Abstract
Background The Mexican programme Oportunidades/Progresa conditionally transfers money to beneficiary families. Over the past 10 years, poor rural women have been obliged to attend antenatal care (ANC) visits and reproductive health talks. We propose that the length of time in the programme influences women’s preferences, thus increasing their use not only of services directly linked to the cash transfers, but also of other services, such as clinic-based delivery, whose utilization is not obligatory.
Objective To analyse the long-term effect of Oportunidades on women’s use of antenatal and delivery care.
Methodology 5051 women aged between 15 and 49 years old with at least one child aged less than 24 months living in rural localities were analysed. Multilevel probit and logit models were used to analyse ANC visits and physician/nurse attended delivery, respectively. Models were adjusted with individual and socio-economic variables and the locality’s exposure time to Oportunidades.
Findings On average women living in localities with longer exposure to Oportunidades report 2.1% more ANC visits than women living in localities with less exposure. Young women aged 15–19 and 20–24 years and living in localities with longer exposure to Oportunidades (since 1998) have 88% and 41% greater likelihood of choosing a physician/nurse vs. traditional midwife for childbirth, respectively. Women of indigenous origin are 68.9% less likely to choose a physician/nurse for delivery care than non-indigenous women.
Conclusions An increase in the average number of ANC visits has been achieved among Oportunidades beneficiaries. An indirect effect is the increased selection of a physician/nurse for delivery care among young women living in localities with greater exposure time to Oportunidades. Disadvantaged women in Mexico (indigenous women) continue to have less access to skilled delivery care. Developing countries must develop strategies to increase access and use of skilled obstetric care for marginalized women.
Keywords: Conditional cash transfer, delivery care, prenatal care, utilization, poor women, Mexico
KEY MESSAGES.
The study findings support the concept of a learning effect that impacts Oportunidades beneficiaries’ reproductive health behaviour and decisions, with an increase in use of antenatal services through the provision of economic incentives in the long term.
The most disadvantaged women (indigenous, illiterate, living in the most deprived areas) continue to have less access to skilled care for delivery.
Developing countries must develop strategies to bring culturally appropriate and effective delivery care interventions to marginalized communities in order to reduce maternal mortality rates.
Introduction
The maternal mortality rate in Mexico has shown a downward trend from the 1970s through to the mid-1990s. Although this achievement was accompanied by a reduction in the gap in mortality rates between rural and urban areas, a difference persists. The risk of dying from maternal causes in the period from 1979 to 1981 was 4.5 times higher in women living in rural areas (less than 2500 inhabitants) compared with those in urban areas (15 000 or more inhabitants); this difference declined to 1.4 times 20 years later (Mojarro et al. 2003). Considerations such as the under-utilization of formal health services (Davis-Tsu 1980), as well as the preference for traditional midwives, were associated with high mortality rates in poor rural areas in Mexico (Parra 1993). In response, public programmes were launched to improve access to maternal and reproductive health services in the late 1990s. The National Reproductive Health programme in 1995 and the Program for Expanding Coverage in 1997 were launched to improve access to basic health services in rural areas. And a Health, Nutrition and Education programme (known by its Spanish acronym Progresa/Oportunidades) was introduced in 1997 to tackle the high poverty rates, by using monetary transfers as incentives for increased use of basic health services and education for children and women. Oportunidades was targeted to the poorest 20% of the rural population in Mexico.
Every 2 months, this programme transfers money to beneficiary families, with the condition that family members comply with gender- and age-specific health, education and nutrition requirements that contribute to long-term poverty reduction (Rawlings 2004). The amount of the transfers depends on the demographic structure of the household. Two of the principal conditions for receiving cash transfers are primary and secondary school attendance for children, and the regular use of health services by pregnant/postpartum women and their children. Over the years, women beneficiaries have been exposed to reproductive health consultations and health talks (called platicas) that they were obliged to attend. Specific information about family planning, pregnancy, delivery and postpartum care are among many of the reproductive health topics that women were informed about during their consultations and talks.
In the short term, impact evaluation of the Oportunidades programme found that among benefiting women, the number of antenatal care (ANC) visits rose to recommended levels (five ANC visits) compared with women in the control group (Gertler 1999). There were also reductions in infant mortality rates attributed to this programme (Barham 2005; Barber and Gertler 2008). Other research has confirmed better access to specific recommended practices during ANC visits among Oportunidades’ beneficiares (Barber and Gertler 2009). However, there are recent findings that have underlined differences in the access to prenatal care between indigenous and non-indigenous women, with non-indigenous women in rural areas having greater access to prenatal care than indigenous women (Barber et al. 2007).
Taking into account that some women have benefited from the programme for nearly 10 years, during which reproductive-aged women have had regular access to care, counselling and reproductive health information, we test whether the length of time in the programme influences women’s preferences and decisions related to the use of other reproductive health services whose utilization is not linked to the cash transfers. Time in the programme could change preferences and decisions through at least two pathways. First, through information and education, women beneficiaries of Oportunidades are expected to attend health talks given by health staff where they receive information regarding preventive and healthy habits related to nutrition, reproductive health and chronic conditions, etc. Additionally, women are expected to attend the clinics regularly for preventive visits, where they presumably learn about more healthy behaviours. Second, because beneficiaries of Oportunidades have to attend the clinics in order to comply with the requirements of the programme, they inevitably have regular contact with the public health system. This constant contact with the health providers can change perceptions and prejudices that households have regarding the public health system. In rural Mexico it is not uncommon that households see the public system as a low quality alternative. Whenever they are able, many rural Mexicans seek private providers, even though the quality of care they receive from low-cost private providers is in most cases very poor. It is understandable that beneficiaries of Oportunidades may change these negative preconceptions over time and eventually begin to trust the public health system. In the case of indigenous families, this effect might include the gradual change of cultural barriers that prevent women from demanding health care. A combination of both of these pathways may be occurring.
In this paper, we refer to this change in preferences of women regarding health services, regardless of the pathway through which such change occurs, as a learning effect. We test whether women with greater exposure time to Oportunidades: (1) demand ANC visits above the levels required by Oportunidades, and (2) increase their demand for delivery care, which is not required by the programme. In either case, we hypothesize that a change of preferences among women can be attributed to the programme.
Methods
Data and variables
The data used in this study are from the 1998, 2003 and 2007 rounds of the Rural Evaluation Survey (Encuesta de Evaluación Rural, ENCEL-RURAL). These three surveys were designed to evaluate the rural Oportunidades programme. The surveys were carried out in 17 states where the programme operated. For the 1998 round, 24 077 households were surveyed; in 2003, 33 888 households were surveyed and in 2007, 43 893 households. The survey is of a panel design where all the households initially in the programme were followed. Originally, the sample was divided into treatment and control localities, but this experimental design was lost in 2000 when all the control localities were incorporated into the programme. In the 2003 and 2007, rounds all newly incorporated households in the localities were also surveyed. These two facts—the incorporation of the control localities in 2000 and the inclusion of all new households in 2003 and 2007—provide variability to the time that households included in the surveys have received programme benefits (including a significant proportion that reported not being beneficiaries of the programme). We took advantage of this variability in this analysis. We analysed the impact of the programme over time using the number of years in which localities have benefited from the programme as an approximation for exposure time to the programme.
