Abstract
Background
The COVID-19 pandemic has shifted mental health care delivery to digital platforms, videoconferencing, and other mobile communications. However, existing reviews of digital health interventions are narrow in scope and focus on a limited number of mental health conditions.
Objective
To address this gap, we conducted a comprehensive systematic meta-review of the literature to assess the state of digital health interventions for the treatment of mental health conditions.
Methods
We searched MEDLINE for secondary literature published between 2010 and 2021 on the use, efficacy, and appropriateness of digital health interventions for the delivery of mental health care.
Results
Of the 3022 records identified, 466 proceeded to full-text review and 304 met the criteria for inclusion in this study. A majority (52%) of research involved the treatment of substance use disorders, 29% focused on mood, anxiety, and traumatic stress disorders, and >5% for each remaining mental health conditions. Synchronous and asynchronous communication, computerized therapy, and cognitive training appear to be effective but require further examination in understudied mental health conditions. Similarly, virtual reality, mobile apps, social media platforms, and web-based forums are novel technologies that have the potential to improve mental health but require higher quality evidence.
Conclusions
Digital health interventions offer promise in the treatment of mental health conditions. In the context of the COVID-19 pandemic, digital health interventions provide a safer alternative to face-to-face treatment. However, further research on the applications of digital interventions in understudied mental health conditions is needed. Additionally, evidence is needed on the effectiveness and appropriateness of digital health tools for patients who are marginalized and may lack access to digital health interventions.
Keywords: digital health, telepsychology, computer-assisted therapy, online therapy, mobile applications, mobile apps, telemedicine, telepsychiatry, virtual reality exposure therapy, mental health, COVID-19
Introduction
Patients with mental health conditions often experience long-term disability, resulting from challenges in accessing mental health services, including low treatment availability and long wait times [1]. Moreover, the COVID-19 pandemic has exposed crucial gaps in mental health care systems, which significantly impact the well-being of many people globally [2-4]. Increased fears of contracting SARS-CoV-2, the burden of quarantine requirements, social distancing, social isolation, rising economic inequities, unemployment, and new workplace requirements are additional stressors brought on by the pandemic, which can exacerbate the symptoms of mental health conditions [5-14]. The pandemic is thought to account for recent increases in mood, anxiety, trauma, and substance use disorders [10-16]. Similar trends in mental illness were observed during the 2003 severe acute respiratory syndrome outbreak, other previous pandemics [10-12,17,18], and recent economic crises [10-12,17,18]. The rise in mental health issues due to the COVID-19 pandemic creates substantial pressures on an already strained mental health care system [12,19], with evidence pointing to a silent mental health crisis as resources are prioritized for stemming the spread of SARS-CoV-2 infections [12].
Consequently, interest in web-based health service delivery has been growing in recent years. These include synchronous and asynchronous therapist contact via messaging, phone call, and videoconferencing; computer, web-based, and mobile delivery of therapy programs; virtual or augmented reality–based programs; computerized or web-based cognitive training, and web-based peer and social support groups (defined below). The global reach of digital health care potentially extends to billions of people with internet access. Web-based and mobile delivery of therapy programs may save practitioner time owing to efficient and effective delivery of treatments at lower associated cost [20]. Digital health interventions may also offer a way to reduce or avert care interruptions while allowing practitioners to adhere to safe social distancing measures [20]. At the onset of the COVID-19 pandemic, health care providers rapidly transitioned to web-based health care delivery to limit the risk of COVID-19 transmission. However, the state of the evidence on the effectiveness of digital interventions is unclear, and the implications for health outcomes of such a drastic shift to digital health platforms are difficult to predict [12,21-25]. Whether clinicians can provide effective and reliable treatment, perform assessments [26,27], identify ailments and symptoms [28], manage suicidal behaviors [26,28,29], and provide personable, compassionate services [26,30,31] remains uncertain. Furthermore, digital delivery of services may be complicated by the symptomatology of some mental health conditions [26,29], concurrent medical conditions [29], and socioeconomic factors [31-42]. A lack of information, resources, and understanding of complex patient-related factors could negatively affect care delivery and overall patient health.
