Abstract
Predominantly asymptomatic infections, such as those for SARS-CoV-2, require robust surveillance testing to identify people who are unknowingly spreading the virus. The US Air Force Academy returned to in-person classes for more than 4000 cadets aged 18-26 years during the fall 2020 semester to meet graduation and leadership training requirements. To enable this sustained cadet footprint, the institution developed a dynamic SARS-CoV-2 response plan using near–real-time data to inform decisions and trigger policies. A surveillance testing program based on mathematical modeling and a policy-driven campus reset option provided a scaled approach to react to SARS-CoV-2 conditions. This program adequately controlled the spread of the virus for the first 2 months of the academic semester but failed to predict or initially mitigate a significant outbreak in the second half of the semester. Although this approach did not completely eliminate SARS-CoV-2 infections in the population, it served as an early warning system to alert public health authorities to potential issues, which allowed timely responses while containment was still possible.
Keywords: SARS-CoV-2, public health, pandemic response, infectious disease, planning
Along with thousands of colleges and universities, the US Air Force Academy in Colorado Springs, Colorado, spent months planning COVID-19 mitigation strategies for the fall 2020 academic semester, which ran from August 12 to December 4, 2020. 1 Unlike other institutions, where many students live off campus 2 and most graduation requirements may be completed virtually, the unique nature of military service academies requires in-person leadership and military components, which do not translate to the online environment.3,4 In addition, previous data on SARS-CoV-2 infections generated from the USS Theodore Roosevelt5,6 and Charles De Gaulle 7 suggested that young, healthy cohorts remain largely asymptomatic, with sailors remaining 60% and 50% asymptomatic, respectively. For the USS Theodore Roosevelt, the 3448 people aboard ranged in age from 18 to 50 years (mean = 27.2; interquartile range, 22-32), placing them in a low-risk category. The data collected throughout the semester on our campus confirmed this prediction, with approximately 80% of cadets either wholly asymptomatic or experiencing only mild, general symptoms, making detection based solely on symptoms ineffective.8,9 Further complicating control measures, cadets live together in 2 dormitories, each cadet has at least 1 roommate, and cadets use shared restrooms and a single dining facility.
During the fall 2020 semester, cadets were assigned to specific dining hours to limit the number of people in the hall at any given time, but the shared nature of all facilities made it difficult to separate cadets, even with wearing face masks, practicing social distancing, and increasing sanitation procedures. Furthermore, athletics and physical fitness is an important part of preparation for a future military officer, with required combative-type classes in the curriculum and a high level of use of the physical fitness spaces, often indoors because of variable weather conditions. To combat the virus, the institution used a SARS-CoV-2 testing strategy heavily focused on surveillance testing to identify people who had positive test results for the virus but no symptoms.10,11 By rigorously testing for the virus in asymptomatic people, infectious virus is isolated from healthy populations before it spreads, limiting the overall number of cases. Aggressive contact tracing and a dedicated facility for quarantine and isolation complemented this methodology, while a campus reset—a robust suite of policy options to curb the spread on campus—provided further mitigations against viral spread.
Purpose
The requirement for in-person lessons at the US Air Force Academy provided an opportunity to collect data on the movement of SARS-CoV-2 infections to evaluate viral transmission dynamics from August 12 through December 4, 2020. This population consisted of 4400 medically screened, healthy cadets aged 18-26 years, with no known comorbidities, rendering them less susceptible to severe courses of SARS-CoV-2 infection than older people or people with underlying health conditions.12,13 Furthermore, the nature of a college located on an active-duty Air Force base improved the ability to control interactions with the local community, by restricting base access to only mission-essential personnel. It also limited the ability of the cadets to leave base, as the military culture reinforces strict adherence to rules and regulations.
