Abstract
Objectives
Early patient disposition is crucial to prevent crowding in emergency departments (EDs). Our study aimed to characterise the need of in-house resources for patients treated in the ED according to the Emergency Severity Index (ESI) and the presenting complaint at the timepoint of triage.
Design
A retrospective single-centre study was conducted.
Setting
Data of all patients who presented to the interdisciplinary ED of a tertiary care hospital in Munich, Germany, from 2014 to 2017 were analysed.
Participants
n=113 694 patients were included.
Measures
ESI Score, medical speciality according to the chief complaint, mode of arrival, admission rates and discharge destination from the ED were evaluated.
Results
Patient disposition varied according to ESI scores in combination with the chief complaint. Patients with low ESI scores were more likely to be admitted after treatment in the ED than patients with high ESI scores. Highly prioritised patients (ESI 1) mainly required admission to an intensive care unit (ICU, 27%), intermediate care unit (IMC, 37%) or immediate intervention (11%). In this critical patient group, 30% of patients with neurological or medical symptoms required immediate intensive care, whereas only 17% of patients with surgical problems were admitted to an ICU. A significant number of patients (particularly with neurological or medical problems) required hospital (and in some cases even ICU or IMC) admission despite high ESI scores.
Conclusions
Overall, ESI seems to be a useful tool to anticipate the need for specialised in-hospital resources on arrival. Patients with symptoms pointing at neurological or medical problems need particular attention as ESI may fail to sufficiently predict the care facility level for this patient group.
Keywords: adult intensive & critical care, accident & emergency medicine
Strengths and limitations of this study.
This is a single-centre study on a large number of emergency patients (n=113 694).
The Emergency Severity Index (ESI) in combination with the medical speciality of the chief complaint was assessed for the prediction of type and amount of required hospital beds.
Data are limited on ESI and required in-house resources; other triage scales or resource consumption within the emergency department were not assessed.
Introduction
Keeping the patient flow in emergency departments (EDs) going is important to prevent (over)crowding. One of the crucial processes is to determine the most probable patient disposition as early as possible. This allows staff on the wards to get prepared even though patients still receive diagnostics before admission. Furthermore, in situations when patients in the ED with a high probability of admission to specific wards (such as general ward, intermediate care, intensive care) outnumber available beds, reallocation or early discharge of in-house patients could help to create resources long before the ED patient is ready to be admitted. Patients arriving at the ED usually undergo triage using standardised scores. These scores are designed to rapidly assess the acuteness of the disease and allow to allocate treatment priorities, which is especially important when demand for medical care exceeds disposable resources such as staff, space or medical equipment.1 The main purpose of triage scores is to avoid waiting time that endangers patients with potential life-threatening diseases. In general, triage scores with five levels are considered to have a superior validity and reliability compared with those with three levels.2 Commonly used five-level triage systems in EDs are the Australasian Triage Scale (ATS), the Manchester Triage System (MTS), the Canadian Triage and Acuity Scale (CTAS) and the Emergency Severity Index (ESI). Initially, the development of the ATS in Australia was the basis for the MTS used in Great Britain and for the CTAS in Canada.3–5 ESI is also a five-level triage algorithm, which was developed in the late 1990s and is nowadays frequently used in many European countries.6 7 Treatment priority according to ESI depends on severity of the disease and expected need of resources. Interobserver reliability of ESI is considered high, reflected by the fact that there are no significant differences in triage by nurses and physicians.8 9 Reliability may be moderate in some subgroups such as in geriatric or paediatric patients,10–13 but overall, ESI is considered to be a valuable tool to assign acceptable maximum waiting times and to protect critical patients from being overlooked in overcrowded EDs. Here, we aimed to characterise the in-house resources needed for ED patients according to ESI scores at triage and the most likely medical discipline that is needed for the patient according to the chief complaint.
Methods
A single-centre retrospective analysis was conducted. Data of all patients who presented to the interdisciplinary ED of a tertiary care hospital in Munich, Germany, within 3 years were analysed (11/2014 until 10/2017). All patients initially underwent a triage process by an experienced and specifically trained nurse supervised by an attending emergency physician. ESI was used for triage of all patients as suggested by the published algorithm.6 Simultaneously, the main complaint was identified for each patient. At discharge from the ED, the discharge destination was documented.
