Abstract
Background:
Nurses are susceptible to several mental problems, such as fear, stress, and depression due to the COVID-19 pandemic, which affects their emotional well-being. However, resilience plays an important role in mitigating the effects of COVID-19.
Objective:
This study was to examine the mediating role of resilience in the relation between fear, stress, and depression of nurses during COVID-19 health emergencies.
Methods:
A cross-sectional—predictive study was carried out. The variables analyzed were fear, resilience, stress, and depression. A total of 286 nurses from 2 hospitals in the cities of Juliaca and Puno, Peru. Data analyses were performed using structural equation modeling (SEM).
Results:
Analyses showed that the variables were significantly related (P < .01). In addition, a confirmatory analysis of the hypothesized model using structural equation modeling shows that fear and stress are predictors of depression, and that resilience plays a role in mediating the effect of fear on stress (X2 = 534.69, gl = 372, P = .000; TLI = .902, CFI = .910, RMSEA = .039 [95% CI = 0.032-0.046], and SRMR = .065).
Conclusion:
Nurses tend to develop fear, stress, and depression. Resilience reduces the impact of these psychological variables. Hospital management should provide psychological support and training for nurses in coping strategies.
Keywords: stress, depression, fear of COVID-19, resilience in the nursing professional
Introduction
The World Health Organization (WHO), through the 72nd World Health Assembly, has designated 2020 as the International Year of Nursing and Midwifery. 1 On the other hand, since the advent of the COVID-19 pandemic, there have been increased reports of mental illnesses such as fear, stress, and depression among health care workers, particularly nurses. 2 The impact of the pandemic on the mental health of healthcare workers has not only short-term but also long-term consequences. 3
Nurses are among the health care professionals on the front lines in the fight against the COVID-19 pandemic. 4 According to the College of Nurses of Peru, 30% of nurses nationwide are infected by COVID-19. 5 In addition, as of January 19, 2021, more than 7700 have been infected and 90 have died. 6 This situation could negatively impact mental health by causing fear among nurses. 7 Fear is a reality among nurses, who spend more time in the patient environment. A survey conducted during the pandemic on the concerns and experiences of nurses during the initial phase of the pandemic in the United States found that 64% were concerned about the safety of their family and friends; while 85% expressed fear of going to their workplace. 8 Fear of infection and the unknown regarding COVID-19 can contribute to serious mental health problems.9,10 Studies have reported that fear could be considered as one of the main causes of COVID-19 related stress among health care workers. 11 This could be due to a sense of danger, the possibility of self-inoculation of the virus, and concern about infecting family members. 11 Indeed, the fear of becoming infected with a potentially deadly virus is an understandable and expected source of stress. 12
One study showed that the main factors associated with stress in healthcare professionals during the COVID-19 outbreak were concern for personal and family safety and worry about patient mortality. 13 In particular, a study conducted among nurses reported that leaving their children alone and high workload were the main causes of high levels of stress and anxiety. 9 Similarly, a study conducted among nurses in China during the pandemic found that COVID-19-related stress was associated with an increased risk of depression and anxiety. 14 These findings highlight the need to understand the mental health issues nurses face to implement potential interventions accompanied by emotional support and resilience. In addition to stress, nurses also experience a high level of depression, which could have long-term psychological implications. Findings from other studies reported that 94% of health care workers experienced mild to severe depression. 15 Additionally, a study that looked at the mental health of health care workers during the COVID-19 outbreak reported significant levels of depression, anxiety, and insomnia. 16
Resilience, defined as the ability to adapt and respond positively to hardship, trauma, tragedy, and adversity, influences the regulation of negative emotions. 17 When people are exposed to adverse situations, resilience becomes a protective factor in maintaining mental health. Particularly, resilience can have significant impacts on fear, stress, and depression among healthcare professionals due to the COVID-19 pandemic.18,19 In fact, the beneficial effects of resilience lie in its ability to buffer stress and depression. 19 One study showed that resilience plays a mediating role between fear of COVID-19 and depression. 20 Nurses with ample resilience would be able to meet and manage the challenges presented in the clinical environments that occurred during the SARS outbreak.