Mobile apps are increasingly used by the public for the treatment of mood and anxiety disorders, sometimes without professional referral or guidance [13,43,44]. There is also some evidence that web-based forums and resources are increasingly common [45-54]. Similarly, over the past decade, there have been noticeable shifts in the provision of cognitive and behavioral training for developmental disorders and dementia to computer and other web-based platforms [55-64]. There are also significant developments in the application of virtual reality tools in health care settings [65-67]. The need for professional guidance in the use of web-based or mobile services and forums is subject to controversy [68-77], and more evidence is needed on optimal ways to integrate these tools into a comprehensive approach to mental health care.
This review is motivated primarily by questions from health care stakeholders in a Canadian setting, who were required to rapidly shift to digital delivery of mental health services during the COVID-19 pandemic. However, to date, there has been no comprehensive review on the use of digital interventions for the treatment of a representative range of mental health conditions. With the present meta-review, we seek to fill this gap and summarize existing evidence on the use of digital health interventions in mental health care. Our hope is that our review will be used by health care stakeholders to inform their consideration of mental health care options for digital delivery.
Methods
Literature Search
We conducted a review of peer-reviewed literature examining the application of digital health interventions for the treatment of mental health conditions described below. We searched Medline on November 1, 2021, for research published after January 1, 2010. We used Medline filters to restrict retrieved records to meta-analyses, systematic reviews, and other types (narrative and conceptual) of literature reviews. We used broad term definitions to maximize the types of digital health interventions and mental health conditions captured in the search. The search strategy consisted of combinations of Medical Subject Headings (MeSH) words and other keywords including the following: virtual reality; telemedicine; computer-assisted therapy; digital health; videoconferencing; mental health; mental health services; psychotherapy; attention deficit and disruptive behavior disorders; anxiety disorders; trauma and stressor related disorders; mood disorders; bipolar and related disorders; dementia; disruptive, impulse control and conduct disorders; dissociative disorders; feeding and eating disorders; neurodevelopmental disorders; neurotic disorders; pain; personality disorders; schizophrenia spectrum and other psychotic disorders; sleep wake disorders; and substance-related disorders (see search query in Multimedia Appendix 1).
Inclusion and Exclusion Criteria
This review is restricted to other reviews that assessed the use of digital interventions for the treatment of mental health conditions. Studies that did not report on the effectiveness of digital interventions on mental health outcomes or did not outline a study protocol were excluded from this review.
Data Extraction, Analysis, and Quality Assessment
Once records were retrieved and deduplicated, TJP, NS, and AJ conducted title and abstract screening where any disagreements were resolved through consensus. Team members then proceeded with mutually exclusive full-text screening to identify articles that qualified for inclusion in the review. As with previous meta-reviews, adherence to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [78] was considered to assess risk of bias in selected studies (maximum score of 1: completely adheres to PRISMA Guidelines). To assess the quality and reliability of research within the field, one reviewer conducted data extraction using a standardized and iterative data extraction form (Multimedia Appendix 2). Extracted data included study details (author, date, and type), participant characteristics (mental health conditions), intervention details (intervention type and effectiveness), number of participants, and controls used (treatment as usual, waitlist, placebo, or not applicable). Quality and bias scores describing the primary literature reported in included studies were averaged and faithfully converted (when necessary) to a consistent 3-point scale (1=low, 2=moderate, and 3=high). Owing to the significant heterogeneity in research approaches and findings, we selected a qualitative and semiquantitative approach to summarize and present research findings.
