Hyperkalemic emergency (HE) refers to life-threatening hyperkalemia consisting of a high serum potassium level with severe complications (e.g., dysrhythmias, cardiac arrest, or myopathy).[1] Hyperkalemic emergencies (HEs) are commonly encountered (2%–3%) in the emergency department (ED).[2,3] In-hospital mortality rate for hospitalized hyperkalemic patients is about 14.1% and 4.5 times higher than that of those with normal potassium.[4] Quick recognition and treatment are critical for decreasing morbidity and mortality.[5] Nevertheless, great variety and sparse evidence lie in current HE treatment. In this article, we will review the current medical literature on the treatment of HEs and propose a treatment flowchart for HEs (Figure 1).
Figure 1.

A flowchart for treatment of hyperkalemic emergencies. ECG: electrocardiogram; POC: point of care; K+: potassium; IV: intravenous; SZC: sodium zirconium cyclosilicate.
THRESHOLDS FOR INITIATING TREATMENT OF HEs
No consistent thresholds for potassium levels warranting treatment have been proposed.[3] First, higher serum potassium is associated with higher mortality. A retrospective multicenter study revealed that higher serum potassium levels, severe underlying diseases, and developing acute kidney injury (AKI) from normal baseline renal function were associated with higher mortality.[6] Second, electrocardiogram (ECG) changes indicate higher risk of mortality in hyperkalemia.[3,7] Elevated serum potassium in cardiac myocytes results in cardiac instability inducing ventricular fibrillation and cardiac arrest.[8] Higher mortality occurs in patients with serum potassium ≥6.0 mmol/L possessing new ECG changes than those without ECG changes.[3,9]
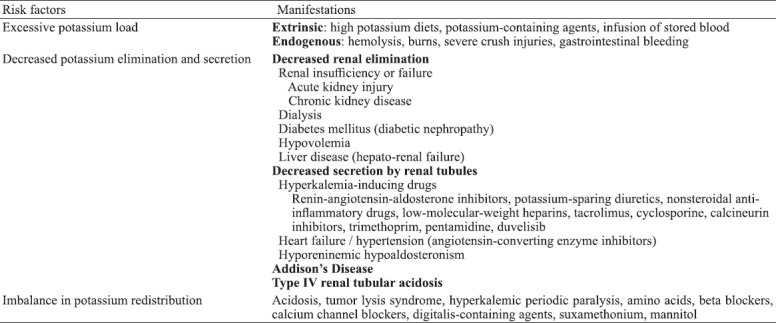
Based on present studies and guidelines, we recommend treatment should be initiated under the following circumstances: (1) serum potassium ≥6.0 mmol/L with or without ECG changes; (2) presence of more than two ECG changes, clinical manifestations of hyperkalemia, and risk factors for hyperkalemia (Table 1), with serum potassium 5.5–5.9 mmol/L;[9] (3) a clinical course likely to progress to hyperkalemia, such as in anuresis patients complicated by rhabdomyolysis or tumor lysis syndrome, even if the serum potassium is <6.0 mmol/L.[7] Nonetheless, more evidence-based studies are necessitated concerning thresholds for HE treatment.
Table 1.
Risk factors for hyperkalemia
TREATMENT
Cardiac myocyte protection—intravenous (IV) calcium salts
Calcium salts antagonize the cardiotoxic effects of hyperkalemia, restore the cardiac membrane potential, and stabilize the myocardium.[10] A total of 10 mL of 10% calcium gluconate or one ampule of calcium chloride should be administered intravenously if new and potentially fatal ECG changes including absent P waves, widened QRS, peaked T waves, sine waves, ventricular arrhythmias, or cardiac arrest, appear.[11] Efficacy of IV calcium salts can be seen within 5 min. If life-threatening ECG changes persist after 5–10 min, repeat calcium salts are necessary.[12]
Since calcium salts do not lower serum potassium levels, they need to be combined with potassium-lowering treatments. More proven side effects of calsium chloride include tissue necrosis, which can be avoided by using a central venous catheters. Hypotension can be induced by the peripheral vasodilation and bradycardia effects of calcium chloride infusions.[7,8] Advanced studies are needed because the efficacy of calcium salts was more based on case reports and anecdotal experience rather than large prospective cohort study.[13]
Shifting serum potassium intracellularly
Insulin and glucose
The combination of insulin and glucose is rapid and a mainstay of treatment for HEs.[2] Insulin increases the activity of sodium- and potassium-activated adenosine triphosphatase (Na+-K+-ATPase) in skeletal muscle cells thus decreasing serum potassium levels.[12] When blood glucose is ≥13.9 mmol/L and serum potassium exceeds 6.0 mmol/L, insulin could be given alone to lower serum potassium. If blood glucose is <13.9 mmol/L, an IV bolus injection of 10 units of regular insulin should be followed by a 25 g (50 mL of a 50% solution) bolus of dextrose. Alternatively, IV infusion with 10 units of insulin in 25 g dextrose (250 mL of a 10% solution) over 60 min is another option. Of the two, IV boluses are the faster means of lowering serum potassium in HEs.[14]
