Abstract
Background
Noninvasive assessment of pulmonary artery systolic pressure by Doppler echocardiography (sPAPECHO) has been widely adopted to screen for pulmonary hypertension (PH), but there is still a high proportion of overestimation or underestimation of sPAPECHO. We therefore aimed to explore the accuracy and influencing factors of sPAPECHO with right heart catheterization (RHC) as a reference.
Methods
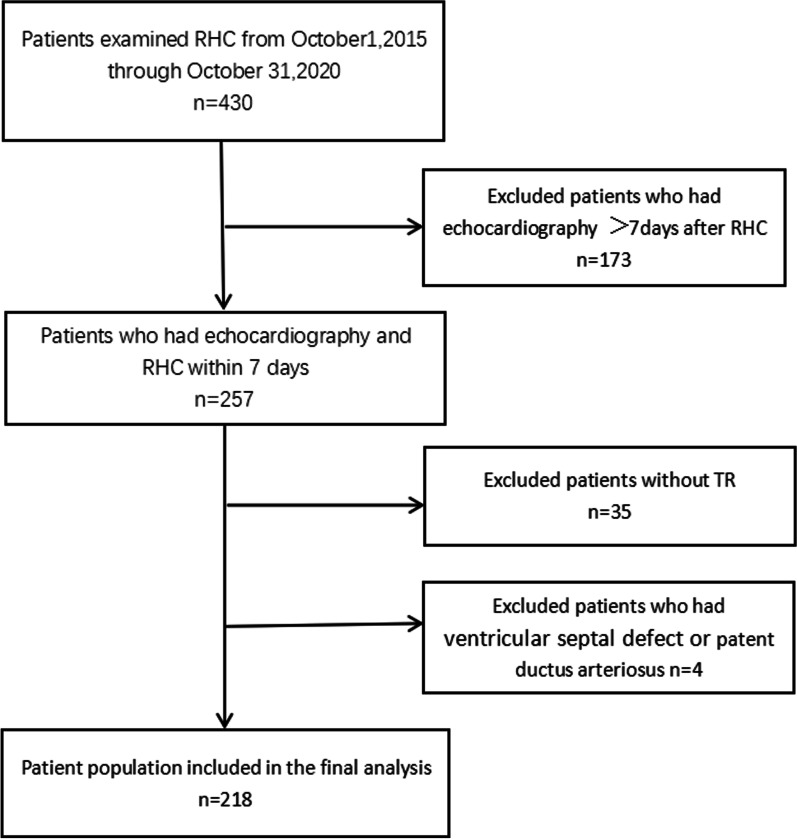
A total of 218 highly suspected PH patients who underwent RHC and echocardiography within 7 days were included. The correlation and consistency between tricuspid regurgitation (TR)-related methods and RHC results were tested by Pearson and Bland–Altman methods. TR-related methods included peak velocity of TR (TR Vmax), TR pressure gradient (TR-PG), TR mean pressure gradient (TR-mPG), estimated mean pulmonary artery pressure (mPAPECHO), and sPAPECHO. With mPAP ≥ 25 mm Hg measured by RHC as the standard diagnostic criterion of PH, the ROC curve was used to compare the diagnostic efficacy of sPAPECHO with other TR-derived parameters. The ratio (sPAPECHO–sPAPRHC)/sPAPRHC was calculated and divided into three groups as follows: patients with an estimation error between − 10% and + 10% were defined as the accurate group; patients with an estimated difference greater than + 10% were classified as the overestimated group; and patients with an estimation error greater than − 10% were classified as the underestimated group. The influencing factors of sPAPECHO were analyzed by ordinal regression analysis.
Results
sPAPECHO had the highest correlation coefficient (r = 0.781, P < 0.001), best diagnostic efficiency (AUC = 0.98), and lowest bias (mean bias = 0.07 mm Hg; 95% limits of agreement, − 32.08 to + 32.22 mm Hg) compared with other TR-related methods. Ordinal regression analysis showed that TR signal quality, sPAPRHC level, and pulmonary artery wedge pressure (PAWP) affected the accuracy of sPAPECHO (P < 0.05). Relative to the good signal quality, the OR values of medium and poor signal quality were 0.26 (95% CI: 0.14, 0.48) and 0.23 (95% CI: 0.07, 0.73), respectively. Compared with high sPAPRHC level, the OR values of low and medium sPAPRHC levels were 21.56 (95% CI: 9.57, 48.55) and 5.13 (95% CI: 2.55, 10.32), respectively. The OR value of PAWP was 0.94 (95% CI: 0.89, 0.99). TR severity and right ventricular systolic function had no significant effect on the accuracy of sPAPECHO.
Conclusions
In this study, we found that all TR-related methods, including sPAPECHO, had comparable and good efficiency in PH screening. To make the assessment of sPAPECHO more accurate, attention should be paid to TR signal quality, sPAPRHC level, and PAWP.
Background
Right heart catheterization (RHC) is recognized as the gold standard for measuring pulmonary artery pressure, but its invasiveness limits its general applicability. Doppler echocardiography (DE) can noninvasively assess pulmonary artery pressure by peak velocity of tricuspid regurgitation (TR Vmax) and its derived parameters, including TR pressure gradient (TR-PG), TR mean pressure gradient (TR-mPG), estimated mean pulmonary artery pressure (mPAPECHO), and pulmonary artery systolic pressure (sPAPECHO). The current guidelines recommend TR Vmax to avoid additional error in the estimated right atrial pressure (RAP) [1]. Furthermore, mPAP has been found to be superior to TR Vmax in identifying pulmonary hypertension (PH) [2]. As the most well-adopted approach in PH screening, sPAPECHO has also been shown to be a reliable method [3]; however, it has not yet been examined whether sPAPECHO is superior to other parameters in determining the probability of PH. sPAPECHO can also provide valuable information for evaluating treatment response and even predicting prognosis [4, 5]; however, there is still a high proportion of overestimation or underestimation of sPAPECHO [6]. To evaluate PH patients’ condition appropriately and avoid too invasive examination, we need to understand situations in which sPAPECHO is under/overestimated. Based on clinical experience and review of previous literature, we assumed that right ventricular systolic function, pulmonary artery pressure level, TR severity, and signal quality would affect the accuracy of sPAPECHO. In addition, as an important parameter to distinguish pre- and post-capillary PH, pulmonary artery wedge pressure (PAWP) was also included in the analysis to examine whether there would be any difference in the accuracy of sPAPECHO. Therefore, the first aim of this study was to compare the efficiency of sPAPECHO and other parameters in PH screening, while the second aim was to find influencing factors that account for the inaccuracy of sPAPECHO.
