Abstract
Study Design:
Retrospective cohort study.
Objective:
Implant subsidence is an important prognostic factor after anterior cervical discectomy and fusion (ACDF). Our purpose in this study was to investigate whether graft position affects subsidence after ACDF and to determine if there is a difference in clinical results based on allograft subsidence and position.
Methods:
We reviewed 92 patients who underwent single-level ACDF with allograft and plate between January 2012 and October 2018. Treatment levels were divided based on allograft position within 2 mm of the posterior margin of the augmented plate (Anterior group) or at greater than 2 mm (Center group). Subsidence was defined as segmental vertebral body height decrease of 2 mm or more at 1 year compared to 1 week after surgery.
Results:
Overall subsidence prevalence was 15 (16%) cases. Subsidence was 11% in the Anterior group (8/73) and 39% in the Center group (7/19; P = .012). The subsidence group showed smaller graft footprint size (graft/endplate ratio) compared with the nonsubsidence group, and pseudarthrosis occurred frequently in the subsidence. There was no significant difference in clinical results according to graft position. These findings indicate that anterior graft position reduces risk of subsidence (95% confidence interval = 0.085-0.949).
Conclusion:
To minimize risk of subsidence, the graft should be positioned on the anterior position of the surgical-level endplate. In addition, using a graft appropriate for endplate size will further reduce subsidence.
Keywords: anterior cervical discectomy and fusion, ACDF, allograft, subsidence, cervical
Introduction
Anterior cervical discectomy and fusion (ACDF) is widely performed for cervical spondylosis and disc disease. Although use of the iliac crest autogenous bone graft remains the gold standard, harvest site complications, such as infection, donor site pain, and fracture, occur frequently.1,2 To avoid donor site complications, many surgeons use allograft as a substitute for autogenous bone graft. However, it has been reported that graft collapse and nonunion occur frequently in ACDF with allograft compared to that with autobone. 3 In particular, previous studies have reported an incidence of graft subsidence in ACDF with allograft of 5% to 62.5%.2,4-6 There is currently controversy and discussion on the association between graft subsidence and clinical outcome.
A few reports have indicated that use of a cage anteriorly during ACDF has lower subsidence than cage at a posterior position, because anterior support of the cortical bone reduces subsidence of the graft.7,8 To our knowledge, no direct research on the relationship between graft position and subsidence in ACDF with allograft and plate augmentation has been reported. We hypothesize that anterior support of the cortical bone will reduce the subsidence of grafts like a stand-alone cage ACDF; this approach could enhance fusion and affect clinical outcomes. Our purpose in this study was to investigate if graft position affects allograft subsidence after ACDF with allograft and plate. In addition, we aimed to determine if there is a difference in clinical results based on allograft subsidence and implant position. We therefore designed this study to assess changes in radiologic parameters (C2-C7 angle, segmental angle, segmental height, graft size, subsidence, and fusion rate) according to graft position after ACDF with allograft and plate augmentation. For prognostic analysis according to subsidence, radiologic parameters and clinical results were compared with or without subsidence.
Methods
This present retrospective cohort study comprised 92 patients (59 male and 33 female patients; mean age, 48.7 years) who underwent single-level ACDF with allograft and plate from January 2012 to October 2018. The inclusion criteria were (1) symptoms of cervical radiculopathy and/or myelopathy, (2) pathologies consistent with cervical spondylosis or herniated cervical disc, (3) underwent single-level ACDF with allograft and plate, and (4) a follow-up period ≥12 months and including cervical spine computed tomography (CT). Patients with additional posterior surgery procedures, infection, or revision surgery were excluded, as were patients with a follow-up <12 months.
All patients underwent single-level ACDF with allograft and plate procedures using the standard Smith-Robinson approach under general anesthesia performed by 2 surgeons in a single center. To accomplish interbody fusion, one surgeon (DKC) used freeze-dried bone allograft, a Skyline plate (DuPuy Synthes), fixed screws at the top of the fusion level and variable screws at the bottom. Another surgeon (KHK) used machined allograft, an Atlantis plate (Medtronic Sofamor-Danek), and fusion was performed using fixed screws.
Radiologic and Clinical Assessments
For radiological assessment, anteroposterior (AP), lateral, and flexion-extension radiographs were obtained preoperatively and postoperatively at 1 week and 12 months after surgery. Cervical spine CT assessments were performed before surgery and 1 year after surgery. Every radiologic parameter was measured at each follow-up period by an independent neurosurgeon and a neuroradiologist who were blinded to the treatment details. The C2-C7 angle, segmental angle of the surgery level, end plate length, graft length, and segmental vertebral body height were measured on neutral lateral radiographs (Figure 1). CT and simple radiography were assessed 1 year after surgical treatment, and pseudarthrosis was assessed with the Bridwell grading system. 9 Fusion was graded from I to IV: fusion with remodeling and trabeculae (I); graft intact, not fully remodeled and incorporated, but no lucency (II); graft intact, potential lucency at the top and bottom of graft (III); and fusion absent with collapse/resorption of graft (IV). According to the Bridwell grading system, solid fusion is defined as grade I based on radiologic outcomes.