Although resilience could be considered a protective factor against mental health problems, particularly during this time of health crisis 21 ; however, the role of resilience with respect to stress-related fear and depression due to COVID-19 among healthcare workers remains unknown. Consequently, there is a need to understand the mediating role of resilience in buffering the effects on emotional well-being. Therefore, this study aimed to determine the mediating role of resilience in the relation between fear, stress, and depression of nurses during COVID-19 health emergencies.
Materials and Methods
Study Design
A cross-sectional—predictive design study was carried out. 22 Variables of interest, such as fear, resilience, stress, and depression, were considered.
Study Population
Participants were selected through the non-probability convenience sampling method. We analyzed the effect size which considers the number of observed and latent variables in the model, the anticipated effect size (λ = .3), the desired statistical significance (α = .05), and the statistical power level (1−β = .95) which considers a minimum recommended sample of 207; however, 286 nurses from 2 hospitals in the city of Juliaca and Puno, Peru, were considered. The age of the participants ranged from 21 to 69 years (mean age = 43.88 years). In terms of the academic levels attained by the participants, 68.2% had a specialty related to their professional career, 15% had a Master’s degree, and 2.8% had a doctorate degree. Finally, 38.5% were single and 35% were married.
Ethical Aspects and Procedures
Ethical procedures followed the standards established in the 1964 Declaration of Helsinki and subsequent modifications. Prior to the application of the questionnaire, the study obtained the approval of the Ethics Committee of a Peruvian university: Registration number: 2021-CE-EPG-000001. Due to the state of emergency for COVID-19, the questionnaire was provided online using Google forms and was sent publicly via e-mails and WhatsApp, preserving at all times the anonymity of the participants. Only employees who agreed to participate in the study on a voluntary basis responded to the questionnaire. Participants who agreed to respond to the questionnaire received information about the objectives of the study with a commitment in return to respect their privacy and responsibility for the use of the data for research purposes only. In addition, they were informed of their voluntary withdrawal at any time during the data collection process. Only the records of persons who agreed to participate voluntarily and signed the informed consent form were included. The time to administer the questionnaire individually was 15 min.
Instruments
COVID-19 pandemic-related perceived stress scale (EEP-10-C) 23 : The EEP-10-C is composed of 10 items and presents 5 response options (0 = never, 4 = always). It allows obtaining a score >25 where a higher value expresses greater stress. Cronbach’s alpha was considered between .65 and .86.
Patient Health Questionnaire-2(PHQ-2) 24 : The PHQ-2 is a short version of the 9-item Patient Health Questionnaire developed to assess depressive symptoms during the past 2 weeks using 2 items: (1) feeling discouraged, depressed, or hopeless, and (2) little interest or pleasure in doing things. The Spanish version was used, 25 presenting 4 response options with scores ranging from 0 to 3 (0 = not at all, 1 = several days, 2 = more than half of the days, and 3 = almost every day). The total score is in the range of 0 to 6, where higher scores indicate greater depressive symptoms. Internal consistency by means of coefficient alpha (α = .75).
Fear of COVID-19 Scale (FCV-19S) 26 : This is a self-administered scale that assesses fear of COVID-19. The 7-item Spanish version was used, 27 which presents optimal internal consistency (ω > .89 and α > .83). It has a Likert scale from 1 (Strongly disagree) to 5 (Strongly agree). The higher the score, the greater the fear of COVID-19.
Connor-Davidson Resilience Scale (CD-RISC) 28 : To evaluate resilience, the Spanish version of the scale was used, 29 which has 10 items and 5-point Likert-type response categories (0 = totally disagree to 4 = totally agree). The internal consistency of the scale was adequate (Cronbach’s alpha = .87).
