Abstract
Background
Strong positive relationships between dietary self-monitoring and eating disorder risk are seen in population-based, observational studies. However, current evidence cannot establish causality. Furthermore, little is known about other mental and behavioral health consequences of dietary self-monitoring among college women, a population vulnerable to eating disorders.
Objective
To determine if introducing dietary self-monitoring via a popular smartphone app to undergraduate women impacts eating disorder risk, other aspects of mental health, or health behaviors including dietary intake and physical activity.
Design
Randomized controlled trial.
Participants/setting
Undergraduate women who had not engaged in dietary self-monitoring in the past year and who were at low-risk for an eating disorder participated between May and October 2019 (n = 200).
Intervention
Participants were randomly assigned to engage in dietary self-monitoring via MyFitnessPal for approximately 1 month or to receive no intervention.
Main outcome measures
Self-report data on eating disorder risk, other mental health outcomes, and health behaviors were collected at baseline and post-intervention.
Statistical analyses performed
Linear and logistic regressions were utilized to test hypotheses.
Results
Adherence to the intervention was high, with participants recording their dietary intake via MyFitnessPal on average 89.1% of days between baseline and post-intervention. Assignment to the intervention was not associated with changes in eating disorder risk, anxiety, depressive symptoms, body satisfaction, quality of life, nutritional intake, physical activity, screen time, or other forms of weight-related self-monitoring (all P > .05).
Conclusions
Among dietary self-monitoring naive undergraduate women with low-risk of an eating disorder, dietary self-monitoring via MyFitnessPal for 1 month did not increase eating disorder risk, impact other aspects of mental health, or alter health behaviors including dietary intake. The null results in our study may be due to the selection of a low-risk sample; future research should explore whether there are populations for whom dietary self-monitoring is contraindicated.
Keywords: Self-monitoring, Dietary intake, College health, Eating disorders, Calorie counting
INDIVIDUALS WHO WANT TO IMPROVE THEIR DIETARY behaviors or lose weight are often encouraged to track their dietary intake.1–3 Theoretically, dietary self-monitoring functions by bringing attention to one’s dietary intake, allowing one to set goals for behavior change, and for some, to monitor how their behavior change may affect their weight.4 Dietary self-monitoring has historically required keeping paper food logs, but in recent years has become easier and more common with the advent of smartphone apps designed for dietary self-monitoring. For example, MyFitness-Pal, one of the most popular dietary self-monitoring apps, currently reports 165 million users with 19.1 million active users a month.5,6 With this increased accessibility and ease of dietary self-monitoring, there is growing concern regarding the potential iatrogenic effects of dietary self-monitoring on eating disorder risk.7,8 Specifically, it is thought that the increased attention on food and weight and perceived malleability of weight based on dietary intake brought upon by dietary self-monitoring may increase eating disorder risk.9
Eating disorders are a major public health concern; the prevalence of eating disorders has increased over time,10 and eating disorders can lead to serious medical complications, other psychiatric disorders, suicide, and mortality.11–13 Numerous studies among the general population of college students demonstrate strong associations between dietary self-monitoring and increased eating disorder risk,14–16 particularly for females.17,18 Furthermore, in a sample of females seeking treatment for an eating disorder, 75% reported using MyFitnessPal to count calories and 73% of those who used MyFitnessPal to count calories believed the app contributed to the development of their eating disorder.19 Conversely, a meta-analysis among samples of boys and girls found that participation in supervised weight management programs, which typically recommended dietary self-monitoring, has been associated with decreases in disordered eating.20 The decrease in disordered eating may be due to other protective aspects included in structured weight management programs such as supervision by nutrition and mental health professionals and social support.8,21,22
Understanding potential impacts of dietary self-monitoring among college women is of particular importance as an estimated 14% to 26% of college students use an app or device to count their calories.15,23,24 Additionally, female college students are especially vulnerable to eating disorders; up to 13.5% of female college students have an eating disorder,10 49.1% report binge eating in the last 4 weeks, and 31.2% report using a compensatory eating disorder behavior such as purging or compulsive exercise25 in the last 4 weeks. Given the lack of experimental evidence regarding the effects of dietary self-monitoring among nonclinical populations, the objective of this study was to identify the effects of dietary self-monitoring on eating disorder risk among college women via a randomized controlled trial. Using a randomized controlled trial design will address limitations of the existing observational literature such as confounding by factors that are common causes of both dietary self-monitoring and eating disorders such as preoccupation with food and/or weight, thereby filling an important gap in the existing literature. Guided by previous research,14–18 we hypothesized that women assigned to use an app for self-monitoring dietary intake would report an increase in eating disorder risk relative to women assigned to the control condition. Furthermore, we hypothesized that dietary self-monitoring would lead to poorer mental health outcomes given the impacts of self-weighing on mental health among this population.8 It has been posited that apps that focus on self-monitoring may decrease mental health via weight bias internalization, which is associated with decreased mental health.9,26
Conversely, we hypothesized that dietary self-monitoring would lead to changes in dietary intake and increased physical activity. This hypothesis was based on the theoretical underpinning of dietary self-monitoring and observational studies among college students showing positive or marginally positive associations between weight-related self-monitoring and health behaviors such as dietary intake and physical activity.27–30 Study findings can inform public health and clinical recommendations regarding dietary self-monitoring outside of supervised weight management programs and among college women specifically.
SUBJECTS AND METHODS
Participants
The present study was restricted to women based on increased risk of eating disorders,10,25 higher prevalence of use of dietary self-monitoring,17,18,24 and evidence that the relationship between dietary self-monitoring and eating disorder risk differs by gender.17,18 Data from a pilot trial conducted by the study team (n = 12/intervention or control condition) suggested that assignment to self-monitor dietary intake using MyFitnessPal for 1 month resulted in moderate-sized increases in eating disorder risk among college women as measured by the Eating Disorder Examination Questionnaire Short Form (EDE-QS) (Cohen’s d = 0.45). A minimum sample size of 78 participants per condition was needed to detect a statistical difference of this effect size or greater with 80% power and type I error α = .05. A sample size of 100 participants/condition was therefore selected prior to the study to ensure sufficient study power and account for potential loss to follow-up.