Organization of Mental Health Conditions
To provide a clearer picture of how digital interventions are used in treating various mental health conditions, we separated mental health conditions based on the parent MeSH terms and Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria. Where we identified dissimilarities or similarities in treatment, we either added a subcategory or combined categories together. We removed attention-deficit/hyperactivity disorder (ADHD) from developmental disorders and added it as a separate category owing to dissimilarities in the treatment and management of this condition versus other developmental disorders. We combined the frequently comorbid anxiety, mood, and trauma disorders owing to similar treatment approaches, effectiveness, and reporting in the literature. Additionally, patients with chronic pain, chronic medical illnesses, and chronic disabilities (shortened to chronic illnesses) often experience mental health issues that are underrecognized, receive little attention within digital health intervention literature [79-83], and have unreliable treatment efficacies [79-83]. Despite the use of similar psychological treatments anxiety, mood, and trauma disorders [84-87], chronic illness treatments also involve acceptance, remediation, music, and virtual reality [79-82,84-86]. We therefore retain chronic illness as a category related to but separate from anxiety, mood, and trauma disorders. Similarly, caregivers are often untrained family members who face significant stress and anxiety in the process of providing care for loved ones. Caregivers also benefit from mental health services such as cognitive behavioral therapy and specific psychoeducation, which overlap with some mental health conditions. but also benefit from peer support, training, and acceptance therapy [70,88-95]. Substance use disorder was included since treatments include therapies based on psychological principles [32,78,96-115], and this disorder is often comorbid with other mental health disorders and is considered a mental health condition by medical associations (eg, Canadian Medical Association, American Medical Association, and World Health Organization) and diagnostic manuals (eg, DSM-5).
This review adheres to PRISMA guidelines [116] (Multimedia Appendix 1).
Results
Included Studies
The PRISMA flowchart of the screening process is presented in Figure 1. We identified 3051 records and used Medline selection tools to exclude primary articles (n=2510), and studies published before 2010 (n=42). Of the remainder, 4 were inaccessible and authors did not respond to copy requests; thus, 466 studies proceeded to full-text review where 159 were excluded for not reporting on intervention effectiveness and 3 were proposals. This selection resulted in 77 meta-analyses, 84 systematic reviews, and 143 literature reviews examining the use of digital health interventions for the treatment of mental health conditions.
Figure 1.
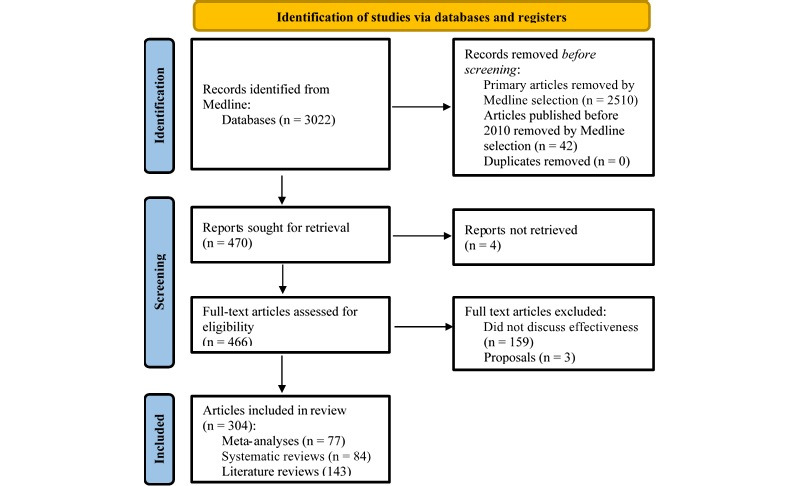
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart for study selection.
Mental Health Conditions
A summary of metadata extracted from database searches, curated secondary literature, curated primary literature, and participant numbers is provided in Table 1. Per participant, studies on substance use disorders account for a majority (n=241,377, 52%) of digital mental health research, followed by mood, anxiety, and trauma disorders (136,121, n=29%), and >5% for other mental health conditions (pain: n=24,327, schizophrenia: n=20,500, dementia: n=10,823, feeding and eating: n=10,441, developmental: n=8736, bipolar: n=3573, sleep-wake: n=3333; and ADHD: n=2428). Additionally, limited research has examined the use of digital health to provide psychological support to caregivers of people with dementia and developmental disorders. Lastly, we retrieved no records examining the use of digital health interventions to treat antisocial, avoidant, borderline, dependent, histrionic, and narcissistic personality, dissociative identity, paraphilic, and sexual health disorders. To demonstrate how the amount and reliability of research can be estimated from metadata, we correlated elements in Table 1 and report a 4D correlation (P<.05; see Table S2 and 4D illustration in Figure S1 in Multimedia Appendix 1). Overall, this illustrates a significant need for the development and testing of digital interventions for other mental health conditions. Nevertheless, the number of research publications has steadily increased since 2015 (Figure 2)—a trend that will likely continue with greater interest in digital mental health research.