Existing data on similar populations (ie, the USS Theodore Roosevelt) suggested that most cadets would be asymptomatic if infected with SARS-CoV-2, offering little warning of an impending rise in SARS-CoV-2 cases. This lack of symptoms complicated the timing of responsive mitigation policies, because a substantial number of infections could rapidly spread through the cadet population undetected. Although our cadet group was at low risk of contracting the virus, many of the long-term effects of contracting SARS-CoV-2 remain unknown, and it is imperative to ensure the health and safety of these young cadets to be able to commission them into the military without any adverse medical complications. Furthermore, approximately 500 faculty and staff members interacted with the 4400 cadets daily. The demographic characteristics of this group did not align with those of a low-risk population, and members of this group also returned to the local community, potentially bringing unidentified SARS-CoV-2 infection with them. Surveillance testing provided a straightforward and effective measurement of the current infection status of cadets and identified people for isolation who may have unknowingly spread the virus, thereby limiting the potential for populations at high risk for SARS-CoV-2 to contract the virus.
Throughout the first half of the semester, this surveillance testing limited the spread of SARS-CoV-2 infections in our population. However, an increase in community prevalence coupled with several ill-timed social gatherings led to a rapid rise in cases, forcing public health officials to implement a lockdown or “reset” procedure to ensure the safety and well-being of all personnel. This reset halted the virus spread and highlighted that, in addition to identifying people who received a positive test result for SARS-CoV-2, random surveillance testing also provides an early warning system to identify increased viral transmission within the tested population. 14
Methods
Planning and Adaptive Daily Surveillance
Analysts used a stochastic Susceptible–Exposed–Infected–Recovered compartmental model previously validated for our population to predict the spread of SARS-CoV-2 infection throughout the cadet population under various surveillance testing rates. 14 The model included symptomatic and asymptomatic infection compartments, as well as quarantine and isolation compartments, permitting detailed forecasts of possible outcomes from various observed conditions. Model parameters (eg, transmissibility, reproductive number, asymptomatic rates) based on institutional population dynamics laid the modeling groundwork to inform policies related to classroom density, military training activities, and off-base liberties (Table). Current infection prevalence and reproductive number estimates were the most critical parameters for forecasting trends from 2 weeks to 2 months into the future and were used to track the effectiveness of the implemented policies. The number of tests performed weekly and the percentage of cadets randomly selected depended on the positivity rate previously observed in the 4400-person cadet cohort. These selected people participated in pooled surveillance testing. 15 To determine positive test results, the laboratory used the guidance provided in the Emergency Use Authorization for the Smart Detect SARS-CoV-2 rRT-PCR Kit (InBios). A presumptive-positive test result amplified on a single viral primer target (envelope, nucleocapsid, or Orf1b), whereas a true-positive test result amplified on at least 2 viral primer targets. If a pooled sample returned a true-positive or presumptive-positive test result, the samples for the 8 people in the pool were rerun individually, to identify the infected individual.
Table.
Lockdown criteria and policy levers used at the US Air Force Academy during the COVID-19 pandemic, August 12–December 4, 2020 a
| Response components | Phase 0: baseline COVID-19 operations | Phase 1: contain the spread | Phase 2: soft lockdown | Phase 3: full lockdown |
|---|---|---|---|---|
| Objective | COVID-19 mitigation and surveillance | Reinforce mitigation compliance, 50% testing increase | Increase testing, reduce interactions by 50% | Identify most infections and reset |
| Criteria | Number of new weekly infections <5 | Number of known active infections >10 | Number of known active infections >20 | Number of known active infections >50 |
| Surveillance testing | 4% daily; 16% weekly; Tuesday through Friday | 6% daily; 24% weekly; Tuesday through Friday | 9% daily; 45% weekly; Monday through Friday | 15% testing daily; 100% weekly; Sunday through Saturday |
| Students | • Full-use common areas • Full freedom to associate |
Limit social interaction to study groups, clubs, etc | • Restricted to living areas and quads • Lounge 50% capacity • Minimum trips to grocery |
• Restricted to room • Takeout dining only |
| Training | All passes | • Day pass only • Overnight pass by exception |
• Off-base access by exception • Military training by distance only |
Off-base passes by exception |
| Academics | 50% Remote teaching | 50% Remote teaching | 75% Remote teaching | • 100% Remote teaching • In-person laboratories by exception |
| Athletics | Gym: 25% capacity | Gym: 25% capacity | • Noncontact physical education courses only • Gym: 15% capacity |
• Remote physical education only • Gym closed |
| Other | Sit-down restaurants and retail shopping permitted | Curbside pick-up only | Intramurals canceled | • Clubs virtual • Facilities closed |
Protocols recommended by the Centers for Disease Control and Prevention, such as wearing face masks and social distancing, were maintained across all phases. Once in Phase 3 (full lockdown), it was possible to revert to previous phases after at least 1 week post-lockdown testing, and when the number of known active infections met the previous phase threshold.