Statistical Analysis
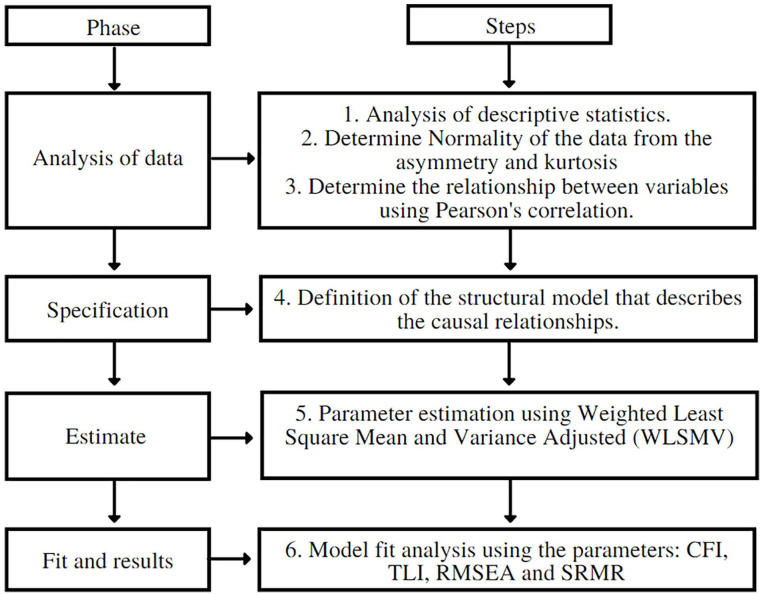
Figure 1 shows the flow of the procedure for the design of a structural equation model (SEM). Descriptive statistics were calculated and the normality of the items was evaluated considering the skewness and kurtosis coefficients (>1.5). The correlations of the variables were analyzed using the Pearson correlation statistic.
Figure 1.
Procedural flow for designing an SEM.
A predictive model where fear of COVID-19 and stress predict depression was analyzed through structural equation modeling (SEM). Because it is an analytical technique that allows examining causal and complex relationships, 30 and considers factor analysis and linear regression modeling simultaneously to explore relationships between constructs. 31 In addition, resilience was considered as a mediating variable. The Weighted Least Square Mean and Variance Adjusted (WLSMV) estimation method was used for this analysis. Moreover, the goodness-of-fit indices of the model were evaluated according to the proposals of Escobedo Portillo et al 32 and Kline. 33 Comparative fit indexes (CFI) and Tucker-Lewis index (TLI) ranging between .90 and .95 would indicate an acceptable fit and values above .95 would indicate an adequate fit. Root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR) indices with values between .05 and .08 would indicate an acceptable fit and values below .05 would indicate an adequate fit.34,35 Statistical analyses were performed using R (version 4.1.1) and R Studio programs.
Results
The descriptive analyses show that 38.5% of the participants were single and 35.0% were married. 68.2% reported that they were pursuing specialization studies. 44.4% had a history of having been infected with COVID-19. Regarding the health condition of the participants, 87.8% did not get sick with COVID-19 and more than 61.5% had a salary higher than $3000.00 (Table 1).
Table 1.
Sociodemographic Characteristics of the Nurses.
| Variable | N | % |
|---|---|---|
| Marital status | ||
| Single | 110 | 38.5 |
| Married | 100 | 35.0 |
| Cohabitant | 57 | 19.9 |
| Divorced | 9 | 3.1 |
| Widower | 10 | 3.5 |
| Academic degree | ||
| Bachelor | 40 | 14.0 |
| Master | 43 | 15.0 |
| Doctor | 8 | 2.8 |
| Specialty | 195 | 68.2 |
| History of COVID-19 infection | ||
| Yes | 127 | 44.4 |
| No | 159 | 55.6 |
| Health condition | ||
| Cardiovascular disease | 20 | 7.0 |
| Diabetes | 7 | 2.4 |
| Respiratory disease | 7 | 2.4 |
| Cancer | 1 | .3 |
| None | 251 | 87.8 |
| Financial income | ||
| <$1700.00 | 76 | 26.6 |
| $1700.00-3000.00 | 34 | 11.9 |
| >$3000.00 | 176 | 61.5 |
Descriptive Analysis
The results show the descriptive data of the variables under study. The normality analyses of data through the Kolmogorov-Smirnov test yielded values of P < .05 and for this it is assumed that the data do not conform to a normal distribution, therefore, the study variables can be considered as nonparametric variables (Table 2).