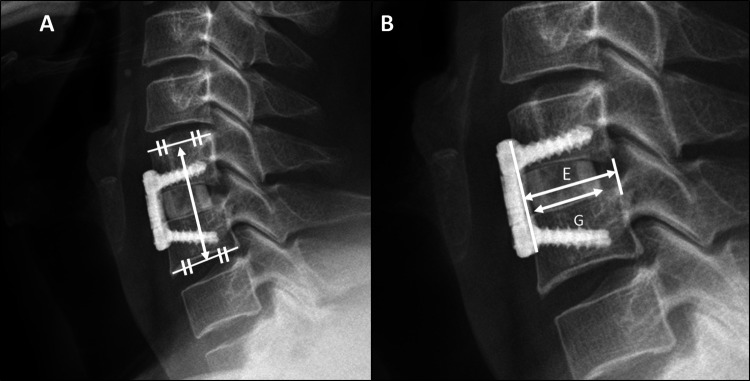
Figure 1.
(A) Segmental vertebral body height: The distance between the midpoint of the cranial vertebra upper endplate and the midpoint of the caudal vertebra lower endplate at the fusion level. (B) “The Graft/Endplate ratio” is defined as graft length (G) divided by endplate length (E) to determine the relative size of the graft to the endplate. E: endplate length: the length of the line passing through the center of the graft from the posterior margin of the plate to the posterior disc margin at the treated level. G: graft length.
We measured C2-C7 angle and segmental angle to evaluate cervical lordosis and local angle. The C2-C7 angle was measured as that formed by a line drawn parallel to the lower endplates of C2 and C7 on a neutral plain radiograph. The segmental angle was assessed as that formed by the lines drawn parallel to the superior margin of the upper vertebral body and the inferior margin of the lower vertebral body of the treated level on a neutral simple radiograph. Segmental vertebral body height for subsidence evaluation was measured as the total vertical height of the 2 vertebral bodies of the treated level. This height was measured by the distance between the midpoint of the upper endplate of the cranial vertebral body at the fusion level and the midpoint of the lower endplate of the caudal vertebral body (Figure 1A). For relative graft size for the vertebral body, the length of the endplate was defined as the length of the line passing through the center of the graft, from the posterior margin of the plate to the posterior disc margin of the treated level. The graft/endplate ratio was assessed as graft length divided by end plate length relative to the size of the graft to the endplate (Figure 1B).
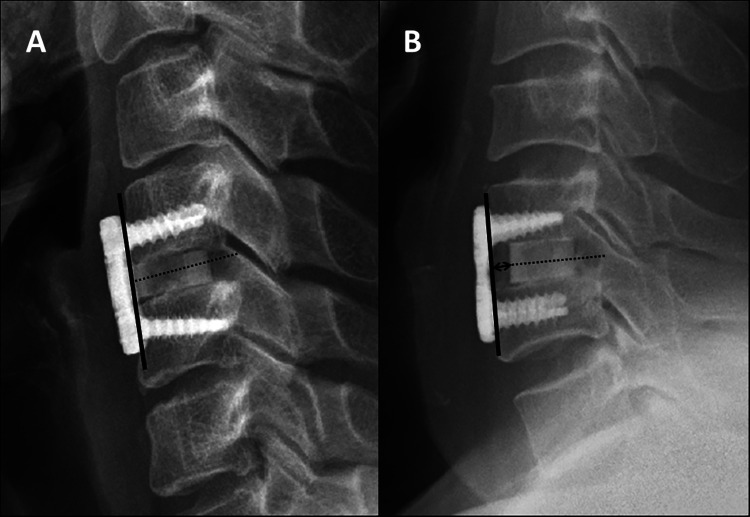
Measurement of subsidence is inconsistently defined in the literature because of use of relative and absolute measurements, and the most frequently used measurement method for definition of subsidence was based on a threshold of 2 mm. Therefore, we defined cases as “subsidence” when the segmental vertebral body height decreased by 2 mm or more in 1 year compared with the results obtained 1 week after surgery (Figure 2). To investigate whether graft position affects allograft subsidence after ACDF with allograft and plate, we divided patients into 2 groups according to graft location. The “Anterior group” was defined as cases where the center of the anterior margin of the inserted allograft was located within 2 mm from the posterior margin of the plate, and the “Center group” was defined as cases where the inserted allograft was located farther than 2 mm (Figure 3). Furthermore, clinical status was evaluated using Visual Analogue Scale (VAS) score and Neck Disability Index (NDI) score preoperatively and at l year after surgery.
