Abstract
Context
The change in understanding of dental caries which is now believed to be a reversible lesion has led to the change in its management.
Aim
To evaluate the remineralizing potential of three remineralizing agents [casein phosphopeptide (CPP)—amorphous calcium phosphate (ACP), CPP-ACP + F, and beta-tricalcium phosphate (β TCP) + F] and their effect on microhardness of enamel using Vickers microhardness test.
Materials and method
Forty freshly extracted premolars, extracted for orthodontic purpose were collected and specimen prepared. The specimens were equally divided into four groups. Baseline surface microhardness measurement was taken for the specimens. Demineralization of enamel was carried out by keeping the specimens in 20 mL of demineralizing solution for 72 hours, and microhardness was evaluated. Remineralizing agents CPP-ACP, CPP-ACP + F, and β TCP + F was applied to Group A, Group B, and Group C, respectively for 28 days and microhardness was evaluated again. Group D was kept as control group. Statistical analysis was done by One-way ANOVA test. Percentage microhardness recovery was calculated to evaluate the regain in microhardness after remineralization and thus assess the remineralizing efficacy of the agents.
Results
After demineralization surface microhardness of enamel decreased to the range of Vickers hardness number (VHN) 155-167 but after application of remineralizing agents surface microhardness for Group B was found to be highest, in other words, VHN 240.78 followed by Group C, in other words, VHN 214.29 and Group A the least VHN 197.90.
Conclusion
The result of this study concludes that surface microhardness of enamel decreased after demineralization procedure and increased after application of all the remineralizing agents. The highest increase was seen in group tested with CPP-ACP + F followed by β TCP and least for CPP-ACP. The values for all the three groups were higher than the control so we can conclude that all the agents can be used as remineralizing agent with CPP-ACP + F being the best among the three.
How to cite this article
Bhat DV, Awchat KL, Singh P, et al. Evaluation of Remineralizing Potential of CPP-ACP, CPP-ACP + F and β TCP + F and Their Effect on Microhardness of Enamel Using Vickers Microhardness Test: An In Vitro Study. Int J Clin Pediatr Dent 2022;15(S-2):S221-S225.
Keywords: Demineralization, Remineralization, Surface microhardness, Vickers hardness test
Introduction
The oral cavity is a constant interplay of demineralization and remineralization.1 There is a is continuous exchange of ions between dental hard tissues and oral environment.2 The hardness of tooth depends on the proportion between demineralization and remineralization.1 .
Imbalance in this exchange of ions leading to shift toward more demineralization lead to white spot lesion.3 These white spot lesions are initial sign of caries process.4 If not treated lesions it may progress to frank cavitation which may require surgical management.5
However, if intervention is done at the initial stage remineralization of white spot lesion is possible. This forms the basis of Minimal Intervention Dentistry.1 The clinically proven anticaries benefits of fluoride have provided a solid benchmark for new formulations or prospective technologies.6,7 Significant research in the development new casein phosphopeptide (CPP) sequence is going on.7 Increased calcium and phosphate concentrations in the oral environment by the use of tri-calcium phosphate agent can also increase remineralization of tooth.8
In this study, demineralization and remineralization was analyzed by using surface microhardness measurements. The aim of the present study was to evaluate the effect of demineralization and to determine remineralizing potential of (casein phosphopeptide amorphous calcium phosphate) CPP-ACP, CPP-ACP + fluoride and (tri-calcium phosphate) β TCP + fluoride on surface microhardness of enamel.
Materials and Methods
Composition and pH values of demineralizing and remineralizing agents used in the study is mentioned below:
Demineralizing agent : COMPOSITION 2.2 mmol CaCl2, 2.2 mmol NaH2PO4, 0.05 M Lactic acid, 0.2 ppm Fluoride (pH of the solution was adjusted with 50% NaOH to 4.5).