Participants were recruited via e-mails sent by the University of Michigan Office of the Registrar in summer and fall of 2019 to a randomly selected sample of 4601 undergraduate students who identified as female and were enrolled in spring, summer, or fall classes in 2019. The e-mail contained information about the study, which was advertised as a study examining how the use of smartphone apps impact college students’ well-being and did not mention eating disorder risk explicitly. Individuals interested in study participation completed a brief online screening survey to determine eligibility. Participants were eligible if they were undergraduate women at the University of Michigan, had daily access to a smartphone, were fluent in English, and were at least 18 years of age. Individuals were excluded if they had a self-reported history of any medical condition that impacts the type or amount of food eaten because these individuals may be used to self-monitoring aspects of their food consumption. Additionally, individuals who reported dietary self-monitoring in the last year were excluded due to the potential that recent use may impact behavior during the trial. Participants who had a current or previous eating disorder diagnosis or an EDE-QS score ≥ 2, indicating high eating disorder risk, were also excluded to reduce the likelihood of participants experiencing severe adverse effects. A cut-off of an EDE-QS score ≥ 2 was selected based on the common use of 4 as the cutoff on the full-length Eating Disorder Examination Questionnaire (EDE-Q) as a marker of high eating disorder risk.31,32 The EDE-Q has twice the number of response options as the EDE-QS, therefore we halved the cutoff for high risk. Data collection occurred between May and October 2019.
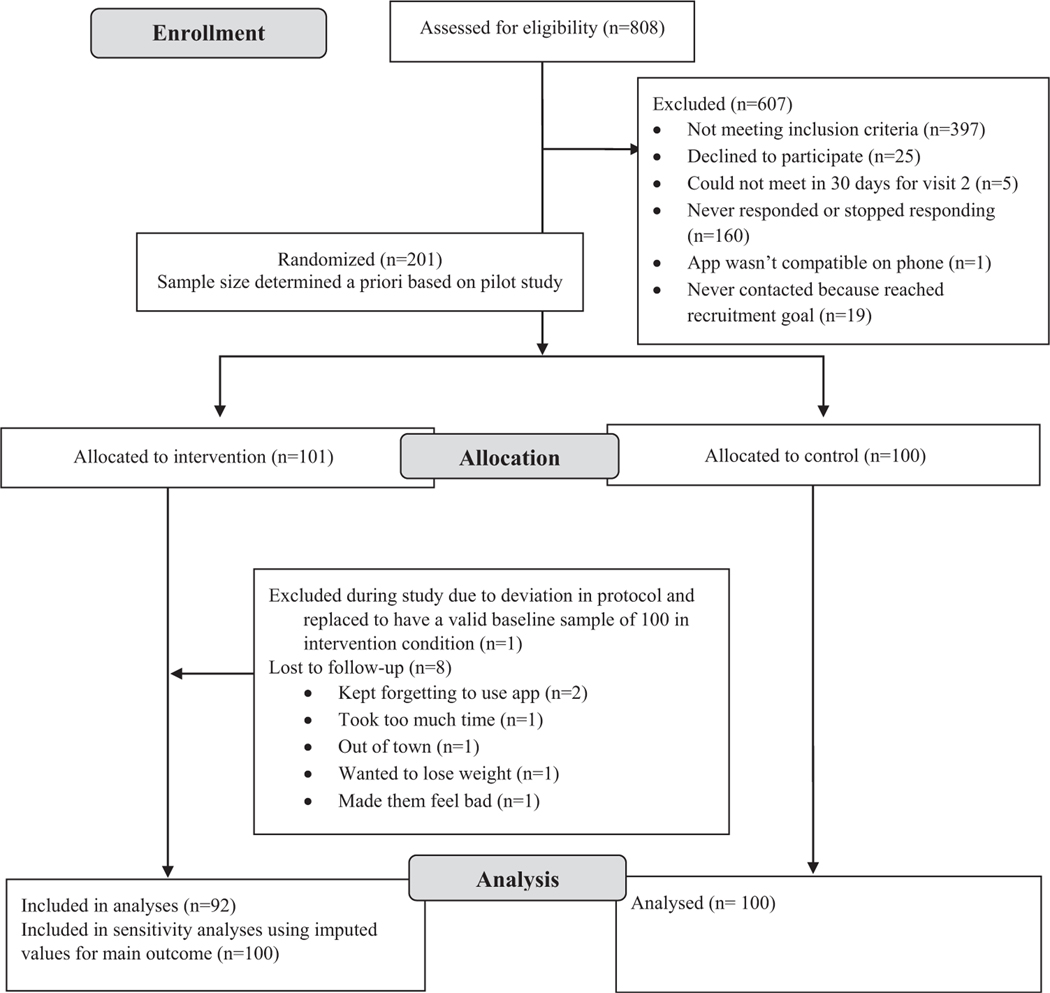
Among the 4601 students e-mailed, 808 (17.6% of those contacted) completed the screening survey and 411 (50.9% of those screened) were eligible for study participation. To reach the a priori sample size of 200 participants, the first 201 eligible participants (48.9% of those deemed eligible) were invited and elected to enroll in the study. One participant was excluded due to deviation from study protocol that invalidated her baseline survey. Therefore, there were 100 individuals in the intervention condition and 100 individuals in the control condition. Eight participants assigned to the intervention condition were lost to follow-up between study visits, thus 92 participants from the intervention condition and 100 participants from the control condition were included in analyses. The study’s CONSORT diagram is included as the Figure. The study was determined to be exempt from oversight by the University of Michigan Institutional Review Board. The study did involve deception, as participants were told that the purpose of the study was to examine how self-monitoring apps influenced college student’s well-being, which was accurate, but not specific as to not bias results. At the end of the study, participants were informed of the true purpose of the study and provided a list of mental health resources. Because of the nature of the study, we opted to include written informed consent, though not required by the institutional review board. The study was registered at clinicaltrials.gov (NCT04052529).
Figure.
Consort diagram.
Procedure
Study visits occurred in person on the University of Michigan campus at the Behavioral Nutrition Lab and were conducted by trained research staff. Participants were randomly assigned to the intervention or control condition by research assistants at a 1:1 ratio. Before participant enrollment began, envelopes were prepared that indicated whether participant would be in the intervention or control condition with an equal number of envelopes prepared for each condition. Prior to the participants first study visit, research assistants randomly selected and opened an envelope to determine which condition the participant would be assigned to. Upon arrival at the baseline study visit, participants provided informed written consent, after which they completed study surveys and had their height (in centimeters) and weight (in kilograms) measured by trained research assistants using a stationary stadiometer (Seca 213 stadiometer) and scale (Seca 873 scale). Study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at the University of Michigan.33,34 REDCap is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for data integration and interoperability with external sources.