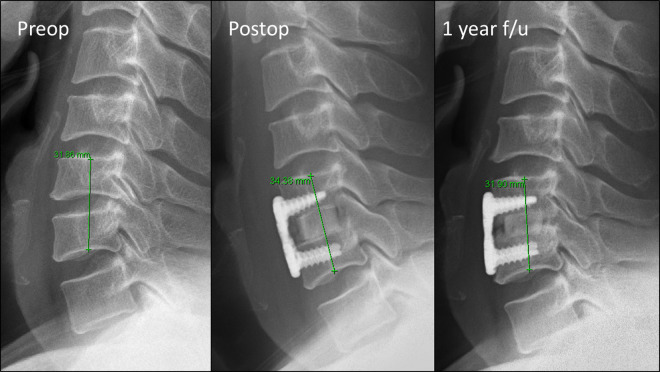
Figure 2.
An illustrative case of implant subsidence in a 48-year-old man with C5/6 degenerative disc disease who underwent discectomy with allograft and plate. Comparison of immediate postoperative lateral study with a 1-year radiograph demonstrates a loss of 2.48 mm of segmental vertebral body height.
Figure 3.
Anterior group (A) was defined as cases where the center of the anterior margin of the inserted allograft was located within 2 mm from the posterior margin of the plate, and the Center group (B) was defined as cases where the inserted allograft was located farther than 2 mm.
Statistical Analysis
Descriptive data are represented as mean ± standard deviation. For statistical analysis, the Mann-Whitney U and Fisher’s exact tests and linear-by-linear association method were used. Multivariate logistic regression analysis was performed to identify risk factors that postoperatively affected subsidence. Significance was achieved at a 95% confidence interval (IBM SPSS 25, IBM Corporation). For post hoc power analysis, G*Power version 3.1.9 (Universität Kiel) 10 was used.
Results
Graft Position: Anterior Group Versus Center Group (Table 1)
Table 1.
Comparison According to Graft Positiona.
| Whole group (n = 92) | Anterior group (n = 73) | Center group (n = 19) | P | |
|---|---|---|---|---|
| Age (years) | 48.7 ± 10.6 | 48.2 ± 10.3 | 48.1 ± 10.4 | .968 |
| Sex (male/female) | 59/33 | 44/29 | 15/4 | .181 |
| Body mass index | 25.0 ± 2.84 | 24.6 ± 2.91 | 25.6 ± 3.1 | .078 |
| Operation segments | ||||
| C3-C4 | 6 | 4 | 2 | |
| C4-C5 | 14 | 13 | 1 | |
| C5-C6 | 47 | 37 | 10 | |
| C6-C7 | 25 | 19 | 6 | .709 |
| Plate/graft/screw type | ||||
| Skyline/FDBA/Fixed+Variableb | 55 | 46 | 9 | |
| Atlantis/Machined/Fixedc | 37 | 27 | 10 | .215 |
| Preoperative radiologic parameters | ||||
| C2-C7 angle (°) | 7.09 ± 12.78 | 8.01 ± 12.37 | 3.53 ± 14.04 | .235 |
| Segmental angled (°) | 4.42 ± 8.16 | 4.93 ± 7.91 | 2.47 ± 8.97 | .403 |
| Segmental height (mm) | 34.43 ± 3.19 | 34.21 ± 3.22 | 35.27 ± 2.97 | .197 |
| Postoperative radiologic parameters | ||||
| 1 week | ||||
| C2-C7 angle (°) | 9.05 ± 9.29 | 9.68 ± 9.10 | 6.59 ± 9.84 | .197 |
| Segmental angled (°) | 5.99 ± 7.23 | 6.45 ± 7.14 | 4.37 ± 6.29 | .251 |
| Segmental height (mm) | 36.36 ± 2.99 | 36.19 ± 3.05 | 36.99 ± 2.75 | .302 |
| Graft/endplate ratioe | 74.5 ± 10.6% | 75.9 ± 11.0% | 69.0 ± 6.58% | .01 |
| 1 year | ||||
| C2-C7 angle (°) | 9.31 ± 10.22 | 10.01 ± 10.37 | 6.60 ± 9.38 | .175 |
| Segmental angled (°) | 5.57 ± 7.28 | 5.99 ± 7.23 | 3.95 ± 7.43 | .406 |
| Segmental height (mm) | 35.20 ± 2.95 | 35.18 ± 2.92 | 35.31 ± 3.12 | .857 |
| Subsidencef | 15 (16%) | 8 (11%) | 7 (39%) | .012 |
| Pseudarthrosis | 13 (14%) | 10 (14%) | 3 (15%) | .727 |
| Clinical result | ||||
| Preoperative VAS | 5.77 ± 1.85 | 5.64 ± 1.84 | 6.26 ± 1.82 | .123 |
| Postoperative 1-year VAS | 2.27 ± 1.65 | 2.30 ± 1.71 | 2.16 ± 1.42 | .67 |
| Preoperative NDI | 30.74 ± 5.63 | 30.55 ± 5.54 | 31.47 ± 6.50 | .322 |
| Postoperative 1-year NDI | 18.00 ± 4.22 | 18.29 ± 4.21 | 16.89 ± 4.15 | .205 |
Abbreviations: FDBA, freeze-dried bone allograft; VAS, Visual Analogue Scale; NDI, Neck Disability Index.
