Abstract
With increasing survival trends for children and adolescents with congenital heart defects (CHD), there is a growing need to focus on transition from pediatric to adult specialty cardiac care. To better understand parental perspectives on the transition process, a survey was distributed to 451 parents of adolescents with CHD who had recent contact with the healthcare system in Georgia (GA) and New York (NY). Among respondents, 90.7% reported excellent, very good or good health-related quality of life (HRQoL) for their adolescent. While the majority of parents (77.8%) had been told by a provider about their adolescent’s need to transition to adult specialty cardiac care, most reported concerns about transitioning to adult care. Parents were most commonly concerned with replacing the strong relationship with pediatric providers (60.7%), locating an appropriate adult provider (48.7%), and accessing adult health insurance coverage (43.6%). These findings may offer insights into transition planning for adolescents with CHD.
Keywords: Congenital, Transition, Heart defects, CHD, Cardiology
Introduction
Approximately 90% of individuals with congenital heart defects (CHD) survive to adulthood [1], reflecting a 63% increase in the number of adults living with CHD since 2000 [2]. Because early life interventions are not curative, the American Heart Association (AHA) and American College of Cardiology (ACC) recommend that individuals with CHD remain in specialty congenital cardiac care throughout their lives to manage residua, sequelae, and comorbidities associated with their condition and its associated interventions [3, 4]. Therefore, the majority of individuals born with CHD will need to transition from pediatric to adult-centered care [5].
In 2008, an AHA Scientific Statement recommended initiation of a formal transition process from pediatric to adult healthcare for individuals with CHD by age 12, with a successful transfer to adult care achieved by 18–21 years [3]. The goal of transition is to improve the quality of life, life expectancy, and productivity of young adults with special health needs [6]. Failure to transition may result in emotional and financial stress, delayed or inappropriate care, or discontinuation of care altogether [7]. Ideally, the care transition process should be purposeful and planned, address medical, psychosocial and educational needs of adolescents [8], and be tailored to the needs and maturity level of the patient [9]. To ensure a smooth transition, the transition team should include the patient, parents/caregivers, the pediatric cardiologist, all adult specialists (medical and surgical), nurse specialists, social workers, and care coordinators [10, 11]. Effective coordination between members of the team should prepare the adolescent to self-advocate and to assume adult roles and responsibilities if cognitively and emotionally able [12].
However, transition outcomes are suboptimal; recent studies have found that only 47% of individuals with CHD transition successfully to adult care and less than 30% of adults with CHD are seen by appropriate specialty cardiac care providers [13, 14]. Multi-year lapses in care become increasingly common as individuals move from adolescence into adulthood, and the first lapse in care occurs, on average, around age 20 [15]. Lapses in care have been linked to a number of adverse outcomes, including an increase in concomitant morbidities, a reduction in reported quality of life, and greater mortality [16, 17].
Structural, social, neurocognitive, and institutional barriers to successful transition of health care for individuals with CHD have been identified [10]. Examples of structural barriers include reduced health insurance availability for adults and insufficient resources for training CHD care providers [18]. Patients, parents, and providers have reported patient-pediatric provider attachment as a perceived social barrier to successful transition [19, 20]. In previous studies, parents have expressed concerns about their children’s willingness and ability to self-advocate, and have reported delays in executive function as a potential neurocognitive barrier to transition [21-23]. As executive function was strongly predictive of quality of life in a study of school-age children with CHD, an exploration of the impact of perceptions of quality of life on transition attitudes and readiness is warranted [24]. Institutional barriers highlighted by patients, parents, and providers in previous studies include a lack of adult congenital heart disease (ACHD) providers, a lack of primary care physicians knowledgeable in CHD, and difficulty navigating a complex healthcare system [20, 25, 26]. However, few studies have measured the influence of existing barriers to accessing healthcare and health-related quality of life (HRQoL).
Parents play an important role in preparing their children for transition to adult health care, serving to foster or hinder independent decision making and maturity in their adolescents. As their children transition from pediatric to adult care, parents must shift from taking full responsibility for their child’s healthcare needs to relinquishing that control to their child [27]. Assessing parental preparedness will provide insight into gaps in knowledge that can be addressed through education to promote optimal transition outcomes [28]. To better understand the parent perspective on perceptions of their adolescent’s HRQoL and the transition process, and how these are inter-related, a survey was distributed to parents of adolescents with CHD in Georgia (GA) and New York (NY).
Materials and Methods
Survey Recruitment
Recruitment differed by site (GA and NY), but was restricted to parents of adolescents (ages 11–19 years on July 1, 2017) identified by healthcare encounters with a CHD-related International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code (range 745–747). To avoid potential misclassification, adolescents with the following CHD-related diagnoses, without other eligible codes, were excluded: congenital heart block (746.86), pulmonary arteriovenous malformation (747.32), absent/hypoplastic umbilical artery (747.5), other anomalies of peripheral vascular system (747.6x) and other specified anomalies of circulatory system (747.8x). Eligible CHD ICD-9-CM diagnosis codes for each adolescent case were categorized into five hierarchical, mutually exclusive severity groups (from top to bottom of hierarchy: severe, shunt + valve, shunt, valve, and other) taking anatomy and hemodynamic severity at birth into consideration [29]. Severity was collapsed further into severe cases and non-severe cases, where severe represents a CHD usually requiring surgical or catheter intervention within the first year of life and non-severe comprises those with a shunt + valve, shunt, valve or other lesion.
In GA, where there is a statewide network of pediatric cardiology clinics, survey participants were recruited from a list of all eligible patients (based on age and having a CHD-related ICD-9-CM diagnosis code in their healthcare record) who had scheduled appointments at any of the statewide clinics during the project period (September 2017 through July 2018). Parents or guardians of adolescent patients, hereafter referred to as “parents,” were contacted via email and telephone to inquire about their interest in survey participation. If interested, he/she was emailed a link to the consent documents and survey. Survey data were collected and managed using Research Electronic Data Capture (REDCap), a web-based data capture tool [30].
