Abstract
Study Design:
Retrospective cohort study.
Objective:
To investigate correlations between preoperative supine imaging and postoperative alignment.
Methods:
A retrospective review was conducted of a single-institution database of patients with adult spinal deformity (ASD). Patients were stratified by fusion location in the lumbar or thoracic spine. Outcomes of interest were postoperative lumbar lordosis (LL) and thoracic kyphosis (TK). Sagittal alignment parameters were compared and correlation analyses were performed. Multilinear stepwise regression was conducted to identify independent predictors of postoperative LL or TK. Regression analyses were repeated within the lumbar and thoracic fusion cohorts.
Results:
A total of 99 patients were included (mean age 63.2 years, 83.1% female, mean body mass index 27.3 kg/m2). Scoliosis Research Society classification demonstrated moderate to severe sagittal and/or coronal deformity (pelvic tile modifier, 18.2% ++; sagittal vertical axis, 27.3% ++, pelvic incidence minus lumbar lordosis mismatch, 29.3% ++, SRS type, 29.3% N type curve and 68.7% L or D type curve). A total of 73 patients (73.7%) underwent lumbar fusion and 50 (50.5%) underwent thoracic fusion. Correlation analyses demonstrated a significant association between pre- and postoperative LL and TK. Multilinear regression demonstrated that LL supine and pelvic incidence were significant predictors of postoperative LL (r2 = 0.568, P < .001). LL supine, TK supine, and age were significant predictors of postoperative TK (r2 = 0.490, P < .001).
Conclusion:
Preoperative supine films are superior to standing in predicting postoperative alignment at 1-year follow-up. Anticipation of undesired alignment changes through supine imaging may be useful in mitigating the risk of iatrogenic malalignment.
Keywords: thoracic fusion, lumbar fusion, supine imaging, postoperative alignment
Introduction
Adult spinal deformity (ASD) is a disabling condition with reported prevalence ranging from 13% to 32%1,2 in the general population and reaching up to 60% in the elderly population. 3 With an increase in life expectancy, the prevalence of ASD is only expected to grow. 4 A recent National Institutes of Health–funded randomized controlled trial demonstrated that surgery can improve outcomes in patients with ASD compared with nonoperative treatment. 5 However, surgical intervention for ASD is fraught with complications, reoperations, and high costs, emphasizing the importance of optimizing outcomes after the index operation.5-8
Over the past decade, ASD-related research has established postoperative surgical alignment goals that maximize the chance of obtaining optimal outcomes while mitigating the risk of mechanical complications.9-14 However, consistently achieving the desired postoperative alignment, especially in long-term follow-up, has proven difficult.15-18 One possible explanation lies in the discrepancy between the patient position as seen on the radiographs used for preoperative planning (ie, the standing position) and in the operative room (ie, prone position). Despite investigations demonstrating the utility of positional radiographs in degenerative pathologies or adolescent deformity, there is limited research on their use in adult spinal deformity.19-25 The possibility that positional radiographs (eg, sitting or recumbent) can predict postoperative outcomes has only recently become a burgeoning area of ASD research.19,26,27
Therefore, the objective of our study was to investigate potential correlations between preoperative supine imaging and postoperative alignment, focusing specifically on factors within the surgeon’s control intraoperatively (ie, lumbar and thoracic curvatures). We hypothesized that supine imaging would be superior to standing imaging as a predictor for postoperative alignment.
Materials and Methods
Patient Sample
A retrospective analysis was performed of surgically treated ASD patients from a single-center, single surgeon database (2014-2018) with a minimum of 1-year follow-up. Charts reviews were conducted after approval by the institutional review board. Inclusion criteria were adult patients (age >18 years) with spinal deformity, defined as coronal Cobb angle greater than 20°, C7 sagittal vertical axis (SVA) > 50 mm, pelvic tilt (PT) >25°, or pelvic incidence minus lumbar lordosis mismatch (PI-LL) >10°. Given that the purpose of the study was to investigate the relationship of supine alignment with postoperative alignment, only patients with full-length lateral radiographs in the standing and supine positions were included. Exclusion criteria were deformities secondary to trauma, cancer, or a neuromuscular condition. All patients involved provided written informed consent to be part of this study.
