Abstract
Background:
The use of complementary and integrative medicine (CIM) continues to grow in palliative care. While research supports the use of many CIM therapies for symptom relief, the scope of provider-focused research on CIM remains poorly characterized.
Objectives:
We conducted a scoping review to characterize provider-focused research on CIM in palliative care in order to map existing evidence and identify knowledge gaps.
Methods:
We developed a protocol outlining the study population, concept, and context; then used a validated approach per the JBI manual and searched MEDLINE, EMBASE, CINAHL, and AMED.
Results:
We identified 34 studies that were conducted primarily in the US (n = 9) and UK (n = 6), focused mostly on nurse (n = 29) and physician (n = 22) providers, and employed questionnaires (n = 16) or qualitative (n = 15) methods. Studies investigated 58 CIM modalities, including massage (n = 13), music therapy (n = 12), and aromatherapy (n = 10), to address common symptoms including pain (n = 17), fatigue (n = 6), and nausea/vomiting (n = 6). Study outcomes included perceived benefits of CIM (n = 17) and types of CIM modalities that providers offer (n = 15). Uncommonly studied phenomena included referral patterns (n = 4), facilitators of provider recommendation of CIM (n = 3), and rates of CIM use (n = 3).
Conclusion:
Provider-focused research on CIM in palliative care can expand its scope by addressing perspectives of interdisciplinary providers, examining CIM modalities that patients report using, addressing symptoms commonly encountered in palliative care, and researching provider-use-focused outcomes. We identify these possibilities for future studies in addition to opportunities for systematic investigations to enhance the safe and efficacious delivery of CIM in the palliative care setting.
Keywords: palliative care, complementary, integrative, alternative, attitudes, scoping review
Introduction
As the use of hospice and palliative services grows,1,2 so too does the need to address prevalent and burdensome symptoms in patients receiving palliative care, including pain, depression, dyspnea, constipation, nausea and vomiting, and sleep disturbance.3–6 Collectively, these symptoms negatively impact quality-of-life of affected patients and their families.7 Patients are turning to complementary and integrative medicine (CIM) therapies to help mitigate these symptoms.8 As many as 1 in 3 Americans use CIM,8,9 and as many as 42% of hospices in the United States have offered CIM to patients.10
Prior studies have reported on patient perspectives and attitudes toward, rates of use of, and symptoms for which they use CIM.8,11 In addition, controlled experiments and systematic reviews have investigated the safety and efficacy of specific CIM modalities. Research has shown benefit associated with the use of yoga, acupuncture, tai-chi, meditation, music therapy, and massage for patients with chronic pain12,13; acupuncture, music therapy, and yoga for symptoms of depression14–17; and meditation and herbal medicines for symptoms of anxiety.18,19 Other studies have shown limited evidence for the use of reiki for pain, St. John’s Wort for depression, and biofeedback for anxiety.20–22 Regardless of the strength of evidence, patients are using a variety of CIM modalities to address a spectrum of symptoms.8,11 These trends underscore the importance of conducting research to enhance the uptake and knowledge of CIM among palliative care providers to ensure safe and efficacious use of these modalities.
There are no consensus findings regarding palliative care provider-focused phenomena related to CIM, including providers’ usage patterns, knowledge base, attitudes, and details surrounding their actual delivery of CIM. The limited existing literature did not support systematic investigations of these and related outcomes. Therefore, we sought to conduct a scoping review to characterize the types of research on provider-focused phenomena related to CIM in the palliative care setting. Whereas systematic reviews summarize evidence to answer a clinical question, scoping reviews examine the literature to map existing evidence, describe the breadth and depth of research to identify trends and knowledge gaps, and understand research methods employed in a field, without analyzing the evidence and its quality. Shedding light on provider-focused outcomes related to CIM can enhance the uptake and delivery of CIM in palliative care, ensure evidence-based use, and improve communication between patients and providers about CIM.
Methods
Overview
We employed the validated JBI methodology for scoping reviews,23 developing an iterative protocol and defining the population, concept, and context (PCC) for the study. We described the population as any interdisciplinary healthcare provider (e.g., MD, DO, NP, PA, RN, Social Worker, Chaplain) that may recommend or administer CIM in the palliative care setting.
The core concept of this scoping review is provider-focused outcomes related to CIM. We defined CIM as non-mainstream practices that can be used alone or along with conventional medicine, or the coordinated use of both.24 We defined provider-focused research as studies in which subjects were providers, and outcomes were related to provider perspectives of, attitudes toward, and usage of CIM.
The context of the scoping review was CIM in the palliative care setting. We defined palliative care as any interdisciplinary effort to improve quality of life for patients of any age with advanced illness and their family members. In addition, we defined the setting of palliative care broadly to include both the acute (hospital) and outpatient setting, as well as care delivered at home (e.g., hospice care). In our pilot screening, we noted a significant number of articles focusing on the use of CIM as supportive care in the setting of patients receiving both curative and non-curative treatment for chronic and terminal medical conditions. In these cases, we only included those that made explicit mentions of palliative care or hospice providers, or palliative care or hospice settings.
Search Strategy
We employed a 3-step search strategy. We first performed an initial limited search of MEDLINE (via PubMed) followed by an analysis of the text words contained in the title and abstract, and of the index terms used to describe the resulting articles. We then performed a second search using all identified keywords and index terms with the following databases: MEDLINE, EMBASE, CINAHL Plus with Full Text, and AMED. We carried out a third and final search of the reference list of all included articles (backward) as well as all those articles citing the included articles (forward) to identify additional studies. The a priori definition of the PCC allowed customization of the search terms to work within each database (see Appendix Table 1 for an example of the search strategy within MEDLINE). This was especially important when defining the CIM modality search terms for each database. As there are no standard lists of CIM modalities, and past systematic reviews related to CIM broadly demonstrated no consistency in modalities included in searches,21,25–28 we constructed a cumulative list of the specific modalities nested under each database’s subject headings related to complementary, integrative, and alternative medicine and then added any other modalities searched for in these past systematic reviews. We consulted with integrative medicine specialists to narrow this list to acomprehensive but reasonably concise list of individual CIM modalities to search in the titles and abstracts along with each database’s broad CIM subject headings and nested terms. We searched for studies published with no start-date-limit through 12/31/2020.
Screening, Selection, and Extraction
After compiling the search results in Covidence,29 2 reviewers (A.G., H.E.) independently assessed the articles for relevance based on the information provided in the title and abstract. The PCC framework guided the search and therefore the inclusion and exclusion criteria. Additional inclusion criteria that were not accounted for in our search filters included only accepting full-text articles published in English. With respect to study design, we considered both quantitative and qualitative studies, as well as reviews. Quantitative designs included any experimental study designs (e.g., controlled trials or other quasi-experimental studies), and observational designs (e.g., descriptive studies, questionnaires, cohort studies, cross-sectional studies). Qualitative designs included any studies that focused on generating qualitative data such as, but not limited to, phenomenology, grounded theory and ethnography designs. We excluded non-experimental literature, such as reports, letters, opinions, case studies, and articles describing development or implementation of programs. At this stage, a significant number of articles were removed that did not pertain to CIM. If the reviewers had doubts about the relevance of a study from the abstract, the full-text article was reviewed for eligibility.
We retrieved the full-text article for all studies that passed this initial screen. Two reviewers (A.G., H.E.) independently examined the full-text articles to determine whether they met the inclusion criteria, again guided by the PCC framework. Any disagreements between reviewers at either stage of screening were resolved through discussion or by a third reviewer (M.P.). We screened studies identified from forward and backward reference search based on their title and abstract.
Two reviewers (A.G., H.E.) independently extracted data from retained articles using a charting instrument we designed based on our research objectives and questions, as indicated by the JBI methodology for scoping reviews.23 Any disagreements that arose between the reviewers were resolved through discussion or by a third reviewer (M.P.).
Data Analysis
For qualitative data points including CIM modalities, diseases, symptoms, and study outcomes-of-interest, 2 reviewers (A.G., H.E.) independently coded these data for further analysis once they had been extracted. We used existing thematic frameworks to analyze CIM modalities24 and symptoms.30 To identify the phenomena- and outcomes-of-interest for each study we relied on the results and discussion headers from all articles, the data tables and figures from quantitative studies, and the reported qualitative data for qualitative studies. As there was no existing framework for coding these outcomes, we reviewed the extracted data and categorized them into codes and themes, resolving conflicts and revising the framework in an iterative fashion employing a constant comparative method.31
Quality Control
We took measures to assure quality control throughout the review process. First, we designed the scoping review protocol a priori, defining the research question, PCC framework, the search strategy, inclusion and exclusion criteria, and data extraction tool. In addition, at the initial (n = 6,794) and full-text (n = 127) screening stages, both reviewers (A.G., H.E.) conducted a pilot screen, each independently reviewing the same 25 articles followed by a discussion of the results to adjust the protocol for clarity as necessary. At the initial data extraction stage (n = 30), the reviewers independently charted the first 5 studies using the pilot data-extraction form, then met to revise the form in order to ensure the form captured the data that would most accurately address the research question. At the data analysis stage, the authors formed a data dictionary for coding of outcomes as described above, and this was considered an iterative document with co-authors suggesting changes as necessary. Finally, we consulted with reference librarians when designing the search and screen methodologies.