Data of all patients were extracted according to ESI Score (levels ESI 1, ESI 2, ESI 3, ESI 4 and ESI 5), the manner in which the patient reached the ED and discharge destination from the ED. Patient flow was analysed for admissions to intensive care unit (ICU), intermediate care unit (IMC), standard wards, monitoring at the emergency ward, intervention, transfer to other hospitals, discharge, discharge against medical advice, lost to follow-up (patients who left the ED without reporting to medical staff) and death in the ED. Subgroup analysis was performed for symptoms that prompted a health problem most likely related to one of nine specialities (internal medicine, trauma surgery, neurology, general surgery, otorhinolaryngology, urology, orthopaedics, gynaecology and neurosurgery).
Data are illustrated in numbers (n) and/or percentages. For statistical analysis, χ2 test of independence was used (SigmaPlot) and p<0.05 was considered significant. Bonferroni alpha correction was applied for multiple comparisons (statistics on admissions according to ESI, p values<0.005 were considered significant). All data were anonymised before the authors accessed them.
Patient and public involvement
Patients and the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Results
ESI levels and most frequent triage symptoms
During the study period, n=113 694 patients presented to the interdisciplinary ED. All patients underwent an initial assessment, including ESI triage and identification of a main presenting symptom (online supplemental material). Three per cent of all patients (n=3046) were triaged with ESI 1, implying that they suffered from an immediate life-threatening health problem. Overall, 5% were scored ESI 2 (n=5222), 42% (n=47 886) were assigned to ESI 3, another 42% (n=47 697) to ESI 4% and 7% (n=9843) to ESI 5. Overall, the most frequent chief complaints on presentation were abdominal pain (8%), limb injury (6%) and chest pain (5%) (table 1).
Table 1.
Percentages of the 10 most frequent chief complaints
| Rank of symptom frequency | All patients | Admitted patients | Discharged patients |
| 1 | Abdominal pain (8%) | Abdominal pain (9%) | Abdominal pain (8%) |
| 2 | Limb injury (6%) | Chest pain (6%) | Limb injury (7%) |
| 3 | Chest pain (5%) | Reduced general condition (6%) | Work accident (6%) |
| 4 | Work accident (4%) | Airway problem (5%) | Headache (4%) |
| 5 | Fall with injury (4%) | Craniocerebral injury (4%) | Fall with injury (4%) |
