Abstract
A woman in her 50s presented with diminution of vision in her left eye (OS) 4 days after COVISHIELDTM vaccination. She had been diagnosed with non-arteritic anterior ischaemic optic neuropathy (NA-AION) of right eye (OD) 8 months earlier. The present episode revealed a best-corrected visual acuity (BCVA) of 20/50 in OD and 20/20 in OS with grade 1 relative afferent pupillary defect. Fundus evaluation showed pale disc in OD and temporal disc oedema in OS. Humphrey’s visual field analysis showed incomplete inferior altitudinal defect in OD and a centro-caecal scotoma in OS. Systemic investigations were normal. OS was diagnosed with NA-AION. She was started on oral aspirin 75 mg. At 1-month follow-up, disc oedema of OS had resolved with BCVA maintaining at 20/20. The patient was lost to follow-up later. The relationship between the vaccine and the ocular event is temporal with no causal association.
Keywords: COVID-19, Eye, Immunological products and vaccines, Medical management, Neuroopthalmology
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection causing coronavirus disease 2019 (COVID-19) pandemic has severely affected the health infrastructure worldwide. Recent estimates by WHO suggest 3.3 million deaths globally.1
Various vaccines have been formulated to negate the ill effects of the pandemic. However, several ophthalmic manifestations have been reported following these vaccines like episcleritis, scleritis, uveitis, multifocal choroiditis, acute macular neuroretinopathy, Vogt-Koyanagi-Harada disease, central serous chorioretinopathy, herpes zoster reactivation or acute retinal necrosis.2–9
Neuro-ophthalmological adverse events have also been reported following COVID-19 vaccination which includes optic neuritis, non-arteritic anterior ischaemic optic neuropathy (NA-AION), postchiasmatic visual pathway involvement, cranial nerve palsies of sixth and seventh nerves.10–17
Reports of NA-AION following COVID-19 vaccination are now available in the literature as one of the adverse ocular events.12–14
Case presentation
A woman in her 50s presented to us with sudden onset of painless diminution of vision of 4 days duration in her left eye (OS). She had received first dose of COVISHIELDTM vaccine 4 days earlier. She had no systemic symptoms associated with administration of vaccine. She had been diagnosed with NA-AION of right eye (OD) 8 months earlier. She was treated with oral prednisolone (30 mg) tapered over 2.5 months by the consulting neurologist. Subsequently, 1 month following the steroid treatment, she was detected to have diabetes mellitus and was started on oral metformin 250 mg. Two months later, the antidiabetic medication was stopped due to good glycaemic control, but the patient continued to self-medicate with metformin.
Previous presentation 8 months earlier showed a Snellen’s best-corrected visual acuity (BCVA) of 20/36 in OD and 20/20 in OS. Relative afferent pupillary defect (RAPD) was noted in OD with normal pupillary examination in OS.
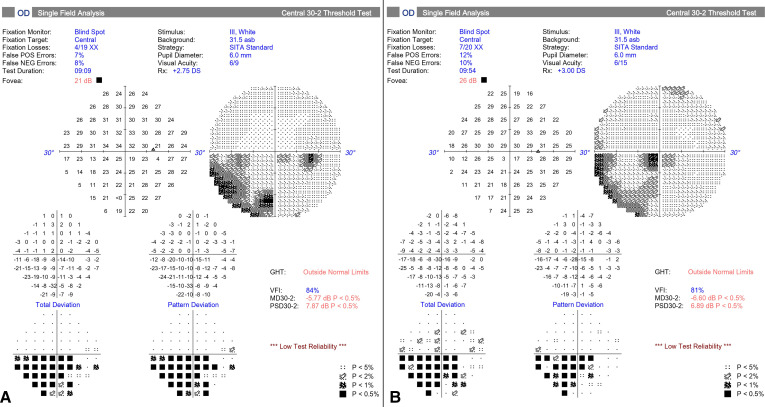
Ocular examination at this presentation revealed BCVA of 20/50 OD and 20/20 OS. Anterior segment examination was normal in both the eyes except nuclear sclerosis grade 2 in OD and early posterior subcapsular cataract in OS. Grade 1 RAPD was noted in OS (figure 1).
Figure 1.
Infrared photograph of the pupil in bright light at presentation showing relative afferent pupillary defect in left eye.
Fundus assessment of OD 8 months earlier showed a crowded hyperaemic disc with peripapillary oedema and fibrous remnant nasally (figure 2A) while OS was normal (figure 3A). Colour vision of OD was abnormal and OS was normal with Ishihara™ screening test.
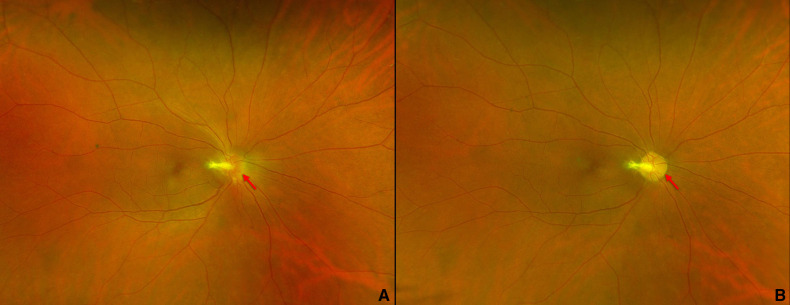
Figure 2.
