Abstract
Background
The extent to which health care systems have adapted to the COVID-19 pandemic to provide necessary cardiac diagnostic services is unknown.
Objectives
The aim of this study was to determine the impact of the pandemic on cardiac testing practices, volumes and types of diagnostic services, and perceived psychological stress to health care providers worldwide.
Methods
The International Atomic Energy Agency conducted a worldwide survey assessing alterations from baseline in cardiovascular diagnostic care at the pandemic’s onset and 1 year later. Multivariable regression was used to determine factors associated with procedure volume recovery.
Results
Surveys were submitted from 669 centers in 107 countries. Worldwide reduction in cardiac procedure volumes of 64% from March 2019 to April 2020 recovered by April 2021 in high- and upper middle-income countries (recovery rates of 108% and 99%) but remained depressed in lower middle- and low-income countries (46% and 30% recovery). Although stress testing was used 12% less frequently in 2021 than in 2019, coronary computed tomographic angiography was used 14% more, a trend also seen for other advanced cardiac imaging modalities (positron emission tomography and magnetic resonance; 22%-25% increases). Pandemic-related psychological stress was estimated to have affected nearly 40% of staff, impacting patient care at 78% of sites. In multivariable regression, only lower-income status and physicians’ psychological stress were significant in predicting recovery of cardiac testing.
Conclusions
Cardiac diagnostic testing has yet to recover to prepandemic levels in lower-income countries. Worldwide, the decrease in standard stress testing is offset by greater use of advanced cardiac imaging modalities. Pandemic-related psychological stress among providers is widespread and associated with poor recovery of cardiac testing.
Key Words: cardiac testing, cardiovascular disease, coronavirus, COVID-19, global health
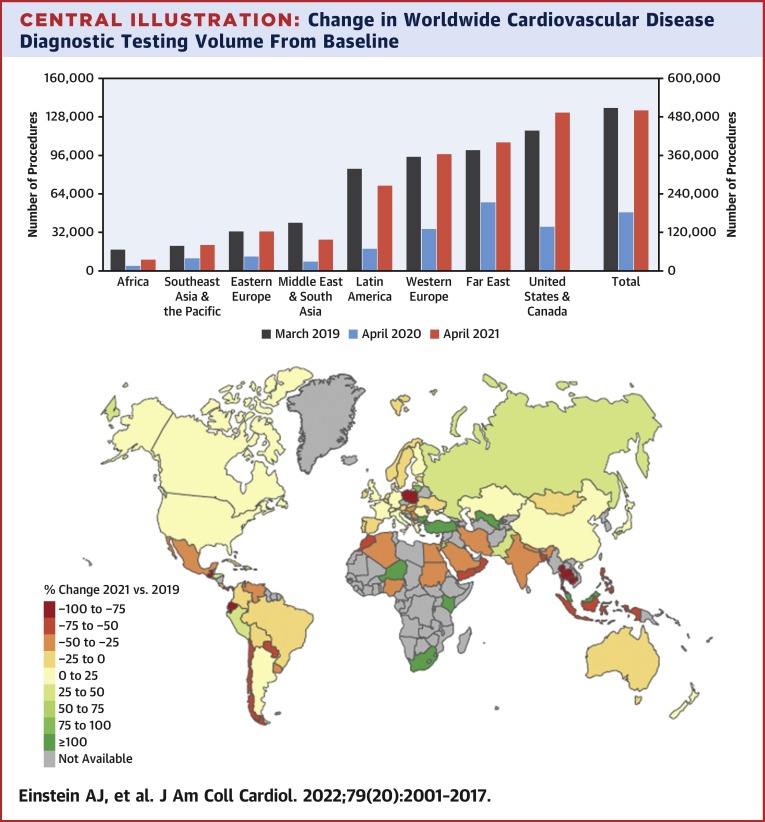
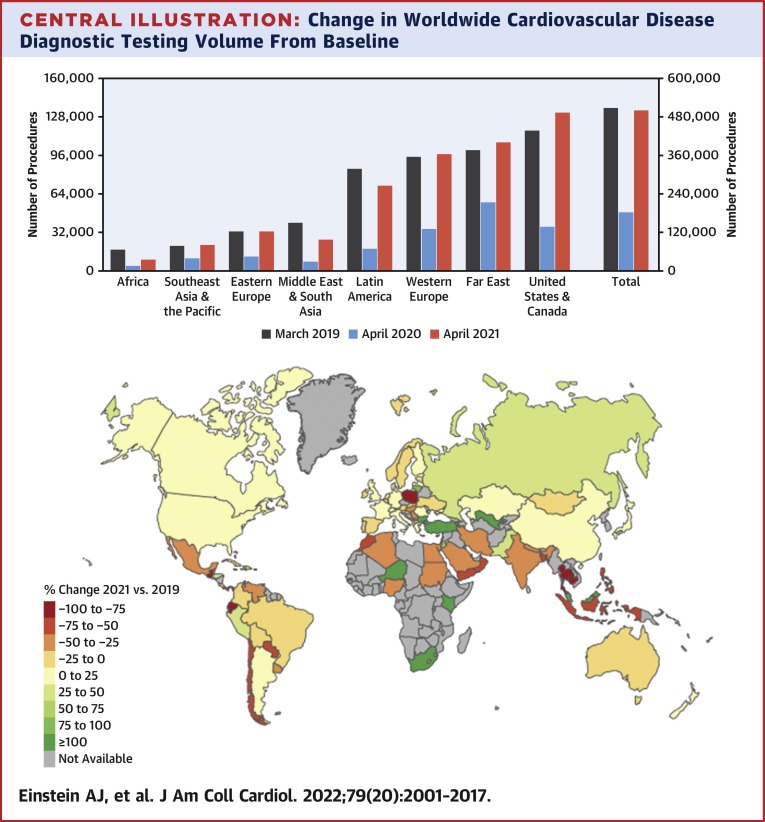
Central Illustration
The COVID-19 pandemic resulted in a sudden global disruption in the performance of diagnostic and therapeutic cardiovascular procedures in early 2020. The International Atomic Energy Agency (IAEA) Division of Human Health previously conducted a large-scale survey, INCAPS COVID (IAEA Noninvasive Cardiology Protocols COVID), to assess the initial impact of the COVID-19 pandemic on changes in noninvasive and invasive cardiovascular diagnostic procedural volumes, staff and patient exposure mitigation strategies, and plans for reopening. This initial study,1 involving >900 sites from 108 countries, quantified the significant global decrease in cardiovascular diagnostic procedure volumes from March 2019 to April 2020 and noted a greater impact of COVID-19 on practices in poorer countries, raising concerns that long-term cardiovascular outcomes may be negatively affected by the decreased availability of timely cardiovascular diagnoses and treatments.
Since the spring of 2020, health care systems have attempted to safely reopen and provide cardiovascular diagnostic testing, despite challenges related to the ongoing COVID-19 pandemic that include financial hardship, staff availability and burnout, and patient avoidance of health care contact because of fear of infection. Recovery of global cardiac testing procedural volumes since the early stages of the pandemic has not been evaluated and is of significant public health importance. Changes in cardiovascular diagnostic testing patterns and modality utilization related to the pandemic may have also occurred and have not been previously quantified. Finally, the prevalence of psychological stress related to COVID-19 on imaging staff members and its impact on subsequent patient care has not been well documented. Therefore, the INCAPS COVID investigators performed a global, web-based survey to reevaluate noninvasive and invasive cardiovascular diagnostic procedural volumes, changes in testing practice, provider well-being, and patient and staff safety practices that occurred in the year following the initial COVID-19 outbreak. Quantifying the ongoing changes in global cardiovascular diagnostic testing practices will better inform future studies aimed at determining COVID-19’s impact on long-term cardiovascular outcomes and shifts in diagnostic testing pathways in the postpandemic environment.
Methods
Study design
With the onset of the COVID-19 pandemic, the IAEA Nuclear Medicine and Diagnostic Imaging Section convened the INCAPS COVID executive committee, composed of experts in clinical cardiology and cardiac imaging from around the world, and conducted an initial study characterizing the impact of the pandemic’s first 2 months on worldwide cardiovascular diagnostic care delivery. To characterize intermediate-term trends in the use and practice of cardiac diagnostic testing, the executive committee devised and conducted a follow-up survey, INCAPS COVID 2, 1 year after the first study. We studied the following tests: transthoracic echocardiography (TTE), transesophageal echocardiography (TEE), cardiac magnetic resonance (CMR), stress testing (stress electrocardiography, echocardiography, single-photon emission computed tomography [SPECT], positron emission tomography [PET], and CMR), positron emission tomographic infection studies, coronary artery calcium scanning, coronary computed tomographic angiography (CTA), and invasive coronary angiography. We designed a questionnaire to capture information on 4 domains: 1) descriptors of participating health care facilities and health care professionals; 2) supplies of materials, practices, and protocols; 3) perceptions of psychological stress to practitioners; and 4) changes in procedural volumes.
Data were obtained from each participating site at the pre-COVID-19 baseline in March 2019 and also in April 2020 and April 2021. We used IAEA-standard country coding for 8 world regions; participating countries in each region are specified in the Supplemental Appendix. We categorized countries as low, lower middle, upper middle, and high income per World Bank classification.2
Data collection
To improve the representativeness of our data, we made many efforts to be inclusive in site participation, as detailed in the Supplemental Methods. A secure web-based platform, the International Research Integration System, was used for data collection. Only 1 entry from a given center was included in the final dataset. Entries were excluded for reasons such as missing or incomplete responses to the questionnaire. No patient-specific or confidential data were collected, and all participation by study sites was voluntary, therefore it was deemed that no external ethics committee review was required; the study complied with the Declaration of Helsinki. Moreover, the Columbia University Institutional Review Board determined that the work did not meet the criteria to be considered human-subjects research under 45 CFR 46, as there was no interaction with subjects; there was no intervention; and private, identifiable information was not collected.
Statistical analysis
Recovery rates from early-stage COVID-19-related decreases in procedure volumes were calculated as: 100% × {1 − [(March 2019 volume − April 2021 volume)/(March 2019 volume − April 2020 volume)]}. Pearson chi-square and Fisher exact tests were performed to compare center characteristics among world regions. Nonparametric statistics using Wilcoxon rank sum and Kruskal-Wallis tests with asymptotic 2-sided P values were used to compare differences in test volumes between time points and differences in continuous variables between world regions. A robust regression model using Huber’s M estimator to minimize the effect of influential outliers was used to determine factors associated with procedure volume recovery rate. Variables considered in the analysis were country income level (World Bank classification), March 2019 (baseline) procedure volume, teaching facility (vs nonteaching), hospital facility (vs nonhospital), and the rate of COVID-19 vaccinations in the country in which the facility operates (vaccinations per 100 people of the country population). Numbers of vaccinations were compiled from national governments and the World Health Organization, while population estimates used to determine rates were based on United Nations World Population Prospects, all via Our World in Data.3 Variables with P values ≤0.25 in univariable analyses were included in the multivariable model. Statistical analysis was performed using Stata/SE version 16.0 (StataCorp) and Excel 365 (Microsoft). Maps were created using the rnaturalearth and tmap packages in R version 4.0.1 (R Development Core Team).