| 6 | Airway problem (4%) | Fall with injury (4%) | Chest pain (4%) |
| 7 | Headache (4%) | Other complaints (4%) | Joint pain (3%) |
| 8 | Craniocerebral injury (3%) | Limb injury (3%) | Vertigo (3%) |
| 9 | Vertigo (3%) | Hemiparesis (3%) | Craniocerebral injury (3%) |
| 10 | Reduced general condition (3%) | Fever (3%) | Micturition problems (3%) |
bmjopen-2021-057684supp001.pdf (15KB, pdf)
Means of transport to the ED
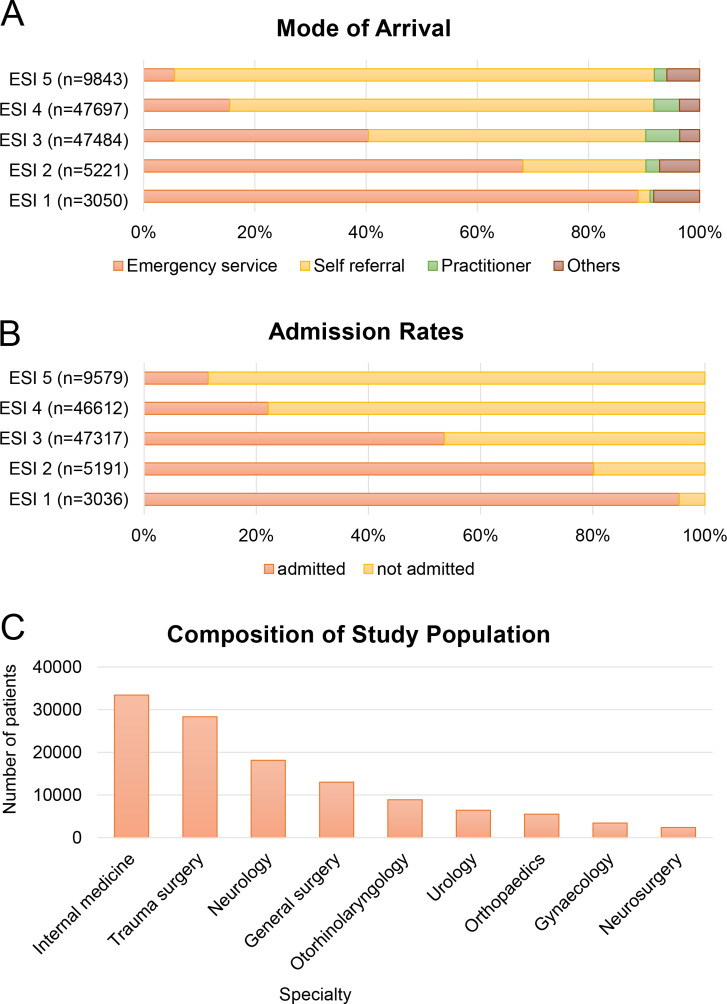
The manners in which patients reached the ED were via emergency service (30%), self-referral (61%), referral by a practitioner at an ambulatory care office (5%) and others (eg, via police or referral from abroad) (4%). Patients with a high treatment priority according to ESI were more likely to present via the emergency service: 89% of ESI 1 patients and 68% of ESI 2 patients were taken to hospital by the emergency services compared with 15% for ESI 4% and 6% for ESI 5 (figure 1A). Patients with a low treatment priority according to ESI, however, mainly presented on their own. Self-referrals were 86% for ESI 5 patients and 76% for ESI 4 patients compared with 50% for ESI 3, 22% for ESI 2% and 2% for ESI 1 (figure 1A).
Figure 1.
Analysis of the study population for mode of arrival (A), admission rate (B) and speciality according to the chief complaint (C). Data of all patients (n=113 694) were analysed for triage results according to the Emergency Severity Index (ESI) and is illustrated for ESI 1, ESI 2, ESI 3, ESI 4 and ESI 5. Possible manners of arrival (A) were via the emergency service, by self-referral, via a practitioner and others (eg, police). After treatment in the ED, patients were either admitted or discharged (B). For further analysis, patients were grouped to medical specialities according to their chief complaint (C): internal medicine, trauma surgery, neurology, general surgery, otorhinolaryngology, urology, orthopaedics, gynaecology or neurosurgery.
Hospital admissions
The general admission rate was 39%, but differed in a subgroup analysis according to the responsible speciality group of the presenting complaint (table 2). High triage priority reflected by a low ESI level was associated with high probability of admission (figure 1B). Admission rates were 96% for ESI 1, 80% for ESI 2, 54% for ESI 3, 22% for ESI 4, and 11% for ESI 5 patients (figure 1B).
Table 2.
Admission rates (%) and total numbers of admitted patients (n) analysed for speciality groups and Emergency Severity Index (ESI)