Fundus photograph of right eye showing (A) crowded hyperaemic disc with peripapillary oedema (red arrow) with fibrous remnant nasally at 8 months earlier (B) fibrous remnant at disc and pale disc with well-defined margins (red arrow) at presentation now.
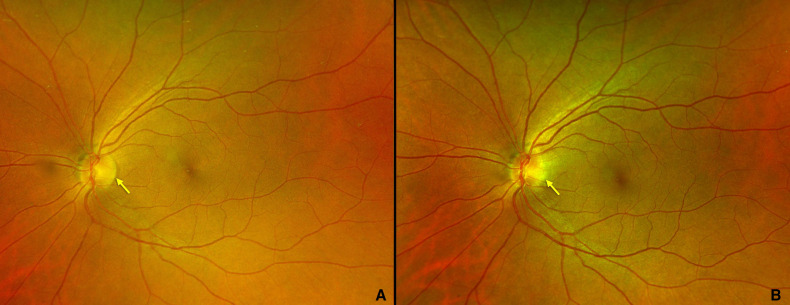
Figure 3.
Fundus photograph of left eye showing (A) well defined disc margin (yellow arrow) at 8 months earlier, (B) blurred temporal disc margin (yellow arrow) with cup disc ratio of 0.2:1 at presentation now.
Posterior segment evaluation at this presentation showed clear anterior vitreous in both eyes (OU) with fibrous remnant at disc and disc pallor in OD (figure 2B). Cup disc ratio could not be assessed in OD. Blurring of temporal disc margin with hyperaemia and cup disc ratio of 0.2:1 was noted in OS (figure 3B). Colour vision was abnormal in OU.
Investigations
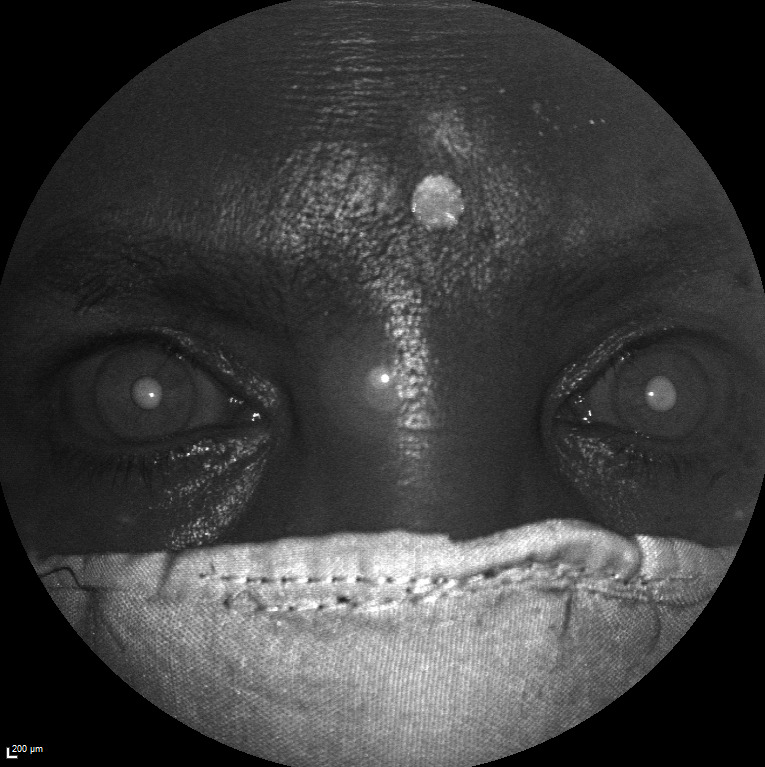
Spectral domain optical coherence tomography (SD-OCT) of retinal nerve fibre layer (RNFL) of OS showed peripapillary swelling temporal to the disc (figure 4). Humphrey’s visual field analysis (HFA) of OS done 8 months earlier (figure 5A) was normal and now had a centro-caecal scotoma (figure 5B). Loss of perifoveal halo was seen in OS in pseudocolour image of the multicolour imaging using SpectralisTM.