For participants randomized to the intervention condition, after surveys and anthropometrics were completed, MyFitnessPal was downloaded to their smartphone and research assistants set up the account using standardized settings. Participants’ daily caloric needs for weight maintenance were calculated using the Mifflin St. Jeor equation35 and entered into the app. The app was set to send participants a daily reminder to track their intake at 10:30 AM. Participants were instructed to log everything they ate or drank using MyFitnessPal immediately after consuming it, starting the day after the baseline study visit and continuing until they were seen for the post-intervention study visit, approximately 30 days following the baseline study visit. Participants were also instructed not to change any of the app settings, including the username and password; not to link MyFitnessPal to any other smartphone app; and to only use MyFitnessPal to track their dietary intake. As 1 exclusion criterion for all participants was any dietary self-monitoring in the past year, the control condition was a lack of introduction to dietary self-monitoring via MyFitnessPal rather than explicit instruction not to engage in dietary self-monitoring. Participants randomized to the control condition completed the written informed consent, which informed them of the purpose of the study, completed the baseline survey, had their anthropometrics taken, scheduled their follow-up study visit, and were dismissed.
Procedures for the post-intervention study visit were similar to those for the baseline study visit. Participants completed study surveys and had their weight measured again. After the completion of measures, participants were informed that the purpose of the study was to examine the effect of dietary self-monitoring via MyFitnessPal on eating disorder risk and were provided a list of locally available mental health resources.
Measures
Eating Disorder Risk.
Risk of eating disorder was assessed using the EDE-QS.36 The EDE-QS is a 12-item measure that assesses eating disorder behaviors and cognitions over the past week. The EDE-QS is reliable when compared with the EDE-Q, the gold standard self-report measure of eating disorder. A global score for the EDE-QS was calculated by averaging response options from the 12 items, which are scored from 0 (0 days) to 3 (6–7 days), or not at all (0) to markedly (3), as is standard.37,38 Individual eating disorder behaviors assessed by the EDE-QS were also examined including fasting (not eaten for 8 or more waking hours to control weight or shape), purging (vomiting or taking laxatives to control weight or shape), compulsive exercise (exercising in a compulsive or driven way to control weight or shape), trying to limit amount of food (to control weight or shape), binge eating, and loss of control eating. Eating disorder behaviors were dichotomized into no versus any use in the last 7 days.
Secondary Mental Health Outcomes.
Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale Revised39; state anxiety was assessed using the state subscale of the State-Trait Anxiety Inventory40; body image was assessed using the Body Image States Scale, which measures momentary body image41; and overall quality of life was assessed using the Brunnsviken Brief Quality of life scale.42 All secondary mental health outcomes were analyzed as recommended by the individual scoring instructions as continuous variables.
Health Behaviors.
Nutrition behaviors were assessed using questions adapted from the Youth Risk Behavior Surveillance System survey,43 as has been done previously among college students,44,45 and responses were made into continuous variables of number of times consumed per week. Nutrition behaviors assessed included intake of fruits, vegetables, combined fruits and vegetables, 100% fruit juice, soda, diet soda, energy drinks (eg, Monster, Red Bull, or Rockstar), sports drinks (eg, Gatorade or Powerade), low-calorie sports drinks, water, and sparkling water (eg, LaCroix). Dietary intake was assessed with the question, “During the past 7 days, how many times did you drink/eat___?” with response options, “I did not eat/drink___ during the past 7 days”; “1 to 3 times during the past 7 days”; “1 time per day”; “2 times per day”; “3 times per day”; and “4 or more times per day”. Breakfast consumption was assessed using the question, “During the past 7 days, on how many days did you eat breakfast?” with response options of 0 to 7. Each nutrition behavior was made into a continuous variable for number of times consumed in the last week, with midpoints of response options used when necessary.
Physical activity was assessed using the following questions, which were modeled after the Youth Risk Behavior Surveillance System43–45: “During the past 7 days, on how many days were you physically active for a total of at least 30 minutes per day? (Add up all the time you spent in any kind of physical activity that increased your heart rate and made you breathe hard some of the time.)”; “During the past 7 days, on how many days did you do exercise to strengthen or tone your muscles, such as push-ups, sit-ups, or weight lifting?”; and “During the past 7 days, how many minutes were you physically active? (Add up all the time you spent in any kind of physical activity that increased your heart rate and made you breathe hard some of the time.)”. The first 2 questions had response options of 0 to 7 days and the third question was open ended and was analyzed as a continuous variable. Participants who reported total exercise of more than 4 hours per day were excluded from the continuous measure of physical activity analyses (n = 2). All variables were treated as continuous outcomes.
Social media use was assessed with a series of questions: “Thinking back over the past week, how much time do you usually spend on____ on a typical day? Include total time spent on all devices.” This question was asked for Facebook, Instagram, Snapchat, and Twitter. Response options for each question included “0 minutes (none)”; “Less than half an hour”; “Between a half an hour to 1 hour”; “More than 1 hour, but less than 2 hours”; “More than 2 hours, but less than 3 hours”; “More than 3 hours, but less than 4 hours”; and “More than 4 hours.” Each form of social media was treated as a continuous outcome using the midpoint of response options where applicable and a combined variable was created for total social media use per day.
Screen time was assessed using 3 questions about time spent in the past 7 days watching TV, watching on-demand services, and playing games or other screen time not related to school work. Response options for each of the 3 questions included “0 minutes (I did not___)”; “Less than 1 hour”; “1 hour or more, but less than 2 hours”; “2 hours or more, but less than 3 hours”; “3 hours or more, but less than 4 hours”; “4 hours or more, but less than 5 hours”; and “5 hours or more.” Each of the 3 types of screen time (TV, on-demand services, and games/other screen time) was treated as a continuous outcome using the midpoint of response options where applicable and a combined variable was created for total screen time use per day.
The question used to assess self-weighing frequency was based on the survey question used in Project EAT (Eating and Activity over Time) and modified to ask about the last week46: “In the past 7 days, how often did you weigh your-self?” with response options of “0 times,” “1 time,” “2–3 times,” “4–6 times,” “Once a day,” and “More than once a day.” The outcome was made into a continuous variable of number of times weighing in the past week using midpoints of response options where applicable. Physical activity self-monitoring was assessed using the following 2 questions: “In the past 7 days, how often did you track your physical activity? This can include wearing a pedometer, keeping track of minutes of exercise, repetitions, etc” and “In the past 7 days, how often did you track the number of calories burned during physical activity?” Response options for both questions included “Never,” “Sometimes,” “About half the time,” “Most of the time,” “Always,” and “I was not physically active in the last 7 days.” Each type of physical activity self-monitoring was treated as a linear variable representing the proportion of time that they tracked (ie, 0% of the time, 25% of the time, 50% of the time, 75% of the time, 100% of the time) with those who had not exercised marked as missing.
Demographics.