Methods
Between October 2015 and October 2020, a total of 430 patients admitted to our center with known or suspected PH were evaluated. The inclusion criteria were age ≥ 18 years and the interval between echocardiography and RHC ≤ 7 days. The exclusion criteria were as follows: lack of TR, pulmonary artery stenosis or right ventricular outflow tract stenosis, poor image quality not suitable for analysis, ventricular septal defect, or patent ductus arteriosus. Patients’ demographic and clinical data were obtained from the electronic medical records. The institutional review board of the China–Japan Friendship Hospital waived the need for written informed consent as the study involved the retrospective analysis of clinically acquired data. The data underlying this article will be shared upon a reasonable request to the corresponding author.
Clinical data
Baseline assessment of the eligible patients included WHO functional class, the level of N-terminal pro B-type natriuretic peptide (NT-proBNP), and a 6-min walk test (6MWT).
RHC
Hemodynamic measurements were performed with a 7F Swan-Ganz catheter Philips Allura X-PER FD20 flat-plate angiography system (Baxter Inc.). The system was zeroed and referenced at patients’ heart level as previously described [7]. Right atrial pressure (RAP), pulmonary systolic artery pressure (sPAPRHC), and PAWP were recorded at end-expiration at baseline over at least three heart cycles. Cardiac output (CO) was obtained using Fick’s method. Pulmonary vascular resistance (PVR), cardiac index, stroke volume, pulse pressure, and diastolic pressure gradient were calculated using standard formulas. Pulmonary artery pressure was classified into low, medium, and high levels according to the tertiles of sPAPRHC.
Echocardiography
Echocardiographic images were acquired using a GE Vivid E95 machine (GE Healthcare, General Electric Healthcare) equipped with M5S phased-array transducers. Analysis was performed independently by two blinded investigators using EchoPAC software (GE Healthcare version 201). Two-dimensional echocardiography and Doppler echocardiography (DE) were performed based on current guidelines. TR-PG was calculated from the TR Vmax obtained from continuous-wave Doppler by the simplified Bernoulli equation: TR-PG = 4 (TR Vmax)2. TR-mPG was obtained by tracing the time–velocity integral of TR. sPAPECHO and mPAPECHO were calculated by adding the estimated RAP to TR-PG and TR-mPG, respectively. RAP was divided into three categories (3, 8, and 15 mm Hg) based on the inferior vena cava (IVC) diameter and its respiratory variation [1]. The ratio (sPAPECHO–sPAPRHC)/sPAPRHC was calculated and divided into three groups as follows: patients with an estimation error between − 10% and + 10% were defined as the accurate group; patients with an estimated difference greater than + 10% were classified as the overestimated group; and patients with an estimation error greater than − 10% were classified as the underestimated group. The severity of TR was classified into three grades by comprehensively evaluating the regurgitation jet area and vena contracta (VC) width. The mild group was defined as jet area < 5 cm2, VC TR ≤ 3 mm; the moderate group as jet area 5–10 cm2, 3 mm < VC TR < 7 mm; and the severe group as jet area > 10 cm2, VC TR ≥ 7 mm. TR signal quality was classified into three types according to the extension of the signal for more than half of the systole and well-defined border. Good signal quality was defined as the one that met both criteria. Medium signal quality met only one of these criteria, while poor signal quality did not meet any of the criteria [8] (Fig. 1). RV systolic function was assessed using multiple parameters, including RV wall thickness (RV WT), tricuspid annular plane systolic excursion (TAPSE), systolic annular tissue velocity of the lateral tricuspid annulus (S’), and RV fractional area change (FAC). All of these parameters were repeatedly measured and averaged. To determine the reproducibility of sPAPECHO measurements, a total of 34 randomly selected examinations were analyzed twice by the first investigator at a 1-week interval and once by the second investigator.
Fig. 1.
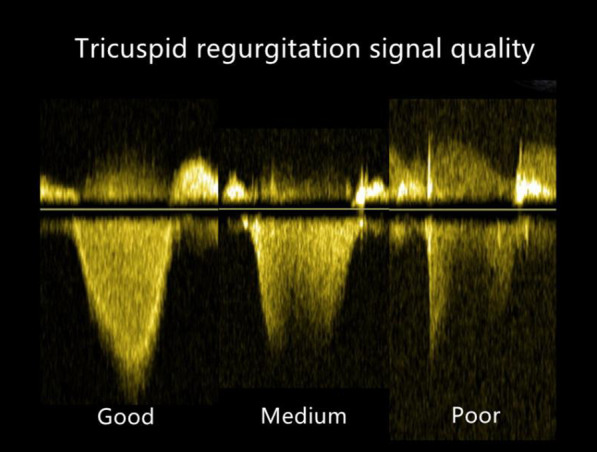
Classification of the TR signal quality using continuous-wave Doppler. Good signal quality, complete envelope; Medium signal quality, partial envelope; Poor signal quality, unreliable envelope or no signal
Statistical analysis
Standard statistical software (SPSS version 26 for Windows, SPSS, Chicago, IL, USA) was used for the statistical analysis. Data are expressed as mean ± standard deviation for quantitative variables with normal distribution, or as median (interquartile range) for variables not complying with normal distribution. The correlation and consistency between TR-derived parameters and RHC results were tested by Pearson and Bland–Altman methods. With mPAP ≥ 25 mm Hg measured by RHC as the standard diagnostic criterion of PH, a receiver operating characteristic (ROC) curve was used to compare the diagnostic efficacy of sPAPECHO and other TR-related methods. The influencing factors of sPAPECHO were analyzed by ordinal regression analysis. The intraclass correlation coefficient was used to determine inter- and intra-observer reproducibility for sPAPECHO from 34 randomly selected patients using an identical cine-loop for each view. For all statistical tests, a P value < 0.05 was used to indicate significance.
