Abstract
Study Design:
Scoping review.
Objective:
Regarding that inappropriate medical care approaches, absence of rehabilitation services, and existing barriers in physical, social, and policy environments lead to poor outcomes in individuals with spinal cord injury (SCI) and provision for appropriate interventions and care must be created by health policymakers, we conducted this scoping review to investigate how policymakers can be persuaded to set new plans for individuals with SCI.
Methods:
This review was performed according to Arksey and O’Malley’s framework. PubMed was searched in February2019 without language limitation. We looked for other potential gray literature sources and some professional websites. References sections of selected articles were also scanned for other relevant literature.
Results:
We included literature that met inclusion criteria to answer our research question. The literature was divided into 3 categories. The first category included economic impact of SCI. The second category included the role of research and developing research strategy. The third category included effective interaction and communication with policymakers.
Conclusion:
It is essential to consider multiple factors for influencing policymakers’ decisions. These factors include knowing how to communicate with policymakers and presenting constructive ideas, providing a source of valid, reliable, and consistent data, considering the role of patients’ advocacy groups and Non-Governmental Organizations (NGOs), and presentation of the importance of early intervention in reducing healthcare system costs. Ultimately, the goal is to have a comprehensive and flexible plan for influencing policymakers.
Keywords: spinal cord injury, policy makers, legislation, health care system, support
Introduction
Spinal Cord Injury (SCI) is a medically complex condition that is associated with life-threatening secondary complications and socioeconomic consequences. SCI is an important public health issue due to its costs for both patients and the health care system. Many of the consequences of SCI are due to inadequate medical care and rehabilitation services, as well as barriers in physical, social, and policy environments. Inappropriate policy can have negative effects on patients’ neurological outcomes and raise personal and economic costs for the patients and the healthcare system. Appropriate interventions and care in prehospital, acute, and post-acute phases can reduce the risk of secondary complications and improve quality of life through maximizing function, independence, overall wellbeing, and community integration. We therefore must convince policymakers to create new plans for appropriate intervention and care policies for individuals with SCI.1-3
Comparison between countries shows that some have more supportive laws for individuals with SCI compared with the others. For instance, access to medical services, social facilities, and other needs have been considered in legislation to help decrease secondary complications and increase quality of life in individuals with SCI. Lack of knowledge, financial resources, job opportunities, facilities and accessibility, social support, and social acceptance have been reported by people with SCI as barriers to adaptation. The wide range of potential barriers shows that new SCI legislation is required. For this reason, the process of policymaking and legislation must be modified.4-6
To improve health system services and reduce health deficiencies, policymakers need to find the best solutions for health problems and the best ways to elicit the desired changes in health systems. Policymakers must understand the beliefs and behaviors related to most of the target population to create appropriate laws. Therefore, we must investigate how to provide a data source that reflects the needs of individuals with SCI to convince policymakers to legislate more supportive laws. While the incidence of SCI is relatively low, the physical, medical, psychological, social, and financial consequences of such injuries are complicated and potentially devastating for individuals with SCI as well as their families. Thus, policymakers are faced with a health system dilemma: a small group of people with a diagnosis that demands specialized care over a long period of time.6-8 The aim of this study is to answer how policymakers can be persuaded to accept specific support for people with SCI.
Methods
To answer how to encourage policymakers to support individuals with SCI, we conducted a scoping review to show how to influence policymakers about individuals with SCI. Because the study is a Scoping Review, it includes any type of studies. 9 This review was performed according to Arksey and O’Malley’s framework. 10 We followed the below steps:
1. Identifying the research question
In the first step, the research question was identified by collaboration with stockholders, as follows:
How can we persuade the policymakers to accept specific support for individuals with SCI?
2. Identifying relevant studies
A search strategy was designed by a health information specialist. PubMed was searched in February 2019 for articles from 1990 without language limitation. The database was searched using the search terms:”federal”, “national”, “government”, “spinal cord injury”, “funding”, plan”,” policy”, “strategy”, “action plan”. Additionally, we looked for potential gray literature sources, such as professional websites, to hand search for related studies. References sections of selected articles were also scanned for other relevant articles. Duplicates were removed. The abstracts of articles were sent to 4 reviewers who were separated into 2 independent groups.
3. Study selection
Two independent groups, each consisting of two reviewers, screened search results according to their titles and abstracts to identify eligible studies. Any discrepancy in the groups’ results was resolved through discussion sessions. In the next step, the reviewers reviewed the full text of articles based on the inclusion criteria that are shown in Table 1. Any disagreement regarding eligibility of studies was resolved through discussion sessions.
Table 1.
Inclusion Criteria.
| Inclusion criteria | Exclusion criteria |
|
|
|
|
|
|
|
We included literature that met the inclusion criteria of answering our research question.
