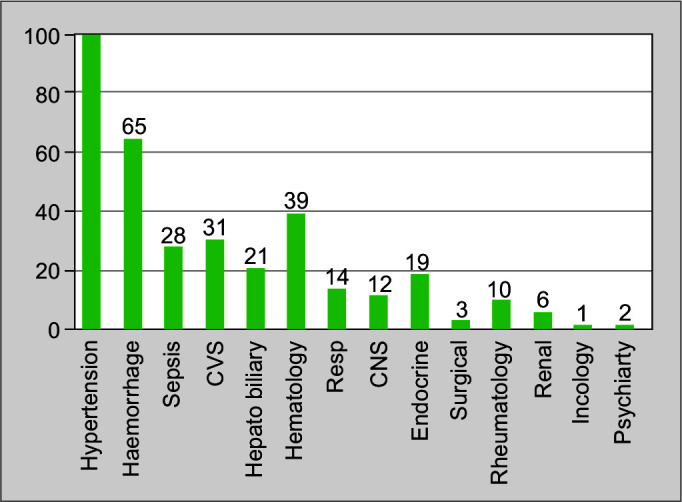
Common causes of pregnant women requiring high-dependency unit and ICU admissions, Clinical audit data, 2015, Fernandez Hospital, Hyderabad, India
Fig. 2.
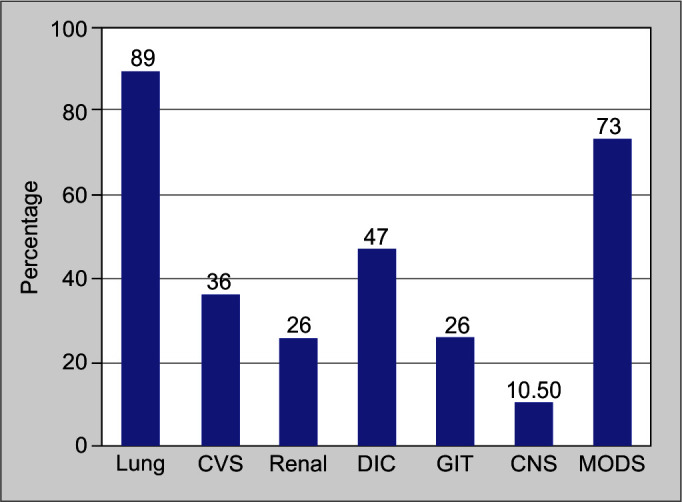
Lung is the most common organ involved in sick parturients requiring ICU admissions, Clinical audit data, Fernandez Hospital, Hyderabad, India
Airway in pregnancy is both anatomically and physiologically challenging with increased oxygen consumption. Hence, any respiratory diseases in pregnant women causing respiratory failure put them at risk of acute-onset hypoxia. Untreated acute maternal hypoxemia leads to fetal hypoxemia and fetal compromise, which if not optimized appropriately often leads to morbidity and mortality. Further, severe ARDS often requires mechanical ventilatory support, prone ventilation, multiorgan support, and sometimes ECMO for maternal and fetal well-being. Hence, a multidisciplinary team approach involving experienced obstetricians, intensivists, obstetric anesthesiologists, and neonatologists should be considered in the patient care pathway to improve the maternal and fetal outcomes and morbidity.
The Berlin definition proposed by the European Society of Intensive Care Medicine defines ARDS as a new or worsening respiratory symptom that includes a combination of acute hypoxemia (PaO2/FiO2 ≤300 mm Hg), in a ventilated patient with a positive end-expiratory pressure (PEEP) of at least 5 cm H2O, and bilateral opacities not fully explained by heart failure or volume overload that occurs within 7 days of a clinical insult.1 The levels of PaO2/FiO2 ratio are used to categorize ARDS as mild (200–≤300 mm Hg), moderate (100–≤200 mm Hg), and severe (≤100 mm Hg).1 The severe inflammatory process in the lungs includes injury to the alveolar-capillary barrier, depletion of the surfactant, and loss of aerated lung tissue.2 These inflammatory changes cause nonhydrostatic protein-rich pulmonary edema that can lead to profound hypoxemia, decreased lung compliance, and increased intrapulmonary shunt and dead space.2
The Kigali modification of the Berlin definition3 uses alternate criteria, including peripheral capillary oxygen saturation (SpO2)-to-FiO2 ratio and chest ultrasound, which is a useful adaptation in the low-resource setting. The Kigali modification considers a SpO2/FiO2 ≤315 for oxygenation, has no PEEP requirement, and considers bilateral chest opacities not fully explained by effusions, lobar/lung collapse, or nodules by the chest radiograph or ultrasound and respiratory failure that is not fully explained by cardiac failure or fluid overload.