Remineralizing Agents
CPP-ACP (GC tooth mousse): COMPOSITION Pure water, glycerol, 10% CPP-ACP (10,000 ppm), D-sorbitol, propylene glycol, silicon dioxide, titanium dioxide, xylitol, phosphoric acid, flavoring agent, zinc oxide, sodium saccharin, ethyl-p-hydroxybenzoate, magnesium oxide, guar gum, propyl p-hydroxybenzoate, butyl p- hydroxybenzoate.
CPP-ACP + F (GC tooth mousse plus) : COMPOSITION Pure water, glycerol, 10% CPP-ACP (10,000 ppm), D-sorbitol, propylene glycol, silicon dioxide, titanium dioxide, xylitol, phosphoric acid, 0.2% sodium fluoride (900 ppm), flavoring agent, zinc oxide, sodium saccharin, ethyl-p-hydroxybenzoate, magnesium oxide, guar gum, propyl p-hydroxybenzoate, butyl p- hydroxybenzoate.
Tricalcium phosphate (Clinprocrème) : COMPOSITION Water, sorbitol, hydrated silica, glycerin, polyethylene-polypropylene glycol, flavoring agent, polyethylene glycol, sodium lauryl sulfate, titanium dioxide, carboxymethyl cellulose, sodium saccharin, 0.21% sodium fluoride (950 ppm), and 0.5% Tri-Calcium Phosphate (500 ppm).
Artificial saliva : COMPOSITION Na3PO4 - 3.90 mmol, NaCl - 4.29 mmol, KCl - 17.98 mmol, CaCl2 - 1.10 mmol, MgCl2 - 0.08 mmol, H2SO4 - 0.50 mmol, NaHCO3 - 3.27 mmol, distilled water and the pH was set at a level of 7.2.
Forty freshly extracted first premolars, extracted for orthodontic reason were collected. Ethical consent for using the extracted teeth for the study was obtained from the patients and patient's guardian as applicable. Only teeth devoid of any caries, hypo plastic lesion, stains, cracks, AND erosion were included for specimen preparation. After removal of radicular part of each tooth, coronal part was partially embedded on the top of partially set acrylic resin for sample preparation. An acid resistant nail varnish was applied around the exposed tooth surface leaving a window of 3 × 3 mm at the center. The specimens were randomly divided in four groups (Group A, B, C, and D) containing 10 specimens each.
Surface microhardness of each specimen was measured using Vickers microhardness tester Lieca Japan, Tokyo. A constant load of 25 grams for 5 seconds was applied (Fig. 1: Vickers hardness tester). The Vickers hardness number (VHN) of five indentations at spacing of 100 microns were taken and the average value was considered the surface microhardness number (SMH) of the corresponding specimen.
Fig. 1.

Vickers hardness tester
After baseline surface microhardness determination, enamel was demineralized by immersing the specimen into glass container containing 20 mL of demineralization solution for 72 hours in an incubator at a temperature of 37°C. Surface microhardness was evaluated for all samples after demineralization.
The specimens were then subjected to the following surface treatments:
Group A: A sufficient layer of CPP-ACP cream (GC tooth mousse) was applied by an applicator brush and left for 3 minutes.
Group B: A sufficient layer of CPP-ACP + F cream (GC tooth mousse plus) was applied and left for 3 minutes.
Group C: A sufficient layer of β-TCP + F (Clipro creme) was applied and left for 3 minutes.
Group D: This group without any surface treatment was taken as a control group.