One in six hyperkalemic patients developed hypoglycemia between 1–3 h after receiving an insulin-glucose treatment,[2,7] which suggests that current glucose and insulin regimens have much room for improvement. An IV infusion of 10% dextrose at a rate of 50–75 mL/h and close monitoring of glucose after IV insulin-glucose treatment for 5–6 h is recommended to avoid iatrogenic hypoglycemia.[15]
Nebulized beta-2 agonists
Beta-2 agonists can also promote potassium moving intracellularly by activating Na+-K+-ATPase.[8] If calcium salts and insulin-glucose fail to control HEs, nebulized beta-2 agonists (albuterol 10–20 mg) should be given as an adjuvant treatment but should not be given as monotherapy due to some hyperkalemia patients being unresponsive to beta-2 agonists.[3,9] Beta-2 agonists induce a mild hyperglycemic state, so simultaneous administration of beta-2 agonists with IV insulin-glucose can achieve better efficacy and lower the risk of hypoglycemia.[7] However, high doses of beta-2 agonists may cause side effects such as palpitations, tremors, headaches, and angina, particularly in patients with coronary heart disease. Therefore, cardiac monitoring is recommended in HEs, particularly in those patients receiving beta-2 agonists.[16]
Sodium bicarbonate
Theoretically, infusing sodium bicarbonate elevates blood pH, promotes the movement of hydrogen ions extracellularly, and activates the sodium-hydrogen exchange and Na+-K+-ATPase, causing potassium to move intracellularly.[15] In clinical practice, however, sodium bicarbonate scarcely lowers serum potassium at all in patients without metabolic acidosis.[17] In patients with metabolic acidosis, the serum potassium lowering effect is not apparent until 4–6 h after infusion.[18] Additionally, excessive sodium bicarbonate induces hypernatremia and fluid overload.[8] In conclusion, sodium bicarbonate is not recommended as a sole agent in HEs in the absence of metabolic acidosis.[3]
Removing potassium from the body
Urinary excretion—diuretics
Loop diuretics increase renal potassium excretion and are particularly beneficial in patients with normal to moderately compromised kidney function or volume overload.[19] Diuretics should be given with caution in hemodynamically unstable patients. Loop diuretics are very effective and can achieve synergistic effects when combined with other diuretics like thiazides.[13] However, diuretics as a monotherapy for HEs are far from enough.
Fecal excretion—potassium binders
Sodium polystyrene sulfate (SPS) is a nonselective potassium binder.[8] SPS has a lot of disadvantages such as uncertain efficacy, risk of hypocalcemia and hypomagnesemia, and significant gastrointestinal adverse effects, life-threatening colonic necrosis, or perforations.[2] SPS is therefore not recommended for HEs unless dialysis or other drugs that remove potassium from the body are ineffective or not available. SPS 15–60 g can be given orally and may be repeated 4–6 h later, if necessary.[20] Sorbitol is no longer suggested to be given with SPS because it may augment the risk of colonic necrosis and perforations.[21]
Sodium zirconium cyclosilicate (SZC) and patiromer are both novel non-absorbed selective cation exchangers and potassium binders.[22] When hemodialysis is not immediately available, 10 g of SZC three times a day for up to 72 h or 8.4 g of patiromer once daily is recommended alongside standard treatment with insulin-glucose and beta-agonists in HEs, which may theoretically postpone or even avoid dialysis. SZC has a relatively fast onset of action of less than 1 h and is also 25 times more selective than patiromer for potassium and is 9.3 times more effective in lowering serum potassium than SPS.[23] SZC and patiromer have higher tolerability than SPS due to less gastrointestinal side-effects, although SZC still has some adverse effects like hypertension, sodium overload, and edema.[24] Constipation, diarrhea, and hypomagnesemia are common adverse effects of patiromer.[7,8]
Potassium binders are independent of kidney function and can be prescribed to anuric HE patients. Studies pertaining to the efficacy and safety of potassium binders in lowering serum potassium were overwhelmingly conducted in mild to moderate chronic hyperkalemia patients. More studies related to whether potassium binders are effective in acute, high-potassium level HE patients is still needed.[25]
Dialysis