Results
Overview
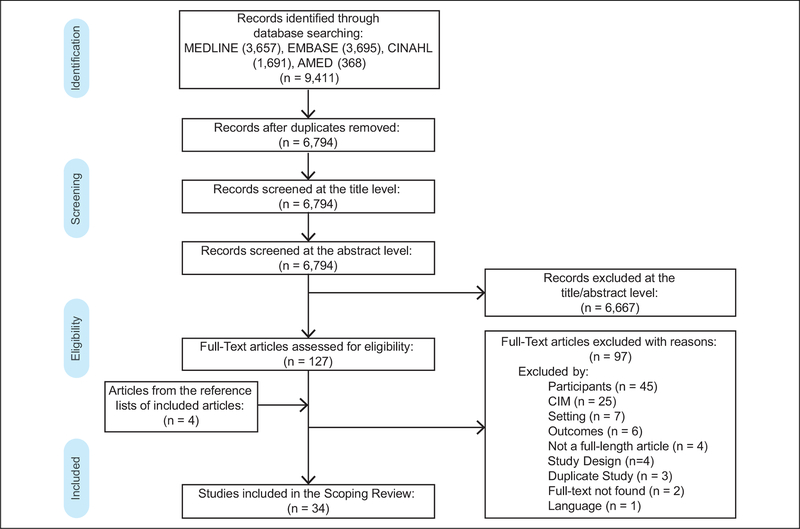
The electronic database searches yielded 9,411 records (MEDLINE: 3,657, EMBASE: 3,695; CINAHL: 1,691; and AMED: 368), which were reduced to 6,794 after de-duplication, which removes copies of citations that resulted in multiple database searches. The title and/or abstract screening of these records left 127 articles that we assessed through full-text screening, of which 30 met criteria for inclusion. A review of their reference lists identified an additional 4 studies, for a final sample of 34 articles.32–65 Figure 1 provides a Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of the screening process. Table 1 shows summary characteristics (e.g., publication year, country of publication, setting, participants/data source, and study design) of the final sample of retained articles. These results demonstrate a secular trend with an increasing number of studies being published in the past 5 years (n = 14). In addition, most studies focused on nurse (n = 29) and physician (n = 22) providers and on the delivery of CIM in the inpatient palliative care setting (n = 20) (Table 1).
Figure 1.
PRISMA flow diagram.
Table 1.
Summary Characteristics of Scoping Review Sample (N = 34).
| Characteristic | Frequency |
|---|---|
| Publication Year | |
| 1990–1995 | 1 |
| 1996–2000 | 1 |
| 2001–2005 | 3 |
| 2005–2010 | 8 |
| 2011–2015 | 7 |
| 2016–2021 | 14 |
| Country of Publication | |
| USA | 9 |
| UK | 6 |
| Australia | 5 |
| Germany | 3 |
| Canada | 2 |
| Japan | 2 |
| Austria | 1 |
| Hong Kong | 1 |
| South Africa | 1 |
| Taiwan | 1 |
| Tanzania | 1 |
| Zambia | 1 |
| Not applicablea | 1 |
| Study Design | |
| Questionnaire | 16 |
| Qualitative semi-structured individual interviews | 10 |
| Qualitative unstructured individual interviews | 2 |
| Qualitative semi-structured focus group interviews | 1 |
| Qualitative structured individual interviews | 1 |
| Quasi-experimental: pre-test/post-test | 1 |
| Mixed Methods: Questionnaire + Quasi-experimental: pre-test/post-test | 1 |
| Mixed Methods: Qualitative semi-structured focus group interviews + Qualitative semi-structured individual interviews | 1 |
| Scoping Review | 1 |
| Participantsb | |
| Nurse | 29 |
| Physician | 22 |
| Social Worker | 8 |
| Chaplain | 7 |
| CIM Therapist | 6 |
| Physiotherapist | 5 |
| Psychologists | 5 |
| Radiation Therapist | 4 |
| Occupational Therapist | 3 |
| Pharmacist | 2 |
| Physician Assistant | 1 |
| Respiratory Therapist | 1 |
| Clinical Educator | 1 |
| Study Settingb | |
| Inpatient Palliative Care | 20 |
| Hospice | 12 |
| Cancer Center | 12 |
| Outpatient Palliative Care | 7 |
| Home Hospice | 5 |
| Unspecified | 4 |
| Pediatric Hospice | 2 |
One study was a scoping review, and thus it is not possible to report the country in which the study was conducted.
Total number exceeds sample size as studies were able to fall within more than 1 category.
For these and other primary outcomes, we present the summary data by article in Table 2. The complete thematic analyses for study phenomena-of-interest, CIM modalities, and symptoms targeted appear in Table 3, Appendix Table 2 and Appendix Table 3, respectively.
Table 2.
Detailed Characteristics of Scoping Review Sample (N = 34).
| Article | Type of source | Participants | Setting(s) | CIM modalities | Diseases | Symptoms | Outcomes/phenomena |
|---|---|---|---|---|---|---|---|
| Amadoru and McFerran32 | Qualitative unstructured individual interviews | Nurse, Other | Pediatric Hospice | Music Therapy | Unspecified | Unspecified | Attitude toward Integration, General Attitude, Perceived Benefits, Types of CIM Offered |
| Atkin, et al33 | Questionnaire | Physician | Inpatient Palliative Care, Outpatient Palliative Care | Unspecified | Unspecified | Anxiety | Access/Availability, Rates of Use, Symptoms Addressed |
| Broom and Tovey34 | Qualitative semi-structured individual interviews | CIM Provider, Nurse, Occupational Therapist, Pharmacist, Physician, Radiation Therapist | Cancer Center, Hospice, Inpatient Palliative Care | Unspecified | Cancer | Unspecified | Attitudes Toward Integration, Communication/Collaboration, General Attitudes, Perceived Barriers, Perceived Efficacy, Perceptions of Evidence Base, Referral Patterns, Symptoms Addressed |
| Bucher, et al35 | Quasi-experimental: pre-test / post-test | Nurse, Other | Inpatient Palliative Care | Breathing Techniques, Essential Oils, Massage | Unspecified | Unspecified | Knowledge of CIM, Likely to Provide, Likely to Recommend, Sufficient Time |
| Campbell and Amin36 | Qualitative unstructured individual interviews | Nurse, Other | Home Hospice | Traditional Healer | Unspecified | Unspecified | Communication/Collaboration, General Attitudes, Perceived Barriers, Perceived Benefits, Types of CIM Offered |
| Christina, et al37 | Qualitative semi-structured individual interviews | Nurse | Cancer Center, Inpatient Palliative Care | Herbal Therapy, Traditional Chinese Medicine, Unspecified | Cancer | Unspecified | General Attitudes, Knowledge of CIM, Personal Use, Sources of Information, Symptoms Addressed, Types of CIM Offered, Willingness to Learn |
| Coelho, et al38 | Scoping review | n/a | Hospice, Home Hospice, Inpatient Palliative Care, Outpatient Palliative Care | Aromatherapy, Art Therapy, Biofeedback, Footsoak, Hypnotherapy, Massage, Music Therapy, Reflexology, Reiki, Therapeutic Touch | Unspecified | Anxiety, Depression, Discomfort, Distress, Fatigue, Pain, Suffering, Well-Being | Characteristics of Delivery, Symptoms Addressed, Contexts for CIM, Patient Characteristics, Types of CIM Offered |
| Conrad, et al39 | Questionnaire | Chaplain, Nurse, Physician, Physiotherapist, Psychologist, Other | Hospice, Inpatient Palliative Care, Outpatient Palliative Care | Acupuncture, Anthroposophic Medicine, Aromatherapy, Art Therapy, Ayurvedic Medicine, Dietary Supplements, Energy Therapy, Homeopathy, Hyperthermia, Light Therapy, Manipulation, Massage, Meditation, Mistletoe, Music Therapy, Osteopathy, Physiotherapy, Phytotherapy, Prayer, Qi Gong, Relaxation, Reflexology, Special Diets, Tai-Chi, Traditional Chinese Medicine, Yoga | Cancer | Unspecified | Communication/Collaboration, Ever Recommended, General Attitudes, Knowledge of CIM, Patient Characteristics, Patient Demand, Perceived Adverse Effects, Perceived Benefits, Perceptions of Evidence Base, Personal Use, Sources of Information, Types of CIM Offered |
| Egeli, et al40 | Qualitative semi-structured individual interviews | Physician | Pediatric Hospice | Massage | Unspecified | Discomfort, Mobility, Pain, Well-Being | Perceived Benefits, Symptoms Addressed |
| Esplen, et al41 | Questionnaire | CIM Provider, Clinical Educator, Nurse, Pharmacist, Physician, Physician Assistant, Psychologist, Radiation Therapist, Respiratory Therapist, Social Worker, Other | Cancer Center, Home Hospice, Inpatient Palliative Care | Music Therapy | Cancer | Cognition, Discomfort, Distress, Memory, Mobility, Pain, Quality of Life, Sleep Disturbance, Well-Being | Access/Availability, Knowledge of CIM, Perceived Barriers, Perceived Efficacy, Perceived Facilitators, Symptoms Addressed, Willingness to Learn |