Results
Centers
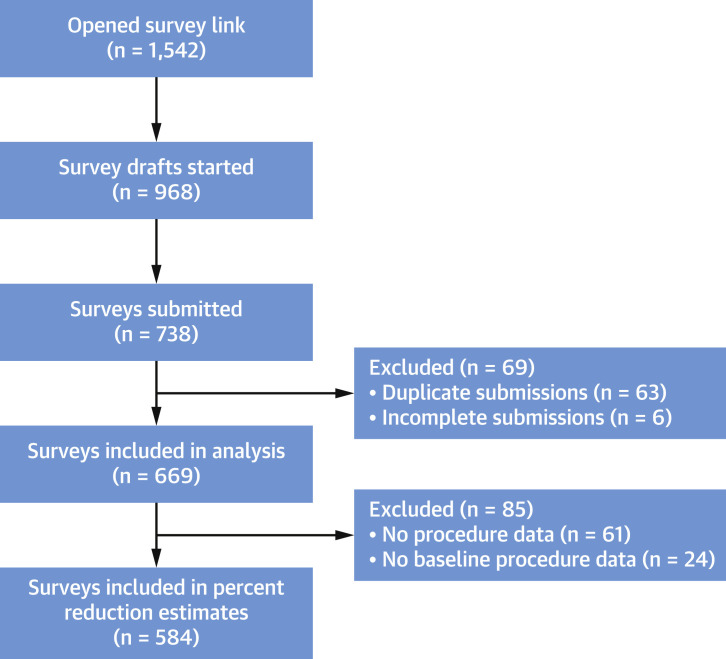
Data were obtained from 669 inpatient and outpatient centers in 107 countries, of which 584 centers in 97 countries provided suitable data on baseline 2019 procedure volumes. Of all centers, 448 (67%) were linked to sites that had participated in INCAPS COVID 1. Figure 1 details the iterative exclusion criteria applied to select the final sample, and characteristics of these centers are summarized in Table 1 . A total of 1.2 million cardiac diagnostic procedures were performed at sites during the 1-month periods considered across the 3 years (March for 2019, April for 2020 and 2021). Stress SPECT was performed at the greatest proportion of responding centers worldwide (62%), followed by coronary CTA (48%), TTE (41%), and stress electrocardiography (41%), while stress CMR (17%), positron emission tomographic infection studies (13%), and stress PET (10%) were performed in the smallest proportions (Supplemental Table 1). Countries contributing data had a combined population of 6.8 billion and more than 147 million cases of COVID-19 as of April 30, 2021, constituting 97.4% of the world’s reported cases, as of the end of the study period.
Figure 1.
Flow Diagram Detailing Survey Completion
The 8-page online survey was completed by July 25, 2021. The survey link was opened 1,542 times, which includes multiple counts for the same respondent opening it on multiple devices. Six hundred sixty-nine participants from 107 countries submitted survey data that were included in the final analysis.
Table 1.
Characteristics of Participating Centers
| Africa | Eastern Europe | Far East | Latin America | Middle East and South Asia | United States and Canada | Southeast Asia and Pacific | Western Europe | Total | P Value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of centers | 38 | 53 | 82 | 135 | 63 | 102 | 45 | 151 | 669 | |
| Participated in INCAPS COVID 1 | 24 (65) | 43 (81) | 64 (78) | 95 (70) | 29 (46) | 75 (74) | 30 (67) | 88 (58) | 448 (67) | |
| Number of countries | 14 | 21 | 7 | 19 | 15 | 2 | 9 | 20 | 107 | |
| Number of procedures | ||||||||||
| March 2019 | 17,206 | 33,021 | 100,864 | 85,450 | 40,064 | 117,085 | 21,384 | 94,376 | 509,450 | |
| April 2020 | 4,151 | 12,246 | 57,144 | 18,867 | 8,557 | 37,366 | 10,407 | 34,733 | 183,471 | |
| April 2021 | 10,057 | 33,088 | 107,682 | 71,326 | 26,694 | 132,047 | 22,187 | 96,924 | 500,005 | |
| Procedures per center | ||||||||||
| March 2019 | 100 (22-675) | 147 (37-907) | 625 (110-1,096) | 139 (61-425) | 330 (106-1,013) | 893 (328-1,738) | 133 (45-933) | 253 (89-997) | 281 (83-1,009) | <0.001 |
| April 2020 | 24 (4-125) | 17 (2-211) | 367 (95-889) | 31 (8-130) | 85 (9-245) | 327 (100-663) | 88 (13-419) | 112 (23-332) | 98 (16-368) | <0.001 |
| April 2021 | 90 (37-333) | 217 (55-985) | 784 (250-1,420) | 148 (50-353) | 240 (61-737) | 964 (326-1,938) | 168 (30-827) | 258 (112-1,002) | 296 (86-1,007) | <0.001 |
| Teaching institution | 25 (66) | 38 (72) | 63 (77) | 74 (55) | 48 (76) | 74 (73) | 33 (73) | 120 (79) | 475 (71) | 0.001 |
| Economic level by center | ||||||||||
| Low | 6 (16) | 0 (0) | 0 (0) | 0 (0) | 1 (2) | 0 (0) | 0 (0) | 0 (0) | 6 (1) | |
| Lower middle | 19 (50) | 3 (6) | 14 (17) | 4 (3) | 37 (59) | 0 (0) | 4 (9) | 0 (0) | 81 (12) | |
| Upper middle | 12 (32) | 26 (49) | 17 (21) | 125 (93) | 9 (14) | 0 (0) | 7 (16) | 2 (1) | 198 (30) | |
| Upper | 1 (3) | 24 (45) | 51 (62) | 6 (4) | 16 (25) | 102 (100) | 34 (76) | 149 (99) | 383 (57) | <0.001 |
Values are n, n (%), or median (IQR). Procedure counts are for centers performing testing in March 2019. P values are from Kruskal-Wallis tests comparing procedures and hospital beds per center among world regions and chi-square tests comparing types of center, teaching institution status, and economic level among world regions.
Changes in procedure volumes
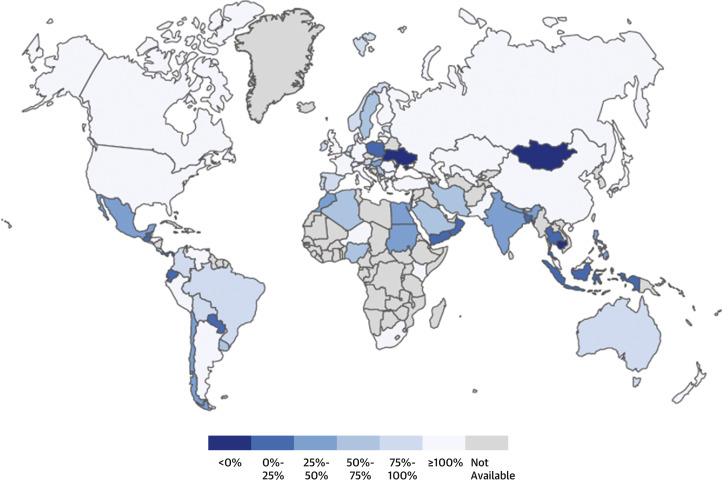
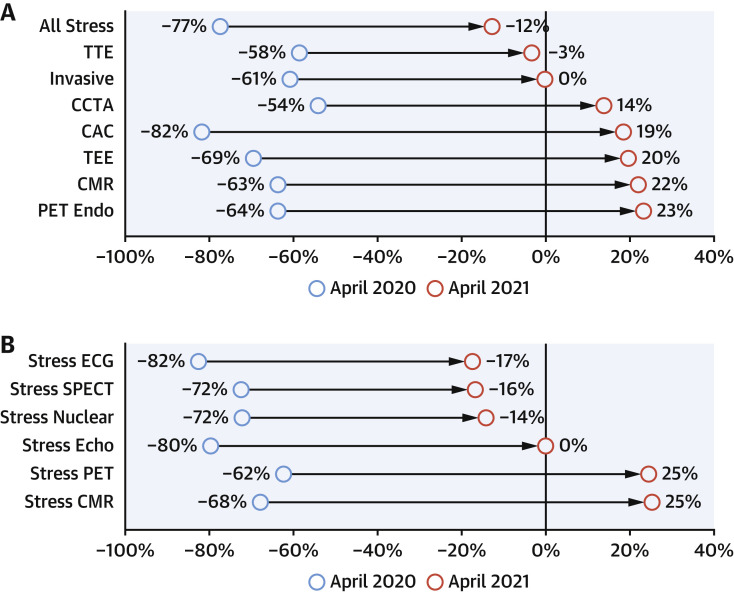
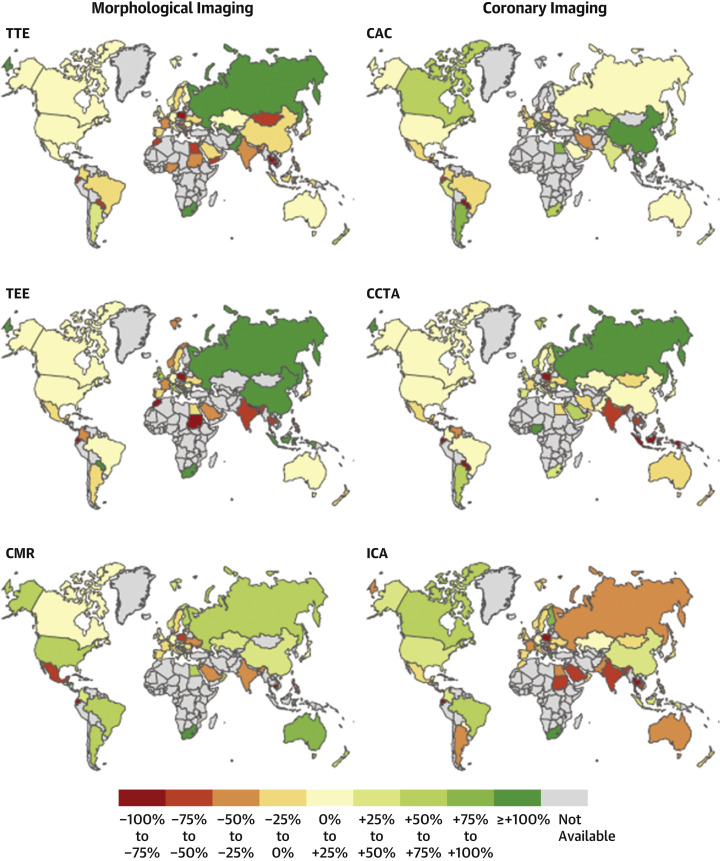
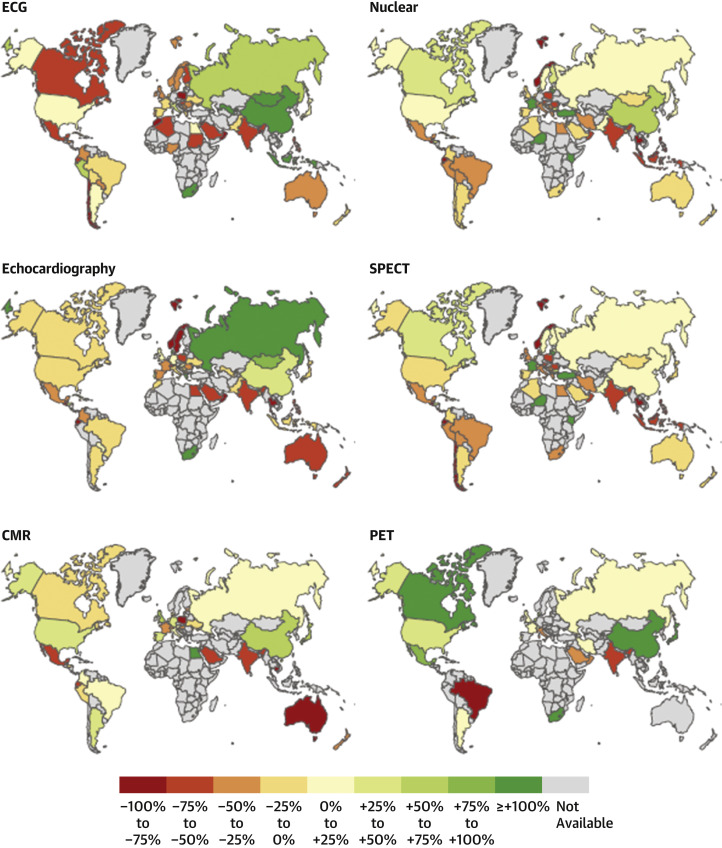
At INCAPS COVID 2 sites worldwide, cardiac diagnostic procedure volumes decreased by 64% from March 2019 to April 2020, but 97% of this decrease had recovered by April 2021, when a 2% reduction from baseline persisted (Central Illustration ). This recovery varied markedly among world regions (Supplemental Table 2) and countries (Figure 2 ). Modest (3%-13%) increases in procedure volumes from 2019 to 2021, associated with recovery rates of 105% to 119%, were observed in the Far East, Southeast Asia and the Pacific, United States and Canada, and Western Europe, and there was full recovery in Eastern Europe. In contrast, decreases persisted in Latin America (17% decrease from 2019, 79% recovery rate), Middle East and South Asia (33% decrease, 58% recovery), and Africa (42% decrease, 45% recovery). Changes in procedure volumes also varied among specific procedure types. Compared with 2019 baselines, stress tests suffered a 77% decline in 2020 and were used 12% less frequently in 2021 (Figure 3 ), corresponding to a recovery rate of 84%. In contrast, cardiac computed tomography (CT) suffered a 61% decline in 2020 compared with 2019 and was used 15% more frequently in 2021 than at baseline, with a recovery rate of 125%. Recovery of cardiac CT exceeded that of stress testing in all regions except for Eastern Europe. In comparison with 2019 baseline, by 2021 TTE (3% decrease, 95% recovery) and invasive coronary angiography (0.2% decrease, 99.7% recovery) had returned close to pre-COVID-19 volumes, whereas TEE (recovery rate 129%), CMR (135%), and PET (139%) had all recovered to modestly surpass pre-COVID-19 use. These changes were significant (P < 0.001) for all procedures. Country-wise changes in individual procedures are illustrated in Figures 4 and 5 .
Central Illustration.
Change in Worldwide Cardiovascular Disease Diagnostic Testing Volume From Baseline