This analysis used data from the survey’s prenatal and delivery care modules. For the descriptive analysis of number of ANC visits, we used information about the last pregnancy for women with a least one child less than 24 months old from each of the three surveys 1998, 2003 and 2007 to make them comparable. Sample sizes for each year were 5774, 3692 and 4757 women, respectively.1
Regression analyses were performed on data from 4757 women who had had a live birth less than 24 months before the survey interview in 2007 (294 with missing values were excluded). In these regressions we included the proxy variable programme exposure time.
Outcome variables
The regression analysis focused on two main outcomes that measure womens’ decisions about reproductive health services. The first is a count variable indicating the number of ANC visits reported by women during their latest pregnancy. For this result we analysed two aspects: (1) the trend of the unadjusted average number of ANC visits in 1998, 2003 and 2007, and (2) the adjusted regression analysis of the utilization of ANC visits in 2007, taking into account the time that women had received the programme. The second outcome was a dichotomous variable indicating whether the last delivery was attended by a physician/nurse or by a traditional midwife in 2007.
Explanatory variables
All regression models were controlled for individual, household and locality characteristics related to prenatal care and delivery. At the individual level we incorporated women’s age and age square assuming that a woman tends to increase her use of prenatal health services as her age increases, then decreases when she reaches the end of her reproductive age span. Marital status, level of education and women’s work status were also incorporated. Marital status has been shown to be associated positively with the use of reproductive health services (Becker et al. 1993; Alexandre et al. 2005; Barber 2006; Biratu and Lindstrom 2006); the women were categorized as married (which included a civil union) as opposed to being single, divorced, separated or widowed. A series of dummy variables indicating the levels of education (elementary school, middle school and professional) were constructed based on the fact that more educated women tend to use more health services. A dichotomous variable indicating if the woman had worked in the last 2 weeks was constructed in order to measure if the participation of women in the job market influences women’s decision to use prenatal/delivery services. Two dichotomous variables indicating the presence of a prenatal medical complication or a complication during delivery were also included. The presence of a prenatal medical complication or pre-partum complication could influence not only the frequency of antenatal care visits, but also the woman’s decision regarding who would attend the delivery.
At household level we included a self-reported variable that indicated if a woman’s family was enrolled in and receiving benefits from the Oportunidades programme. Variables including indigenous head of household, social security coverage and the socio-economic level of the family were also incorporated in the model. A dummy variable identifying indigenous households was included because historically this group in Mexico has less access to basic health services. The variable ‘access to any public health insurance’, in general, identifies those families with better access to, and use of, health services. This variable includes both those women insured through the social security system (IMSS, ISSSTE and others) and Seguro Popular, the public social insurance that targets the poor.
We used a welfare index at household level as a proxy for the family’s socio-economic level. This index was constructed with a group of household assets using principal components, particularly the polychoric correlation (Kolenikov and Angeles 2004; McKenzie 2005). We considered the availability of assets such as refrigerator, TV, telephone, oven, stove, etc. With this asset index we generated dummies indicating terciles of the asset index at household level as an approximation of household wealth.
At locality level we incorporated dichotomous variables indicating the availability of a health centre and the accessibility of a midwife, as the access to these health resources could influence women’s decisions about both the intensity of service use and the selection of care for delivery. Lastly, we considered a deprivation index for each locality. The deprivation index was obtained from the Consejo Nacional de Población (CONAPO 2005). This measure of deprivation is constructed with eight indicators at locality level that measure welfare status: percentage of population 15 years or older that are illiterate; percentage of population 15 years or older with primary school not finished; percentage of households without sewage; percentage of households without piped water; percentage of households without electricity; percentage of households with some level of overcrowding; percentage of households with dirt floors and percentage of households without a refrigerator. A higher index implies greater deprivation.
We added a proxy variable that indicated the quality of the reproductive health services at each locality level. A structural quality index was constructed based on information from four categories related to the minimum infrastructure needed for the provision of reproductive health services: the proportion of space available for reproductive health services (either ANC or delivery) within the units, the proportion of health units with the medical equipment needed for reproductive care, and the proportion of health units with adequate medical supplies and personnel to provide reproductive health services. This information was collected at each health unit as part of the quality module from the ENCEL 2007 survey. A factor analysis was applied in order to construct the index of structural quality with 408 observations (Gutiérrez et al. 2008). With this index a series of dichotomous variables was created to indicate very low-, low-, middle-, high- and very high structural quality for reproductive health services. The cut-offs were defined based on the distribution of the quality index.
A series of dummies were constructed to indicate the year (1998, 2000, 2003–07) when the locality began offering the Oportunidades programme. The year was identified through administrative files that included information about when each locality started to receive cash transferences from the programme. This variable is a proxy of the degree of exposure to the programme.
Analysis
First, we described the number of ANC visits in the 3 years 1997, 2003 and 2007 to illustrate the changes in one of Oportunidades’ principal target outcomes: the intensity of use of antenatal health services. This initial description was not adjusted for any variable; this part of the analysis simply shows the trends in the mean of the number of ANC visits in each cross-section year and its relation to individual variables such as education, indigenous condition and deprivation grade. Each of the three subsamples is the group of women that reported having a child of less than 24 months old. Comparing the mean differences of individual characteristics of the different samples, such as a women’s age, marital and working status, we did not find significant differences. In contrast, women’s education and socio-economic variables presented significant differences that may be attributed, in part, to the potential effects of the Oportunidades programme.
The second analysis focused on two aspects: (1) we analysed, using a Poisson regression, the factors that determined the mean number of ANC visits for women who report having children aged less than 24 months in 2007; and (2) we estimated, using a multilevel logistic regression, the likelihood of seeking obstetric care with a physician/nurse vs. a traditional midwife with the same subsample of women in 2007.
The multilevel model with random intercept allowed us to relax the assumption of independence of women’s answers that belongs to the same locality. We assumed that women’s attitudes with respect to the use of preventive health services within a locality could be similar, taking into account that women from the same locality had similar characteristics: they lived in rural areas, they were very poor, they were exposed to the same sort of anti-poverty social programmes and they had access to the same provider options. In this way, the use of health services by women from the same locality could be correlated as a result of their similarities. Both models included a random intercept per each locality ζ ∼ N(0, ) in the lineal predictor.
) in the lineal predictor.
For the Poisson model the result variable was a count variable yij for each woman i living in a locality j, where yij = 0, 1, 2, 3, … . The Poisson regression model is described as follows:
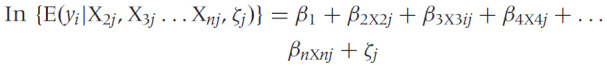 |
We adjusted this model with a series of explanatory variables at individual, household and locality levels. We also included the proxy variable of the exposure to the Oportunidades programme at locality level that indicated the year in which the locality where the woman lives was incorporated into the programme. The regression also included the random intercept, ζj, which models the variability at locality level.
For the logistic model the result variable is a dichotomy variable yij for each woman i living in a locality j, where yij = 1 if the woman was attended by a physician/nurse for her delivery and yij = 0 if the woman was attended by a traditional midwife. The logistic regression model is defined as follows:
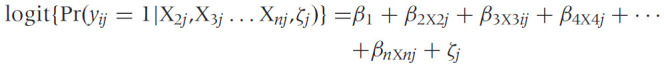 |
We added a fixed effect that included a group of individual, household and locality variables, a proxy variable of the exposure to the Oportunidades programme and a random intercept ζj. Both models were estimated with the stata command gllamm available in the StataCorp 9.2 programme (StataCorp LP, College Station, Texas, USA).