Data Collection
Demographic parameters such as age, sex, gender, and body mass index (BMI) were collected from the electronic medical record. Full length lateral radiographs were collected preoperatively in standing and supine position, and postoperatively in standing position only (Figure 1). For supine radiographs, the patient was asked to lay on the table with their shoulders with their fingertips touching their clavicles (identical to the standing position films). Radiographs were analyzed by a researcher outside of the primary clinical team using a validated and dedicated software (Spineview, ENSAM ParisTech, Paris) for the following parameters: PI, PT, PI-LL (LL, L1-S1), thoracic kyphosis (TK, T4-T12), T1-pelvic angle (TPA), SVA (standing radiographs only), coronal C7 plumb line (C7PL, standing radiographs only), and maximum coronal Cobb angle (MaxCobb). 10 The measurements were verified by a second, more experienced researcher.
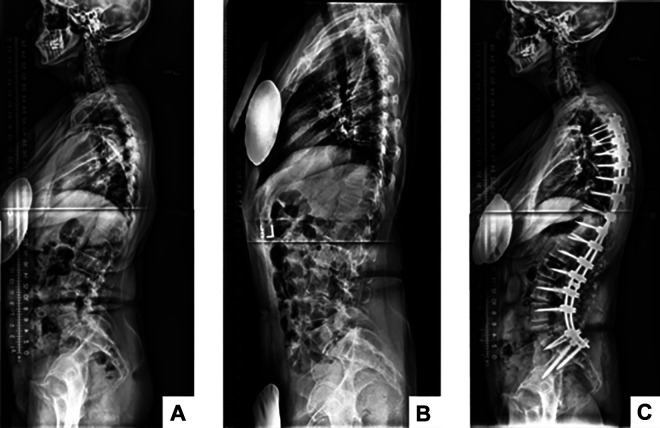
Figure 1.
Example of supine radiographs. Preoperative standing (A), preoperative supine (B), postoperative standing (C).
Statistical Analyses
Patients were characterized by the type of fusion they underwent. Lumbar (or lumbothoracic) fusion was characterized as a fused spine spanning at least all the lumbar vertebra (L1-S1) with no limit to upper instrumented vertebra. Thoracic fusion was characterized by a fusion of the entire thoracic spine (T4-T12) with the majority of the lumbar spine left untouched. The incidence of 3-column osteotomies (3COs) was also recorded. Schwab–Scoliosis Research Society (Schwab-SRS) modifiers were applied to each patient. 9
Pre- to postoperative radiographic parameters were compared using paired t tests. Postoperative PI-LL mismatch was compared between patients who underwent a 3CO and those who did not. Postoperative LL and TK were chosen as outcomes of interest, given that intraoperative modifications to these sagittal alignment measures mechanistically drive overall correction of global alignment. Univariate associations between demographics and preoperative radiographic parameters and postoperative parameters were explored using Pearson correlations. A multilinear stepwise regression was performed to control for confounding and identify independent correlations with postoperative alignment at 1 year. Finally, the cohort was stratified by type of fusion and the regression was repeated. Type I error rate was set as P < .05. Statistical analysis was conducted using SPSS Version 22.0 (IBM).
Results
Patient Sample
A total of 101 patients met inclusion criteria. Supine radiographs were available for 99 of these patients. The cohort was majority female (83.1%) and middle aged (mean 57 ± 11.6 years), with mean BMI of 27.3 kg/m2. Mean follow-up period was 21.0 ± 9.8 months. When sagittal deformity was classified using preoperative Schwab-SRS modifiers, 18.2% of the cohort had a ++ PT modifier, 27.3% had a ++ SVA modifier, and 29.3% had a ++ PI-LL modifier. In terms of coronal SRS type, 29.3% of the cohort had an N type curve, while 68.7% had an L or D type curve. Approximately one-fifth (20.6%) of patients underwent a 3CO.
