Abstract
Background
It is not known whether post-traumatic stress disorder (PTSD) increases HIV-risk behaviours among young people in sub-Saharan Africa. We assessed associations of PTSD symptoms with sexual behaviour, HIV risk perception, and attitudes towards PrEP among young people taking part in the CHAPS community survey. We hypothesised that PTSD symptoms would increase sexual behaviours associated with HIV risk, hinder PrEP uptake and influence preference for daily versus on-demand PrEP.
Methods
Young people without HIV, aged 13–24 years, were purposively recruited in Johannesburg and Cape Town in South Africa, Wakiso in Uganda, and Chitungwiza in Zimbabwe, and surveyed on socio-demographic characteristics, PrEP knowledge and attitudes, sexual behaviour, HIV perception and salience, and mental health. PTSD symptoms were measured using the Primary Care PTSD Screen for the Diagnostic and Statistical Manual of Mental Disorders 5 (PC-PTSD-5). Logistic and ordinal logistic regression was used to assess associations between PC-PTSD-5 score and socio-demographic characteristics, sexual behaviour, HIV risk perception, PrEP attitudes, and substance use, adjusting for age, sex, setting, depression and anxiety.
Results
Of 1330 young people (51% male, median age 19 years), 522 (39%) reported at least one PTSD symptom. There was strong evidence that having a higher PC-PTSD-5 score was associated with reported forced sex (OR 3.18, 95%CI: 2.05–4.93), self-perception as a person who takes risks (OR 1.12, 95%CI: 1.04–1.20), and increased frequency of thinking about risk of HIV acquisition (OR 1.16, 95%CI: 1.08–1.25). PTSD symptoms were not associated with willingness to take PrEP, preference for on-demand versus daily PrEP, or actual HIV risk behaviour such as condomless sex.
Conclusions
Symptoms consistent with probable PTSD were common among young people in South Africa, Uganda and Zimbabwe but did not impact PrEP attitudes or PrEP preferences. Evaluation for PTSD might form part of a general assessment in sexual and reproductive health services in these countries. More work is needed to understand the impact of PTSD on HIV-risk behaviour, forced sex and response to preventive strategies including PrEP.
Supplementary information
The online version contains supplementary material available at 10.1186/s12879-022-07430-2.
Keywords: Post-traumatic stress disorder, Young people, Mental health, HIV, PrEP, Sub-Saharan Africa
Background
HIV remains a major global public health problem; in 2019 an estimated 38 million people were living with HIV and there were an estimated 1.7 million new infections globally [1]. In sub-Saharan Africa (SSA) the number of people newly infected with HIV per year remains consistently high [2], with young people, particularly young women, experiencing the highest rates of infection [3]. This is despite the existence of effective HIV preventive strategies including pre-exposure prophylaxis (PrEP), which is recommended by the World Health Organisation (WHO) for persons at substantial risk of HIV acquisition as part of a combination preventive approach [4]. However, availability, user acceptability and uptake of PrEP is highly variable and often limited across the region, especially for young people [5].
As well as being a period of increased HIV acquisition risk, early adulthood is also the period in which mental disorders such as depression and anxiety frequently emerge [6]. Post-traumatic stress disorder (PTSD) [7], often as a consequence of sexual violence [8], is common in general population settings in SSA with a recent systematic review estimating a prevalence of probable PTSD of 22% [9]. Although comorbidity between PTSD and other mental disorders is common [10] and symptoms often overlap [11], PTSD occurring on its own may represent a different phenotype with distinct biological and psychological profiles compared to PTSD in the presence of co-morbid mental disorders [12].
Among young people in SSA, there is some, albeit inconclusive, evidence that common mental disorders such as depression and anxiety, and prior exposure to trauma including trauma due to sexual violence, may increase HIV-risk behaviours [13, 14] and HIV acquisition [15], and reduce HIV treatment adherence and outcomes [16, 17]. They may also impact adherence to PrEP for prevention of HIV, although evidence is mixed: a study in men who have sex with men and transgender women including participants from South Africa found that depression did not contribute to decreased adherence to daily PrEP on a population scale [18], but studies in Kenya and Uganda [19], and South Africa [20] found that depression was associated with poor adherence to daily PrEP among women but not among men. Limited research has been conducted among young people, although a study in the USA found that adolescents with and without mental disorders did not differ in PrEP retention outcomes [21]. Few studies have investigated whether PTSD, either in combination with other mental disorders or in isolation, impacts PrEP usage, and to our knowledge, no studies have examined the potential impact of PTSD on PrEP-related preferences in SSA.
The Combined HIV Adolescent PrEP and Prevention Study (CHAPS) is a mixed methods study conducted among young people in South Africa, Uganda and Zimbabwe [22]. It included a quantitative social science survey, with the overarching aim of identifying barriers and motivators towards the uptake of PrEP [22]. The survey, which included questions on PTSD symptoms, provided an opportunity to assess the primary objective of the current analysis: to assess whether probable PTSD was associated with attitudes towards PrEP, and with sexual behaviour and perceptions of HIV risk. Mental health disorders are known barriers to health care engagement and daily medication adherence, thus we hypothesise that probable PTSD may hinder willingness to take PrEP and disclose its usage, and influence preference for daily versus on demand PrEP. Evidence on this could have implications for how PrEP is offered to young people and whether a history of trauma would need to be taken into account when providing PrEP. We also hypothesise that probable PTSD may increase sexual risk behaviours associated with HIV risk, as has been previously demonstrated in other sub-Saharan African settings specifically for trauma due to sexual violence [13].
Methods
Study design
The primary aim of the current analysis was to assess associations of self-reported probable PTSD with sexual behaviour, perceptions of HIV risk, and attitudes towards PrEP among young people taking part in the CHAPS social science quantitative survey. Since PTSD occurring in the absence of other mental health co-morbidities may represent a different phenotype with distinct biological and psychological profiles compared to PTSD in the presence of co-morbid mental disorders, the secondary aim was to investigate whether other mental health co-morbidities modified any associations seen between probable PTSD and sexual behaviour, HIV risk and PrEP attitudes.
Study setting and participants
Between March and December 2019, we used purposive community sampling [23] to recruit young people aged 13–24 years—prioritising those who were sexually active and living without known HIV—in four settings: Johannesburg and Cape Town in South Africa, Wakiso in Uganda, and Chitungwiza in Zimbabwe. Information on the study was first presented at community meetings organised with local officials and community mobilisers, who helped to identify locations at which young people congregated. CHAPS fieldworkers then visited these locations, coordinating with local leaders and community mobiliers (and Village Health Teams in Uganda) to provide information on the study, and to answer questions from potential participants and their parents/guardians. In South Africa, participants were recruited from community groups, schools, churches, bars, taxi ranks and other public meeting places. In Zimbabwe participants were recruited from community groups, youth centres, bars, voluntary counselling and testing sites, taxi ranks, and public meeting places. In Uganda, participants were recruited at fish landing sites.