a Descriptive data represents mean ± standard deviation. Boldface indicate that the number is statistically significant, p<0.05.
b Skyline anterior cervical plate (manufactured by Dupuy) with FDBA, freeze-dried bone allograft, fixed with fixed-angle type screws at the top of the fusion level and variable-angle type screws at the bottom.
c Atlantis anterior cervical plate (manufactured by Medtronic) with machined structural allograft spacer, fixed with fixed-angle type screws.
d Segmental angle is the angle formed by the lines drawn parallel to the superior margin of the upper vertebral body and the inferior margin of the lower vertebral body of the treated level.
e Graft/endplate ratio is defined as graft length divided by endplate length.
f Subsidence is defined segmental vertebral body height decreased by more than 2 mm at 1 year after surgery than at 1 week after surgery.
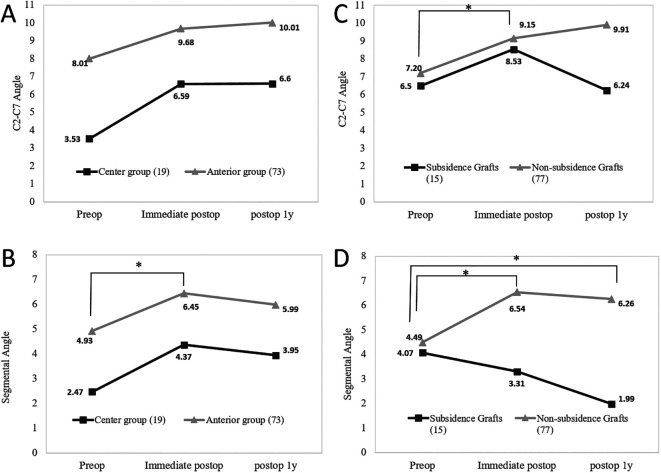
Of the 92 grafts, 73 were anteriorly positioned (Anterior group) and 19 were center-positioned (Center group). The 2 groups (Anterior/Center) showed similar characteristics regarding age, sex, body mass index, surgery level, instruments types (grafts, plates, screws), and preoperative radiologic parameters. However, the Graft/Endplate ratio was larger in the Anterior group (75.9%) than in the Center group (69.0%; P = .01). Graft displacement and extrusion of implants were not observed. Overall, subsidence occurred in 15 of 92 (16.3%) grafts. Subsidence occurred in 8 of 73 (11%) grafts in the Anterior group and in 7 of 19 (39%) cases in the Center group (P = .012). There was no difference in C2-C7 angle, segmental angle, or segmental height according to graft position at any period, but the change in segmental vertebral body height between the first week and the first year after surgery was greater in the Center group (36.99 to 35.31 mm) than the Anterior group (36.19 to 35.18 mm; Figure 4). When comparing C2-C7 and segmental angle changes before surgery and 1 week after surgery, the segmental angle significantly increased at 1 week after surgery in the Anterior group (4.93° to 6.45°, P = .04). There was no significant change in segmental angle in the Center group and no significant difference in C2-C7 angle in either group at any period (Figure 5A and B).
Figure 4.
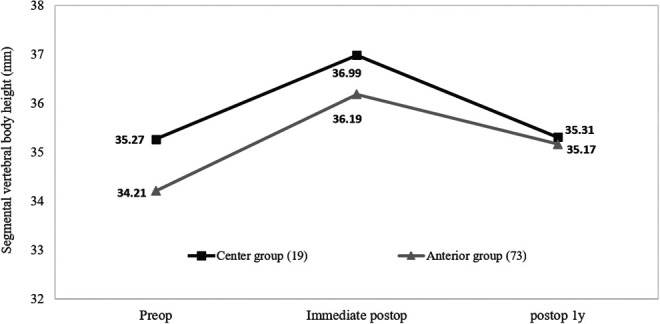
Segmental vertebral body height of the Anterior group and Center group at each period; there was no difference in segmental vertebral body height between groups. However, at 1 year after surgery, the decrease in segmental vertebral body height of the Center group (36.99 to 35.31 mm) was greater than that in the anterior group (36.19 to 35.18 mm).