In NY, adolescents with CHD meeting the inclusion criteria above and whose residence at birth was in one of eleven target NY counties (i.e., Allegany, Bronx, Cattaraugus, Chautauqua, Eire, Genesee, Monroe, Niagara, Orleans, Westchester, Wyoming) were identified using the Congenital Malformations Registry (CMR), a population-based registry of children born or residing in NY and diagnosed with a CHD before two years of age. To find adolescents with recent healthcare encounters, the identified cases from the CMR were linked to a database of 2011–2013 healthcare encounters developed for the NY Congenital Heart Defects Across the Lifespan project. Healthcare encounter data included inpatient and outpatient records in the Statewide Planning and Research Cooperative System (SPARCS), a comprehensive, integrated, all-payer data reporting system, Medicaid claims data, and cardiology clinical records. Updated mailing addresses for this adolescent cohort were identified using the New York State Immunization Information System (NYSIIS), a statewide immunization information system which maintains real-time, computerized immunization medical record data of persons of all ages, LexisNexis® Accurint®, a computer-assisted, data-linking locate-and-research software tool, and www.ReferenceUSAGov.com, an Internet-based reference service from the Government Division of Infogroup™. Parents for whom updated residential address information could be identified were sent survey materials. Individuals whose updated residential address was outside of New York state were excluded.
The survey was approved by the institutional review boards of Emory University (EU) in Atlanta, GA and New York State Department of Health (NYSDOH). The U.S. Office of Management and Budget (OMB) approved data collection activities. Survey respondents received a $10 gift card upon receipt of the completed survey.
Survey Measures
The parent-reported survey included questions on the adolescent’s recent healthcare utilization, HRQoL, perceptions and concerns about transitioning health care from a pediatric to an adult specialty cardiac provider, and education and resource preferences for learning about transition-related information (Table 1). Appendix 1 contains the survey instrument.
Table 1.
Components of survey assessing healthcare perceptions of transition among parents of adolescents with congenital heart defects in two sites, Georgia and New York
| Survey component | Measured By |
|---|---|
| Patient (adolescent) demographics | Parental educational attainment Adolescent’s age Adolescent’s grade in school Health insurance status (current) Race Hispanic/Latino ethnicity Adolescent’s sex |
| Health care utilization | When child last saw any provider When child last saw pediatric cardiologist Location of interaction with pediatric cardiologist Inability to meet need for interaction with provider |
| Quality of life | Pediatric Quality of Life Inventory ™ (PedsQL™) (cardiac module) covering: Disease impact Psychosocial impact |
| Transition perceptions | Perceptions of needed care in adulthood Perceptions of provider for adult specialty cardiac care Expected age for adolescent to transfer to adult provider Perceived barriers for transition to adult provider |
Demographics
Parents reported information about their own (parental) educational attainment, as well as their adolescent’s age, grade in school, health insurance status, race, ethnicity and sex.
Health Care Utilization
Parents reported when their adolescent was last seen by any healthcare provider and by a pediatric cardiologist, as well as the location of these visits and whether they had attempted or wanted any interaction with the health care system in the past three months.
Health-Related Quality of Life (HRQoL)
HRQoL was measured by the adolescent version of the Pediatric Cardiac Quality of Life Inventory (PCQLI), a disease-specific HRQoL instrument validated for parent reporting for adolescents (13–18 years of age) with congenital or acquired heart disease [31, 32]. The PCQLI is derived directly from concerns generated by patients, parent/guardians, and cardiac medical providers [33]. The PCQLI inventory begins with one general health perception question, “In general, would you say your child’s health is…” with response options ranging from 1 (excellent) to 5 (poor) on a Likert scale. Responses to this question are not included in the scale scoring but used as an overall measure of parental perception of their child’s quality of life. For analysis, this variable was dichotomized into the categories “Lower HRQoL” if the parent reported a 4 or 5 and “Higher HRQoL” if the parent reported a 1, 2 or 3. We analyzed 29 items belonging to two subscales: (1) the Disease Impact Subscale (17 items), measuring physical functioning; and (2) the Psychosocial Impact Subscale (12 items), measuring psychological and social functioning. HRQoL was measured with the Disease Impact and Psychosocial Impact subscales, as well as the PCQLI Total Score.
Disease Impact and Psychosocial Impact subscale scores were calculated individually using the following formula:
PCQLI Total Score was calculated by adding the two subscale scores which sums to a maximum of 100 points. Per the PCQLI guidance document, for individuals missing ≤ 2 items on a PCQLI subscale, the mean of that subscale was substituted for each missing response. Individuals missing ≥ 3 items on a subscale were excluded from analysis and a total score was not calculated [34].
Transition Perceptions
To better understand perceptions of the transition process from pediatric to adult specialty cardiac care, parents were asked: (1) whether they had been told by a healthcare professional that their child would continue to need cardiac care into adulthood; (2) what type of physician (cardiologist, primary care physician, don’t know) they expected would provide adult cardiac care; (3) if a cardiologist was selected, what type of cardiologist would likely provide adult cardiac care to their child (adult congenital heart disease specialist, pediatric cardiologist, general adult cardiologist, don’t know); and (4) at what age did the parent expect their child to transfer from pediatric to adult cardiac health care. Parents were also asked whether they had seven specific concerns about the transition process (e.g., replacing relationship with pediatric provider, accessing adult health insurance).
Analysis
All datasets were cleaned and checked for systematic biases of missing data in the PCQLI scale. Prior to mean substitution for the PCQLI, demographic characteristics and CHD severity of participants with no missing data on the scales and those with missing data on scales were compared using chi-square tests. Respondents with missing data on demographic characteristics or other survey variables were excluded from analyses where those variables were required.