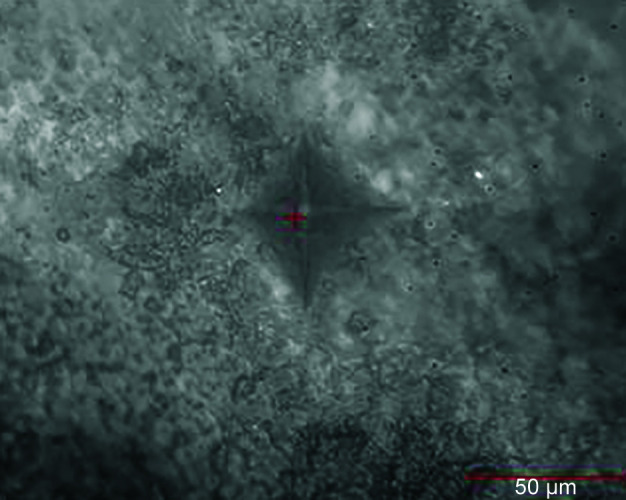
After application of remineralizing agent the specimens were washed and stored in artificial saliva. This treatment was done twice daily for 28 days and again the surface microhardness was assessed (Fig. 2—Normal sample, Fig. 3—Sample after remineralization of Group A, Fig. 4—Sample after remineralization of Group B & Fig. 5— Sample after remineralization of Group C).
Fig. 2.
Normal sample
Fig. 3.

Sample after remineralization of group A
Fig. 4.

Sample after remineralization of group B
Fig. 5.

Sample after remineralization of group C
After getting the microhardness values the microhardness recovery in percentage was calculated for each tooth sample in all groups by using following formula:
Microhardness recovery (%)
Remineralized hardness - Demineralized hardness
= ------------------------------- × 100
Baseline hardness - Demineralized hardness
Results
Baseline surface microhardness measurements of the specimen is shown in Table 1.
Table 1.
Showing mean and standard deviation value of baseline surface microhardness, surface microhardness after demineralization, surface microhardness after remineralization and percentage microhardness recovery of specimens in the four groups
| Procedure | Specimens | Group A | Group B | Group C | Group D |
|---|---|---|---|---|---|
| 1. Baseline surface microhardness | Mean | 251.81 | 305.10 | 282.20 | 257.74 |
| Standard deviation | ± 39.70 | ± 29.75 | ± 43.53 | ± 42.61 | |
| 2. Surface microhardness after demineralization | Mean | 156.59 | 167.01 | 157.99 | 159.84 |
| Standard deviation | ± 12.34 | ± 16.59 | ± 20.73 | ± 30.73 | |
| 3. Surface microhardness after remineralization | Mean | 197.90 | 240.78 | 214.29 | 152.70 |
| Standard deviation | ± 19.16 | ± 20.34 | ± 40.58 | ± 31.87 | |
| 4. Percentage microhardness recovery | Mean | 45.0403 | 53.0650 | 50.9873 | -7.285 |
| Standard deviation | ± 13.21 | ± 11.10 | ± 10.80 | ± 1.82 |
Samples in all the groups showed decreased surface hardness values after demineralization as compared to the baseline values. The surface microhardness value of group B after remineralization is highest among all groups while it is lowest for group D. By comparing values in the Table 1, it is seen that the surface microhardness of all specimens except group D increases after remineralization (Figs 6 and 7).
Fig. 6.

Graphical representation of baseline surface microhardness compared with surface microhardness of enamel after demineralization and remineralization procedures in various groups
Fig. 7.

Graph shows percentage surface microhardness recovery of enamel after the remineralization procedures in various groups
From the Table 2, it is observed that value of p > 0.05, in other words, 0.301, thus it can be concluded that there is not any statistically significant difference between Group A, Group B, and Group C.
Table 2.