Figure 5.
Changes over time in C2-C7 (A) and segmental angle (B) according to graft position and changes in C2-C7 (C) and segmental angle (D) according to subsidence. *Indicates significant change in angle during the specific period (P < .05).
At 1 year after surgery, fusion was evident for 79 (85.9%) of the 92 inserted grafts. Pseudarthrosis occurred in 10 of 73 (14%) patients in the Anterior group and 3 of 19 (15%) patients in the Center group (P = .727). The VAS (Anterior, 5.64 to 2.30; Center, 6.26 to 2.16; P < .001) and NDI scores (Anterior, 30.55 to 18.29; Center, 31.47 to 18.29; P < .001) improved at 1 year after surgery in both groups. These results revealed no significant difference between groups for either value (Table 1).
Subsidence Versus Nonsubsidence Grafts (Table 2)
Table 2.
Clinical and Radiologic Results According to Subsidencea.
| Subsidence (n = 15) | Nonsubsidence (n = 77) | Univariate logistic regression | Multivariate logistic regression | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |||
| Age (years) | 51.93 ± 6.87 | 48.03 ± 10.83 | 1.038 (0.982-1.098) | .183 | ||
| Sex (male/female) | 11/4 | 48/29 | 1.661 (0.484-5.705) | .42 | ||
| Body mass index | 24.6 ± 2.91 | 25.6 ± 3.1 | 0.909 (0.749-1.102) | .331 | ||
| Operation level | ||||||
| C3-C4 | 1 (7%) | 5 (6%) | 1 | |||
| C4-C5 | 1 (7%) | 13 (17%) | 0.385 (0.020-7.404) | .527 | ||
| C5-C6 | 6 (40%) | 41 (53%) | 0.732 (0.073-7.384) | .791 | ||
| C6-C7 | 7 (47%) | 18 (23%) | 1.944 (0.192-19.741) | .574 | ||
| Plate/graft/screw type | ||||||
| Skyline/FDBA/Fixed+Variableb | 10 (67%) | 45 (58%) | 1 | |||
| Atlantis/Machined/Fixedc | 5 (33%) | 32 (42%) | 0.703 (0.219-2.255) | .554 | ||
| Preoperative radiologic parameters | ||||||
| C2-C7 angle (°) | 6.50 ± 12.80 | 7.20 ± 12.86 | 1.004 (0.962-1.048) | .845 | ||
| Segmental angled (°) | 4.07 ± 6.15 | 4.49 ± 8.52 | 1.006 (0.940 -1.077) | .857 | ||
| Postoperative radiologic parameters | ||||||
| Graft position (anterior/center) | 8/7 | 65/12 | 0.211 (0.064-0.691) | .01 | 0.280 (0.083-0.949) | .041 |
| 1 week | ||||||
| C2-C7 angle (°) | 8.53 ± 9.31 | 9.15 ± 9.34 | 1.007 (0.948-1.070) | .814 | ||
| Segmental angled (°) | 3.31 ± 4.57 | 6.54 ± 7.27 | 1.073 (0.985 -1.169) | .105 | ||
| Graft/endplate ratioe | 68.7 ± 9.2% | 75.6 ± 10.6% | 0.481 (0.254-0.913) | .025 | 0.530 (0.266-1.056) | .071 |
| 1 year | ||||||
| C2-C7 angle (°) | 6.24 ± 9.66 | 9.91 ± 10.27 | ||||
| Segmental angled (°) | 1.99 ± 5.76 | 6.26 ± 7.37 | ||||
| Pseudarthrosis | 6 (40%) | 7 (9%) | ||||
| Clinical result | ||||||
| Preoperative VAS | 6.33 ± 2.19 | 5.66 ± 1.77 | ||||
| Postoperative 1-year VAS | 2.33 ± 1.68 | 2.26 ± 1.66 | ||||
| Preoperative NDI | 29.80 ± 6.01 | 30.92 ± 5.57 | ||||
| Postoperative 1-year NDI | 16.67 ± 3.48 | 18.26 ± 4.32 | ||||
Abbreviations: OR, odds ratio; CI, confidence interval; VAS, Visual Analogue Scale; NDI, Neck Disability Index.
a Descriptive data represents mean ± standard deviation. Boldface indicate that the number is statistically significant, p<0.05.
b Skyline anterior cervical plate (manufactured by Dupuy) with FDBA, freeze-dried bone allograft, fixed with fixed-angle type screws at the top of the fusion level and variable-angle type screws at the bottom.
c Atlantis anterior cervical plate (manufactured by Medtronic) with machined structural allograft spacer, fixed with fixed-angle type screws.
d Segmental angle is the angle formed by the lines drawn parallel to the superior margin of the upper vertebral body and the inferior margin of the lower vertebral body of the treated level.
e Graft/endplate ratio is defined as graft length divided by endplate length and odds ratio of the Graft/Endplate ratio is per 0.1.