In our cohort 73.7% of patients underwent a lumbar (or lumbothoracic) fusion and 50% underwent a thoracic fusion. The pre-to-post comparison of standing alignment demonstrated a significant change in alignment (Table 1) with an average decrease of PI-LL, PT, SVA, TPA, and an average increase in T4-T12 (all Ps < .001). There were no significant differences in postoperative PI-LL between patients who received or did not receive a 3CO (P = .175).
Table 1.
Radiographic Parameters of the Patient Sample Before and After Surgery Using Standing and Supine Imaging.
| Pre-standing | Pre-supine | Post-standing | Repeated measuresa | ||||
|---|---|---|---|---|---|---|---|
| Overall | Pre-supine | Pre-post | Supine-post | ||||
| PI, deg | 52.6 ± 13.6 | 52.4 ± 13.7 | 52.3 ± 13 | 0.458 | 1.000 | 0.673 | 1.000 |
| PT, deg | 21 ± 11.5 | — | 15.9 ± 10.1 | <.001 b | — | <.001 b | — |
| PI-LL, deg | 11.6 ± 20.1 | 5.5 ± 16.4 | −2.7 ± 14 | <.001 | <.001 | <.001 | <.001 |
| LL, deg | 40.9 ± 22.8 | 46.9 ± 18.7 | 55 ± 14.4 | <.001 | <.001 | <.001 | <.001 |
| TK, deg | −35.5 ± 19.7 | −26.7 ± 16.8 | −41.6 ± 13.4 | <.001 | <.001 | .001 | <.001 |
| TPA, deg | 19.7 ± 13.8 | 12 ± 12 | 11.8 ± 10.2 | <.001 | <.001 | <.001 | 1.000 |
| SVA, mm | 58 ± 80 | — | 14 ± 50 | <.001 b | — | <.001 b | — |
| C7PL, mm | 35 ± 33 | — | 24 ± 20 | .003 b | — | .003 b | — |
| MaxCobb, deg | 46.7 ± 23.1 | 38.1 ± 21.2 | 23 ± 15.4 | <.001 | <.001 | <.001 | <.001 |
Abbreviations: PI, pelvic incidence; PT, pelvic tilt; PI-LL, pelvic incidence–lumbar lordosis mismatch; LL, lumbar lordosis; TK, thoracic kyphosis; TPA, T1 pelvic angle; SVA, sagittal vertical axis; C7PL, C7 plumb line; MaxCobb, maximum Cobb angle.
a Boldfaced values indicate statistical significance (P < .05).
b Comparison conducted with paired t-test due to lack of supine measurements.
Univariate Correlations With Postoperative Alignment
On univariate analysis, several factors were associated with postoperative LL and TK (Table 2). Specifically, postoperative LL significantly correlated with preoperative LL in supine (r = 0.668, P < .001) and standing positions (r = 0.608, P < .001), as well as with PI (r = 0.577, P < .001). Similarly, postoperative TK significantly correlated with preoperative TK in standing (r = 0.549, P < .001) and supine positions (r = 0.488, P < .001) along with age (r = 0.280, P < .005).
Table 2.
Univariate Correlation Between Preoperative Radiographic Parameters, Demographics, and Postoperative LL and TK.a
| LL Postoperative | TK Postoperative | |||||||
|---|---|---|---|---|---|---|---|---|
| All patients | Lumbar fused | All patients | Thoracic fused | |||||
| r | P | r | P | r | P | r | P | |
| LL preoperative supine | 0.668 | <.001 | 0.716 | <.001 | −0.320 | .001 | −0.313 | .027 |
| LL preoperative standing | 0.608 | <.001 | 0.691 | <.001 | −0.287 | .004 | NS | .389 |
| TK preoperative supine | −0.208 | <.001 | NS | .154 | 0.488 | <.001 | 0.530 | <.001 |
| TK preoperative standing | −0.225 | <.001 | NS | .122 | 0.549 | <.001 | 0.454 | .001 |
| Pelvic incidence | 0.557 | <.001 | 0.553 | <.001 | NS | .148 | NS | .065 |
| Patient age | NS | .545 | NS | .169 | −0.280 | .005 | −0.468 | .001 |
Abbreviations: LL, lumbar lordosis; TK, thoracic kyphosis; NS, nonsignificant.
a Boldfaced values indicate statistical significance (P < .05).