| Garnett42 | Qualitative semi-structured individual interviews | CIM Provider, Nurse, Physician, Other | Inpatient Palliative Care | Unspecified | Unspecified | Unspecified | Perceived Benefits |
| Groen43 | Questionnaire | CIM Provider, Nurse | Home Hospice, Hospice | Acupuncture, Aromatherapy, Art Therapy, Guided Imagery, Herbal Therapy, Humor Therapy, Hypnotherapy, Massage, Music Therapy, Pet Therapy, Reflexology, Reiki, Therapeutic Touch, Yoga | Unspecified | Anxiety, Communication, Coping, Depression, Grief, Isolation, Mental Status, Pain, Restlessness, Spirituality | Access/Availability, Contexts for CIM, Referral Patterns, Symptoms Addressed, Types of CIM Offered |
| Hartwig44 | Qualitative structured individual interviews | Nurse, Social Worker, Other | Inpatient Palliative Care | Music Therapy | Unspecified | Anxiety, Depression, Isolation, Pain, Spirituality | Characteristics of Delivery, Perceived Adverse Effects, Perceived Benefits, Perceived Efficacy, Symptoms Addressed |
| Helmrich, et al45 | Qualitative semi-structured focus group interviews | Nurse | Inpatient Palliative Care | Acupressure, Acupuncture, Aromatherapy, Guided Imagery, Hyperthermia, Hypothermia, Manipulation, Massage, Reflexology, Reiki, Relaxation, Therapeutic Touch, Other (Unspecified) | Unspecified | Pain | Access/Availability, Knowledge of CIM, Perceived Barriers, Perceived Facilitators, Perceptions of Evidence Base, Symptoms Addressed, Types of CIM Offered |
| Iwase, et al46 | Questionnaire | Physician | Cancer Center, Inpatient Palliative Care | Traditional Japanese Medicines | Cancer | Anemia, Anorexia, Constipation, Depression, Diarrhea, Dysgeusia, Dysphagia, Dyspnea, Edema, Fatigue, Mental Status, Muscle Pain, Nausea/Vomiting, Numbness, Pain, Sleep Disturbance, Xerostomia | Characteristics of Delivery, Patient Demand, Perceived Barriers, Perceived Benefits, Perceived Efficacy, Perceptions of Evidence Base, Symptoms Addressed, Types of CIM Offered, Where in Line of T reatment |
| Kienle, et al47 | Qualitative semi-structured individual interviews | Physician | Cancer Center, Inpatient Palliative Care, Outpatient Palliative Care | Art Therapy, Eurythmy, Herbal Therapy, Hyperthermia, Massage, Mistletoe, Special Diet, Other (Unspecified) | Cancer | Anorexia, Anxiety, Cognition, Edema, Fatigue, Freezing, Nausea/Vomiting, Pain, Quality of Life, Sleep Disturbance, Stiffness | Characteristics of Delivery, Communication/Collaboration, General Attitudes, Patient Demand, Perceived Benefits, Perceived Adverse Effects, Sources of Information, Symptoms Addressed |
| Kwekkeboom, et al48 | Questionnaire | Nurse | Cancer Center | Distraction, Guided Imagery, Music Therapy, Relaxation | Cancer | Pain | Access/Availability, Knowledge of CIM, Patient Characteristics, Perceived Adverse Effects, Perceived Attitudes of Other Healthcare Professionals, Perceived Benefits, Perceived Efficacy, Perceived Patient Receptivity, Perceived Value of Time Spent, Perceptions of Evidence Base, Rate of Use, Sufficient Time |
| Lewith, et al49 | Questionnaire | CIM Provider, Nurse, Physiotherapist, Physician, Radiation Therapist, Other | Cancer Center, Hospice | Aromatherapy, Massage, Reflexology, Relaxation, Other (Unspecified) | Cancer | Unspecified | Attitudes Toward Integration, Types of CIM Offered, Willingness to Learn |
| Lin, et al50 | Questionnaire | Chaplain, Nurse, Physician, Psychotherapist, Social Worker | Hospice, Inpatient Palliative Care | Acupressure, Acupuncture, Chiropractic, Traditional Chinese Medicine | Unspecified | Anorexia, Constipation, Dizziness, Dyspnea, Edema, Nausea/Vomiting, Pain, Sleep Disturbance, Ulcer, Wound, Xerostomia | Knowledge of CIM, Perceived Adverse Effects, Perceived Efficacy, Perceptions of CIM Training, Referral Patterns, Sources of Information |
| Masel, et al51 | Qualitative semi-structured individual interviews | Chaplain, Nurse, Physiotherapist, Physician, Other | Inpatient Palliative Care | Herbal Therapy | Cancer | Well-Being | Perceived Adverse Effects, Perceived Benefits |
| Mason, et al52 | Questionnaire | Physician | Unspecified | Manipulation | Unspecified | Dyspnea, Pain | Perceived Efficacy, Symptoms Addressed, Types of CIM Offered, Willingness to Learn |
| Millison and Dudley53 | Questionnaire | Chaplain, Nurse, Psychologist, Physician, Social Worker, Other | Hospice | Guided Imagery, Meditation, Prayer | Unspecified | Unspecified | Perceived Barriers, Perceived Efficacy, Perceived Facilitators, Types of CIM Offered |
| Muecke, et al54 | Questionnaire | Nurse, Physician, Other | Cancer Center, Inpatient Palliative Care, Unspecified | Acupuncture, Anthroposophic Medicine, Aromatherapy, Dietary Supplements, Herbal Therapy, Homeopathy, Meditation, Mistletoe, Qi-Gong, Reflexology, Relaxation, Special Diet, Tai-Chi, Vitamins, Yoga, Other (Unspecified) | Unspecified | Unspecified | Perceived Efficacy, Perceptions of Evidence Base, Personal Use, Sources of Information, Types of CIM Offered |
| Munkombwe, et al55 | Qualitative semi-structured individual interviews | Nurse | Home Hospice, Hospice, Inpatient Palliative Care | Unspecified | Unspecified | Pain | Characteristics of Delivery, General Attitudes, Perceived Barriers, Perceived Benefits, Where in Line of T reatment |
| Nakano, et al56 | Qualitative semi-structured individual interviews | Nurse, Physician | Inpatient Palliative Care | Aromatherapy, Art Therapy, Massage, Music Therapy, Pet Therapy | Cancer | Unspecified | Attitudes Toward Caregiver Involvement, Context for CIM, General Attitudes, Perceived Efficacy, Where in Line of Treatment |
| Newell and Sanson-Fisher57 | Questionnaire | Physician | Cancer Center | Acupuncture, Aromatherapy, Coffee Enema, Dietary Supplements, Faith Healing, Guided Imagery, Herbal Therapy, Homoeopathy, Hypnotherapy, Iridology, Magnetotherapy, Meditation, Microwave Therapy, Mistletoe, Naturopathy, Ozone Therapy, Relaxation, Shark Cartilage, Special Diet | Cancer | Unspecified | Knowledge of CIM, Perceived Adverse Effects, Perceived Benefit, Perceived Patient Use |
| O’Kelly and Koffman58 | Qualitative semi-structured individual interviews | Chaplain, CIM Provider, Nurse, Occupational Therapist, Physiotherapist, Physician, Social Worker, Other | Hospice | Music Therapy | Unspecified | Cognition, Pain | Attitudes toward Integration, General Attitudes, Perceived Scope of CIM |
| Sproat59 | Questionnaire, Quasi-experimental: pre-test / post-test | Chaplain, Nurse, Social Worker, Other | Hospice | Aromatherapy, Art Therapy, Breathing Exercises, Massage, Meditation, Music Therapy, Yoga, Other (Unspecified) | Unspecified | Unspecified | Attitudes toward Integration, Availability/Access, Knowledge of CIM, Perceived Barriers, Perceived Efficacy, Perceptions of Evidence Base, Personal Use, Source of Information, Types of CIM Offered |
| Stewart and Cox-Davenport60 | Questionnaire | Nurse, Other | Hospice, Unspecified | Breathing Exercises, Guided Imagery, Hyperthermia, Hypothermia, Manipulation, Massage, Music Therapy, Therapeutic Touch | Unspecified | Pain | Access/Availability, Perceived Barriers, Perceived Efficacy, Perceived Patient Receptivity, Perceptions of Training, Rates of Use, Types of CIM Offered |