We compared the results for cases of subsidence grafts and nonsubsided grafts. The graft subsided in 15 patients and was not subsided in 77 patients. The 2 groups showed similar distributions of age, sex, body mass index, operation level, instruments types (grafts, plates, screws), and preoperative radiologic parameters. However, the Graft/Endplate ratio was larger in the nonsubsidence (75.9%) than subsidence group (68.7%; P = .018). As mentioned above, the number of subsidence grafts was 8/73 (11%) in the Anterior group and 7/19 (37%) in the Center group, whereas the instance of nonsubsidence was 65/73 (89%) in the Anterior group and 12/19 (63%) in the Center group. Pseudarthrosis occurred frequently in subsidence (6/15, 40%) compared with nonsubsidence (7/77, 9%) cases (P = .006).
Among postoperative radiologic parameters, C2-C7 (7.20° to 9.15°, P = .01) and segmental angle (4.49° to 6.54°, P = .01) became more lordotic 1 week after surgery in the nonsubsidence cases (Figure 5C and D). Segmental angle (4.49° to 6.26°, P = .01) also became more lordotic 1 year after surgery in the nonsubsidence cases, but there were no lordotic changes in the subsidence group (Figure 5D). In comparison, segmental angle in the subsidence group 1 year after surgery was less lordotic than that in nonsubsidence (1.99 vs 6.26, P = .03) cases (Figure 5D). There was no difference in the change of segmental vertebral body height according to subsidence between before surgery and the first week after surgery (Nonsubsidence: 34.3 to 36.2 mm; Subsidence: 35.3 to 37.3 mm). Clinical results indicated that VAS and NDI scores improved at 1 year after surgery in both groups (P < .001). However, these were not significantly different between the 2 groups at any period (Table 2).
Risk Factors of Subsidence (Table 2)
In simple logistic regression analysis, the estimated odds ratio (OR) and 95% confidence interval (95% CI) were 0.481 (0.254-0.913) per 0.1 increase in Graft/Endplate ratio and 0.211 (0.064-0.691) per 0.1 increase in graft position. Age, sex, body mass index, preoperative C2-C7 angle, operation level, and preoperative radiologic parameters were not significantly associated with subsidence. Multiple logistic regression test, with factors statistically significant in univariate logistic regression test, indicated that anterior graft positioning was only associated with subsidence (OR = 0.280, 95% CI 0.085-0.949; Table 2).
Discussion
ACDF has been established as a standard operation for cervical degenerative disease. Iliac bone autograft for interbody graft showed good clinical outcome in terms of fusion rate, 1 and the most frequently reported complications are donor site complications, including pain at the donor site, hematoma, infection, hip fracture, and cosmetic problems. However, allografts developed to resolve these problems produce severe complications such as pseudarthrosis without plate fixation; therefore, plating is recommended when using allobone graft. Dai and Jiang studied radiologic and clinical results after ACDF with and without a plate and reported higher subsidence in the ACDF group without a plate. 11 Although additional plate fixation is associated with better surgical outcomes, complications such as subsidence, graft dislodgement, and pseudarthrosis have been reported during ACDF with a plate.1,2,12 In particular, subsidence is a complication that reduces intervertebral height and is related to foraminal stenosis. Several risk factors associated with subsidence have been studied, and there are reports that osteoporosis and old age increase the risk. 11 Some studies have demonstrated that subsidence occurs more often when cages are positioned far from the anterior border of the vertebra in ACDF with a stand-alone cage.13,14 When the graft material is located in the center of the endplate, it is likely to penetrate into the vulnerable part of the endplate and cause subsidence.
In this study, graft position in ACDF with allograft and plate surgery was related to subsidence. The overall subsidence rate was 16%, and there was significantly reduced subsidence for allograft cases that were anterior-located (9%) compared with cases that were center-located (42%). These results were concordant with other studies.13,14 In comparison, graft position did not directly influence rate of pseudarthrosis. To define anterior graft position, we measured the sagittal graft position to determine whether the graft was located within 2 mm of the posterior margin of the plate. A previous study measured the distance from the endplate as a continuous variable, 8 while another divided patients by relative implant position, as anterior, middle, or posterior. 7 Ritzel et al reported in an anatomical study that the mean cortical thickness in the cervical spine of controls was 3.29 mm for the ventral shell and 2.40 mm for the dorsal shell. 15 Therefore, if the graft is located within 2 mm of the anterior margin, it could be located within the cortical bone of a cervical vertebral body.
