Abstract
Study Design:
This was a prospective controlled study.
Objective:
To compare the accuracy and clinical outcomes of robot-assisted (RA) and fluoroscopy-guided (FG) pedicle screw placement in posterior cervical surgery.
Methods:
This study included 58 patients. The primary outcome measures were the 1-time success rate and the accuracy of pedicle screw placement according to the Gertzbein-Robbins scales. The secondary outcome measures, including the operative time, intraoperative blood loss, hospital stay, cumulative radiation time, radiation dose, intraoperative advent events, and postoperative complications, were recorded and analyzed. The Japanese Orthopedics Association (JOA) scores and Neck Disability Index (NDI) were used to assess the neurological function of patients before and at 3 and 6 months after surgery.
Results:
The rate of grade A was significantly higher in the RA group than in the FG group (90.6% and 71.1%; P < .001). The clinically acceptable accuracy was 97.2% in the RA group and 90.7% in the FG group (P = .009). Moreover, the 1-time success rate was significantly higher in the RA group than in the FG group. The RA group had less radiation time (P < .001) and less radiation dose (P = .002) but longer operative time (P = .001). There were no significant differences in terms of intraoperative blood loss, hospital stay, intraoperative adverse events, postoperative complications, JOA scores, and NDI scores at each follow-up time point between the 2 groups.
Conclusions:
The RA technique achieved higher accuracy and 1-time success rate of pedicle screw placement in posterior cervical surgery while achieving comparable clinical outcomes.
Keywords: robot-assisted, fluoroscopy-guided, posterior cervical surgery, pedicle screw placement
Introduction
Pedicle screw fixation is widely used in clinical practice because it can provide strong spinal stability.1,2 Solid and reliable internal fixation mainly depends on perfect placement of the pedicle screw. However, because of the complex anatomical structure of the spine and the morphological variation of the individual vertebral pedicle, conventional free-hand pedicle screw insertion is often inaccurate or even unsuccessful based on the anatomical markers and intraoperative fluoroscopy, resulting in serious complications, including vascular, nerve, or spinal cord injury.3-7 Although the accuracy of free-hand pedicle screw placement would significantly improve with the increasing number of operations and the increasing experience of the surgeon, it was reported that the rate of misplaced screws under fluoroscopy guidance remained high, ranging from 8.3% to 50.3%.8,9
In recent years, robots have been introduced into spinal surgery to overcome the insufficiencies of conventional fluoroscopy-guided (FG) screw placement, such as limited surgical field of view, fatigue, and varied accuracy. 10 The robot-assisted (RA) technology was reported to achieve acceptable accuracy of pedicle screw placement in different lumbar and/or thoracic surgical procedures compared with conventional FG spine surgery, whereas the effective consequence of robot assistance on operative time, hospital stay, and radiation exposure remains controversial. 11
Unlike thoracic and lumbar vertebrae, the pedicles of the cervical spine are thinner and narrower, and the surrounding anatomy is more complex than the rest of the spine. Thus, up to now, FG cervical pedicle screw placement remains a challenge for most surgeons, requiring highly extensive experience. The emerging RA technique reportedly has the potential to overcome some limits of free-hand spine surgery, although there are few studies on performance in cervical pedicle screw placement. Kostrzewski et al 12 first described a robotic system for atlantoaxial fixation, which was insufficient for clinical application for high translational error (1.94 mm). The TiRobot, an orthopaedic robot completely created in China (TINAVI Medical Technologies Co, Ltd, Fenton, MO), which can be used in spinal, pelvic, and limb surgeries,13,14 had been used to perform RA odontoid fracture fixation and lumbar spine surgery and achieved acceptable accuracy. 15 In this study, we aimed to compare the accuracy and clinical outcomes of pedicle screw placement in posterior cervical surgery using the TiRobot-assisted technique versus the conventional FG technique.
Materials and Methods
Study Design and Participants
This is a prospective nonrandomized and controlled study. A total of 58 patients in Renji Hospital from December 2018 to December 2019 were consecutively recruited and assigned to 2 groups without randomization. It was up to the patients to choose RA or FG treatment after a detailed explanation of the 2 kinds of surgeries. All posterior cervical surgeries were performed by the same team, and all the pedicle screw insertions in both groups were completed by the senior surgeon. The study was approved by the Renji Hospital Ethics Committee, and all participants received detailed information on this study and gave written informed consent.