| Uritsky, et al61 | Questionnaire | Nurse, Physician, Social Worker, Other | Hospice, Unspecified | Marijuana | Unspecified | Agitation, Anorexia, Anxiety, Depression, Discomfort, Distress, Headache, Nausea/Vomiting, Pain, Restlessness | General Attitudes, Knowledge of CIM, Patient Demand, Perceived Adverse Effects, Perceived Benefit, Perceived Patient Use |
| Wagland, et al62 | Qualitative semi-structured focus groups interviews, Qualitative semi-structured individual interviews | Nurse, Occupational Therapist, Physiotherapist, Physician | Cancer Center, Inpatient Palliative Care, Outpatient Palliative Care | Unspecified | Cancer | Cough, Dyspnea, Fatigue | Characteristics of Delivery, General Attitudes, Patient Characteristics, Perceived Benefit, Perceived Efficacy, Referral Patterns, Where in Line of Treatment |
| Wang, et al63 | Qualitative semi-structured individual interviews | Nurse | Cancer Center, Outpatient Palliative Care | Acupuncture, Aromatherapy, Dietary Supplement, Magnetotherapy, Massage, Naturopathy, Reiki, Therapeutic Touch | Cancer | Distress, Fatigue, Nausea/Vomiting, Pain | General Attitudes, Knowledge of CIM, Perceived Attitudes of Other Healthcare Workers, Perceived Benefit, Perceived Efficacy, Perceived Patient Use, Perceptions of Evidence Base, Personal Use, Types of CIM Offered, Willingness to Learn |
| Weekly, et al64 | Questionnaire | Nurse, Other | Inpatient Palliative Care | Massage | Unspecified | Unspecified | Attitudes Toward Integration, Perceived Benefit |
| Wong, et al65 | Questionnaire | CIM Provider, Nurse, Physician | Cancer Center, Inpatient Palliative Care, Outpatient Palliative Care | Acupressure, Acupuncture, ElectroAcupuncture, Hyperthermia, Moxibustion, Traditional Chinese Medicine | Cancer | Fatigue, Nausea/Vomiting, Pain, Quality of Life | Attitudes Toward Integration, General Attitudes Toward CIM, Perceived Adverse Effects, Perceived Benefits, Perceived Inequities in CIM Delivery, Perceived Patient Receptivity, Perceptions of Evidence Base |
CIM = complementary and integrative medicine.
Table 3.
Study Outcomes and Phenomena of Interest.
| Theme | Code | Count |
|---|---|---|
| Usage | Types of CIM Offered | 15 |
| Symptoms Addressed | 12 | |
| Characteristics of CIM Delivery | 6 | |
| Personal Use | 5 | |
| Referral Patterns | 4 | |
| Where in Line-of-treatment | 4 | |
| Contexts for CIM | 3 | |
| Facilitators | 3 | |
| Rates of Use | 3 | |
| Ever Recommended CIM | 1 | |
| Likely to Provide CIM | 1 | |
| Likely to Recommend CIM | 1 | |
| 58 | ||
| Efficacy | Perceived Benefits | 17 |
| Perceived Efficacy | 14 | |
| Perceived Adverse Effects | 9 | |
| Perceptions of Evidence Base | 9 | |
| 49 | ||
| Attitudes | General Attitudes Toward CIM | 13 |
| Barriers to CIM | 9 | |
| Attitudes toward Integration | 7 | |
| Perceived Attitudes of Other Healthcare Professionals Toward CIM | 2 | |
| Perceived Inequities in CIM Delivery | 1 | |
| Perceived Value of Time Spent | 1 | |
| 33 | ||
| Knowledge | Knowledge of CIM | 11 |
| Sources of Information | 6 | |
| Willingness to Learn about CIM | 5 | |
| Perceptions of CIM Training | 2 | |
| Perceived Scope of CIM | 1 | |
| 25 | ||
| Patient Factors | Patient Characteristics | 4 |
| Patient Demand | 4 | |
| Patient Use of CIM | 3 | |
| Perceived Patient Receptivity | 3 | |
| Perceptions of Caregiver Involvement | 1 | |
| 15 | ||
| Logistics | Access/Availability | 7 |
| Communication/Collaboration | 4 | |
| Sufficient Time | 2 | |
| 13 | ||
| Total | 193 |
CIM Modalities
Traditionally, complementary and integrative modalities are organized into 5 themes: manipulative/body-based therapies, mind-body therapies, biologically-based therapies, energy therapies, and whole medical systems.24 In analyzing the CIM modalities studied in the 34 articles, we coded 58 unique modalities and then categorized these codes into this framework (Appendix Table 2).
Across the 34 reports, there were 66 mentions of 17 unique modalities in the mind-body therapies theme, including music therapy (n = 12), aromatherapy (n = 10), and art therapy (n = 6). We identified 57 mentions of 15 unique manipulative and body-based therapies, including massage (n = 13), acupuncture (n = 8), and reflexology (n = 6). There were 26 mentions of 11 unique biologically based therapies, such as dietary supplements (n = 5), special diets (n = 4), and herbal therapy (n = 4). We found 17 mentions of 9 unique whole medical systems such as Traditional Chinese Medicine (n = 4) and homeopathy (n = 3). Finally, there were 7 mentions of 6 unique energy therapies, including magnetotherapy (n = 2) and biofeedback therapy (n = 1).
Overall, the most common modalities studied were massage (n = 13), music therapy (n = 12), and aromatherapy (n = 10). Among the least common codes were Traditional Chinese Medicine (n = 4), yoga (n = 4), osteopathy (n = 2), qui-gong (n = 2), tai-chi (n = 2), Ayurveda (n = 1), essential oils (n = 1), and marijuana (n = 1).
Diseases and Symptoms of Interest
While there are no standard frameworks for thematically analyzing diseases of interest in palliative care, this study revealed that the only specified disease of interest was cancer in 14 articles, while the remaining 20 studies did have a single disease focus. However, most studies did specify symptoms targeted by 1 or more CIM modality. We developed 38 unique symptom codes, and classified them into existing domains.26 Relevant symptom domains include physical; psychological and psychiatric; social; and spiritual, religious, and existential aspects of care (Appendix Table 3).
The most common domain addressed was physical aspects of care, with 62 mentions of 22 unique codes within this domain. Common codes included pain (n = 17), fatigue (n = 6), and nausea and vomiting (n = 6). There were 24 mentions of 9 symptoms coded under psychological and psychiatric aspects of care, such as anxiety (n = 5), depression (n = 5), and distress (n = 4). There were 11 mentions of 5 symptoms coded within the spiritual, religious, and existential aspects of care domain including well-being (n = 5), quality of life (n = 3), and spirituality (n = 2). Finally, there were 6 mentions of 2 codes in the social aspects of care domain, comfort (n = 4) and isolation (n = 2).
Overall, the most common codes represented throughout the 34 articles were pain (n = 17), fatigue (n = 6), nausea and vomiting (n = 6), anxiety (n = 5), and depression (n = 5). Some of the least frequently mentioned codes were constipation (n = 2), mental status (n = 2), agitation (n = 1), cough (n = 1), and dysphagia (n = 1).
Study Outcomes
The main aim of this review was to examine the outcomes-and phenomena-of-interest in provider-focused research on CIM use in palliative care. As described in the Methods, we generated 35 unique outcome codes and categorized them into 6 themes: usage of CIM, knowledge of CIM, patient factors in CIM, attitudes toward CIM, efficacy of CIM, and logistics surrounding CIM (Table 3).