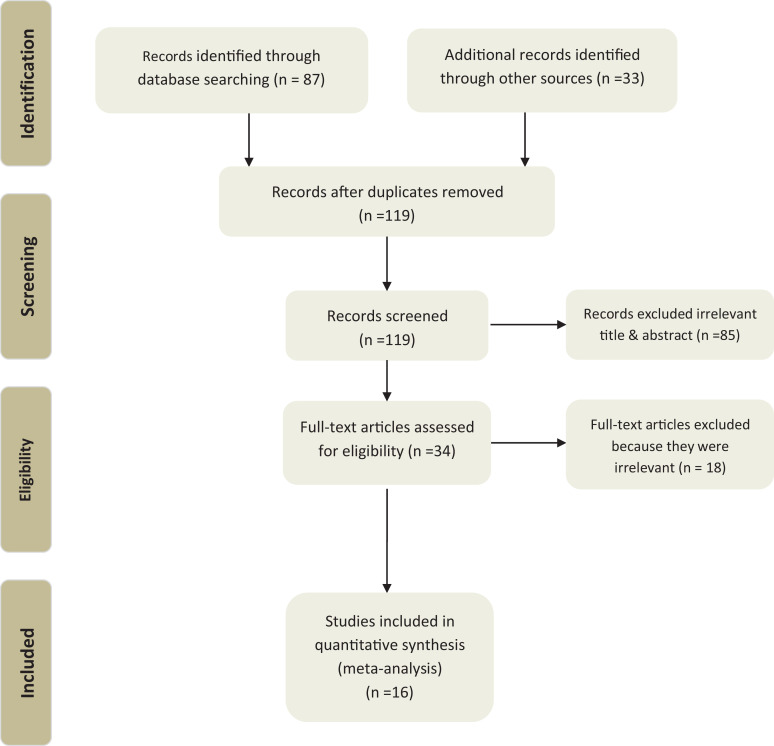
A flowchart shows the process of literature search and study selection (Figure 1).
Figure 1.
Flowchart of search process.
4. Charting the data
The groups of reviewers independently continued data extraction from included studies and were collected data in a pre-designed data collection chart, which included the title of the study, author(s), year of publication, journal, aims of study, type of study, date of study, study location (where the study was conducted), study population and sample size (if applicable), intervention type/duration (if applicable), comparator (if applicable), outcome measures (if applicable), duration of the intervention (if applicable), outcomes (if applicable), key findings that relate to the scoping review question, and limitations.
5. Collating, summarizing, and reporting the results
Finally, the results were summarized and reported.
Results
There were16 articles related to the research question. Literature was extracted from different types of sources. Most of the literature were research articles, and the rest were collected from other sources, including books, booklets, comments, surveys, development models, structured stockholder dialog, and policy statements. The literature and their key findings are presented in Table 2. Literature was divided into 3 categories (Figure 2). The first category included articles related to the economic impact of SCI on health systems and the cost-efficiency of medical and rehabilitation services. The second category included articles related to the role of research and developing a research strategy. The third category included articles related to effective interaction and communication with policymakers.
Table 2.
Summary of Literature.
| No | Author & year of publication | Type of literature | Key findings |
|---|---|---|---|
| 1 | Truchon et al: 201712 | Retrospective study | • Increasing of rehabilitation sessions is positively associated with changes in patients’ functional outcomes, which can lead to reduced resource utilization and cost savings. |
| 2 | Turner-Stokes et al: 201614 | Prospective cohort study | • Hyper-acute rehabilitation has high cost, but reduces on-going
care costs. • The high cost of hyper-acute rehabilitation is offset by savings on long-term care costs. • Even if the patient still needs care after hyper-acute rehabilitation, the patient’s need for care is reduced. |
| 3 | Turner-Stokes et al: 201615 | Prospective cohort study | • Specialized inpatient rehabilitation for the patients with complex neurological disabilities including SCI has high cost but it is highly cost-efficient and significantly reduces ongoing care costs. |
| 4 | Middleton et al: 201520 | Structured stakeholder dialog | • Developing a SCI research strategy supports the SCI research
community in conducting high-quality research, which increases
relevant high-quality research. • High-quality research can positively impact health policy. |
| 5 | Noonan et al: 201217 | To present developing a model | • The Operations Research (OR) technique such as simulation
modeling is used to evaluate the factors affecting the processes
of the health care system and to suggest effective changes in
SCI health care system. • The findings of various simulated processes, from the scene of injury to community reintegration, are used to influence policymakers and engage them to optimize SCI health care system. |
| 6 | Miyai et al: 201119 | Retrospective cohort study | • Incorporation of rehabilitation services in national insurance
facilitates access to these services, increases the quantity of
rehabilitation interventions, and improves patient
outcomes. • Increasing therapy coverage leads to improved rate of home discharge. |
| 7 | Merritt et al: 201918 | Narrative review | • Rehabilitation and training of people with SCI about secondary
complications not only saves money but also reduces the costs of