Results
Trends for number of antenatal care visits 1998, 2003 and 2007
Table 1 shows the trend in the mean number of ANC visits for the three cross-sectional years. Significant differences in the mean number of ANC visits for women living in localities influenced by Oportunidades were observed in the period from 1998 to 2007: the unadjusted average of ANC visits among populations benefiting from Oportunidades increased from 4.4 ANC visits in 1998 to 5.7 ANC visits in 2003 and 6.4 in 2007.
Table 1.
Trends for number of antenatal care visits 1998, 2003 and 2007
| Baseline |
Oportunidades follow-ups |
Difference of means |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 1998 |
2003 |
2007 |
1998 vs. 2003 | 1998 vs. 2007 | 2003 vs. 2007 | ||||
| Mean | SD | Mean | SD | Mean | SD | ||||
| Number of antenatal care visits | 4.40 | 2.19 | 5.69 | 2.36 | 6.36 | 2.88 | 1.29*** | 1.96*** | 0.67** |
| Number of antenatal care visits by education level: | |||||||||
| Elementary school | 4.45 | 2.19 | 5.67 | 2.35 | 6.34 | 2.81 | 1.22*** | 1.89*** | 0.67*** |
| Middle school | 4.98 | 2.26 | 5.93 | 2.29 | 6.48 | 2.60 | 0.94*** | 1.49*** | 0.55*** |
| University/technical | 4.99 | 2.41 | 5.62 | 2.19 | 7.57 | 2.74 | 0.64 | 2.59*** | 1.95*** |
| Number of antenatal care visits among: | |||||||||
| Indigenous women (self-report-head of household) | 3.76 | 2.04 | 5.41 | 2.39 | 5.73 | 2.78 | 1.65*** | 1.96*** | 0.31*** |
| Indigenous women with elementary school | 3.88 | 2.14 | 5.37 | 2.42 | 6.82 | 2.89 | 1.48*** | 2.93*** | 1.45*** |
| Illiterate women | 3.85 | 2.04 | 5.44 | 2.39 | 5.48 | 3.20 | 1.59*** | 1.63*** | 0.04 |
| Women living in localities with high deprivation index | 3.90 | 2.06 | 5.13 | 2.38 | 6.31 | 2.83 | 1.23*** | 2.40*** | 1.17*** |
| Women living in localities with high deprivation index and indigenous | 3.71 | 1.98 | 4.59 | 2.27 | 5.70 | 2.80 | 0.88*** | 1.99*** | 1.12*** |
| Women living in localities with high deprivation index and illiterate | 3.78 | 1.99 | 4.84 | 2.42 | 5.41 | 3.10 | 1.06*** | 1.63*** | 0.57 |
| Women living in localities with high deprivation index, indigenous and illiterate | 3.61 | 1.82 | 4.40 | 2.22 | 4.73 | 3.19 | 0.79*** | 1.12** | 0.33 |
***P < 0.01, **P < 0.05, *P < 0.1.
When the mean number of visits is shown by specific characteristics such as level of education, indigenous condition and deprivation level, we found a greater significant increment in the number of ANC visits among more educated women: while women with university education showed an increment of ANC visits from 4.99 in 1998, to 5.62 in 2003 and 7.57 in 2007, the increment among illiterate women was from 3.85 in 1998, to 5.44 in 2003 and 5.48 in 2007. There was an upward trend in average number of ANC visits among women living in localities with high deprivation levels; 3.9 ANC visits in 1998, 5.13 ANC visits in 2003 and 6.31 ANC visits in 2007. But this trend was less pronounced among more disadvantaged women, i.e. indigenous, illiterate and those living in highly deprived localities: 3.61 ANC visits in 1998, 4.4 ANC visits in 2003 and 4.7 ANC visits in 2007.
Sample characteristics of the 2007 cross-sectional dataset
Table 2 reports descriptive statistics of the 2007 sample. This sample was composed of women with a child less than 2 years old, who were themselves on average 29 years old.2 These women had a relatively low level of education: 68% with elementary school, 26% with middle school and 4% with superior education. The majority were married or in a civil union (89%), and only 10% mentioned working. From this sub-sample, 27% of women belonged to households where the head-of-household reported speaking an indigenous language. Almost 47% of women reported being enrolled in a social insurance programme (IMSS, ISSSTE, PEMEX,3 or public insurance, i.e. Seguro Popular4) and 63% self-reported that at least one family member was covered by the Oportunidades programme. In approximately 34% of the households, respondents were classified in the first tercile of the socio-economic index, 34% in the second tercile and 32% in the third tercile.
Table 2.
Descriptive statistics for the 2007 sample
| Variables | Obs | Mean | Std Dev. |
|---|---|---|---|
| Sample size | 4757 | ||
| Outcomes | |||
| Delivery care by physician/nurse (1)+ | 0.80 | 0.40 | |
| Number of antenatal care visits | 6.44 | 2.79 | |
| Covariates | |||
| Individual characteristics | |||
| Age (in years) | 29.43 | 5.83 | |
| Age groups | |||
| 15–19 years+ | 0.05 | 0.21 | |
| 20–24 years+ | 0.11 | 0.32 | |
| 25–35 years+ | 0.69 | 0.46 | |
| 36–49 years+ | 0.15 | 0.36 | |
| Married+ | 0.89 | 0.31 | |
| Women working (2)+ | 0.10 | 0.31 | |
| Indigenous self-identity (head of household) (3)+ | 0.27 | 0.40 | |
| Health complications during delivery+ | 0.31 | 0.46 | |
| Health complications during pregnancy+ | 0.54 | 0.50 | |
| Education level: | |||
| No education+ | 0.002 | 0.05 | |
| Elementary school+ | 0.68 | 0.47 | |
| Middle school+ | 0.26 | 0.44 | |
| University/technical+ | 0.06 | 0.24 | |
| Household characteristics | |||
| Access to any public health insurance+ | 0.47 | 0.50 | |
| Socio-economic level approximate by asset index | |||
| Socio-economic level 1+ | 0.34 | 0.47 | |
| Socio-economic level 2+ | 0.34 | 0.47 | |
| Socio-economic level 3+ | 0.32 | 0.47 | |
| Benefited by Oportunidades programme+ | 0.63 | 0.48 | |
| Benefited by Oportunidades and indigenous | 0.18 | 0.36 | |
| Locality characteristics | |||
| Quality of health units | |||
| Low quality+ | 0.10 | 0.30 | |
| Middle-low quality+ | 0.38 | 0.48 | |
| Middle-high quality+ | 0.41 | 0.49 | |
| High quality+ | 0.11 | 0.31 | |
| With a health centre+ | 0.66 | 0.48 | |
| With a traditional midwife+ | 0.22 | 0.41 | |
| Benefited by Oportunidades since (4) | |||
| 1998+ | 0.36 | 0.48 | |
| 2000+ | 0.25 | 0.43 | |
| 2003–07+ | 0.39 | 0.35 | |
| Grade of deprivation (5) | |||
| Low+ | 0.08 | 0.27 | |
| Middle+ | 0.16 | 0.37 | |
| High+ | 0.76 | 0.43 |
Notes:+ Dummy variable: Yes = 1; No = 0.