Physiological Changes in the Respiratory System of Pregnant Women
Hormonal changes and consequences, mechanistic effects of the enlarging uterus, increased metabolic demands of the fetoplacental unit, changing lung volumes, mechanics of ventilation, control of respiration, and decrease in functional residual capacity (FRC) are some of the changes mediated by pregnancy.4,5 Chest wall and total respiratory compliances decrease by approximately 30% although pregnancy does not change lung compliance.6 The normal partial pressure of carbon dioxide (PaCO2) during pregnancy is 27–34 mm Hg and is mediated by the effects of progesterone.7 The partial pressure of oxygen (PaO2) ranges between 90 and 110 mm Hg in pregnant women.4,5 An increase in the oxygen demand and decrease in FRC causes smaller airways to close earlier when the lung volume is reduced, leading to an increased risk of rapid desaturation in pregnancy.8 Fetoplacental oxygen transfer is decreased by low pressure in the uterine artery and during uterine contractions. Determinants of fetoplacental blood flow include hemoglobin and hemoglobin saturation, uteroplacental blood flow, and maternal hypotension. A maternal PaO2 >75 mm Hg is needed to protect the fetus from a hypoxic injury, and a fetal PaCO2 of ≥65 mm Hg and/or persistent respiratory alkalosis (pH >7.48) causes decreased fetal perfusion and adverse perinatal outcomes.9,10
Causes of ARDS in Pregnancy
ARDS in pregnancy can result from a direct obstetric cause or may be modified by an obstetric cause. ARDS is more common in the third trimester of pregnancy and has an estimated incidence that varies between 1 per 6,000 and 1 per 10,000 deliveries.11,12 The common obstetric causes for ARDS in pregnancy include hypertensive disorders of pregnancy, tocolytic-induced pulmonary edema, amniotic fluid embolism, placental abruption, retained products of conception, chorioamnionitis, endometritis, obstetric hemorrhage–related causes, and septic abortions.4 Common nonobstetric causes for ARDS in pregnancy include trauma, massive blood transfusions, pneumonia (bacterial, viral—H1N1, SARS-CoV-2, varicella, etc.), gastric aspiration, pyelonephritis, sepsis, fat embolism, and pancreatitis.4 ARDS in pregnancy is a significant contributor to perinatal and maternal mortality rates with an estimated 30–50% maternal mortality on pregnant women with ARDS and an estimated 20–25% perinatal mortality rate.13 High rates of neonatal death, spontaneous preterm births, and fetal heart rate abnormalities are common in pregnancies complicated by ARDS.4
Wanderer et al.14 have reported a 24.6% incidence of acute respiratory failure in pregnant women at the time of ICU admission. At our center, we found that respiratory causes were associated with 2.55% of all ICU and high-dependency unit admissions, and the lung (89%) was the most common organ affected in the obstetric critical care unit (Figs 1 and 2).