Young people were eligible to participate in the survey if they were aged 13–24 years and willing to undergo HIV testing. In South Africa and Zimbabwe, this was administered as part of the screening and only young people without HIV were eligible for inclusion, while in Uganda, HIV status was not part of eligibility criteria, but recruited participants with reactive HIV test results (n = 9) based on samples obtained at enrolment, were not included in this analysis in order to ensure comparability in inclusion criteria across all settings.
Ethical considerations
Ethical approval was obtained from the Human Research Ethics Committees of the University of Cape Town (290/2018) and the University of the Witwatersrand (180906B, M1811148 and 180,108) in South Africa, the Uganda Virus Research Institute Research and Ethics Committee (GC127/18/3/638) and Uganda National Council for Science and Technology (HS2534) in Uganda, the Joint Research Ethics Committee for the University of Zimbabwe, College of Health Sciences and the Parirenyatwa Group of Hospitals (JREC/195/18), the Medical Research Council of Zimbabwe and the Research Council of Zimbabwe (MRCZ/A/2356) in Zimbabwe, and the London School of Hygiene and Tropical Medicine Ethics Committee (15,629 and 16,182) in the UK.
Written, informed consent was obtained from all participants aged 18 years or over and written, informed parental consent and assent was obtained for participants aged under 18 years. A waiver of parental consent for emancipated minor participants was approved by ethical boards for use in Cape Town, Wakiso and Chitungwiza. Consent materials were available in Zulu and Sesotho in South Africa, Luganda in Uganda, Shona in Zimbabwe, and English in all settings. They were translated from English into other languages by bilingual outreach workers involved in HIV and adolescent programmes, followed by independent back translation, with further review and revision until agreement was reached, and final review by the above-named ethical review committees. Participants were reimbursed for participation-related time and travel costs following setting-specific national guidelines.
Data collection and measures
Following written informed consent, and HIV testing, participants completed the quantitative survey. The survey was developed collaboratively with South African, Ugandan, Zimbabwean, and UK experts in adolescent health and HIV prevention and treatment, and was piloted among Adolescent Community Advisory Board members in each country. The survey was available in the same languages as described above for the consent materials, using the same approach to translation. Participants completed the survey on hand-held electronic devices in their language of choice at a private mutually convenient community location, with the support of trained interviewers available if necessary. The survey took approximately 45 min to complete and included questions on socio-demographic characteristics, knowledge and attitudes towards PrEP, past and current sexual behaviour characteristics, HIV perception and salience, mental health, and substance use, as described below.
Socio-demographic characteristics considered as exposures for this analysis were study setting, sex, age group, the highest level of education attended, whether the participant was the household head, age of household head, and the number of adults and rooms in the household. Data on historical sexual behaviour included age of first sex and any history of transactional sex. Information collected on recent or current sexual behaviour included forced sex or forcing sex in the last 6 months, number of partners in the last 6 months, sex frequency in the past month, degree of advance knowledge of the most recent sexual encounter, and current relationship status. Information on age, relationship, type, condom use, and HIV status of most recent partner was also collected. Participants were asked about whether they perceived themselves generally as a person who takes risks through two questions: (1) “Are you generally a person who takes risks? I am going to read three answer choices and I would like you to tell me which one is closest to the truth about you personally”, with possible responses “I take risks”, “I am somewhere in between”, “I avoid taking risks”, and (2) “Please rate yourself from 0 to 10, where 0 means you are unwilling to take any risks and 10 means you are always willing take risks”. They were also asked about how often they had thought about the risk of acquiring HIV in the last 3 months, and how likely they felt they were to become infected with HIV in the next 3 months. Regarding PrEP, the two main ways in which PrEP can be taken were described to the participants as i) Daily PrEP: one pill every day whether you are having sex or not; and ii) On-demand PrEP: taking two pills before you have sex and two pills after sex. Participants were asked whether they felt they would prefer on-demand or daily PrEP, whether they would choose to take PrEP if it cost the same amount as a hot meal and whether they would disclose PrEP use to their partner.
Information on exposure to traumatic events and post-traumatic stress symptoms was collected using the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5), a 5-item screen related to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnosis criteria for PTSD that was designed for use in primary care settings to identify respondents with probable PTSD [24]. Respondents indicating no exposure to any traumatic event throughout their life are assigned a score of 0. Respondents reporting lifetime exposure to any traumatic event are asked five additional binary questions about how that trauma exposure has affected them over the past month. The number of positive responses are added to give a total PC-PTSD-5 score. Since the tool has not been validated in SSA youth (and an appropriate cut-off has not been determined), the total PC-PTSD-5 score was used for primary analysis. In secondary analysis, we also investigated using a PC-PTSD-5 cut-off score of ≥ 3 which has been shown to have 90% sensitivity and 80% specificity as a screen for PTSD in US army veterans [25], to perform well for detecting probable PTSD among young people in the US [26] and has been previously implemented, although not validated, among young people in South Africa [27]. Following completion of PC-PTSD-5 questions, study staff did not have access to participants’ responses but asked participants if there were any experiences or feelings that they would like to discuss; those who said they did want to talk to someone could receive counselling from trained staff at the study clinic or clinic close to the location of interview.
As previously described [28], information on depressive symptoms was collected using the 9-item Patient Health Questionnaire (PHQ-9) [29]. Participants were classified as having moderate/severe depressive symptoms if their PHQ-9 score was ≥ 10. The PHQ-9 is validated in many languages including those used in the CHAPS study [30–32]. Generalised anxiety symptoms were assessed using the Generalized Anxiety Disorder-2 item tool (GAD-2) [33], with participants with a score ≥ 3 classified as having anxiety symptoms. The GAD-2 tool is validated in many languages including those used in the CHAPS study [34, 35]. Information on alcohol use was collected as the frequency of binge drinking, defined as 6 or more drinks. Information on whether other substances had been used in the last 30 days was also collected.
Statistical analysis
Statistical analysis was done using Stata version 16. The sample size provides 90% power to detect a difference in proportion with PC-PTSD-5 ≥ 3 of 22% vs. 15% for exposures with 50% prevalence. Responses for the PC-PTSD-5 tool were summarised for all participants and separately by study setting. Since data were collected using a cross-sectional study design, it is not possible to determine causality. For associations between PTSD score and socio-demographic characteristics, PC-PTSD-5 score was considered as the outcome of interest, and related to socio-demographic characteristics using ordinal logistic regression to obtain crude and adjusted odds ratios (OR) and 95% confidence intervals (CI), and the likelihood ratio test to obtain p-values. For examining associations of PTSD score with sexual behaviour, HIV risk perception, attitudes towards PrEP, and substance use, PC-PTSD-5 score was included as the exposure of interest in separate regression models for each of these outcomes. Logistic regression and ordinal logistic regression models were fitted for binary and ordered categorical outcomes, respectively. The proportional odds assumption for ordinal logistic regression models was tested. For self-perception as a person who takes risks score measured on a continuous scale from 0 to 10, linear regression was used to assess the association with PC-PTSD-5 score. In secondary analyses, PC-PTSD-5 score was classified as ≥ 3 versus < 3 and modelled as a binary outcome variable (for associations with socio-demographica characteristics) or a binary exposure variable (for associations with sexual behaviour, HIV risk perception, attitudes towards PrEP and substance use).