Table 2.
Descriptive and Analysis of the Distribution of the Study Variables.
| Variable | M | SD | 95% CI (LL-UL) | K-S | P-value | |
|---|---|---|---|---|---|---|
| Stress | 15.24 | 5.82 | 14.57 | 15.92 | 0.06 | .01 |
| Depression | 1.20 | 1.41 | 1.03 | 1.36 | 0.28 | .00 |
| Fear of COVID-19 | 17.96 | 5.86 | 17.28 | 18.64 | 0.06 | .01 |
| Resilience | 39.06 | 5.60 | 38.41 | 39.71 | 0.10 | .00 |
Abbreviations: CI, Confidence Interval; K-S, Kolmogorov-Smirnov; LL, Lower Limit; M, mean; SD, standard deviation; UL, Upper Limit.
Correlation analysis (Table 3) yielded that high stress scores correlated with high depression scores (ρ = .535, P < .01) and fear of COVID-19 (ρ = .549, P < .01), and correlated with low resilience scores (ρ = −.410, P < .01). Furthermore, it was observed that high depression scores correlated with high COVID-19 fear scores (ρ = .528, P < .01) and with low resilience scores (ρ = −.236, P < .01). Finally, high COVID-19 fear scores correlated with low resilience scores (ρ = −.285, P < .01).
Table 3.
Análisis de correlaciones entre las variables de estudio.
| 1 | 2 | 3 | 4 | α | |
|---|---|---|---|---|---|
| 1. Stress | 1.000 | .85 | |||
| 2. Depression | .535** | 1.000 | .80 | ||
| 3. Fear of COVID-19 | .549** | .528** | 1.000 | .91 | |
| 4. Resilience | −.410** | −.236** | −.285** | 1.000 | .86 |
The correlation is significant at the .01 level (bilateral).
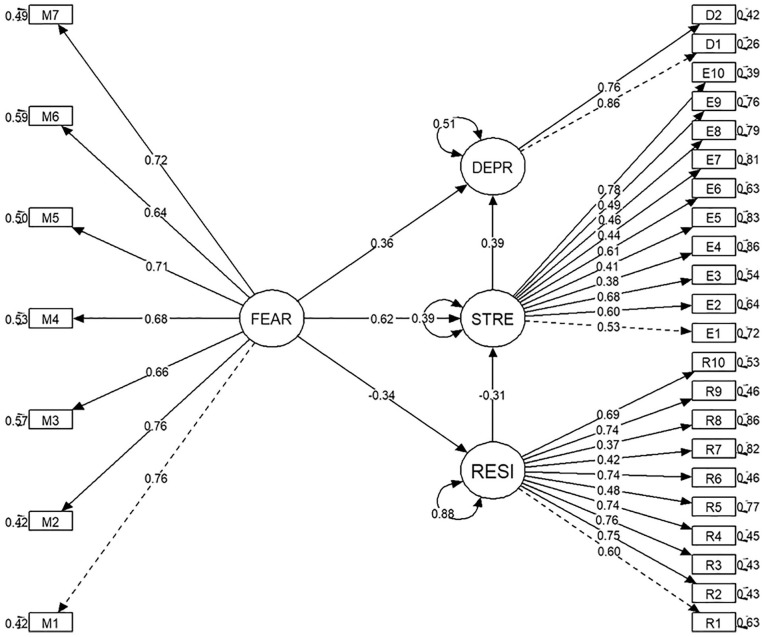
For the variables that presented significant correlations, a predictive model of stress and depression was evaluated using structural equation modeling (Figure 2). Fear of COVID-19 and resilience were considered as predictor variables. The results showed that fear of COVID-19 was a variable that negatively influenced resilience (β = −.34, P < .001), but in turn positively influenced stress (β = .62, P < .001) and depression (β = .36, P < .001). Similarly, a negative influence of resilience to stress was observed (β = −.31, P < .001). However, a decrease in the effect of fear of COVID-19 on stress was observed. Likewise, stress had a positive influence on depression (β = .39, P < .001). Therefore, resilience can be considered as a variable that plays a mediating role in the relationship between fear of COVID-19 and stress. While fear of COVID-19 and stress are predictors of depression, resilience plays a role in mediating the effect of fear on stress. This analysis presents adequate goodness-of-fit indices indicating that the structural model adequately fits the hypothesized model (X2 = 534.69, gl = 372, P = .000; TLI = .902, CFI = .910, RMSEA = .039 [95% CI = 0.032-0.046], and SRMR = .065).