Descriptive statistics for all respondents, including chi-square statistics for comparing demographic characteristics and CHD severity across and by the two sites, were generated. Response rates in GA were calculated as the number of completed surveys divided by the number of parents contacted for survey participation. Response rates in NY were calculated as the number of completed surveys divided by the number of parents mailed a survey, excluding parents whose surveys were returned as undeliverable. A stepwise logistic regression model with interaction terms between insurance status and project site (state) and between race and state was conducted to determine whether demographic characteristics predicted HRQoL. In addition, perceptions of the transition process from pediatric to adult specialty cardiac care were examined.
Results
A total of 451 surveys were completed, with response rates of 47.1% (GA) and 37.5% (NY). No statistically significant demographic differences were identified when individuals with and without missing data were compared, suggesting that data were missing at random. In GA, we were unable to assess whether respondents differed significantly from non-respondents due to restricted access to the demographic information of non-respondents. In NY, there were no statistically significant differences between respondents and non-respondents by adolescent CHD severity or age. However, non-respondents were more likely to be parents of black and Hispanic adolescents (P < 0.0001). Demographic and health characteristics of participants also varied by site. Percentages of adolescents in GA who were male, 11–12 years of age, non-Hispanic, uninsured, had a non-severe CHD, had received any healthcare in the past 6 months, and had received care from a cardiologist within the past 6 months were over 5 percentage points higher than among those in NY (Table 2). Of note, because parent/adolescent dyads recruited from Georgia necessarily had recent contact with the healthcare system, higher reports of having received care among GA patients is not unexpected.
Table 2.
Frequencies and percentages of parent-reported demographic characteristics of adolescents with congenital heart defects (CHD) overall and by site, Georgia and New York
| Combined (N = 451) | Georgia (GA) n = 274 (60.7%) |
New York (NY) n = 177 (39.3%) |
P value | |
|---|---|---|---|---|
| Adolescent characteristics | ||||
| Sex | 0.0640 | |||
| Male | 248 (55.1) | 160 (58.6) | 88 (49.7) | |
| Female | 202 (44.9) | 113 (41.4) | 89 (50.3) | |
| Missing | 1 | 1 | 0 | |
| Race | 0.4102 | |||
| White | 316 (72.8) | 185 (70.9) | 131 (75.7) | |
| Black | 81 (18.7) | 54 (20.7) | 27 (15.6) | |
| Other/mixed race | 37 (8.5) | 22 (8.4) | 15 (8.7) | |
| Missing | 17 | 13 | 4 | |
| Ethnicity | 0.0445 | |||
| Not Hispanic | 407 (92.3) | 251 (94.4) | 156 (89.1) | |
| Hispanic | 34 (7.7) | 15 (5.6) | 19 (10.9) | |
| Missing | 10 | 8 | 2 | |
| Age (years) | 0.1046 | |||
| 11–12 | 59 (13.1) | 43 (15.7) | 16 (9.0) | |
| 13–14 | 130 (28.8) | 74 (27.0) | 56 (31.6) | |
| 15–19 | 262 (58.1) | 157 (57.3) | 105 (59.3) | |
| CHD severity | 0.1161 | |||
| Non-severe | 255 (56.5) | 163 (59.5) | 92 (52.0) | |
| Severe | 196 (43.5) | 111 (40.5) | 85 (48.0) | |
| Insurance | 0.0070 | |||
| Private only | 214 (49.4) | 134 (49.1) | 80 (50.0) | |
| Any public | 203 (46.9) | 123 (45.1) | 80 (50.0) | |
| Selfpay/uninsured | 16 (3.7) | 16 (5.9) | 0 (0.0) | |
| Missing | 18 | 1 | 17 | |
| Last saw health care provider | 0.0616 | |||
| Within past 6 months | 384 (86.7) | 244 (89.1) | 140 (82.8) | |
| > 6 months ago | 59 (13.3) | 30 (10.9) | 29 (17.2) | |
| Missing | 8 | 0 | 8 | |
| Last saw cardiologist | < 0.0001 | |||
| Within past 6 months | 274 (61.7) | 200 (73.3) | 74 (43.3) | |
| > 6 months ago | 170 (38.3) | 73 (26.7) | 97 (56.7) | |
| Missing | 7 | 1 | 6 | |
| Parent characteristic | ||||
| Education | 0.6344 | |||
| High school or less | 85 (19.0) | 49 (17.9) | 36 (20.9) | |
| Some college/assoc./trade | 147 (33.0) | 94 (34.3) | 53 (30.8) | |
| College or higher | 214 (48.0) | 131 (47.8) | 83 (48.3) | |
| Missing | 5 | 0 | 5 |
Sample includes consented parents of adolescents with a congenital heart defect between ages 11 and 19 years. P values for X2 comparison between the two study sites and do not include missing data; bolded P values are significant. All measures are for adolescents, except parental education
Among parents who responded to the first question of the PCQLI regarding their perception of their child’s general health (n = 407), 90.7% reported that their adolescent with CHD had an excellent, very good, or a good HRQoL (Fig. 1). This finding did not differ significantly by site (data not shown).
Fig. 1. Parent-reported health-related quality of life of adolescents with congenital heart defects across Sites, Georgia and New York (n = 407*).