For all analyses, multivariable regression models controlled for age, sex and study setting. For analyses including PC-PTSD-5 score as the exposure of interest, and measures of sexual behaviour, HIV risk perception and attitudes towards PrEP as outcomes of interest, regression models further adjusted for depression and anxiety to assess whether these acted as possible confounders of any associations. Finally, the role of these other mental health co-morbidities as potential modifiers of the relationship of PC-PTSD-5 score with sexual behaviour, HIV risk perception and PrEP attitudes was assessed, by fitting interaction terms between PC-PTSD-5 score and a binary variable for depression and/or anxiety to assess whether PC-PTSD-5 score and depression/anxiety combined multiplicatively in their impact on outcomes. A likelihood ratio test was used to formally test for interaction with a p-value of less than 0.05 interpreted as evidence for effect modification.
Results
A total of 1330 participants aged 13–24 years (mean: 19 years) took part in the survey. Table 1 summarises responses to the PC-PTSD-5 tool, overall and by study setting. A total of 653 participants (49%) reported experiencing a traumatic event during their lifetime. Of these, the majority (522, 80%) reported at least one symptom of post-traumatic stress that they had experienced in the last month and that they associated with that event. A total of 254 (19%) had PC-PTSD-5 ≥ 3.
Table 1.
Responses to Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) questions, overall and by study setting
| Question | Cape Town (n = 239) | Johannesburg (n = 200) | Entebbe (n = 491) | Chitungwiza (n = 400) | Total (n = 1330) |
|---|---|---|---|---|---|
| Have you ever experienced a traumatic event? | |||||
| No | 95 (40%) | 95 (48%) | 243 (49%) | 244 (61%) | 677 (51%) |
| Yes | 144 (60%) | 105 (53%) | 248 (51%) | 156 (39%) | 653 (49%) |
| In the past month, have you experienced nightmares about the event?a | |||||
| No | 68 (47%) | 60 (57%) | 144 (58%) | 79 (51%) | 351 (54%) |
| Yes | 76 (53%) | 45 (43%) | 105 (42%) | 77 (49%) | 302 (46%) |
| In the past month, have you tried hard not to think about the event or avoided situations that remind you of the event?a | |||||
| No | 41 (28%) | 40 (38%) | 126 (51%) | 54 (35%) | 261 (40%) |
| Yes | 103 (72%) | 65 (62%) | 122 (49%) | 102 (65%) | 392 (60%) |
| In the past month, have you been constant on guard, watchful or easily startled?a | |||||
| No | 94 (65%) | 63 (60%) | 159 (64%) | 107 (69%) | 423 (65%) |
| Yes | 50 (35%) | 42 (40%) | 89 (36%) | 49 (31%) | 230 (35%) |
| In the past month, have you felt numb or detached from people, activities or your surroundings?a | |||||
| No | 79 (55%) | 57 (54%) | 192 (77%) | 96 (62%) | 424 (65%) |
| Yes | 65 (45%) | 48 (46%) | 56 (23%) | 60 (38%) | 229 (35%) |
| In the past month, have you felt guilty or unable to stop blaming yourself or others for the event?a | |||||
| No | 88 (61%) | 63 (60%) | 184 (74%) | 99 (63%) | 434 (66%) |
| Yes | 56 (39%) | 42 (40%) | 64 (26%) | 57 (37%) | 219 (34%) |
| Total scale score | |||||
| 0 | 107 (45%) | 111 (56%) | 324 (66%) | 266 (67%) | 808 (61%) |
| 1 | 25 (10%) | 13 (7%) | 46 (9%) | 24 (6%) | 108 (8%) |
| 2 | 42 (18%) | 29 (15%) | 42 (9%) | 47 (12%) | 160 (12%) |
| 3 | 30 (13%) | 22 (11%) | 28 (6%) | 32 (8%) | 112 (8%) |
| 4 | 24 (10%) | 20 (10%) | 34 (7%) | 24 (6%) | 102 (8%) |
| 5 | 11 (5%) | 5 (3%) | 17 (3%) | 7 (2%) | 40 (3%) |
| Post-traumatic stress symptoms score, categorised | |||||
| PC-PTSD-5 score < 3 | 174 (73%) | 153 (77%) | 412 (84%) | 337 (84%) | 1076 (81%) |
| PC-PTSD-5 score ≥ 3 | 65 (27%) | 47 (24%) | 79 (16%) | 63 (16%) | 254 (19%) |
aAmong those who reported ever experiencing a traumatic event
Table 2 shows associations between socio-demographic characteristics and historical sexual behaviour, and PC-PTSD-5 score. PC-PTSD-5 scores were higher on average among participants in both South African settings (particularly Cape Town) and lower among participants in Wakiso and Chitungwiza. There was no evidence of association of PC-PTSD-5 score with sex, age group, education, number of rooms in the household, or number of adults per room in the household. However, there was some evidence that participants who were household heads, who had a higher number of adults in their households, or who had older household heads had higher PC-PTSD-5 scores (Table 2). After adjusting for age, sex and study setting, there was no evidence of an association with PC-PTSD-5 score for ever having sex or age at first sex. Participants reporting ever having had transactional sex were more likely to have a higher PC-PTSD-5 score (adjusted OR 1.89, 95% CI 1.34–2.66, p < 0.001). There was strong evidence that forced sex was associated with PC-PTSD-5 score in both crude and adjusted analyses (adjusted ORs 3.18, 95% CI: 2.05–4.93 and 2.93, 95% CI: 1.74–4.94 for being forced to have sex and forcing someone else to have sex, respectively; p < 0.001).
Table 2.