Shows one-way ANOVA test to compare between group A, group B, and group C
| Source | Degree of freedom | Sum of squares | Mean sum of squares | ‘F‘ | p value |
|---|---|---|---|---|---|
| Factor | 2 | 0.347 | 0.173 | 1.26 | 0.301 |
| Error | 27 | 3.728 | 0.138 | ||
| Total | 29 | 4.075 |
Discussion
Dental caries is a prevalent chronic disease that has been a concern for human beings.9 First sign of caries is a white spot lesion. If treated at this stage it can be remineralized but if left untreated it may progress to form a frank cavity. White spot lesion is the first clinical presentation of dental caries (Margolis et al.).5
Enamel remineralization is not a new topic but nowadays remineralization of both noncavitated and cavitated lesion is attempted. The strategy for carrying out remineralization is to provide ions (calcium, phosphate, and fluoride) directly to where and when they are needed.10
Though clinical studies are better for determining remineralizing efficacy of agents but in vitro studies are also a reliable alternative.11 Featherstone in the year 1981 used surface microhardness profiles of enamel to compare changes during demineralization and remineralization.12
In vitro surface microhardness studies have the advantage of being simple, easy to conduct, noninvasive and is not affected by patient burnout, also the same specimen can be used for multiple times which reduces the chances of experimental error.11,13
In Vickers hardness method, the length of indentation suggests mineral loss or gain. Increase in length of indentation suggests that the tissue has lost mineral and on the other hand decrease in length indicates gain of mineral. To calculate the Vickers Diamond Pyramid hardness number, length of diagonals of the indentation are measured and the mean is calculated. Mean value is used with load to determine the value of microhardness.14
Initially, in this study baseline surface microhardness values were obtained for all specimens which were in the range of VHN 245-310. These values satisfies the VHN range of normal enamel tissue according to studies done by S Priyadarshini,9 S Lata,13 S Jabbarifar,15 I Fadhil,16 MR Malekipour,17 N Shrinivasan.18
An in vitro preparation of caries like lesion in the enamel provides lesion of about same depth in all samples which provides standard to compare between different remineralizing agents.19 In the present study, the specimens kept in the demineralization solution for 72 hours at 37°C created a subsurface demineralization of approximately 150 microns deep simulating an early enamel lesion. After demineralization surface microhardness values decreased for all specimens of each group which is in accordance with studies conducted by S Lata,13 N Srinivasan,18 JDB Featherstone,12 MR Maleki-Pour,17 I Fadhil,16 SE Jabbarifar15, and FC Rehder Neto.11
In this study, we used artificial saliva to store specimens during remineralization treatment which mimic the oral environment since the remineralizing agents need to be in contact with saliva to enhance the remineralization.11
In the present study microhardness mean values increased after remineralization for Group A, in other words, 197.90 ± 19.16, for Group B, in other words, 240.78 ± 20.34 and for Group C, in other words, 214.29 ± 40.58 but no increase in microhardness was seen for Group D, in other words, 152.70 ± 31.87 which act as a negative control. No mineral regain occurs in group D. This may be because of equilibrium of calcium and phosphate ion content of the specimen and remineralizing agent, in other words, artificial saliva.13
The mean value for group B, in other words, 240.78 ± 20.34 is more than group A, in other words, 197.90 ± 19.16. so we can say that efficacy of group B, in other words, CPP-ACP + fluoride is better than group A, in other words, CPP-ACP. Incorporation of fluoride to CPP-ACP produce an additive anticariogenic effect through the formation of stabilized amorphous calcium fluoride phosphate.20 This result of the present study is similar with studies carried out by Reynolds21, Walsh22, Kumar20, and Cross7.