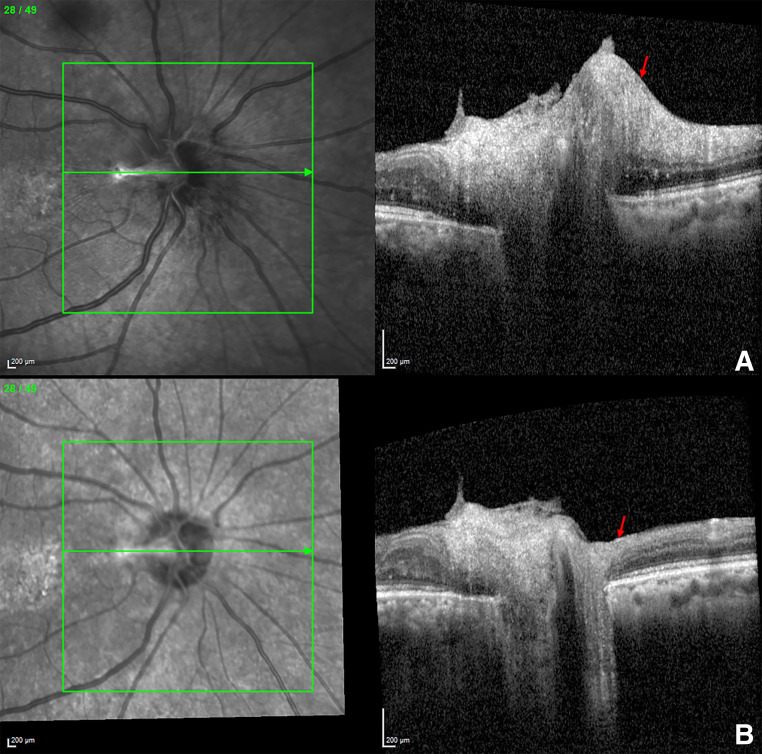
Figure 4.
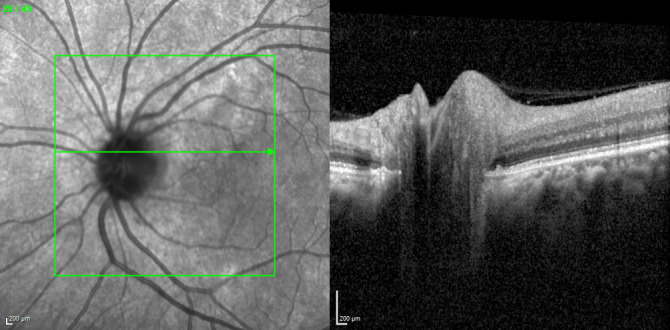
Spectral domain optical coherence tomography (SD-OCT) of retinal nerve fibre layer image of left eye showing peripapillary swelling temporal to the disc.
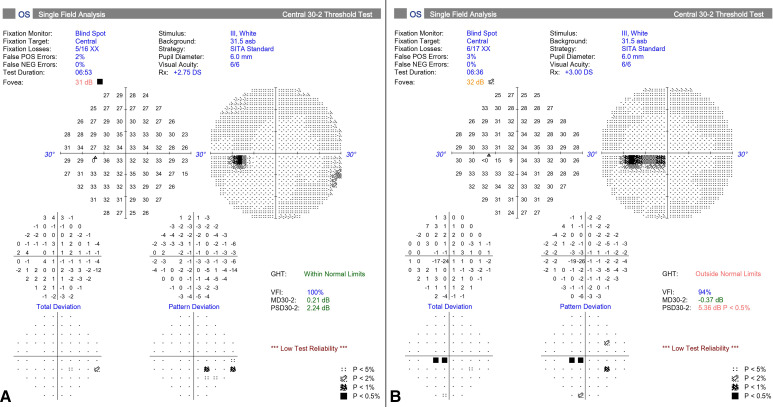
Figure 5.
Humphrey’s visual field analysis of left eye (OS) showing (A) normal fields at 8 months earlier (B) centrocaecal scotoma at presentation now.
Previous presentation 8 months earlier her SD-OCT RNFL of OD showed peripapillary swelling (figure 6) and SD-OCT macula showed inner retinal swelling.
Figure 6.
Spectral domain optical coherence tomography image of retinal nerve fibre layer of right eye showing (A) peripapillary swelling (red arrow) with hyperreflective band into vitreous cavity correlating with the fibrous remnant at 8 months earlier, (B) significant reduction in peripapillary swelling (red arrow) at presentation now.
HFA in OD of OD 8 months earlier revealed incomplete inferior altitudinal scotoma in OD (figure 7A), which persisted even at this presentation (figure 7B).
Figure 7.
Humphrey’s visual field analysis of right eye (OD) showing (A) incomplete inferior altitudinal scotoma at 8 months earlier, (B) reduction in the extent of inferior altitudinal scotoma at presentation now. GHT, glaucoma hemi field test; NEg, Negative; POS, positive; PSD, pattern standard deviation; VFI, visual field indices.
Blood investigations (table 1) done 8 months back did not show any systemic involvement.
Table 1.
Shows investigations done at first presentation
| Blood investigations | Patient | Normal values |
| Complete blood count | Normal | Normal |
| Erythrocyte sedimentation rate | 20 | 0–29 mm/hour |
| C reactive protein | 0.9 | 0.8–1.0 mg/dL |
| Rheumatoid factor | <9.4 | 0–20 IU/mL |
| Treponema pallidum haemagglutination | Non-reactive | Non-reactive |
| HIV tridot screening test | Non-reactive | Non-reactive |
| Serum vitamin D levels | 48.12 | >20 ng/mL |
| Serum ACE levels | 36 | 12–68 U/L |
| Antineutrophilic antibody | 0.75 | <1:160 |
| Lipid profile | Normal | Normal |
| Serum creatinine | 0.82 | 0.6–1.0 mg/dL |
Reverse-transcriptase PCR (RT-PCR) test for SARS-CoV-2 was negative in our patient at both presentations. Chest X-ray, urine analysis and MRI of orbit and brain were within normal limits. Mantoux test was negative.