(Top) Bar chart of cardiovascular disease test volumes at the 669 participating centers, by International Atomic Energy Agency world regions, for 2019 baseline, the beginning of the pandemic (April 2020), and 1 year into the pandemic (April 2021). Note different y-axes for world regions and worldwide. Percentage reductions from 2019 are reported at the tops of the columns. (Bottom) World map demonstrating changes in total cardiovascular procedural volume from March 2019 to April 2021 across the 107 participating countries. Countries or territories of a country in gray did not have data available. Procedures recorded included morphologic and other types of rest imaging (transthoracic and transesophageal echocardiography, cardiac magnetic resonance [CMR], and positron emission tomography [PET] for infective endocarditis), coronary imaging (coronary computed tomographic angiography, coronary artery calcium scoring, and invasive coronary angiography), and stress testing (stress electrocardiography, stress echocardiography, nuclear stress imaging [single-photon emission computed tomography and PET], and stress CMR). For each numerical range specified by a color, the lower limit provided is inclusive whereas the upper limit is exclusive; for example, –100 to –75 reflects a % change that is ≥–100%, but <–75%, while 75 to 100 reflects a % change that is ≥75%, but <100%.
Figure 2.
Worldwide Recovery in Cardiac Diagnostic Testing
Recovery is defined as percentage return in 2021 to 2019 baseline, from 2020 volumes at the initial phase of the pandemic. Lightest blue reflects full recovery, and darker shades of blue reflect lower recovery. For each range specified by a shade of blue in the color bar, the lower limit provided is inclusive whereas the upper limit is exclusive; for example, 0%-25% reflects a percentage recovery that is ≥0%, but <25%.
Figure 3.
Changes From Baseline Procedure Volumes
Percentage change from March 2019 baseline, for the early phase of the pandemic (April 2020; blue circles) and 1 year later (April 2021; red circles). (A) Changes for noninvasive testing procedures. (B) Changes for the different types of stress tests. CAC = coronary artery calcium scoring; CCTA = coronary computed tomographic angiography; CMR = cardiac magnetic resonance; ECG = electrocardiography; Echo = echocardiography; Nuclear = single-photon emission computed tomography and positron emission tomography combined; PET = positron emission tomography; PET Endo = positron emission tomography for infective endocarditis; SPECT = single-photon emission computed tomography; TEE = transesophageal echocardiography; TTE = transthoracic echocardiography.
Figure 4.
Worldwide Changes in Morphologic and Coronary Imaging Procedure Volumes
Maps displaying by-country estimated changes in procedure volume for common morphologic imaging (left column) and coronary imaging (right column) procedures, from prepandemic to 1 year into the pandemic. Changes as displayed are color coded on the basis of percentage change in volume from March 2019 to April 2021. For each range specified by a color in the color bar, the lower limit provided is inclusive whereas the upper limit is exclusive; for example, –100% to –75% reflects a % change that is ≥–100%, but <–75%, while +75% to +100% reflects a % change that is ≥75%, but <100%. ICA = invasive coronary angiography; other abbreviations as in Figure 3.
Figure 5.
Worldwide Changes in Stress Testing Procedure Volumes
Maps displaying by-country estimated changes in procedure volume for common cardiac stress testing procedures, from prepandemic to 1 year into the pandemic. Changes are color coded on the basis of percentage change in volume from March 2019 to April 2021. For each range specified by a color in the color bar, the lower limit provided is inclusive whereas the upper limit is exclusive; for example, –100% to –75% reflects a % change that is ≥–100%, but <–75%, while +75% to +100% reflects a % change that is ≥75%, but <100%. Abbreviations as in Figure 3.
Center capacity, practice, and protocols
Numerous changes in center capacity, practice, and protocols were observed between 2019 and 2021 (Table 2 ). These were broadly consistent worldwide, with modest differences among regions. A substantial minority of sites did at some point extend hours for cardiac diagnostic testing (32%) and add new weekend hours (23%) compared with before the pandemic, but in 2021 about one-half of these had reverted to prepandemic conditions. Nearly one-half of sites (48%) had reduced hours for cardiac diagnostic testing, but in 2021 this remained so at only 17%. Some sites had (34%) or currently have (42%) systematic approaches to rescheduling and testing patients whose studies were postponed because of the pandemic. The majority of cardiac diagnostic testing sites have used telehealth during the pandemic, including for registration and consent (58%), for remote reading or reporting of studies (50%), and/or review of studies with referring physicians (43%), and the majority of this use has persisted to the present.
Table 2.
Changes in Cardiovascular Testing Capacity, Practice, and Protocols During the COVID-19 Pandemic
| Prior Use During COVID-19 Pandemic (n = 669) | Current Use (n = 669) | |
|---|---|---|
| Change in capacity | ||
| Reduced hours compared with prepandemic | 204 (31) | 113 (17) |
| Systemic approach to rescheduling/testing patients whose studies were canceled/postponed because of pandemic | 223 (34) | 278 (42) |
| Use telehealth for patient interaction aspects (registration, consent) | 114 (17) | 269 (41) |
| Use remote reading/reporting of studies (telehealth) | 92 (14) | 239 (36) |
| Use telehealth for review of studies with referring providers | 82 (12) | 203 (31) |
| Change in practice | ||
| Test for COVID-19 in patients prior to all diagnostic testing | 143 (22) | 112 (17) |
| Test for COVID-19 in patients prior to some diagnostic testing | 134 (20) | 304 (46) |
| Change in protocols | ||
| Pharmacologic stress testing preferred over exercise to reduce risk for coronavirus transmission | 172 (26) | 233 (36) |
| Expedited imaging protocols | 140 (21) | 260 (39) |
| SPECT myocardial perfusion imaging (eg, stress-first/stress-only) | 60 (16) | 177 (47) |
| PET myocardial perfusion imaging (eg, shorter protocols) | 25 (7) | 52 (15) |
| MRI (eg, single gadolinium injection) | 41 (12) | 92 (27) |
| CT (eg, modify rate-control protocols such as increased use of prescan oral beta-blocker) | 32 (9) | 142 (41) |
| Transthoracic echocardiography (eg, focused examination) | 80 (23) | 145 (42) |
| Transesophageal echocardiography (eg, focused examination) | 69 (20) | 112 (33) |
Values are n (%). Current use reflects use at time of survey response.