Associations between socio-demographic characteristics, historical sexual behaviour and post-traumatic stress symptoms
| Characteristic | Category | PC-PTSD score | Crude results | Adjusted resultsa | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | OR (95% CI) | p | OR (95% CI) | p | ||
| Study setting | Cape Town | 107 (45%) | 25 (10%) | 42 (18%) | 30 (13%) | 24 (10%) | 11 (5%) | 2.21 (1.65, 2.97) | < 0.001 | 2.25 (1.67, 3.02) | < 0.001 |
| Johannesburg | 111 (56%) | 13 (7%) | 29 (15%) | 22 (11%) | 20 (10%) | 5 (3%) | 1.58 (1.15, 2.19) | 1.59 (1.15, 2.19) | |||
| Entebbe | 324 (66%) | 46 (9%) | 42 (9%) | 28 (6%) | 34 (7%) | 17 (3%) | Baseline | Baseline | |||
| Chitungwiza | 266 (67%) | 24 (6%) | 47 (12%) | 32 (8%) | 24 (6%) | 7 (2%) | 0.98 (0.75, 1.29) | 0.99 (0.75, 1.30) | |||
| Sex | Male | 405 (60%) | 69 (10%) | 96 (14%) | 47 (7%) | 42 (6%) | 14 (2%) | Baseline | 0.39 | Baseline | 0.37 |
| Female | 403 (61%) | 39 (6%) | 64 (10%) | 65 (10%) | 60 (9%) | 26 (4%) | 1.10 (0.89, 1.36) | 1.10 (0.89, 1.37) | |||
| Age group | 13–15 | 90 (60%) | 15 (10%) | 25 (17%) | 11 (7%) | 8 (5%) | 1 (1%) | 0.89 (0.64, 1.25) | 0.43 | 0.83 (0.60, 1.17) | 0.29 |
| 16–17 | 152 (63%) | 24 (10%) | 25 (10%) | 12 (5%) | 23 (10%) | 4 (2%) | 0.84 (0.63, 1.11) | 0.82 (0.62, 1.10) | |||
| 18–24 | 566 (60%) | 69 (7%) | 110 (12%) | 89 (9%) | 71 (8%) | 35 (4%) | Baseline | Baseline | |||
| Highest level of education attended | Still studying | 420 (60%) | 65 (9%) | 89 (13%) | 53 (8%) | 52 (7%) | 17 (2%) | Baseline | 0.45 | Baseline | 0.96 |
| ≤ Grade 7 | 85 (66%) | 9 (7%) | 15 (12%) | 7 (5%) | 8 (6%) | 4 (3%) | 0.80 (0.54, 1.18) | 0.97 (0.63, 1.48) | |||
| Grade 7–12 | 274 (60%) | 31 (7%) | 53 (12%) | 44 (10%) | 42 (9%) | 15 (3%) | 1.10 (0.88, 1.39) | 1.06 (0.82, 1.38) | |||
| Post-school | 29 (62%) | 3 (6%) | 3 (6%) | 8 (17%) | 0 (0%) | 4 (9%) | 1.06 (0.59, 1.92) | 1.00 (0.55, 1.84) | |||
| Participant is household head | No | 714 (61%) | 89 (8%) | 143 (12%) | 99 (8%) | 89 (8%) | 32 (3%) | Baseline | 0.38 | Baseline | 0.03 |
| Yes | 94 (57%) | 19 (12%) | 17 (10%) | 13 (8%) | 13 (8%) | 8 (5%) | 1.15 (0.84, 1.58) | 1.47 (1.04, 2.08) | |||
| Household head age | Per unit increase | 1.02 (1.01, 1.02) | 0.001 | 1.01 (1.00, 1.02) | 0.02 | ||||||
| Number of adults in householdb | 1–2 | 266 (67%) | 29 (7%) | 38 (10%) | 29 (7%) | 22 (6%) | 13 (3%) | Baseline | 0.002 | Baseline | 0.05 |
| 3–4 | 376 (60%) | 42 (7%) | 85 (14%) | 52 (8%) | 53 (9%) | 14 (2%) | 1.32 (1.02, 1.71) | < 0.001f | 1.26 (0.95, 1.66) | 0.01f | |
| 5+ | 165 (53%) | 37 (12%) | 37 (12%) | 31 (10%) | 27 (9%) | 13 (4%) | 1.69 (1.26, 2.26) | 1.49 (1.09, 2.03) | |||
| Number of rooms in household | 1–2 | 298 (65%) | 33 (7%) | 50 (11%) | 35 (8%) | 26 (6%) | 13 (3%) | Baseline | 0.03 | Baseline | 0.24 |
| 3–4 | 240 (57%) | 41 (10%) | 57 (14%) | 32 (8%) | 38 (9%) | 13 (3%) | 1.39 (1.07, 1.80) | 1.26 (0.95, 1.66) | |||
| 5+ | 270 (59%) | 34 (7%) | 53 (12%) | 45 (10%) | 38 (8%) | 14 (3%) | 1.31 (1.01, 1.71) | 1.20 (0.90, 1.60) | |||
| Number of adults per room in householdb | < 1 | 325 (60%) | 44 (8%) | 66 (12%) | 49 (9%) | 40 (7%) | 15 (3%) | Baseline | 0.66 | Baseline | 0.89 |
| ≥ 1 and < 2 | 320 (60%) | 40 (8%) | 66 (12%) | 42 (8%) | 44 (8%) | 19 (4%) | 1.02 (0.81, 1.30) | 1.02 (0.80, 1.31) | |||
| ≥ 2 | 162 (63%) | 24 (9%) | 28 (11%) | 21 (8%) | 18 (7%) | 6 (2%) | 0.90 (0.67, 1.20) | 0.95 (0.69, 1.30) | |||
| Ever had sexc | No | 196 (70%) | 19 (7%) | 29 (10%) | 16 (6%) | 15 (5%) | 5 (2%) | Baseline | < 0.001 | Baseline | 0.24 |
| Yes | 611 (58%) | 89 (9%) | 131 (13%) | 95 (9%) | 86 (8%) | 35 (3%) | 1.67 (1.27, 2.21) | 1.22 (0.87, 1.71) | |||
| Age of first sex | Per unit increase | 0.95 (0.91, 0.99) | 0.02 | 0.96 (0.91, 1.01) | 0.12 | ||||||
| Transactional sex, everd | No | 748 (63%) | 92 (8%) | 139 (12%) | 92 (8%) | 91 (8%) | 33 (3%) | Baseline | < 0.001 | Baseline | < 0.001 |
| Yes | 57 (45%) | 16 (13%) | 19 (15%) | 19 (15%) | 9 (7%) | 7 (6%) | 1.84 (1.32, 2.57) | 1.89 (1.34, 2.66) | |||
| Forced sex, last 6 monthse | No | 777 (62%) | 102 (8%) | 152 (12%) | 101 (8%) | 84 (7%) | 34 (3%) | Baseline | < 0.001 | Baseline | < 0.001 |
| Yes | 30 (39%) | 6 (8%) | 7 (9%) | 10 (13%) | 17 (22%) | 6 (8%) | 3.06 (1.98, 4.71) | 3.18 (2.05, 4.93) | |||
| Forcing sex, last 6 monthse | No | 788 (62%) | 102 (8%) | 154 (12%) | 105 (8%) | 91 (7%) | 35 (3%) | Baseline | < 0.001 | Baseline | < 0.001 |
| Yes | 19 (37%) | 6 (12%) | 5 (10%) | 6 (12%) | 10 (20%) | 5 (10%) | 2.99 (1.78, 5.01) | 2.93 (1.74, 4.94) | |||
aAdjusted for study setting, sex and age group
b1 missing value
c3 preferred not to say
d8 preferred not to say
e4 preferred not to say
fTest for trend
Table 3 shows associations between PC-PTSD-5 score as the exposure variable of interest with outcomes of sexual behaviour characteristics, perceptions of HIV risk, attitudes towards PrEP, and drug and alcohol use. After adjusting for study setting, sex and age, group, a higher PC-PTSD-5 score was associated with increased number of partners, and increased odds of the last sexual encounter being with a non-regular partner. There was no evidence of association with any other sexual behaviour characteristics (Table 3).