Treatment
She was started on oral aspirin 75 mg by the neurologist. The patient took the medication for a month.
Outcome and follow-up
A month later, the BCVA in OS was 20/20 at 1 month with resolved disc oedema. The patient was lost to follow-up later.
Discussion
Epidemiology
In adults over the age of 50, NA-AION is the most common cause of optic neuropathy.18 In USA, the NA-AION prevalence ranges between 2.3 and 10.2 per 100 000. It is more common in Caucasians due to small optic disc cups, which are the greatest risk factor for developing NA-AION and less commonly seen in people of African origin as they tend to have larger cup to disc ratio.19
Aetiology
NA-AION has been strongly associated with risk factors like diabetes mellitus, hypertension, hypercholesterolaemia, cardiovascular disease, cerebrovascular disease and obstructive sleep apnoea.20 Obstructive sleep apnoea has also been recognised more recently to also be an independent risk factor for NA-AION, which is likely due to its effect on nocturnal blood pressure.21
In men, the use of sildenafil/tadalafil (a phospodiesterase (PDE-5) inhibitor)) may also contribute to the occurrence of NA-AION.22 23 PDE-5 inhibitors are also weak inhibitors of phosphodiesterase type six functions in phototransduction. However, NA-AION cannot be explained by phosphodiesterase type 6 inhibition. The vasodilator effect of PDE-5 inhibitors may be considered in the aetiology of NA-AION but no clear evidence seems available.24
COVID-19 has been implicated as a possible cause of NA-AION.25–27 The postulated mechanisms include hypercoagulable and hyperinflammatory state post-COVID-19, which lead to microangiopathic and thrombotic events in the body including the eye.27
Raised anticardiolipin antibody has been noted in a case of NA-AION.28
Pathogenesis
Crowded discs or ‘disc-at-risk’ is the strongest risk factor for developing NA-AION. A disc-at-risk is characterised as optic nerve head (ONH) that has a small diameter and small cup-to-disc ratio, typically 0.2 or less.
While the exact pathogenesis of an NA-AION has not been elucidated, the prevailing theory is that it is caused by hypoperfusion of the short posterior ciliary arteries supplying the optic nerve. In a disc-at-risk, ONH oedema induced by ischaemic injury is thought to cause compression of the axons within a smaller, rigid scleral tunnel20 leading to apoptosis and death of the ganglion cells whose axons comprise the optic nerve most often in the superior half of the ONH.19 29 30
Arteriosclerosis of branches of ophthalmic artery and intimal thickening of short posterior ciliary arteries may be seen in patients with diabetes mellitus, hypertension and hyperlipidaemia.31 Optic disc drusen can also lead to axonal compression within the tight confines of the ONH.19
Diagnosis
The diagnosis of NA-AION is usually clinical. Patients present with a typical history of acute, painless, unilateral vision loss and have the classic findings on fundus examination including a hyperaemic and swollen optic nerve with peripapillary splinter haemorrhages and a fellow eye with a small cup to disc ratio. Mostly, no additional testing is required.
Investigations
Visual fields are mostly altitudinal, probably due to semicircle distribution of short posterior ciliary arteries supplying the ONH.29 There are different types of visual field defects described in NA-AION. Hayreh and Zimmermann described different types of field defects in NA- AION. These included generalised field defects with or without scotoma within 30* of visual field, inferior or superior altitudinal defects with or without sparing of central 5*, quadrantic defects, constricted visual fields and superior or inferior arcuate defects.32
Another useful investigation is OCT of optic disc and the peripapillary area. It may show thickening of the RNFL.19
Differential diagnosis
The differential diagnosis that should be considered would be demyelinating optic neuritis and antibody-mediated (aquaporin-4 and antimyelin oligodendrocyte glycoprotein (MOG) antibody) optic neuritis. Demyelinating optic neuritis patients have pain on eye movements and majority of them recover complete visual function unlike those with NA-AION. Patients with anti-MOG-associated optic neuritis may have a similar clinical presentation but visual prognosis is more favourable compared with those with NA-AION.
Arteritic anterior ischaemic optic neuropathy (AAION) secondary to giant cell arteritis (GCA) in patients over 60 years should be considered as a differential diagnosis. Vision loss due to GCA could also be due to central retinal artery occlusion. These patients have headache, jaw claudication, scalp tenderness, fever and other systemic symptoms and serum markers like erythrocyte sedimentation rate and C reactive protein are together highly suggestive of the disease.33
Compressive optic neuropathies can present with swollen optic disc, but their onset is slow unlike the acute onset of NA-AION.34
If there is an accompanying pain associated with optic nerve swelling, the following diagnoses may have to be considered. Central nervous system inflammatory diseases like multiple sclerosis or neuromyelitis optica, intracranial hypertension or hypotension, optic neuropathies secondary to ischaemic (GCA), immunomediated (sarcoidosis, Wegener’s granulomatosis), neoplastic (myeloma, germinoma, fibrous dysplasia), infective (bacterial, viral, TB) diseases have to be borne in mind and investigated accordingly.34
Optic neuritis was one of the differential diagnoses in our female patient with features of centrocaecal scotoma on HFA. Optic neuritis is more prevalent in females.35 The features which were against classical optic neuritis/retrobulbar neuritis included absence of pain on eye movement with normal MRI brain and orbit.