the health system. • Lack of access to care and rehabilitation services is associated with more secondary complications and increases health care costs for patients with SCI. • Although timely treatment and rehabilitation services leads to improved outcomes, access to these services is difficult because of their costs. |
| 8 | Johnson et al: 199611 | Prospective study | • Cost of treating secondary complications is much higher than
cost of routine medical examination. • Secondary complications can be identified in early stages by routine medical examination and treated with lower cost. |
| 9 | French et al: 200716 | Observational study | • Determination of the long-term costs of care for people with SCI is important for policymakers tomanage and allocate resources properly. |
| 10 | Miller et al: 201613 | Narrative review | • Physical activity is useful for health conditions of patients
with SCI and even moderate physical activity levels have
significant health benefits for these
patients. • Rehabilitation and use of assistive devices facilitate physical activity of patients with SCI and significantly reduce the risk of medical complications and costs associated with SCI. |
| 11 | Oliver et al: 201921 | Systematic review | • Key tips to influence policymaking are: conduct good quality research which should be relevant and clear, understand policy making process, keep in touch with policymakers timely and always be available for them, be flexible and respectful in your communication with policymakers, determine your role before contact with them, make a relationship with them based on basic principles, learn the consequences of your actions. |
| 12 | Tilley et al: 201722 | Booklet | • Things to influence policymakers are: (a) what you want to influence, (b)who you want to influence, (c)when to influence, (d)it is important to work with other people and organizations, (e) policymaking is complex and dynamic and involves a lot of different people and parts, (f) policymakers’ values, experience and expertise play an important role in influencing how they make decisions, (g) it is necessary to focus on clear messages and avoid technical language, (h) policymakers need constructive ideas (i) policymaking is a slow process without clear impact in the short term (j) it is important to remain flexible and adapt to new contexts and opportunities |
| 13 | Wang et al: 201023 | Comment | • Non-governmental organizations and patient advocacy groups
have an important role to influence policymakers. • The activities of these organizations have raised the attention of people and governments. |
| 14 | Conradsson et al: 20185 | prospective cohort study | • There is a significant gap of knowledge regarding the nature
of traumatic SCI care in low-to-middle income
countries. • There are lack of epidemiological data and lack of monitoring health condition of patients with SCI after discharge in developing countries. • There is lack of available resources for persons with SCI in developing countries. |
| 15 | European SCI Federation: 20086 | Policy Statement | • To establish regional and/or national spinal cord registers in
all European countries to inform and facilitate national health
care system budgeting and investment initiatives • To call on European countries to promote the centralization of treatment, rehabilitation, and life-long care of people with SCI, to manage all requirements of people with SCI including medical care and rehabilitation services. • To support the families of people with SCI |
| 16 | Lavis et al: 20047 | Narrative review | • Research is important to inform public
policymaking. • Systematic reviews can inform public policymaking by providing research-based answers to questions. • Health system policymakers are required to make important and costly health system decisions. |
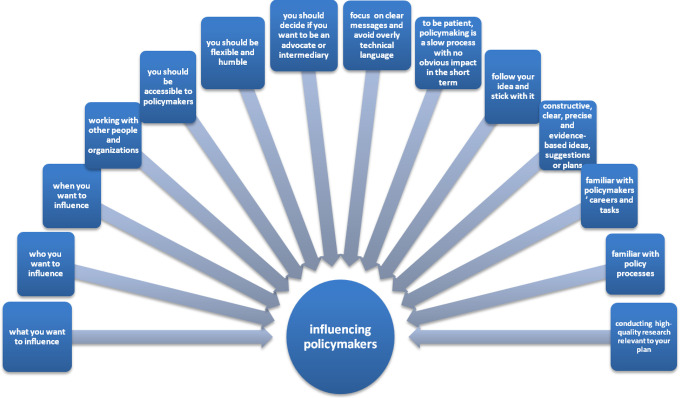
Figure 2.
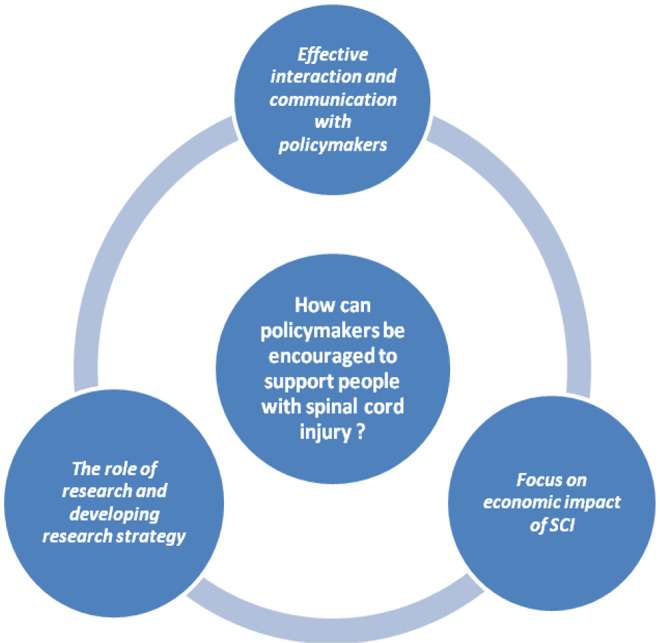
The ways to encourage policymakers to support individuals with spinal cord injury.