Table 1.
Metadata per mental health condition examining article and participant numbers.
| Mental health conditions | Total literaturea, n | Secondary literatureb, n | Primary literaturec, n | Participants, n (%) |
| Attention-deficit/hyperactivity disorder | 90 | 8 | 35 | 2428 (0.5) |
| Anxiety, mood, stress, trauma | 1205 | 123 | 923 | 136,121 (29.5) |
| Bipolar and related disorders | 65 | 9 | 42 | 3573 (0.8) |
| Dementia | 246 | 24 | 180 | 10,823 (2.3) |
| Developmental disorders (excluding attention-deficit/hyperactivity disorder) | 326 | 24 | 349 | 8736 (1.9) |
| Feeding and eating disorders | 154 | 23 | 117 | 10,441 (2.3) |
| Pain | 147 | 23 | 348 | 24,327 (5.3) |
| Schizophrenia and psychotic disorders | 263 | 30 | 304 | 20,500 (4.4) |
| Sleep-wake disorders | 145 | 8 | 29 | 3333 (0.7) |
| Substance-related disorders | 555 | 59 | 466 | 241,377 (52.3) |
aTotal number of articles from Medline searches.
bSelected secondary literature.
cPrimary literature curated by secondary sources.
Figure 2.
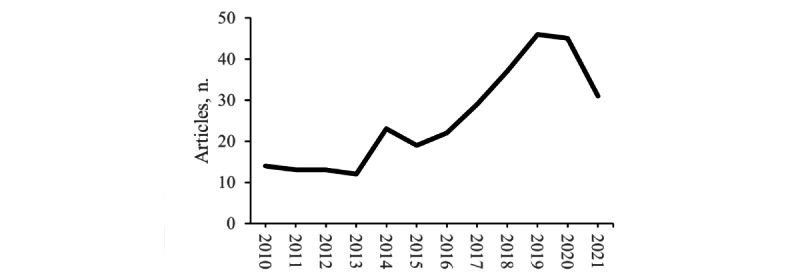
Number of included articles per year.
Digital Health Interventions
To more precisely measure the amount of research available to treat specific mental health conditions using a specific digital health intervention, we superimposed the primary digital health interventions on study characteristics and conclusions drawn from our search results (Table 2). All digital health interventions are supplementary to synchronous or real-time communication.
Table 2.
Digital health interventions used to treat mental health conditions.
| Condition | Therapist contact | Online peer support | Web-based therapy | Mobile therapy | Virtual reality | Cognitive training | |||||||
| Attention-deficit/hyperactivity disorder | |||||||||||||
|
|
RCT-TAUa (patients/studies), n/n | 45/1 | —b | — | — | — | 363/4 | ||||||
|
|
RTC-otherc (patients/studies), n/n | 968/6 | — | — | — | — | 929/14 | ||||||
|
|
Observational (patients/studies), n/n | 45/4 | — | — | — | 2/1 | 36/5 | ||||||
|
|
Reported study quality (1=low to 3=high) | Not reported | — | — | — | 1.00 | 1.00 | ||||||
|
|
Overall strength of evidenced | Medium | — | — | — | Low | Medium | ||||||
|
|
Effective as treatment modality?e | Yes | — | — | — | Emerging | Inconclusive | ||||||
|
|
Effective as assessment modality?e | Yes [55,56,117-119] | — | — | — | Emerging [56,120,121] | Inconclusive [56,57,117,118, 122] | ||||||
| Anxiety-, mood-, stress-, and trauma-related disorders | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | 7156/60 | — | 19,803/105 | 1333/6 | 2842/65 | 42/3 | ||||||
|
|
RTC-other (patients/studies), n/n | 5460/38 | 73/1 | 51,074/279 | 3905/22 | 2974/69 | 222/6 | ||||||
|
|
Observational (patients/studies), n/n | 1567/41 | — | 31,461/93 | 45/1 | 305/21 | — | ||||||
|
|
Reported study quality (1=low to 3=high) | 2.33 (SD 0.57) | Not reported | 2.38 (SD 0.68) | 1.64 (SD 0.64) | 1.78 (SD 0.68) | 1.00 | ||||||
|
|
Overall strength of evidence | High | Low | High | Medium | High | Low | ||||||
|
|
Effective as treatment modality? | Yes | Emerging | Yes | Yes | Yes | Emerging | ||||||
|
|