The inclusion criteria were as follows: (1) age from 18 to 80 years, (2) able to give informed consent to study participation, (3) male and female patients, and (4) indication for posterior cervical surgery for degenerative or traumatic conditions. The exclusion criteria were as follows: (1) inability to complete follow-up or provide informed consent, (2) patients with incomplete pedicle wall or severe pedicle deformity, (3) patients with a history of relevant posterior cervical spine surgery, (4) patients with bad general conditions, (5) patients unable to tolerate surgery, (6) revision surgery.
Robot-Assisted Implantation
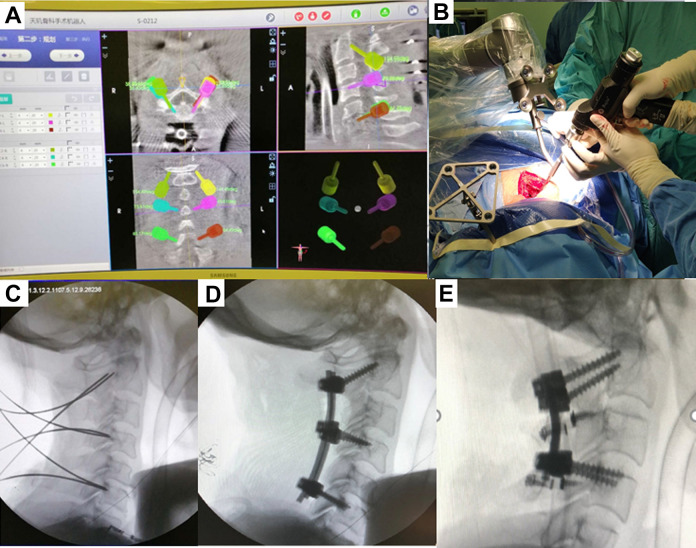
The TiRobot is mainly composed of a surgical robotic arm, an optical tracking device, and a surgical planning and controlling workstation (Figure 1). The whole intraoperative operation procedure can be divided into 6 parts: robot preparation, 3D image acquisition, automatic registration, pedicle screw path planning, pedicle screw placement, and postoperative image verification.
Figure 1.
The TiRobot system is mainly composed of a surgical robotic arm, an optical tracking device, and a surgical planning and controlling workstation.
The patients were placed in prone position on the spinal operating table after general anesthesia, with their head fixed in the Mayfield frame. The operative vertebra was defined by fluoroscopy, and a posterior midline incision was made at the spinous process of the operative vertebra. The patient tracker was placed in the Mayfield frame. The calibrator at the end of the robotic arm moved as close as possible to the surgical site. The 3D images were acquired by the C-arm scanner and transferred to the workstation. According to the images, the surgeon planed the optimal entry point, and angle and depth of the pedicle screw and determined the diameter and length of the screws (Figure 2A). Then, the robotic arm moved according to the preplanned screw trajectory and showed the insertion point and direction of the screws (Figure 2B). The K-wires were successfully inserted along the guidance tube at the end of the robotic arm (Figure 2C). Finally, the hollow screws were precisely inserted along the K-wires (Figure 2D). After screw placement, decompression and interbody fusion were performed when needed.
Figure 2.
A. Preoperative planning of pedicle screw trajectory. B-D. Robot-assisted pedicle screw placement. E. Fluoroscopy-guided pedicle screw placement.
Fluoroscopy-Guided Implantation
The patients were placed in prone position on the spinal operating table after general anesthesia, with their heads fixed. Anterior and lateral fluoroscopy of the cervical vertebra was performed using the C-arm scanner before surgery to determine the surgical site. A posterior midline incision was made at the surgical site. The anatomical landmarks of the insertion point of each cervical vertebra was fully exposed, and the screws were inserted along the axial angle of each pedicle (Figure 2E).