Results
Patients’ characteristics
A total of 218 patients were finally identified and analyzed, as shown in Fig. 2. Baseline demographic and clinical characteristics are provided in Table 1. The mean age of the patients was 50.9 ± 13.3 years; 40.3% of them were men; 197 (90.4%) patients had PH. None of the patients experienced major cardiac events between DE and RHC examinations. Table 2 lists the DE and RHC variables grouped by estimated accuracy.
Fig. 2.
Flow chart of patient screening
Table 1.
Clinical and demographic characteristics
| Variables | Value |
|---|---|
| Age (years) | 50.9 ± 13.3 |
| Males (%) | 90 (41.3) |
| BMI | 1.67 (1.57, 1.84) |
| Systolic BP (mmHg) | 120 (108, 132) |
| Diastolic BP (mmHg) | 77 (70, 87) |
| Heart rate (bpm) | 76 (68.65, 80) |
| Interval between TTE and RHC, days | 2.5 (1, 5) |
| NT-pro BNP (pg/ml) | 451 (175, 1043) |
| 6 M WT (m) | 365.5 ± 104.6 |
| WHO functional class | |
| I Class (%) | 20 (9.2) |
| II Class (%) | 93 (42.7) |
| III Class (%) | 89 (40.8) |
| IV Class (%) | 16 (7.3) |
| PH (n) | 197 (90.4%) |
| Idiopathic, heritable, drug and toxic induced | 37 |
| Associated with Connective tissue disease | 25 |
| Portal hypertension | 2 |
| Congenital heart disease | 8 |
| PH due to left heart disease | 6 |
| PH due to lung disease and/or hypoxia | 6 |
| Chronic thromboembolic PH | 95 |
| PH with unclear and/or multifactorial mechanisms | 13 |
| Pulmonary veno-occlusive disease and/or pulmonary capillary haemangiomatosis | 5 |
| Non-PH (n) | 21 (9.6%) |
Values are presented as mean ± SD, median (IQR), or n (%)
BMI body mass index; TTE, transthoracic echocardiography; RHC right heart catheterization; BP blood pressure; NT-pro BNP N-terminal pro B-type natriuretic peptide; 6 M WT 6-min walk test; PH pulmonary hypertension
Table 2.
Univariable and multivariable ordered analysis for accuracy of sPAPECHO
| Variables | Overestimation (n = 79) | Accurate (n = 81) | Underestimation (n = 58) | Univariable analysis | Multivariable analysis | ||
|---|---|---|---|---|---|---|---|
| P | OR (95% CI) | P | OR (95% CI) | ||||
| Echocardiographic parameters | |||||||
| RAD (mm) | 49.1 ± 10.2 | 49.9 ± 11.1 | 49.4 ± 10.0 | 0.816 | 0.997 (0.974, 1.021) | ||
| RVDD (mm) | 45.4 ± 7.3 | 46.2 ± 7.6 | 46.5 ± 6.5 | 0.323 | 0.984 (0.952,1.016) | ||
| RV WT (mm) | 5.3 ± 1.5 | 5.4 ± 1.4 | 5.8 ± 1.6 | 0.055 | 0.845 (0.712,1.003) | ||
| TAPSE(mm) | 16.8 ± 3.9 | 16.3 ± 3.4 | 15.9 ± 3.7 | 0.110 | 1.057 (0.988,1.130) | ||
| FAC (%) | 30.6 ± 9.3 | 29.8 ± 8.3 | 27.7 ± 7.6 | 0.064 | 1.029 (0.998,1.061) | ||
| TR severity | 0.546 | ||||||
| Mild | 44 (20.2%) | 51 (23.5%) | 36 (16.5%) | 0.944 | 1.031 (0.441,2.408) | ||
| Moderate | 28 (12.8%) | 22 (10.1%) | 16 (7.3%) | 0.480 | 1.386 (0.560,3.431) | ||
| Severe | 7 (3.2%) | 8 (3.7%) | 6 (2.8%) | ||||
| TR signal quality | 0.020 | ||||||
| Good | 53 (24.3%) | 49 (22.5%) | 25 (11.5%) | ||||
| Medium | 23 (10.6%) | 26 (11.9%) | 27 (12.4%) | 0.017 | 0.525 (0.309,0.892) | 0.000 | 0.258 (0.138,0438) |