Effective as assessment modality? | Yes [68,96,123-144] | No studies [129] | Emerging [1,30,31,68, 69,84-86,96, 118,124,125,129, 130,133-135,137, 138,142,144-192] | Yes [1,43,68,96, 144,185-187,191, 193-204] | Emerging [65-67,134,183, 184,205-229] | Emerging [166,230] | ||||||
| Bipolar and Related Disordersf | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | — | — | 992/14 | 132/1 | — | — | ||||||
|
|
RTC-other (patients/studies), n/n | 14/1 | 286/3 | 1499/7 | — | — | — | ||||||
|
|
Observational (patients/studies), n/n | —/3 | 156/1 | 273/5 | 51/1 | — | — | ||||||
|
|
Reported study quality (1=low to 3=high) | Not reported | 1.00 | 1.00 | 2.75 | — | — | ||||||
|
|
Overall strength of evidence | Low | Medium | Medium | Low | — | — | ||||||
|
|
Effective as treatment modality? | Yes | Emerging | Noj | Emerging | — | — | ||||||
|
|
Effective as assessment modality? | Yes [231,232] | No studies [233] | No studies [231-235] | No studies [201,231,236,237] | [231] | — | ||||||
| Dementia and Related Disorders | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | 483/6 | — | — | 3981/7 | 331/11 | 590/16 | ||||||
|
|
RTC-other (patients/studies), n/n | 486/4 | — | — | —/30 | 30/1 | 1222/19 | ||||||
|
|
Observational (patients/studies), n/n | 1695/29 | — | — | —/30 | 273/10 | 282/16 | ||||||
|
|
Reported study quality (1=low to 3=high) | 1.75 (SD 0.75) | — | — | Not reported | 1.50 (SD 0.50) | 1.63 (SD 0.41) | ||||||
|
|
Overall strength of evidence | Medium | — | — | Medium | Medium | Medium | ||||||
|
|
Effective as treatment modality? | Yes | — | — | Yes | Inconclusive | Yes | ||||||
|
|
Effective as assessment modality? | Yes [58,238-245] | — | — | Yes [59,60,240,242,246] | No studies [221,240,242, 247-249] | Yes [61-64,166,240, 242,250-252] | ||||||
| Dementia: caregiver support | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | 773/8 | 11/1 | 1054/10 | — | — | — | ||||||
|
|
RTC-other (patients/studies), n/n | 1019/10 | 384/4 | 2852/17 | — | — | — | ||||||
|
|
Observational (patients/studies), n/n | 78/3 | 54/2 | 176/6 | — | — | — | ||||||
|
|
Reported study quality (1=low to 3=high) | 1.50 | 1.50 | 1.50 | — | — | — | ||||||
|
|
Overall strength of evidence | Medium | Low | Medium | — | — | — | ||||||
|
|
Effective as treatment modality? | Yes | Emerging | Yes | — | — | — | ||||||
|
|
Effective as assessment modality? | Yes [88,89,240] | No studies [70,88-91] | Emerging [70,88,89] | — | — | — | ||||||
| Developmental disorders (excluding attention-deficit/hyperactivity disorder) | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | 535/13 | — | — | 107/4 | 222/7 | 984/20 | ||||||
|
|
RTC-other (patients/studies), n/n | 327/10 | — | 80/3 | 69/3 | 877/24 | 1298/55 | ||||||
|
|
Observational (patients/studies), n/n | 3330/88 | — | 7/1 | 7/2 | 212/24 | 392/37 | ||||||
|
|
Reported study quality (1=low to 3=high) | 1.56 (SD 0.77) | — | 1.00 | 1.50 | 2.50 (SD 0.50) | 1.00 (SD 0) | ||||||
|
|
Overall strength of evidence | High | — | Low | Low | Medium | High | ||||||
|
|
Effective as treatment modality? | Yes | — | Inconclusive | Inconclusive | Inconclusive | Yes | ||||||
|
|
Effective as assessment modality? | Yes [92,119,253-263] | — | No studies [119,263] | No studies [264] | No studies [120,221,253,265,266] | Yes [118,253,267-270] | ||||||