Outcome Measures and Postoperative Follow-up
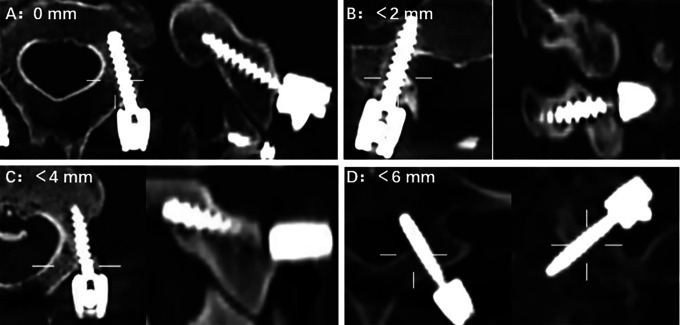
One of the primary outcome measures was the accuracy of pedicle screw placement, which was assessed on postoperative computed tomography (CT) according to the Gertzbein and Robbins scale, 9 classified as grade A (screw completely within the pedicle), grade B (pedicle cortical breach < 2 mm), grade C (pedicle cortical breach ≥ 2 to < 4 mm), grade D (pedicle cortical breach ≥ 4 to < 6 mm), or grade E (pedicle cortical breach ≥ 6 mm; Figure 3). The 1-time success rate referred to the ratio of the number of pedicle screws successfully completed in 1 attempt to the total number. Other outcome measurements, including operative time, intraoperative blood loss, hospital stay, cumulative radiation time, radiation dose, and complication rates were recorded and analyzed. The Japanese Orthopedics Association (JOA) scores and Neck Disability Index (NDI) were used to assess the neurological function of patients before and at 3 and 6 months after surgery.
Figure 3.
The Gertzbein-Robins classification for screw positioning: (A) grade A: no breach of the cortical layer of the pedicle or vertebral body; (B) grade B: cortical breach < 2 mm; (C) grade C: penetration of < 4 mm; (D) grade D: penetration of < 6 mm (grade E: not shown).
Statistical Analysis
The data in this study was analyzed using SPSS (version 20.0). The χ2 test, t-test, and rank-sum test were used depending on the data type. Values are presented as the mean ± SD. A P value less than .05 was considered statistically significant.
Results
A total of 58 patients met the criteria and were included in this study, including 32 male and 26 female patients, with an average age of 60.36 ± 5.00 years. There were 28 patients (15 male and 13 female) in the RA group, with an average age of 60.40 ± 4.99 years, and 30 patients (17 male and 13 female) in the FG group, with an average age of 60.33 ± 5.23 years. There were no significant differences in age, gender, body mass index, and the level and segment between the 2 groups (Table 1). All the patients underwent successful surgery, and no iatrogenic nerve or vascular injury occurred. The postoperative symptoms were significantly relieved. A postoperative cervical collar was required for each patient for 1 month.
Table 1.
Patient Demographics.
| Variable | RA group (n = 28) | FG group (n = 30) | P value |
|---|---|---|---|
| Age (years) | 60.40 ± 4.99 | 60.33 ± 5.23 | .821 |
| Male/female | 15/13 | 17/13 | .813 |
| BMI (kg/m2) | 23.53 ± 3.22 | 23.59 ± 2.64 | .349 |
| Diagnosis | .849 | ||
| Radiculopathy | 6 | 7 | |
| CSM | 16 | 15 | |
| Radiculopathy and CSM | 5 | 8 | |
| Cervical spine fracture | 1 | 0 | |
| Level | .950 | ||
| 1 | 6 | 6 | |
| 2 | 12 | 14 | |
| 3 | 8 | 7 | |
| 4 | 2 | 3 | |
| Number of screws used | 180 | 194 |
Abbreviations: BMI, body mass index; CSM, cervical spondylotic myelopathy; FG, fluoroscopy-guided; RA, robot assisted.
Primary Outcome Measurement
Of the 180 screws inserted in the RA group, 163 were grade A (90.6%), and 12 (6.7%), 4 (2.2%), 1 (0.6%), and 0 (0%) screws were classified as grades B, C, D, and E, respectively. Of the 194 screws in the FG group, 138 achieved a perfect trajectory (grade A; 71.1%), with 39 screws (20.1%) scored as grade B, 16 screws (8.2%) scored as grade C, 2 screws (1.0%) scored as grade D, and 0 screws (0%) scored as grade E. The accuracy of grade A was significantly higher in the RA group than in the FG group (P < .001). Furthermore, the accuracy of clinically acceptable screws (grades A and B) was significantly higher in the RA group (P = .009). Besides, the 1-time success rate of pedicle screw placement was significantly higher in the RA group than in the FG group (Table 2).