Economic Impact of SCI
Johnson et al demonstrated that the cost of treatment to identify secondary complications in early stages of SCI is 6 times greater than the cost of a routine medical exam. Secondary complications identified in early stages may therefore lead to lower costs. 11 Truchon et al examined the relationship between rehabilitation therapy, functional outcome, bed utilization, and care costs after traumatic SCI. Their study showed that an increase in the amount of therapy can reduce care cost and resource utilization. Their simulation analysis showed that an increase in the amount of therapy has an important role in reducing length of stay (LOS) and bed utilization, leading to savings in care costs. 12 Miller et al showed that individuals with SCI take advantage of physical activity to reduce secondary complications and increase cost of care savings. It has been shown that even moderate physical activity has an impact on improving health and reducing the rate of hospitalization. Since use of new technologies in assistive devices improves efficiency, rehabilitation and use of these novel assistive devices facilitates physical activity of individuals with SCI in the home setting and significantly reduces the risk of medical complications and cost associated with SCI. 13 Turner-Stokes et al compared the care cost of patients using hyper-acute rehabilitation with other patients with SCI. Despite the higher cost of hyper-acute rehabilitation, it is highly cost-efficient due to costs being offset by savings in ongoing care within 28 months. Their findings showed that despite the expensive cost of hyper-acute rehabilitation, it would lead to a long-term benefit for individuals with SCI due to a reduction in secondary complications and an increase in functional independence. Use of hyper-acute rehabilitation therefore has an important role in health system cost savings. 14 Additionally, the authors illustrated that use of specialist inpatient rehabilitation for patients with complex neurological disabilities including SCI can help reduce long-term care cost. 15 French et al described that policymakers must know about the cost of secondary complications related to the injury. This knowledge provides a view of long-term costs of care for individuals with SCI and helps them to allocate resources properly. 16 These studies showed that a reduction in secondary complications reduces economic burden on the health care system.
Noonan et al mentioned the effect of systematic care on patient outcomes and the cost of care using Operations Research (OR) techniques, such as simulation modeling. This type of research can be used for clinical decision-making and to engage policymakers to optimize the SCI health care system. 17
Merritt et al showed that although use of rehabilitation services and timely, organized treatment can improve patients’ outcomes, these services are not accessible for all people due to high costs. Lack of access to care and rehabilitation services has been associated with additional secondary complications and increased health care costs for individuals with SCI. 18 To make proper medical and rehabilitation services more accessible for individuals with SCI, we must strengthen infrastructure, such as the capacity of the health and rehabilitation workforce and early response services, improve coordination, and expand health insurance coverage. 2 Through a retrospective cohort study of patients with disabilities including traumatic SCI over 10 years, Miyai et al investigated changes in insurance coverage policies of inpatient rehabilitation and its effects on rehabilitation outcomes. The authors used Barthel Index and the Functional Independence Measure (FIM) as indicators to evaluate patient improvement. This study demonstrated that despite an increased number of severely disabled patients, increasing therapy insurance coverage led to improved rates of home discharge. The results of this study suggest that changes in national policy directly influence rehabilitation services and patient outcomes. 19
The European Spinal Cord Injury Federation (ESCIF) policy statement on the treatment, rehabilitation, and life-long care of people with SCI emphasizes establishing regional and national spinal cord registries in all European countries to inform and facilitate national health care system budgeting and investment initiatives. This statement calls for European countries to promote centralization of the treatment, rehabilitation, and life-long care of individuals with SCI to manage all requirements, including medical care and rehabilitation services. Based on this statement, national authorities should ensure that all individuals with SCI are referred to a specialized SCI center that provides treatment, rehabilitation, and care for individuals with SCI and their families, and research in this field. The statement mentions that national SCI organizations should receive financial support from the relevant authorities, such as the government and the health or social sector, to fund their contribution to these services and activities 6
The Role of Research and Developing Research Strategy
Middleton et al mentioned that advanced research and developing a research strategy play an important role in engaging policymakers and convincing them to enact legislation supporting individuals with SCI. Developing aresearch strategy can direct future research toward providing appropriate health care services and improving patient outcomes. By identifying cost management strategies, high quality SCI research strategies may reduce social and economic costs of spinal cord injury. 20 Lavis et al explained that systematic reviews can provide research-based answers for health system policymakers’ questions and help them to make appropriate decisions based on validated evidence and information. 7