| Speciality | Admission ESI 1 | Admission ESI 2 | Admission ESI 3 | Admission ESI 4 | Admission ESI 5 |
| All specialities | 96% (n=2898) | 80% (n=4162) | 54% (n=25 333) | 22% (n=10 321) | 11% (n=1096) |
| Internal medicine | 99% (n=777) | 80% (n=1791) | 62% (n=13 062) | 35% (n=3016) | 21% (n=208) |
| Trauma surgery | 96% (n=874) | 72% (n=260) | 45% (n=3457) | 13% (n=2054) | 7% (n=260) |
| Neurology | 93% (n=725) | 86% (n=1844) | 46% (n=3662) | 28% (n=1588) | 20% (n=139) |
| General surgery | 93% (n=214) | 78% (n=226) | 57% (n=2690) | 24% (n=1379) | 11% (n=190) |
| Otorhinolaryngology | 100% (n=13) | 60% (n=70) | 45% (n=822) | 18% (n=970) | 10% (n=151) |
| Urology | 90% (n=9) | 48% (n=45) | 40% (n=872) | 20% (n=714) | 14% (n=75) |
| Orthopaedics | 50% (n=2) | 53% (n=10) | 41% (n=329) | 16% (n=546) | 11% (n=113) |
| Gynaecology | 100% (n=5) | 58% (n=14) | 29% (n=285) | 16% (n=275) | 6% (n=19) |
| Neurosurgery | 95% (n=410) | 84% (n=96) | 68% (n=657) | 54% (n=398) | 54%(n=51) |
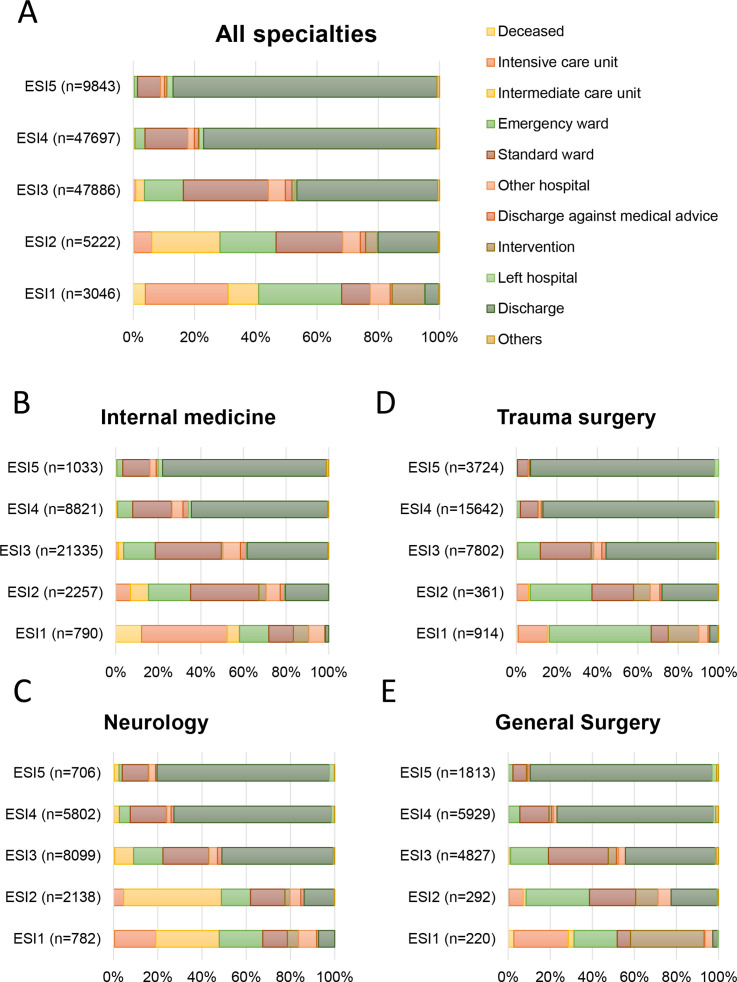
Required care facility levels of admitted patients
Patients with ESI 1 and ESI 2 frequently required ICU or IMC (figure 2). ESI 1 patients had the highest admission rates to ICU (27%), interventions (11%) or IMC (37%, including stroke unit, chest pain unit and emergency ward admission unit). Most patients assigned to ESI 4 and ESI 5 were discharged after treatment in the ED (76% and 86%) and only infrequently required ICU (ESI 4 0.1%, ESI 5 0.1%) or IMC (ESI 4 3.7%, ESI 5 1.3%). In numbers, 9 patients triaged to ESI 5 and 59 patients triaged to ESI 4 needed intensive care. The patients who required intensive care despite initial triage to ESI 5 had presented with dehydration, headache, a common cold, suspected shunt infection (n=2) or problems not further specified at triage (n=4). Similarly, patients who were triaged to ESI 4 and required intensive care mainly suffered from a symptom indicating an internal medical (n=33) or a neurological/neurosurgical problem (n=10). Typical triage symptoms in this subgroup were, for example, abdominal pain (n=8), reduced general condition (n=6), headache (n=4), chest pain (n=2), nausea/vomiting (n=2), dehydration (n=2) or airway problems (n=2).
Figure 2.
Patient disposition in general and according to the responsible medical speciality. Patient disposition according to Emergency Severity Index (ESI) for all patients (A) and for patients with chief complaints pointing at problems related to internal medicine (B), neurology (C), trauma surgery (D) or general surgery (E).