Management of ARDS in Pregnancy
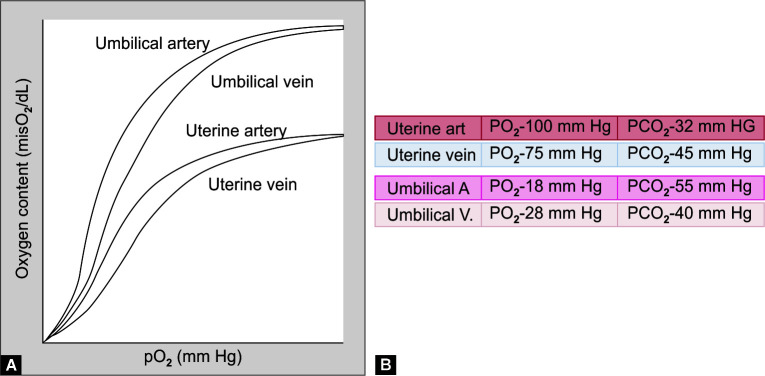
There is a lack of effective pharmacologic interventions for ARDS, and the initial management aims to stabilize gas exchange and minimize further injury to the lung tissues. The basic premise is optimizing maternal and placental gas exchange. Figure 3 depicts the oxygenation levels at the maternofetal unit.
Fig. 3.
Placental gas exchange
The objective is to maintain maternal PaO2 levels at 65–70 mm Hg and above to ensure adequate fetal oxygen delivery, unlike nonpregnant women, where even low PaO2 is accepted. The clinician taking care of pregnant women with ARDS should remember that the placenta is a concurrent flow oxygen membrane, and determinants of fetal oxygen delivery depend upon the maternal hematocrit, hemoglobin saturation, uteroplacental blood flow which is maximally dilated and is directly dependant of maternal mean arterial pressure (MAP), influence of MAP by aortocaval compression, and the need for left uterine displacement. Maternal hypotension is the single most important factor to reduce fetal blood flow.
The lethal triad for fetal demise is maternal hypotension, hypoxia, and anemia. Understanding of maternal–fetoplacenal dynamics and oxygen dissociation curves for mother and fetus, Figure 4 (double Bohr and double Haldane effect), is vital to optimize oxygen delivery to mother and fetus.
Figs 4A and B.
(A) Oxygen dissociation curves for mother and fetus; (B) Maternofetal gas values
Depending upon the severity of maternal hypoxemia and work of breathing, gas exchange is optimized by simple oxygen delivery by nasal prongs, venturi masks, nonrebreathing high-flow oxygen masks to high-flow nasal cannula (HFNC), noninvasive ventilation (NIV), or full mechanical ventilatory supportive measures.
Noninvasive Ventilation/HFNC
NIV avoids the complications of endotracheal intubation, and sedation has been used for the management of ARDS in pregnancy with an inspiratory pressure of 12–15 cm H2O and an expiratory pressure of 5–8 cm H2O.23 Supervised NIV can reduce the duration of ICU stay and hospitalization. There is an increased risk of gastric aspiration due to a combination of reduced tone of the lower gastroesophageal sphincter, increased intragastric pressure, and decreased gastric emptying.4 NIV is done only for alert and conscious parturients who retain protective airway reflexes, have a good respiratory drive, and have stable hemodynamics without severe acid–base disturbances.4
Our center has experience of using NIV in over 800 parturients with an excellent safety record. In protocolized (Fig. 5) and experienced centers, the risk of aspiration can be mitigated. Our center's protocol is as follows:
Fig. 5.