CT = computed tomography; MRI = magnetic resonance imaging; PET = positron emission tomographic; SPECT = single-photon emission computed tomographic.
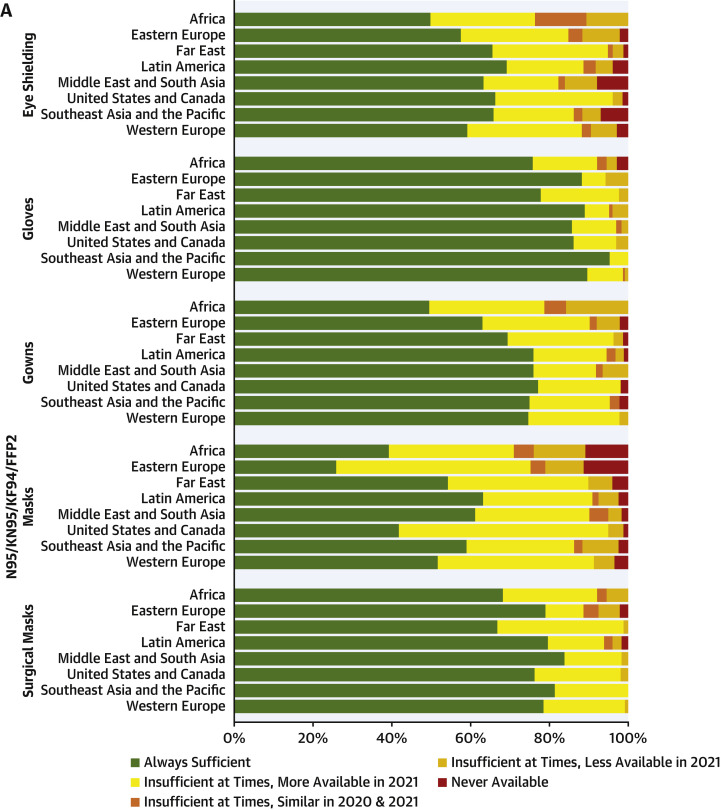
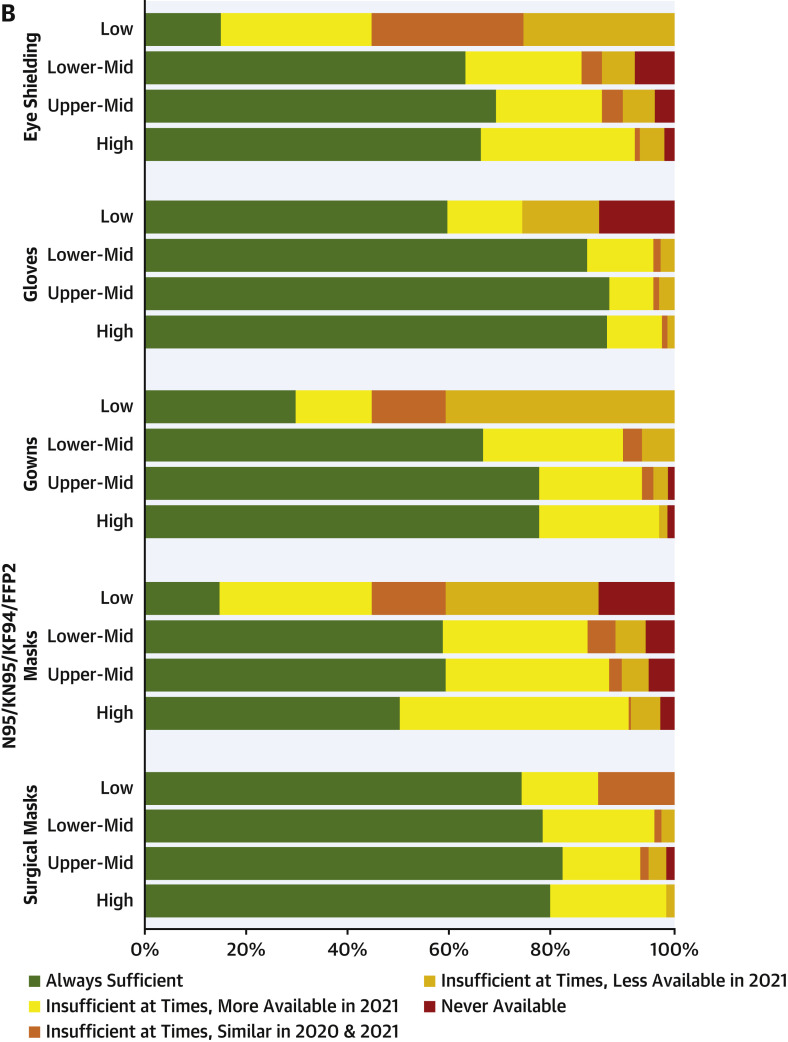
Changes in practice aimed at social distancing, such as alterations in the waiting room, limiting family members, and spacing elevators, and efforts such as mandatory masking and temperature checks, have occurred, although not uniformly, at a strong majority of sites and remained in use at the time of the survey (Table 2 ). Shortages of personal protective equipment occurred at many sites worldwide, especially in low-income countries and especially for high-filtration (N95/KN95/KF94/FFP2) masks. Protective equipment shortages in general resulted in less availability in 2020 than in 2021 (Figure 6 ).
Figure 6.
Worldwide Shortages of Personal Protective Equipment
Percentage of centers reporting types of shortage of 5 important forms of personal protective equipment during the COVID-19 pandemic. Green denotes no shortage, red denotes lack of availability throughout the pandemic, and shades of yellow/orange denote shortage at some times, with specific shade specifying whether availability was greater in 2020 or 2021. (A) By world region. (B) By World Bank income level.
Testing protocols
Imaging and catheterization protocols have also changed because of the pandemic. For example, pharmacologic stress testing was preferred during the pandemic over exercise stress testing at 62% of sites in 2020, and that remained the case at 36% of sites in 2021. Expedited imaging protocols were used during the pandemic with varying rates across testing modalities, the highest rates being for TTE (eg, focused examination; 65%) and single-photon emission computed tomographic myocardial perfusion imaging (eg, stress-first or stress-only protocol; 63%). Most of these expedited protocols remained in place at the time of the survey. As of the end of April 2021, 20% of sites worldwide required COVID-19 testing prior to stress testing in all patients, and an additional 9% of sites required such testing for nonvaccinated patients (Supplemental Table 3). Slightly lower rates of testing (16% for all, 7% for unvaccinated) were observed for noninvasive imaging, with higher rates observed for TEE (49% and 7%) and diagnostic cardiac catheterization (57% and 6%).
Staffing and impact of the pandemic on staff members
The economic crisis from COVID-19 has led to numerous changes in staffing. More than one-third of sites (n = 231 [35%]) fired or temporarily furloughed physicians or staff members or reduced salaries. These pandemic-related staffing changes occurred more frequently in 2020 (n = 200 [30%]) and had to a large degree decreased in frequency by 2021 (n = 72 [11%]). For example, while imaging staff members and physicians were furloughed at 4% and 3% of sites in 2021, an additional 17% and 12% of sites had undertaken such furloughs earlier in the pandemic.
On the basis of the estimates of survey respondents, close to 40% of cardiac diagnostic testing staff members had excess psychological stress because of the pandemic. These estimated rates were similar for physician and nonphysician staff members and across world regions (Table 3). This psychological stress was reported to affect patient care in 78% of sites, including a moderate impact at 23% of sites and a profound impact at 8% of sites. No significant difference was observed in the perceived impact of physician and other clinical staff psychological stress on patient care for facilities that perform advanced cardiac imaging modalities (ie, CT, magnetic resonance imaging, or PET) vs those that do not perform advanced imaging (P = 0.060) (Supplemental Table 4).
Table 3.
Psychological Impact of the Pandemic
| Africa | Eastern Europe | Far East | Latin America | Middle East and South Asia | United States and Canada | Southeast Asia and the Pacific | Western Europe | Worldwide | |
|---|---|---|---|---|---|---|---|---|---|
| Clinical staff estimated to have excess psychological stress related to pandemic | |||||||||
| Physician, % | 36 ± 29 | 38 ± 36 | 35 ± 30 | 46 ± 33 | 40 ± 32 | 40 ± 31 | 28 ± 35 | 29 ± 29 | 37 ± 32 |
| Nonphysician, % | 38 ± 28 | 42 ± 34 | 38 ± 33 | 48 ± 29 | 43 ± 32 | 44 ± 31 | 35 ± 37 | 33 ± 30 | 40 ± 31 |
| Impact of pandemic-related psychological stress on patient care | |||||||||
| None | 7 (19) | 17 (33) | 19 (23) | 18 (13) | 14 (22) | 16 (16) | 11 (25) | 41 (27) | 143 (22) |
| Mild | 18 (50) | 23 (44) | 38 (46) | 62 (46) | 28 (44) | 51 (51) | 22 (50) | 74 (49) | 316 (48) |
| Moderate | 9 (25) | 9 (17) | 24 (29) | 36 (27) | 17 (27) | 21 (21) | 5 (11) | 28 (19) | 149 (23) |
| Profound | 2 (6) | 3 (6) | 1 (1) | 19 (14) | 4 (6) | 12 (12) | 6 (14) | 7 (5) | 54 (8) |
Values are mean ± SD or n (%). Percentages in the bottom half of the table may not sum to 100% because of rounding.
Differences among types of centers
Procedure change and recovery rates differed among types of centers (Supplemental Table 2). Of note, outpatient imaging–only centers remained hardest hit, with a 14% reduction in procedures from 2019 to 2021, compared with hospitals, which had a 2% reduction, and outpatient facilities with physician practices, which had a 36% increase. University-affiliated teaching sites experienced lower reductions in procedures than nonteaching facilities in 2020 (62% vs 70% overall), but both types of sites nearly recovered to baseline in 2021 (recovery rates of 96% and 100%, respectively). Changes from 2019 to 2021 procedure volume (8% higher for hospitals in the highest tertile of number of beds, 4% lower for the middle tertile, and 19% lower for the lowest tertile) and recovery rates (114%, 95%, and 74%, respectively) were higher at larger hospitals than smaller ones (Supplemental Figure 1). There were no differences in procedure volume recovery or percentage of staff members with excess psychological stress related to the pandemic between sites that reported furloughs or layoffs during the pandemic and those that did not (Supplemental Table 5).