Independent Predictors of Postoperative Alignment
When the preoperative parameters were entered into multilinear regression analysis, only preoperative supine LL and PI emerged as independent correlates with postoperative LL (r2 = 0.533). Similarly, preoperative supine LL, age, and preoperative standing TK were retained as independent correlates of postoperative TK (r2 = 0.429).
The analysis was repeated after stratification of the sample by type of fusion (Table 3). In the lumbar fusion patients, preoperative supine LL and PI remained the only independent correlates of postoperative LL (r2 = 0.514). Results were similar for the thoracic fusion patients, showing that preoperative supine LL, preoperative supine TK, and age were independently associated with postoperative TK.
Table 3.
Correlation Between Pre- and Postoperative Lumbar Lordosis and Thoracic Kyphosis With Substratification by Fusion Group.a
| Parameters | LL postoperative | TK postoperative | ||||||
|---|---|---|---|---|---|---|---|---|
| All patients | Lumbar fused | All patients | Thoracic fused | |||||
| β | P | β | P | β | P | β | P | |
| Constant | 29.291 | <.001 | 19.791 | <.001 | −11.248 | .016 | −11.261 | .041 |
| LL preoperative supine | 0.410 | .000 | 0.421 | <.001 | −0.164 | .011 | −0.220 | .006 |
| LL preoperative standing | NS | .221 | NS | .256 | NS | .200 | NS | .190 |
| TK preoperative supine | NS | .830 | NS | .912 | NS | .293 | 0.162 | .043 |
| TK preoperative standing | NS | .808 | NS | .909 | 0.312 | <.001 | NS | .252 |
| Pelvic incidence | 0.247 | .007 | 0.292 | .009 | NS | .680 | NS | .697 |
| Patient age | −0.118 | .030 | NS | .979 | −0.209 | <.001 | −0.273 | <.001 |
| Model r2 | 0.533 | 0.514 | 0.429 | 0.490 | ||||
Abbreviations: LL, lumbar lordosis; TK, thoracic kyphosis; NS, nonsignificant.
a Boldfaced values indicate statistical significance.
Discussion
Our investigation found that ASD patients’ alignment changed from the standing to supine position, with an overall increase in LL and decrease in TK leading to improved PI-LL mismatch (<10°) and normalized TPA (<14°). 10 We focused our outcomes of interest on postoperative LL and TK as these 2 parameters are directly controlled by the surgeon during the fusion. Similarly, we concentrated on these 2 outcomes of interest for the lumbar and thoracic fusion cohorts to ensure that we were analyzing patients who had underwent intraoperative correction of their LL (ie, lumbar fusion patients) or TK (ie, thoracic fusion patients). In these respective subgroups, univariate analyses demonstrated that both preoperative standing and supine LL and TK correlated with postoperative LL and TK. However, when these parameters were entered into multilinear regression models, only supine LL and TK were retained as independent correlates of postoperative LL and TK, respectively.
While we could not assess preoperative planning or intraoperative decision making, we hypothesize that there is a clinically useful relationship between supine imaging and the techniques needed for correction. In every case, supine imaging was obtained for preoperative planning purposes, specifically to estimate whether an osteotomy may be needed to achieve alignment goals. Our findings lead us to hypothesize that the supine film likely correlated with the intraoperative alignment of the spine after relaxation and positioning. 25 For flexible, mild-moderate deformity this intraoperative alignment was likely very close to the desired outcome. On the other hand, when supine films did not show an acceptable regional alignment, then extra effort was exerted through osteotomies. This second point is supported by the fact that similar corrections were obtained with or without a 3CO (ie, patients who corrected through intraoperative positioning did not require a 3CO while those who did not correct underwent a 3CO). In other words, supine imaging correlated with the intraoperative decision making, which correlated with final alignment goals. This leads us to conclude that supine imaging is a useful preoperative planning tool that can predict the correction obtained by intraoperative positioning (ie, the flexibility of the spine) and subsequently, the need for further corrective techniques.