Participants reported demographic characteristics including race/ethnicity, parental education, and age. Race/ethnicity was assessed using the question “What is your race/ethnicity? Select all that apply.” Response options included “Asian or Pacific Islander,” “Black or African American,” “Hispanic or Latino,” “Native American or American Indian,” “White,” and “Other.” All individuals who selected “Hispanic or Latino” were considered Hispanic/Latina; individuals who selected more than 1 race or selected “Native American or American Indian” or “Other” were considered other race/ethnicity. Parent education was assessed with the request “Select the highest level of education achieved by a parent.” Response options included: “Less than a high school education,” “High school education or GED equivalent,” “Some college,” “Associate’s or other 2-year degree,” “Bachelor’s degree,” and “Advanced degree (master’s degree or higher).” For analytic purposes, the categories were condensed to high school or less, some college or associate’s degree, bachelor’s degree, and graduate degree. Age was calculated using the day of their first study visit and their birthday, which was ascertained using the question “What is your birthday?” Body mass index (BMI; calculated as kilograms per square meter) was also calculated using the measured height and weight and categorized based on standard classifications: less than 18.5, 18.5–24.9, 25–29.9 and 30 and above.47
Intervention Fidelity.
Intervention fidelity was assessed by calculating the proportion of days between study visits that individuals logged at least 500 calories in MyFitnessPal.
Statistical Analyses
Univariate and bivariate descriptive statistics of baseline characteristics were computed for the sample overall and by study condition. Linear regression models were developed to examine the continuous outcomes described previously as dependent variables with condition assignment as the independent variable and baseline score of the dependent variable included as a covariate. For dichotomous variables, logistic regression models were developed to calculate the odds of participants assigned to the intervention condition engaging in the behavior post-intervention compared with those assigned to the control condition, adjusting for baseline use of behavior. Odds ratios (ORs) with 95% CIs were reported for all dichotomous variables. All analyses were conducted using SAS Software, Version 9.4 (SAS Institute Inc., Cary, NC, USA). Results were considered statistically significant if P < .05.
RESULTS
Approximately half of the study sample identified as White (51.0%) and nearly a third as Asian (29.3%); half of participants reported having at least 1 parent with a graduate degree (Table 1). The average BMI was 23.1, with approximately two-thirds of the sample having a BMI between 18.5 and 24.9, and the average age was 20.2 years old.
Table 1.
Baseline characteristics of sample of 200 undergraduate women, overall and by intervention condition assigned in randomized controlled trial
| Overall (n = 200) | Intervention (n = 100) | Control (n = 100) | |
|---|---|---|---|
|
| |||
| Sociodemographic Characteristic |
|
||
| Race/ethnicity | |||
| White | 101 (51.0) | 49 (50.0) | 52 (52.0) |
| Black or African | 13 (6.6) | 6 (6.1) | 7 (7.0) |
| American | |||
| Hispanic/Latina | 12 (6.1) | 6 (6.1) | 6 (6.0) |
| Asian | 58 (29.3) | 30 (30.6) | 28 (28.0) |
| Other | 14 (7.1) | 7 (7.1) | 7 (7.0) |
| Parent education | |||
| High school or less | 19 (9.5) | 8 (8.0) | 11 (11.0) |
| Some college or | 31 (15.5) | 15 (15.0) | 16 (16.0) |
| associate’s degree | |||
| Bachelor’s degree | 50 (25) | 23 (23.0) | 27 (27.0) |
| Graduate degree | 100 (50.0) | 54 (54.0) | 46 (46.0) |
| Body mass index a | |||
| <18.5 | 16 (8.0) | 9 (9.0) | 7 (7.0) |
| 18.5–24.9 | 135 (67.5) | 73 (73.0) | 62 (62.0) |
| 25–29.9 | 33 (16.5) | 12 (12.0) | 21 (21.0) |
| ≥30.0 | 16 (8.0) | 6 (6.0) | 10 (10.0) |
|
|
|||
| Body mass index | 23.1 (4.8) | 22.6 (4.0) | 23.6 (5.5) |
| Age, y | 20.2 (2.4) | 20.4 (3.1) | 20.0 (1.2) |
Calculated as kilograms per square meter.
On average, participants randomized to the intervention condition who completed the study used the app 89.1% of the days between study visits (SD = 16.9%, interquartile range: 85.3% to 100.0%) and a median of 94.1% of days. There were no differences in EDE-QS score between study conditions post-intervention (β = −.04, 95% CI: −.11 to 0.02, P = .17) (Table 2). The intervention also did not change participants’ likelihood of fasting (OR = 0.47, 95% CI: 0.12–1.78, P = .27), compulsive exercising (OR = 0.61, 95% CI: 0.25–1.52, P = .29), binge eating (OR = 1.51, 95% CI: 0.57–4.01, P = .41), limiting amount of food (OR 0.55, 95% CI: 0.27–1.12, P .10), or engaging in loss of control eating (OR = 0.70, 95% CI: 0.32–1.57, P = .39). No participants reported purging at the end of the study, therefore an odds ratio could not be computed. The intervention also did not affect secondary mental health outcomes including state anxiety (β = .30, 95% CI: = −.52 to 1.11, P = .48), depressive symptoms (β = −.22, 95% CI: − 1.21 to .77, P = .66), body image (β − .03, 95% CI: −.26 to 0.21, P = .81), or quality of life (β = −1.75, 95% CI: − 5.51 to 2.01, P = .36) (Table 3).
Table 2.
Effects of introducing dietary self-monitoring via MyFitnessPal on eating disorder risk and behaviors among undergraduate women in randomized controlled triala
| Eating Disorder Behavior | Baseline prevalence | End of study prevalence | Odds ratio | 95% CI |
|---|---|---|---|---|
|
| ||||
| Fasting |
|
|||
| Intervention | 11 (11.0) | 4 (4.4) | 0.47 | 0.12–1.78 |
| Control | 11 (11.1) | 9 (9.1) | ||
| Purging | ||||
| Intervention | 0 (0.0) | 0 (0.0) | — | — |
| Control | 1 (1.0) | 0 (0.0) | ||
| Compulsive exercise | ||||
| Intervention | 8 (8.0) | 9 (9.9) | 0.61 | 0.24–1.52 |
| Control | 18 (18.4) | 18 (18.0) | ||
| Limiting amount of food | ||||
| Intervention | 44 (44.0) | 27 (29.4) | 0.55 | 0.27–1.12 |
| Control | 42 (42.0) | 40 (40.0) | ||
| Binge eating | ||||
| Intervention | 10 (10.0) | 13 (14.1) | 1.51 | 0.57–4.01 |
| Control | 10 (10.1) | 10 (10.2) | ||
| Loss of control eating | ||||
| Intervention | 24 (24.0) | 19 (20.7) | 0.70 | 0.32–1.57 |
| Control | 19 (19.2) | 22 (22.2) | ||
| Eating Disorder Risk | Baseline | End of study | β (SE)b | P value |
|
| ||||
| EDE-QS c |
|
|||
| Intervention | 0.42 (0.37) | 0.38 (0.29) | −0.04 (0.03) | .17 |
| Interventiond | 0.42 (0.37) | 0.40 (0.31) | −0.04 (0.03) | .23 |
| Control | 0.47 (0.42) | 0.47 (0.40) | ||
Eating disorder behaviors are dichotomized based on any use in the 7 days prior to survey; fasting (8 or more waking hours without eating), purging (vomiting or using laxatives), compulsive exercise (exercising in a compulsive or driven manner), and limiting amount of food were specifically for weight or shape control.