The most common theme studied was usage of CIM. There were 58 mentions across 12 unique codes, such as specific CIM modalities offered by providers (n = 15), the symptoms addressed with CIM use (n = 12), and the characteristics of CIM delivery (n = 6). Infrequent codes included actual referral patterns (n = 4), facilitators for provider recommendation (n = 3), and rates of use of CIM use (n = 3). There were 49 mentions across 4 codes within the efficacy theme, including perceived benefits of CIM (n = 17), perceived efficacy underlying CIM (n = 14), perceived adverse effects of CIM (n = 9), and perceptions of the evidence base for CIM (n = 9). There were 33 mentions of 6 codes within the attitudes theme; the most common codes were general attitudes toward CIM (n = 13) and perceived barriers to CIM (n = 9). There were 25 mentions across 5 codes within the knowledge theme, including prior knowledge of CIM (n = 11), sources of information on CIM (n = 6), and willingness to learn about CIM (n = 5). There were 15 mentions across 5 codes within the patient factors theme, such as perceived patient demand for CIM (n = 4) and characteristics of patients receiving CIM (n = 4). Finally, there were 13 mentions across 3 codes in the logistics theme including provider access to and availability of CIM equipment and providers (n = 7) and communication and collaboration with CIM providers (n = 4).
Overall, the most common phenomena studied were perceived benefits of CIM (n = 17), the modalities offered (n = 15), perceived efficacy of CIM (n = 14), and general attitudes toward CIM (n = 12). Infrequently addressed outcomes included referral patterns (n = 4), facilitators (n = 3), rates of use (n = 3), and if providers have ever recommended CIM (n = 2).
Discussion
To the best of our knowledge, this is the first scoping review to examine provider-focused research on CIM use in the palliative care setting. The secular trend, with over 40% of studies published in just the past 5 years (Table 1), aligns with the growing popularity of non-pharmacologic approaches to manage symptoms in palliative care.8,11,21 With respect to research design, the equal presence of quantitative and qualitative studies and absence of controlled experiments (Table 1) both suggest that the field of studying provider use of CIM in palliative care is in its early stages of the research pipeline.
Study Characteristics
A substantial majority of studies focused on 2 specific provider groups, i.e. nurses and physicians, while social workers and chaplains were infrequently study subjects. Further, none of the studies provided results on Advance Practice Registered Nurses (APRN) (Table 1). These results demonstrate a significant gap, given the highly interdisciplinary nature of hospice and palliative care delivery. National trends show 84% of palliative care teams have an APRN, 69% have a Social Worker, 54% have a chaplain, and 41% consist of all 3 and a physician.66 While there is potential for systematic investigation of physician and nurse attitudes, future research should also focus on capturing the understudied perspectives of these additional team-members who are likely to be frequently recommending CIM to patients.
With respect to study setting, 59% of the articles examined the use of CIM in the inpatient palliative care setting, while 35% focused on hospice without further specifying a location where care was delivered (Table 1). This distribution reflects current models of palliative care, which continues to be delivered primarily in the inpatient and hospice-care settings, with increasing attention in the outpatient setting.2,67–69 Given the growth of office-based palliative care, future research should continue to study these varied clinical spaces, as many CIM modalities are better suited as referrals to office-based CIM providers, can be taught in the office-setting, and do not require specialized equipment.
CIM Modalities
In addition to these study design characteristics, we examined the CIM modalities studied in each article. Massage, music therapy, and aromatherapy were commonly studied, while both the greatest variety of codes and the most mentions of codes fell into the category of mind-body medicine (Appendix Table 2). These results are in agreement with a prior systematic review that found either massage alone or combined with aromatherapy or meditation were the most common CIM modalities whose efficacy were assessed in the palliative care setting.21 Despite the need for licensed and certified providers, we speculate massage and music therapy are among the most accessible in the inpatient setting.
The articles in this review examined 55 unique CIM modalities in addition to those noted above. In the absence of literature documenting providers’ motivation for the use of particular CIM modalities, we cannot speculate why these modalities and not others are prevalent in our sample. However, their presence in the literature reveals an important gap between research and actual patient behaviors. We considered the prevalence in our sample (Appendix Table 2) of CIM modalities patients most commonly use,8,11 such as natural products (15%), breathing exercises (9%), meditation (15%), chiropractic (3%) and osteopathic manipulation (9%), massage (38%), yoga, tai-chi (6%), and qi-gong (6%). With the exception of massage, these particular CIM modalities were infrequently studied. In the absence of documented barriers and facilitators for using these particular modalities, we suspect that the absence of a provider role (natural products do not require prescriptions), lack of provider training (most of these modalities require experience), and lack of access in the inpatient setting are possible barriers to their inclusion in research on provider perspectives. This lack of concordance between the modalities appearing in provider-focused literature and those used by patients necessitates a shift in focus, as examining the provider perspectives on these particular modalities can reveal important alignments and differences in beliefs and motivations between patients and providers that could serve as facilitators and barriers, respectively, to safe and efficacious recommendation of CIM.
Diseases and Symptoms of Interest
The analyzed studies did not typically focus on patients with a specific disease, except for cancer, in agreement with a national report that cancer is the most common primary diagnosis in patients for which palliative care is consulted.66 The articles did, however, generally specify the symptomatic context in which the provider perspective on CIM was being examined. Pain, fatigue, nausea and vomiting, anxiety, and depression were among those symptoms most commonly studied (Appendix Table 3). Surveys on actual patient use of CIM have found that patients most often target symptoms of back, neck and joint pain; anxiety; headache; sleep disturbance; stress; and depression.11 Thus, the symptoms addressed by the review sample are appropriately aligned with those symptoms that patients seek to address when they employ CIM. However, we noted several symptoms that are prevalent in the palliative care setting3,4,6 yet were relatively understudied (Appendix Table 3), such as agitation (3%), altered mental status (6%), constipation (6%), dysphagia (3%), and mobility impairment (6%). We recommend systematic investigation into provider perspectives of the common patient-reported symptoms that are also prevalent in the literature, as well as a future focus on those symptoms for which patients do not report using CIM as frequently yet are commonly encountered by palliative care providers to begin to understand provider behaviors and attitudes.
Study Outcomes
Perhaps the most notable trends and knowledge gaps relate to the outcomes-and phenomena-of-interest in the sample. The reports predominantly focused on outcomes related to the theme of use of CIM in the palliative care setting (Table 3). 44% and 35% of the articles had a primary outcome of identifying the specific CIM modalities and specific symptoms providers seek to address with CIM, respectively. While we extracted the results of these measures as separate data points in this review, these data suggest an ongoing focus on assessing the clinical contexts in which providers use CIM in palliative care. Beyond these outcomes and phenomena, others that were commonly studied (Table 3) include providers’ perceptions of the benefits (50%) and efficacy (41%) of CIM, providers’ prior knowledge of CIM (32%), and their general attitudes toward CIM (38%). Future systematic review into these outcomes could identify where providers’ perceptions of CIM efficacy do and do not align with existing evidence, providers’ self-perceptions of their knowledge base, and trends in general attitudes, all of which may lead to improved targeting of efforts to increase uptake of CIM.
While we identified these prevalent outcomes of interest, we discovered an even larger set of understudied phenomena that merit further exploration. Most notably, only 9% of articles examined actual provider rates of use of specific CIM modalities and only 12% focused on referral patterns to CIM providers (Table 3). Studying rates of use of specific CIM modalities for specific symptoms is an important metric in calibrating actual practice patterns to the evidence on safety and efficacy, where both appropriate and inappropriate use would present opportunities for training and development of guidelines.
Future investigations into the remainder of the understudied outcomes (Table 3), particularly assessing barriers (26%) and facilitators (9%) to recommending CIM, perceptions of the evidence base (26%), sources of information about CIM (18%), willingness to learn about CIM (15%), perceptions of patient demand for CIM (12%), and access to and availability of CIM resources (21%), are all essential to identifying the best ways to increase palliative care provider use of CIM.
Limitations
This scoping review has certain limitations that warrant consideration. With respect to our search strategy, given our inability to search for every known CIM modality, it is possible that there are particular therapies that were not captured by our selected CIM search terms. Specifically, in the case of therapies that are not indexed in databases as subject headings related complementary, alternative, or integrative medicines, while certain articles on these therapies were captured by broader search terms, some were likely missed. This limitation has been noted in past systematic investigations in this field.21 We excluded non-English language studies and did not search outside the traditional academic literature, thereby limiting our ability to capture the entire breadth of research in this field. While each screening stage relied on 2 independent reviewers, it is still possible that manual reviews of citations resulted in inappropriate exclusion. Finally, the approach to scoping reviews does not include methodological, quality, or bias assessment that could affect the conclusions we present.