Table 2.
Primary Measures.
| Variables | RA group | FG group | P value |
|---|---|---|---|
| Total | 180 | 194 | |
| One-time success rate, n (%) | 172 (95.6%) | 168 (86.6%) | P = .003 |
| Gertzbein and Robbins Scale | P < .001 | ||
| Grade A screws, n (%) | 163 (90.6%) | 138 (71.1%) | |
| Grade B screws, n (%) | 12 (6.7%) | 39 (20.1%) | |
| Grade C screws, n (%) | 4 (2.2%) | 16 (8.2%) | |
| Grade D screws, n (%) | 1 (0.6%) | 2 (1.0%) | |
| Grade E screws, n (%) | 0 (0%) | 0 (0%) | |
| Grade A and B screws, n (%) | 175 (97.2%) | 176 (90.7%) | P = .009 |
Abbreviations: FG, fluoroscopy guided; RA, robot assisted.
Clinical Outcomes
The average operative time in the RA group was significantly longer than that in the FG group (RA: 267.00 ± 22.03 minutes; FG: 240.00 ± 25.23 minutes; P = .001). The radiation time (RA: 2.21 ± 0.83 minutes, FG: 3.47 ± 0.50 minutes; P < .001) and radiation dose (RA: 43.59 ± 17.33 μSv; FG: 62.23 ± 5.47 μSv; P = .002) were significantly lower in the RA group than in the FG group. There was no statistical difference in postoperative hospital stay between the 2 groups (RA: 6.60 ± 0.97 days; FG: 6.92 ± 0.99 days; P = .460). Besides, there were no significant differences in intraoperative blood loss (RA: 237.17 ± 16.67 mL; FG: 232.50 ± 17.68 mL; P = .532), intraoperative adverse events, and postoperative complications between groups (Table 3). One patient in the FG group suffered wound infection after surgery, and no patient in the 2 groups required revision surgery.
Table 3.
Perioperative and Postoperative Results Between the RA and FG Groups.
| Variables | RA group | FG group | P value |
|---|---|---|---|
| Operative time (minutes) | 267.00 ± 22.03 | 240.00 ± 25.23 | .001 |
| Intraoperative blood loss (mL) | 237.17 ± 16.67 | 232.50 ± 17.68 | .532 |
| Radiation time (minutes) | 2.21 ± 0.83 | 3.47 ± 0.50 | < .001 |
| Radiation dose (μSv) | 43.59 ± 17.33 | 62.23 ± 5.47 | .002 |
| Hospital stay (days) | 6.60 ± 0.97 | 6.92 ± 0.99 | .460 |
| Intraoperative adverse events | 0 | 0 | >.999 |
| Postoperative complications | 0 | 1 | .422 |
Abbreviations: FG, fluoroscopy guided; RA, robot assisted.
Postoperative Follow-up
Significant improvement in NDI scores and JOA scores were found after surgery in the 2 groups. But there were no significant differences in the NDI and JOA scores between groups at each follow-up time point (Table 4).
Table 4.
The JOA and NDI Scores Between the RA and FG Groups.
| Variable | RA group | FG group | P value |
|---|---|---|---|
| JOA scores | |||
| Preoperative | 8.30 ± 0.48 | 7.83 ± 0.72 | .096 |
| 3 Months after surgery | 12.40 ± 0.84 | 12.50 ± 1.17 | .824 |
| 6 Months after surgery | 14.20 ± 0.92 | 14.33 ± 0.89 | .733 |
| NDI scores | |||
| Preoperative | 34.00 ± 1.70 | 35.33 ± 1.30 | .058 |
| 3 Months after surgery | 15.50 ± 1.43 | 16.42 ± 1.16 | .113 |
| 6 Months after surgery | 12.80 ± 1.14 | 13.25 ± 1.22 | .384 |
Abbreviations: FG, fluoroscopy guided; JOA, Japanese Orthopedic Association; NDI, Neck Deformity Index; RA, robot assisted.