(1) Dummy = 1 if women’s delivery was attended by a physician/nurse and = 0 if attended by a traditional midwife.
(2) Dummy = 1 if the woman was working at the time of the interview, = 0 otherwise.
(3) Dummy = 1 if women identify themselves as indigenous, = 0 otherwise.
(4) Dummies indicating the year of incorporation of the locality to the Oportunidades programme.
(5) Dummies indicating the grade of deprivation taking into account variables such as employment, public services availability, infrastructure, socio-economic characteristics, educational levels at locality level.
At locality level, only 12% of women lived in a locality where reproductive health services were categorized as high quality and 10% as low quality services. Most of the women lived in localities where reproductive health services were characterized as middle-low (38%) and middle-high (41%) quality. More than half of the women (66%) lived in localities where a health centre was readily available and 24% where only a traditional midwife was available. The majority of women (76%) lived in highly deprived localities. Approximately 36% of women in this sample belonged to a locality that had benefited from the Oportunidades programme since 1998, 25% to a locality benefiting since 2000 and 39% to a locality benefiting since 2003.
Among users of prenatal health services from the 2007 survey, almost 96% of non-indigenous women and 91% of indigenous women mentioned having visited a physician for prenatal care. Almost 36% of these women also reported visiting an additional provider for antenatal care; and in half of these cases, the second provider was a traditional midwife.
With respect to obstetric care reported by women in 2007, overall 79% of women reported having been attended by a physician/nurse for their most recent delivery. Of these, 99% were with a physician. Among indigenous women, 57% reported having been attended by a physician/nurse in the latest delivery and 38% by a traditional midwife.5 In contrast, 84% of non-indigenous women mentioned having been attended by a physician/nurse and 13% by a traditional midwife. The remaining women reported having delivered alone or being attended by another person (such as husband, mother, mother-in-law).
Multivariate analyses
The first Poisson multilevel regression model for the 2007 sample is shown in Table 3. Results of the model in column (1) assessed the association between the number of ANC visits and the year in which the locality began to benefit from the Oportunidades programme, the family’s membership in the programme at the time of the interview, as well as other explanatory variables at individual, household and locality levels.
Table 3.
Poisson model for number of antenatal care visits
| (1) |
(2) |
(3) |
(4) |
|||||
|---|---|---|---|---|---|---|---|---|
| OR | s.e. | OR | s.e. | OR | s.e. | OR | s.e. | |
| Individual characteristics | ||||||||
| 15–19 years old(a)+ | 0.96 | 0.04 | 0.96 | 0.04 | 1.00 | 0.06 | 1.01 | 0.06 |
| 20–24 years old(a)+ | 1.07** | 0.03 | 1.05** | 0.03 | 1.09** | 0.04 | 1.09** | 0.04 |
| 25–35 years old(a)+ | 1.04* | 0.02 | 1.04* | 0.02 | 1.02* | 0.05 | 1.02* | 0.05 |
| Married woman | 1.12*** | 0.03 | 1.14*** | 0.03 | 1.13*** | 0.03 | 1.13*** | 0.03 |
| Woman working | 0.98 | 0.03 | 0.98 | 0.03 | 0.98 | 0.03 | 0.98 | 0.03 |
| Health complication during pregnancy+ | 1.05*** | 0.02 | 1.05*** | 0.02 | 1.05*** | 0.02 | 1.05*** | 0.02 |
| Education level: middle school(b)+ | 1.10*** | 0.02 | 1.06* | 0.03 | 1.10*** | 0.02 | 1.08** | 0.03 |
| Education level: professional(b)+ | 1.18*** | 0.04 | 1.10** | 0.04 | 1.17*** | 0.04 | 1.11*** | 0.04 |
| Household characteristics | ||||||||
| Benefited by Oportunidades (self-report)+ | 0.99 | 0.01 | 0.99 | 0.01 | 1.00 | 0.01 | 0.99 | 0.01 |
| Indigenous (self-identity)+ | 0.92* | 0.04 | 0.92* | 0.04 | 0.92* | 0.04 | 0.92* | 0.04 |
| Access to any public health insurance+ | 1.10*** | 0.02 | 1.09*** | 0.02 | 1.09*** | 0.02 | 1.09*** | 0.02 |
| Socio-economic level 2(c)+ | 1.01 | 0.02 | 1.01 | 0.02 | 1.01 | 0.02 | 1.01 | 0.02 |
| Socio-economic level 3(c)+ | 0.99 | 0.02 | 0.99 | 0.02 | 0.99 | 0.02 | 0.99 | 0.02 |
| Quality of locality health resources | ||||||||
| Middle-low quality(d)+ | 1.05 | 0.06 | 1.05 | 0.06 | 1.05 | 0.06 | 1.04 | 0.06 |
| Middle-high quality(d)+ | 1.00 | 0.06 | 1.00 | 0.06 | 0.99 | 0.06 | 0.99 | 0.06 |
| High quality(d)+ | 0.94 | 0.07 | 0.93 | 0.07 | 0.93 | 0.07 | 0.92 | 0.07 |
| Locality characteristics | ||||||||
| With a health centre+ | 0.98 | 0.04 | 0.99 | 0.04 | 0.98 | 0.04 | 0.99 | 0.04 |
| With a traditional midwife+ | 0.94 | 0.04 | 0.95 | 0.04 | 0.95 | 0.04 | 0.95 | 0.04 |
| Benefited by Oportunidades since 1998(e)+§ | 0.98 | 0.04 | 0.97 | 0.04 | 1.06 | 0.07 | 1.06 | 0.07 |
| Benefited by Oportunidades since 2000(e)+§ | 1.02* | 0.05 | 1.01 | 0.05 | 1.04 | 0.07 | 1.05 | 0.07 |
| Deprivation index | 1.00 | 0.02 | 1.01 | 0.02 | 1.01 | 0.02 | 1.01 | 0.02 |
| Interactions | ||||||||
| Middle school x Oportunidades since 1998(f)+ | 1.07 | 0.05 | 1.06 | 0.05 | ||||
| University x Oportunidades since 1998(f)+ | 1.12 | 0.10 | 1.13 | 0.10 | ||||
| Middle school x Oportunidades since 2000(g)+ | 1.00 | 0.05 | 0.99 | 0.05 | ||||
| University x Oportunidades since 2000(g)+ | 1.38*** | 0.12 | 1.20** | 0.11 | ||||
| Middle school x Oportunidades since 2003–07(h)+ | 1.10* | 0.06 | 1.09* | 0.06 | ||||
| University x Oportunidades since 2003–07(h)+ | 1.15 | 0.12 | 1.19* | 0.12 | ||||
| Aged 15–19 yrs x Oportunidades since 1998(i)+ | 1.09* | 0.09 | 1.15** | 0.09 | ||||
| Aged 15–19 yrs x Oportunidades since 2000(i)+ | 0.90 | 0.09 | 0.90 | 0.09 | ||||
| Aged 20–24 yrs x Oportunidades since 1998(j)+ | 1.16** | 0.07 | 1.24** | 0.07 | ||||
| Aged 20–24 yrs x Oportunidades since 2000(j)+ | 1.27*** | 0.09 | 1.23*** | 0.09 | ||||
| Aged 25–35 yrs x Oportunidades since 1998(k)+ | 0.89** | 0.05 | 0.89** | 0.05 | ||||
| Aged 25–35 yrs x Oportunidades since 2000(k)+ | 0.93 | 0.05 | 0.93 | 0.05 | ||||
| Sample size | 4785 | 4775 | 4757 | 4757 | ||||
| Log likelihood | −8787 | −8775 | −8768 | −8762 | ||||
***P < 0.01, **P < 0.05, *P < 0.1.
+Dummy variable: Yes = 1; No = 0.