Figure 2.
Structural equation model. Goodness-of-fit indices (X2 = 534.69, gl = 372, P = .000; TLI = .902, CFI = .910, RMSEA = .039 [95% CI = 0.032-0.046], and SRMR = .065).
Discussion
During the COVID-19 pandemic, nurses were exposed to high levels of fear and stress leading to depressive disorders. As a result, work, psychosocial, and occupational performance have been compromised, affecting quality of life. In this situation, the concept of resilience has become important in this scenario of health crisis. 36
The findings of this study support the hypothesized model and provide evidence on fear and psychological factors in nurses. Specifically, this study reports on the mediating role of resilience in relation to fear of COVID-19, stress, and depression. As predicted, correlation analyses indicated that nurses with a high fear of COVID-19 tend to have higher stress. These results are consistent with the literature, as fear of infection contributes to greater stress at work, due to the high risk of becoming infected, infecting family members, friends, and colleagues.37,38 Likewise, the findings also indicated that fear was related to depression, as in previous studies. 39 In other words, the higher the frequency of fear, the stronger the association with depression.2,40 This is because nurses have worked with COVID-19 patients are more vulnerable to experiencing depression. 41
Previous studies and the results of the current study showed that nurses’ fear of COVID-19 was negatively related to resilience. 42 Resilience was also associated with work stress and anxiety induced during the COVID-19 epidemic. 43 Increased stress leads to an increased risk of depression as shown by our results. 44 Previous studies indicate that lower levels of resilience are associated with higher levels of stress. 45 This is because resilience acts as a personal resource for reducing the negative effects of stress and is an important factor against the symptoms of depression. 44 In addition, resilience may buffer the effect of fear and a wide range of posttraumatic outcomes. The findings indicated that resilience functions as a moderator in relationship to fear, stress, and depression, meaning that fear has a significant positive impact on stress, and depression in conditions of low resilience. In sum, resilience acts as a psychological force to preserve mental health.26,46 Therefore, there is a need to maximize support for nurses with high levels of stress and depression. 47 It is also suggested that, despite fear of infection, one of the reasons for staying and accepting risks in a resilient or altruistic manner is a sense of commitment and awareness as a nursing professional. 48 In view of this, to mitigate the depression and fear of nurses, it is important to improve their working conditions, favoring the allocation of resources, and better living conditions during the COVID-19 pandemic.
The contribution of the study is to clarify the interaction approaches between fear, resilience, and psychological factors. Resilience protects against levels of fear, stress, and depression; however, more research is needed to explore these long-term effects during the pandemic. Unfortunately, the COVID-19 crisis is a constant threat to the work of nurses. It is important to consider reducing the workload, increasing the number of nursing staff, and improving financial conditions. A better labor system that includes social protection for nurses should be prepared. As most nurses have direct contact with patients, they will have higher levels of stress, anxiety, and depression. Therefore, it is important to conduct ongoing training on how to deal with the constant psychological threats to which they are subjected. Since it is important to safeguard the psychological well-being of health care workers, one must be psychologically prepared to mitigate the ravages of COVID-19. It is important to propose interventions for the early identification of fear, stress, and anxiety to favor later preventive effects.