| Poor | 3 (1.4%) | 6 (2.8%) | 6 (2.8%) | 0.055 | 0.375 (0.138,1.020) | 0.013 | 0.233 (0.074,0.734) |
| Catheterization parameters | |||||||
| sPAPRHC level | 0.000 | ||||||
| Low | 43 (19.7%) | 25 (11.5%) | 2 (0.9%) | 0.000 | 15.574 (7.563,31.961) | 0.000 | 21.561 (9.574,48.554) |
| Medium | 30 (13.8%) | 27 (12.4%) | 17 (7.9%) | 0.000 | 5.279 (2.752.10.125) | 0.000 | 5.125 (2.545,10.321) |
| High | 6 (2.8%) | 29 (13.3%) | 39 (17.9%) | ||||
| sPAPRHC (mmHg) | 60.5 ± 19.6 | 74.4 ± 23.1 | 92.4 ± 23.1 | 0.000 | 0.958 (0.947,0.970) | ||
| RAP (mmHg) | 2.2 ± 4.2 | 3.3 ± 4.7 | 5.2 ± 6.1 | 0.002 | 0.921 (0.875,0.970) | ||
| PVR (Wood Units) | 8.4 ± 5.9 | 11.2 ± 6.2 | 14.0 ± 8.5 | 0.000 | 0.912 (0.878,0.947) | ||
| PAWP (mmHg) | 6.9 ± 5.2 | 7.5 ± 5.2 | 10.1 ± 7.0 | 0.003 | 0.932 (0.889,0.977) | 0.018 | 0.939 (0.892,0.989) |
| mPAP (mmHg) | 38.6 ± 35.6 | 43.3 ± 14.7 | 53.9 ± 15.5 | 0.000 | 0.961 (0.944,0.978) | ||
| Clinical parameters | |||||||
| 6 M WT (m) | 370.9 ± 105.7 | 355.9 ± 123.0 | 367.8 ± 84.1 | 0.868 | 1.000 (0.996,1.005) | ||
| WHO functional class | 0.907 | ||||||
| I | 5 (2.3%) | 10 (4.6%) | 5 (2.3%) | 0.805 | 0.858 (0.256,2.880) | ||
| II | 38 (17.4%) | 29 (13.3%) | 26 (11.9%) | 0.745 | 1.176 (0.443,3.127) | ||
| III | 30 (13.8%) | 37 (17.0%) | 22 (10.1%) | 0.919 | 1.052 (0.395,2.805) | ||
| VI | 6 (2.8%) | 5 (2.3%) | 5 (2.3%) | ||||
RAD right atrial diameter; RVDD right ventricle diastolic diameter; RV WT right ventricle wall thickness; TAPSE tricuspid annular plane systolic excursion; RV FAC right ventricle fractional area change; RAP right atrial pressure; PVR pulmonary vascular resistance; PAWP pulmonary artery wedge pressure; mPAP mean pulmonary artery pressure; 6 M WT 6-min walk test
Observer variability of sPAPECHO estimation
The intraclass correlation coefficient for interobserver reproducibility of sPAPECHO was 0.988 (95% CI: 0.977–0.994), and the intraclass correlation coefficient for intraobserver reproducibility of sPAPECHO was 0.992 (95% CI, 0.984–0.996).
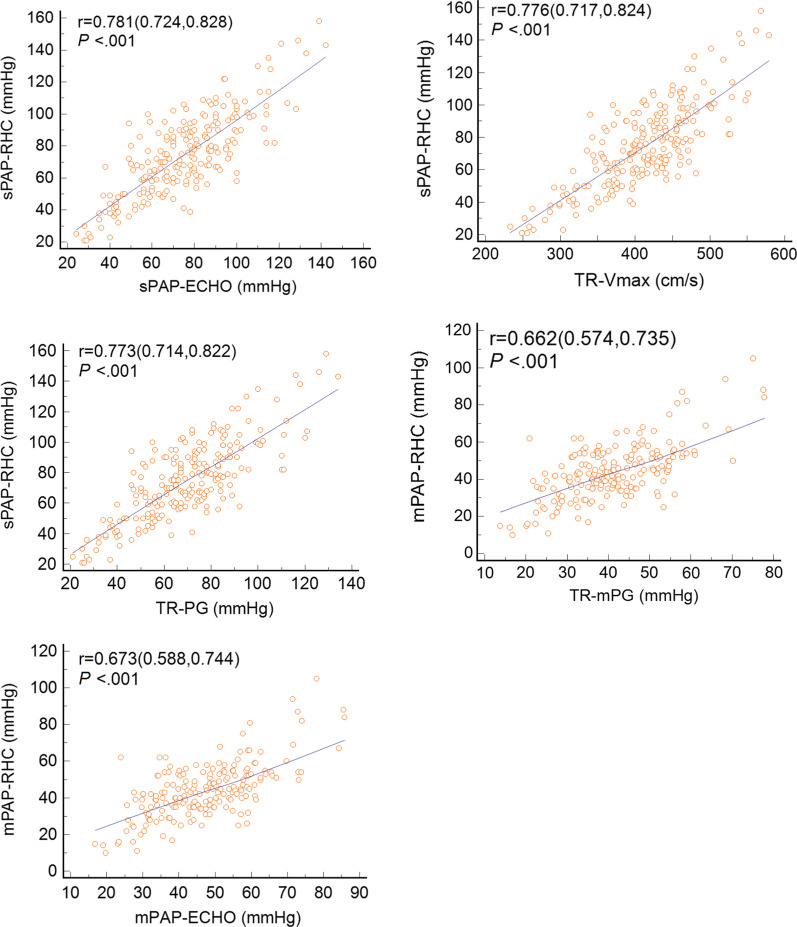
Association between invasively determined parameters and TR-derived parameters
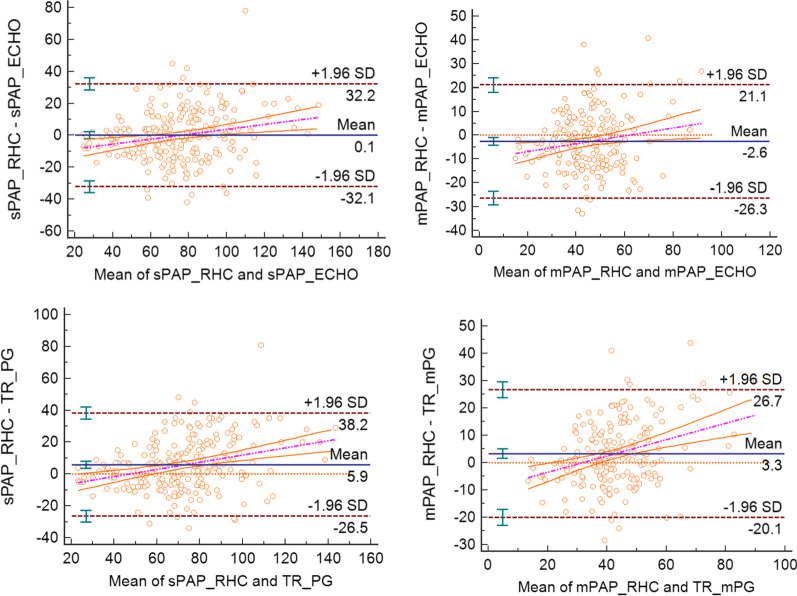
All of the TR-derived parameters, including TR Vmax, TR-PG, TR-mPG, mPAPECHO, and sPAPECHO, showed a positive correlation with related RHC results (Fig. 3). sPAPECHO had the highest correlation coefficient (r = 0.782, P < 0.001). Bland–Altman analysis demonstrated low bias between RHC and echocardiographic results, with wide limits of agreements (Fig. 4). The bias of sPAPECHO (mean bias = 0.1 mm Hg; 95% limits of agreement: −32.1 to +32.2 mm Hg) was lower than that of TR-PG (mean bias = 5.9 mm Hg; 95% limits of agreement: −26.5 to +38.2 mm Hg). The mean deviations of mPAPECHO and TR-mPG from mPAPRHC were −2.6 mm Hg (95% limits of agreement: −26.3 to +21.1 mm Hg) and 3.3 mm Hg (95% limits of agreement: −20.1 to +26.7 mm Hg), respectively.