NIV in a term parturient with maternal and fetal monitoring
Mild-to-moderate ARDS
Short-term need (<48–72 hours) or post-extubation/as a weaning strategy
Hemodynamically stable parturient
Awake and responsive with good cough reflex
Parenteral acid aspiration prophylaxis (H2 blockers or proton pump inhibitors with metoclopramide)
Always propped-up position/lateral position
Small clear liquid feeds or nil by mouth [if continuous CPAP/pressure support ventilation (PSV)] by using conventional parenteral acid aspiration prophylaxis, propped-up position, and either nil by mouth. The indications and contraindication are the same as those for nonpregnant women. The following figure (Fig. 5) shows term antepartum patients with NIV being induced for labor with close fetal monitoring
Appropriate interface is very important. The most commonly used is orofacial or nasal. Helmets have also been used, but most patients develop claustrophobia with helmets (personal experience)
NIV has been found to be superior to HFNC in parturients with moderate-to-severe hypoxemia. However, for those who are claustrophobic, HFNC is a better option, if clinical targets are met
Proning (semiprone) is a relatively easier option in patients receiving NIV/HFNC, as they can do it on their own when properly explained
Mechanical Ventilation
Anticipate difficult intubation. CPAP/PSV or HFNC can be tried to build up FRC prior to intubating sick parturients with poor physiological reserve. The presence of mucosal edema, capillary engorgement, and increase in breast size in pregnant women necessitates that a 0.5-mm smaller endotracheal tube is used compared to the size used for nonpregnant women of similar height and age.4 We can start with a 7-mm endotracheal tube for most pregnant women.4
Several lung-protective strategies are considered for mechanical ventilation in parturients. These include low tidal volume—~6 mL/kg, low driving pressures (plateau pressure [Pplat]–PEEP), Pplat <30 cm H2O, and optimizing PEEP, particle flow rate >250 mm Hg (FiO2 < 0.5), and PaCO2 < 50 mm Hg. A previous study has reported a reduction in mortality when patients received lower tidal volumes (initial tidal volume of 6 mL/kg).15 These benefits of low tidal volumes are attributed to the reduction in overdistention of ventilated lungs that occurs with high regional volumes and pressures or volutrauma and barotrauma.16 Open lung ventilation strategies improve lung mechanics, oxygenation, and inflammatory markers.17 The strategy is aimed at the use of optimal lung recruitment to increase the fraction of the lung that is aerated so that the set tidal volume is delivered to the largest functional lung.17 PEEP benefits patients with ARDS by preventing the cyclic opening and closing of alveoli, enabling recruitment of collapsible lung units at the end of exhalation. There is no demonstrable benefit of high PEEP over low PEEP when low tidal volumes and limitations of Pplat are considered.18 The association of high airway pressures with poor outcomes in ARDS prompted a focus on the minimization of the Pplat. The physiologic parameter best associated with the outcomes is the driving pressure (Pplat–PEEP) and is determined by the delivered tidal volume and the compliance of the respiratory system.19 A few studies that looked at the possibility of decremental, physiologically targeted PEEP titration methods and esophageal manometry to titrate PEEP did not provide good results possibly due to the methodological limitations.20,21 Further studies are needed in this regard.
Adequate fetal oxygenation requires a PaO2 of 70 mm Hg, which corresponds to a maternal SpO2 of about 95%.9 A gradient of nearly 10 mm Hg is required for the clearance of fetal PaCO2 by the placenta.9 The limited evidence available suggests that PaCO2 levels of 45–55 mm Hg are reasonable in the latter part of pregnancy.10 Hence, permissive hypercapnia beyond PaCO2 is not a safe option from a fetal viewpoint.
The guidelines of the ARDS network study remain the standard that is followed in invasive ventilation in pregnant women.15 The tidal volume can be increased if Pplat remains <30 cm H2O and respiratory acidosis (PaCO2 > 65 mm Hg) persists despite high respiratory rates.22 A higher Pplat limit is considered, but the general opinion is that the ARDS network guidelines must be followed as it is lung compliance which is the major determinant of total respiratory compliance rather than the effect of pregnancy on chest wall compliance.22
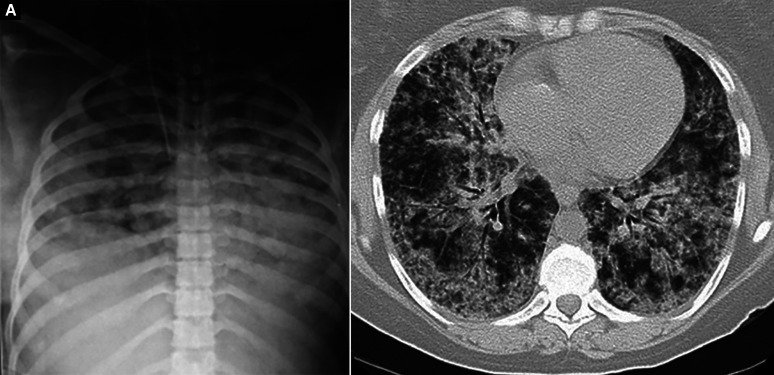
Several alternate strategies are proposed if refractory hypoxemia persists during pregnancy as shown in Figure 6. High-frequency oscillation ventilation is no longer used in the management of ARDS in pregnancy. Other alternate strategies include ECMO, prone position, venovenous-ECMO (VV-ECMO), and a combination of prone position and VV-ECMO, and informed decision on the timing of childbirth has to be a multidisciplinary decision at experienced centers.