Conradsson et al evaluated health care systems of traumatic SCI in South Africa and Sweden. They compared non-specialized care in South Africa (a developing country) versus specialized traumatic SCI care in Sweden (a developed country). This study demonstrated that there is a relationship between the type of care and outcomes of individuals with SCI. The authors found that there is a lack of knowledge regarding traumatic SCI care and research on SCI epidemiological data in developing countries. The lack of monitoring systems and post-injury health care in developing countries for individuals with SCI may lead to problems identifying patient needs. This study showed that the requirements of SCI patients are different in developed and developing countries. The findings of this study are high-quality evidence for policymakers to assess the feasibility and cost-effectiveness of life-saving changes in health care processes of SCI patients. 5
Effective Interaction and Communication with Policymakers
We must have effective communication with policymakers. Oliver et al recommended key tips that should be considered when communicating with policymakers, including conducting good quality, relevant, and legible research; understanding the policymaking process; keeping in touch with policymakers and always remaining available to them; being flexible and respectful when communicating with policymakers; determining your role before contacting them; establishing a relationship with them based on basic principles; and learning the consequences of your actions. 21 Tilley et al presented 10 things to influence policymakers: (1) what you want to influence, (2) who you want to influence, (3) when you want to influence, (4)working with other people and organizations, (5) policymaking is complex and dynamic and involves many different people and parts, (6) policymakers’ values, experience and expertise play an important role in influencing how they make decisions, (7) it is necessary to focus on clear messages and avoid overly technical language, (8) policymakers do not need to be told the problem; rather, they need constructive ideas, (9) often policymaking is a slow process with no obvious impact in the short term, and (10) it is important to remain flexible and adapt to new contexts and opportunities 22 (Figure 3). We provide a checklist based on these tips in Table 3.
Figure 3.
Tips for influencing policy makers. (Modified based on Tilley et al & Oliver et al).
Table 3.
Checklist of the Key Questions That are Essential to Influence Policymakers.21,22
| key questions | Yes | No |
|---|---|---|
| Do you know who you want to influence? | ||
| Do you know what you want to influence? | ||
| Do you know when you should to influence policymakers? | ||
| Do you work with other people and organizations to influence policymakers? | ||
| Are you accessible to policymakers? | ||
| Are you flexible and humble? | ||
| Have you decided if you want to be an advocate or intermediary? | ||
| Do you communicate with policymakers effectively? | ||
| Are you familiar with policymakers’ careers and tasks? | ||
| Are you familiar with policy processes? | ||
| Do you focus on clear messages and avoid technical language? | ||
| Do you have constructive, clear, precise and evidence-based ideas, suggestions or plans? | ||
| Do you follow your idea and stick with it? | ||
| Have you conducted high-quality research relevant to your plan to present policymakers? |
Wang et al highlighted the role of non-governmental organizations (NGOs) and patients’ advocacy groups in policymaking and meeting patient needs. They explained that NGOs are also developing and disseminating information, raising public awareness, fundraising, and improving patient access to health care. NGO activity has led to a rise in public and government attention. 23
Discussion
SCI is an injury with complex needs and various complications. Any delay in management leads to multiple complex and costly consequences. 24 Appropriate and timely medical care, proper rehabilitation services, and social support can lead to better outcomes and a productive life for individuals with SCI as well as their families. Action by governments and other institutions is necessary. Lack of effective action can exacerbate complications, thereby imposing costs on the health system.2,25 The costs of injury prevention and the treatment of secondary complications in early stages of SCI is much lower than treating these complications in later stages. However, access to timely treatment and rehabilitation services and assistive devices is difficult due to up-front costs.11,12,18
In many countries, patients with complex disabilities and high dependency, including individuals with SCI, may be deprived of rehabilitation because of expensive costs. The studies indicate that life expectancy for individuals with SCI in low-income countries is shorter than for individuals with SCI in high income countries. Because, in low-income countries, individuals with SCI do not have access to socio-economic and medical support that it leads to many problems. On the other hand, socio-economic level affects on caregiver burden. Lower socio-economic level is associated with higher caregiver burden.This means that caregivers with higher socioeconomic status reported less care burden.26,27 However, specialized rehabilitation can be highly cost-efficient for these patients and can lead to significant savings in ongoing care costs and reduce the pressure on acute care services. Studies have shown that SCI patients who are admitted earlier to specialized SCI units have a shorter LOS and fewer secondary medical complications compared to those admitted later.14,15,28 Expanding insurance coverage can be a solution to access of timely rehabilitation and treatment. Incorporating rehabilitation programs into the medical insurance system can lead to significant improvement in patient outcomes, reduction of the onset–admission interval and LOS, while also improving the rate of discharge. 19