Optic neuritis masquerade with abnormal HFA should lead us to consider possibility of migraine or a cerebrovascular event.36
All cases of optic neuropathy should undergo imaging to rule out intraorbital/cranial pathology.
In our patient, blood investigations, chest X-ray and urine analysis ruled out infectious aetiology of optic neuritis. Disc at risk (cup disc ratio of 0.2) in OS with previous history of contralateral (OD) NA-AION favoured a diagnosis of NA-AION in OS.
Ischaemic optic neuropathy has also been reported with SARS-CoV-2 infection. SARS-CoV-2-associated endotheliopathy could be the likely hypothesis for this.37 Prone positioning which has been recommended for COVID-19 patients for improving oxygen saturation in lungs, could also play a role in causing NA-AION.38 It is postulated that prone position can cause intraocular pressure fluctuations by mechanisms like orbital compression and increased central venous pressure, further reducing perfusion of ONH.38 However RT-PCR ruled out active COVID-19 in our patient.
Management of NA-AION
NA-AION management is challenging with no effective treatment. One of the very few randomised controlled clinical trials in neuro-ophthalmology evaluating whether patients with NA-AION would benefit from ONH decompression via vitrectomy and demonstrated that surgery was not beneficial and potentially harmful.39
Intravitreal injections of bevacizumab, as well as triamcinolone, have been tried with disappointing results as well.40
A clinical trial evaluating intravitreal injection of QRK207, a caspase 2 inhibitor preventing apoptosis, in patients with recent (within 14 days from onset) onset of NA-AION did not demonstrate its efficacy and was stopped early.19
Subcutaneous injections of RPh201, an isolated botanical extract of gum mastic, for patients who had an onset of NA-AION within 1–5 years prior to enrolment was a feasibility trial which supported a requirement for a large trial.41 In the study, RPh201 two times weekly for 26 weeks at a dose of 20 mg to participants with previous NA-AION did not raise any safety concerns. Some improvements in visual function were observed in this small Phase 2a study. They concluded that efficacy of RPh201 in improving visual function needs to be further investigated in adequately powered phase 3 studies.41
Outcome
Ischaemic optic neuropathies lead to atrophy to the optic nerve in one or both the eyes and can lead to permanent blindness.19
Prognosis
The Ischaemic Optic Neuropathy Decompression Trial showed that 30% of NA-AION patients would regain three or more lines of vision at 2 years follow-up, 20% would lose three or more lines of vision and in the majority of patients, the vision would remain unchanged after the onset.39
Vaccination, optic neuritis and NA-AION
Neuro-ophthalmological manifestations such as optic neuritis have been previously reported with various viral vaccines like rabies, Measles, Mumps, Rubella (MMR), smallpox, influenza, hepatitis (A, B), polio or yellow fever.26
Neuromyelitis optica and other neuroimmunological disorders have also been described in the literature following COVID-19 vaccination42–44
NA-AION in OS was diagnosed our patient after the first dose of COVISHIELDTM vaccination, which the patient had received 4 days earlier and to the best of our knowledge may be the first report. There is no causality associated with this ocular event.
NA-AION has been reported following influenza and COVID-19 vaccination.12 45
Tsukii et al12 reported an unilateral NA-AION 7 days after receiving first dose of Pfizer-BioNTechTM COVID-19 vaccine. Similar to our patient, they found diffuse optic disc oedema with a BCVA of 20/20 and RAPD. However, unlike our case, the contralateral eye was normal in their patient. HFA in their patient noted an incomplete altitudinal field defect whereas similar field defect was seen in OD of our patient but a centro-caecal field defect in the OS. They observed resolution of disc oedema with observation for 2 months and maintenance of BCVA of 20/20. Similar to Tsukii et al, we also treated the patient conservatively with only oral aspirin.12 Nachbor et al13 described a 64-year-old woman with type 2 diabetes mellitus who developed acute unilateral painless visual loss. She was subsequently diagnosed with progressive NA-AION which had worsened after the second dose of BNT162b2 COVID-19 vaccine.13 They postulated that the vaccine-induced inflammatory cascade could have led to an immune-mediated microangiopathy in the ‘at-risk’ disc.
Bolletta et al in their series on ocular complications following COVID-19 vaccination reported a 46-year-old female patient who had unilateral sectoral papillary oedema and was diagnosed to have NA-AION. The patient did not have any other systemic risk factors and all the investigations were negative. Brain imaging was also normal.14
Our case report can be categorised in the possible adverse drug reaction (ADR) (total score 1–4) according to Naranjo Algorithm-ADR Probability Scale.46
COVISHIELDTM vaccine is a ChAdOx1 nCoV- 19 Corona Virus Recombinant Vaccine which does not contain aluminium salts.47 The excipients in COVISHIELDTM vaccine could likely regulate the immune response and the associated side effects.