β is linear regression coefficient representing change in EDE-QS post score for those in intervention condition compared with the control condition.
EDE-QS = Eating Disorder Examination Questionnaire Short Form (range 0–3, higher score indicate higher eating disorder risk30).
Sensitivity analyses where baseline values were imputed as end of study values for those lost to follow-up.
Table 3.
Effects of introducing dietary self-monitoring via MyFitnessPal on secondary mental health outcomes among undergraduate women in randomized controlled trial
| Mental Health Outcome | Baseline | End of study | β (SE)a | P value |
|---|---|---|---|---|
|
| ||||
|
|
||||
| Anxiety (state subscale of STAI b ) | ||||
| Intervention | 10.7 (3.5) | 11.4 (3.8) | 0.30 (0.41) | .48 |
| Control | 10.9 (3.1) | 11.2 (3.1) | ||
| Depression symptoms (CESD-R-10 c ) | ||||
| Intervention | 5.9 (4.0) | 6.4 (4.8) | −0.22 (0.50) | .66 |
| Control | 6.2 (4.1) | 6.8 (4.4) | ||
| Body image (BISS d ) | ||||
| Intervention | 5.4 (1.1) | 5.4 (1.2) | −0.03 (0.12) | .81 |
| Control | 5.1 (1.3) | 5.1 (1.2) | ||
| Quality of life (BBQ e ) | ||||
| Intervention | 61.1 (17.7) | 57.7 (17.5) | −1.75 (1.91) | .36 |
| Control | 61.7 (17.5) | 59.6 (15.5) | ||
β is linear regression coefficient representing change in mental health outcome for those in intervention condition compared to the control condition.
STAI = State-Trait Anxiety Inventory (range 6–24, higher numbers indicate higher levels of state anxiety).
CESD-R-10 = Center for Epidemiologic Studies Depression Scale Revised (range 0–30, higher numbers indicate higher levels of depressive symptoms).
BISS = Body Image States Scale (range 1–9, higher numbers indicate higher body image).
BBQ = Brunnsviken Brief Quality of Life Scale (range 0–96, higher number indicate higher quality of life).
The intervention did not influence any of the health behaviors assessed including dietary intake, amount of physical activity, social media use, or screen time (Table 4). BMI also did not change differentially by intervention condition (β = .05, 95% CI: −.08 to .18, P = .44). Self-weighing frequency decreased in the intervention condition (β −.35, 95% CI: −.63 to −.07, P = .02), but intervention condition was not associated with either form of physical activity self-monitoring.
Table 4.
Effects of introducing dietary self-monitoring via MyFitnessPal on health behaviors among undergraduate women in randomized controlled trial
| Health Behavior | Baseline | End of Study | β(SE)a | P value |
|---|---|---|---|---|
|
| ||||
|
|
||||
| Nutrition, times/wk | ||||
| Fruit | ||||
| Intervention | 6.62 (5.67) | 6.23 (5.75) | 0.16 (0.64) | .81 |
| Control | 6.23 (5.36) | 6.01 (4.73) | ||
| Vegetables | ||||
| Intervention | 12.94 (8.07) | 11.60 (6.64) | −0.25 (0.81) | .76 |
| Control | 11.19 (6.47) | 10.89 (7.05) | ||
| Combined fruit and vegetables | ||||
| Intervention | 19.56 (11.11) | 17.83 (9.85) | −0.14 (1.14) | .90 |
| Control | 17.42 (10.00) | 16.90 (9.91) | ||
| Drink 100% fruit juice | ||||
| Intervention | 1.23 (1.93) | 1.79 (4.07) | 0.27 (0.50) | .59 |
| Control | 1.49 (2.37) | 1.61 (2.93) | ||
| Soda | ||||
| Intervention | 0.81 (1.53) | 0.87 (1.52) | −0.09 (0.21) | .68 |
| Control | 0.98 (1.80) | 1.07 (2.04) | ||
| Diet soda | ||||
| Intervention | 0.35 (1.19) | 0.37 (1.71) | 0.16 (0.16) | .31 |
| Control | 0.30 (1.49) | 0.19 (1.00) | ||
| Energy drinks | ||||
| Intervention | 0.24 (0.76) | 0.21 (0.74) | 0.04 (0.08) | .61 |
| Control | 0.16 (0.55) | 0.14 (0.51) | ||
| Sports drinks | ||||
| Intervention | 0.52 (1.72) | 0.41 (1.07) | 0.15 (0.12) | .22 |
| Control | 0.39 (1.58) | 0.24 (0.65) | ||
| Low-calorie sports drinks | ||||
| Intervention | 0.14 (0.76) | 0.12 (0.63) | 0.06 (0.07) | .40 |
| Control | 0.11 (0.60) | 0.06 (0.34) | ||
| Water | ||||
| Intervention | 21.81 (7.57) | 20.74 (7.51) | −0.54 (0.78) | .49 |
| Control | 21.42 (8.20) | 21.12 (7.50) | ||
| Sparkling water | ||||
| Intervention | 0.51 (1.53) | 0.51 (1.44) | 0.05 (0.18) | .77 |
| Control | 1.08 (3.13) | 0.91 (2.42) | ||
| Breakfast | ||||
| Intervention | 4.92 (2.21) | 4.87 (2.08) | 0.15 (0.21) | .49 |
| Control | 4.90 (2.14) | 4.71 (2.10) | ||
| Physical activity | ||||
| Physical activity, min/wk | ||||
| Intervention | 134.3 (111.6) | 124.1 (108.8) | −25.71 (16.33) | .12 |
| Control | 143.6 (134.9) | 153.3 (148.5) | ||
| Number of days active for at least 30 min | ||||
| Intervention | 3.12 (1.99) | 2.79 (2.06) | −0.35 (0.23) | .13 |
| Control | 2.95 (2.06) | 2.94 (2.13) | ||
| Number of strength training days | ||||
| Intervention | 1.10 (1.54) | 0.92 (1.34) | 0.14 (0.16) | .40 |
| Control | 1.18 (1.45) | 0.85 (1.13) | ||
| Screen time, h/wk | ||||
| Intervention | 0.65 (0.82) | 0.60 (0.74) | −0.09 (0.09) | .30 |
| Control | 0.74 (0.93) | 0.73 (0.91) | ||
| Intervention | 1.28 (1.13) | 1.09 (0.87) | −0.06 (0.10) | .56 |
| Control | 1.36 (1.14) | 1.18 (1.02) | ||
| Snapchat | ||||
| Intervention | 1.03 (0.98) | 1.02 (0.92) | 0.11 (0.09) | .26 |
| Control | 1.37 (1.14) | 1.12 (0.97) | ||
| Intervention | 0.67 (1.07) | 0.62 (1.04) | 0.07 (0.08) | .40 |
| Control | 0.63 (1.03) | 0.50 (0.81) | ||
| Total social media | ||||
| Intervention | 3.61 (2.60) | 3.33 (2.28) | 0.00 (0.25) | .99 |
| Control | 4.08 (2.68) | 3.53 (2.25) | ||
| TV | ||||
| Intervention | 0.55 (0.94) | 0.80 (1.28) | 0.17 (0.16) | .29 |
| Control | 0.41 (0.94) | 0.59 (1.07) | ||
| On-demand service | ||||
| Intervention | 1.52 (1.45) | 1.31 (1.37) | −0.15 (0.15) | .33 |
| Control | 1.50 (1.44) | 1.43 (1.29) | ||
| Games/other screen time | ||||
| Intervention | 1.98 (1.89) | 1.42 (1.71) | −0.06 (0.20) | .76 |
| Control | 2.10 (1.78) | 1.55 (1.73) | ||
| Screen time (combined TV, on-demand, games) | ||||
| Intervention | 4.04 (2.95) | 3.53 (2.86) | −0.09 (0.31) | .78 |
| Control | 4.01 (2.54) | 3.56 (2.54) | ||
| Self-monitoring | ||||
| Self-weighing, frequency/wk | ||||
| Intervention | 0.66 (1.36) | 0.33 (0.72) | −0.35 (0.14) | 0.02 |
| Control | 0.44 (1.00) | 0.60 (1.38) | ||