§Odds ratios of models (2), (3) and (4) statistically similar.
References: (a) Aged 36–49 years old. (b) Education level: No education/elementary school. (c) Socio-economic level 1. (d) Low quality. (e) Benefited by Oportunidades 2003–07. (f)(g)(h) No education/elementary school x Oportunidades since 1998, 2000 and 2003–07, respectively. (i)(j)(k) Aged 15–19 yrs, aged 20–24 yrs, and aged 25–35 yrs x Oportunidades 2003–207, respectively.
Source: Encuesta de Evaluación Rural (ENCEL-RURAL) 1998, 2003 and 2007.
Most of the individual and household level variables showed significant associations. Women who were married reported on average 11.9% more ANC visits than unmarried women. Having had a prenatal health complication during the pregnancy predicted 5.1% more ANC visits than those who did not have any complication. Women with higher education, both middle school and university levels, increased their number of ANC visits by 10.0% and 18.0%, respectively, compared with women who had no or only elementary school education. Insurance coverage was associated with a 10.0% increase in ANC visits with respect to those without health insurance. We found a negative association between the use of antenatal health services and women who lived in families where the head of household reported being indigenous: women with an indigenous head of household decreased their use of prenatal health services by 8.0%, compared with those who lived in households where the head of the family was not indigenous. No significant associations were found with either the self-reported variable of women living in households benefited by Oportunidades or the indicator of household socio-economic level. The latter might be related to the fact that socio-economic limitations for ANC visits were overcome by the economic incentives of Oportunidades.
Surprisingly, at locality level, there was no significant association between ANC visits and the variable for quality of health services. We found a significant association between those women who lived in localities that were exposed to Oportunidades since 2000 and the number of ANC visits: on average, women who lived in localities exposed to Oportunidades since 2000 reported 2.1% more visits than women who lived in localities exposed to Oportunidades since 2003–07.
In column (2) of Table 3 we show the Poisson regression model adding some interactions. We present the interaction between the locality’s year of incorporation into Oportunidades and some covariables that could favour/disfavour the effect of year of incorporation to Oportunidades on the number of ANC visits. We also show the interaction between the year of incorporation into the programme with the level of deprivation and women’s education. We did not find any significant association with the deprivation index (results not shown). However, women with university/technical education who lived in localities incorporated into the programme in 2000 and those with middle school education incorporated into the programme in 2003 reported 38.0% and 10.0%, respectively, more ANC visits than those women without education or with elementary education. When we added interactions of age group and each year of incorporation to the programme, we found no major changes in the results except the effect of incorporation of localities in 2000 on the number of ANC visits, which was no longer statistically significant.
The multilevel logistic model for delivery care is shown in Table 4. Most of the individual characteristics were statistically significant. Married/civil union women on average were 95.4% more likely to be attended by a physician/nurse than unmarried women; women who reported having had any health complication either during the pregnancy or during the delivery were 75.7% and 139%, respectively, more likely to be cared for by a physician/nurse. Women with middle school and university education were over 100% more likely to be attended by a physician/nurse for delivery care than non-educated or women with elementary school education.
Table 4.
Logit model for delivery care with a doctor vs. a traditional midwife
| (1) |
(2) |
(3) |
(4) |
|||||
|---|---|---|---|---|---|---|---|---|
| OR | s.e. | OR | s.e. | OR | s.e. | OR | s.e. | |
| Individual characteristics | ||||||||
| 15–19 years(a)+ | 1.67 | 0.57 | 1.66 | 0.57 | 2.12 | 0.98 | 2.33* | 1.07 |
| 20–24 years(a)+ | 1.07 | 0.28 | 1.04 | 0.28 | 0.94 | 0.34 | 1.01 | 0.37 |
| 25–35 years(a)+ | 1.08 | 0.19 | 1.03 | 0.19 | 1.47 | 0.39 | 1.41 | 0.37 |
| Married woman | 1.95*** | 0.43 | 2.02*** | 0.44 | 1.96*** | 0.43 | 2.00*** | 0.45 |
| Woman working | 1.32 | 0.30 | 1.32 | 0.30 | 1.38 | 0.32 | 1.37 | 0.31 |
| Health complication during pregnancy+ | 1.76*** | 0.24 | 1.80*** | 0.25 | 1.74*** | 0.24 | 1.78*** | 0.25 |
| Health complication during delivery+ | 2.39*** | 0.37 | 2.34*** | 0.36 | 2.40*** | 0.37 | 2.36*** | 0.37 |
| Education level: middle school(b)+ | 2.74*** | 0.48 | 1.59* | 0.40 | 2.81*** | 0.50 | 1.69** | 0.43 |
| Education level: professional(b)+ | 5.43*** | 2.01 | 3.31*** | 1.35 | 5.44*** | 2.02 | 3.47*** | 1.43 |
| Household characteristics | ||||||||
| Benefited by Oportunidades (self report)+ | 0.66*** | 0.09 | 0.66*** | 0.09 | 0.66*** | 0.08 | 0.66*** | 0.08 |
| Indigenous (self identity)+ | 0.31*** | 0.12 | 0.30*** | 0.12 | 0.31*** | 0.12 | 0.29*** | 0.11 |
| Access to any public health insurance+ | 1.83*** | 0.26 | 1.84*** | 0.26 | 1.84*** | 0.26 | 1.84*** | 0.26 |
| Socio-economic level 2(c)+ | 1.15 | 0.16 | 1.16 | 0.16 | 1.16 | 0.16 | 1.17 | 0.16 |
| Socio-economic level 3(c)+ | 1.15 | 0.18 | 1.15 | 0.18 | 1.16 | 0.18 | 1.17 | 0.19 |
| Quality of locality health resources | ||||||||
| Middle-low quality(d)+ | 0.62 | 0.35 | 0.62 | 0.35 | 0.60 | 0.34 | 0.61 | 0.35 |
| Middle-high quality(d)+ | 0.49 | 0.27 | 0.49 | 0.28 | 0.47 | 0.26 | 0.48 | 0.27 |
| High quality(d)+ | 0.41 | 0.27 | 0.39 | 0.26 | 0.41 | 0.27 | 0.39 | 0.26 |
| Locality characteristics | ||||||||
| With a health centre+ | 0.85 | 0.28 | 0.90 | 0.30 | 0.84 | 0.28 | 0.88 | 0.29 |
| With a traditional midwife+ | 0.38*** | 0.14 | 0.39*** | 0.14 | 0.38*** | 0.14 | 0.39*** | 0.14 |
| Benefited by Oportunidades since 1998(e)+§ | 2.40** | 0.86 | 2.13** | 0.79 | 3.47*** | 1.76 | 3.22** | 1.65 |
| Benefited by Oportunidades since 2000(e)+§ | 3.32*** | 1.36 | 2.92** | 1.22 | 3.79*** | 2.62 | 3.39*** | 2.42 |
| Deprivation index | 0.37*** | 0.08 | 0.38*** | 0.08 | 0.37*** | 0.08 | 0.38*** | 0.08 |
| Interactions | ||||||||
| Middle school x Oportunidades since 1998(f)+ | 2.65** | 1.15 | 2.17* | 0.97 | ||||
| University x Oportunidades since 1998(f)+ | 4.63 | 5.87 | 3.35 | 4.26 | ||||
| Middle school x Oportunidades since 2000(g)+ | 2.58** | 1.16 | 2.78** | 1.28 | ||||
| University x Oportunidades since 2000(g)+ | 4.18 | 5.38 | 3.31 | 4.41 | ||||
| Middle school x Oportunidades since 2003–07(h)+ | 3.96* | 2.90 | 3.58* | 2.63 | ||||
| University x Oportunidades since 2003–07(h)+ | 9.36 | 16.21 | 5.51 | 4.37 | ||||
| Aged 15–19 yrs x Oportunidades since 1998(i)+ | 2.32** | 2.18 | 1.88* | 1.81 | ||||