We are not the first investigators to note the utility of supine imaging in preoperative planning for lumbar deformity correction. In severe sagittal deformity (SVA > 10 cm), a 33% change in LL between supine to standing has been suggested as a “stiffness threshold” for requiring a 3CO in the lumbar spine. 19 In an analysis of standing, supine, and intraoperative radiographs (taken before the surgery began), the same investigators demonstrated that prone positioning on a Jackson table significantly increased LL in patients with decreased preoperative lordosis (eg, degenerative flatback deformity). 25 Furthermore, they showed that the intraoperative positional lordosis was near equivalent to that of a supine radiograph. We were able to show that supine LL correlated with postoperative LL in patients who underwent lumbar fusions, seeming to indicate the correction obtained by positioning may be the most important predictor of the overall correction maintained at 1 year. Interestingly, Harimaya et al 25 also demonstrated that the positional change in lordosis occurred primarily through the upper lumbar segments (L1-L4), with less change from L4-S1. In the context of our findings, this is a very important observation, as the distribution of lordosis is increasingly recognized as a factor associated with outcomes.28-30 Other than supine LL, our model also found that PI was an independent predictor of lumbar lordosis. Given that the cases in this study were performed within the past 5 years, this relationship is likely attributable to the clinical application of the past decade of ASD research, which has repeatedly demonstrated the intimate associations between pelvic parameters and LL.14,29
Apart from the utility in planning lumbar surgeries, our study provides support for the use of supine imaging in thoracic deformity surgery as well. The correlations between supine thoracic kyphosis and 1-year postoperative TK suggest that intraoperative positioning likely plays a key role in how the thoracic spine is fused. Our research joins a growing body of literature suggesting that the position of the patient influences the sagittal alignment of the thoracic spine,26,31 despite suggestions by previous authors that the sagittal thoracic spine is not subject to positional changes due to the stiffness conferred by the rib cage. 32 For example, several authors have advocated for the use of supine imaging to evaluate flexibility of the thoracic spine in Scheuermann’s disease.23,24,33,34 In the setting of adult thoracolumbar deformity, analyses of thoracic spine flexibility using sitting or supine imaging have demonstrated the flexibility of the thoracic spine can predict changes in the unfused segments after thoracolumbar fusions (T10-pelvis).26,27 Our analysis shows that supine imaging is also useful in predicting postoperative alignment in the fused segments of the thoracic spine as the degree of TK obtained in supine imaging predicted TK in the fused segments for the thoracic fusion cohort. This is particularly important when considering patients who experience a flattening of the TK with supine/prone positioning. These patients may be particularly predisposed to fusion in a flatter-than-ideal position, a documented risk factor for proximal junctional kyphosis.35,36 Further investigations incorporating all 3 modes of imaging (supine, standing, sitting) may not only provide a more complete model for predicting postoperative alignment of the fused and unfused segments but also improve our ability to determine the risk of mechanical complications. 27
Other factors associated with postoperative TK included age and supine LL. The reasons behind these associations are identical to those explaining the relationship between supine LL and PI; namely, the past decade of ASD research has emphasized the importance of respecting age-related normative values of thoracic kyphosis in spinal deformity surgery.10,13,37,38 Multiple series of asymptomatic adult patients have demonstrated increased TK with age.37,38 This has led researchers to propose that elderly patients should be fused with more thoracic kyphosis compared with their younger counterparts, a strategy recommended as a method to reduce mechanical complications.13,28 The relationship between postoperative TK and supine LL is similar—research has shown that reciprocity between curves is necessary to restore the spine’s anatomic alignment. 39 Clinically, severe mismatch between TK and LL has been associated with poor outcomes. 40 Therefore, we believe that the associations between postoperative TK, age, and preoperative supine LL are products of advancements in ASD research.