Campus Reset
Once cases met the reset threshold and the readiness posture shifted from Phase 2 to Phase 3 (Table), 100% of the cadet population was tested on day 0, 50% again by day 7, and the remaining 50% by day 14, culminating at the end of the semester with 100% testing of the entire cadet student body (Figure). Once triggered to begin Phase 3, operations remained at this level for a minimum of 2 weeks. After 2 weeks elapsed, operations resumed at a lower phase, based on the number of known active infections at the time. We defined a known active infection as an individual who received a positive test result and either was within the 10-day required isolation period or had not received 2 negative real-time polymerase chain reaction (RT-PCR) test results.
Figure.
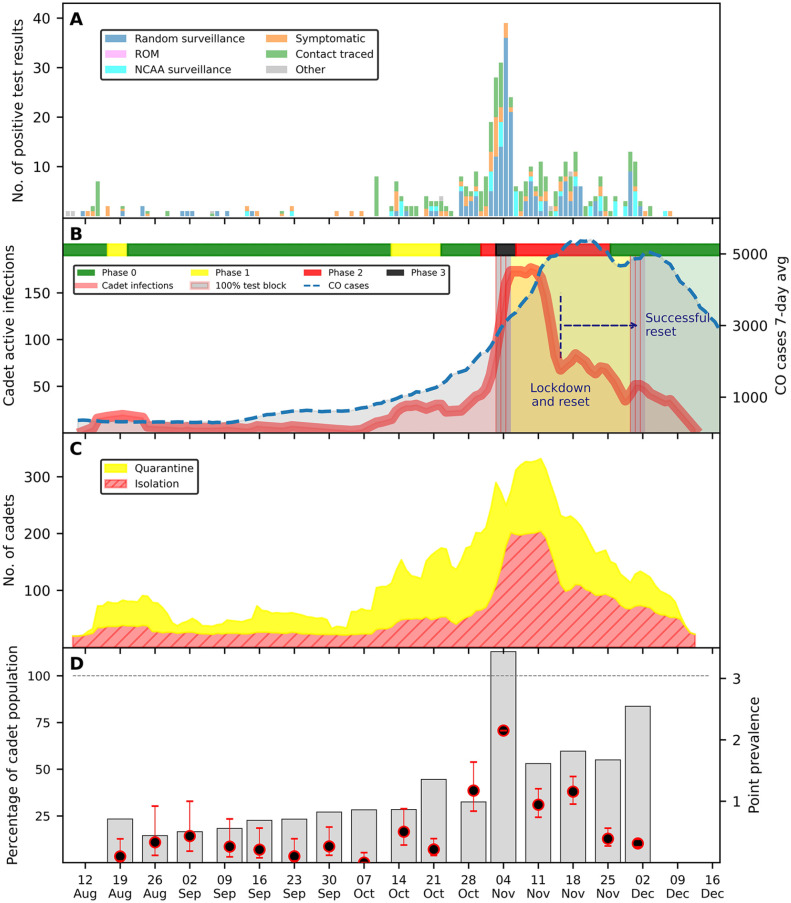
US Air Force Academy cadet COVID-19 case and surveillance summary during fall semester 2020 (August 12–December 4) for 4400 cadets. (A) Daily number of positive SARS-CoV-2 test results, by origin of testing. (B) Number of active infections among cadets, by phase of surveillance operation, and cumulative number of cases in Colorado (100% of susceptible cadet student body tested during 3 days in indicated 100% test blocks). (C) Total number of cadets in quarantine (those who had been in close contact [within 6 feet] with an infected individual) and isolation (a positive test result for SARS-CoV-2). (D) Percentage of the cadet student body tested in each week and prevalence of infection estimated from surveillance testing. Circles indicate point prevalence; errors bars indicate 95% Wilson hypergeometric CIs. The bar for November 4 exceeds 100%, as that week some people were tested twice, Monday and Friday. Abbreviations: CO, Colorado; NCAA, National Collegiate Athletic Association; ROM, restriction of movement.