Health status and life satisfaction in individuals with SCI are related to many factors, such as psychosocial status and severity of injury. Psychosocial status is more important than the severity of injury as a predictor of life satisfaction. Long life-care management can minimize secondary medical complications. SCI patients should be trained to cope with these complications. Individuals with SCI have mentioned physical and social barriers as factors in preventing adaptation to injury. They believed that because of these barriers, it is difficult to adapt to their new situation. Injury-related variables impact health status and social functioning, and as a result influence life satisfaction. The most important injury-related variables are housing, self-care equipment, transportation facilities, psychosocial condition, and social integration as a useful and productive member, not as a consumer. Social support significantly improves psychological and physical health and wellbeing. Additional social support is associated with greater life satisfaction and improved physical wellbeing. Meeting the needs of people with SCI requires the action of policymakers, and further research is needed to effectively influence the process of policymaking and legislation.4,29-31
To improve the health system and reduce deficiencies, policymakers are required to consider significant and costly decisions. They must determine long-term costs of care for SCI patients to make decisions for allocating resources properly. High-quality research such as systematic reviews can provide research-based answers to policymaking questions and help policymakers find the best solution for policymaking issues. It is recommended that researchers do not rely on empirical evidence, as this may lead to significant misunderstanding and costly consequences. Policymakers can make more informed policies by requesting systematic reviews on prioritized issues.7,16,21 There is a lack of accessible resources and essential epidemiological data and statistics, as well as a lack of identifying the unmet needs, of SCI patients in developing countries. 5 Epidemiological data and information on the needs of individuals with SCI are useful for policymakers and could be used to improve health care policies. A patient registry is an organized collecting data system that is used for scientific, clinical, or policy purposes. Access to valid, reliable, and consistent data is essential for evidence-based decisions. Registry systems can serve as a source for these data. Registration and follow-up of individuals with SCI is necessary to maintain continuity of care by health policymakers. This leads to timely access to services and reduces physical and mental complications and costs. It also prevents the waste of national system health resources. There is an urgent need to increase and improve data collection and research on SCI. SCI registries that collect data from hospitals are the best ways of collecting SCI data. Policymakers need data on costs, outcomes, and cost-benefits.2,3,32
High-quality research can positively impact health policy. Developing an SCI research strategy increases quality of relevant research. This leads to optimized outcomes for SCI patients, a reduction in the economic and social costs of SCI, and support for the SCI research community. To develop an SCI research strategy, we need to clearly determine priorities and build capacities and infrastructure such as physical and human resources, databases and registries, and an adequate and sustainable budget. 20 Management of resources for providing optimal care remains an essential requirement in the health care system. Techniques such as simulation modeling have been used to predict the impact of best practices and policy initiatives on outcomes in both the health care system and in patients. Findings from various simulated scenarios from the time of injury until community reintegration can be used to provide the evidence required to support clinical decision-making, to highlight standards of care, and to engage policymakers. 17
Effective interaction with policymakers is particularly important. Essential aspects of communicating with policymakers include knowing when, what, or who you want to influence, focussing on clear messages, and avoiding overly technical language. Policymakers need creative and beneficial ideas (Table 3).Therefore, statements that contain a precise and clear idea should be used. Flexibility and adaptation to new contexts and opportunities are important. 21 Patient advocacy groups and NGOs play an effective role in influencing policymakers. They are involved in supporting patients, establishing policies, and informing policymakers on patients’ unmet needs. 23 Also, they are involved in informing the people and raising public awareness, gathering funds, and helping patient’s access to health care. These organizations advocate for patients’ rights and can inform the authorities about the unmet needs of patients. On the other hand, by informing the public about patients’ unmet needs, NGOs play an important role in sensitizing the community to these needs and thus encouraging policymakers to address these needs and support patients.Hence, NGOs are active in various fields from medical care, education, and employment to policy and law, Patients training, volunteer medical service, focus group meetings and draw special attention to patients including SCI patients. Understanding other countries’ experiences in supporting individuals with SCI and similar individuals, such as patients with rare diseases, can be helpful. ESCIF encourages all European countries to promote the treatment, rehabilitation, and life-long care of individuals with SCI and to support them and their families.6,33 It should be noted that our study included only a database, which is a limitation for this study.