Table 3.
Associations between post-traumatic stress symptom score (PC-PTSD-5 ≥ 3 versus PC-PTSD-5 < 3) and sexual behaviour, PrEP attitudes and mental health co-morbidities
| Outcome variable and categoriesa | Crude results | Adjusted for study setting, sex and age group | Further adjusted for depression and anxiety | |||
|---|---|---|---|---|---|---|
| ORb (95% CI) | p-value | ORb (95% CI) | p-value | ORb (95% CI) | p-value | |
| Sexual behaviour characteristics | ||||||
| Number partners, last 6 months (0, 1, 2, 3+) | 1.15 (1.08, 1.23) | < 0.001 | 1.08 (1.01, 1.16) | 0.02 | 1.08 (1.01, 1.16) | 0.03 |
| Sex frequency, past month (never, weekly-monthly, >weekly) | 1.14 (1.06, 1.22) | < 0.001 | 1.04 (0.96, 1.12) | 0.32 | 1.03 (0.96, 1.11) | 0.41 |
| Last time had sex, how far in advance knew (> 24 h, 12–23 h, 2–12 h, < 2 h) | 1.04 (0.97, 1.12) | 0.27 | 1.02 (0.95, 1.10) | 0.55 | 1.02 (0.95, 1.10) | 0.55 |
| Condom use last sex with recent partner (no, yes) | 0.94 (0.87, 1.02) | 0.14 | 0.93 (0.85, 1.01) | 0.09 | 0.95 (0.87, 1.03) | 0.23 |
| Type of relationship, most recent partner (regular, casual/paying/other) | 1.11 (1.00, 1.22) | 0.04 | 1.15 (1.03, 1.28) | 0.01 | 1.14 (1.02, 1.27) | 0.02 |
| HIV status, most recent partner (negative, positive/don’t know) | 1.07 (0.98, 1.15) | 0.12 | 1.09 (1.00, 1.18) | 0.05 | 1.09 (1.00, 1.19) | 0.05 |
| General risk taking and HIV salience characteristics | ||||||
| Self-perception of frequency of risk-taking (never, sometimes, often) | 1.16 (1.09, 1.25) | < 0.001 | 1.13 (1.05, 1.21) | 0.001 | 1.12 (1.04, 1.20) | 0.004 |
| Thought about risk of HIV, last 3 months (never, rarely, sometimes, often) | 1.23 (1.15, 1.31) | < 0.001 | 1.18 (1.10, 1.27) | < 0.001 | 1.16 (1.08, 1.25) | < 0.001 |
| Chance of HIV, next 3 months (none, some, moderate/high) | 1.16 (1.08, 1.24) | < 0.001 | 1.10 (1.03, 1.19) | 0.01 | 1.09 (1.01, 1.17) | 0.02 |
| Attitudes towards PrEP | ||||||
| PrEP preference (on demand, daily) | 1.09 (1.01, 1.18) | 0.02 | 1.04 (0.96, 1.13) | 0.32 | 1.04 (0.96, 1.13) | 0.36 |
| Would take PrEP if same price as hot meal (no, yes) | 1.08 (0.99, 1.17) | 0.07 | 1.06 (0.97, 1.15) | 0.18 | 1.07 (0.99, 1.17) | 0.10 |
| Would disclose PrEP to partner (no, yes) | 1.03 (0.95, 1.12) | 0.42 | 1.01 (0.93, 1.09) | 0.85 | 1.02 (0.94, 1.11) | 0.58 |
| Alcohol and drug use | ||||||
| Frequency of binge drinking (don’t drink; never, <monthly, ≥monthly) | 1.21 (1.14, 1.30) | < 0.001 | 1.14 (1.06, 1.23) | < 0.001 | 1.14 (1.06, 1.23) | 0.001 |
| Drug use, last 30 days (no, yes) | 1.14 (1.03, 1.26) | 0.01 | 1.08 (0.96, 1.22) | 0.19 | 1.06 (0.94, 1.19) | 0.34 |
aFor binary outcome variables, the reference group is listed first; for ordered categorical outcome variables, the categories are listed in order;
bOdds ratio represent the increase in odds for a one unit increase in PC-PTSD-5 score
There was strong evidence that PC-PTSD-5 score was associated with increased self-perceived risk taking, both assessed on a three-point Likert scale (OR 1.12, 95% CI: 1.04–1.20, p = 0.004) and as a continuous scale between 0 (unwilling to take risks) and 10 (always willing to take risks): adjusted difference in mean self-perceived risk-taking score 0.16 (95% CI: 0.07–0.26, p = 0.001) for each unit increase in PC-PTSD-5 score. There was also strong evidence that PC-PTSD-5 score was associated with the frequency of thinking about the risk of HIV in the last 3 months (OR 1.16, 95% CI: 1.08–1.25, p < 0.001) and with perceived chance of acquiring HIV in the next 3 months (OR 1.09, 95% CI: 1.01–1.17, p = 0.02). In adjusted analyses, there was no evidence of an association of PC-PTSD-5 score with preference for daily versus on demand PrEP, willingness to take PrEP if it cost the same as a hot meal, willingness to disclose PrEP use to a partner, or drug use but there was evidence of an association with increased frequency of binge drinking, both before and after adjusting for depression and anxiety (adjusted OR 1.14, 95% CI: 1.06–1.23, p = 0.001). Results from analyses analysing PC-PTSD-5 score as a binary variable (≥ 3 versus < 3) were consistent (Additional file 1: Tables S1, S2).
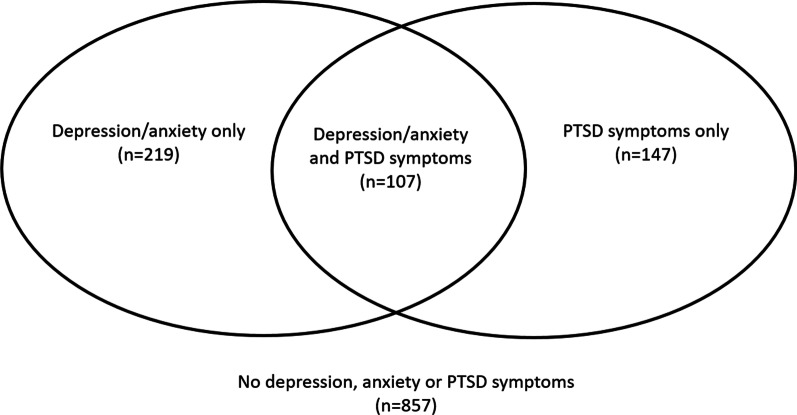
Of the 254 participants with PC-PTSD-5 ≥ 3, 147 (57%) did not report symptoms of either depression or anxiety (Fig. 1). As noted above, adjustment for these co-morbidities had little impact on most associations reported. We included interaction terms to assess whether the association of PC-PTSD-5 score with outcomes differed in the presence (versus absence) of these other mental health co-morbidities. For nearly all outcomes assessed, there was no evidence that their association with PC-PTSD-5 score differed in the presence versus absence of depression and/or anxiety. The only exception was for the type of relationship with the most recent partner (interaction p-value 0.02): among people who had depression or anxiety, PC-PTSD-5 score was associated with higher odds of casual sex (adjusted OR 1.35, 95% CI: 1.13–1.61) but there was no association of PC-PTSD-5 score with causal sex among those who did not have depression or anxiety (adjusted OR 1.03, 95% CI: 0.89–1.19).