Isolation and Quarantine
Upon receiving a positive test result or being identified via contact tracing, individuals moved to isolation or quarantine quarters, respectively. These individuals were subsequently tested on day 7, day 10, and day 14, per local guidelines. Contact tracing included roommates, teammates, and classmates sitting within 6 feet of the infected individual. Public health personnel conducted interviews with infected individuals to determine additional people of interest.
Laboratory Testing
Trained medical technicians obtained nasopharyngeal swab specimens stored in saline or viral transport medium. The Smart Detect SARS-CoV-2 rRT-PCR Kit run on a Bio-Rad CFX96, or the Cepheid GeneXpert Xpert Xpress SARS-CoV-2 Emergency Use Authorization assays determined SARS-CoV-2 presence. For pooled surveillance testing, samples were processed using the QIAamp Viral RNA Mini Kit (Qiagen), modified for 8 individuals per RNA extraction. Modifications included 1120 µL total human sample (140 µL per sample × 8 individuals), lysed with 1120 µL buffer and quenched with 1120 µL ethanol, then processed per the manufacturer’s instructions. The turnaround time for test results depended on the number of samples processed. During Phases 0, 1, and 2, results were available for the pooled samples within 4-6 hours of sample drop-off, with follow-up on individual tests requiring an additional 2-4 hours, depending on the number of pools with a positive test result. For Phase 3 operations, the laboratory provided results on pooled samples and follow-up on individuals within 12-16 hours of sample drop-off. The US Air Force Academy Institutional Review Board determined the surveillance testing and mathematical modeling (FAC20200024N and FAC20200025N, respectively) were not human subjects research in accordance with 32 CR 219, DoDI3216.02 and AFI 40-402.
Outcomes
Modeling simulations, experience from previous semesters, and senior leadership input helped create tiered responses (Table) to appropriately balance limiting SARS-CoV-2 spread with maintaining cadet morale. These criteria also accounted for quarantine and isolation capacity: by triggering increases in mitigation efforts early enough to ensure availability, based on predicted viral spread dynamics. Despite the large emphasis on random surveillance testing, continued positive case identification in symptomatic people (15%, n = 59) as well as people who were contact traced based on previous positive test results (32%, n = 125) was also instrumental in preventing outbreaks (Figure, Panel A).
The surveillance testing program identified 18 and 13 cases of SARS-CoV-2 in August and September, respectively. However, the number of cases steadily increased throughout October (Figure, Panel B) until it hit 79 cases, with more than 150 cadets in quarantine or isolation (Figure, Panel C), triggering a “population reset” or 100% cadet testing event from November 3-7, when 122 people received a positive test result for SARS-CoV-2 (Figure, Panel D). The original reset trigger was set to 50 cases; however, because of the spread throughout the cadet population, 28 people received a positive test result on 1 day, prompting the reset. In November, 298 people received a positive test result. After the reset and additional testing, the number of positive cases decreased, with 17 people receiving a positive test result during December, marking the end of the semester (Figure).