Figs 6A and B.
(A) Bedside chest X-ray showing severe features of ARDS bilaterally due to H1N1 pneumonia; (B) CT scan of the chest showing severe ground glass opacities bilaterally with refractory hypoxemia, COVID-19 pneumonia
Prone Position
Prone position ventilation is recommended in parturients if there is a refractory hypoxemia with nonavailability/waiting for ECMO and a hemodynamically stable patient. Prone ventilation has been found effective in parturients with severe ARDS (Fig. 7). However, prone position ventilation is not an easy choice and has several limitations that include the difficulty to perform this on term antepartum patients, a hemodynamically unstable patient, the possibility of aortocaval compression (semiprone/lateral decubitus is recommended), imminent delivery, and the need for an experienced unit with a protocolized approach (sufficient experienced manpower).
Figs 7A and B.
Prone ventilation in a parturient with free abdominal wall to minimize aortocaval compression
Placing patients in the prone position has physiologic benefits that include improved oxygenation attributable to the homogenous distribution of perfusion and recruitment of collapsed lung units.16 The functional size of the lungs may be increased and reduces the risk of volutrauma/barotrauma.16 The PROSEVA trial26 reported a mortality benefit (32.8 vs 16.0% 28-day mortality) in patients who are placed in the prone position early in illness (<48 hours after ARDS onset) and who are maintained in the prone position for most of the day (up to 17 hours/day) and until the gas exchange is significantly improved. Duration of 8–20 hours of prone positioning has been reported in obstetric patients but these are from a few case reports.27 Further studies are necessary to determine the utility and applicability of prone positioning and to determine which subgroups may be more suitable for this procedure.
Extracorporeal Membrane Oxygenation
ECMO may be initiated early if a parturient is determined to have refractory hypoxemia although it exposes the fetus to the possible complications of systemic heparinization and extracorporeal circulation.4 ECMO also can influence the decision on cesarean sections due to an increased risk of thrombosis and bleeding associated with heparin. A previous study on the use of ECMO in pregnancy has reported that ECMO circuit–related complications were rare with a circuit change needed in two cases and no sudden circuit failure.24 However, bleeding was a common complication and led to large volumes of blood cell transfusion and was the main cause of mortality.24 Figure 8 shows a pregnant patient on VV-ECMO support.
Fig. 8.

Patient on VV-ECMO support
Extracorporeal life support (ECLS) must be considered if there is a mortality risk ≥50% which can be identified by a PaO2/FiO2 <150, a FiO2 >90%, and/or a Murray score of 2–3.25 ECLS is indicated if the mortality risk is ≥80% which can be identified by a PaO2/FiO2 <80, a FiO2 >90%, and/or a Murray score of 3–4.25 ECLS may also be considered if there is a severe air leak syndrome or PaCO2 >80 or inability to achieve safe inflation pressures.25
Fetal Monitoring
It is reasonable to monitor fetal heart rates daily and do a weekly fetal Doppler test with repeat tests based on fetal Doppler parameters and at least fortnightly monitoring of fetal growth. However, the primary focus is to stabilize maternal health and not alter decisions based on the fetal monitoring status alone. Radiological investigations like chest X-ray may be needed to monitor the health of the mother, and these can be achieved through well-collimated X-ray beams and abdominal shields.
Childbirth
The decision on the timing and mode of childbirth must be a multidisciplinary team decision. The risk and benefits to the mother and the fetus must be ascertained carefully and based on the underlying causes and progression of ARDS. If the fetus is viable, fetal monitoring can help ascertain fetal health till fetal maturity is achieved. Delivery can be planned if fetal maturity is achieved; however, it is not recommended to wait for fetal maturity in the presence of a decline in maternal health. The risk vs benefit to the health of the mother is the primary concern. The method of childbirth depends on what is considered safe for the mother. Decisions around cesarean section must consider the risks of bleeding and thrombosis.