Fig. 1.
The overlap between PTSD, depression and anxiety in CHAPS survey participants
Discussion
In this large cross-sectional study of young people aged 13–24 years from four different settings in South Africa, Uganda and Zimbabwe, symptoms of post-traumatic stress disorder were common. Young people with a higher PC-PTSD-5 score had increased odds of reporting forced sex or forcing someone else to have sex. PTSD symptoms were also associated with increased number of sexual partners, recent sex with a non-regular partner, increased self-perception as a person who takes risks, with the frequency of thinking about the risk of HIV, and with binge drinking. However, contrary to our hypotheses, after controlling for confounders we did not find evidence that PTSD symptoms were associated with willingness to take PrEP, disclose PrEP use or preference for daily versus on-demand PrEP.
The level of PTSD symptoms reported in CHAPS survey participants is consistent with estimates from other general population settings in SSA [9], and from youth in low- and middle-income countries [36]. Our results also align with findings from South Africa suggesting that links between probable PTSD and other socio-demographic factors such as education are not as evident as in high-income countries [37]. The high level of PTSD symptoms in this sample of young people, with the caveat that this is a non-probability based sample and thus study participants are not representative of all youth in these settings, suggests that evaluation for PTSD should form part of a general assessment in sexual and reproductive health services in these countries.
PTSD symptoms often co-existed with depression and anxiety in our study participants, however around 60% of participants with a PC-PTSD-5 score ≥ 3 were not classified as having either depression or anxiety, a higher proportion than was observed in a study among youth from a European setting [38], which assessed mental disorders using a diagnostic interview. PTSD symptoms remained independently and strongly associated with forced sex, self-perception as a person who takes risks, and frequency of thinking about the risk of HIV, regardless of whether or not the participant also had symptoms of depression or anxiety. In other words, even among participants who did not have depression or anxiety, PTSD symptoms were associated with these outcomes. However, there was a suggestion of an association between PTSD symptoms and casual sex only among those with depression or anxiety, which was not seen among those without these co-morbidities.
Contrary to our hypothesis, we found little evidence that PTSD symptoms were associated with willingness to take PrEP, willingness to disclose PrEP usage or preference for on-demand versus daily PrEP. Furthermore, results from the same study demonstrated that depression and anxiety symptoms (without consideration of PTSD score) were similarly not associated with willingness to take PrEP or with preference for on demand versus daily PrEP, although they were associated with participant-held concerns that they would be more likely to have riskier sex if they were to take PrEP [28]. Possible explanations for this lack of association include the fact that many participants were unfamiliar with PrEP before taking part in the survey and this may have precluded them from forming opinions on PrEP that could in turn be influenced by any underlying mental health conditions. Furthermore, since both daily and on demand PrEP regimens were described to participants before collecting information on their attitudes towards PrEP, it is plausible that PrEP might not be considered in the same way as medications which are designed to be taken daily, such as ARVs for which previous evidence has suggested that trauma may be a barrier to adherence. However, given the limitations discussed below with ascertaining PTSD, further work is needed to understand whether past trauma should be specifically considered when delivering PrEP.
We found some evidence that PTSD symptoms were associated with sexual behaviour, consistent with previous findings which have related increased traumatic experience exposure to high risk sexual behaviour. For example, a positive association between childhood sexual violence and infrequent condom use and an increased number of partners has been reported among young people in Tanzania [13]. In South Africa lifetime traumatic experiences have been correlated with transactional sex and the number of sexual partners [39]. Since this was a cross-sectional survey, we were not able to assess causality, however the observed association of probable PTSD with forced sex may indicate that probable PTSD occurred as a consequence of forced sex for some participants.
A key limitation of this work is that it did not use a tool that has been validated for assessing probable PTSD in this population. As described previously [22], the overarching aim of the CHAPS survey was to identify barriers and motivators towards the uptake of PrEP, of which PTSD was one of several considered; thus the survey tool included only a brief screen for traumatic experiences and consequent feelings, which has been validated for use in identifying US veterans with probable PTSD [24], and validated among young people in the US [26] and previously used but not validated in young people in SSA [27]. For this reason, our primary analysis is based on the PC-PTSD-5 score rather than based on a specific cutpoint for this tool. We also did not collect information on the types of traumatic experiences that led to the reporting of symptoms. Other studies have shown that childhood traumas are highly prevalent among young people in urban communities in South Africa [14] and associated with PTSD [40]; exposure to violence, particularly sexual violence is also common [41, 42]. However, in the absence of a more in-depth assessment, we cannot speculate on the possible causes of probable PTSD.
Further limitations of the analysis include the cross-sectional study design, which precludes conclusions about the direction of causation. Participants were recruited into the study through a community outreach approach, and not through a probability-based sampling approach. Thus they are not be representative of all young people in their communities, so that our results may not be generalisable to all young people in these settings, and we cannot make comparisons between the different study settings in terms of prevalence. This also means that we cannot obtain an estimate of response rate, thus we cannot assess whether characterstics of our participants were similar to those of others who were made aware of the study but chose not to take part. Data collected were self-reported, which could have introduced measurement bias, with some behavioural variables in particularly likely to be subject to underreporting. Our study had several strengths including the large sample size which provided good power to detect associations, and the inclusion of participants from different settings in SSA.
Conclusions
In summary, PTSD symptoms were common in young people in South Africa, Uganda and Zimbabwe and associated with forced sex but not with other sexual behaviour characteristics or with attitudes towards PrEP. Further work should employ a PTSD tool that has been specifically validated in the target population, and should also assess possible causes of PTSD. Although mental health screening for depression and anxiety should be incorporated into PrEP counselling as it can impact adherence to PrEP [19, 20], the impact of PTSD on PrEP adherence is not known and needs investigation. The large proportion of young people with symptoms suggestive of probable PTSD in the absence of anxiety or depression suggests that young people should be screened for PTSD as well as for other common mental disorders. Such evaluation might form part of a general assessment in sexual and reproductive health services in these countries.
Supplementary Information
Additional file 1: Table S1. Associations between socio-demographic characteristics, historical sexual behaviour and post-traumatic stress symptoms (PC-PTSD-5 ≥3). Table S2. Associations between post-traumatic stress symptom score (PC-PTSD-5≥3 versus PC-PTSD-5<3) and sexual behaviour, PrEP attitudes and mental health co-morbidities.
Acknowledgements
We would like to recognize the study participants, their communities and the CHAPS study teams in Uganda, South Africa and Zimbabwe.