Lessons Learned
Although surveillance testing detected a spike in COVID-19 cases during October, the rapid rise of infections quickly surpassed multiple decision thresholds, triggering a lockdown and reset event. This reset was resource intensive—more than 12 000 tests were conducted across 1500 pools in a 4-week period—but the results highlight the importance and practicality of surveillance testing. This strategy took a 2-week commitment to see results and required the cadets to adhere to strict policies aimed at reducing viral transmission. The number of SARS-CoV-2 infections dropped from 175 known active cases at the peak of the outbreak on November 7 to 75 known active cases 2 weeks later. The increase in cases in the surrounding El Paso County community documented by the Colorado Department of Public Health 16 coincided with an increase in surveillance testing by 50% throughout the remainder of November because of the lingering level of COVID-19 infections among cadets. The increase in surveillance testing also served to pick up any potential secondary infections caused by the 175 people who received a positive test result and were in isolation, leading to the identification of an additional 150 people with SARS-CoV-2 infection.
Timeliness was critical to surveillance testing. Determining test results within 8 hours enabled faster isolation of positive cases and reduced spread. Pooled testing provided a relatively rapid means of conducting hundreds of tests. When public health personnel identified people in a pool with positive test results, they instructed the pool members to quarantine in their dormitory rooms for the additional 2-4 hours until individual tests were completed. This process, versus the 24-48 hours required to resolve hundreds of individual tests, allowed public health personnel to identify individuals with initially positive test results early and restrict their movement in a way that minimized the risk of SARS-CoV-2 spread among potentially positive people, until the final test results were available a few hours later.
In addition to an increase in testing, several transmission mitigation policies were implemented, including restrictive measures that took a mental health toll on the population. As the phases of lockdown increased, it was essential to increase access to mental health providers to ensure each cadet received the care and support he or she needed. This requirement is especially necessary in a military academy, where people come from across the United States and internationally, with little established support structure in the local area, but a lot of leadership and military responsibilities that force them to perform under adverse conditions. Future implementations should deliberately anticipate and plan for this increase in mental health support to ensure that resources are available when required.
For some institutions or populations at high risk of acquiring SARS-CoV-2 infection, where many infections result in hospitalization or death, our approach may not be viable. The young, healthy Air Force Academy population experienced no hospitalizations or fatalities, but the virus still spread rapidly throughout the institution when testing was inadequate. Our approach is useful in younger populations, where medical professionals must balance the physical risk of SARS-CoV-2 with the mental risk of extended isolation. Further, this plan provided an additional use for surveillance testing, as an early warning system. Although it is important to detect SARS-CoV-2 cases, it is even more important to be able to react to the information received from these tests. By predetermining policies and the thresholds required to trigger these decision points regarding policy implementation, it is possible to react in a timely manner to curb infections, while monitoring for a safe return to routine operations.
Conclusions
SARS-CoV-2 infections within a population are dynamic. In the scenario described in this case study, a robust surveillance plan enabled near–real-time feedback into planning parameters and mathematical modeling, giving leaders the information required to make policy decisions. Surveillance testing served as a warning system, offered a means of control, and provided a monitoring system to university officials to implement policies limiting interactions, thereby halting further spread of SARS-CoV-2. Although on-hand surveillance testing options capable of surging to meet the heavy test load required to reset a population may seem daunting, through pooled testing and a strategy reliant on minimizing exposure, organizations may feel confident in their ability to respond and resume routine operations after an outbreak.