This study is not without limitations. Most notably, the retrospective design precluded the capture of any information regarding the preoperative planning or intraoperative decision-making. We cannot assess whether the alignment achieved intraoperatively was in line with the goals of the surgery. Regardless, we still believe that the relationship of supine alignment with long-term (1 year) postoperative alignment is significant, as it allows the surgeon to preoperatively assess the corrections they will need to make once the patient is on the table. Furthermore, if supine imaging shows an undesired change (eg, a decrease in TK when a large LL correction is planned), this allows the surgeon to anticipate this positional change and plan accordingly. Second, while we assume that the intraoperative position was similar to supine films (as has been previously reported by Harimaya et al 25 ), we did not take precorrection intraoperative films. Third, these findings represent a single-center experience, with surgeons who exclusively employ all-posterior, single stage surgeries. For these reasons, the results may not be externally valid to centers that use different techniques. Multicenter studies will be necessary, provided care is taken that the supine imaging is performed similarly among centers (ie, passive supine imaging, no forced hyperextension or patient-directed activity). Fourth, we did not stratify data by the presence of a 3CO. We attempted to mitigate this limitation by demonstrating that patients who underwent a 3CO had the same degree of postoperative correction as those who did not. Regardless, the relationship between supine and postop LL may have been different if only patients who had underwent a 3CO were analyzed. Although our analysis suggests that the degree of LL achieved through positioning is likely the most important determinant of long-term alignment, a larger series of patients with 3CO will be needed to differentiate the amount of correction achieved by a 3CO compared with the amount achieved from positioning alone. Fifth, we only included 1-year outcomes—a 2-year analysis may have shown further loss of alignment. However, we hypothesize that any loss of alignment past one year would likely be secondary to changes in the unfused segments. This hypothesis is supported by the fact that our correlations were similar in patients with fused thoracic or lumbar spines (Table 2).
In conclusion, our study provides evidence that supine LL and TK are superior predictors of long-term postoperative LL and TK compared to measurements made on standard preoperative imaging. Supine imaging is a useful preoperative planning tool as it allows surgeons to anticipate alignment changes that will occur once the patient is positioned for surgery. For mild-moderate deformity, relaxation of the spine with intraoperative positioning may get alignment close to the desired postoperative goals. On the other hand, if regional alignment remains unacceptable on supine films, then the need for an osteotomy should be anticipated. Furthermore, supine imaging allows surgeons to identify which segments of the spine are most flexible, as distribution of lordosis is increasingly recognized as an important influencer of mechanical outcomes. 30 The anticipation of undesired alignment changes (eg, reduced thoracic kyphosis) through the utilization of supine imaging is especially useful in ensuring surgeons mitigate the risk of iatrogenic malalignment. A multicenter study will be needed to provide external validation for our results, as surgical techniques vary. Future investigations should also consider the incorporation of various radiographic positions (sitting, standing, supine) in order to formulate the most complete predictive model of postoperative radiographic outcomes.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Francis Lovecchio, MD  https://orcid.org/0000-0001-5236-1420
https://orcid.org/0000-0001-5236-1420
Renaud Lafage, MS  https://orcid.org/0000-0002-4820-1835
https://orcid.org/0000-0002-4820-1835
Bryan Ang, BS  https://orcid.org/0000-0002-4174-997X
https://orcid.org/0000-0002-4174-997X
Han Jo Kim, MD  https://orcid.org/0000-0003-2170-3592