Dialysis is the definitive and the most effective treatment for HEs and the only treatment that achieves normalized serum potassium within 4 h.[2,7] Rossignol et al[12] suggested that emergency dialysis should be considered in patients with persistent ECG changes or those with an insufficient response to beta-2 agonists or insulin-glucose, particularly in patients with renal insufficiency. Pirklbauer[25] indicated that emergency blood purification was mandatory whenever acute renal failure presented with severe hyperkalemia due to the impending risk of fatal arrhythmias. However, whether dialysis is performed in HE symptomless patients with chronic kidney disease remains controversy. Notwithstanding its extraordinary capacity to lower serum potassium, dialysis is invasive, costly, and may not immediately be available in the ED.[4]
MONITORING
Frequent monitoring of serum potassium and glucose is necessary for timely treatment adjustments. Medications that lower serum potassium work together most efficiently for about 2 h. A rebound effect due to additional potassium being released from intracellular stores may appear at 2–3 h if further treatments eliminating potassium from the body have not been instituted.[13,19] Thus, re-evaluation of serum potassium is recommended at 1–2 h after medication administration.[9]
CONCLUSIONS
Timely treatment can avoid life-threatening complications of hyperkalemia. However, treatment of hyperkalemia in the ED is highly variable, and no agreed flowchart exists because prospective, randomized controlled trials are minimal. Nevertheless, there is widespread agreement on three approaches to treatment: cardiac myocyte protection, shifting serum potassium intracellularly, and removing potassium from the body. Systematic treatment with frequent monitoring and evaluation according to the proposed flowchart might help ED clinicians make quick and reasonable decisions and improve outcomes.
Footnotes
Funding: This research received no funding from any funding agency, commercial or not-for-profit entity.
Ethics approval: Not applicable.
Conflicts of interest: Authors have no financial or other conflicts of interest related to this submission.
Contributors: YW proposed the study and wrote the first draft. JX and JHW edited the manuscript. All authors reviewed and approved the final version of the manuscript.
REFERENCES
- 1.Wu L, Fang Y, Zhang BR. Andersen-Tawil syndrome associated with myopathy. World J Emerg Med. 2020;11(4):267–9. doi: 10.5847/wjem.j.1920-8642.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peacock WF, Rafique Z, Clark CL, Singer AJ, Turner S, Miller J, et al. Real world evidence for treatment of hyperkalemia in the emergency department (REVEAL-ED):a multicenter, prospective, observational study. J Emerg Med. 2018;55(6):741–50. doi: 10.1016/j.jemermed.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Rafique Z, Peacock F, Armstead T, Bischof JJ, Hudson J, Weir MR, et al. Hyperkalemia management in the emergency department:an expert panel consensus. J Am Coll Emerg Physicians Open. 2021;2(5):e12572. doi: 10.1002/emp2.12572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rafique Z, Kosiborod M, Clark CL, Singer AJ, Turner S, Miller J, et al. Study design of Real World Evidence for Treatment of Hyperkalemia in the Emergency Department (REVEAL-ED):a multicenter, prospective, observational study. Clin Exp Emerg Med. 2017;4(3):154–9. doi: 10.15441/ceem.17.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karmacharya P, Poudel DR, Pathak R, Rettew A, Alweis R. Acute hyperkalemia leading to flaccid paralysis:a review of hyperkalemic manifestations. J Community Hosp Intern Med Perspect. 2015;5(3):27993. doi: 10.3402/jchimp.v5.27993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.An JN, Lee JP, Jeon HJ, Kim DH, Oh YK, Kim YS, et al. Severe hyperkalemia requiring hospitalization:predictors of mortality. Crit Care. 2012;16(6):R225. doi: 10.1186/cc11872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rafique Z, Chouihed T, Mebazaa A, Frank Peacock W. Current treatment and unmet needs of hyperkalaemia in the emergency department. Eur Heart J Suppl. 2019;21(Suppl A):A12–9. doi: 10.1093/eurheartj/suy029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sidhu K, Sanjanwala R, Zieroth S. Hyperkalemia in heart failure. Curr Opin Cardiol. 2020;35(2):150–5. doi: 10.1097/HCO.0000000000000709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alfonzo A, Soar J, MacTier R, Fox J, Shillday I, Nolan J, et al. Clinical practice guidelines:treatment of acute hyperkalaemia in adults. Available at: https://ukkidney.org .