Conclusions
This scoping review examined the characteristics and outcomes of 34 studies related to provider perspectives of CIM in the palliative care setting. While we identified trends and commonalities in the literature that provide opportunity for systematic investigation to generate stronger conclusions, we also demonstrate that future research in this growing field should broaden in scope by incorporating perspectives of interdisciplinary team members, studying more common modalities, addressing symptoms commonly seen in the palliative care setting, and most importantly, targeting more heterogenous phenomena of interest to improve uptake of evidenced-based CIM amongst providers. As the field of CIM in palliative care continues to expand, so can the practices and policies that promote safe and efficacious use of CIM in relieving burdensome symptoms.
Acknowledgments
We thank Veerawat Phongtankuel, MD, Assistant Professor and Milagros D. Silva, MD, Assistant Professor, in the Division of Geriatrics and Palliative Medicine, Weill Cornell Medicine for their helpful comments on earlier drafts of this manuscript. We also thank Michelle Demetres, MLIS, Assistant Librarian, Samuel J. Wood Library & C.V. Starr Biomedical Information Center, Weill Cornell Medicine, who assisted in designing the scoping review methods. Anurag Goel conducted this research as part of the Areas of Concentration (AOC) Program of the Weill Cornell Medicine MD Program curriculum.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: MCR is supported by grants from the National Institute on Aging [K24AGO53462, P30AG022845].
Appendix
Table 1.
Example of Search Strategy: Keyword and MeSH Headings Searched Within MEDLINE.
| Search term | Keywords and MeSH headings |
|---|---|
| 1 | MH Palliative Care |
| 2 | MH Palliative Medicine |
| 3 | TIAB Palliative |
| 4 | MH Hospices |
| 5 | MH Hospice Care |
| 6 | MH Hospice and Palliative Care Nursing |
| 7 | TIAB hospice* |
| 8 | MH Terminal Care |
| 9 | TIAB terminal care |
| 10 | TIAB end of life |
| 11 | TIAB end-of-life |
| 12 | MH Complementary Therapies |
| 13 | TIAB complementary therap* |
| 14 | TIAB complementary medicine |
| 15 | MH Integrative Medicine |
| 16 | TIAB integrative medicine |
| 17 | TIAB alternative therap* |
| 18 | TIAB alternative medicine |
| 19 | TIAB non-pharmacologic* |
| 20 | TIAB non pharmacologic* |
| 21 | MH Acupuncture |
| 22 | TIAB acupuncture |
| 23 | MH Acupressure |
| 24 | TIAB acupressure |
| 25 | TIAB cupping |
| 26 | TIAB dry needl* |
| 27 | TIAB homeopath* |
| 28 | MH Medicine, Ayurvedic |
| 29 | TIAB traditional medicine |
| 30 | TIAB ayurved* |
| 31 | TIAB Asian medicine |
| 32 | TIAB Chinese medicine |
| 33 | TIAB folk medicine |
| 34 | MH Herbal Medicine |
| 35 | TIAB herbal medicine |
| 36 | TIAB mind body |
| 37 | TIAB mind-body |
| 38 | TIAB aromatherapy |
| 39 | TIAB biofeedback |
| 40 | TIAB breathing exercise |
| 41 | TIAB hypnosis |
| 42 | TIAB guided imagery |
| 43 | TIAB laughter |
| 44 | TIAB meditation |
| 45 | TIAB relaxation |
| 46 | TIAB qigong” |
| 47 | TIAB qi-gong” |
| 48 | TIAB tai-ji |
| 49 | TIAB taiji |
| 50 | TIAB tai ji |
| 51 | TIAB tai-chi |
| 52 | TIAB taichi |
| 53 | TIAB tai chi |
| 54 | TIAB therapeutic touch |
| 55 | TIAB reiki |
| 56 | TIAB yoga |
| 57 | MH Chiropractic |
| 58 | MH Osteopathic Medicine |
| 59 | TIAB manipulation |
| 60 | TIAB chiropractic |
| 61 | TIAB osteopath* |
| 62 | TIAB massage |
| 63 | TIAB naturopath* |
| 64 | MH Dietary Supplements |
| 65 | TIAB dietary supplement” |
| 66 | MH Nutrition Therapy |
| 67 | TIAB nutrition” |
| 68 | TIAB art therapy |
| 69 | TIAB dance therapy |
| 70 | TIAB music therapy |
| 71 | TIAB attitude* |
| 72 | TIAB knowledge |
| 73 | TIAB pattern* |
| 74 | TIAB competen* |
| 75 | TIAB awareness |
| 76 | TIAB usage |
| 77 | TIAB utiliz* |
| 78 | TIAB provision |
| 79 | TIAB delivery |
| 80 | TIAB survey* |
| 81 | TIAB questionnaire* |
| 82 | TIAB interview* |
| 83 | TIAB refer* |
| 84 | TIAB consult* |
| 85 | TIAB challenge* |
| 86 | TIAB barrier* |
| 87 | MH Interviews as Topic |
| 88 | MH Clinical Competence |
| 89 | MH Surveys and Questionnaires |
| 90 | MH Health Services Research |
| 91 | MH Institutional Practice |
| 92 | MH Referral and Consultation |
| 93 | MH Attitude of Health Personnel |
| 94 | MH Attitude to Health |
| 95 | MH Health Care Costs |
| 96 | MH Health Resources |
| 97 | MH Practice Patterns, Nurses’ |
| 98 | MH Practice Patterns, Physicians’ |
| 99 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 |
| 100 | 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR42 OR 43 OR44 OR 45 OR 46 OR 47 OR 48 OR 49 OR 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59 OR 60 OR 61 OR 62 OR 63 OR 64 OR 65 OR 66 OR 67 OR 68 OR 69 OR 70 |
| 101 | 71 OR 72 OR 73 OR 74 OR 75 OR 76 OR 77 OR 78 OR 79 OR 80 OR 81 OR 82 OR 83 OR 84 OR 85 OR 86 OR 87 OR 88 OR 89 OR 90 OR 91 OR 92 OR 93 OR 94 OR 95 OR 96 OR 97 OR 98 |
| 102 | 99 AND 100 AND 101 |
MH = MEDLINE Medical Subject Heading keyword; TIAB = MEDLINE Title and Abstract keyword search.
The asterisk symbol (*) was used in PubMed searches as a wildcard character.
Table 2.
CIM Modalities.
| Theme | Code | Count |
|---|---|---|
| Mind-Body Medicine | Music Therapy | 12 |
| Aromatherapy | 10 | |
| Art Therapy | 6 | |
| Guided Imagery | 6 | |
| Relaxation | 6 | |
| Meditation | 5 | |
| Yoga | 4 | |
| Breathing Exercises | 3 | |
| Horticulture Therapy | 2 | |
| Pet Therapy | 2 | |
| Prayer | 2 | |
| Qi-Gong | 2 | |
| Tai-Chi | 2 | |
| Distraction | 1 | |
| Eurythmy | 1 | |
| Faith Healing | 1 | |
| Humor Therapy | 1 | |
| 66 | ||
| Manipulative/Body-Based Therapies | Massage | 13 |
| Acupuncture | 8 | |
| Reflexology | 6 | |
| Hyperthermia | 5 | |
| Therapeutic Touch | 5 | |
| Reiki | 4 | |
| Acupressure | 3 | |
| Hypnotherapy | 3 | |
| Manipulation | 3 | |
| Hypothermia | 2 | |
| Chiropractic | 1 | |
| Electroacupuncture | 1 | |
| Footsoak | 1 | |
| Moxibustion | 1 | |
| Physiotherapy | 1 | |
| 57 | ||
| Biologically-Based Therapies | Supplements | 5 |
| Diets | 4 | |
| Herbal Therapy | 4 | |
| Mistletoe | 4 | |
| Minerals | 2 | |
| Vitamins | 2 | |
| Coffee Enema | 1 | |
| Essential Oils | 1 | |
| Marijuana | 1 | |
| Phytotherapy | 1 | |
| Shark Cartilage Therapy | 1 | |
| 26 | ||
| Whole Medical Systems | Traditional Chinese Medicine | 4 |
| Homeopathy | 3 | |
| Anthroposophy | 2 | |
| Naturopathy | 2 | |
| Osteopathy | 2 | |
| Ayurveda | 1 | |
| Iridology | 1 | |
| Traditional Healer | 1 | |
| Traditional Japanese Medicine | 1 | |
| 17 | ||
| Energy Therapies | Magnetotherapy | 2 |
| Biofeedback | 1 | |
| Energy Therapy | 1 | |
| Light Therapy | 1 | |
| Microwave Therapy | 1 | |
| Ozone Therapy | 1 7 |
|
| Unspecified | 10 | |
| Total | 183 |
Table 3.