Acknowledgments
The authors thank the men and women of the 10th Medical Group for their sampling support throughout the semester and Cadet Wing leadership for maintaining an effective quarantine and isolation space. Furthermore, deep gratitude is extended to members of the Department of Biology: Katherine Bates, PhD, Dave Westmoreland, PhD, Lt Col Matt Adkins, Lt Col Odaro Huckstep, Lt Col Emily Marr, Lt Col Dave Morris, Maj Austin Almand, Maj John Des Jarlais, Maj Travis Tubbs, Capt Carlee Koutnik, and Capt Max Lucero with help from the Department of Chemistry Lt Col Winfred Dela Cruz, Maj Dan Higgins, Capt Courtney Kiggins, and Capt Alexa Whipple, for processing all the samples, and the US Air Force Academy Dean of Faculty, Brig Gen Linell Letendre, for her unwavering support. The views expressed in this article are those of the authors and do not reflect the official policy or position of the US Air Force, US Department of Defense, or the US government. This article is released under Distribution Statement A: Approved for public release: distribution unlimited, PA#: USAFA-DF-2021-98.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The work was funded by the US Air Force Academy and the Defense Health Agency Clinical Investigations Program.
ORCID iD: Erin A. Almand, PhD  https://orcid.org/0000-0002-5034-9652
https://orcid.org/0000-0002-5034-9652
References
- 1. Paltiel AD, Zheng A, Walensky RP. Assessment of SARS-CoV-2 screening strategies to permit the safe reopening of college campuses in the United States. JAMA Netw Open. 2020;3(7):e2016818. doi: 10.1001/jamanetworkopen.2020.16818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Center for Education Statistics. National Postsecondary Student Aid Study—overview. Accessed March 27, 2021. https://nces.ed.gov/surveys/npsas
- 3. US Air Force Academy. Academy overview. Accessed January 23, 2021. https://www.usafa.edu/about
- 4. Baettig SJ, Parini A, Cardona I, Morand GB. Case series of coronavirus (SARS-CoV-2) in a military recruit school: clinical, sanitary and logistical implications. BMJ Mil Health. 2021;167(4):251-254. doi: 10.1136/bmjmilitary-2020-001482 [DOI] [PubMed] [Google Scholar]
- 5. Kasper MR, Geibe JR, Sears CL, et al. An outbreak of COVID-19 on an aircraft carrier. N Engl J Med. 2020;383(25):2417-2426. doi: 10.1056/NEJMoa2019375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Payne DC, Smith-Jeffcoat SE, Nowak G, et al. SARS-CoV-2 infections and serologic responses from a sample of U.S. Navy service members—USS Theodore Roosevelt, April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):714-721. doi: 10.15585/mmwr.mm6923e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leclerc QJ, Fuller NM, Knight LE, Funk S, Knight GM. What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Res. 2020;5:83. doi: 10.12688/wellcomeopenres.15889.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406-1407. doi: 10.1001/jama.2020.2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):377-381. doi: 10.15585/mmwr.mm6913e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3):2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Denny TN, Andrews L, Bonsignori M, et al. Implementation of a pooled surveillance testing program for asymptomatic SARS-CoV-2 infections on a college campus—Duke University, Durham, North Carolina, August 2–October 11, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(46):1743-1747. doi: 10.15585/mmwr.mm6946e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yadav R, Aggarwal S, Singh A. SARS-CoV-2-host dynamics: increased risk of adverse outcomes of COVID-19 in obesity. Diabetes Metab Syndr. 2020;14(5):1355-1360. doi: 10.1016/j.dsx.2020.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Endocrinol Metab. 2020;318(5):E736-E741. doi: 10.1152/ajpendo.00124.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cullenbine CA, Rohrer JW, Almand EA, et al. Fizzle testing: an equation utilizing random surveillance to help reduce COVID-19 risks. Math Comput Appl. 2021;26(1):16. doi: 10.3390/mca26010016 [DOI] [Google Scholar]
- 15. Ben-Ami R, Klochendler A, Seidel M, et al. Large-scale implementation of pooled RNA extraction and RT-PCR for SARS-CoV-2 detection. Clin Microbiol Infect. 2020;26(9):1248-1253. doi: 10.1016/j.cmi.2020.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Colorado Department of Public Health and Environment. Colorado COVID-19 data. Accessed October 18, 2021. https://covid19.colorado.gov/data