Mortality in the ED
Patients assessed to ESI 1 were at highest risk of death in the ED: 4% of all ESI 1 patients died in the ED. Four patients with ESI 4 deceased in the ED, all of them were suffering from medical problems such as heart failure (n=2), sepsis or hypovolemic shock. None of the patients appointed to ESI 5 died.
Analysis of medical subgroups
Speciality groups involved in the treatment according to the chief complaint were internal medicine, trauma surgery, neurology, general surgery, otorhinolaryngology, urology, orthopaedics, gynaecology and neurosurgery (figure 1C). Patients assigned to the main conservative disciplines (internal medicine and neurology) were more likely to present via the emergency service (37%) than patients of the main surgical disciplines (trauma surgery and general surgery, 26%, p<0.001). For conservative disciplines, referrals via practitioners were more common than for surgical disciplines (7% vs 3%, p<0.001).
All in all, ESI triage scores were associated with admission rates (table 2) as patients with numerically low ESI scores had higher admission rates and contrariwise (p<0.001 for all single comparisons). This held true for all ESI subgroups of patients with symptoms assigned to internal medicine, trauma surgery, neurology, otorhinolaryngology and general surgery (p<0.001 for all single comparisons). In urology, orthopaedics, gynaecology and neurosurgery, admission rates did not differ between ESI 1 and ESI 2, but the absolute numbers of patients were low in these groups. In urology and orthopaedics, differences in admission rates between patients triaged to ESI 2 and ESI 3 could also not be found. Furthermore, there were no significant differences between ESI 1 and ESI 3 or ESI 4 in orthopaedics, ESI 3 or ESI 4 and ESI 5 in neurosurgery.
Subgroup analysis showed that the required in-house resources according to ESI differed between the medical specialities (figure 2). ESI 1 patients with surgical problems (trauma surgery and general surgery) less often (17%) required immediate intensive care capacities than patients of conservative disciplines (internal medicine and neurology; 30%) (p<0.001). In turns, 19% of surgical ESI 1 patients required immediate interventions such as surgery compared with 6% in the conservative group (p<0.001).
Patients with neurological symptoms
In neurology and neurosurgery, admission rates were above the average admission rate of 39%: 46% of neurological and 69% of neurosurgical patients needed admission. Of interest, neurological and neurosurgical patients with low treatment priorities according to ESI still had high admission rates (table 2). Most important, admission rates for ESI 3, ESI 4 and ESI 5 patients to ICU and IMC were above average. Remarkably, five of the nine ESI 5 patients who required ICU presented with a symptom that was suspicious for a neurological or neurosurgical problem.
Discussion
The main findings of our study were: (1) ESI scores were associated with mode of arrival, mortality in the ED and need for admission, (2) individual patients required even intermediate or intensive care despite high ESI scores, (3) the predicative value of ESI was high for most speciality subgroups (except urology, orthopaedics, gynaecology and neurosurgery) and (4) a significant number of patients with high ESI scores required admission when the chief complaint pointed at a neurosurgical, neurological and medical problem.
The distribution of ESI levels in our study cohort is comparable to those previously described.6 9 We observed an association of ESI with mode of arrival, which goes along with the expected urgency of treatment and is supported by the literature, showing that ambulance use is related to severity of injury or illness.14 15 Regarding hospital admission and mortality, one retrospective observation with fairly large numbers of patients of four EDs (37 974 patients triaged with ESI and 34 258 patients triaged with MTS) found that both ESI and MTS predicted the necessity of hospital admission and mortality, which is in accordance with our data.16 However, in this study, triage results were missing in many patients, the study period only involved a few weeks and there was no differentiation for specialities. From a general point of view, besides ESI and MTS also other triage scales are known to predict outcomes including mortality, hospital admission and resource consumption within the ED but numbers were generally low and the relevance of the chief complaint was not assessed in most studies.17
Remarkably, admissions (even to intermediate or intensive care) in supposedly low-acuity ED patients assessed by ESI were observed. This is of particular interest in times of overcrowded EDs, when critics and politicians claim an inappropriate use of emergency resources by patients with low treatment priority. Our data show that less urgent triage scores do not necessarily argue for an inappropriate attendance of an ED as often supposed in political discussions on emergency resources. For example, in Australia, the ATS is not only used to assess treatment priority, but it is also the basis of Urgency Related Groups and thereby essential for the ED funding in the country.3 Furthermore, even in the group of ED patients who are not admitted, a significant amount of medical support has to be applied within the ED to many of these patients to ensure a save discharge home. One reason for the need of an admission despite a high ESI Score might be that patients presenting with subacute complaints may often be assigned to ESI scores with low priority but might turn out to suffer from electrolyte disturbance or subacute stroke (just to mention examples) and require further treatment at an IMC or stroke unit. The fact that these patients require IMC, however, does not necessarily mean that the high triage scores expose them to a medical risk within the ED. Reasons for ambulance use despite high ESI scores could be the recovery of patients by the time of triage as well as immobility due to age or pre-existing illness.18 All in all, our data show that a profound emergency workup is needed irrespective of the triage level to distinguish patients who could be discharged (but still may have required emergency treatment) from those qualifying for admission.