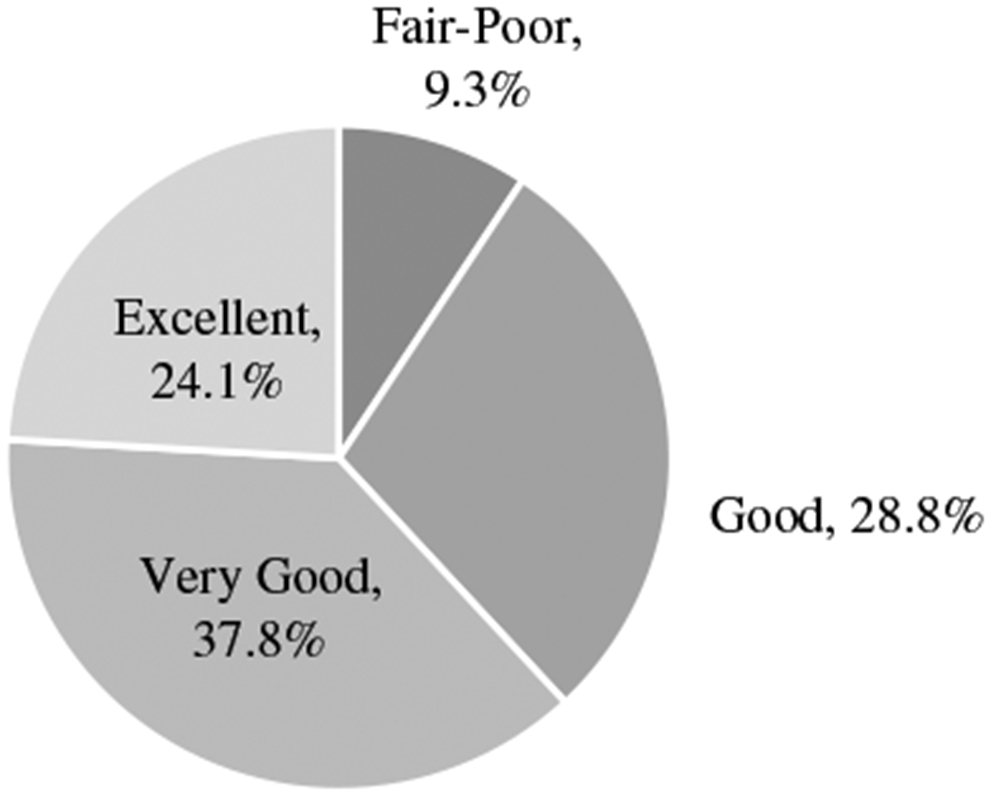
* Information was not provided by n=44 survey respondents
Eleven adolescents (GA = 1; NY = 10) were missing information needed to calculate PCQLI Disease Impact and Psychosocial Impact Subscale Scores. An additional adolescent from NY was missing information needed for the Disease Impact Subscale Score only. PCQLI Total Scores were calculated only for those respondents with both subscale scores (n = 439). Table 3 shows mean PCQLI Total Scores (out of 100 points) for demographic characteristics both across and by study site. PCQLI subscale data are reported, but not shown. Adolescents with non-severe CHD compared to those with a severe CHD had significantly better parent-reported HRQoL overall and in terms of Disease Impact and Psychosocial Impact. Similarly, those who had last seen a cardiologist more than 6 months prior had higher parent-reported subscale and Total HRQoL scores compared with those who had seen a cardiologist within 6 months. Distributions on both PCQLI subscale scores and the Total PCQLI Score differed between parents who earned a college degree or higher and those with some college/trade education or high school or less, respectively [for Disease Impact PCQLI subscale: 37.12 vs. 34.29 and 34.03, P = 0.01; for Psychosocial Impact PCQLI subscale: 39.99 vs. 37.71 and 36.31, P = 0.005; for Total PCQLI Score: 77.11 vs. 72.01 and 70.67, P = 0.007]. Similarly, PCQLI distributions differed between parents whose teens were covered by private insurance only as well as those who were self-pay/uninsured and those whose teens were covered by any public insurance on both PCQLI subscale scores and the Total PCQLI Score, respectively [for Disease Impact PCQLI subscale: (37.56 and 37.21 vs. 33.00, P < 0.0001; for Psychosocial Impact PCQLI subscale: 40.01 and 39.18 vs. 36.52, P = 0.0009; for Total PCQLI Score: 77.58 and 76.39 vs. 69.67, P < 0.0001].
Table 3.
Parent-reported health-related quality of life total score for adolescents with congenital heart defects (CHD) across site (combined) and by site, Georgia and New York
| Combined (N = 439) Mean (SD) |
P value | Georgia (GA) (n = 273) Mean (SD) |
P value | New York (NY) (n = 166) Mean (SD) |
P value | |
|---|---|---|---|---|---|---|
| Severity | 0.0001 | 0.0018 | 0.0077 | |||
| Not severe | 77.12 (19.17) | 74.92 (19.54) | 81.19 (17.88) | |||
| Severe | 70.21 (17.58) | 67.58 (17.78) | 73.92 (16.71) | |||
| Parent’s education | 0.0071 | 0.0473 | 0.1624 | |||
| HS or less | 70.67 (19.28) | 67.91 (18.82) | 74.75 (19.50) | |||
| Some college/trade | 72.01 (18.09) | 70.07 (18.53) | 75.87 (16.72) | |||
| College or higher | 77.11 (18.83) | 74.86 (19.42) | 80.67 (17.37) | |||
| Insurance | < 0.0001 | 0.0039 | 0.0026 | |||
| Private only | 77.58 (17.38) | 75.24 (18.11) | 81.59 (15.33) | |||
| Any public | 69.67 (19.21) | 67.65 (19.11) | 73.01 (19.04) | |||
| SelfPay/uninsured | 76.39 (22.40) | 76.39 (22.40) | – | |||
| Last saw cardiologist | 0.0004 | 0.0504 | 0.0797 | |||
| Within past 6 months | 71.75 (19.17) | 70.49 (19.57) | 75.44 (17.56) | |||
| > 6 months | 78.28 (17.64) | 75.60 (17.39) | 80.40 (17.63) |
Sample incl. consented parents of children & adolescents with a congenital heart defect between ages 11 and 19 years
P values for t-test analysis (mean differences between 2 groups) and ANOVA analysis (mean differences among > 2 groups); bolded P values are significant
Among the combined sample in the logistic regression model, none of the proposed demographic risk factors (age, sex, race, CHD severity, insurance coverage) were significantly associated with reported HRQoL.