Weaning and Rehabilitation
Patients requiring long-term mechanical ventilation or VV-ECMO may require delivery while on ventilatory support or while on ECMO. If on ECMO, anticoagulation is temporarily suspended for 48–72 hours and restarted with low-molecular-weight heparin to minimize the risk of postpartum hemorrhage.
Postdelivery, weaning becomes easy and can be fast-tracked by early extubation followed by NIV support.
Our center's experience, establishing early maternal bonding (Figs 9A and B) while on ventilatory support, minimizes the incidence of lactation failure and also motivates the parturients for early weaning. Also, passive and when possible active endurance building (Fig. 9C) by the dedicated physio and psychological rehab teams help these patients come back to normal routine rapidly and help in minimizing the long-term psychosocial issues.
Figs 9A to C.
(A) Early maternal and family bonding; (B) Early breastfeeding while on mechanical ventilatory support; (C) Early rehabilitation, ambulation while on ventilatory support
Conclusion
Management of ARDS in pregnancy requires a multidisciplinary team approach at experienced centers. Survival rates depend upon the etiology of ARDS and in experienced centers are greater than 95% in parturients requiring NIV alone, 8% and above in parturients mechanical ventilation and greater than 60% in patients requiring VV-ECMO. The decision to deliver and the mode of delivery have to be a multidisciplinary decision, mother's survival being the primary criteria. Postdelivery, early maternal bonding and rehabilitation help in faster recovery and also minimize lactation failure.
Footnotes
Source of support: Nil
Conflict of interest: None
Orcid
Sunil T Pandya https://orcid.org/0000-0002-7494-3058
Sai J Krishna https://orcid.org/0000-0001-5651-8915
References
- 1.Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 2.Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):69. doi: 10.1186/s13613-019-0540-9. 31197492 PMC6565761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riviello ED, Buregeya E, Twagirumugabe T. Diagnosing acute respiratory distress syndrome in resource limited settings: the Kigali modification of the Berlin definition. Curr Opin Crit Care. 2017;23(1):18–23. doi: 10.1097/MCC.0000000000000372. 27875408 [DOI] [PubMed] [Google Scholar]
- 4.Bhatia PK, Biyani G, Mohammed S, Sethi P, Bihani P. Acute respiratory failure and mechanical ventilation in pregnant patient: a narrative review of literature. J Anaesthesiol Clin Pharmacol. 2016;32(4):431–439. doi: 10.4103/0970-9185.194779. 28096571 PMC5187605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hegewald MJ, Crapo RO. Respiratory physiology in pregnancy. Clin Chest Med. 2011;32(1):1–13. doi: 10.1016/j.ccm.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Bobrowski RA. Pulmonary physiology in pregnancy. Clin Obstet Gynecol. 2010;53(2):285–300. doi: 10.1097/GRF.0b013e3181e04776. [DOI] [PubMed] [Google Scholar]
- 7.Crapo RO. Normal cardiopulmonary physiology during pregnancy. Clin Obstet Gynecol. 1996;39(1):3–16. doi: 10.1097/00003081-199603000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Templeton A, Kelman GR. Maternal blood-gases (PaO2-PaO2), hysiological shunt and VD/VT in normal pregnancy. Br J Anaesth. 1976;48(10):1001–1004. doi: 10.1093/bja/48.10.1001. [DOI] [PubMed] [Google Scholar]
- 9.Catanzarite V, Williams D, Wong D, Landers C, Cousins L, Schrimmer D. Acute respiratory distress syndrome in pregnancy and the puerperium: Causes, courses, and outcomes. Obstet Gynecol. 2001;97(5 Pt1):760–764. doi: 10.1016/s0029-7844(00)01231-x. [DOI] [PubMed] [Google Scholar]