| Feeding and eating disorders | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | 833/15 | — | 2497/23 | 276/3 | 628/9 | — | ||||||
|
|
RTC-other (patients/studies), n/n | 97/1 | 275/3 | 3361/29 | 143/3 | — | — | ||||||
|
|
Observational (patients/studies), n/n | 296/8 | — | 1928/18 | 107/5 | — | — | ||||||
|
|
Reported study quality (1=low to 3=high) | 2.00 | 2.00 | 1.83 (SD 0.69) | 1.00 | 1.00 | — | ||||||
|
|
Overall strength of evidence | Medium | Medium | High | Medium | Medium | — | ||||||
|
|
Effective as treatment modality? | Yes | Emerging | Yes | Emerging | Yes | — | ||||||
|
|
Effective as assessment modality? | Yes [28,71,72,271,272] | No studies [72] | Emerging [71-74,171,272-278] | Emerging [74,276,279-282] | No studies [120,211,283-285] | N/A | ||||||
| Chronic pain, disability, and other medical illness | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | 4350/54 | — | 1339/10 | 0 | 3583/43 | — | ||||||
|
|
RTC-other (patients/studies), n/n | 3203/46 | — | 5666/37 | — | 2642/35 | — | ||||||
|
|
Observational (patients/studies), n/n | 2066/66 | — | — | — | 1478/56 | — | ||||||
|
|
Reported study quality (1=low to 3=high) | 1.42 (SD 0.55) | — | 2.0 (SD 0.71) | — | 1.21 (SD 0.37) | — | ||||||
|
|
Overall strength of evidence | High | — | High | — | High | — | ||||||
|
|
Effective as treatment modality? | Yes | — | Yes | — | Yes | — | ||||||
|
|
Effective as assessment modality? | No studies [286,287] | — | Emerging [79,80,85,286-289] | — | No studies [81-83,290-301] | — | ||||||
| Schizophrenia and psychotic disordersg | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | — | —/4 | —/9 | 1580/6 | 292/4 | 1495/33 | ||||||
|
|
RTC-other (patients/studies), n/n | 3287/5 | —/2 | 101/3 | 5837/4 | 1735/28 | 1783/31 | ||||||
|
|
Observational (patients/studies), n/n | 404/5 | —/2 | 20/2 | 1891/23 | 1267/32 | 86/5 | ||||||
|
|
Reported study quality (1=low to 3=high) | 1.50 (SD 0.87) | 1.67 (SD 0.94) | 2.00 (SD 1.00) | 1.83 (SD 0.62) | 2.25 (SD 1.0) | 2.50 (SD 0.41) | ||||||
|
|
Overall strength of evidence | Medium | Low | Low | Medium | High | High | ||||||
|
|
Effective as treatment modality? | Yes | Yes | Yes | Yes | Inconclusive | Yes | ||||||
|
|
Effective as assessment modality? | Yes [231,232,302-304] | No studies [304-306] | Emerging [231,232,304,305, 307,308] | Emerging [201,231,232, 302-305,307,308] | No studies [120,211,221,309-315] | Yes [231,252,312, 316-321] | ||||||
| Sleep-wake disorders | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | — | — | 1779/9 | — | — | — | ||||||
|
|
RTC-other (patients/studies), n/n | — | — | 1220/13 | — | — | — | ||||||
|
|
Observational (patients/studies), n/n | — | — | 334/6 | — | — | — | ||||||
|
|
Reported study quality (1=low to 3=high) | — | — | 2.00 (SD 0.63) | — | — | — | ||||||
|
|
Overall strength of evidence | — | — | Medium | — | — | — | ||||||
|
|
Effective as treatment modality? | — | — | No | — | — | — | ||||||
|
|
Effective as assessment modality? | — | — | No studies [182,322-328] | — | — | — | ||||||
| Substance use disorders | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | 8151/21 | — | 61,896/93 | 4650/8 | 11/1 | — | ||||||