Limitations
The findings of the study should be interpreted considering some limitations. The study was conducted in a single specific region of Peru, so it is necessary to extend the sample to other hospitals nationwide to make generalizations to other hospitals. The health restriction and surveillance and control plans on workers with exposure in hospitals made it difficult for the researchers to reach the target population and collect the data, as they could not easily access the online survey. The study was cross-sectional and a survey questionnaire was used for data collection, so causal relationships cannot be revealed. Longitudinal designs could be used in future research, allowing for broader follow-up, greater benefits, and applications. In addition, the Neyman bias (incidence-prevalence) was present in the study given the time lapse between exposure and selection of participants. This eventuality could greatly reduce the fact that participants with higher anxiety could be absent due to lack of acceptance or desertion. Therefore, the study results tend to show a distorted exposure frequency.49,50
Conclusions
The pandemic has contributed to fear, stress, and depression in nurses, negatively affecting their emotional well-being, work activities, and quality of care. Resilience plays an important role in the care and protection of nurses’ mental health against the effect of psychological distress during health crisis by COVID-19. The present study contributes to the current literature by suggesting that resilience plays a crucial role in mitigating psychological effects. Hospital administration should prioritize the implementation of interventions in the reduction of fear, stress, and depression and expand knowledge about resilience in nurses.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Sonia Chura  https://orcid.org/0000-0003-4072-4946
https://orcid.org/0000-0003-4072-4946
Jacksaint Saintila  https://orcid.org/0000-0002-7340-7974
https://orcid.org/0000-0002-7340-7974
Rut Mamani  https://orcid.org/0000-0002-7038-0155
https://orcid.org/0000-0002-7038-0155
Wilter C. Morales-García  https://orcid.org/0000-0003-1208-9121
https://orcid.org/0000-0003-1208-9121
References
- 1. Organización Mundial de la Salud (OMS). Año Internacional del Personal de Enfermería y de Partería. OMS; 2020. [Google Scholar]
- 2. De los Santos JAA, Labrague LJ. The impact of fear of COVID-19 on job stress, and turnover intentions of frontline nurses in the community: a cross-sectional study in the Philippines. Traumatology (Tallahass Fla). 2021;27(1):52-59. doi: 10.1037/TRM0000294 [DOI] [Google Scholar]
- 3. Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11-17. doi: 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gross JV, Mohren J, Erren TC. COVID-19 and healthcare workers: a rapid systematic review into risks and preventive measures. BMJ Open. 2021;11(1):e042270. doi: 10.1136/BMJOPEN-2020-042270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Colegio de Enfermeros del Perú. Actualidad & noticias [Web]. Lima-Perú: CEP;2022. [Google Scholar]
- 6. Diario Gestion. “Más de 7.700 enfermeras fueron contagiadas con COVID-19 y 15 están en UCI”, según decana del Colegio de Enfermeros Coronavirus Perú segunda ola nndc | PERU | GESTIÓN. 2021. [Google Scholar]
- 7. Fernandes MA, Alves A, Ribeiro A. Salud mental y estrés ocupacional en trabajadores de la salud a la primera línea de la pandemia de COVID-19. Rev Cuidarte. 2020;11(2):e1222. doi: 10.15649/CUIDARTE.1222 [DOI] [Google Scholar]
- 8. American Nurses Association. Survey: Nurses fear going to work due to lack of protection from virus more than 32k Nurses share experience from the Front Lines [Web]. Maryland-Estados Unidos: ANA; 2020. [Google Scholar]