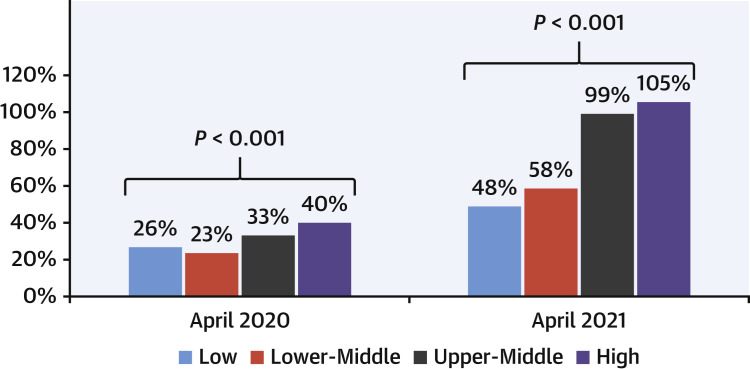
Disparities between levels of economic development
We observed significant differences in recovery of overall cardiac testing between economically challenged and wealthier countries. Although in 2020, volumes of cardiac diagnostic testing procedures decreased for all income levels, especially for low-income and lower middle-income countries, by 2021 overall diagnostic testing had recovered to pre-COVID-19 levels in high-income and upper middle-income countries, with recovery rates of 108% and 99%, respectively. However, cardiac testing remained depressed in 2021 in lower middle-income and low-income countries, at levels 58% and 48% of those before COVID-19 (Figure 7 ) and with recovery rates of 46% and 30%. However estimated excess pandemic-related psychological stress to providers was similar across levels of economic development: 38% of physicians and 39% of nonphysician providers in low-income and lower middle-income countries, compared with 37% of physicians and 41% of nonphysician providers in upper middle-income and high-income countries.
Figure 7.
Procedure Volumes Compared With 2019 Baseline, by World Bank Income Group
The bar graph demonstrates the greater effect of the pandemic on cardiac testing procedure volume on poorer countries, with a persisting reduction from March 2019 baseline in low-income and lower middle-income countries, but strong recovery in upper middle- and high-income countries
In multivariable regression, mean recovery of procedure volumes was 28% lower for facilities located in low-income or lower middle-income countries compared with facilities in upper middle- or high-income countries (95% CI: 11%-45%; P = 0.002), 0.23% lower for every 1% increase in proportion of physicians with excess psychological stress (95% CI: 0.07%-0.38%; P = 0.004), and 0.40% higher for every 1 vaccination per 100 people in the country (95% CI: 0.21%-0.60%; P < 0.001). Baseline procedure volume, teaching facility status, and hospital facility status were not significant predictors of recovery in multivariable analysis (Supplemental Table 6).
This observation of better recovery in wealthier countries was generally observed across procedure types, with some variation. For example, growth in coronary CTA from 2019 to 2021 was limited to upper middle- and high-income countries, while coronary CTA procedure volumes decreased by 23% from pre-COVID-19 levels in lower middle-income countries. TTE levels recovered to baseline in upper middle- and high-income countries but remained decreased by 41% in lower middle-income countries and by 50% in low-income countries. Moreover, abbreviated transthoracic echocardiographic protocols (eg, with fewer views), which have been used at some time during the pandemic at a majority of sites across all income levels, remained abbreviated in 2021 in a higher proportion (56%) of low- and lower middle-income sites compared with upper middle-income (44%) and high-income (37%) sites. The decline in stress testing was more profound in poorer countries, whereas PET and CMR stress testing increased from pre-COVID-19 levels in upper middle- and high-income countries. Greater proportions of sites in low-income and lower middle-income countries currently have reduced hours for cardiac testing compared with prepandemic (57% low, 36% lower middle, 26% upper middle, and 8% high income) and have used reduced hours at some point during the pandemic (71%, 70%, 61%, and 37%, respectively).
Discussion
The COVID-19 pandemic has had an immeasurable impact on the health and well-being of populations around the world, yet little is known regarding the impact of COVID-19 on diagnostic testing patterns for cardiovascular disease and other chronic diseases, during both peak and recovery phases of the pandemic. We present worldwide findings on cardiovascular diagnostic testing use from 669 inpatient and outpatient centers from 107 countries, with a combined population of 6.8 billion and nearly 98% of the world’s reported cases of COVID-19. We previously reported a reduction of 64% in cardiac diagnostic procedure volumes during the early phase of the pandemic in 2020.1 In our present report, we reveal marked recovery of most (97%) of the cardiovascular diagnostic testing procedure volume worldwide during 2021. However, patterns of recovery varied substantively across world regions and countries, with notably less robust recovery in economically challenged countries compared with wealthier countries. In 2021, recovery rates for cardiovascular diagnostic procedures continued to lag in low-income and lower middle-income countries, well behind the rest of the world, and remain depressed compared with prepandemic volumes. These important findings highlight the collateral impact of the pandemic on chronic conditions, such as cardiovascular disease, and how it has exacerbated disparities in health care for non-COVID-19 conditions worldwide. If these challenges are not assessed, the devastating effects of COVID-19 may threaten advances that have been made toward the United Nations Sustainable Development Goals.4
Disparities of diagnostic testing in lower-income countries
Throughout the pandemic, higher COVID-19 positivity rates have been reported in lower- compared with higher-income areas, likely attributable to population density and health care systems ill equipped to handle high rates of transmission, along with limited availability of testing and vaccines.5 , 6 The pandemic also created a worldwide financial crisis, with growing debt in lower-income countries and an expanded population entering poverty, intensifying issues regarding food insecurity as well as access to and funding for health care.7, 8, 9 An estimated 77% of individuals living in low-income countries live in households that have lost income during the pandemic.7 The INCAPS COVID 2 survey shows that COVID-19 has further exacerbated preexisting health inequalities in low-income and lower middle-income countries. The frequency of cardiac diagnostic testing in low-income and lower middle-income countries lagged behind upper middle- and high-income countries prior to the pandemic4 and remains depressed compared with prepandemic levels. Our analysis revealed that procedure volume recovery was 31% lower at facilities located in low- and lower middle-income countries compared with centers in upper middle- or high-income countries (P = 0.001). There is growing evidence of ongoing disruptions to essential health services in low-income and lower middle-income countries that have been caused by the ongoing pandemic, including essential health services10 and maternal and child health.11 The recent World Health Organization national pulse survey showed that high-income countries reported fewer disruptions to essential health services in January to March 2021 compared with lower income countries.10 Without mitigation of these effects, the COVID-19 pandemic will continue to exacerbate worldwide disparities in health care for noncommunicable disease, such as cardiovascular disease.
Psychological impact of the COVID-19 pandemic on health care workers
Early studies reported a variable psychological impact of the pandemic on health care workers; with more recent reports that symptoms related to post-traumatic stress are commonly occurring among medical staff members.12, 13, 14 From this INCAPS COVID 2 study, respondents reported an alarming degree of excess psychological stress related to the pandemic among both physicians and nonphysician staff members, and the perceived proportion of staff members with increased stress was a significant predictor of decreased recovery of cardiac testing (P = 0.003) in multivariable analysis. Both the acute psychological impact of the pandemic’s early phases and the chronic impact of the ongoing pandemic on health care workers must be considered.15 Several previous studies have identified high rates of depression, anxiety, post-traumatic stress disorder, and burnout among health care workers during the COVD-19 pandemic.16, 17, 18, 19, 20 In our study, there were no major regional and economic level differences in the prevalence of psychological distress, suggesting that this is a universal feature facing health care systems worldwide. The long-term impact of the pandemic on health care workers is currently unknown, and clearly prioritizing near- and long-term mental well-being is of vital importance to the health care community.
Changes in test selection and performance: emergence of advanced imaging modalities and decreased exercise stress
Beyond these findings, the worldwide growth in “advanced” cardiac imaging modalities—CT, magnetic resonance imaging, and PET—was an additional emerging pattern from our most recent survey that is as of yet unexplained. Recovery of cardiac CT exceeded that of stress testing in all regions, except for Eastern Europe. Specifically, cardiac CT suffered a 61% decline in 2020 and was used 15% more frequently in 2021 than at baseline, with a recovery rate of 125%. It remains plausible that the improved safety profile for health care providers and technologists during coronary CTA, related to decreased procedural times and lower rates of aerosolization during testing compared with stress testing,21 may be driving this increase or that acute care needs for evaluation of suspected unstable angina among patients with COVID-19 may also be affecting this testing pattern. In addition, challenges in radiotracer supply chains may also have decreased the use of stress SPECT. Another factor potentially affecting use of stress testing and other noninvasive tests is that the documented increase in acute coronary syndromes22 and delay in care during the pandemic may have led to bypassing cardiac imaging, with more patients proceeding directly to invasive procedures; however, we observed no change between 2019 and 2021 in the use of invasive angiography. Regardless, the shift to higher utilization of coronary CTA is consistent with increasing support from European and American clinical practice guidelines on management of coronary disease and chest pain.23, 24, 25
We also observed a significant and sustained decrease in the overall use of exercise stress testing. Among patients who underwent nuclear stress testing, there was a significant shift toward using pharmacologic stress following the onset of the COVID-19 pandemic. This practice, if persistent, may result in long-term decreases in the routine use of exercise stress electrocardiography, echocardiography, and SPECT. At the same time, notwithstanding decreases in stress electrocardiography (17%) and SPECT (16%) from 2019 to 2021, stress testing using PET and CMR, although at considerably lower volumes, increased by 25% over the same time period, closely matched by rest uses of these modalities. These findings are consistent with recent pre-COVID-19 trends in the U.S. Medicare population.26 Whether the worldwide decline in procedure volumes of more traditional modalities and growth of advanced cardiac imaging persist, and how these trends vary geographically, is an important subject for further study. The economic impact of continued increased use of PET, CT, and CMR, which may be more expensive tests to perform compared with traditional stress testing, requires further study across health care systems and payment models. Although in an observational registry of patients with suspected coronary disease in 41 centers in the United States and Canada, advanced imaging with PET and coronary CTA led to higher 2-year costs than did SPECT,27 driven largely by more subsequent invasive procedures, research is mixed, with PET, CT, and CMR found to be cost effective in several other studies in comparison with alternative testing pathways.28 , 29
Study limitations
As with all self-reported surveys, there is the possibility of selection and nonresponse bias, recall bias, unverified answers, and incomplete data, thus making the data collected subject to multiple potential sources of inaccuracy. The findings from the 669 centers included in the analyses may not entirely reflect centers that were not part of the study. Although sites were instructed to report reasonably accurate estimates of procedural volumes, the potential for inaccurate reporting exists. Extensive attempts were made to include as many centers as possible. Nevertheless, some countries had more respondents than others. The number of responses from low-income countries was small, partly reflecting lack of access to many of these advanced diagnostic tests in low-income countries. The pandemic continues to affect countries and regions throughout the world differently, and our survey represented 1 month when countries may have been in different phases of the pandemic. Each site’s use of cardiac testing in April 2021 may reflect to some degree the local severity of the pandemic at that time, and this was not quantified. The data on the pandemic’s impact on psychological stress were estimates reflecting perceived excess stress among physicians and nonphysician testing staff members and their impact on patient care; the influence of referring providers’ stress on the use of testing requires further study.