Fig. 3.
Correlation of invasively determined parameters with TR derived parameters. pearson’s rank correlation coefficients are presented with 95% CI in brackets
Fig. 4.
Bland–Altman plot showing the relationship between invasively determined parameters with TR derived parameters
Performance of different TR methods for predicting PH
The ROC analysis showed that sPAPECHO had better predictive efficiency and sensitivity for determining the possibility of PH than other TR-related methods, including TR Vmax, TR-PG, TR-mPG, and mPAPECHO (Table 3), but their differences were not significant (P > 0.05). Using Youden index quantification, the optimal cutoff value for our cohort was 49.5 mm Hg for the sPAPECHO method with a sensitivity of 94.9% and a specificity of 85.7%.
Table 3.
Receiver operating characteristic curve analysis of DE parameters for detecting PH (mPAP ≥ 25 mmHg)
| AUC | Cut-off value | Sensitivity (%) | Specificity (%) | Accuracy (%) | PPV (%) | NPV (%) | |
|---|---|---|---|---|---|---|---|
| sPAPECHO | 0.981 | 49.5 mmHg | 94.9 | 85.7 | 94.0 | 98.4 | 64.3 |
| TR Vmax | 0.977 | 350.0 cm/s | 91.9 | 90.5 | 91.7 | 98.9 | 54.3 |
| TR-PG | 0.978 | 46.5 mmHg | 94.4 | 85.7 | 93.6 | 98.4 | 62.1 |
| mPAPECHO | 0.956 | 30.6 mmHg | 94.4 | 84.6 | 93.7 | 98.8 | 52.4 |
| TR-mPG | 0.945 | 27.6 mmHg | 92.7 | 84.6 | 92.2 | 98.8 | 45.8 |
PPV Positive predictive value; NPV Negative predictive value; sPAPECHO: pulmonary systolic pressure estimated by echocardiography; TR Vmax: maximum velocity of tricuspid regurgitation; TR-PG tricuspid regurgitation pressure gradient; mPAPECHO mean pulmonary artery pressure estimated by echocardiography; TR-mPG tricuspid regurgitation mean pressure gradient
Factors affecting the accuracy of sPAPECHO estimation
There were 79 patients (36.2%) in the overestimated group, 81 patients (37.2%) in the accurate group, and 58 patients (26.6%) in the underestimated group. sPAPRHC was divided into three levels according to its tertiles (63 mm Hg, 85 mm Hg). The low-level group was defined sPAPRHC less than 63 mm Hg. Patients with sPAPRHC between 63 mm Hg and 85 mm Hg were considered the medium-level group, while patients with sPAPRHC higher than 85 mmHg were classified as the high-level group. The univariate ordinal analysis demonstrated that RV WT, FAC, TR signal quality, sPAPRHC level, RAP, PVR, PAWP, and mPAP were associated with the inaccuracy of sPAPECHO estimation (Table 2). After multivariate ordinal regression analysis, we found that TR signal quality, PAWP, and sPAPRHC level significantly affected the accuracy of sPAPECHO (P < 0.05). Relative to good signal quality, the OR values of medium and poor signal quality were 0.26 (95% CI: 0.14, 0.48) and 0.23 (95% CI: 0.07, 0.73), respectively. Compared with high sPAPRHC level, the OR values of low and medium sPAPRHC levels were 21.56 (95% CI: 9.57, 48.55) and 5.13 (95% CI: 2.55, 10.32), respectively. The OR value of PAWP was 0.94 (95% CI: 0.89, 0.99). In contrast, TR severity and RV systolic function parameters (such as TAPSE, S’, and FAC) did not remain in the final equation.
Discussion
Key findings of our study are as follows: (1) All TR-related methods, including sPAPECHO, have comparable and good efficiency in PH screening. (2) The assessment of sPAPECHO would be more reliable after taking TR signal quality, sPAPRHC levels, and PAWP into account.
Performance of sPAPECHO in PH screening
In our study, sPAPECHO showed comparable efficiency to other TR-related methods in PH screening. Compared with mPAPECHO, sPAPECHO is more convenient to measure. As a derived variable of TR Vmax, sPAPECHO did not amplify measurement errors in assessing pulmonary artery pressure as indicated by the current guidelines; on the contrary, it showed better sensitivity while maintaining similar specificity. Relative to TR Vmax, TR-PG, and TR-mPG, sPAPECHO contains more information from RAP, which may account for its better accuracy and lower bias. RAP elevates with the increase of RV overload [9], so it is an important measurement that provides heart failure and prognostic information [10]. Hellenkamp’s study [2] on mPAPECHO also supported that RAP is of additional diagnostic value in predicting PH. Compared with mPAPECHO, sPAPECHO has the advantage of being simple and convenient. Taken together, sPAPECHO can be a convenient and effective measurement for clinical application in PH screening.