Issues of Transition and Transfer of Care
For the combined sample, 77.8% of parents of adolescents with CHD reported being told by a provider that their adolescent would need cardiac care into adulthood (Table 4). When asked about the expected age of transfer from pediatric to adult health care for their adolescents with CHD, 95.9% of parents reported expected age of transfer to be 18 years or older. Almost 86% of parents reported a cardiologist would provide adult cardiac care to their adolescent once they transitioned, with 60.8% reporting the cardiologist would be an adult congenital CHD specialist, while 11.0% of did not know who would provide adult health care to their child. However, a significantly higher proportion of GA case parents reported that they expected to be cared for by an adult congenital cardiologist (65.3% for GA vs 52.9% for NY), while a higher proportion of NY case parents reported pediatric cardiologist (14.0% for NY vs 5.9% for GA) or don’t know (14.7% for NY vs 8.9% for GA).
Table 4.
Transition perceptions reported by parents of adolescents with congenital heart defects (CHD) combined across sites, Georgia and New York
| Transition questions | Combined N (%) | Georgia (GA) n (%) | New York (NY) n (%) | P value |
|---|---|---|---|---|
| Told by a provider your child will continue to need cardiac care into adulthood? | 0.0521 | |||
| Yes | 348 (77.8) | 220 (80.6) | 128 (73.6) | |
| No | 45 (10.1) | 20 (7.3) | 25 (14.4) | |
| Unsure | 54 (12.1) | 33 (12.1) | 21 (12.1) | |
| Missing | 4 | 1 | 3 | |
| Who will provide heart care in adulthood? | 0.0246 | |||
| Cardiologist | 376 (85.8) | 239 (88.9) | 137 (81.1) | |
| Primary care physician | 20 (4.6) | 7 (2.6) | 13 (7.7) | |
| Don’t know | 42 (9.6) | 23 (8.6) | 19 (11.2) | |
| Missing | 13 | 5 | 8 | |
| What type of cardiologist will provide care in adulthood? | 0.0108 | |||
| Adult congenital cardiologist | 226 (60.8) | 154 (65.3) | 72 (52.9) | |
| Pediatric cardiologist | 33 (8.9) | 14 (5.9) | 19 (14.0) | |
| General adult cardiologist | 72 (19.4) | 47 (19.9) | 25 (18.4) | |
| Don’t know | 41 (11.0) | 21 (8.9) | 20 (14.7) | |
| Missing | 4 | 3 | 1 | |
| Age of expected transition | 0.0473 | |||
| < 18 years | 16 (4.1) | 9 (3.8) | 7 (4.6) | |
| 18–20 years | 234 (60.0) | 155 (64.9) | 79 (52.3) | |
| ≥ 21 + years | 140 (35.9) | 75 (31.4) | 65 (43.1) | |
| Missing | 61 | 35 | 26 | |
| Parents reporting at least one transition-related concern | 0.2601 | |||
| Yes | 391 (91.6) | 254 (92.7) | 137 (89.5) | |
| No | 36 (8.4) | 20 (7.3) | 16 (10.5) | |
| Missing | 24 | 0 | 24 | |
| Potential Concerns of Transitioning to Adult Care* | ||||
| Replacing the strong relationship with the existing provider/team | 259 (60.7) | 163 (59.5) | 96 (62.8) | 0.5090 |
| Difficulty finding an appropriate adult health care provider | 208 (48.7) | 145 (52.9) | 63 (41.2) | 0.0199 |
| Difficulty accessing health insurance as an adult | 186 (43.6) | 142 (51.8) | 44 (28.8) | < 0.0001 |
| Adult providers not understanding your child’s medical condition | 154 (36.1) | 102 (37.2) | 52 (34.0) | 0.5039 |
| Child’s anxiety about a new provider | 144 (33.7) | 104 (38.0) | 40 (26.1) | 0.0133 |
| Insurance issues due to switching to new health care provider | 131 (30.7) | 100 (36.5) | 31 (20.3) | 0.0005 |
| Geographic distance to an adult health care provider | 78 (18.3) | 56 (20.4) | 22 (14.4) | 0.1203 |
Bolded P values are significant
Approximately 92% of respondents reported at least one concern related to transition for their child. The top three concerns related to transition across both sites were issues of replacing the strong existing relationship between the patient and their pediatric health care provider (60.7%), difficulty finding an appropriate health care provider (48.7%), and difficulty accessing health insurance for their adolescent once they become an adult (43.6%). Notably, a much higher proportion of GA case parents reported concerns with their child accessing health insurance as an adult (51.8% of parents for GA vs 28.8% of parents for NY).
Discussion
These findings reflect the current status of an in-care patient population of adolescents with CHD in two states and demonstrate that among those already in the health care system, the majority reported high HRQoL in both states, but with means consistently higher in NY than in GA. Despite overall high parent-reported HRQoL for this adolescent patient population, there remains parental concern and uncertainty about the transition from pediatric to adult cardiac care. While the majority of parents reported awareness of the need to transition their adolescent from pediatric to adolescent health care, more than 1 in 5 did not, and 14% of parents expected their adolescent to be cared for by a primary care physician or did not know who would provide their child’s health care as an adult. Guidance from the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines suggests that ACHD patients should be managed by specialists with expertise in CHD/ACHD [4]. The phrasing of the survey question did not ask “who should provide care?” but rather asked, “who will provide care?” Given the possibility of limited access to adult congenital cardiologists, parental responses may reflect either lack of knowledge or a realistic expectation, and this difference cannot be determined using data from this survey. There were also differences by study site, which may be reflective of the different sampling strategies; GA participants were recruited from their care locations making it reasonable to hypothesize that they have been privy to more discussions about transition with their providers.