Conclusions
Worldwide, there has been a 97% recovery in cardiac diagnostic testing procedure volumes. However, complete recovery was observed primarily in high-income and upper middle-income countries, whereas procedure volumes in low-income and lower middle-income countries have yet to fully recover. Greater recovery rates and even new growth was observed for advanced cardiac imaging modalities: CT, MRI, and PET. The permanency of lagging recovery for other modalities, such as stress SPECT, remains unknown. Psychological stress was prevalent across providers at surveyed health care facilities and significantly affected recovery in cardiac care, necessitating greater attention to the near- and long-term impact of the COVID-19 pandemic for health care staff members around the world.
Perspectives.
COMPETENCY IN SYSTEMS-BASED PRACTICE: The COVID-19 pandemic initially reduced diagnostic testing for heart disease, and a year after the first wave of the pandemic, the situation has not improved in lower-income countries. A high level of psychological stress among practitioners attributable to the pandemic has had a negative impact on the restoration of diagnostic services.
TRANSLATIONAL OUTLOOK: Efforts are needed to mitigate the deleterious effects of the pandemic on the psychological wellness of physicians and other caregivers and to ensure timely access to diagnostic cardiac testing, especially in lower income countries.
Funding Support and Author Disclosures
Dr Williams is supported by the British Heart Foundation (FS/ICRF/20/26002). Dr Einstein has received speaker fees from Ionetix; has received consulting fees from W. L. Gore & Associates; has received authorship fees from Wolters Kluwer Healthcare – UpToDate; and has received grants or grants pending to his institution from Attralus, Canon Medical Systems, Eidos Therapeutics, GE Healthcare, Pfizer, Roche Medical Systems, W. L. Gore & Associates, and XyloCor Therapeutics. Dr Williams has received speaker fees from Canon Medical Systems. Dr Dorbala has received honoraria from Pfizer and GE Healthcare; and has received grants to her institution from Pfizer and GE Healthcare. Dr Sinitsyn has received congress speaker honoraria from Bayer, GE Healthcare, Siemens, and Philips. Dr Kudo has received research grants from Nihon Medi-physics and FUJIFILM Toyama Chemical. Dr Bucciarelli-Ducci is CEO (part-time) of the Society for Cardiovascular Magnetic Resonance; and has received speaker fees from Circle Cardiovascular Imaging, Bayer, and Siemens Healthineers. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The INCAPS COVID 2 Investigators Group, listed by name in the Supplemental Appendix, thanks cardiology and imaging professional societies worldwide for their assistance in disseminating the survey to their memberships. These include, alphabetically and not limited to, the American Society of Nuclear Cardiology, the Arab Society of Nuclear Medicine, the Australasian Association of Nuclear Medicine Specialists, the Australia-New Zealand Society of Nuclear Medicine, the Belgian Society of Nuclear Medicine, the Brazilian Nuclear Medicine Society, the British Society of Cardiovascular Imaging, the Conjoint Committee for the Recognition of Training in CT Coronary Angiography, the Consortium of Universities and Institutions in Japan, Gruppo Italiano Cardiologia Nucleare, the Indonesian Society of Nuclear Medicine, the Japanese Society of Nuclear Cardiology, the Philippine Society of Nuclear Medicine, the Russian Society of Radiology, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Thailand Society of Nuclear Medicine.
Footnotes
Listen to this manuscript's audio summary by Editor-in-Chief Dr Valentin Fuster onwww.jacc.org/journal/jacc.
Khurram Nasir, MD, MPH, served as the Guest Associate Editor for this paper. Christie Ballantyne, MD, served as the Guest Editor-in-Chief for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For a list of members of the INCAPS COVID 2 Investigators Group, supplemental methods, a supplemental figure, supplemental tables, country participation, and the data collection instrument, please see the online version of this paper.
Contributor Information
INCAPS COVID 2 Investigators Group:
Andrew J. Einstein, Diana Paez, Maurizio Dondi, Nathan Better, Rodrigo Cerci, Sharmila Dorbala, Ganesan Karthikeyan, Thomas N.B. Pascual, Leslee J. Shaw, Todd C. Villines, Joao V. Vitola, Michelle C. Williams, Yaroslav Pynda, Gerd Hinterleitner, Yao Lu, Olga Morozova, Zhuoran Xu, Cole B. Hirschfeld, Yosef Cohen, Ikenna Erinne, Eli Malkovskiy, Michael Randazzo, Lorenzo Sewanan, Mrinali Shetty, Andrew Choi, Juan Lopez-Mattei, Purvi Parwani, Artan Goda, Ervina Shirka, Salah Bouyoucef, Lydia Chelghoum, Farouk Mansouri, Abdelkader Medjahedi, Qais Naili, Mokhtar Ridouh, Diego Alasia, Lucia Alberghina, Natalia Aramayo, Diego Buchara, Franco Gabriel Busso, Jose Javier Bustos Rivadero, Jorge Camilletti, Hugo Campanelli, Roxana Campisi, Ricardo Belisario Castro, Mariana Daicz, Horacio del Riego, Laura Dragonetti, Diego Echazarreta, Juan Erriest, Fernando Faccio, Adolfo Facello, Hugo Gallegos, Ricardo Geronazzo, Horacio Glait, Victor Hasbani, Victor Jäger, Julio Manuel Lewkowicz, Jose Lotti, Neiva Maciel, Osvaldo Masoli, Edgardo Mastrovito, Maria Medus, Maria Fernanda Merani, Susana Molteni, Marcos Montecinos, Gustavo Parisi, Claudio Pereyra Sueldo, Diego Perez de Arenaza, Luis Quintana, Alejandro Radzinschi, Marcela Redruello, Marina Rodríguez, Horacio Rojas, Arturo Romero Acuña, Daniel Schere, Sonia Traverso, Gustavo Vazquez, Susana Zeffiro, Mari Sakanyan, Scott Beuzeville, Raef Boktor, Michael Crowley, D'Arne Downie, Girish Dwivedi, Barry Elison, Omar Farouque, Kim Jasper, Subodh Joshi, Joseph Lee, Kenneth Lee, Elaine Lui, Peter Mcconachie, Joanne Meaker, Dee Nandurkar, Johanne Neill, Edward O'Rourke, Patricia O'Sullivan, George Pandos, Manuja Premaratne, David Prior, Natalie Rutherford, Connor Saunders, Kim Taubman, Andrew Tauro, Andrew Taylor, James Theuerle, Paul Thomas, Jonathan Tow, Anthony Upton, Shankar Vamadevan, Victor Wayne, Eva Alina Wegner, David Wong, John Younger, Dietrich Beitzke, Gudrun Feuchtner, Oliver Sommer, Konrad Weiss, Natallia Maroz-Vadalazhskaya, Uladzimir Tserakhau, Filip Homans, Caroline M. Van De Heyning, Raúl Araujo, Valentina Soldat-Stankovic, Sinisa Stankovic, Augusto Almeida, Carlos Anselmi, Guilherme S.A. Azevedo, Marcio Sommer Bittencourt, Diego Bromfman Pianta, Estevan Cabeda, Lara Carreira, Rodrigo Cerci, Igor Coelho, Fernando de Amorim Fernandes, Andrea de Lorenzo, Roberta Delgado, Fernanda Erthal, Fabio Fernandes, Juliano Fernandes, Thiago Ferreira de Souza, Murilo Foppa, Wilson Furlan Matos Alves, Cibele Gontijo, Ilan Gottlieb, Gabriel Grossman, Maria Helena Albernaz Siqueira, Cesar Higa Nomura, Katia Hiromoto Koga, Ronaldo Lima, Rafael Lopes, Hugo Humberto Marçal Filho, Paulo Masiero, Luiz Mastrocola, Maria Eduarda Menezes de Siqueira, Claudio Mesquita, Danilo Naves, Filipe Penna, Ibraim Pinto, Thércio Rocha, Juliana Leal Rocha, Alfredo Rodrigues, Leila Salioni, Adelina Sanches, Marcelo Santos, Leonardo Sara Da Silva, Paulo Schvartzman, Cristina Sebastião Matushita, Tiago Senra, Marcelo Silva, Carlos Eduardo Soares, Bernardo Spiro, Carlos Eduardo Suaide Silva, Rafael Torres, Guilherme Urpia Monte, Andrea Vilela, Alexandre Volney Villa, Joao Vitola, Themissa Voss, Roberto Waltrick, Marcello Zapparoli, Hamid Naseer, Marina Garcheva-Tsacheva, Tiémégna Florence Ouattara, Sarameth Thou, Soley Varoeun, Gad Abikhzer, Rob Beanlands, Michael Chetrit, Dominique Dabreo, Carole Dennie, Matthias Friedrich, Mohmmed Nassoh Hafez, Kate Hanneman, Robert Miller, Anastasia Oikonomou, Idan Roifman, Gary Small, Vikas Tandon, Adwait Trivedi, James White, Katherine Zukotynski, Rita Alay, Carmen Concha, Teresa Massardo, Pedro Abad, Kelly Anzola, Harold Arturo, Luis Benitez, Alberto Cadena, Carlos Caicedo Zamudio, Antonio Calderón, Claudia T. Gutierrez Villamil, Claudia Jaimes, Juan L. Londono, Nelson Lopez, Sonia Merlano-Gaitan, Ramon Murgieitio-Cabrera, Manuel Valencia, Damiana Vergel, Alejandro Zuluaga Santamaria, Felix Solis, Tonci Batinic, Maja Franceschi, Maja Hrabak Paar, Marina Prpic, Cuba: Juan Felipe Batista, Lazaro Omar Cabrera, Amalia Peix, Yamilé Peña, Luis Manuel Rochela Vázquez, Ioannis Ntalas, Milan Kaminek, Vladimir Kincl, Otto Lang, Jawdat Abdulla, Morten Bøttcher, Martin Busk, Uka Geisler, Lars C. Gormsen, Nicolaj Hansson, Søren