| Aged 15–19 yrs x Oportunidades since 2000(i)+ | 1.24* | 0.20 | 1.18** | 0.15 | ||||
| Aged 20–24 yrs x Oportunidades since 1998(j)+ | 1.67** | 1.03 | 1.41** | 0.89 | ||||
| Aged 20–24 yrs x Oportunidades since 2000(j)+ | 1.26* | 0.79 | 1.03* | 0.68 | ||||
| Aged 25–35 yrs x Oportunidades since 1998 (k)+ | 0.54* | 0.23 | 0.56* | 0.24 | ||||
| Aged 25–35 yrs x Oportunidades since 2000 (k)+ | 0.51* | 0.27 | 0.49* | 0.27 | ||||
| Sample size | 4757 | 4757 | 4757 | 4757 | ||||
| Log likelihood | −1247 | −1240 | −1240 | −1235 | ||||
***P < 0.01, **P < 0.05, *P < 0.1.
+Dummy variable: Yes = 1; No = 0.
References: (a) Aged 36–49 years old. (b) Education level: No education/elementary school. (c) Socio-economic level 1. (d) Low quality. (e) Benefited by Oportunidades 2003–07. (f)(g)(h) No education/elementary school x Oportunidades since 1998, 2000 and 2003–07, respectively. (i)(j)(k) Aged 15–19 yrs, aged 20–24 yrs and aged 25–35 yrs x Oportunidades 2003–07, respectively.
§ In models (1) and (2) Wald tests linear hypotheses after estimation indicates significant differences (P < 0.05). In models (3) and (4) this test indicates no statistically significant differences (P > 0.10) in these coefficients.
Source: Encuesta de Evaluación Rural (ENCEL-RURAL) 1998, 2003 and 2007.
Women who belonged to families benefiting from the Oportunidades programme were 33.7% less likely to be cared for by a physician/nurse than women who did not benefit from the programme.6 No significant association was found with the family’s socio-economic level. Furthermore, women of indigenous origin were 68.9% less likely to be cared for by a physician/nurse than women of non-indigenous background. In contrast, women who belonged to families entitled to some form of health insurance had an 82.8% greater likelihood of being attended by a physician/nurse with respect to women without any health insurance.
Locality level highlights the fact that women who lived in localities where only a traditional midwife was available were 61.8% less likely to go to a physician/nurse for childbirth than those who lived in localities where there was no traditional midwife. The same tendency was found in poor localities. A one unit increase in the deprivation index (worse conditions) was associated with a 63.3% decrease in the probability of being attended by a physician/nurse for delivery, holding all other predictors constant.
In contrast to what was found with the variable indicating whether or not the family belonged to Oportunidades, women who belonged to localities benefiting from Oportunidades for a longer period of time were significantly more likely to have their delivery attended by a physician/nurse than by a traditional midwife. Women from localities incorporated into the programme since 1998 had 140% greater likelihood of going to a physician/nurse for childbirth than those in localities incorporated since 2003. Women who lived in localities incorporated into Oportunidades since 2000 had 232.1% greater probability of going to physician/nurse for delivery than those in localities incorporated since 2003. Note that when we added interactions to control for differences in education levels among women who started benefiting from Oportunidades in the same year, as well as interactions that indicate the potential differences among women from the same age group over the different time exposures to the programme, we did not find any significant difference in the magnitude of the effects of living in localities exposed to the programme from 1998 and 2000 with respect to 2003–07 (see Table 4, columns 2 and 3).
When adding both the interactions of age groups and year of incorporation, we found that for young women (15–19 years old) the probability of going to a physician for delivery care among those who belong to localities incorporated in 1998 with respect to 2003–07, is greater (88%) than those from the same age group living in localities incorporated in 2000 (18%) (see Table 4, column 4). The same pattern is found among young women aged 20–24; the probability to go to a physician among those women living in localities incorporated in 1998 (41%) is larger than for women in localities incorporated in 2000 (3.0%) with respect to 2003–07. However, we did not find a similar significant association among women in the 25–35 year age group. Looking at the interaction variables of a woman’s education and locality’s year of incorporation to the programme (Table 4, column 4), we found significant effects for women with middle-school education in each of the years analysed. Taking as a reference category those less-educated women (women with no education or only elementary school in each year), we found that women with more education (middle school) had a greater probability of going to a physician/nurse for delivery in 1998 (117.0% greater), in 2000 (178.0% greater) and in 2003–07 (258% greater).
Discussion
Our findings support the concept of a learning effect that impacts Oportunidades beneficiaries’ reproductive health behaviour and decisions. These findings suggest that there have been positive effects of the Oportunidades programme in improving the use of antenatal services through the provision of economic incentives in the long term. We also found that the programme’s effect has extended its impact on women’s preference for delivery care, particularly among the youngest women. Young women who belonged to localities with longer exposition to Oportunidades, particularly from 1998 and 2000, preferred to seek care with a physician/nurse for delivery more than those of the same age group who were more recently enrolled in the programme (2003–07).
We also found that indigenous women living in localities with Oportunidades preferred a traditional midwife for delivery care. This confirms findings from other studies in Latin America that underline the limited access to basic western health care among the indigenous population (Wilkinson et al. 2001). This restricted access to health services among the indigenous population has been associated both with financial, geographic and cultural barriers and with insensitive, discriminatory or unfriendly health staff (Wilkinson et al. 2001).
The role of traditional midwives in providing antenatal and delivery care in rural areas is of particular importance (Anderson et al. 2004). In poor rural areas elsewhere in Latin America there is still a preference for childbirth care with traditional midwives (or ‘comadronas’) than with physicians in formal health services (Replogle 2007). This has, in part, been explained by the interpersonal relationship that midwives establish with pregnant women and by their attention to the traditional and cultural practices that women seek (emotional support, massage, herbal therapy, repositioning the baby). It is clear that although the Oportunidades programme has influenced women’s selection for formal delivery care in rural areas, physician/nurse care for delivery among indigenous women was not routine nor actively sought out. Interestingly, nor was the choice of delivery care associated with the health centres’ quality index.