Discussion
FG pedicle screw placement of the cervical spine remains a challenge for most surgeons, requiring highly extensive experience because of thinner and narrower pedicles and more complex anatomy around. In recent years, there has been mounting interest in RA techniques in spine surgery, which have reportedly overcome several insufficiencies of traditional surgery while achieving comparable or better accuracy and clinical outcomes. 11 However, there are few studies on the cervical spine. Therefore, in this study, we aimed to compare the accuracy and clinical outcomes of RA and FG pedicle screw placement in posterior cervical surgery. The results showed that the RA group had higher accuracy and 1-time success rate of pedicle screw placement while achieving comparable clinical outcomes versus the FG group in posterior cervical surgery.
Compared with the FG group, the RA group achieved higher accuracy of pedicle screw placement, in agreement with some previous studies with other RA spine techniques.10,16-18 This could be attributed to 2 reasons. First, the cumbersome and laborious surgical procedures could easily lead to physical and mental fatigue of the surgeon, thus reducing the accuracy of pedicle screw placement, 19 whereas the robots could perform repetitive tasks precisely without fatigue and eliminate manual errors.20-22 Second, the 3D images of the operation area obtained by intraoperative C-arm scan could help the surgeon choose the optimal insertion point, direction, and depth, and finally, the screws could be inserted accurately in accordance with the predetermined screw path, making the operator’s operation visualized and multidimensional and avoiding the danger area to the maximum extent. However, in contrast to the higher accuracy, the opposite findings were reported by Ringel et al 22 —namely, that there was significantly lower pedicle screw accuracy in the RA group versus the FG group in lumbar spine surgery. Currently, the accuracy of pedicle screw placement with robot assistance is variable and remains controversial, and some authors thought that these conflicting results were partly a result of different robotic designs and manufacturers. 18
The RA group had a significantly higher 1-time success rate, which may be because the coordination of the sensitive optical tracking system and the flexible robotic arm accurately locating at the preplanned pedicle screw trajectory ensured the reliability and repeatability of the preplanned screw path and direction, even if the patient’s actual position changed during the operation. 23 The higher 1-time success rate suggested that the RA technique could avoid the process of repeatedly pulling out, adjusting, and putting in, thus avoiding an oversized screw path, increasing the pedicle’s holding force on screws and decreasing, loosening, or even failure of the internal fixation. Furthermore, the higher 1-time success rate also indicated less damage to the cervical pedicle, facet joints, and soft tissues around. This is another advantage of the RA technique in cervical pedicle screw placement because unlike thoracic and lumbar vertebrae, the characteristic anatomy (thinner and narrower pedicles) of the cervical spine does not tolerate the repeated process of in and out.
Radiation exposure to the patients, defined as the cumulative dose of fluoroscopy required for screw placement, was significantly less in the RA group compared with the FG group, consistent with previous studies on the lumbar spine.10,20,24 This was mainly because the TiRobot-assisted navigation system did not rely too much on fluoroscopy, and the whole operation only needed 1 CT scan and 2 fluoroscopies—namely, preoperative planning and postoperative verification. Furthermore, the TiRobot system provided sufficient guarantee for precise screw placement, avoiding the repeated adjustment caused by screw trajectory deviation, thus reducing further fluoroscopy and radiation exposure. Besides, the RA imaging system had a faster imaging speed, which could reduce the radiation time of patients. Even experienced surgeons using TiRobot-assistance technology could reportedly reduce radiation exposure compared with conventional FG spinal surgery. 25
The results showed that the TiRobot-assisted technique required significantly longer operative time compared with the conventional free-hand technique, whereas some studies proposed that there was no significant difference in the operative time between the RA group and the FG group. 10 Currently, the use of the RA technique in spinal surgery is still in its early clinical stages, and a new technique always requires a learning curve before it reaches a state of proficiency and stability. The increased operative time can be attributed in part to the learning curve and the adjustment time between the surgeon and the new machine. In addition, the preoperative robot preparation and pedicle screw path planning also increased the operative time.