Further, parental respondents conveyed concerns about several aspects of obtaining adult health care for their children with CHD, ranging from replacing the strong long-term relationship most pediatric CHD patients have with their doctor, having seen him/her since birth, to health care access issues. Of particular note, nearly 50% of respondents noted concerns about accessing appropriate ACHD providers, with the problem seemingly larger in GA than in NY; this issue is supported by the literature, which demonstrates that geographic proximity to ACHD providers is a key driver of successful transition [35] as well as the realities of the healthcare systems in the two states, where GA has only one adult congenital heart clinic in metro-Atlanta and NY has six self-identified clinics throughout the state [36]. While changes to the health care system over the last decade, which disallowed increasing insurance premiums based on pre-existing conditions, may have mitigated some insurance access issues [37], this remains a concern for nearly one-half of parents in our survey and suggests a need for further education and, perhaps, support for accessing insurance. Again, state health system differences may partially explain why this is perceived as a bigger problem for parents in GA. Whereas NY expanded Medicaid on the Affordable Care Act, GA did not, and many young adults may age out of Medicaid or the Children’s Health Insurance Program (CHIP) in GA, losing their insurance coverage.
Overall, the survey findings suggest that health care providers are reaching most parents of children with CHD with information regarding transition; however, a substantial percentage are not receiving or recalling information on transition and areas of concern, both with regards to patient/parental education and healthcare access. This analysis is limited only to demographic information of adolescents with CHD identified through healthcare encounters. In GA, participants were identified directly from a cardiology clinic where they had scheduled a recent appointment; in NY, participants were identified as having a health care encounter at least once in the 3 to 6 years before survey completion. There may be more barriers to care, and lower reported HRQoL in the general population of adolescents with CHD not receiving health care. While out of care populations are particularly hard to reach for survey purposes, information on this population is needed. As adolescents age, they are increasingly likely to drop out of health care, with anywhere from 21 to 76% lost to follow-up care at the time of transition [14, 38-40]. Although the majority of parents in our survey reported that a provider had discussed with them that their adolescent would need to transition to adult cardiac care, less than half of the parents of adolescents with CHD in a recent national survey reported having any transition discussions with health care providers [41]. This difference may be attributed to surveying parents of adolescents with CHD, the large majority with recent healthcare encounters, versus targeting parents of adolescents with CHD regardless of healthcare utilization for the national survey. However, it is concerning that nearly a quarter of parents of adolescents with health care utilization in our survey reported that they had not or were not sure they had discussed transition with a provider.
An additional limitation is that survey responses were parent-reported, rather than reported by the adolescent. Previous work suggests differences in parental and adolescent perceptions of transition and HRQoL [19, 41]. Nonetheless, whereas HRQoL for adolescents with CHD has been examined previously [31, 32, 41-43], to our knowledge this is the first survey to combine comprehensive information about HRQoL for adolescents with CHD, combined with information about transition perceptions and concerns. Based on these findings, considerations for improving the transition from adolescent to adult care could include: (1) helping adolescents and their families identify adult providers earlier in the transition process; (2) allowing adolescents/parents to focus on building/strengthening relationships with adult providers; and (3) addressing access issues with adult providers, including insurance coverage and geographic proximity. Having resources available to help families learn about options early in the transition process, before transfer to adult health care occurs, may allow families to plan and make decisions that facilitate continuation of appropriate health care for adolescents and young adults with CHD. The preliminary findings from this study suggest that adolescents with CHD who have been connected to the health system demonstrate a relatively high quality of life but continue to face concerns about transition. Whereas state health system factors are not easily malleable, these study findings may inform health care providers and clinics treating adolescents with CHD, and public health systems on ways to continue to improve the transition process to adult health care.
Supplementary Material
Funding
Centers for Disease Control and Prevention (CDC), Grant/Award Number: CDC-RFA-DD15-1506.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Electronic supplementary material The online version of this. article (https://doi.org/10.1007/s00246-020-02378-z) contains. supplementary material, which is available to authorized users.
Code Availability
Analysis was carried out using Statistical Analysis Software (SAS) 9.4. All codes are available upon request.
DCDD Replication Statement
This analysis has undergone replication by Olushola Fapo.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Ethics Approval The survey was approved by the institutional review boards of Emory University (EU) in Atlanta, GA and New York State Department of Health (NYSDOH). The U.S. Office of Management and Budget (OMB) approved data collection activities. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Conflict of interest The authors declare that they have no conflicts of interest.
Data Availability
Patient data are protected and not publicly available. Surveys and methods may be shared publicly.