Conclusion
In conclusion, due to the complexity of the policy process, it is essential to consider multiple factors for encouraging policymakers to make laws that support individuals with SCI. It is necessary to understand how best to communicate with policymakers and to present constructive, precise, and evidence-based ideas. High-quality research and registry systems must be used to provide valid, reliable, and consistent data. A validated and accessible database is essential for evidence-based decisions and can effectively influence the process of policymaking and legislation. Furthermore, patient advocacy groups and non-governmental organizations (NGOs) play a key role in influencing policymakers’ decisions. NGOs are involved in establishing policies and addressing patients’ unmet needs. In addition, highlighting the cost-effective role of early intervention and timely specialized care in preventing secondary complications and reducing health care system costs can be beneficial. Continuity of care from the scene of injury until arrival at a specialized care center will improve patient functionality and health status. Incorporating rehabilitation program into the medical insurance system can make patients’ access to these services substantially easier. Prior experiences of other countries in this field can be helpful. Ultimately, comprehensive, and flexible planning is necessary to influence policymakers.
Footnotes
Authors’ Note: The Ethics Committee of Sina Trauma and Surgery Research Center, Tehran University of Medical Sciences, approved the study, and the reference number is 97-03-38-331.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: There is no conflict of interest regarding our paper except Alexander R. Vaccaro who has the following conflicts of interest:
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by Sina Trauma and Surgery Research Center, Tehran University of Medical Sciences [grant number is 97-03-38-39 808].
Royalties: Aesculap; Atlas Spine; Globus; Medtronics; SpineWave; Stryker Spine; Elsevier; Jaypee; Taylor Francis/Hodder and Stoughton; Thieme
Stock Options: Advanced Spinal Intellectual Properties; Atlas Spine; Avaz Surgical; Bonovo Orthopaedics; Computational Biodynamics; Cytonics; Deep Health; Dimension Orthotics LLC; Electrocore; Flagship Surgical; FlowPharma; Globus; Innovative Surgical Design; Insight Therapeutics; Jushi; Nuvasive; Orthobullets; Paradigm Spine; Parvizi Surgical Innovation; Progressive Spinal Technologies; Replication Medica; Spine Medica; Spinology; Stout Medical; Vertiflex; ViewFi Health
ORCID iD: Vafa Rahimi-Movaghar, MD  https://orcid.org/0000-0001-7347-8767
https://orcid.org/0000-0001-7347-8767
Alexander R. Vaccaro, MD  https://orcid.org/0000-0002-8073-0796
https://orcid.org/0000-0002-8073-0796
References
- 1.Sharwood LN, Stanford R, Middleton JW, et al. Improving care standards for patients with spinal trauma combining a modified e-Delphi process and stakeholder interviews: a study protocol. BMJ Open. 2017;7(1):e012377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. International perspectives on spinal cord injury: World Health Organization/International Spinal Cord Society; 2013. [Google Scholar]
- 3.World Health Organization. Fact-Sheets/Spinal Cord Injury. spinal cord injury; Accessed 19 November, 2013. [Google Scholar]
- 4.Babamohamadi H, Negarandeh R, Dehghan-Nayeri N. Barriers to and facilitators of coping with spinal cord injury for Iranian patients: a qualitative study. Nurs Health Sci. 2011;13(2):207–215. [DOI] [PubMed] [Google Scholar]
- 5.Conradsson D, Rhoda A, Mlenzana N, et al. Strengthening health systems for persons with traumatic spinal cord injury in south Africa and Sweden: a protocol for a longitudinal study of processes and outcomes. Front Neurol. 2018;9:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Federation ESCI. ESCIF Policy Statement on the treatment, rehabilitation and life long care of persons with spinal cord injuries (SCI). Europian Spinal Cord Injury Federation; 2008. www.http://www.escif.org/ [Google Scholar]
- 7.Lavis JN, Posada FB, Haines A, Osei E. Use of research to inform public policymaking. Lancet. 2004;364(9445):1615–1621. [DOI] [PubMed] [Google Scholar]
- 8.Martin R.Law as a tool in promoting and protecting public health: always in our best interests? Public Health. 2007;121(11):846–853. [DOI] [PubMed] [Google Scholar]
- 9.Peters MDJ GC, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: scoping reviews. In: Aromataris E MZE, ed. Joanna Briggs Institute Reviewer’s Manual, JBI. Published 2014. Updated March 2020. Accessed June 28, 2020. Available from https://reviewersmanual.joannabriggs.org/.