| Physical activity self-monitoring, proportion | ||||
| Intervention | 0.30 (0.37) | 0.36 (0.40) | 0.05 (0.05) | 0.32 |
| Control | 0.33 (0.36) | 030 (0.35) | ||
| Track calories burned during physical activity, proportion | ||||
| Intervention | 0.12 (0.25) | 0.20 (0.34) | 0.06 (0.04) | 0.13 |
| Control | 0.15 (0.29) | 0.14 (0.26) | ||
β is linear regression coefficient representing change in mental health outcome for those in intervention condition compared with the control condition.
DISCUSSION
Assignment of 1 month of dietary self-monitoring via MyFitnessPal did not change eating disorder risk, state anxiety, depressive symptoms, body image, or quality of life among college women with low baseline eating disorder risk. Additionally, no effects were seen on other forms of physical activity self-monitoring, nutritional behaviors, physical activity, screen time, or social media use. These findings suggest that for undergraduate women who have not recently engaged in dietary self-monitoring and have low eating disorder risk, the short-term introduction of dietary self-monitoring does not impact their mental health or health behaviors.
Study findings were counter to our hypothesis that dietary self-monitoring would increase risk of eating disorders, which was informed by previous cross-sectional studies that identified positive associations between dietary self-monitoring and eating disorder risk among college students.14–18 There are 2 possible explanations for the apparent discrepancy between our findings and the cross-sectional literature. First, individuals who are already concerned about eating and weight may go on to engage in dietary self-monitoring and develop higher eating disorder risk concurrently, both stemming from preexisting eating and weight concern. Alternatively, dietary self-monitoring may be a symptom of excessive concern related to eating and weight, thus explaining the strong cross-sectional associations. Together, these findings suggest that dietary self-monitoring may be a component of or occur concurrently to eating disorder cognitions and behaviors, but dietary self-monitoring by itself does not cause increased eating disorder risk among this population.
Findings from previous work indicate that dietary self-monitoring, particularly calorie counting, is often not used in isolation.15,17,18 Therefore, it is important to consider that the null results in the present study may be due to insufficient dose or exposure to weight-related self-monitoring. Specifically, dietary self-monitoring may not increase eating disorder risk when used independently, but there may be synergistic effects when used with other behaviors such as tracking weight. We did see that self-weighing decreased in the intervention group, likely an artifact of the intervention, and ultimately, decreasing self-weighing may have neutralized any effects of dietary self-monitoring. Alternatively, it is possible that engagement in 1 type of self-monitoring may offset other types for some individuals. Additionally, some individuals may be more susceptible to the potential consequences of dietary self-monitoring than others; for example, we see no increased eating disorder risk among our baseline low-risk sample, but other studies among individuals with eating disorders have reported that they believe dietary self-monitoring apps like MyFitnessPal contributed to the development of their eating disorder.19,48 Therefore, null results in our study may be due to the selection of a low-risk sample, and future research should explore whether there are populations for whom dietary self-monitoring is contraindicated. For example, for individuals who are already at high-risk for an eating disorder, the increased attention to food, exercise, or weight may exacerbate their preexisting food or weight concerns. Similarly, personality traits such as perfectionism may amplify susceptibility to disordered eating among those who engage in dietary self-monitoring.49 Individuals with perfectionism hold themselves to high standards and may see their behaviors as right or wrong when tracking.50 Therefore, individuals with perfectionistic traits may become exceedingly rigid about meeting weight-related self-monitoring goals, which may ultimately lead to obsessional thinking about food, exercise, or weight.49,51 Further in support of this theory, neuroticism has been shown to be a mediator in the relationship between female sex and calorie counting app use.23
We also found that dietary self-monitoring did not alter other mental health outcomes or health behaviors. To our knowledge, this is the first study to assess these relationships among undergraduate women and outside the context of weight management or structured intervention. Our results ran counter to our hypothesis that mental health would deteriorate, which was based on the results from a randomized controlled trial examining the effects of self-weighing among college women that found repeated weighing led to increases in anxiety and depression and a decrease in self-esteem.8 Similar to eating disorder risk, individuals who are more likely to feel guilt or shame may be more likely to experience negative mental health effects, but that there is no effect among those less likely to feel guilt or shame. For example, in previous studies examining online forums, researchers found that some users who fail to meet goals set by themselves or by the app experience stress or feelings of guilt that may lead to increases in anxiety or other negative emotional states.49,51 Furthermore, in structured weight management populations, null or positive results in mental health outcomes after self-monitoring are likely confounded by the fact that mental health improves short term with weight loss and the social support that is often part of structured weight management programs.8,21,22 Therefore, in studies among nonclinical populations, results may be null or negative due to there being no weight change or social support.