The mean value of group B, in other words, 240.78 ± 20.34 is more than group C, in other words, 214.29 ± 40.58 therefore remineralizing potential of group B, in other words, CPP-ACP + F is more than group C, in other words, β-TCP + F. This result is in accordance with the study conducted by Gupta and Prakash. In the year 2011, Gupta and Prakash stated that ACP within CPP-ACP + F do not react with fluoride to precipitate into calcium fluoride due to low fluoride concentration as in TCP + F after contact with the saliva.22
Percentage microhardness recovery was calculated to evaluate regain in microhardness after remineralization and thus the efficacy of different remineralizing agents. Increased in microhardness recovery with Group B, in other words, 53.06 ± 11.10 and Group C, in other words, 50.98 ± 10.80 than Group A, in other words, 45.04 ± 13.21 can be attributed to the presence of fluoride in group B and C. Fluoride improves the crystalline tooth structure with less internal crystalline stress and strain.3
Reason for greater microhardness recovery of group B, in other words, 53.06 ± 11.10 than Group C, in other words, 50.98 ± 10.80 may be attributed to presence of Casein phosphopeptides in group B which interact with calcium, phosphate, and fluoride ions to produce a stabilized Amorphous calcium fluoride phosphate phase.23
This protein nanotechnology combines proteins from bovine milk resulting in formation of amorphous calcium phosphate (ACP). The proportion of calcium ions phosphate ions and CPP is 144, 96, and 6, respectively.69 Under neutral and alkaline conditions, the casein phosphopeptides stabilize calcium and phosphate ions forming metastable solutions that are supersaturated with respect to the calcium phosphate phases.23
To compare statistically remineralizing potential of the remineralizing agents (i.e., CPP-ACP + F, CPP-ACP & TCP + F) further ANOVA test was carried out for group A, B, and C. It was found that as the value of p > 0.05, in other words, p = 0.301 difference between the group A, B, and C is statistically nonsignificant. This is in accordance with the study conducted by S Lata,13 Elsayad,23 Kumar.20
In vitro remineralization may be quite different when dynamic complex changes taking place in oral cavity and in vitro setup may not mimic in vivo conditions.24
Conclusion
Following conclusions can be drawn from the results:
After demineralization surface microhardness of enamel get reduced, in other words, loss of minerals from the surface of enamel takes place.
After application of remineralizing agents surface microhardness of enamel increased, in other words, regain of minerals on the surface of enamel takes place.
Among three experimental remineralizing agents used in the present study CPP-ACP + Fluoride has highest remineralizing potential followed by TCP + Fluoride and CPP-ACP.
Hence, it can be concluded that combination of fluoride and metastable solution of calcium and phosphate produced better remineralization than combination of crystalline calcium, phosphate with fluoride and metastable solution of calcium phosphate alone.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Rao A, Malhotra N. The role of remineralizing agents in dentistry: a review. Compend Contin Educ Dent. 2011 [PubMed] [Google Scholar]
- 2.Susana MW, Catia R. Microhardness of enamel restored with fluoride and non-fluoride releasing dental materials. Braz Dent J. 2001;12(01):35–38. [PubMed] [Google Scholar]
- 3.Jaime AC, Livia MAT. Enamel remineralization: controlling the caries disease or treating early caries lesions. Braz Oral Res. 2009:23. doi: 10.1590/s1806-83242009000500005. [DOI] [PubMed] [Google Scholar]
- 4.Cochrane NJ, Cai F, Huq NL, et al. New approaches to enhanced remineralization of tooth enamel. J Dent Res. 2010;89(11):1187–1197. doi: 10.1177/0022034510376046. [DOI] [PubMed] [Google Scholar]