Symptoms.
| Theme | Code | Count |
|---|---|---|
| Physical Aspects of Care | Pain | 17 |
| Fatigue | 6 | |
| Nausea/Vomiting | 6 | |
| Anorexia | 4 | |
| Dyspnea | 4 | |
| Sleep Disturbance | 4 | |
| Edema | 3 | |
| Constipation | 2 | |
| Mobility | 2 | |
| Xerostomia | 2 | |
| Cough | 1 | |
| Diarrhea | 1 | |
| Dizziness | 1 | |
| Dysgeusia | 1 | |
| Dysphagia | 1 | |
| Freezing | 1 | |
| Headache | 1 | |
| Muscle pain | 1 | |
| Numbness | 1 | |
| Stiffness | 1 | |
| Ulcer | 1 | |
| Wound | 1 | |
| 62 | ||
| Psychological and Psychiatric Aspects | Anxiety | 5 |
| Depression | 5 | |
| Distress | 4 | |
| Cognition | 3 | |
| Mental Status | 2 | |
| Restlessness | 2 | |
| Agitation | 1 | |
| Communication | 1 | |
| Grief | 1 | |
| 24 | ||
| Spiritual, Religious, and Existential Aspects of Care | Well-being | 4 |
| Quality of Life | 3 | |
| Spirituality | 2 | |
| Coping | 1 | |
| Suffering | 1 | |
| 11 | ||
| Social Aspects of Care | Comfort | 4 |
| Isolation | 2 | |
| 6 | ||
| Unspecified | 14 | |
| Total | 117 |
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Center to Advance Palliative Care. America’s Care of Serious Illness: 2019 State-by-State Report Care on Access to Palliative Care in our Nation’s Hospitals. Palliative Care, Report Card. Published 2019. Accessed April 16, 2021. https://reportcard.capc.org/ [Google Scholar]
- 2.National Hospice and Palliative Care Organization. NHPCO’s Facts & Figures on Hospice Care in America. Published 2020. Accessed April 16, 2021. https://www.nhpco.org/factsfigures/
- 3.Bookbinder M, McHugh ME. Symptom management in palliative care and end of life care. Nurs Clin North Am. 2010;45(3):271–327. [DOI] [PubMed] [Google Scholar]
- 4.Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Interv Aging. 2011;6:243–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mercadante S, Adile C, Ferrera P, Masedu F, Valenti M, Aielli F. Sleep disturbances in advanced cancer patients admitted to a supportive/palliative care unit. Support Care Cancer. 2017;25(4):1301–1306. [DOI] [PubMed] [Google Scholar]
- 6.Moens K, Higginson IJ, Harding R; EURO IMPACT. Are there differences in the prevalence of palliative care-related problems in people living with advanced cancer and eight non-cancer conditions? A systematic review. J Pain Symptom Manage. 2014;48(4):660–677. [DOI] [PubMed] [Google Scholar]
- 7.Blinderman CD, Billings JA. Comfort care for patients dying in the hospital. N Engl J Med. 2015;373(26):2549–2561. [DOI] [PubMed] [Google Scholar]
- 8.Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl Health Stat Report. 2015;(79):1–16. [PMC free article] [PubMed] [Google Scholar]
- 9.Nahin RL, Barnes PM, Stussman BJ. Expenditures on complementary health approaches: United States, 2012. Natl Health Stat Report. 2016;(95):1–11. [PubMed] [Google Scholar]
- 10.Bercovitz A, Sengupta M, Jones A, Harris-Kojetin LD. Complementary and alternative therapies in hospice: The national home and hospice care survey: United States, 2007. Natl Health Stat Report. 2011;(33):1–20. [PubMed] [Google Scholar]
- 11.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;(12):1–23. [PubMed] [Google Scholar]
- 12.Lin Y-C, Wan L, Jamison RN. Using integrative medicine in pain management: an evaluation of current evidence. Anesth Analg. 2017;125(6):2081–2093. [DOI] [PubMed] [Google Scholar]
- 13.Nahin RL, Boineau R, Khalsa PS, Stussman BJ, Weber WJ. Evidence-based evaluation of complementary health approaches for pain management in the United States. Mayo Clin Proc. 2016;91(9):1292–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aalbers S, Fusar-Poli L, Freeman RE, et al. Music therapy for depression. Cochrane Database Syst Rev. 2017;11(11):CD004517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cramer H, Lauche R, Klose P, Lange S, Langhorst J, Dobos GJ. Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1(1):CD010802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linde K, Kriston L, Rücker G, et al. Efficacy and acceptability of pharmacological treatments for depressive disorders in primary care: systematic review and network meta-analysis. Ann Fam Med. 2015;13(1):69–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith CA, Armour M, Lee MS, Wang LQ, Hay PJ. Acupuncture for depression. Cochrane Database of Syst Rev. 2018;3(3):CD004046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goyal M, Singh S, Sibinga EMS, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sarris J, Panossian A, Schweitzer I, Stough C, Scholey A. Herbal medicine for depression, anxiety and insomnia: a review of psychopharmacology and clinical evidence. Eur Neuropsychopharmacol. 2011;21(12):841–860. [DOI] [PubMed] [Google Scholar]
- 20.Thabrew H, Ruppeldt P, Sollers JJ. Systematic review of biofeedback interventions for addressing anxiety and depression in children and adolescents with long-term physical conditions. Appl Psychophysiol Biofeedback. 2018;43(3):179–192. [DOI] [PubMed] [Google Scholar]
- 21.Zeng YS, Wang C, Ward KE, Hume AL. Complementary and alternative medicine in hospice and palliative care: a systematic review. J Pain Symptom Manage. 2018;56(5):781–794.e4. [DOI] [PubMed] [Google Scholar]
- 22.St. John’s Wort and Depression: In Depth. National Center for Complementary and Integrative Health. Published 2017. Accessed April 16, 2021. https://www.nccih.nih.gov/health/st-johns-wort-and-depression-in-depth [Google Scholar]
- 23.Peters MDJ, Godfrey C, McInerney P, et al. Scoping reviews (2020 version). In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. 2020:chap 11. https://synthesismanual.jbi.global. 10.46658/JBIMES-20-12 [DOI] [Google Scholar]
- 24.National Center for Complementary and Integrative Health. Complementary, alternative, or integrative health: what’s in a name? Published 2018. Accessed April 16, 2021. https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name
- 25.Gamret AC, Price A, Fertig RM, Lev-Tov H, Nichols AJ. Complementary and alternative medicine therapies for psoriasis: a systematic review. JAMA Dermatol. 2018;154(11):1330–1337. [DOI] [PubMed] [Google Scholar]
- 26.Pan CX, Morrison RS, Ness J, Fugh-Berman A, Leipzig RM. Complementary and alternative medicine in the management of pain, dyspnea, and nausea and vomiting near the end of life. A systematic review. J Pain Symptom Manage. 2000;20(5):374–387. [DOI] [PubMed] [Google Scholar]
- 27.Ruan QZ, Chen AD, Tran BNN, et al. Integrative medicine in plastic surgery: a systematic review of our literature. Ann Plast Surg. 2019;82(4):459–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tillery R, McGrady ME. Do complementary and integrative medicine therapies reduce healthcare utilization among oncology patients? A systematic review of the literature and recommendations. Eur J Oncol Nurs. 2018;36:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Accessed April 16, 2021. www.covidence.org [Google Scholar]
- 30.Ferrell BR, Twaddle ML, Melnick A, Meier DE. National Consensus Project Clinical Practice Guidelines for Quality Palliative Care Guidelines, 4th ed. J Palliat Med. 2018;21(12):1684–1689. [DOI] [PubMed] [Google Scholar]
- 31.Constant Comparative Method. Encyclopedia of Evaluation. Sage Publications, Inc; 2005. [Google Scholar]
- 32.Amadoru S, McFerran K. The role of music therapy in children’s hospices. Eur J Palliat Care. 2007;14(3):124–127. [Google Scholar]
- 33.Atkin N, Vickerstaff V, Candy B. “Worried to death”: the assessment and management of anxiety in patients with advanced life-limiting disease, a national survey of palliative medicine physicians. BMC Palliat Care. 2017;16(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Broom A, Tovey P. Therapeutic pluralism? Evidence, power and legitimacy in UK cancer services. Sociolo Health Illn. 2007;29(4):551–569. [DOI] [PubMed] [Google Scholar]
- 35.Bucher T, Davies CC, Clements-Hickman AL, Weaver C, Breakall A, Yackzan S. The effect of education on nursing personnel’s knowledge and attitudes regarding the use of integrative care techniques with hospice and palliative care patients. Nurs Forum. Published online November 24, 2020. doi: 10.1111/nuf.12529 [DOI] [PubMed] [Google Scholar]