Our results show that the utilization of public health services by women living in poor rural areas, whether indigenous or not, has increased considerably in the 10 years of Oportunidades implementation. More relevant is the fact that women belonging to families with greater time of exposure to Oportunidades had a greater likelihood that their last delivery was attended by a physician/nurse. This coincides with previous findings that have shown the relationship between access to more antenatal procedures and the greater probability of a skilled institutional delivery (Barber 2006). However, we also found that indigenous women continue to prefer having their births attended by a traditional midwife. This situation is similar to other developing countries where there is a growing use of public ANC services not matched by a similar increase in the use of public obstetric services (Elo 1992).
Approximately 500 000 women die from complications of pregnancy and childbirth annually, and more than 99% of these deaths occur in less developed regions. The target for Millennium Development Goal 5 is that the number of maternal deaths be reduced by three-quarters by 2015 (WHO 2009). This was presumed an attainable goal given the fact that the principal causes of these deaths are associated with the lack of appropriate and quality health care (Kvåle et al. 2005). During the 10 years since the implementation of Oportunidades, the use of formal services for maternal health care (antenatal and delivery care) has improved substantially among the localities under its influence. However, access and use of formal obstetric services among women of indigenous origin represents a continuing challenge, particularly taking into account the high maternal mortality rates that persist in states (Chiapas, Oaxaca, Guerrero, Veracruz) with the highest proportion of indigenous population (INMUJERES 2009).
The World Health Organization has emphasized the importance of skilled attendance at birth as a primary strategy to decrease maternal mortality (WHO 2009). Mexico and other developing countries with a high proportion of indigenous population must develop strategies to bring culturally appropriate and effective delivery care interventions to these communities in order to reduce maternal mortality rates. This entails overcoming not only the cultural and communication barriers to the use of formal health services and physical access to these services, but also meeting standards of skilled attendance at delivery. Oportunidades has proven its potential to improve utilization of formal health services among its beneficiaries; however, there are still questions about whether women are receiving adequate skilled care during pregnancy and delivery that promotes early identification and management of obstetric complications which in turn could impact maternal mortality.
Examples of programmes in Latin America that have taken into account the specific context of the indigenous population to improve their access to and use of reproductive health services have been reported in Guatemala (Netzer and Mallas 2005), Bolivia (Gonzales-Salguero et al. 2005) and Perú (Davenport 2007). These studies have focused on identifying barriers related to service provision as well as attitudinal and socio-cultural constraints for the indigenous. These interventions have focused on improving family planning (FP) and reproductive health (RH) service delivery specifically by strengthening the skills of health personnel to adequately provide FP/RH services complemented with supervision of health providers. Important components are the inclusion of community–provider participation as part of the supervision process and mechanisms to offer culturally appropriate health services. Similarly, programmes intending to expand obstetric care for indigenous beneficiaries of Oportunidades must also consider and focus on those elements that are key to assuring access and high quality care.
Conclusions
An important increase in the average of the number of ANC visits has been achieved among women living in localities influenced by the Oportunidades programme over 10 years of programme implementation. The learning effect, as an indirect effect of the programme, illustrates how women living in localities with greater exposure time to Oportunidades had a higher probability that their last delivery was attended by a physician/nurse vs. a traditional midwife. However, the most disadvantaged women (indigenous, illiterate and living in the most deprived localities) had less access to skilled care for delivery.
An important modifier of the woman’s selection of health provider during delivery was her level of education. Women with greater education preferred a physician/nurse for delivery than a traditional midwife.
This study has several limitations. Self-reported data obtained from women who described their last pregnancy and delivery could be affected by recall bias. The data describe low-income rural women and this group of women is not representative of the population as a whole. Rural poor women are more likely to be indigenous and to be more reliant on traditional health providers for care. Although we controlled for the presence of other health programmes, such as the introduction of Seguro Popular, as well as other aspects related to changes in women’s attitudes towards the use of health services (such as the age and level of education) that could also influence the use of reproductive health services during the period analysed, there may be other long-term factors that influence women’s choices of care. For example, in Mexico, another public programme targeting pregnant women in rural areas is ‘Arranque Parejo’ and this may have had an effect not considered in this evaluation.
Data about the quality of reproductive health services was limited in this study. Information on quality was available only from those localities where health units were available. The area of influence for these health units was assumed to include all the nearest localities without health units. Although the quality index included in this analysis considers structural elements, neither aspects of technical quality nor patient perception of quality were considered for its construction.
Ethical clearance
Data collection and development of this research was approved by the Research, Ethics and Biosecurity commissions from the Mexican National Institute of Public Health. Consent for participation was obtained from all participants and data collection was implemented considering the confidentiality and reserved rights stipulated by the Mexican Statistical and Geographical information law.
Funding
Data collection and a first version of this analysis was funded by the Mexican programme Oportunidades as part of the External Evaluation of Oportunidades, commissioned by the Mexican Ministry of Social Development, SEDESOL (particularly by the Dirección General de Información Geoestadística, Análisis y Evaluación de Oportunidades) to the National Institute of Public Health (INSP) (http://evaluacion.oportunidades.gob.mx).
Acknowledgements
We thank Stefano Bertozzi for inviting us to participate in the study and for his support and leadership. We also thank anonymous reviewers from the Oportunidades Programme for their comments on the first version of this analysis. The views do not represent the official position of any of the institutions that funded or facilitated that evaluation. The organizations did not have any role in study design, analysis or interpretation; nor in the writing of the manuscript or the decision to submit the manuscript for publication. The authors are solely responsible for the contents.
Endnotes
1 Mean differences in individual variables such as woman’s age, woman’s marital status, woman’s working status are similar among the three subsamples. In contrast, as it could be expected, educational and socio-economic variables are different among the three subsamples considering the potential impact of the programme on women’s socio-economic condition and educational level. The Oportunidades programme is focused on providing economic support to the families, promoting school attendance among children and the use of preventive health services.
2 The average age of women with children aged 2 years or less was almost 28 years in 2007, while the average age of the analytical sample is 29 years.
3 By law, workers from the formal private sector are covered by a social insurance programme named IMSS. Workers from the public sector are covered by different social insurance programmes such as ISSSTE, PEMEX or SEDENA depending on their place of work.
4 Seguro Popular is a voluntary health insurance targeting the uninsured poorest groups of population that has been implemented since 2001.
5 Five per cent of indigenous women mentioned having been attended by another person in the place where they live.
6 Women who are not benefited by Oportunidades live in less deprived localities with higher quality health services (descriptive not shown).
Contributor Information
Sandra G Sosa-Rubí, Health Economics Division, Mexican School of Public Health/National Institute of Public Health (INSP), Cuernavaca, Mexico and 2Reproductive Health Division, Mexican School of Public Health/National Institute of Public Health (INSP), Cuernavaca, Mexico.
Dilys Walker, Health Economics Division, Mexican School of Public Health/National Institute of Public Health (INSP), Cuernavaca, Mexico and 2Reproductive Health Division, Mexican School of Public Health/National Institute of Public Health (INSP), Cuernavaca, Mexico.