References
- 1.Moons P, Bovijn L, Budts W, Belmans A, Gewillig M (2010) Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation 122(22):2264–2272 [DOI] [PubMed] [Google Scholar]
- 2.Gilboa SM, Devine OJ, Kucik JE, Oster ME, Riehle-Colarusso T, Nembhard WN, Xu P, Correa A, Jenkins K, Marelli AJ (2016) Congenital heart defects in the United States: estimating the magnitude of the affected population in 2010. Circulation 134(2):101–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, Del Nido P, Fasules JW, Graham TP Jr, Hijazi ZM, Hunt SA, King ME, Landzberg MJ, Miner PD, Radford MJ, Walsh EP, Webb GD (2008) ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 52(23):e143–e263 [DOI] [PubMed] [Google Scholar]
- 4.Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, Crumb SR, Dearani JA, Fuller S, Gurvitz M, Khairy P, Landzberg MJ, Saidi A, Valente AM, Van Hare GF (2019) 2018 AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 139:e698–e800 [DOI] [PubMed] [Google Scholar]
- 5.Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L (2007) Congenital heart disease in the general population: changing prevalence and age distribution. Circulation 115(2):163–172. 10.1161/CIRCULATIONAHA.106.627224 [DOI] [PubMed] [Google Scholar]
- 6.Blum RW, Garell D, Hodgman CM, Jorissen TW, Okinow NA, Orr DP, Slap GB (1993) Transition from child-centered to adult health-care systems for adolescents with chronic conditions. J Adolesc Health 14:570–576 [DOI] [PubMed] [Google Scholar]
- 7.Sable C, Foster E, Uzark K, Bjornsen K, Canobbio MM, Connolly HM, Graham TP, Gurvitz MZ, Kovacs A, Meadows AK, Reid GJ, Reiss JG, Rosenbaum KN, Sagerman PJ, Saidi A, Schonberg R, Shah S, Tong E, Williams RG et al. (2011) Best practices in managing transition to adulthood for adolescents with congenital heart disease: the transition process and medical and psychosocial issues: a scientific statement from the American Heart Association. Circulation 123(13):1454–1485. 10.1161/CIR.0b013e3182107c56 [DOI] [PubMed] [Google Scholar]
- 8.Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM (2003) Transition to adult health care for adolescents and young adults with chronic conditions. J Adolesc Health 33(4):309–311 [DOI] [PubMed] [Google Scholar]
- 9.Warnes CA, Liberthson R, Danielson GK, Dore A, Harris L, Hoffman JIE, Somerville J, Williams RG, Webb GD (2001) Task Force 1: The changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 10.1016/S0735-1097(01)01272-4 [DOI] [PubMed] [Google Scholar]
- 10.Everitt IK, Gerardin JF, Rodriguez FH 3rd, Book WM (2017) Improving the quality of transition and transfer of care in young adults with congenital heart disease. Congenit Heart Dis 12(3):242–250. 10.1111/chd.12463 [DOI] [PubMed] [Google Scholar]
- 11.Deanfield J, Thaulow E, Warnes C, Webb G, Kolbel F, Hoffman A, Sorenson K, Kaemmer H, Thilen U, Bink-Boelkens M, Iserin L, Daliento L, Silove E, Redington A, Vouhe P, Priori S, Alonso MA, Blanc JJ, Budaj A, Cowie M, Deckers J, Fernandez Burgos E, Lekakis J, Lindahl B, Mazzotta G, Morais J, Oto A, Smiseth O, Trappe HJ, Klein W, Blomstrom-Lundqvist C, de Backer G, Hradec J, Mazzotta G, Parkhomenko A, Presbitero P, Torbicki A et al. (2003) Management of grown up congenital heart disease. Eur Heart J 24(11):1035–1084. 10.1016/s0195-668x(03)00131-3 [DOI] [PubMed] [Google Scholar]
- 12.American Academy of P, American Academy of Family P, American College of P, Transitions Clinical Report Authoring G, Cooley WC, Sagerman PJ (2011) Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 128(1):182–200. 10.1542/peds.2011-0969 [DOI] [PubMed] [Google Scholar]
- 13.Reid GJ, Irvine MJ, McCrindle BW, Sananes R, Ritvo PG, Siu SC, Webb GD (2004) Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics 113(3 Pt 1):e197–205 [DOI] [PubMed] [Google Scholar]
- 14.Mackie A, Ionescu-Ittu R, Therrien J, Pilote L, Abrahamowicz M, Marielli A (2009) Children and adults with congenital heart disease lost to follow up: who and when? Circulation 120(4):302–309 [DOI] [PubMed] [Google Scholar]
- 15.Gurvitz M, Valente AM, Broberg C, Cook S, Stout K, Kay J, Ting J, Kuehl K, Earing M, Webb G, Houser L, Opotowsky A, Harmon A, Graham D, Khairy P, Gianola A, Verstappen A, Landzberg M et al. (2013) Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (The Health, Education, and Access Research Trial). J Am Coll Cardiol 61(21):2180–2184. 10.1016/j.jacc.2013.02.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yeung E, Kay J, Roosevelt GE, Brandon M, Yetman AT (2008) Lapse of care as a predictor for morbidity in adults with congenital heart disease. Int J Cardiol 125(1):62–65. 10.1016/j.ijcard.2007.02.023 [DOI] [PubMed] [Google Scholar]
- 17.Moons P, Hilderson D, Van Deyk K (2008) Implementation of transition programs can prevent another lost generation of patients with congenital heart disease. Eur J Cardiovasc Nurs 7(4):259–263. 10.1016/j.ejcnurse.2008.10.001 [DOI] [PubMed] [Google Scholar]
- 18.Bohun CM, Woods P, Winter C, Mitchell J, McLarry J, Weiss J, Broberg CS (2016) Challenges of intra-institutional transfer of care from paediatric to adult congenital cardiology: the need for retention as well as transition. Cardiol Young 26(2):327–333. 10.1017/S1047951115000220 [DOI] [PubMed] [Google Scholar]
- 19.Fernandes SM, O’Sullivan-Oliveira J, Landzberg MJ, Khairy P, Melvin P, Sawicki GS, Ziniel S, Kenney LB, Garvey KC, Sobota A, O’Brien R, Nigrovic PA, Sharma N, Fishman LN (2014) Transition and transfer of adolescents and young adults with pediatric onset chronic disease: the patient and parent perspective. J Pediatr Rehabil Med 7(1):43–51. 10.3233/PRM-140269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fernandes SM, Khairy P, Fishman L, Melvin P, O’Sullivan-Olivereira J, Sawicki GS, Ziniel S, Breitinger P, Williams R, Takahashi M, Landzberg MJ (2012) Referral patterns and perceived barriers to adult congenital heart disease care: results of a survey of U.S. pediatric cardiologists. J Am Coll Cardiol 60(23):2411–2418 [DOI] [PubMed] [Google Scholar]