https://orcid.org/0000-0003-2170-3592
References
- 1.Jimbo S, Kobayashi T, Aono K, Atsuta Y, Matsuno J. Epidemiology of degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2012;37:1763–1770. [DOI] [PubMed] [Google Scholar]
- 2.Robin GC, Span Y, Steinberg R, Makin M, Menczel J. Scoliosis in the elderly: a follow-up study. Spine (Phila Pa 1976). 1982;7:355–359. [DOI] [PubMed] [Google Scholar]
- 3.Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30:1082–1085. [DOI] [PubMed] [Google Scholar]
- 4.Passias PG, Jalai CM, Worley N, et al. Adult spinal deformity: national trends in the presentation, treatment, and perioperative outcomes from 2003 to 2010. Spine Deform. 2017;5:342–350. [DOI] [PubMed] [Google Scholar]
- 5.Kelly MP, Lurie JD, Yanik EL, et al. Operative versus nonoperative treatment for adult symptomatic lumbar scoliosis. J Bone Joint Surg Am. 2019;101:338–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raman T, Nayar SK, Liu S, Skolasky RL, Kebaish KM. Cost-effectiveness of primary and revision surgery for adult spinal deformity. Spine (Phila Pa 1976). 2018;43:791–797. [DOI] [PubMed] [Google Scholar]
- 7.Pitter FT, Lindberg-Larsen M, Pedersen AB, Dahl B, Gehrchen M. Readmissions, length of stay, and mortality after primary surgery for adult spinal deformity: a 10-year Danish nationwide cohort study. Spine (Phila Pa 1976). 2019;44:E107–E116. [DOI] [PubMed] [Google Scholar]
- 8.Hamilton DK, Kanter AS, Bolinger BD, et al. Reoperation rates in minimally invasive, hybrid and open surgical treatment for adult spinal deformity with minimum 2-year follow-up. Eur Spine J. 2016;25:2605–2611. [DOI] [PubMed] [Google Scholar]
- 9.Terran J, Schwab FJ, Shaffrey CI, et al. The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery. 2013;73:559–568. [DOI] [PubMed] [Google Scholar]
- 10.Lafage R, Schwab F, Challier V, et al. Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976). 2016;41:62–68. [DOI] [PubMed] [Google Scholar]
- 11.Scheer JK, Lafage R, Schwab FJ, et al. Under-correction of sagittal deformities based on age-adjusted alignment thresholds leads to worse HRQOL while over-correction provides no additional benefit. Spine (Phila Pa 1976). 2018;43:388–393. doi:10.1097/BRS.0000000000002435 [DOI] [PubMed] [Google Scholar]
- 12.Rothenfluh DA, Mueller DA, Rothenfluh E, Min K. Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J. 2014;24:1251–1258. [DOI] [PubMed] [Google Scholar]
- 13.Lafage R, Schwab F, Glassman S, et al. Age-adjusted alignment goals have the potential to reduce PJK. Spine (Phila Pa 1976). 2017;42:1275–1282. [DOI] [PubMed] [Google Scholar]
- 14.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34:E599–E606. [DOI] [PubMed] [Google Scholar]
- 15.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35:2224–2231. [DOI] [PubMed] [Google Scholar]
- 16.Bach K, Ahmadian A, Deukmedjian A, Uribe JS. Minimally invasive surgical techniques in adult degenerative spinal deformity: a systematic review. Clin Orthop Relat Res. 2014;472:1749–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho KJ, Suk S, Il, Park SR, et al. Risk factors of sagittal decompensation after long posterior instrumentation and fusion for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2010;35:1595–1601. doi:10.1097/BRS.0b013e3181bdad89 [DOI] [PubMed] [Google Scholar]
- 18.Bridwell KH, Baldus C, Berven S, et al. Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine (Phila Pa 1976). 2010;35:1849–1854. [DOI] [PubMed] [Google Scholar]
- 19.Karikari IO, Lenke LG, Bridwell KH, et al. Key role of preoperative recumbent films in the treatment of severe sagittal malalignment. Spine Deform. 2018;6:568–575. [DOI] [PubMed] [Google Scholar]
- 20.Chen X, Zhou QS, Xu L, et al. Does kyphotic configuration on upright lateral radiograph correlate with instability in patients with degenerative lumbar spondylolisthesis? Clin Neurol Neurosurg. 2018;173:96–100. doi:10.1016/j.clineuro.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 21.Chan V, Marro A, Rempel J, Nataraj A. Determination of dynamic instability in lumbar spondylolisthesis using flexion and extension standing radiographs versus neutral standing radiograph and supine MRI. J Neurosurg Spine. 2019;31:155–297. [DOI] [PubMed] [Google Scholar]