It is postulated in the literature that immune-mediated pathogenetic mechanisms may be associated with vaccination.48 49 Moreover, presence of adjuvants in the vaccines like aluminium salts, toll-like receptor agonists or mineral oils can also exaggerate this immune response.50
Another hypothesis could be that the extracellular RNA in COVID-19 vaccines can promote coagulation and thrombus formation51 causing vessel occlusion, which could likely be a reason for NA-AION. In our patient the disc oedema resolved after starting oral aspirin 75 mg.
Occurrence of NA-AION following vaccination may be a temporal event. Ophthalmologists must seek a history of previous COVID-19 vaccination or a recent COVID-19 when evaluating patients with optic neuropathy.
Patient’s perspective.
I was very anxious after I developed blurring of vision after COVID-19 vaccination. I already had decreased vision in my other eye few months earlier. I was worried that my only seeing eye now had problem. I came immediately and with the reassurance the doctor gave me along with the oral medicines, I felt better after 1 month of treatment.
Learning points.
Previous non-arteritic anterior ischaemic optic neuropathy (NA-AION) in the contralateral eye could be a risk factor for the other eye.
NA-AION is a clinical diagnosis and all other causes of optic nerve swelling need to be investigated and ruled out if there are atypical clinical features.
The COVID-19 and adverse ocular event like NA-AION in the absence of other systemic risk factors may be temporally occurring with no causal association.
Acknowledgments
Dr Sujit Kumar, Neurologist, Apollo Hospitals, Bengaluru and Narayana Nethralaya, Bengaluru.
Footnotes
Twitter: @saneyedoc
Contributors: SS: design, concept, data acquisition, data analysis, manuscript writing, manuscript editing, intellectual content. IA: data acquisition, data analysis, manuscript writing, manuscript editing. AR: data acquisition, data analysis, manuscript writing, manuscript editing, intellectual content. RS: data acquisition, data analysis, manuscript editing. intellectual content. All authors gave the final approval.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
References
- 1.The impact of COVID-19 on global health goals, 2021. Available: https://www.who.int/news-room/spotlight/the-impact-of-covid-19-on-global-health-goals [Accessed 21 Jan 2022].
- 2.Pichi F, Aljneibi S, Neri P, et al. Association of ocular adverse events with inactivated COVID-19 vaccination in patients in abu dhabi. JAMA Ophthalmol 2021;139:1131–5. 10.1001/jamaophthalmol.2021.3477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goyal M, Murthy SI, Annum S. Bilateral multifocal choroiditis following COVID-19 vaccination. Ocul Immunol Inflamm 2021;29:753–7. 10.1080/09273948.2021.1957123 [DOI] [PubMed] [Google Scholar]
- 4.Koong LR, Chee WK, Toh ZH, et al. Vogt-Koyanagi-Harada disease associated with COVID-19 mRNA vaccine. Ocul Immunol Inflamm 2021;29:1212–5. 10.1080/09273948.2021.1974492 [DOI] [PubMed] [Google Scholar]
- 5.Fowler N, Mendez Martinez NR, Pallares BV, et al. Acute-Onset central serous retinopathy after immunization with COVID-19 mRNA vaccine. Am J Ophthalmol Case Rep 2021;23:101136. 10.1016/j.ajoc.2021.101136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mishra SB, Mahendradas P, Kawali A. Reactivation of varicella zoster infection presenting as acute retinal necrosis post COVID 19 vaccination in an Asian Indian male. Eur J Ophthalmol 2021;18:11206721211046485. 10.1177/11206721211046485 [DOI] [PubMed] [Google Scholar]
- 7.Sanjay S, Ponnuru D, Kumar S. Herpes zoster reactivation after COVID-19 vaccination in patients with autoimmune diseases. Indian J Rheumatol 2021. 10.4103/injr.injr_137_21 [DOI] [Google Scholar]
- 8.Sanjay S, Gadde SGK, Kumar Yadav N, et al. “Bilateral Sequential Acute Macular Neuroretinopathy in an Asian Indian Female with β Thalassemia Trait following (Corona Virus Disease) COVID-19 Vaccination and Probable Recent COVID Infection- Multimodal Imaging Study.”. Ocul Immunol Inflamm 2022;14:1–6 https://pubmed.ncbi.nlm.nih.gov/35050826/ 10.1080/09273948.2022.2026978 [DOI] [PubMed] [Google Scholar]
- 9.Sanjay S, Kawali A, Mahendradas P. Acute macular neuroretinopathy and COVID-19 vaccination. Indian J Ophthalmol 2022;70:345–6. 10.4103/ijo.IJO_2542_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pawar N, Maheshwari D, Ravindran M, et al. Ophthalmic complications of COVID-19 vaccination. Indian J Ophthalmol 2021;69:2900–2. 10.4103/ijo.IJO_2122_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leber HM, Sant'Ana L, Konichi da Silva NR, et al. Acute thyroiditis and bilateral optic neuritis following SARS-CoV-2 vaccination with CoronaVac: a case report. Ocul Immunol Inflamm 2021;29:1200–6. 10.1080/09273948.2021.1961815 [DOI] [PubMed] [Google Scholar]