Edson Serván, Health Economics Division, Mexican School of Public Health/National Institute of Public Health (INSP), Cuernavaca, Mexico and 2Reproductive Health Division, Mexican School of Public Health/National Institute of Public Health (INSP), Cuernavaca, Mexico.
Sergio Bautista-Arredondo, Health Economics Division, Mexican School of Public Health/National Institute of Public Health (INSP), Cuernavaca, Mexico and 2Reproductive Health Division, Mexican School of Public Health/National Institute of Public Health (INSP), Cuernavaca, Mexico.
References
- Alexandre PK. Crandall L. Saint-Jean G. Prenatal care utilization in rural areas and urban areas of Haiti. Revista Panamericana de Salud Pública. 2005;18:84–92. doi: 10.1590/s1020-49892005000700002. [DOI] [PubMed] [Google Scholar]
- Anderson B. Anderson E. Franklin T. Dzib-Xihum de Cen A. Pathways of decision making among Yucatan Mayan traditional birth attendants. Journal of Midwifery & Women’s Health. 2004;49:312–9. doi: 10.1016/j.jmwh.2004.03.008. [DOI] [PubMed] [Google Scholar]
- Barber SL. Does the quality of prenatal care matter in promoting skilled institutional delivery? A study in rural Mexico. Maternal and Child Health Journal. 2006;10:419–25. doi: 10.1007/s10995-006-0079-x. [DOI] [PubMed] [Google Scholar]
- Barber SL. Gertler PJ. The impact of Mexico’s conditional cash transfer programme, Oportunidades, on birth weight. Tropical Medicine and International Health. 2008;13:1405–14. doi: 10.1111/j.1365-3156.2008.02157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber SL. Gertler P. Health workers, quality of care, and child health: Simulating the relationships between increases in health staffing and child length. Health Policy. 2009;91:148–55. doi: 10.1016/j.healthpol.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber SL. Bertozzi S. Gertler P. Variations in prenatal care quality for the rural poor in Mexico. Health Affairs. 2007;26:310–23. doi: 10.1377/hlthaff.26.3.w310. [DOI] [PubMed] [Google Scholar]
- Barham T. Mimeo. Boulder, CO: Department of Economics and Institute of Behavioral Science, University of Colorado; 2006. Providing a healthier start to life: The impact of conditional cash transfers on neo-natal and infant mortality. Online at: at: www.stanford.edu/group/SITE/archive/SITE_2006/Web%20Session%202/Barham.pdf. [Google Scholar]
- Becker S. Peters DH. Gray RH. Gultiano C. Black RE. The determinants of use of maternal and child health services in Metro Cebu, the Philippines. Health Transition Review. 1993;3:77–89. [PubMed] [Google Scholar]
- Biratu B. Lindstrom D. The influence of husbands’ approval on women’s use of prenatal care: results from Yirgalem and Jimma towns, south west Ethiopia. Ethiopian Journal of Health Development. 2006;20:84–92. [Google Scholar]
- Consejo Nacional de Población (CONAPO) Mexico City: 2005. Índice de marginación 2005. Online at: http://www.conapo.gob.mx/publicaciones/margina2005/01_b.pdf. [Google Scholar]
- Davenport A. Atlanta, GA: CARE; 2007. VOICES from the VILLAGE: improving lives through CARE’s sexual and reproductive health programs. The FEMME Project in Peru: partnerships for improved health. Case Study, Number 2. Online at: http://www.care.org.pe/websites/femme/index.htm. [Google Scholar]
- Davis-Tsu V. Underutilization of health centers in rural Mexico: a qualitative approach to evaluation and planning. Studies in Family Planning. 1980;11:145–54. [PubMed] [Google Scholar]
- Elo IT. Utilization of maternal health-care services in Peru: the role of women’s education. Health Transition Review. 1992;2:1–20. [PubMed] [Google Scholar]
- Gertler P. Do conditional cash transfers improve child health? Evidence from PROGRESA’s Control Randomized Experiment. The American Economic Review. 1999;94:336–41. doi: 10.1257/0002828041302109. [DOI] [PubMed] [Google Scholar]
- Gonzales-Salguero F. Martín MA. Pérez-Mendoza R. Vernon R. Washington, DC: Agency for International Development (USAID); 2005. Cross-cultural adaptation of reproductive health services in Bolivia. The Health Policy Initiative; pp. 28–9. [Google Scholar]
- Gutiérrez JP. Leroy J. DeMarie L. et al. México, DF: Secretaría de Desarrollo Social; 2008. Evaluación de la calidad de los servicios de atención a la salud asignados a la población beneficiaria de Oportunidades. In: Evaluación externa del Programa de Oportunidades 2008. A diez años de intervención en zonas rurales (1997–2007). Tomo II, El reto de la calidad de los servicios: resultados en salud y nutrición. [Google Scholar]
- INMUJERES. Mexico City: Instituto Nacional de las Mujeres; 2009. La Población Indígena Mexicana. Online at: http://cedoc.inmujeres.gob.mx/documentos_download/100782.pdf, accessed 25 August 2009. [Google Scholar]
- Kolenikov S. Angeles G. Chapel Hill, NC: Carolina Population Center, University of North Carolina; 2004. The use of discrete data in principal component analysis: theory, simulations, and applications to socioeconomic indices. Working Paper of MEASURE/Evaluation project, No. WP-04-85. [Google Scholar]
- Kvåle G. Olsen BE. Hinderaker SG. Ulstein M. Bergsjø P. Maternal deaths in developing countries: a preventable tragedy. Norsk Epidemiologi. 2005;15:141–9. [Google Scholar]
- McKenzie D. Measuring inequality with assets indicators. Journal of Population Economics. 2005;18:229–60. [Google Scholar]
- Mojarro O. Tapia-Colocia G. Hernández-López MP. Macín-Pérez I. Mexico City: CONAPO; 2003. Mortalidad Materna y Marginación Municipal. La Situación Demográfica de México. Online at: http://www.conapo.gob.mx/publicaciones/sdm/sdm2003/09.pdf, accessed 25 August 2009. [Google Scholar]
- Netzer S. Mallas L. Washington, DC: US Agency for International Development (USAID); 2008. Increasing access to family planning among indigenous Groups in Guatemala. The Health Policy Initiative; pp. 1–18. [Google Scholar]
- Parra PA. Midwives in the Mexican health system. Social Science & Medicine. 1993;37:1321–9. doi: 10.1016/0277-9536(93)90162-w. [DOI] [PubMed] [Google Scholar]
- Rawlings L. Washington, DC: Human Development Network, The World Bank; 2004. A new approach to social assistance: Latin America’s experience with conditional cash transfer programs. Social Protection Discussion Paper Series, No. 416. August 2004. [Google Scholar]
- Replogle J. Training traditional birth attendants in Guatemala. The Lancet. 2007;369:177–8. doi: 10.1016/S0140-6736(07)60090-7. [DOI] [PubMed] [Google Scholar]
- Wilkinson D. Ryan P. Hiller J. Variation in mortality rates in Australia: correlation with Indigenous status, remoteness and socio-economic deprivation. Journal of Public Health Medicine. 2001;23:74–77. doi: 10.1093/pubmed/23.1.74. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) World Health Statistics 2009. 2009. Online at: http://www.who.int/whosis/whostat/EN_WHS09_Full.pdf, accessed 26 August 2009. [Google Scholar]