The novelty about our data is the evaluation of the speciality group according to the presenting chief complaint in addition to ESI in a large number of emergency patients. The literature on ESI for specific patient groups is limited and usually restricted either to specific diseases or symptoms19 20 or focused on age groups, such as adults, geriatric or paediatric patients.10 13 Different specialities within one interdisciplinary study cohort have—to the best of our knowledge—not been investigated before. The differences we found for the predicative power of ESI in some speciality groups need particular attention. We observed that required ICU capacities differed among patients with neurological or medical symptoms and patients with surgical symptoms. This could be of practical relevance: knowing the responsible speciality group in case of an admission is essential in Germany, as wards are usually restricted to specific specialities and therefore patients cannot be assigned to any available bed within a hospital.
Patients with symptoms belonging to neurosurgery, neurology and internal medicine had high admission rates and ESI only poorly predicted the need for in-hospital care in neurological and neurosurgical patients with high ESI scores. First of all, the high admission rates in these specialities might be a result of the limited emergency workup capacities for the underlying diseases, which may lead to hospital admission for more elaborate investigation. Additionally, selection bias is likely as a large number of neurological patients with medium or low priority ESI scores was referred to our ED by practitioners (9% of ESI 3, 10% of ESI 4% and 8% of ESI 5 in neurological patients vs 6% of ESI 3, 5% of ESI 4% and 2% of ESI 5 in general). The relatively high rate of neurological admissions to IMC is in part a result of the need for stroke unit care in many of these patients. Some attempts were made to overcome the limitations of the most common triage systems for neurological patients. One triage system designed for patients with neurological complaints to identify those with urgent need for medical treatment, thereby reducing resource consumption and duration of treatment is the Heidelberg Neurological Triage System.21 22 This triage system has been evaluated not only in a highly specialised neurological ED but also in an interdisciplinary emergency setting. However, study periods were short, the number of patients was limited and the restriction to four levels might affect its applicability in large EDs where five-level triage scores are standard.2 The authors made a great effort to integrate the score into ESI but this still needs evaluation.22 Overall, it seems not feasible to use speciality specific triage systems in large multidisciplinary EDs. However, for some diseases such as sepsis, combination of ESI with shock index or quick sepsis-related organ failure assessment might improve validity and mortality.20 23 Whether ESI triage for neurological patients might be improved by adding neurological scores, for example, Glasgow Coma Scale or the Face Arm Speech Test, still needs to be evaluated.
There are several limitations of our study. First of all, data were collected retrospectively and at a single tertiary care university hospital. Therefore, our results cannot be generalised. Selection bias might have influenced the patient mix as a significant number of patients presents to the ED for specialised advice according to long-term treatment at the hospital. Our emergency setup includes the frequent use of specialised consultations, diagnostics and treatment at any time to avoid admission. As a consequence of the extended workup in the ED, admission rates might be lower than in other hospitals. Besides, resource consumption within the ED and discharged patients were not further analysed. However, this was not the aim of our investigation and has already been addressed by previous studies.24 Furthermore, we did not control for other risk factors, such as age or pre-existing illness. And, last but not least, other triage scales besides ESI were not evaluated, but would have been of major interest with regard to the variety of triage systems in use and the ambition for an international comparability.3
Conclusion
There are various approaches that aim to improve coordination of ED care by reducing time for triage, treatment and transfer of patients.25–28 Our work suggests that ESI might be a promising tool to improve coordination of care by predicting type and amount of hospital beds required for specific ED patient groups. Patients with symptoms pointing at neurological problems need particular attention as ESI failed to sufficiently predict the care facility level needed in this patient group.