- 12.Tsukii R, Kasuya Y, Makino S. Nonarteritic anterior ischemic optic neuropathy following COVID-19 vaccination: consequence or coincidence. Case Rep Ophthalmol Med 2021;14. 10.1155/2021/5126254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nachbor K, Naravane AV, Adams OE. Non-Arteritic anterior ischemic optic neuropathy associated with COVID-19 vaccination. J Neuro-Ophthalmol 2021;00:1–3. 10.1097/WNO.0000000000001423 [DOI] [PubMed] [Google Scholar]
- 14.Bolletta E, Iannetta D, Mastrofilippo V, et al. Uveitis and other ocular complications following COVID-19 vaccination. J Clin Med 2021;10:5960. 10.3390/jcm10245960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jumroendararasame C, Panyakorn S, Othong R, et al. Transient visual field loss after COVID-19 vaccination: experienced by ophthalmologist, case report. Am J Ophthalmol Case Rep 2021;24:101212. 10.1016/j.ajoc.2021.101212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reyes-Capo DP, Stevens SM, Cavuoto KM. Acute abducens nerve palsy following COVID-19 vaccination. J Aapos 2021;25:302–3. 10.1016/j.jaapos.2021.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shemer A, Pras E, Einan-Lifshitz A, et al. Association of COVID-19 vaccination and facial nerve palsy: a case-control study. JAMA Otolaryngol Head Neck Surg 2021;147:739–43. 10.1001/jamaoto.2021.1259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hayreh SS. Ischemic optic neuropathy. Prog Retin Eye Res 2009;28:34–62. 10.1016/j.preteyeres.2008.11.002 [DOI] [PubMed] [Google Scholar]
- 19.Raizada K, Margolin E. Non-arteritic anterior ischemic optic neuropathy. Treasure Island (FL): StatPearls Publishing, 2022. [PubMed] [Google Scholar]
- 20.Archer EL, Pepin S. Obstructive sleep apnea and nonarteritic anterior ischemic optic neuropathy: evidence for an association. J Clin Sleep Med 2013;9:613–8. 10.5664/jcsm.2766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamann S, Malmqvist L, Wegener M, et al. Young adults with anterior ischemic optic neuropathy: a multicenter optic disc drusen study. Am J Ophthalmol 2020;217:174–81. 10.1016/j.ajo.2020.03.052 [DOI] [PubMed] [Google Scholar]
- 22.Galvez-Ruiz A, Arishi N, Sequential AN. Sequential, non-arteritic anterior ischemic optic neuropathy in patients taking sildenafil: a report of ten cases. Saudi J Ophthalmol 2013;27:241–6. 10.1016/j.sjopt.2013.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shir Yen W, Yathavan S, Ramli MA, et al. Bilateral sequential Non-arteritic anterior ischemic optic neuropathy (NAION). Cureus 2021;13:e19408. 10.7759/cureus.19408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verit A. Non-arteritic anterior ischemic optic neuropathy, PDE-5 inhibitors, and amiodarone: may there be a sex hormone effect for the eye? Med Hypotheses 2007;69:470–1. 10.1016/j.mehy.2006.12.014 [DOI] [PubMed] [Google Scholar]
- 25.Sanoria A, Jain P, Arora R, et al. Bilateral sequential non-arteritic optic neuropathy post-COVID-19. Indian J Ophthalmol 2022;70:676–9. 10.4103/ijo.IJO_2365_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Babazadeh A, Barary M, Ebrahimpour S, et al. Non-arteritic anterior ischemic optic neuropathy as an atypical feature of COVID-19: a case report. J Fr Ophtalmol 2022;45:e171–3. 10.1016/j.jfo.2021.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Golabchi K, Rezaee A, Aghadoost D, et al. Anterior ischemic optic neuropathy as a rare manifestation of COVID-19: a case report. Future Virol 2021. 10.2217/fvl-2021-0068. [Epub ahead of print: 12 01 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Serrador-García M, Santos-Bueso E, Sáenz-Francés F, et al. Non-arteritic anterior ischemic optic neuropathy as first manifestation of antiphospholipid syndrome in a young patient. Arch Soc Esp Oftalmol 2014;89:368–72. 10.1016/j.oftale.2014.08.018 [DOI] [PubMed] [Google Scholar]
- 29.Sharma RA, Newman NJ, Biousse V. New concepts on acute ocular ischemia. Curr Opin Neurol 2019;32:19–24. 10.1097/WCO.0000000000000634 [DOI] [PubMed] [Google Scholar]
- 30.Tournaire-Marques E. [Ischemic optic neuropathies]. J Fr Ophtalmol 2020;43:552–8. 10.1016/j.jfo.2019.10.020 [DOI] [PubMed] [Google Scholar]
- 31.Kerr NM, Chew SSSL, Danesh-Meyer HV. Non-arteritic anterior ischaemic optic neuropathy: a review and update. J Clin Neurosci 2009;16:994–1000. 10.1016/j.jocn.2009.04.002 [DOI] [PubMed] [Google Scholar]