The results of our analysis revealed that a larger contact area is associated with a lower subsidence rate. Several reports suggest that size of the contact area of the graft-end plate interface might play an important role in prevention of graft subsidence.7,13 We hypothesize that this is attributable to balanced weight distribution through the graft to prevent excessive force from concentrating on the adjacent endplate. As a result, a larger graft that fits the size of the endplate could reduce the risk of subsidence. There are no studies with a clear answer on whether the insertion of an oversized graft with overdistraction of the disc space during surgery or the insertion of a graft affects subsidence.13,16 In our study, it is difficult to know whether the graft height was appropriate because endplate preparations and distractions were performed according to the situation in each case during discectomy, but there was no difference in the change of segmental vertebral body height before and the first week after surgery according to subsidence. Implant placement and distance from the anterior margin of the vertebral endplate were more frequently associated with radiographic findings of subsidence. Therefore, to prevent implant subsidence, graft should be placed anteriorly with a size that fits the patient’s vertebral body size. In addition, surgery with anterior plate fixation may reduce fear of graft dislodgement, and it is preferential to avoid placing the graft in the center of the vulnerable area of the endplate.
In our study, as with many reports, subsidence did not affect clinical results. There was no difference in changes of VAS and NDI scores between subsidence and nonsubsidence grafts. The impact of subsidence on clinical patient outcomes has been controversial, and current debates discuss whether implant subsidence affects clinical outcome. Some authors have indicated that graft subsidence has no effect on clinical outcome.17-21 Mende et al report that a group with subsidence had better outcomes than a group without subsidence, 7 and some studies showed worse outcomes in pain or quality of life in groups with subsidence.22-24 In our analysis, segmental angles of nonsubsidence grafts were more lordotic than subsidence grafts at one year after surgery. The Anterior group and nonsubsidence graft cases had a more lordotic angle at 1 week after surgery; even at 1 year later, nonsubsidence grafts had a significantly larger lordotic angle than before the surgery. Following a post hoc power analysis, researchers determined study powers were 0.82 (α error of 0.05) for graft position and subsidence, 0.68 for Graft/Endplate ratio and subsidence. In terms of clinical outcome and subsidence, study powers of 0.05 (for postoperative VAS), 0.30 (for postoperative NDI scores) were measured. In consideration of this analysis, to conclude that subsidence and clinical result are not related, the possibility of type II error exists. It is necessary to study with larger patients group to increase in statistical power.
There were some limitations to this study. The retrospective nature and small patient groups limit the statistical power and application of the results. To prevent overfitting, in multivariate logistic analysis for controlling for potential confounding variables, we could use only 2 factors statistically significant in univariate logistic regression, because of our limited sample size and event rate. Second, we used plates from 2 manufacturers, the shape and characteristics of which were similar; however, but if we had used only one product, the results could have been more reliable. Bone mineral density that affected subsidence in ACDF was reported; however, because we did not regularly measure bone mineral density, we were not able to determine a specific relationship. 25 Although the 2 surgeons in this study performed the surgery in the same way, the 2 different individuals may have affected the consistency of the surgical technique. Therefore, the results of this study need to be further emphasized by prospective, randomized, and large patient group studies with long follow-up periods.
Conclusion
To minimize risk of subsidence, the graft should be positioned on the anterior position of the surgical level endplate at a size appropriate for the endplate. Finally, large-scale patient studies with long follow-up periods are needed to further elucidate the influence of graft location on rate of subsidence.