Reasons for the inaccuracy in sPAPECHO estimation
First, our findings confirmed previous reports that the TR signal quality would affect the accuracy of sPAPECHO [11]. Poor signal quality leads to the underestimation of sPAPECHO, because interpretation error of peak velocity is further amplified by the square of the Bernoulli equation. We also found that good signal quality could bring overestimation of sPAPECHO for some cases. In our cohort, sPAPECHO was still overestimated in 41% of the patients who obtained good signal quality of TR. After further analysis, we found that the lower sPAPRHC level and PAWP were significantly associated with the overestimation of sPAPECHO in patients with good signal quality. This phenomenon suggests that we cannot simply rely on good signal quality, and attention should also be paid to sPAPRHC level and PAWP because they both affect the accuracy of sPAPECHO.
Second, as for the effect of sPAPRHC level on the accuracy of sPAPECHO, Groh et al. [12] found that echocardiography inaccurately estimated right ventricular pressure in children with elevated right heart pressure. Our results provided further evidence that sPAPECHO tends to be underestimated at a high sPAPRHC level. We assumed that the coupling mechanism between RV contractility and its load may account for this phenomenon. When sPAPRHC mildly elevates during the initial phase of PH, RV coupling could be maintained by enhanced RV contractility [13, 14], and the estimation of sPAPRHC by DE is relatively reliable. However, as PH progresses and RV uncoupling occurs, CO would decrease and RV preload would increase, along with elevated RAP, so the right atrioventricular pressure gradient would decrease, and DE would underestimate sPAPRHC. sPAPRHC level may affect the accuracy of sPAPECHO through the coupling mechanism between RV contractility and its load. This finding suggests that we should synthesize more echocardiographic signs when evaluating the efficacy of PH, because the decrease in sPAPECHO at this time is not necessarily a result of disease improvement, but may also be a sign of underestimation of sPAPECHO caused by RV decoupling.
Third, we found that echocardiography tended to underestimate pulmonary artery pressure when PAWP increased. We speculated that the underestimation of sPAPECHO due to the higher PAWP may be related to the lower threshold in post-capillary PH patients. Amsallem et al. [15] found that higher PAWP was associated with lower sPAPECHO threshold for PH diagnosis, which is consistent with our findings. The optimal cutoff value of our cohort was 49.5 mm Hg, which is higher than the cutoff values in previous studies that had focused on post-capillary PH patients with higher PAWP [16, 17]. Pre-capillary PH patients with lower PAWP accounted for 85.8% of the cohort, which may explain this phenomenon. Finkelhor et al. [18] also found that PAWP had a strong inverse correlation with the difference between sPAPRHC and sPAPECHO. They speculated that elevated left atrial pressure can be transmitted to the right atrium via the shared interatrial septum as well as through pericardial constraint and limit TR velocities, thereby also affecting the accuracy of sPAPECHO. Until now, the mechanism by which PAWP affects the accuracy of sPAPECHO is still unclear, so more multicenter studies are needed to validate this deduction. Based on the above findings, we think that the accuracy of sPAPECHO would be improved if combined with the assessment of left ventricular filling pressure by echocardiography. Although RHC is the gold standard for PAWP or left ventricular filling pressure, whether PAWP is elevated can be assessed by indirect signs of echocardiography, such as the ratio of mitral E peak velocity and averaged e’velocity (E/e'm ratio), TR Vmax, and left atrium volume index. Echocardiologists can synthesize such information to determine whether patients have PAWP elevation, to assess the sPAPECHO and the possibility of PH more reasonably.
Furthermore, there is no consensus as to how TR severity would interfere with the accuracy of the sPAPECHO. Hioka et al. [19] reported that echocardiography increasingly overestimated the TR PG with the advance of TR severity, as was theoretically predicted by the pressure recovery phenomenon associated with the laminar regurgitant flow. However, Parasuraman et al. [20] reported that severe TR could cause equalization of right atrial and ventricular pressures, which may cause the TR Doppler envelope to be cut short, thereby leading to underestimation of sPAPECHO. Our study differed from other studies in that the TR severity did not significantly affect the accuracy of sPAPECHO. It should be noted that only 9.6% of patients in our cohort had severe TR, which was in line with the actual clinical situation that severe TR only appears in the minority of patients. However, in patients with mild or moderate TR, we could also obtain good signal quality and estimate sPAPECHO appropriately (Fig. 5). TR severity was also affected by RV contractility and dimension. Thus, the overall impact of TR severity on the accuracy of sPAPECHO is not as significant as that of TR signal quality.
Fig. 5.