Hess, Jens Hove, Lars Thorbjoern Jensen, Magnus T. Jensen, Kristian Hay Kragholm, Bjarne L. Nørgaard, Kristian Øvrehus, Jan Rasmussen, Niels Peter Rønnow Sand, Hanne Sondergaard, Tomas Zaremba, Herwin Speckter, Nelson Amores, Mayra Sanchez Velez, Taghreed Abd Alrahman, Sherif Abd Elsamad, Alia Abdelfattah, Adel Allam, Sameh Elkaffas, Mona Hassan, Elshaymaa Hussein, Ahmed Ibrahim, Ahmed Kandeel, Mohamed Mandour Ali, Mahmoud Shaaban, Camila Flores, Verónica Vanesa Gómez Leiva, Anita Liiver, Martti Larikka, Valtteri Uusitalo, Denis Agostini, Clothilde Berger, Matthieu Dietz, Fabien Hyafil, Mickaël Ohana, Kevin Prigent, Hamza Regaieg, Laure Sarda-Mantel, Darach O. H-Ici, Harold Ayetey, George Angelidis, Christina Fragkaki, Chrysoula Fragkiadaki, Panagiotis Georgoulias, Maria Koutelou, Elena Kyrozi, Niki Lama, Ioannis Ntalas, Vassilis Prassopoulos, Michael Spartalis, Theodora Zaglavara, Carla Gonzalez, Goleat Gutierrez, Alejandro Maldonado, Yassine Martinez, Attila Kovács, Bálint Szilveszter, Nilesh Banthia, Vivek Bhat, Mona Bhatia, Partha Choudhury, Vijay Sai Chowdekar, Johann Christopher, Tushar Garg, Naresh Kumar Goyal, Ripen Kumar Gupta, Abhishek Gupta, Julie Hephzibah, Shashank Jain, Jesu Krupa, Parveen Kumar, Sukriti Kumar, Arati Lalchandani, Animesh Mishra, Vivaswan Dutt Mishra, Parul Mohan, Ahmad Ozair, Shivani Pandey, Ramanathapuram Parameswaran, Chetan Patel, Tapan Patel, Shivani Patel, Leena Robinson Vimala, Dr Pradosh Kumar Sarangi, Shantanu Sengupta, Arvind Sethi, Amit Sharma, Awadhesh Kumar Sharma, Punit Sharma, Apurva Shrigiriwar, Santosh Singh, Harpreet Singh, Ashwani Sood, Atul Verma, Ajay Vyas, Erwin Affandi Soeriadi, Edison Bun, Febby Hutomo, Hilman Syawaluddin, Ryan Yudistiro, Amjed Albadr, Majid Assadi, Farshad Emami, Alireza Emami-Ardekani, Saeed Farzanehfar, Ramezan Jafari, Reyhaneh Manafi-Farid, Maryam Tajik, Yoav Arnson, Shmuel Fuchs, Ronen Goldkorn, John Kennedy, Marina Leitman, Aryeh Shalev, Wanda Acampa, Domenico Albano, Pierpaolo Alongi, Gaspare Arnone, Roberta Assante, Anna Baritussio, Matteo Bauckneht, Francesco Bianco, Rachele Bonfiglioli, Francesco Bovenzi, Isabella Bruno, Andrea Bruno, Elena Busnardo, Elena Califaretti, Roberta Casoni, Vittorio Censullo, Franca Chierichetti, Marcello Chiocchi, Corrado Cittanti, Alberto Clemente, Alberto Cuocolo, Maria Luisa De Rimini, Giuseppe De Vincentis, Veronica Della Tommasina, Santo Dellegrottaglie, Paola Anna Erba, Laura Evangelista, Lara Faggi, Evelina Faragasso, Luigia Florimonte, Viviana Frantellizzi, Marco Gatti, Angela Gaudiano, Fabrizia Gelardi, Alberto Gerali, Alessia Gimelli, Marco Guglielmo, Lucia Leccisotti, Riccardo Liga, Carlo Liguori, Giampiero Longo, Margherita Maffione, Claudio Marcassa, Giovanni Matassa, Donato Mele, Elisa Milan, Luca Mircoli, Andrea Paccagnella, Sara Pacella, Federica Padovano, Dario Pellegrini, Valeria Pergola, Luca Pugliese, Natale Quartuccio, Lucia Rampin, Fabrizio Ricci, Giuseppe Rubini, Vincenzo Russo, Gianmario Sambuceti, Alessandra Scatteia, Roberto Sciagrà, Gianluca Spidalieri, Antonella Stefanelli, Carlo Tedeschi, Guido Ventroni, Dainia Baugh, Ernest Madu, Tadao Aikawa, Hiroshi Asano, Shinichiro Fujimoto, Koichiro Fujise, Yoshimitsu Fukushima, Kae Fukuyama, Yasutaka Ichikawa, Reiko Ideguchi, Nobuo Iguchi, Masamichi Imai, Hayato Ishimura, Satoshi Isobe, Kimiteru Ito, Yu Izawa, Toshiaki Kadokami, Tokuo Kasai, Takao Kato, Takashi Kawamoto, Shigeru Kiryu, Shinichiro Kumita, Osamu Manabe, Hirotaka Maruno, Naoya Matsumoto, Masao Miyagawa, Masao Moroi, Shigeki Nagamachi, Kenichi Nakajima, Ryo Nakazato, Mamoru Nanasato, Masanao Naya, Takashi Norikane, Yasutoshi Ohta, Yoichi Otomi, Hideki Otsuka, Noriko Oyama-Manabe, Masaki Saito, Masayoshi Sarai, Junichi Sato, Daisuke Sato, Shinya Shiraishi, Kentaro Takanami, Kazuya Takehana, Yasuyo Taniguchi, Hiroki Teragawa, Nobuo Tomizawa, Kyoko Umeji, Yasushi Wakabayashi, Shinichiro Yamada, Shinya Yamazaki, Tatsuya Yoneyama, Mohammad Rawashdeh, Tairkhan Dautov, Khalid Makhdomi, Mostafa Abass, Masoud Garashi, Qaisar Siraj, Marika Kalnina, Mohamad Haidar, Renata Komiagiene, Giedre Kviecinskiene, Donatas Vajauskas, Noor Khairiah A. Karim, Mady Doucoure, Luise Reichmuth, Anthony Samuel, Mohamed Lemine Dieng, Ambedhkar Shantaram Naojee, Estrella Aguilera Hernandez, Cesar Rene Alducin Tellez, Erick Alexánderson-Rosas, Erika Barragan, Manuel Cabada, Daniel Calderón, Isabel Carvajal-Juarez, José Esparza, Manlio Gerardo Gama-Moreno, Virginia Garcia Quinto, Nelsy Coromoto Gonzalez, Mary Carmen Herrera-Zarza, Aloha Meave, Jesus Gregorio Medina Verdugo, Gabriela Melendez, Rafael Humberto Morales Murguia, Carlos Salvador Navarro Quiroz, Mario Ornelas, Andres Preciado-Anaya, Oscar Ulises Preciado-Gutiérrez, Adriana Puente, Aristóteles Ramírez Salazar, Sandra Graciela Rosales Uvera, Sandra Rosales-Uvera, Jose Antonio Serna Macias, Lilia Sierra-Galan, Lilia M. Sierra-Galan, Juan Carlos Tirado Alderete, Enrique Vallejo, Marc Faraggi, Erdenechimeg Sereegotov, Nouzha Ben Rais, Nadia Ismaili Alaoui, Thiri Kyiphyu, Su Thet Oo, Soe Myat Win, Htin Zar, Ram Ghimire, Madhu Neupane, Andor Glaudemans, Riemer Slart, Derk Verschure, Berry Allen, John Edmond, Clare Mckenzie, Stuart Tie, Niels Van Pelt, Kirsten Worthington, Calum Young, Idrissa Adamou Soli, Shehu Kana, Uchenna Onubogu, Mahmoud Sani, Anders Tjellaug Bråten, Arve Jørgensen, Hanne-Elin Vassbotn, Humoud Al Dhuhli, Zabah Jawa, Naima Tag, Shazia Fatima, Muhammad Babar Imran, Muhammad Numair Younis, Mohammad Saadullah, Yariela Herrera Malo, Dora Lenturut-Katal, Manuel Castillo, José Ortellado, Afroza Akhter, F. Aaysha Cader, Raihan Hussain, Saidur Rahman Khan, Tapati Mandal, Faria Nasreen, Yunqiang An, Dianbo Cao, Lianggeng Gong, Yang Hou, Chongfu Jia, Tao Li, Caiying Li, Hui Liu, Wenya Liu, Jinkang Liu, Bin Lu, Ming-Yen Ng, Heshui Shi, Chunxiang Tang, Ximing Wang, Zhaoqian Wang, Yining Wang, Jiang Wu, Yan Yi, Li Yuan, Tong Zhang, Longjiang Zhang, Edith Chavez, Carlos Cruz, Christian Llontop, Rosanna Morales, Paz Abrihan, Asela Bustos-Barroso, Michele Duldulao-Ogbac, Christopher Eduarte, Jerry Obaldo, Alvin Quinon, Belinda San Juan, Carlo Joe San Juan, Marie Rhiamar Sauler-Gomez, Mila Uy, Magdalena Kostkiewicz, Jolanta Kunikowska, Anna Teresinska, Tomasz Urbanik, Nuno Bettencourt, Ricardo Fontes-Carvalho, Cristina Gavina, Lino Gonçalves, Filipe Macedo, Nuno Moreno, Carla Sousa, Ana Teresa Timoteo, Maria João Vidigal, Mahmoud Al Heidous, Subramaniyan Ramanathan, Samer Arnous, Said Aytani, Angela Byrne, Tadhg Gleeson, David Kerins, Julie O'Brien, Ji-In Bang, Henry Bom, Miju Cheon, Gi Jeong Cheon, Sang-Geon Cho, Chae Moon Hong, Yong Hyu Jeong, Won Jun Kang, Yeon-Koo Kang, Ji-Young Kim, So Won Oh, Young So, Ho-Chun Song, Kyoung Sook Won, Soo Woong Yoo, Irena Mitevska, Marija Vavlukis, Barbara Gužic Salobir, Monika Štalc, Theodora Benedek, Marian Pop, Claudiu Stan, Alexey Ansheles, Olga Dariy, Nina Gagarina, Irina Itskovich, Anatoliy Karalkin, Alexander Kokov, Gulya Marina, Ekaterina Migunova, Viktor Pospelov, Daria Ryzhkova, Guzaliya Sayfullina, Vladimir Sergienko, Irina Shurupova, Valentin Sinitsyn, Margarita Vakhromeeva, Nailia Valiullina, Konstantin Zavadovsky, Kirill Zhuravlev, Rami Abazid, Turki Al Garni, Mirvat Alasnag, Ahmed Aljizeeri, Hamid Amer, Ahmad Amro, Hesham Hamdy, Osama Smettei, Dragana Sobic Saranovic, Marina Vlajkovic, Felix Keng, Jason See, Zuzana Berecova, Jana Polakova Mistinova, Osayande Evbuomwan, Nerisha Govender, Jonathan Hack, Bawinile Hadebe, Khanyisile Hlongwa, Mitchell Kaplan, Hoosen Lakhi, Katarina Milos, Moshe Modiselle, Stuart More, Ntanganedzeni Muambadzi, Leonie Scholtz, Manuel Barreiro-Perez, Isabel Blanco, Jordi Broncano, Alicia Camarero, Irene Casáns-Tormo, Javier De Haro, Albert Flotats, Elia García, Ceferino Gutierrez Mendiguchia, Amelia Jimenez-Heffernan, Ruben Leta, Javier Lopez Diaz, Luis Lumbreras Vega, Ana Manovel-Sánchez, Amparo Martinez Monzonis, Bianca Patrut, Virginia Pubul, Ricardo Ruano Perez, Nahla Zeidan, Damayanthi Nanayakkara, Ahmed Suliman, Henrik Engblom, Mustafa Murtadha, Ellen Ostenfeld, Magnus Simonsson, Hatem Alkadhi, Ronny Ralf Buechel, Peter Burger, Christoph Gräni, Christel Kamani, Nadine Kawel-Böhm, Bernd Klaeser, Robert Manka, John Prior, Tawika Kaewchur, Benjapa Khiewvan, Arpakorn Kositwattanarerk, Sirianong Namwongprom, Tanyaluck Thientunyakit, Haluk Burcak Sayman, Mahmut Yüksel, Mugisha Julius Sebikali, Emmy Okello, Pavlo Korol, Iryna Noverko, Maryna Satyr, Tahir Ahmad, Khaled