- 21.Kirk S (2008) Transitions in the lives of young people with complex healthcare needs. Child Care Health Dev 34(5):567–575 [DOI] [PubMed] [Google Scholar]
- 22.Woodward JF, Swigonski NL, Ciccarelli MR (2012) Assessing the health, functional characteristics, and health needs of youth attending a noncategorical transition support program. J Adolesc Health 51(3):272–278 [DOI] [PubMed] [Google Scholar]
- 23.Marelli A, Miller SP, Marino BS, Jefferson AL, Newburger JW (2016) Brain in congenital heart disease across the lifespan: the cumulative burden of injury. Circulation 133(20):1951–1962. 10.1161/CIRCULATIONAHA.115.019881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sanz JH, Wang J, Berl MM, Armour AC, Cheng YI, Donofrio MT (2018) Executive function and psychosocial quality of life in school age children with congenital heart disease. J Pediatr 202:63–69. 10.1016/j.jpeds.2018.07.018 [DOI] [PubMed] [Google Scholar]
- 25.Clarizia NA, Chahal N, Manlhiot C, Kilburn J, Redington AN, McCrindle BW (2009) Transition to adult health care for adolescents and young adults with congenital heart disease: perspectives of the patient, parent and health care provider. Can J Cardiol 25(9):S317–S322. 10.1016/S0828-282X(09)70145-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Knauth A, Verstappen A, Reiss J, Webb GD (2006) Transition and transfer from pediatric to adult care of the young adult with complex congenital heart disease. Cardiol Clin 24(4):619–629. 10.1016/j.ccl.2006.08.010 [DOI] [PubMed] [Google Scholar]
- 27.Higgins SS, Tong E (2003) Transitioning adolescents with congenital heart disease into adult health care. Prog Cardiovasc Nurs 18(2):93–98 [DOI] [PubMed] [Google Scholar]
- 28.Betz CL (1998) Adolescent transitions: a nursing concern. Pediatr Nurs 24(1):23–28 [PubMed] [Google Scholar]
- 29.Glidewell J, Book W, Raskind-Hood C, Hogue C, Dunn J, Gurvitz M, Ozonoff A, McGarry C, Van Zutphen A, Lui G, Downing K, Riehle-Colarusso T (2018) Population-based surveillance of congenital heart defects among adolescents and adults: surveillance methodology. Birth Defects Res 110(19):1395–1403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J (2009) Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Uzark K, Jones K, Limbers CA, Burwinkle TM, Varni JW (2008) Quality of life in children with heart disease as perceived by children and parents. Pediatrics 121(5):2006–3778 [DOI] [PubMed] [Google Scholar]
- 32.Marino BS, Shera D, Wernovsky G, Tomilson R, Aguirre A, Gallagher M, Lee A, Cho C, Stern W, Davis L, Tong E, Teitel D, Mussatto K, Ghanayem N, Gleason M, Gaynor J, Wray J, Helfaer M, Shea J (2008) The development of the pediatric cardiac quality of life inventory: a quality of life measure for children and adolescents with heart disease. Qual Life Res 17(4):613–626 [DOI] [PubMed] [Google Scholar]
- 33.Marino BS, Tomlinson RS, Wernovsky G, Drotar D, Newburger JW, Mahony L, Mussatto K, Tong E, Cohen M, Andersen C, Shera D, Khoury P, Wray J, Gaynor WJ, Helfaer MA, Kazak AE, Shea JA (2010) Validation of the pediatric cardiac quality of life inventory. Pediatrics 126:498–508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marino BS, Cassedy A, Drotar DD. The Pediatric Cardiac Quality of Life Inventory (PCQLI): a brief user’s guide. Ann & Robert H. Lurie Children’s Hospital; of Chicago, IL [Google Scholar]
- 35.Gerardin J, Raskind-Hood C, Rodriguez F, Hoffman T, Kalogeropoulos A, Hogue C, Book W (2019) Lost in the system? Transfer to adult congenital heart disease care: challenges and solutions. Congenit Heart Dis 14(4):541–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adult Congenital Heart Association (2020) ACHD Clinic Directory. https://www.achaheart.org/your-heart/clinic-directory/clinic-listings/. Accessed 23 Apr 2020
- 37.Lin C, Novak E, Rich M, Billadello J (2018) Insurance access in adults with congenital heart disease in the Affordable Care Act era. Congenit Heart Dis 13(3):384–391 [DOI] [PubMed] [Google Scholar]
- 38.Reid GJ, Irvine MJ, McCrindle BW, Sananes R, Ritvo P, Siu S, Webb G (2004) Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics 113(3):197–205 [DOI] [PubMed] [Google Scholar]
- 39.Gurvitz M, Valente A, Broberg C, Cook S, Stout K, Kay J, Ting J, Kuehl K, Earing M, Webb G, Houser L, Opotowsky A, Harmon A, Graham D, Khairy P, Gianola A, Verstappen A, Landsberg M et al. (2013) Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (The Health, Education, and Access Research Trial). J Am Coll Cardiol 61(21):2180–2184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Downing KF, Oster ME, Farr SL (2017) Preparing adolescents with heart problems for transition to adult care, 2009–2010 National Survey of Children with Special Health Care Needs. Congenit Heart Dis 12(4):497–506. 10.1111/chd.12476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ruggiero KM, Hickey PA, Leger RR, Vessey JA, Hayman LL (2018) Parental perceptions of disease-severity and health-related quality of life in school-age children with congenital heart disease. J Spec Pediatr Nurs. 10.1111/jspn.12204 [DOI] [PubMed] [Google Scholar]
- 42.Mozlon ES, Mullins LL, Cushing CC, Chaney JM, McNall R, Mayes S (2018) The relationship between barriers to care, caregiver distress, and child health-related quality of life in caregivers of children with cancer: a structural equation modeling approach. Child Health Care 47(1):1–15 [Google Scholar]
- 43.Uzark K, Jones K, Burwinkle TM, Varni JW (2003) The Pediatric Quality of Life Inventory™ in children with heart disease. Prog Pediatr Cardiol 18(2):141–148 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Patient data are protected and not publicly available. Surveys and methods may be shared publicly.