Supplementary Material
Acknowledgments
We thank Edin Hedzic for his contribution to acquire the data.
Footnotes
Contributors: Study concept and design were developed by SV and MK. Acquisition of data was done by SV. MK, SH, AB, JGD, UK and H-WP were responsible for the interpretation of data and critical revision of the manuscript. SV and MK accept full responsibility for the work, had access to the data, and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Original data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was approved by the Ethics Committee of the University of Munich (project number 18-409).
References
- 1.Anon . Consensus statement on the triage of critically ill patients. Society of critical care medicine ethics Committee. JAMA 1994;271:1200–3. 10.1001/jama.1994.03510390070032 [DOI] [PubMed] [Google Scholar]
- 2.Kuriyama A, Urushidani S, Nakayama T. Five-Level emergency triage systems: variation in assessment of validity. Emerg Med J 2017;34:703–10. 10.1136/emermed-2016-206295 [DOI] [PubMed] [Google Scholar]
- 3.FitzGerald G, Jelinek GA, Scott D, et al. Emergency department triage revisited. Emerg Med J 2010;27:86–92. 10.1136/emj.2009.077081 [DOI] [PubMed] [Google Scholar]
- 4.Beveridge R. CAEP issues. The Canadian triage and acuity scale: a new and critical element in health care reform. Canadian association of emergency physicians. J Emerg Med 1998;16:507–11. 10.1016/s0736-4679(98)00031-6 [DOI] [PubMed] [Google Scholar]
- 5.Mackway-Jones K. Emergency triage: Manchester triage group. BMJ Publishing Group, 1997. [Google Scholar]
- 6.Mirhaghi A, Heydari A, Mazlom R, et al. Reliability of the emergency severity index: meta-analysis. Sultan Qaboos Univ Med J 2015;15:e71–7. [PMC free article] [PubMed] [Google Scholar]
- 7.Wuerz RC, Milne LW, Eitel DR, et al. Reliability and validity of a new five-level triage instrument. Acad Emerg Med 2000;7:236–42. 10.1111/j.1553-2712.2000.tb01066.x [DOI] [PubMed] [Google Scholar]
- 8.Esmailian M, Zamani M, Azadi F, et al. Inter-Rater agreement of emergency nurses and physicians in emergency severity index (ESI) triage. Emerg 2014;2:158–61. 10.22037/emergency.v2i4.6449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fong RY, Glen WSS, Mohamed Jamil AK, et al. Comparison of the emergency severity index versus the patient acuity category scale in an emergency setting. Int Emerg Nurs 2018;41:13–18. 10.1016/j.ienj.2018.05.001 [DOI] [PubMed] [Google Scholar]
- 10.Travers DA, Waller AE, Katznelson J, et al. Reliability and validity of the emergency severity index for pediatric triage. Acad Emerg Med 2009;16:843–9. 10.1111/j.1553-2712.2009.00494.x [DOI] [PubMed] [Google Scholar]
- 11.Platts-Mills TF, Travers D, Biese K, et al. Accuracy of the emergency severity index triage instrument for identifying elder emergency department patients receiving an immediate life-saving intervention. Acad Emerg Med 2010;17:238–43. 10.1111/j.1553-2712.2010.00670.x [DOI] [PubMed] [Google Scholar]
- 12.Storm-Versloot MN, Ubbink DT, Kappelhof J, et al. Comparison of an informally structured triage system, the emergency severity index, and the Manchester triage system to distinguish patient priority in the emergency department. Acad Emerg Med 2011;18:822–9. 10.1111/j.1553-2712.2011.01122.x [DOI] [PubMed] [Google Scholar]
- 13.Grossmann FF, Zumbrunn T, Frauchiger A, et al. At risk of undertriage? Testing the performance and accuracy of the emergency severity index in older emergency department patients. Ann Emerg Med 2012;60:317–25. 10.1016/j.annemergmed.2011.12.013 [DOI] [PubMed] [Google Scholar]