- 32.Hayreh SS, Zimmerman B. Visual field abnormalities in nonarteritic anterior ischemic optic neuropathy: their pattern and prevalence at initial examination. Arch Ophthalmol 2005;123:1554–62. 10.1001/archopht.123.11.1554 [DOI] [PubMed] [Google Scholar]
- 33.Dinkin M, Johnson E. One giant step for giant cell arteritis: updates in diagnosis and treatment. Curr Treat Options Neurol 2021;23:6. 10.1007/s11940-020-00660-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marzoli SB, Criscuoli A. Pain in optic neuropathies. Neurol Sci 2018;39:25–31. 10.1007/s10072-018-3334-1 [DOI] [PubMed] [Google Scholar]
- 35.Braithwaite T, Subramanian A, Petzold A, et al. Trends in optic neuritis incidence and prevalence in the UK and association with systemic and neurologic disease. JAMA Neurol 2020;77:1514–23. 10.1001/jamaneurol.2020.3502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McVeigh K, Vakros G, Girgis R. Masquerading optic neuritis. BMJ Case Rep 2015;2015. 10.1136/bcr-2015-210259. [Epub ahead of print: 03 Aug 2015]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moschetta L, Fasolino G, Kuijpers RW. Non-arteritic anterior ischaemic optic neuropathy sequential to SARS-CoV-2 virus pneumonia: preventable by endothelial protection? BMJ Case Rep 2021;14:e240542. 10.1136/bcr-2020-240542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clarke KM, Riga V, Shirodkar A-L, et al. Proning related bilateral anterior ischaemic optic neuropathy in a patient with COVID-19 related acute respiratory distress syndrome. BMC Ophthalmol 2021;21:276. 10.1186/s12886-021-02028-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ischemic optic neuropathy decompression trial: twenty-four-month update. Arch Ophthalmol 2000;118:793–8. 10.1001/archopht.118.6.793 [DOI] [PubMed] [Google Scholar]
- 40.Rootman DB, Gill HS, Margolin EA. Intravitreal bevacizumab for the treatment of nonarteritic anterior ischemic optic neuropathy: a prospective trial. Eye 2013;27:538–44. 10.1038/eye.2012.296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rath EZ, Hazan Z, Adamsky K, et al. Randomized controlled phase 2A study of RPh201 in previous nonarteritic anterior ischemic optic neuropathy. J Neuroophthalmol 2019;39:291–8. 10.1097/WNO.0000000000000786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen S, Fan X-R, He S, et al. Watch out for neuromyelitis optica spectrum disorder after inactivated virus vaccination for COVID-19. Neurol Sci 2021;42:3537–9. 10.1007/s10072-021-05427-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fujikawa P, Shah FA, Braford M, et al. Neuromyelitis optica in a healthy female after severe acute respiratory syndrome coronavirus 2 mRNA-1273 vaccine. Cureus 2021;13:e17961. 10.7759/cureus.17961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Helmchen C, Buttler GM, Markewitz R, et al. Acute bilateral optic/chiasm neuritis with longitudinal extensive transverse myelitis in longstanding stable multiple sclerosis following vector-based vaccination against the SARS-CoV-2. J Neurol 2022;269:1–6. 10.1007/s00415-021-10647-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Manasseh G, Donovan D, Shao EH, et al. Bilateral sequential non-arteritic anterior ischaemic optic neuropathy following repeat influenza vaccination. Case Rep Ophthalmol 2014;5:267–9. 10.1159/000366472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.LiverTox . Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012–. Adverse Drug Reaction Probability Scale (Naranjo) in Drug Induced Liver Injury, 2019. [PubMed] [Google Scholar]
- 47.Serum Institute Of India - ChAdOx1 nCoV- 19 Corona Virus Vaccine (Recombinant) - COVISHIELD [Internet], 2021. Available: https://www.seruminstitute.com/product_covishield.php [Accessed 8 Dec 2021].
- 48.Tishler M, Shoenfeld Y. Vaccination may be associated with autoimmune diseases. Isr Med Assoc J 2004;6:430–2. [PubMed] [Google Scholar]
- 49.Agmon-Levin N, Paz Z, Israeli E, et al. Vaccines and autoimmunity. Nat Rev Rheumatol 2009;5:648–52. 10.1038/nrrheum.2009.196 [DOI] [PubMed] [Google Scholar]
- 50.Liang Z, Zhu H, Wang X, et al. Adjuvants for coronavirus vaccines. Front Immunol 2020;11:589833. 10.3389/fimmu.2020.589833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kannemeier C, Shibamiya A, Nakazawa F, et al. Extracellular RNA constitutes a natural procoagulant cofactor in blood coagulation. Proc Natl Acad Sci U S A 2007;104:6388–93. 10.1073/pnas.0608647104 [DOI] [PMC free article] [PubMed] [Google Scholar]