In addition, the lack of association between self-monitoring and health behavior change was unexpected. Although cross-sectional studies show that dietary self-monitoring and health app use is associated with increased consumption of healthy foods among college students, the results may be confounded by nutritional knowledge or interest.27,28,30 In weight management trials, participants often receive nutrition education along with instruction on dietary self-monitoring; taken together, it is likely that nutrition knowledge or nutrition education could explain better dietary intake rather than the act of self-monitoring itself improving dietary intake.
The study had several strengths, most notably the use of a randomized controlled trial design, which to our knowledge has never previously been used to understand the impacts of dietary self-monitoring in nonclinical populations. Additionally, all mental health outcomes were assessed using validated scales and dietary intake, and physical activity questions were modeled after those used in national surveillance surveys.36,39–43 However, this study is not without limitations. Because the sample was limited to women at a single institution, results may not be generalizable to all college students or young adults. Loss to follow-up was also exclusively experienced in the intervention condition. However, sensitivity analysis in which post-intervention EDE-QS scores were imputed from baseline measurements did not alter findings.
CONCLUSIONS
This study provides valuable information on the effects of dietary self-monitoring on the health of undergraduate women. Although cross-sectional data show a strong relationship between dietary self-monitoring and eating disorder risk, our findings demonstrate that dietary self-monitoring does not increase eating disorder risk among undergraduate women who have not recently engaged in dietary self-monitoring and have low baseline eating disorder risk. Thus, dietary self-monitoring may be an indicator of increased eating disorder risk but not a direct causal contributor to eating disorder risk for this population. Furthermore, the findings suggest that dietary self-monitoring outside of clinical weight management contexts may not increase engagement in health-promoting behaviors for this population. Overall, a precision health lens may be warranted in further understanding for whom dietary self-monitoring is a neutral, beneficial, or harmful behavior.
RESEARCH SNAPSHOT.
Research Question:
Does introducing dietary self-monitoring via a popular smartphone app impact undergraduate women’s eating disorder risk, mental health, or health behaviors?
Key Findings:
A randomized controlled trial (n = 200) showed that among undergraduate women who were at low baseline risk for an eating disorder and had not engaged in dietary self-monitoring in the year prior, dietary self-monitoring for approximately 1 month did not impact eating disorder risk. Furthermore, the intervention did not lead to changes in other mental health outcomes or health behaviors.
ACKNOWLEDGEMENTS
We would like to thank the students who participated in the research study as well as the research assistants who made this study possible.
FUNDING/SUPPORT
The University of Michigan Rackham Predoctoral Fellowship assisted in the funding for the dissertation of S. L. Hahn, of which this research was a part. Additionally, the Rackham Graduate Student Research Grant assisted in paying for this research. The time to write this manuscript by S. L. Hahn was partially funded by Grant Number T32MH082761 from the National Institute of Mental Health (principal investigator: Scott Crow). Research Electronic Data Capture was provided through the Michigan Institute for Clinical and Health Research (Clinical and Translational Science Award UL1TR002240). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institute of Health.
Footnotes
STATEMENT OF POTENTIAL CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
TRIAL REGISTRATION
Registered with clinicaltrials.gov, trial registration number: NCT04052529.
The Continuing Professional Education (CPE) quiz for this article is available for free to Academy members through the MyCDRGo app (available for iOS and Android devices) and through www.jandonline.org (click on “CPE” in the menu and then “Academy Journal CPE Articles”). Log in with your Academy of Nutrition and Dietetics or Commission on Dietetic Registration username and password, click “Journal Article Quiz” on the next page, then click the “Additional Journal CPE quizzes” button to view a list of available quizzes. Non-members may take CPE quizzes by sending a request to journal@eatright.org. There is a $45 fee per quiz (includes quiz and copy of article) for non-members. CPE quizzes are valid for 3 years after the issue date in which the articles are published.
References
- 1.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129:S102–S138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harvey J, Krukowski R, Priest J, West D. Log often, lose more: Electronic dietary self-monitoring for weight loss. Obesity (Silver Spring). 2019;27:380–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obes Res. 1998;6:219–224. [DOI] [PubMed] [Google Scholar]
- 4.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13:623–649. [Google Scholar]
- 5.MyFitnessPal—how an App got 165 Million Users. In: Jones D, ed. Mobile Engagement Podcast. iTunes; 2016. [Google Scholar]
- 6.Verto Analytics. Most popular health and fitness apps in the United States as of May 2018, by monthly active users (in millions). Accessed April 27, 2019. https://www.statista.com/statistics/650748/health-fitness-app-usage-usa/.
- 7.Neumark-Sztainer D, van den Berg P, Hannan PJ, Story M. Self-weighing in adolescents: helpful or harmful? Longitudinal associations with body weight changes and disordered eating. J Adolesc Health. 2006;39:811–818. [DOI] [PubMed] [Google Scholar]
- 8.Ogden J, Whyman C. The effect of repeated weighing on psychological state. Eur Eat Disord Rev. 1997;5:121–130. [Google Scholar]
- 9.Berry R, Rodgers R, Campagna J. Outperforming iBodies: A conceptual framework integrating body performance self-tracking technologies with body image and eating concerns. Sex Roles. 2020;85(1):1–12. [Google Scholar]
- 10.Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000e2018 period: a systematic literature review. Am J Clin Nutr. 2019;109:1402–1413. [DOI] [PubMed] [Google Scholar]
- 11.Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2006;19:438–443. [DOI] [PubMed] [Google Scholar]
- 13.Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68:714–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Romano KA, Swanbrow Becker MA, Colgary CD, Magnuson A. Helpful or harmful? The comparative value of self-weighing and calorie counting versus intuitive eating on the eating disorder symptomology of college students. Eat Weight Disord. 2018;23:841–848. [DOI] [PubMed] [Google Scholar]
- 15.Simpson CC, Mazzeo SE. Calorie counting and fitness tracking technology: Associations with eating disorder symptomatology. Eat Behav. 2017;26:89–92. [DOI] [PubMed] [Google Scholar]