Although the results showed that the RA group needed longer operative times, there was no significant difference in the intraoperative blood loss. The increased operative time in the RA group was mainly a result of preoperative surgical robot preparation and pedicle screw path planning. But these 2 parts did not cause significant blood loss. Besides, there were no significant differences between groups in terms of postoperative functional recovery and postoperative complications. However, the TiRobot-assisted technique had been reported to be associated with less exposure of the facet joints, less postoperative residual pain at the surgical site, and less damage to nerves and blood vessels, contributing to the postoperative recovery of patients. 14 In contrast, the free-hand pedicle screw placement was associated with excessive exposure of the lateral edge of the joints and other anatomical structures, causing severe damage to soft tissue. 14 During the operations, we did observe less facet joint injury and less tissue dissection in the RA group, especially in the proximal and distal facet joints. This is another advantage of the RA technique, which may cause less adjacent segment degeneration, and long-term follow up is required in future studies.
In summary, the TiRobot-assisted technology can help surgeons better plan and simulate pedicle screw placement and significantly improve the accuracy and 1-time success rate of posterior cervical pedicle screw placement while achieving comparable clinical outcomes. Moreover, accurate positioning of the entry point allows maximum avoidance of the danger area and less damage to facet joints, pedicles, and soft tissues around and further reduces the risk of surgery, especially in patients with cervical deformity and vertebral artery deformity. In addition, RA technology can reduce the radiation time and dose of patients. However, this study had some limitations. First, this study was not randomized, and the treatment for patients (RA or FG) depended on their own choice. Second, the sample size of this study is small, so a large-sample study is needed for more convincing results. Third, the follow-up duration is too short for functional outcomes, and long-term follow up is required. Finally, as a new product of artificial intelligence, the TiRobot still has room for improvement, such as the longer operative time.
Conclusion
The RA technique achieved higher accuracy and 1-time success rate of pedicle screw placement in posterior cervical surgery while achieving comparable clinical outcomes.
Footnotes
Authors’ Note: Xin-Jin Su and Zhen-Dong Lv contributed equally to this work and should be considered as co–first authors.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Smart Medical Special Research Project of Shanghai Municipal Commission of Health and Family Planning (2018ZHYL0215) and the Program of Shanghai Subject Chief Scientist (PYIV-17-002).
ORCID iD: Li-Feng Lao, MD, PhD  https://orcid.org/0000-0003-2933-3514
https://orcid.org/0000-0003-2933-3514
Hong-Xing Shen, MD, PhD  https://orcid.org/0000-0001-9220-821X
https://orcid.org/0000-0001-9220-821X
References
- 1.Lau D, Terman SW, Patel R, La Marca F, Park P. Incidence of and risk factors for superior facet violation in minimally invasive versus open pedicle screw placement during transforaminal lumbar interbody fusion: a comparative analysis. J Neurosurg Spine. 2013;18:356–361. [DOI] [PubMed] [Google Scholar]
- 2.Gaines RW, Jr. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82:1458–1476. [DOI] [PubMed] [Google Scholar]
- 3.Panjabi M, Goel V, Oxland T, et al. Human lumbar vertebrae: quantitative three-dimensional anatomy. Spine (Phila Pa 1976). 1992;17:299–306. [DOI] [PubMed] [Google Scholar]
- 4.Kothe R, O’Holleran JD, Liu W, Panjabi MM. Internal architecture of the thoracic pedicle: an anatomic study. Spine (Phila Pa 1976). 1996;21:264–270. [DOI] [PubMed] [Google Scholar]