- 9. Mo Y, Deng L, Zhang L, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. 2020;28(5):1002-1009. doi: 10.1111/jonm.13014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jackson D, Bradbury-Jones C, Baptiste D, et al. Life in the pandemic: some reflections on nursing in the context of COVID-19. J Clin Nurs. 2020;29(13-14):2041-2043. doi: 10.1111/jocn.15257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wu W, Zhang Y, Wang P, et al. Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. J Med Virol. 2020;92(10):1962-1970. doi: 10.1002/jmv.25914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Arnetz JE, Goetz CM, Arnetz BB, Arble E. Nurse reports of stressful situations during the COVID-19 pandemic: qualitative analysis of survey responses. Int J Environ Res Public Health. 2020;17(21):1-12. doi: 10.3390/ijerph17218126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Parums DV. Editorial: the National COVID Cohort Collaborative Consortium combines population data with machine learning to evaluate and predict risk factors for the severity of COVID-19. Med Sci Monit. 2021;27:e934171. doi: 10.12659/MSM.934171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tu ZH, He JW, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study. Medicine. 2020;99(26):e20769. doi: 10.1097/MD.0000000000020769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aly HM, Nemr NA, Kishk RM, Elsaid NMAB. Stress, anxiety and depression among healthcare workers facing COVID-19 pandemic in Egypt: a cross-sectional online-based study. BMJ Open. 2021;11(4):e045281. doi: 10.1136/bmjopen-2020-045281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Global Health. 2020;16(1):89. doi: 10.1186/s12992-020-00621-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shatté A, Pulla V, Shatté A, Warren S. Perspectives on Coping and Resilience. Authors Press Books; 2012. [Google Scholar]
- 18. Shatté A, Perlman A, Smith B, Lynch WD. The positive effect of resilience on stress and business outcomes in difficult work environments. J Occup Environ Med. 2017;59(2):135-140. doi: 10.1097/JOM.0000000000000914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Barzilay R, Moore TM, Greenberg DM, et al. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry. 2020;10(1):291. doi: 10.1038/s41398-020-00982-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chen Y, Liu Y, Zhang Y, Li Z, Zhou T. The effect of fear of the COVID-19 on depression among Chinese outbound students studying online in China amid the COVID-19 pandemic period: the Role of resilience and social support. Front Psychol. 2021;12:750011. doi: 10.3389/fpsyg.2021.750011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kumar S, Lee NK, Pinkerton E, Wroblewski KE, Lengyel E, Tobin M. Resilience: a mediator of the negative effects of pandemic-related stress on women’s mental health in the USA. Arch Womens Ment Health. 2022;25:137-146. doi: 10.1007/s00737-021-01184-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ato M, López-García JJ, Benavente A. Un sistema de clasificación de los diseños de investigación en psicología. An Psicol. 2013;29(3):1038-1059. doi: 10.6018/analesps.29.3.178511 [DOI] [Google Scholar]
- 23. Campo-Arias A, Pedrozo-Cortés MJ, Pedrozo-Pupo JC. Escala de estrés percibido relacionado con la pandemia de COVID-19: una exploración del desempeño psicométrico en línea. Rev Colomb Psiquiatr. 2020;49(4):229-230. doi: 10.1016/J.RCP.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi: 10.1046/J.1525-1497.2001.016009606.X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Baños-Chaparro J, Ynquillay-Lima P, Lamas F, Fuster FG. Evidencias psicométricas del Patient Health Questionnarie-2 para la evaluación de síntomas depresivos en adultos peruanos. Rev Ciencias Médicas Pinar del Río. 2021;25(5):1-9. [Google Scholar]
- 26. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. Published online March 27, 2020. doi: 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Huarcaya-Victoria J, Villarreal-Zegarra D, Podestà A, Luna-Cuadros MA. Psychometric properties of a Spanish version of the fear of COVID-19 scale in general population of Lima, Peru. Int J Ment Health Addict. 2022;20:249-262. doi: 10.1007/s11469-020-00354-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Connor KM, Davidson JR. Development of a new Resilience scale: the Connor-Davidson Resilience scale (CD-RISC). Depress Anxiety. 2003;18(2):76-82. doi: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 29. Soler Sánchez MI, Meseguer de, Pedro M, García Izquierdo M. Propiedades psicométricas de la versión española de la escala de resiliencia de 10 ítems de Connor-Davidson (CD-RISC 10) en una muestra multiocupacional. Rev Latinoam Psicol. 2016;48(3):159-166. doi: 10.1016/j.rlp.2015.09.002 [DOI] [Google Scholar]
- 30. Kwok O-M, Cheung MWL, Jak S, Ryu E, Wu JY. Editorial: recent advancements in structural equation modeling (SEM): from both methodological and application perspectives. Front Psychol. 2018;9:1936. doi: 10.3389/fpsyg.2018.01936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Williams LJ, Vandenberg RJ, Edwards JR. 12 structural equation modeling in management research: a guide for improved analysis. Acad Manag Ann. 2009;3(1):543-604. doi: 10.5465/19416520903065683 [DOI] [Google Scholar]