- 16.Plateau CR, Bone S, Lanning E, Meyer C. Monitoring eating and activity: Links with disordered eating, compulsive exercise, and general wellbeing among young adults. Int J Eat Disord. 2018;51: 1270–1276. [DOI] [PubMed] [Google Scholar]
- 17.Hahn SL, Sonneville KR, Kaciroti N, Eisenberg D, Bauer KW. Relationships between patterns of technology-based weight-related self-monitoring and eating disorder behaviors among first year university students. Eat Behav. 2021;42:101520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hahn SL, Bauer KW, Kaciroti N, Eisenberg D, Lipson SK, Sonneville KR. Relationships between patterns of weight-related self-monitoring and eating disorder symptomology among undergraduate and graduate students. Int J Eat Disord. 2021;54(4):595–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levinson CA, Fewell L, Brosof LC. My Fitness Pal calorie tracker usage in the eating disorders. Eat Behav. 2017;27:14–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jebeile H, Gow ML, Baur LA, Garnett SP, Paxton SJ, Lister NB. Treatment of obesity, with a dietary component, and eating disorder risk in children and adolescents: A systematic review with meta-analysis. Obes Rev. 2019;20:1287–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gow ML, Tee MSY, Garnett SP, et al. Pediatric obesity treatment, self-esteem, and body image: A systematic review with meta-analysis. Pediatr Obes. 2020;15. 2020;e12600. [DOI] [PubMed] [Google Scholar]
- 22.Benn Y, Webb TL, Chang BP, Harkin B. What is the psychological impact of self-weighing? A meta-analysis. Health Psychol Rev. 2016;10:187–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Embacher Martin K, McGloin R, Atkin D. Body dissatisfaction, neuroticism, and female sex as predictors of calorie-tracking app use amongst college students. J Am Coll Health. 2018;66:608–616. [DOI] [PubMed] [Google Scholar]
- 24.Hahn SL, Lipson SK, Sonneville KR. Dietary self-monitoring is associated with increased likelihood of problematic alcohol use among college students. J Am Coll Health; 2020:1–6. 10.1080/07448481.2020.1741592. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lipson SK, Sonneville KR. Eating disorder symptoms among undergraduate and graduate students at 12 U.S. colleges and universities. Eat Behav. 2017;24:81–88. [DOI] [PubMed] [Google Scholar]
- 26.Kahan S, Puhl RM. The damaging effects of weight bias internalization. Obesity (Silver Spring). 2017;25:280–281. [DOI] [PubMed] [Google Scholar]
- 27.Christoph MJ, Ellison B. A cross-sectional study of the relationship between nutrition label use and food selection, servings, and consumption in a university dining setting. J Acad Nutr Diet. 2017;117:1528–1537. [DOI] [PubMed] [Google Scholar]
- 28.Graham DJ, Laska MN. Nutrition label use partially mediates the relationship between attitude toward healthy eating and overall dietary quality among college students. J Acad Nutr Diet. 2012;112:414–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quick V, Larson N, Eisenberg ME, Hannan PJ, Neumark-Sztainer D. Self-weighing behaviors in young adults: Tipping the scale toward unhealthy eating behaviors? J Adolesc Health. 2012;51:468–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarcona A, Kovacs L, Wright J, Williams C. Differences in eating behavior, physical activity, and health-related lifestyle choices between users and nonusers of mobile health apps. Am J Health Educ. 2017;48:298–305. [Google Scholar]
- 31.Fairburn CG, Beglin SJ. Eating Disorder Examination Questionnaire (6.0). In: Fairburn CG, ed. Cognitive Behavior Therapy and Eating Disorders. Guilford Press; 2008. [Google Scholar]
- 32.Carter JC, Stewart DA, Fairburn CG. Eating disorder examination questionnaire: norms for young adolescent girls. Behav Res Ther. 2001;39:625–632. [DOI] [PubMed] [Google Scholar]
- 33.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:241–247. [DOI] [PubMed] [Google Scholar]
- 36.Gideon N, Hawkes N, Mond J, Saunders R, Tchanturia K, Serpell L. Development and psychometric validation of the EDE-QS, a 12 item short form of the Eating Disorder Examination Questionnaire (EDE-Q). PLoS One. 2016;11. 2016;e0152744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duffy ME, Calzo JP, Lopez E, Silverstein S, Joiner TE, Gordon AR. Measurement and construct validity of the Eating Disorder Examination Questionnaire Short Form in a transgender and gender diverse community sample. Psychol Assess. 2021;33:459–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prnjak K, Mitchison D, Griffiths S, et al. Further development of the 12-item EDE-QS: Identifying a cut-off for screening purposes. BMC Psychiatry. 2020;20:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med. 1999;159:1701–1704. [DOI] [PubMed] [Google Scholar]
- 40.Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). Br J Clin Psychol. 1992;31(Pt 3):301–306. [DOI] [PubMed] [Google Scholar]
- 41.Cash TF, Fleming EC, Alindogan J, Steadman L, Whitehead A. Beyond body image as a trait: the development and validation of the Body Image States Scale. Eat Disord. 2002;10:103–113. [DOI] [PubMed] [Google Scholar]
- 42.Lindner P, Frykheden O, Forsstrom D, et al. The Brunnsviken Brief Quality of Life Scale (BBQ): Development and Psychometric Evaluation. Cogn Behav Ther. 2016;45:182–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kann L, McManus T, Harris WA, et al. Youth Risk Behavior Surveillance—United States, 2015. MMWR Surveill Summ. 2016;65:1–174. [DOI] [PubMed] [Google Scholar]
- 44.Youth Risk Behavior Surveillance: National College Health Risk Behavior Survey—United States, 1995. MMWR CDC Surveill Summ. 1997;46:1–56. [PubMed] [Google Scholar]
- 45.Wiley DC, James G, Furney S, Jordan-Belver C. Using the Youth Risk Behavior Survey to compare risk behaviors of Texas high school and college students. J Sch Health. 1997;67:45–49. [DOI] [PubMed] [Google Scholar]
- 46.Quick V, Loth K, MacLehose R, Linde JA, Neumark-Sztainer D. Prevalence of adolescents’ self-weighing behaviors and associations with weight-related behaviors and psychological well-being. J Adolesc Health. 2013;52:738–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894(i-xii): 1–253. [PubMed] [Google Scholar]
- 48.Linardon J, Messer M. My fitness pal usage in men: Associations with eating disorder symptoms and psychosocial impairment. Eat Behav. 2019;33:13–17. [DOI] [PubMed] [Google Scholar]
- 49.McCaig D, Elliott MT, Prnjak K, Walasek L, Meyer C. Engagement with MyFitnessPal in eating disorders: Qualitative insights from online forums. Int J Eat Disord. 2020;53:404–411. [DOI] [PubMed] [Google Scholar]
- 50.Boone L, Soenens B, Luyten P. When or why does perfectionism translate into eating disorder pathology? A longitudinal examination of the moderating and mediating role of body dissatisfaction. J Abnorm Psychol. 2014;123:412–418. [DOI] [PubMed] [Google Scholar]
- 51.Eikey EV, Reddy MC, Booth KM, et al. Desire to be underweight: Exploratory study on a weight loss app community and user perceptions of the impact on disordered eating behaviors. JMIR Mhealth Uhealth. 2017;5:e150. [DOI] [PMC free article] [PubMed] [Google Scholar]