Abbreviations
- CHAPS
Combined HIV Adolescent PrEP and Prevention Study
- CI
Confidence interval
- DSM-5
Diagnostic and Statistical Manual of Mental Disorders
- GAD-2
Generalized Anxiety Disorder-2
- MRC
Medical Research Council
- OR
Odds ratio
- PC-PTSD-5
Primary Care PTSD Screen for DSM-5
- PHQ-9
Patient Health Questionnaire
- PrEP
Pre-exposure prophylaxis
- PTSD
Post traumatic stress disorder
- SSA
Sub-Saharan Africa
Author contributions
ELW analysed the data and wrote the first draft of the manuscript. JJD, LGB, HAW, JS, LSC, JF conceived and designed the study. ASS, TGN, SH, GT, RM, MA, TB participated in data collection. AK, GM contributed to data management and analysis. TGN, MAA, HAW, LSC, JF contributed to data interpretation and manuscript revisions. All authors read and approved the final version of the manuscript.
Funding
This publication was produced by Project CHAPS which is part of the EDCTP2 programme supported by the European Union (Grant number RIA2016MC-1616-CHAPS, J. Fox). ELW and HAW were part funded by an award from the UK Medical Research Council (MRC) (Grant reference: MR/R010161/1, H. Weiss); this award is jointly funded the UK MRC and the UK Department for International Development (DFID) under the MRC/DFID Concordat agreement and is also part of the EDCTP2 programme supported by the European Union. The work reported herein for JJD was made possible through funding by the South African Medical Research Council (SAMRC) through its Division of Research Capacity Development under the SAMRC Postdoctoral Programme (for funding received from the South African National Treasury) as well as the CIPHER GROWING THE LEADERS OF TOMORROW grant from the International AIDS Society. SH is supported by the Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (Grant No-B 8606.R02), Sida (Grant No:54100029), the DELTAS Africa Initiative (Grant No: 107768/Z/15/Z).
The funding bodies had no role in the design of the study or in the collection, analysis and interpretation of data or in writing the manuscript.
Availability of data and materials
The analysis dataset will be made available upon request and accessed through the LSHTM Data Compass repository (https://datacompass.lshtm.ac.uk/).
Declarations
Ethics approval and consent to participate
Approval was obtained from the Human Research Ethics Committees of the University of Cape Town (290/2018) and the University of the Witwatersrand (180906B, M1811148 and 180108) in South Africa, the Uganda Virus Research Institute Research and Ethics Committee (GC127/18/3/638) and Uganda National Council for Science and Technology (HS2534) in Uganda, the Joint Research Ethics Committee for the University of Zimbabwe Faculty of Medicine and Health Sciences and the Parirenyatwa Group of Hospitals (JREC/195/18), the Medical Research Council of Zimbabwe and the Research Council of Zimbabwe (MRCZ/A/2356) in Zimbabwe, and the London School of Hygiene and Tropical Medicine Ethics Committee (15629 and 16182) in the UK. The procedures used in this study adhere to the tenets of the Declaration of Helsinki. Written, informed consent to participate in the study was obtained from all participants aged 18 years or over and written, informed parental consent was obtained for participants aged under 18 years. A waiver of parental consent for emancipated minor participants was approved by ethical boards for use in Cape Town, Wakiso and Chitungwiza.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UNAIDS. Global HIV & AIDS statistics—2020 fact sheet. 2020.
- 2.Collaborators GH. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet HIV. 2019;6(12):e831-e59. [DOI] [PMC free article] [PubMed]
- 3.Karim SSA, Baxter C. HIV incidence rates in adolescent girls and young women in sub-Saharan Africa. Lancet Glob Health. 2019;7(11):e1470-e1. doi: 10.1016/S2214-109X(19)30404-8. [DOI] [PubMed] [Google Scholar]
- 4.Organisation WH. WHO implementation guidance for pre-exposure prophylaxis of HIV infection. Geneva: World Health Organisation; 2016. [Google Scholar]
- 5.Cowan FM, Delany-Moretlwe S, Sanders EJ, Mugo NR, Guedou FA, Alary M, et al. PrEP implementation research in Africa: what is new? J Int AIDS Soc. 2016;19(7(Suppl 6):21101. doi: 10.7448/IAS.19.7.21101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Organisation WH. Health for the world’s adolescents: a second chance in the second decade. Geneva: World Health Organisation; 2014. [Google Scholar]
- 7.Yehuda R. Post-traumatic stress disorder. N Engl J Med. 2002;346(2):108–14. doi: 10.1056/NEJMra012941. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, et al. Trauma and PTSD in the WHO World Mental Health Surveys. Eur J Psychotraumatol. 2017;8(sup5):1353383. doi: 10.1080/20008198.2017.1353383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ng LC, Stevenson A, Kalapurakkel SS, Hanlon C, Seedat S, Harerimana B, et al. National and regional prevalence of posttraumatic stress disorder in sub-Saharan Africa: a systematic review and meta-analysis. PLoS Med. 2020;17(5):e1003090. doi: 10.1371/journal.pmed.1003090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rytwinski NK, Scur MD, Feeny NC, Youngstrom EA. The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. J Trauma Stress. 2013;26(3):299–309. doi: 10.1002/jts.21814. [DOI] [PubMed] [Google Scholar]
- 11.Gros DF, Price M, Magruder KM, Frueh BC. Symptom overlap in posttraumatic stress disorder and major depression. Psychiatry Res. 2012;196(2–3):267–70. doi: 10.1016/j.psychres.2011.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flory JD, Yehuda R. Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialogues Clin Neurosci. 2015;17(2):141–50. doi: 10.31887/DCNS.2015.17.2/jflory. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiang LF, Chen J, Gladden MR, Mercy JA, Kwesigabo G, Mrisho F, et al. HIV and childhood sexual violence: implications for sexual risk behaviors and HIV testing in Tanzania. AIDS Educ Prev. 2015;27(5):474–87. doi: 10.1521/aeap.2015.27.5.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gibbs A, Dunkle K, Washington L, Willan S, Shai N, Jewkes R. Childhood traumas as a risk factor for HIV-risk behaviours amongst young women and men living in urban informal settlements in South Africa: a cross-sectional study. PLoS ONE. 2018;13(4):e0195369. doi: 10.1371/journal.pone.0195369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jewkes RK, Dunkle K, Nduna M, Jama PN, Puren A. Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse Negl. 2010;34(11):833–41. doi: 10.1016/j.chiabu.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dow DE, Turner EL, Shayo AM, Mmbaga B, Cunningham CK, O’Donnell K. Evaluating mental health difficulties and associated outcomes among HIV-positive adolescents in Tanzania. AIDS Care. 2016;28(7):825–33. doi: 10.1080/09540121.2016.1139043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watt MH, Dennis AC, Choi KW, Ciya N, Joska JA, Robertson C, et al. Impact of sexual trauma on HIV care engagement: perspectives of female patients with trauma histories in Cape Town, South Africa. AIDS Behav. 2017;21(11):3209–18. doi: 10.1007/s10461-016-1617-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehrotra ML, Glidden DV, McMahan V, Amico KR, Hosek S, Defechereux P, et al. The effect of depressive symptoms on adherence to daily oral PrEP in men who have sex with men and transgender women: a marginal structural model analysis of the iPrEx OLE study. AIDS Behav. 2016;20(7):1527–34. doi: 10.1007/s10461-016-1415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Velloza J, Baeten JM, Haberer J, Ngure K, Irungu E, Mugo NR, et al. Effect of depression on adherence to Oral PrEP among men and women in East Africa. J Acquir Immune Defic Syndr. 2018;79(3):330–8. doi: 10.1097/QAI.0000000000001821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Velloza J, Heffron R, Amico KR, Rowhani-Rahbar A, Hughes JP, Li M, et al. The effect of depression on adherence to HIV pre-exposure prophylaxis among high-risk South African Women in HPTN 067/ADAPT. AIDS Behav. 2020;24(7):2178–87. doi: 10.1007/s10461-020-02783-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayer CM, Siddiqui RD, Adams MA, Strauss B, Mathur A, Tristram DA, et al editors. Retention among adolescents with mental health diagnoses on pre-exposure prophylaxis (RAMP) study. Washington DC: Open Forum Infectious Diseases; 2019.