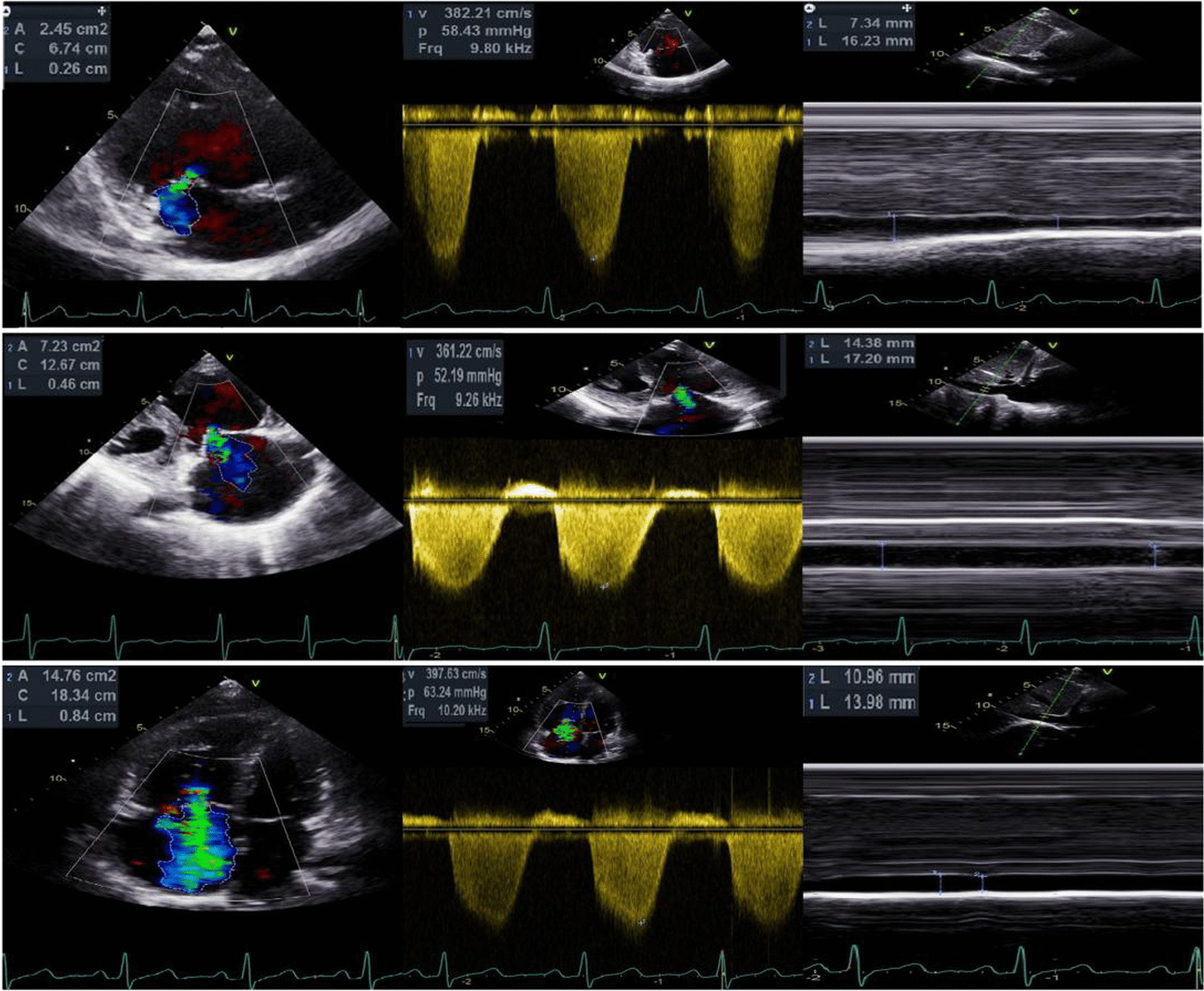
Examples of different severity of TR with good signal quality and accurate sPAPECHO. The upper image presents a 40 years old female with mild TR whose sPAPECHO and sPAPRHC were 59 and 61 mmHg, respectively. The medium image shows a 50 years old female with moderate TR whose sPAPECHO and sPAPRHC were 60 and 60 mmHg, respectively. The lower image demonstrates a 34 years old female with severe TR whose sPAPECHO and sPAPRHC were 71 and 73 mmHg, respectively
We found that none of the RV systolic parameters had a significant impact on the accuracy of sPAPECHO. Theoretically, RV systolic function would gradually decrease [21], but RV can remain coupled for the large increase in load by increasing contractility until heart failure [13]. Therefore, RV systolic parameters are relatively stable before the end-stage of PH. In addition, the heart movement and measurement angle dependence also affect the accuracy of the relevant parameters. Although RV systolic parameters had clinical significance for the assessment of PH, they did not have a significant effect on the accuracy of sPAPECHO.
Finally, incorporating TR signal quality, sPAPRHC level, and PAWP into the assessment of sPAPECHO would improve its accuracy and avoid overly invasive examination.
Limitations
This study has several limitations. First, this was a retrospective study with a small sample size. Although 90.5% of our patients had PH, and in 47.7% of them, PH was due to chronic pulmonary thromboembolism, the sample size of other types of PH was relatively small. Thus, we could not give specific suggestions for each type of PH. Second, we included patients who had undergone RHC and echocardiography within 7 days due to the restriction of clinical actual conditions. However, the average interval time was 3 days in this study, and the majority of patients had pre-capillary PH, which indicated that the patients’ hemodynamics was relatively stable and did not change dramatically during this short time. Furthermore, contrast microbubbles were not adopted to enhance the tricuspid regurgitation jet for patients with mild regurgitation or poor signal quality. Finally, the single-center nature of the present study limited generalization.
Conclusions
In this study, we found that all TR-related methods, including sPAPECHO, had comparable and good efficiency in PH screening. To make the assessment of sPAPECHO more accurate, attention should be paid to TR signal quality, sPAPRHC level, and PAWP.
Acknowledgements
We thank all the patients who participated in this study.
Abbreviations
- PH
Pulmonary hypertension
- RHC
Right heart catheterization
- DE
Doppler echocardiography
- TR
Tricuspid regurgitation
- sPAPRHC
Pulmonary artery systolic pressure measured by RHC
- sPAPECHO
Pulmonary artery systolic pressure estimated by DE
- mPAP
Mean pulmonary artery pressure measured by RHC
- mPAPECHO
Mean pulmonary artery pressure estimated by DE
- PAWP
Pulmonary artery wedge pressure
- RAP
Right atrial pressure
- CO
Cardiac output
- TR PG
TR pressure gradient
- TR-mPG
TR mean pressure gradient
- PVR
Pulmonary vascular resistance
- RV
Right ventricle
- RV WT
RV wall thickness
- TAPSE
Tricuspid annular plane systolic excursion
- S’
Systolic annular tissue velocity of the lateral tricuspid annulus
- FAC
RV Fractional area change
- IVC
Inferior vena cava
Author contributions
A-LL proposed research ideas, collected and measured echocardiographic data, revised the paper, and reviewed it academically. G-JL was responsible for literature review, data analysis, and writing the manuscript. X-TC performed right heart catheterization. Y-NZ and YZ measured and collected echocardiographic data. QG, W-MX, and Z-GZ collected the clinical data. J-PL gave guidance on the statistics. All authors read and approved the final manuscript.
Funding
This study was supported by grants from the Capital Health Development Research Project (2020–2-4063) and the National Natural Key Clinical Specialty Construction Project (2020-QTL-009).