- 10.Al-Ansari MA, Hameed AA, Al-jawder SE, Saeed HM. Use of noninvasive positive pressure ventilation during pregnancy: case series. Ann Thorac Med. 2007;2(1):23–25. doi: 10.4103/1817-1737.30358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mabie WC, Barton JR, Sibai BM. Adult respiratory distress syndrome in pregnancy. Am J Obstet Gynecol. 1992;167(4 Pt 1):950–957. doi: 10.1016/s0002-9378(12)80018-4. [DOI] [PubMed] [Google Scholar]
- 12.Smith JL, Thomas F, Orme JF, Clemmer TP. Adult respiratory distress syndrome during pregnancy and immediately postpartum. West J Med. 1990;153(5):508–510. 2260285 PMC1002600 [PMC free article] [PubMed] [Google Scholar]
- 13.Perry KG, Martin RW, Blake PG, Roberts WE, Martin JN. Maternal mortality associated with adult respiratory distress syndrome. South Med J. 1998;91(5):441–444. doi: 10.1097/00007611-199805000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Wanderer JP, Leffert LR, Mhyre JM, Kuklina EV, Callaghan WM, Bateman BT. Epidemiology of obstetric-related ICU admissions in Maryland: 1999-2008. Crit Care Med. 2013;41(8):1844–1852. doi: 10.1097/CCM.0b013e31828a3e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 16.Peck TJ, Hibbert KA. Recent advances in the understanding and management of ARDS. F1000Res. 2019;8(F1000 Faculty Rev-):1959. doi: 10.12688/f1000research.20411.1. 31824644 PMC6880255 [DOI] [Google Scholar]
- 17.Kacmarek RM, Villar J, Sulemanji D, Montiel R, Ferrando C, Blanco J, et al. Open lung approach for the acute respiratory distress syndrome: a pilot, randomized controlled trial. Crit Care Med. 2016;44(1):32–42. doi: 10.1097/CCM.0000000000001383. [DOI] [PubMed] [Google Scholar]
- 18.Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351(4):327–336. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 19.Amato MB, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–755. doi: 10.1056/NEJMsa1410639. [DOI] [PubMed] [Google Scholar]
- 20.Cavalcanti AB, Suzumura ÉA, Laranjeira LN, de Moraes Paisani D, Damiani LP, et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318(14):1335–1345. doi: 10.1001/jama.2017.14171. Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beitler JR, Sarge T, Banner-Goodspeed VM, Gong MN, Cook D, Novack V, et al. Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure-guided strategy vs an empirical high PEEP-FiO2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2019;321(9):846–857. doi: 10.1001/jama.2019.0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campbell LA, Klocke RA. Implications for the pregnant patient. Am J Respir Crit Care Med. 2001;163(5):1051–1054. doi: 10.1164/ajrccm.163.5.16353. [DOI] [PubMed] [Google Scholar]
- 23.Banga A, Khilnani GC. Use of non-invasive ventilation in a pregnant woman with acute respiratory distress syndrome due to pneumonia. Indian J Chest Dis Allied Sci. 2009;51(2):115–117. 19445449 [PubMed] [Google Scholar]
- 24.Nair P, Davies AR, Beca J, Bellomo R, Ellwood D, Forrest P, et al. Extracorporeal membrane oxygenation for severe ARDS in pregnant and postpartum women during the 2009 H1N1 pandemic. Intensive Care Med. 2011;37(4):648–654. doi: 10.1007/s00134-011-2138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moore SA, Dietl CA, Coleman DM. Extracorporeal life support during pregnancy. J Thorac Cardiovasc Surg. 2016;151(4):1154–1160. doi: 10.1016/j.jtcvs.2015.12.027. 26825433 [DOI] [PubMed] [Google Scholar]
- 26.Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 27.Samanta S, Samanta S, Wig J, Baronia AK. How safe is the prone position in acute respiratory distress syndrome at late pregnancy? Am J Emerg Med. 2014;32(6):687.e1–687.e3. doi: 10.1016/j.ajem.2013.12.021. 24412021 [DOI] [PubMed] [Google Scholar]