- 22.Nash S, Dietrich J, Ssemata AS, Herrera C, O’Hagan K, Else L, et al. Combined HIV adolescent prevention study (CHAPS): comparison of HIV pre-exposure prophylaxis regimens for adolescents in sub-Saharan Africa-study protocol for a mixed-methods study including a randomised controlled trial. Trials. 2020;21(1):900. doi: 10.1186/s13063-020-04760-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cresswell JW, Plano Clark VL. Designing and conducting mixed method research. 3. Thousand Oaks: SAGE; 2017. [Google Scholar]
- 24.Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, et al. The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med. 2016;31(10):1206–11. doi: 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bovin MJ, Kimerling R, Weathers FW, Prins A, Marx BP, Post EP, et al. Diagnostic accuracy and acceptability of the primary care posttraumatic stress disorder screen for the diagnostic and statistical manual of mental disorders (Fifth Edition) among US Veterans. JAMA Netw Open. 2021;4(2):e2036733. doi: 10.1001/jamanetworkopen.2020.36733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soleimanpour S, Schapiro NA, Faxio A, Brindis CD. A preliminary study examining the validity of brief trauma screening tools for young adolescents in School-Based Health Centers. J Nurs Meas. 2021;29(1):53–65. doi: 10.1891/JNM-D-19-00043. [DOI] [PubMed] [Google Scholar]
- 27.Haas AD, Technau KG, Pahad S, Braithwaite K, Madzivhandila M, Sorour G, et al. Mental health, substance use and viral suppression in adolescents receiving ART at a paediatric HIV clinic in South Africa. J Int AIDS Soc. 2020;23(12):e25644. doi: 10.1002/jia2.25644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nematadzira T, editor. Effect of common mental disorder symptoms and substance use on attitudes towards PrEP among young people in South Africa, Uganda and Zimbabwe HIVR4P; 2020; Virtual conference.
- 29.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akena D, Joska J, Obuku EA, Stein DJ. Sensitivity and specificity of clinician administered screening instruments in detecting depression among HIV-positive individuals in Uganda. AIDS Care. 2013;25(10):1245–52. doi: 10.1080/09540121.2013.764385. [DOI] [PubMed] [Google Scholar]
- 31.Botha M. Validation of the patient health questionnaire (PHQ-9) in an African context Northwest University.
- 32.Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184(3):E191-6. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sapra A, Bhandari P, Sharma S, Chanpura T, Lopp L. Using generalized anxiety disorder-2 (GAD-2) and GAD-7 in a primary care setting. Cureus. 2020;12(5):e8224. doi: 10.7759/cureus.8224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chibanda D, Verhey R, Gibson LJ, Munetsi E, Machando D, Rusakaniko S, et al. Validation of screening tools for depression and anxiety disorders in a primary care population with high HIV prevalence in Zimbabwe. J Affect Disord. 2016;198:50–5. doi: 10.1016/j.jad.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 35.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 36.Yatham S, Sivathasan S, Yoon R, da Silva TL, Ravindran AV. Depression, anxiety, and post-traumatic stress disorder among youth in low and middle income countries: a review of prevalence and treatment interventions. Asian J Psychiatr. 2018;38:78–91. doi: 10.1016/j.ajp.2017.10.029. [DOI] [PubMed] [Google Scholar]
- 37.Atwoli L, Stein DJ, Williams DR, McLaughlin KA, Petukhova M, Kessler RC, et al. Trauma and posttraumatic stress disorder in South Africa: analysis from the South African Stress and Health Study. BMC Psychiatry. 2013;13:182. doi: 10.1186/1471-244X-13-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perkonigg A, Kessler RC, Storz S, Wittchen HU. Traumatic events and post-traumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiatr Scand. 2000;101(1):46–59. doi: 10.1034/j.1600-0447.2000.101001046.x. [DOI] [PubMed] [Google Scholar]
- 39.Gibbs A, Hatcher A, Jewkes R, Sikweyiya Y, Washington L, Dunkle K, et al. Associations between lifetime traumatic experiences and HIV-risk behaviors among young men living in informal settlements in South Africa: a cross-sectional analysis and structural equation model. J Acquir Immune Defic Syndr. 2019;81(2):193–201. doi: 10.1097/QAI.0000000000002010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Choi KW, Sikkema KJ, Velloza J, Marais A, Jose C, Stein DJ, et al. Maladaptive coping mediates the influence of childhood trauma on depression and PTSD among pregnant women in South Africa. Arch Womens Ment Health. 2015;18(5):731–8. doi: 10.1007/s00737-015-0501-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Otwombe KN, Dietrich J, Sikkema KJ, Coetzee J, Hopkins KL, Laher F, et al. Exposure to and experiences of violence among adolescents in lower socio-economic groups in Johannesburg, South Africa. BMC Public Health. 2015;15:450. doi: 10.1186/s12889-015-1780-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scorgie F, Baron D, Stadler J, Venables E, Brahmbhatt H, Mmari K, et al. From fear to resilience: adolescents’ experiences of violence in inner-city Johannesburg, South Africa. BMC Public Health. 2017;17(Suppl 3):441. doi: 10.1186/s12889-017-4349-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Associations between socio-demographic characteristics, historical sexual behaviour and post-traumatic stress symptoms (PC-PTSD-5 ≥3). Table S2. Associations between post-traumatic stress symptom score (PC-PTSD-5≥3 versus PC-PTSD-5<3) and sexual behaviour, PrEP attitudes and mental health co-morbidities.
Data Availability Statement
The analysis dataset will be made available upon request and accessed through the LSHTM Data Compass repository (https://datacompass.lshtm.ac.uk/).