- 22.Tarpada SP, Cho W, Chen F, Amorosa LF. Utility of supine lateral radiographs for assessment of lumbar segmental instability in degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976). 2018;43:1275–1280. [DOI] [PubMed] [Google Scholar]
- 23.Kaiser R, Behrbalk E, Walsh M, Waldauf P, Romera ABP, Mehdian H. Can MRI predict flexibility in Scheuermann kyphosis patients? Clin Spine Surg. 2017;30:E938–E941. [DOI] [PubMed] [Google Scholar]
- 24.Lovecchio F, Steinhaus M, Kim HJ. Scheuermann’s kyphosis. In: Baaj A, Kakarla K, Kim HJ, eds. Surgery of the Thoracic Spine: Principles and Techniques. Thieme; 2019:74–81. [Google Scholar]
- 25.Harimaya K, Lenke LG, Mishiro T, Bridwell KH, Koester LA, Sides BA. Increasing lumbar lordosis of adult spinal deformity patients via intraoperative prone positioning. Spine (Phila Pa 1976). 2009;34:2406–2412. [DOI] [PubMed] [Google Scholar]
- 26.Janjua MB, Tishelman JC, Vasquez-Montes D, et al. The value of sitting radiographs: analysis of spine flexibility and its utility in preoperative planning for adult spinal deformity surgery. J Neurosurg Spine. 2018;29:414–421. [DOI] [PubMed] [Google Scholar]
- 27.Decker S, Mayer M, Hempfing A, et al. Flexibility of thoracic kyphosis affects postoperative sagittal alignment in adult patients with spinal deformity. Eur Spine J. 2020;29:813–820. doi:10.1007/s00586-019-06245-1 [DOI] [PubMed] [Google Scholar]
- 28.Lafage R, Obeid I, Liabaud B, et al. Location of correction within the lumbar spine impacts acute adjacent-segment kyphosis. J Neurosurg Spine. 2018;30:69–77. [DOI] [PubMed] [Google Scholar]
- 29.Pesenti S, Lafage R, Stein D, et al. The amount of proximal lumbar lordosis is related to pelvic incidence. Clin Orthop Relat Res. 2018;476:1603–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yilgor C, Sogunmez N, Boissiere L, et al. Global Alignment and Proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am. 2017;99:1661–1672. [DOI] [PubMed] [Google Scholar]
- 31.Pierce KE, Horn SR, Jain D, et al. The impact of adult thoracolumbar spinal deformities on standing to sitting regional and segmental reciprocal alignment. Int J Spine Surg. 2019;13:308–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bernstein P, Hentschel S, Platzek I, et al. The assessment of the postoperative spinal alignment: MRI adds up on accuracy. Eur Spine J. 2012;21:733–738. doi:10.1007/s00586-011-2115-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee SS, Lenke LG, Kuklo TR, et al. Comparison of Scheuermann kyphosis correction by posterior-only thoracic pedicle screw fixation versus combined anterior/posterior fusion. Spine (Phila Pa 1976). 2006;31:2316–2321. [DOI] [PubMed] [Google Scholar]
- 34.Johnston CE, 2nd, Elerson E, Dagher G. Correction of adolescent hyperkyphosis with posterior-only threaded rod compression instrumentation: is anterior spinal fusion still necessary? Spine (Phila Pa 1976). 2005;30:1528–1534. [DOI] [PubMed] [Google Scholar]
- 35.Maruo K, Ha Y, Inoue S, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976). 2013;38:E1469–E1476. [DOI] [PubMed] [Google Scholar]
- 36.Kim YJ, Lenke LG, Bridwell KH, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976). 2007;32:2731–2738. [DOI] [PubMed] [Google Scholar]
- 37.Hu Z, Man GCW, Yeung KH, et al. Age-and gender-related normative value of whole-body sagittal alignment based on 584 asymptomatic Chinese adult population from age 20 to 89. Spine (Phila Pa 1976). 2020;45:79–87. doi:10.1097/BRS.0000000000003187 [DOI] [PubMed] [Google Scholar]
- 38.Bassani T, Galbusera F, Luca A, Lovi A, Gallazzi A, Brayda-Bruno M. Physiological variations in the sagittal spine alignment in an asymptomatic elderly population. Spine J. 2019;19:1840–1849. [DOI] [PubMed] [Google Scholar]
- 39.Roussouly P, Pinheiro-Franco JL. Sagittal parameters of the spine: biomechanical approach. Eur Spine J. 2011;20(suppl 5):578–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang C, Yang M, Wei X, et al. Lumbar lordosis minus thoracic kyphosis: a novel regional predictor for sagittal balance in elderly populations. Spine (Phila Pa 1976). 2016;41:399–403. [DOI] [PubMed] [Google Scholar]