- 14.Ruger JP, Richter CJ, Lewis LM. Clinical and economic factors associated with ambulance use to the emergency department. Acad Emerg Med 2006;13:879–85. 10.1197/j.aem.2006.04.006 [DOI] [PubMed] [Google Scholar]
- 15.Bosia T, Malinovska A, Weigel K, et al. Risk of adverse outcome in patients referred by emergency medical services in Switzerland. Swiss Med Wkly 2017;147:w14554. 10.4414/smw.2017.14554 [DOI] [PubMed] [Google Scholar]
- 16.van der Wulp I, Schrijvers AJP, van Stel HF. Predicting admission and mortality with the emergency severity index and the Manchester triage system: a retrospective observational study. Emerg Med J 2009;26:506–9. 10.1136/emj.2008.063768 [DOI] [PubMed] [Google Scholar]
- 17.Zachariasse JM, van der Hagen V, Seiger N, et al. Performance of triage systems in emergency care: a systematic review and meta-analysis. BMJ Open 2019;9:e026471. 10.1136/bmjopen-2018-026471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pearson C, Kim DS, Mika VH, et al. Emergency department visits in patients with low acuity conditions: factors associated with resource utilization. Am J Emerg Med 2018;36:1327–31. 10.1016/j.ajem.2017.12.033 [DOI] [PubMed] [Google Scholar]
- 19.Pouyamehr A, Mirhaghi A, Sharifi MD, et al. Comparison between emergency severity index and heart failure triage scale in heart failure patients: a randomized clinical trial. World J Emerg Med 2019;10:215–21. 10.5847/wjem.j.1920-8642.2019.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kwak H, Suh GJ, Kim T, et al. Prognostic performance of emergency severity index (ESI) combined with qSOFA score. Am J Emerg Med 2018;36:1784–8. 10.1016/j.ajem.2018.01.088 [DOI] [PubMed] [Google Scholar]
- 21.Hoyer C, Stein P, Ebert A, et al. Comparing expert and Non-Expert assessment of patients presenting with neurological symptoms to the emergency department: a retrospective observational study. Neuropsychiatr Dis Treat 2020;16:447–56. 10.2147/NDT.S236160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oßwald HM, Harenberg L, Jaschonek H, et al. Development and validation of the Heidelberg neurological triage system (HEINTS). J Neurol 2019;266:2685–98. 10.1007/s00415-019-09472-0 [DOI] [PubMed] [Google Scholar]
- 23.Torabi M, Moeinaddini S, Mirafzal A, et al. Shock index, modified shock index, and age shock index for prediction of mortality in emergency severity index level 3. Am J Emerg Med 2016;34:2079–83. 10.1016/j.ajem.2016.07.017 [DOI] [PubMed] [Google Scholar]
- 24.Tanabe P, Gimbel R, Yarnold PR, et al. The emergency severity index (version 3) 5-level triage system scores predict ED resource consumption. J Emerg Nurs 2004;30:22–9. 10.1016/j.jen.2003.11.004 [DOI] [PubMed] [Google Scholar]
- 25.Vegting IL, Nanayakkara PWB, van Dongen AE, et al. Analysing completion times in an academic emergency department: coordination of care is the weakest link. Neth J Med 2011;69:392–8. [PubMed] [Google Scholar]
- 26.De Freitas L, Goodacre S, O'Hara R, et al. Interventions to improve patient flow in emergency departments: an umbrella review. Emerg Med J 2018;35:626–37. 10.1136/emermed-2017-207263 [DOI] [PubMed] [Google Scholar]
- 27.Lauks J, Mramor B, Baumgartl K, et al. Medical team evaluation: effect on emergency department waiting time and length of stay. PLoS One 2016;11:e0154372. 10.1371/journal.pone.0154372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Villa S, Weber EJ, Polevoi S, et al. Decreasing triage time: effects of implementing a step-wise ESI algorithm in an EHR. Int J Qual Health Care 2018;30:375–81. 10.1093/intqhc/mzy056 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-057684supp001.pdf (15KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Original data are available upon reasonable request.