- 5.Tan SH, Teo EC, Chua HC. Quantitative three-dimensional anatomy of cervical, thoracic and lumbar vertebrae of Chinese Singaporeans. Eur Spine J. 2004;13:137–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bredow J, Oppermann J, Kraus B, et al. The accuracy of 3D fluoroscopy-navigated screw insertion in the upper and sub-axial cervical spine. Eur Spine J. 2015;24:2967–2976. [DOI] [PubMed] [Google Scholar]
- 7.Lvov I, Grin A, Talypov A, et al. Potential intraoperative factors of screw-related complications following posterior transarticular C1-C2 fixation: a systematic review and meta-analysis. Eur Spine J. 2019;28:400–420. [DOI] [PubMed] [Google Scholar]
- 8.Tian W, Liu Y, Zheng S, Lv Y. Accuracy of lower cervical pedicle screw placement with assistance of distinct navigation systems: a human cadaveric study. Eur Spine J. 2013;22:148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976). 1990;15:11–14. [DOI] [PubMed] [Google Scholar]
- 10.Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions: a randomized controlled trial. Spine (Phila Pa 1976). 2017;42:353–358. [DOI] [PubMed] [Google Scholar]
- 11.Ghasem A, Sharma A, Greif DN, Alam M, Al Maaieh M. The arrival of robotics in spine surgery: a review of the literature. Spine (Phila Pa 1976). 2018;43:1670–1677. [DOI] [PubMed] [Google Scholar]
- 12.Kostrzewski S, Duff JM, Baur C, Olszewski M. Robotic system for cervical spine surgery. Int J Med Robot. 2012;8:184–190. [DOI] [PubMed] [Google Scholar]
- 13.Han X, Tian W, Liu Y, et al. Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomized controlled trial. J Neurosurg Spine. Published online February 8, 2019. doi:10.3171/2018.10.SPINE18487 [DOI] [PubMed] [Google Scholar]
- 14.Feng S, Tian W, Sun Y, Liu Y, Wei Y. Effect of robot-assisted surgery on lumbar pedicle screw internal fixation in patients with osteoporosis. World Neurosurg. 2019;125:e1057–e1062. [DOI] [PubMed] [Google Scholar]
- 15.Tian W, Wang H, Liu YJ. Robot-assisted anterior odontoid screw fixation: a case report. Orthop Surg. 2016;8:400–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kantelhardt SR, Martinez R, Baerwinkel S, Burger R, Giese A, Rohde V. Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J. 2011;20:860–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roser F, Tatagiba M, Maier G. Spinal robotics: current applications and future perspectives. Neurosurgery. 2013;72(suppl 1):12–18. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Q, Han XG, Xu YF, et al. Robot-assisted versus fluoroscopy-guided pedicle screw placement in transforaminal lumbar interbody fusion for lumbar degenerative disease. World Neurosurg. 2019;125:e429–e434. [DOI] [PubMed] [Google Scholar]
- 19.Overley SC, Cho SK, Mehta AI, Arnold PM. Navigation and robotics in spinal surgery: where are we now? Neurosurgery. 2017;80(3S):S86–S99. [DOI] [PubMed] [Google Scholar]
- 20.Joseph JR, Smith BW, Liu X, Park P. Current applications of robotics in spine surgery: a systematic review of the literature. Neurosurg Focus. 2017;42:E2. [DOI] [PubMed] [Google Scholar]
- 21.Lieberman IH, Hardenbrook MA, Wang JC, Guyer RD. Assessment of pedicle screw placement accuracy, procedure time, and radiation exposure using a miniature robotic guidance system. J Spinal Disord Tech. 2012;25:241–248. [DOI] [PubMed] [Google Scholar]
- 22.Ringel F, Stuer C, Reinke A, et al. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomized comparison to conventional freehand screw implantation. Spine (Phila Pa 1976). 2012;37:E496–E501. [DOI] [PubMed] [Google Scholar]
- 23.Lonjon N, Chan-Seng E, Costalat V, Bonnafoux B, Vassal M, Boetto J. Robot-assisted spine surgery: feasibility study through a prospective case-matched analysis. Eur Spine J. 2016,25:947–955. [DOI] [PubMed] [Google Scholar]
- 24.Perisinakis K, Damilakis J, Theocharopoulos N, Papadokostakis G, Hadjipavlou A, Gourtsoyiannis N. Patient exposure and associated radiation risks from fluoroscopically guided vertebroplasty or kyphoplasty. Radiology. 2004;232:701–707. [DOI] [PubMed] [Google Scholar]
- 25.Keric N, Doenitz C, Haj A, et al. Evaluation of robot-guided minimally invasive implantation of 2067 pedicle screws. Neurosurg Focus. 2017;42:E11. [DOI] [PubMed] [Google Scholar]