- 5.Slayton RL, Bryers JD, Milgrom P. Biotechnology and biomaterials to reduce the caries epidemic. BMC Oral Health. 2006;6:S9. doi: 10.1186/1472-6831-6-S1-S1. (Suppl 1): [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ten Cate JM, Duijsters PP. Alternating demineralization and remineralization of artificial enamel lesions. Caries Res. 16(03):201–210. doi: 10.1159/000260599. [DOI] [PubMed] [Google Scholar]
- 7.Nongonierma AB, FitzGerald RJ. Biofunctional properties of caseinophosphopeptides in the oral cavity. Caries Res. 2012;46:234–267. doi: 10.1159/000338381. [DOI] [PubMed] [Google Scholar]
- 8.Pradeep K, Rao PK. Remineralizing agents in the non-invasive treatment of early carious lesions. Int J Dent. 2011;1(02):73–84. [Google Scholar]
- 9.Priyadarshini S, Raghu R, Shetty A, et al. Effect of organic verses inorganic fluoride on enamel microhardness: an in vitro study. J Conserv Dent. 2013;16(03):203–207. doi: 10.4103/0972-0707.111314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malcmacher L. Minimal intervention dentistry and caries prevention. Academy of Dental Therapeutics and Stomatology. 2011 [Google Scholar]
- 11.Rehder Neto FC, Maeda FA, Turssi CP, et al. Potential agents to control enamel caries-like lesions. J Dent. 2009;37:786–790. doi: 10.1016/j.jdent.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Pinkham. Texbook of pediatric dentistry. Infancy through adolescence [Google Scholar]
- 13.Pai D, Bhat SS, Taranath A, et al. Use of laser fluorescence and scanning electron microscope to evaluate remineralization of incipient enamel lesions remineralized by topical application of casein phospho peptide amorphous calcium phosphate (CPP-aCP) containing cream. J Clin Pediatr Dent. 2008;32(03):201–206. doi: 10.17796/jcpd.32.3.d083470201h58m13. [DOI] [PubMed] [Google Scholar]
- 14.Arends J, Bosch JJ. Demineralisation and remineralisation evaluation techniques. J Dent Res. 1992;71:924–928. doi: 10.1177/002203459207100S27. [DOI] [PubMed] [Google Scholar]
- 15.Lata S, Varghese NO, Varughese JM. Remineralization potential of fluoride and amorphous calcium phosphate-casein phospho peptide on enamel lesions: an in vitro comparative evaluation. J Conserv Dent. 2010;13(01):42–46. doi: 10.4103/0972-0707.62634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fadhil I. Effect of casein phosphopeptides stabilize amorphous calcium phosphate on hardness of enamel. J Bagh Coll Dentistry. 2010;22(03):62–64. [Google Scholar]
- 17.Maleki-Pour MR, Shirani F, Mirzakoochaki P, et al. Changes in bleached enamel microhardness after application of fluoride and CPP-ACP. J Islam Dent Assoc Iran. 2012;24(01):15–20. [Google Scholar]
- 18.Srinivasan N, Kavitha M, Loganathan SC. Comparison of the remineralization potential of CPP-ACP and CPP-ACP with 900 ppm fluoride on eroded human enamel: an in situ study. Arch Oral Biol. 2010;55:541–544. doi: 10.1016/j.archoralbio.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Karlinsey RL, Mackey AC, Walker ER. Surfactant-modified b-TCP: structure, properties, and in vitro remineralization of subsurface enamel lesions. J Mater Sci. 2010;21:2009–2020. doi: 10.1007/s10856-010-4064-y. [DOI] [PubMed] [Google Scholar]
- 20.Kumar VLN, Itthagarun A, King NM. The effect of casein phosphopeptide-amorphous calcium phosphate on remineralization of artificial caries-like lesions: an in vitro study. Australian Dent J. 2008;53:34–40. doi: 10.1111/j.1834-7819.2007.00006.x. [DOI] [PubMed] [Google Scholar]
- 21.Reynolds EC. Casein phosphopeptide-amorphous calcium phosphate: the scientific evidence. Adv Dent Res. 2009;21(01):25–29. doi: 10.1177/0895937409335619. [DOI] [PubMed] [Google Scholar]
- 22.Walsh LJ. Contemporary technologies for remineralization therapies: a review. Int Den 2009; 11(06):6–16. [Google Scholar]
- 23.Elsayad I, Sakr A, Badr Y. Combining casein phosphopeptide-amorphous calcium phosphate with fluoride: synergistic remineralization potential of artificially demineralized enamel or not. J Biomed Opt. 2009;14(04) doi: 10.1117/1.3210780. [DOI] [PubMed] [Google Scholar]
- 24.Yamazaki H, Margolis HC. Enhanced enamel remineralization under acidic conditions in vitro. J Dent Res. 2008;87(06):569–574. doi: 10.1177/154405910808700612. [DOI] [PubMed] [Google Scholar]