- 10.Arksey H, O’Malley L.Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 11.Johnson RL, Brooks CA, Whiteneck GG. Cost of traumatic spinal cord injury in a population-based registry. Spinal Cord. 1996;34(8):470–480. [DOI] [PubMed] [Google Scholar]
- 12.Truchon C, Fallah N, Santos A, Vachon J, Noonan VK, Cheng CL. Impact of therapy on recovery during rehabilitation in patients with traumatic spinal cord injury. J Neurotrauma. 2017;34(20):2901–2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller LE, Herbert WG. Health and economic benefits of physical activity for patients with spinal cord injury. Clinicoecon Outcomes Res. 2016;8:551–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turner-Stokes L, Bavikatte G, Williams H, Bill A, Sephton K. Cost-efficiency of specialist hyperacute in-patient rehabilitation services for medically unstable patients with complex rehabilitation needs: a prospective cohort analysis. BMJ Open. 2016;6(9):e012112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turner-Stokes L, Williams H, Bill A, Bassett P, Sephton K. Cost-efficiency of specialist inpatient rehabilitation for working-aged adults with complex neurological disabilities: a multicentre cohort analysis of a national clinical data set. BMJ Open. 2016;6(2):e010238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.French DD, Campbell RR, Sabharwal S, Nelson AL, Palacios PA, Gavin-Dreschnack D. Health care costs for patients with chronic spinal cord injury in the Veterans Health Administration. J Spinal Cord Med. 2007;30(5):477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noonan VK, Soril L, Atkins D, et al. The application of operations research methodologies to the delivery of care model for traumatic spinal cord injury: the access to care and timing project. J Neurotrauma. 2012;29(13):2272–2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merritt CH, Taylor MA, Yelton CJ, Ray SK. Economic impact of traumatic spinal cord injuries in the United States. Neuroimmunol Neuroinflammation. 2019;6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miyai I, Sonoda S, Nagai S, et al. Results of new policies for inpatient rehabilitation coverage in Japan. Neurorehabil Neural Repair. 2011;25(6):540–547. [DOI] [PubMed] [Google Scholar]
- 20.Middleton JW, Piccenna L, Lindsay Gruen R, et al. Developing a spinal cord injury research strategy using a structured process of evidence review and stakeholder dialogue. Part III: outcomes. Spinal Cord. 2015;53(10):729–737. [DOI] [PubMed] [Google Scholar]
- 21.Oliver K, Cairney P. The dos and don’ts of influencing policy: a systematic review of advice to academics. Palgrave Communications. 2019;5(1):1–1. [Google Scholar]
- 22.Tilley H, Shaxson L, Rea J, Ball L. 10 things to know about how to influence policy with research. In: Institute OD, ed. Overseas Development Institute; Published January 2017. Accessed September 29, 2019. https://www.odi.org/publications/10671-10-things-know-about-how-influence-policy-research/ [Google Scholar]
- 23.Wang JB, Guo JJ, Yang L, Zhang YD, Sun ZQ, Zhang YJ. Rare diseases and legislation in China. Lancet. 2010;375(9716):708–709. [DOI] [PubMed] [Google Scholar]
- 24.Donovan L, Francis L, Muter P, Nevin S, Warren R. Spinal cord injuries: overcoming barriers to seamless care for patients. Br J Nurs. 2017;26(6):324–330. [DOI] [PubMed] [Google Scholar]
- 25.Carlson M, Vigen CLP, Rubayi S, et al. Lifestyle intervention for adults with spinal cord injury: Results of the USC-RLANRC Pressure Ulcer Prevention Study. J Spinal Cord Med. 2019;42(1):2–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tough H, Brinkhof MWG, Siegrist J, Fekete C. Social inequalities in the burden of care: a dyadic analysis in the caregiving partners of persons with a physical disability. Int J Equity Health. 2019;19(1):1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Øderud T. Surviving spinal cord injury in low income countries. African journal of disability. 2014;3(2):80–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amber Harnett ABM, Amanda McIntyre, Ruchi Parikh, James Middleton, Mohit Arora, Dalton Wolfe, Swati Mehta. Spinal Cord Injury Rehabilitation Practices. Updated 2020. Accessed July 4, 2020, https://scireproject.com/evidence/rehabilitation…/rehabilitation-practices/
- 29.Anson CA, Stanwyck DJ, Krause JS. Social support and health status in spinal cord injury. Paraplegia. 1993;31(10):632–638. [DOI] [PubMed] [Google Scholar]
- 30.Rintala DH, Young ME, Hart KA, Clearman RR, Fuhrer MJ. Social support and the well-being of persons with spinal cord injury living in the community. Rehabilitation Psychology. 1992;37(3):155. [PubMed] [Google Scholar]
- 31.Post MW, de Witte LP, van Asbeck FW, van Dijk AJ, Schrijvers AJ. Predictors of health status and life satisfaction in spinal cord injury. Arch Phys Med Rehabil. 1998;79(4):395–401. [DOI] [PubMed] [Google Scholar]
- 32.Noonan VK, Kwon BK, Soril L, et al. The Rick Hansen Spinal Cord Injury Registry (RHSCIR): a national patient-registry. Spinal Cord. 2012;50(1):22–27. [DOI] [PubMed] [Google Scholar]
- 33.Dharssi S, Wong-Rieger D, Harold M, Terry S. Review of 11 national policies for rare diseases in the context of key patient needs. Orphanet J Rare Dis. 2017;12(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]