- 36.Campbell LM, Amin NN. A qualitative study: potential benefits and challenges of traditional healers in providing aspects of palliative care in rural South Africa. Rural Remote Health. 2014;14:2378. [PubMed] [Google Scholar]
- 37.Christina J, Abigail W, Cuthbertson LA, Whitehead D.Nurses’ knowledge and attitudes toward complementary and alternative medicine for adult patients with cancer in Bandung, West Java, Indonesia: a qualitative study. J Holist Nurs. 2019;37(2):130–139. [DOI] [PubMed] [Google Scholar]
- 38.Coelho A, Parola V, Cardoso D, Bravo ME, Apóstolo J. Use of non-pharmacological interventions for comforting patients in palliative care: a scoping review. JBI Database System Rev Implement Rep. 2017;15(7):1867–1904. [DOI] [PubMed] [Google Scholar]
- 39.Conrad AC, Muenstedt K, Micke O, Prott FJ, Muecke R, Huebner J. Attitudes of members of the German Society for Palliative Medicine toward complementary and alternative medicine for cancer patients. J Cancer Res Clin Oncol. 2014;140(7):1229–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Egeli D, Bainbridge L, Miller T, Potts J. Interdisciplinary perspectives on the value of massage therapy in a pediatric hospice. J Hosp Palliat Nurs. 2019;21(4):319–325. [DOI] [PubMed] [Google Scholar]
- 41.Esplen MJ, Foster B, Pearson S, et al. A survey of oncology healthcare professionals’ knowledge and attitudes toward the use of music as a therapeutic tool in healthcare. Support Care Cancer. 2020;28(1):381–388. [DOI] [PubMed] [Google Scholar]
- 42.Garnett M Sustaining the cocoon: the emotional inoculation produced by complementary therapies in palliative care. Eur J Cancer Care. 2003;12(2):129–136. [DOI] [PubMed] [Google Scholar]
- 43.Groen KM. Pain assessment and management in end of life care: a survey of assessment and treatment practices of hospice music therapy and nursing professionals. J Music Ther. 2007;44(2):90–112. [DOI] [PubMed] [Google Scholar]
- 44.Hartwig R. Music therapy in the context of palliative care in Tanzania. Int J Palliat Nurs. 2010;16(10):499–504. [DOI] [PubMed] [Google Scholar]
- 45.Poulton V, Hobman A, Berggren L, Nash P, Helmrich S, Yates P. Factors influencing nurses’ decisions to use non-pharmacological therapies to manage patients’ pain. Aust J Adv Nurs. 2001;19(1):27–35. [PubMed] [Google Scholar]
- 46.Iwase S, Yamaguchi T, Miyaji T, Terawaki K, Inui A, Uezono Y. The clinical use of Kampo medicines (traditional Japanese herbal treatments) for controlling cancer patients’ symptoms in Japan: a national cross-sectional survey. BMC Complement Altern Med. 2012;12(1):222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kienle GS, Mussler M, Fuchs D, Kiene H.individualized integrative cancer care in anthroposophic medicine: a qualitative study of the concepts and procedures of expert doctors. Integr Cancer Ther. 2016;15(4):478–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kwekkeboom KL, Bumpus M, Wanta B, Serlin RC. Oncology nurses’ use of nondrug pain interventions in practice. J Pain Symptom Manage. 2008;35(1):83–94. [DOI] [PubMed] [Google Scholar]
- 49.Lewith GT, Broomfield J, Prescott P. Complementary cancer care in Southampton: a survey of staff and patients. Complement Ther Med. 2002;10(2):100–106. [DOI] [PubMed] [Google Scholar]
- 50.Lin Y-J, Chang H-T, Lin M-H, et al. Professionals’ experiences and attitudes toward use of Traditional Chinese Medicine in hospice palliative inpatient care units: a multicenter survey in Taiwan. Integr Med Res. 2021;10(2):100642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Masel EK, Trinczek H, Adamidis F, et al. Vitamin “G”arden: a qualitative study exploring perception/s of horticultural therapy on a palliative care ward. Support Care Cancer. 2018;26(6):1799–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mason DC, McElrath S, Penn-Erskine C, Kramer-Feeley V, Pomerantz SC, Cavalieri TA. Practice patterns of osteopathic physicians providing end-of-life care: a survey-based study. J Am Osteopath Assoc. 2008;108(5):240–250. [PubMed] [Google Scholar]
- 53.Millison M, Dudley JR. Providing spiritual support: a job for all hospice professionals. Hosp J. 1992;8(4):49–66. [DOI] [PubMed] [Google Scholar]
- 54.Muecke R, Paul M, Conrad C, et al. Complementary and alternative medicine in palliative care: a comparison of data from surveys among patients and professionals. Integr Cancer Ther. 2016;15(1):10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Munkombwe WM, Petersson K, Elgán C. Nurses’ experiences of providing nonpharmacological pain management in palliative care: a qualitative study. J Clin Nurs. 2020;29(9–10):1643–1652. [DOI] [PubMed] [Google Scholar]
- 56.Nakano K, Sato K, Katayama H, Miyashita M. Living with pleasure in daily life at the end of life: recommended care strategy for cancer patients from the perspective of physicians and nurses. Palliat Support Care. 2013;11(5):405–413. [DOI] [PubMed] [Google Scholar]
- 57.Newell S, Sanson-Fisher RW. Australian oncologists’ self-reported knowledge and attitudes about non-traditional therapies used by cancer patients. Med J Aust. 2000;172(3):110–113. [PubMed] [Google Scholar]
- 58.O’Kelly J, Koffman J. Multidisciplinary perspectives of music therapy in adult palliative care. Palliat Med. 2007;21(3):235–241. [DOI] [PubMed] [Google Scholar]
- 59.Sproat M. Exploration of the knowledge, attitudes, and practices of complementary and alternative medicine in hospice. Georgetown University-Graduate School of Arts & Sciences. Published 2018. Accessed April 16, 2021. https://repository.library.georgetown.edu/handle/10822/1050809 [Google Scholar]
- 60.Stewart M, Cox-Davenport RA. Comparative analysis of registered nurses’ and nursing students’ attitudes and use of nonpharmacologic methods of pain management. Pain Manage Nurs. 2015;16(4):499–502. [DOI] [PubMed] [Google Scholar]
- 61.Uritsky TJ, McPherson ML, Pradel F. Assessment of hospice health professionals’ knowledge, views, and experience with medical marijuana. J Palliat Med. 2011;14(12):1291–1295. [DOI] [PubMed] [Google Scholar]
- 62.Wagland R, Ellis J, Bailey CD, et al. Considerations in developing and delivering a non-pharmacological intervention for symptom management in lung cancer: the views of health care professionals. Support Care Cancer. 2012;20(10):2565–2574. [DOI] [PubMed] [Google Scholar]
- 63.Wang S-YC, Yates P. Nurses’ responses to people with cancer who use complementary and alternative medicine. Int J Nurs Pract. 2006;12(5):288–294. [DOI] [PubMed] [Google Scholar]
- 64.Weekly T, Riley B, Wichman C, Tibbits M, Weaver M. Impact of a massage therapy intervention for pediatric palliative care patients and their family caregivers. J Palliat Care. 2019;34(3):164–167. [DOI] [PubMed] [Google Scholar]
- 65.Wong CHL, Wu IXY, Adams J, et al. Development of evidence-based Chinese medicine clinical service recommendations for cancer palliative care using Delphi approach based on the evidence to decision framework. Integr Cancer Ther. 2020;19:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rogers M, Heitner R. Latest Trends and Insights from the National Palliative Care Registry™. Presented at: The Center to Advance Palliative Care National Seminar; November 2019; Atlanta, Georgia. https://media.capc.org/recorded-webinars/slides/Final_Registry_Presentation_August_2019_6y0ElUf.pdf [Google Scholar]
- 67.Gomes B, Calanzani N, Curiale V, McCrone P, Higginson IJ. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev. 2013;(6):CD007760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Morrison RS, Maroney-Galin C, Kralovec PD, Meier DE. The growth of palliative care programs in United States hospitals. J Palliat Med. 2005;8(6):1127–1134. [DOI] [PubMed] [Google Scholar]
- 69.Riolfi M, Buja A, Zanardo C, Marangon CF, Manno P, Baldo V. Effectiveness of palliative home-care services in reducing hospital admissions and determinants of hospitalization for terminally ill patients followed up by a palliative home-care team: a retrospective cohort study. Palliat Med. 2014;28(5):403–411. [DOI] [PubMed] [Google Scholar]