Alfakih, Ivo Andrade, Susan Buckingham, Anda Bularga, John-Paul Carpenter, Graham Cole, David Cusack, Sarojini David, Patrick Davis, Timothy Fairbairn, Arjun Ghosh, Prasad Guntur Ramkumar, Mark Hamilton, Faisal Haque, Benjamin Hudson, Annette Johnstone, V.J. Karthikeyan, Mike Kay, Mohammad Ali Khan, Jamie Kitt, Chen Sheng Low, Elisa Mcalindon, David Mccreavy, Brian Morrissey, Manish Motwani, Dilip Na, Edward Nicol, Dilip Patel, Jonathan Rodrigues, Chris Rofe, Rebecca Schofield, Thomas Semple, Azeem Sheikh, Apurva Sinha, Deepak Subedi, William Topping, Katherine Tweed, Stephen Richard Underwood, Jonathan Weir-Mccall, Hamed Zuhairy, Taimur Abbasi, Shady Abohashem, Sandra Abramson, Mouaz Al-Mallah, Mohan Ashok Kumar, Mallory Balmer-Swain, Daniel Berman, Adam Bernheim, Sabha Bhatti, Robert Biederman, Erik Bieging, Scott Bingham, Stephen Bloom, Sean Blue, Andressa Borges, Kelley Branch, Paco Bravo, Sujatha Buddhe, Matthew Budoff, Renée Bullock-Palmer, Michael Cahill, Candace Candela, Jane Cao, Saurav Chatterjee, Yiannis Chatzizisis, Nita Ray Chaudhuri, Michael Cheezum, Anjali Chelliah, Tiffany Chen, Marcus Chen, Lu Chen, Andrew Choi, Aalap Chokshi, Jina Chung, Sorin Danciu, William DeSisto, Michael Dilorenzo, Rami Doukky, William Duvall, Maros Ferencik, Cameron Foster, Anthon Fuisz, Michael Gannon, David German, Myron Gerson, Jeffrey Geske, Fadi Hage, Agha Haider, Sofia Haider, Yasmin Hamirani, Karen Hassen, Robert Hendel, Jacqueline Henkel, Stephen Horgan, Mark Hyun, Rajesh Janardhanan, Scott Jerome, Dinesh Kalra, David Kassop, Mona Kinkhabwala, George Kinzfogl, Bernard Koch, Lynne Koweek, Joseph Krepp, Younghoon Kwon, Jay Layer, John Lesser, Steve Leung, Bernadette Lisske, Juan Lopez-Mattei, Kathleen Magurany, Jeremy Markowitz, Brenda Mccullough, Azita Moalemi, Chanan Moffitt, Juan Montanez, Warren Moore, Shamil Morayati, Mahmud Mossa-Basha, Zorana Mrsic, Venkatesh Murthy, Prashant Nagpal, Katarina Nelson, Prabhjot Nijjar, Rupal O’Quinn, Purvi Parwani, Edward Passen, Toral Patel, Pravin Patil, Amit Pursnani, Nancy Quachang, Mark Rabbat, Pragya Ranjan, Patricia Rodriguez Lozano, Mary Schemmer, Rebecca Seifried, Nishant Shah, Amee Shah, Sujata Shanbhag, Gaurav Sharma, Robert Skotnicki, Michael Sobczak, Prem Soman, Vincent Sorrell, Monvadi Srichai, Jim Streeter, Leah Strickland, Suliman Suliman, Naghmeh Tebyanian, Dustin Thomas, Randall Thompson, Seth Uretsky, Srikanth Vallurupalli, Marian Vandyck-Acquah, Vikas Verma, Todd Villines, Joseph Weinstein, David Wolinsky, Karolina Zareba, Michael Zgaljardic, Mario Beretta, Rodolfo Ferrando, Miguel Kapitan, Fernando Mut, Omoa Djuraev, Gulnora Rozikhodjaeva, Luisa Vera, Binh Duong Duc, Xuan Canh Nguyen, and Phuoc Minh Hiep Nguyen
Appendix
References
- 1.Einstein A.J., Shaw L.J., Hirschfeld C., et al. International impact of COVID-19 on the diagnosis of heart disease. J Am Coll Cardiol. 2021;77:173–185. doi: 10.1016/j.jacc.2020.10.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Bank Data Team World Bank country and lending groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups Available at:
- 3.Mathieu E., Ritchie H., Ortiz-Ospina E., et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5:947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 4.United Nations UN/DESA Policy Brief #81: impact of COVID-19 on SDG progress: a statistical perspective. https://www.un.org/development/desa/dpad/publication/un-desa-policy-brief-81-impact-of-covid-19-on-sdg-progress-a-statistical-perspective/ Available at:
- 5.Thienemann F., Pinto F., Grobbee D.E., et al. World Heart Federation briefing on prevention: coronavirus disease 2019 (COVID-19) in low-income countries. Glob Heart. 2020;15:31. doi: 10.5334/gh.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steinhauser G., Shah S. Poor countries ask wealthy ones to do more to stave off COVID-19 surge. https://www.wsj.com/articles/poor-countries-ask-wealthy-ones-to-do-more-to-stave-off-covid-19-surge-11621602003 Available at:
- 7.Josephson A., Kilic T., Michler J.D. Socioeconomic impacts of COVID-19 in low-income countries. Nat Hum Behav. 2021;5:557–565. doi: 10.1038/s41562-021-01096-7. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Global Leadership Coalition. COVID-19 brief: impact on the economies of low-income countries. https://www.usglc.org/coronavirus/economies-of-developing-countries/ Available at:
- 9.Nishio A. COVID-19 is hitting poor countries the hardest. Here’s how World Bank’s IDA is stepping up support. https://blogs.worldbank.org/voices/covid-19-hitting-poor-countries-hardest-heres-how-world-banks-ida-stepping-support Available at:
- 10.World Health Organization Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1 Available at:
- 11.Roberton T., Carter E.D., Chou V.B., et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8:e901–e908. doi: 10.1016/S2214-109X(20)30229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cabarkapa S., Nadjidai S.E., Murgier J., Ng C.H. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: a rapid systematic review. Brain Behav Immun Health. 2020;8:100144. doi: 10.1016/j.bbih.2020.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Kock J.H., Latham H.A., Leslie S.J., et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21:104. doi: 10.1186/s12889-020-10070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prasad K., McLoughlin C., Stillman M., et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: a national cross-sectional survey study. EClinicalMedicine. 2021;35:100879. doi: 10.1016/j.eclinm.2021.100879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehta S., Machado F., Kwizera A., et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med. 2021;9:226–228. doi: 10.1016/S2213-2600(21)00068-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lai J., Ma S., Wang Y., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carmassi C., Foghi C., Dell’Oste V., et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 2020;292:113312. doi: 10.1016/j.psychres.2020.113312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Couarraze S., Delamarre L., Marhar F., et al. The major worldwide stress of healthcare professionals during the first wave of the COVID-19 pandemic—the international COVISTRESS survey. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0257840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saragih I.D., Tonapa S.I., Saragih I.S., et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. 2021;121:104002. doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zoghbi W.A., DiCarli M.F., Blankstein R., et al. Multimodality cardiovascular imaging in the midst of the COVID-19 pandemic: ramping up safely to a new normal. J Am Coll Cardiol Img. 2020;13:1615–1626. doi: 10.1016/j.jcmg.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Knuuti J., Wijns W., Saraste A., et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–477. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 24.Collet J.P., Thiele H., Barbato E., et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289–1367. doi: 10.1093/eurheartj/ehaa575. [DOI] [PubMed] [Google Scholar]
- 25.Gulati M., Levy P.D., Mukherjee D., et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78(22):e187–e285. doi: 10.1016/j.jacc.2021.07.053. [DOI] [PubMed] [Google Scholar]
- 26.Reeves R.A., Halpern E.J., Rao V.M. Cardiac imaging trends from 2010 to 2019 in the Medicare population. Radiol Cardiothorac Imaging. 2021;3 doi: 10.1148/ryct.2021210156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hlatky M.A., Shilane D., Hachamovitch R., Dicarli M.F. for the SPARC Investigators. Economic outcomes in the Study of Myocardial Perfusion and Coronary Anatomy Imaging Roles in Coronary Artery Disease registry: the SPARC study. J Am Coll Cardiol. 2014;63:1002–1008. doi: 10.1016/j.jacc.2013.11.038. [DOI] [PubMed] [Google Scholar]
- 28.Trägårdh E., Tan S.S., Bucerius J., et al. Systematic review of cost-effectiveness of myocardial perfusion scintigraphy in patients with ischaemic heart disease: a report from the cardiovascular committee of the European Association of Nuclear Medicine. Endorsed by the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2017;18:825–832. doi: 10.1093/ehjci/jex095. [DOI] [PubMed] [Google Scholar]
- 29.Terpenning S., Stillman A. Cost-effectiveness for imaging stable ischemic disease. Br J Radiol. 2020;93:20190764. doi: 10.1259/bjr.20190764. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.