- 32. Escobedo Portillo MT, Hernández Gómez JA, Estebané Ortega V, Martínez Moreno G. Modelos de ecuaciones estructurales: características, fases, construcción, aplicación y resultados. Cienc Trab. 2016;18(55):16-22. doi: 10.4067/s0718-24492016000100004 [DOI] [Google Scholar]
- 33. Kline RB. Principles and Practice of Structural Equation Modeling. 4th ed. Guilford Press; 2016. [Google Scholar]
- 34. Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. 4th ed. Taylor & Francis; 2016. [Google Scholar]
- 35. Kline RB. Principles and Practice of Structural Equation Modeling. Cuarta ed. Guilford Press; 2016. [Google Scholar]
- 36. Fox S, Lydon S, Byrne D, Madden C, Connolly F, O’Connor P. A systematic review of interventions to foster physician resilience. Postgrad Med J. 2018;94(1109):162-170. doi: 10.1136/postgradmedj-2017-135212 [DOI] [PubMed] [Google Scholar]
- 37. Tayyib NA, Alsolami FJ. Measuring the extent of stress and fear among registered nurses in KSA during the COVID-19 outbreak. J Taibah Univ Med Sci. 2020;15(5):410-416. doi: 10.1016/j.jtumed.2020.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lorente L, Vera M, Peiró T. Nurses’ stressors and psychological distress during the COVID-19 pandemic: the mediating role of coping and resilience. J Adv Nurs. 2021;77(3):1335-1344. doi: 10.1111/JAN.14695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. 2021;16(3):e0247679. doi: 10.1371/journal.pone.0247679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lu MY, Ahorsu DK, Kukreti S, et al. The prevalence of post-traumatic stress disorder symptoms, sleep problems, and psychological distress among COVID-19 frontline healthcare workers in Taiwan. Front Psychiatry. 2021;12:705657. doi: 10.3389/fpsyt.2021.705657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Abid M, Riaz M, Bano Z, Parveen T, Umar Fayyaz M, Sadia Qureshi H. Association between fear of COVID-19 and emotional distress in nurses with mediating role of socio-demographic features. Front Psychol. 2021;12:734623. doi: 10.3389/fpsyg.2021.734623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hu D, Kong Y, Li W, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMedicine. 2020;24:100424. doi: 10.1016/j.eclinm.2020.100424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hong Y, Lee J, Lee HJ, et al. Resilience and work-related stress may affect depressive symptoms in nursing professionals during the COVID-19 pandemic era. Psychiatry Investig. 2021;18(4):357-363. doi: 10.30773/pi.2021.0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yörük S, Güler D. The relationship between psychological resilience, burnout, stress, and sociodemographic factors with depression in nurses and midwives during the COVID-19 pandemic: a cross-sectional study in Turkey. Perspect Psychiatr Care. 2021;57(1):390-398. doi: 10.1111/ppc.12659 [DOI] [PubMed] [Google Scholar]
- 45. Li ZS, Hasson F. Resilience, stress, and psychological well-being in nursing students: a systematic review. Nurse Educ Today. 2020;90:104440. doi: 10.1016/j.nedt.2020.104440 [DOI] [PubMed] [Google Scholar]
- 46. Yıldırım M, Güler A. Coronavirus anxiety, fear of COVID-19, hope and resilience in healthcare workers: a moderated mediation model study. Health Psychol Rep. 2021;9(4):388-397. doi: 10.5114/HPR.2021.107336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Roberts NJ, McAloney-Kocaman K, Lippiett K, Ray E, Welch L, Kelly C. Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respir Med. 2021;176:106219. doi: 10.1016/j.rmed.2020.106219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Varasteh S, Esmaeili M, Mazaheri M. Factors affecting Iranian nurses’ intention to leave or stay in the profession during the COVID-19 pandemic. Int Nurs Rev. Published online September 25, 2021. doi: 10.1111/inr.12718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Delgado-Rodriguez M. Bias. J Epidemiol Community Health. 2004;58(8):635-641. doi: 10.1136/JECH.2003.008466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Schwaid G. Epidemiology and biostatistics. Board Rev Prev Med Public Heal. 2017;2017:79-185. doi: 10.1016/B978-0-12-813778-9.00003-7 [DOI] [Google Scholar]