Footnotes
Ethical Approval: The Institutional Review Board of Gangnam Severance Hospital, Yonsei University College of Medicine, approved this study (No. 2019-0856-001).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Jeong-Yoon Park, MD, PhD  https://orcid.org/0000-0002-3728-7784
https://orcid.org/0000-0002-3728-7784
References
- 1.Shriver MF, Lewis DJ, Kshettry VR, Rosenbaum BP, Benzel EC, Mroz TE. Pseudoarthrosis rates in anterior cervical discectomy and fusion: a meta-analysis. Spine J. 2015;15:2016–2027. [DOI] [PubMed] [Google Scholar]
- 2.Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976). 2005;30:2138–2144. [DOI] [PubMed] [Google Scholar]
- 3.Bishop RC, Moore KA, Hadley MN. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate: a prospective comparative analysis. J Neurosurg. 1996;85:206–210. [DOI] [PubMed] [Google Scholar]
- 4.Martin GJ, Jr, Haid RW, Jr, MacMillan M, Rodts GE, Jr, Berkman R. Anterior cervical discectomy with freeze-dried fibula allograft: overview of 317 cases and literature review. Spine (Phila Pa 1976). 1999;24:852–859. [DOI] [PubMed] [Google Scholar]
- 5.Song KJ, Choi BY. Current concepts of anterior cervical discectomy and fusion: a review of literature. Asian Spine J. 2014;8:531–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghahreman A, Rao PJ, Ferch RD. Dynamic plates in anterior cervical fusion surgery: graft settling and cervical alignment. Spine (Phila Pa 1976). 2009;34:1567–1571. [DOI] [PubMed] [Google Scholar]
- 7.Mende KC, Eicker SO, Weber F. Cage deviation in the subaxial cervical spine in relation to implant position in the sagittal plane. Neurosurg Rev. 2018;41:267–274. [DOI] [PubMed] [Google Scholar]
- 8.Park JY, Choi KY, Moon BJ, Hur H, Jang JW, Lee JK. Subsidence after single-level anterior cervical fusion with a stand-alone cage. J Clin Neurosci. 2016;33:83–88. [DOI] [PubMed] [Google Scholar]
- 9.Brantigan JW, Steffee AD, Lewis ML, Quinn LM, Persenaire JM. Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system: two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine (Phila Pa 1976). 2000;25:1437–1446. [DOI] [PubMed] [Google Scholar]
- 10.Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. [DOI] [PubMed] [Google Scholar]
- 11.Dai LY, Jiang LS. Anterior cervical fusion with interbody cage containing beta-tricalcium phosphate augmented with plate fixation: a prospective randomized study with 2-year follow-up. Eur Spine J. 2008;17:698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vaccaro AR, Falatyn SP, Scuderi GJ, et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11:410–415. [PubMed] [Google Scholar]
- 13.Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 2007;16:1395–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yamagata T, Takami T, Uda T, et al. Outcomes of contemporary use of rectangular titanium stand-alone cages in anterior cervical discectomy and fusion: cage subsidence and cervical alignment. J Clin Neurosci. 2012;19:1673–1678. [DOI] [PubMed] [Google Scholar]
- 15.Ritzel H, Amling M, Pösl M, Hahn M, Delling G. The thickness of human vertebral cortical bone and its changes in aging and osteoporosis: a histomorphometric analysis of the complete spinal column from thirty-seven autopsy specimens. J Bone Miner Res. 1997;12:89–95. [DOI] [PubMed] [Google Scholar]
- 16.Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 2011;3:16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haden N, Latimer M, Seeley H, Laing R. Loss of inter-vertebral disc height after anterior cervical discectomy. Br J Neurosurg. 2005;19:469–474. [DOI] [PubMed] [Google Scholar]
- 18.Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. 2006;58:502–508. [DOI] [PubMed] [Google Scholar]
- 19.Brenke C, Dostal M, Scharf J, Weiß C, Schmieder K, Barth M. Influence of cervical bone mineral density on cage subsidence in patients following stand-alone anterior cervical discectomy and fusion. Eur Spine J. 2015;24:2832–2840. [DOI] [PubMed] [Google Scholar]
- 20.Cho DY, Lee WY, Sheu PC. Treatment of multilevel cervical fusion with cages. Surg Neurol. 2004;62:378–385. [DOI] [PubMed] [Google Scholar]
- 21.Klingler JH, Krüger MT, Sircar R, et al. PEEK cages versus PMMA spacers in anterior cervical discectomy: comparison of fusion, subsidence, sagittal alignment, and clinical outcome with a minimum 1-year follow-up. ScientificWorldJournal. 2014;2014:398396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee YS, Kim YB, Park SW. Risk factors for postoperative subsidence of single-level anterior cervical discectomy and fusion: the significance of the preoperative cervical alignment. Spine (Phila Pa 1976). 2014;39:1280–1287. [DOI] [PubMed] [Google Scholar]
- 23.Kast E, Derakhshani S, Bothmann M, Oberle J.Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev. 2009;32:207–214. [DOI] [PubMed] [Google Scholar]
- 24.Kim SC, Kang SW, Kim SH, Cho KH, Kim SH. Clinical and radiological outcomes of anterior cervical interbody fusion using hydroxyapatite spacer. J Korean Neurosurg Soc. 2009;46:300–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lim TH, Kwon H, Jeon CH, et al. Effect of endplate conditions and bone mineral density on the compressive strength of the graft-endplate interface in anterior cervical spine fusion. Spine (Phila Pa 1976). 2001;26:951–956. [DOI] [PubMed] [Google Scholar]