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study complied with the Declaration of Helsinki. Ethical approval number was 2020-95-K59. The protocol was approved by the Ethic Committee of China-Japan Friendship Hospital. The institutional review board of the China-Japan Friendship Hospital waived the need for written patient informed consent as this study involved the retrospective analysis of clinically acquired data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Galie N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT) Eur Respir J. 2015;46(4):903–975. doi: 10.1183/13993003.01032-2015. [DOI] [PubMed] [Google Scholar]
- 2.Hellenkamp K, Unsold B, Mushemi-Blake S, et al. Echocardiographic estimation of mean pulmonary artery pressure: a comparison of different approaches to assign the likelihood of pulmonary hypertension. J Am Soc Echocardiogr. 2018;31(1):89–98. doi: 10.1016/j.echo.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Greiner S, Jud A, Aurich M, et al. Reliability of noninvasive assessment of systolic pulmonary artery pressure by Doppler echocardiography compared to right heart catheterization: analysis in a large patient population. J Am Heart Assoc. 2014;3(4):e001103. doi: 10.1161/JAHA.114.001103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santiago-Vacas E, Lupon J, Gavidia-Bovadilla G, et al. Pulmonary hypertension and right ventricular dysfunction in heart failure: prognosis and 15-year prospective longitudinal trajectories in survivors. Eur J Heart Fail. 2020;22(7):1214–1225. doi: 10.1002/ejhf.1862. [DOI] [PubMed] [Google Scholar]
- 5.Jalalian R, Moghadamnia AA, Tamaddoni A, et al. Comparing the efficacy of tadalafil versus placebo on pulmonary artery systolic pressure and right ventricular function in patients with beta-thalassaemia intermedia. Heart Lung Circ. 2017;26(7):677–683. doi: 10.1016/j.hlc.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Wang Y, Li H, et al. Evaluation of the hemodynamics and right ventricular function in pulmonary hypertension by echocardiography compared with right-sided heart catheterization. Exp Ther Med. 2017;14(4):3616–3622. doi: 10.3892/etm.2017.4953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krishnan A, Markham R, Savage M, et al. Right heart catheterisation: how to do it. Heart Lung Circ. 2019;28(4):e71–e78. doi: 10.1016/j.hlc.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Van Riel AC, Opotowsky AR, Santos M, et al. Accuracy of echocardiography to estimate pulmonary artery pressures with exercise: a simultaneous invasive-noninvasive comparison. Circ Cardiovasc Imaging 2017;10(4):e005711. [DOI] [PMC free article] [PubMed]
- 9.Querejeta RG, Campbell P, Claggett B, et al. Right atrial function in pulmonary arterial hypertension. Circ Cardiovasc Imaging 2015;8(11):e3521. [DOI] [PMC free article] [PubMed]
- 10.Austin C, Alassas K, Burger C, et al. Echocardiographic assessment of estimated right atrial pressure and size predicts mortality in pulmonary arterial hypertension. Chest. 2015;147(1):198–208. doi: 10.1378/chest.13-3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amsallem M, Sternbach JM, Adigopula S, et al. Addressing the controversy of estimating pulmonary arterial pressure by echocardiography. J Am Soc Echocardiogr. 2016;29(2):93–102. doi: 10.1016/j.echo.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Groh GK, Levy PT, Holland MR, et al. Doppler echocardiography inaccurately estimates right ventricular pressure in children with elevated right heart pressure. J Am Soc Echocardiogr. 2014;27(2):163–171. doi: 10.1016/j.echo.2013.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vonk NA, Westerhof BE, Westerhof N. The relationship between the right ventricle and its load in pulmonary hypertension. J Am Coll Cardiol. 2017;69(2):236–243. doi: 10.1016/j.jacc.2016.10.047. [DOI] [PubMed] [Google Scholar]
- 14.Margonato D, Ancona F, Ingallina G, et al. Tricuspid regurgitation in left ventricular systolic dysfunction: marker or target? Front Cardiovasc Med. 2021;8:702589. doi: 10.3389/fcvm.2021.702589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amsallem M, Tedford RJ, Denault A, et al. Quantifying the influence of wedge pressure, age, and heart rate on the systolic thresholds for detection of pulmonary hypertension. J Am Heart Assoc. 2020;9(11):e16265. doi: 10.1161/JAHA.119.016265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sawada N, Kawata T, Daimon M, et al. Detection of pulmonary hypertension with systolic pressure estimated by doppler echocardiography. Int Heart J. 2019;60(4):836–844. doi: 10.1536/ihj.18-453. [DOI] [PubMed] [Google Scholar]
- 17.Greiner S, Jud A, Aurich M, et al. Reliability of noninvasive assessment of systolic pulmonary artery pressure by Doppler echocardiography compared to right heart catheterization: analysis in a large patient population. J Am Heart Assoc. 2014;3(4):e1103. doi: 10.1161/JAHA.114.001103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finkelhor RS, Scrocco JD, Madmani M, et al. Discordant Doppler right heart catheterization pulmonary artery systolic pressures: importance of pulmonary capillary wedge pressure. Echocardiography. 2014;31(3):279–284. doi: 10.1111/echo.12361. [DOI] [PubMed] [Google Scholar]
- 19.Hioka T, Kaga S, Mikami T, et al. Overestimation by echocardiography of the peak systolic pressure gradient between the right ventricle and right atrium due to tricuspid regurgitation and the usefulness of the early diastolic transpulmonary valve pressure gradient for estimating pulmonary artery pressure. Heart Vessels. 2017;32(7):833–842. doi: 10.1007/s00380-016-0929-4. [DOI] [PubMed] [Google Scholar]
- 20.Parasuraman S, Walker S, Loudon BL, et al. Assessment of pulmonary artery pressure by echocardiography-A comprehensive review. Int J Cardiol Heart Vasc. 2016;12:45–51. doi: 10.1016/j.ijcha.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kong D, Shu X, Pan C, et al. Evaluation of right ventricular regional volume and systolic function in patients with pulmonary arterial hypertension using three-dimensional echocardiography. Echocardiography. 2012;29(6):706–712. doi: 10.1111/j.1540-8175.2012.01681.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.