- 10.Wang CH, Huang CH, Chang WT, Tsai MS, Yu PH, Wu YW, et al. The effects of calcium and sodium bicarbonate on severe hyperkalaemia during cardiopulmonary resuscitation:a retrospective cohort study of adult in-hospital cardiac arrest. Resuscitation. 2016;98:105–11. doi: 10.1016/j.resuscitation.2015.09.384. [DOI] [PubMed] [Google Scholar]
- 11.Liu MY, Rafique Z. Acute management of hyperkalemia. Curr Heart Fail Rep. 2019;16(3):67–74. doi: 10.1007/s11897-019-00425-2. [DOI] [PubMed] [Google Scholar]
- 12.Rossignol P, Legrand M, Kosiborod M, Hollenberg SM, Peacock WF, Emmett M, et al. Emergency management of severe hyperkalemia:guideline for best practice and opportunities for the future. Pharmacol Res. 2016;113(Pt A):585–91. doi: 10.1016/j.phrs.2016.09.039. [DOI] [PubMed] [Google Scholar]
- 13.Long B, Warix JR, Koyfman A. Controversies in management of hyperkalemia. J Emerg Med. 2018;55(2):192–205. doi: 10.1016/j.jemermed.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Sterns RH, Grieff M, Bernstein PL. Treatment of hyperkalemia:something old, something new. Kidney Int. 2016;89(3):546–54. doi: 10.1016/j.kint.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Mandelberg A, Krupnik Z, Houri S, Smetana S, Gilad E, Matas Z, et al. Salbutamol metered-dose inhaler with spacer for hyperkalemia:how fast?How safe? Chest. 1999;115(3):617–22. doi: 10.1378/chest.115.3.617. [DOI] [PubMed] [Google Scholar]
- 16.Greenberg A. Hyperkalemia:treatment options. Semin Nephrol. 1998;18(1):46–57. [PubMed] [Google Scholar]
- 17.Blumberg A, Weidmann P, Ferrari P. Effect of prolonged bicarbonate administration on plasma potassium in terminal renal failure. Kidney Int. 1992;41(2):369–74. doi: 10.1038/ki.1992.51. [DOI] [PubMed] [Google Scholar]
- 18.Lindner G, Burdmann EA, Clase CM, Hemmelgarn BR, Herzog CA, Małyszko J, et al. Acute hyperkalemia in the emergency department:a summary from a Kidney Disease:Improving Global Outcomes Conference. Eur J Emerg Med. 2020;27(5):329–37. doi: 10.1097/MEJ.0000000000000691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gruy-Kapral C, Emmett M, Santa Ana CA, Porter JL, Fordtran JS, Fine KD. Effect of single dose resin-cathartic therapy on serum potassium concentration in patients with end-stage renal disease. J Am Soc Nephrol. 1998;9(10):1924–30. doi: 10.1681/ASN.V9101924. [DOI] [PubMed] [Google Scholar]
- 20.Sterns RH, Rojas M, Bernstein P, Chennupati S. Ion-exchange resins for the treatment of hyperkalemia:are they safe and effective? J Am Soc Nephrol. 2010;21(5):733–5. doi: 10.1681/ASN.2010010079. [DOI] [PubMed] [Google Scholar]
- 21.Rafique Z, Liu MY, Staggers KA, Minard CG, Peacock WF. Patiromer for treatment of hyperkalemia in the emergency department:a pilot study. Acad Emerg Med. 2020;27(1):54–60. doi: 10.1111/acem.13868. [DOI] [PubMed] [Google Scholar]
- 22.Kosiborod M, Rasmussen HS, Lavin P, Qunibi WY, Spinowitz B, Packham D, et al. Effect of sodium zirconium cyclosilicate on potassium lowering for 28 days among outpatients with hyperkalemia:the HARMONIZE randomized clinical trial. JAMA. 2014;312(21):2223–33. doi: 10.1001/jama.2014.15688. [DOI] [PubMed] [Google Scholar]
- 23.Cooper K. Letter to the editor regarding “patiromer for the treatment of hyperkalemia”. Expert Rev Clin Pharmacol. 2020;13:1283–4. doi: 10.1080/17512433.2020.1828542. [DOI] [PubMed] [Google Scholar]
- 24.Pergola PE, Spiegel DM, Warren S, Yuan JW, Weir MR. Patiromer lowers serum potassium when taken without food:comparison to dosing with food from an open-label, randomized, parallel group hyperkalemia study. Am J Nephrol. 2017;46(4):323–32. doi: 10.1159/000481270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pirklbauer M. Hemodialysis treatment in patients with severe electrolyte disorders:management of hyperkalemia and hyponatremia. Hemodial Int. 2020;24(3):282–9. doi: 10.1111/hdi.12845. [DOI] [PMC free article] [PubMed] [Google Scholar]