|
|
RTC-other (patients/studies), n/n | 15,610/31 | — | 97,802/180 | 12,385/22 | 219/5 | — | ||||||
|
|
Observational (patients/studies), n/n | 984/5 | — | 14,603/35 | 5231/30 | 181/8 | — | ||||||
|
|
Reported study quality (1=low to 3=high) | 2.13 (SD 0.74) | — | 2.07 (SD 0.63) | 2.26 (SD 0.74) | 1.33 (SD 0.47) | — | ||||||
|
|
Overall strength of evidence | High | — | High | High | Medium | — | ||||||
|
|
Effective as treatment modality? | Yes | — | Yes | Yes | Inconclusive | — | ||||||
|
|
Effective as assessment modality? | Yes [32,75,96-99, 329-345] | — | Yes [32,75,78, 96-114,188,277, 332-339,344,346-354] | Emerging [32,99,100, 333-339, 344,346-348,354-359] | No studies [115,120,211,221] | — | ||||||
| Total | |||||||||||||
|
|
RCT-TAU (patients/studies), n/n | 22,326/178 | 11/5 | 89,360/273 | 11,927/34 | 7909/140 | 3474/76 | ||||||
|
|
RTC-other (patients/studies), n/n | 30,471/152 | 1018/13 | 163,655/569 | 22,521/63 | 8477/162 | 5494/125 | ||||||
|
|
Observational (patients/studies), n/n | 10,465/252 | 210/5 | 48,802/166 | 7332/92 | 3718/152 | 796/63 | ||||||
|
|
Reported study quality (1=low to 3=high) | 1.69 | 1.54 | 1.86 | 1.83 | 1.64 | 1.45 | ||||||
|
|
Overall strength of evidence | High | Low | High | Medium | High | Medium | ||||||
|
|
Effective as treatment modality? | Yes | Emerging | Inconclusive | Inconclusive | Inconclusive | Yes | ||||||
|
|
Effective as assessment modality? | Yes | No studies | Yes | Emerging | Emerging | Yes | ||||||
aRCT-TAU control: Randomized controlled trials with a treatment-as-usual control.
b—: not determined.
cRCT-other control: Randomized controlled trials with a waitlist or placebo control.
dHigh confidence based on >30 randomized controlled trials with >2000 participants in total; Medium confidence owing to <30 randomized controlled trials with <2000 participants; Low confidence owing to <500 participants; N/A: not applicable.
eYes=positive treatment outcomes and low drop-out rates; Inconclusive=mixed findings, may be effective; Emerging=novel area of research with insufficient evidence; No=no significant difference in outcomes between intervention and controls.
fWeb-based programs developed for bipolar disorders only address depression symptoms but not mania symptoms.
gPatients with schizophrenia and psychotic disorders or symptoms may not be willing to use any digital modalities owing to paranoia about technology, which stems from the underlying psychopathology.
Digital health interventions can be separated into 7 primary categories.
Synchronous and Asynchronous Therapist Contact
Synchronous contact refers to methods where providers and patients communicate at the same time (eg, phone call and videoconference). With better technology practitioners have gravitated toward videoconferencing, but a telephone call is used in the event of technical issues [232,360,361]. Delivery of assessment or treatment (eg, prescribing medication, parent and caregiver training, and various therapies) are usually provided using synchronous forms of communication. Nonetheless, it may also be more difficult to deliver time-dependent neurological tests [238]. Synchronous contact remains the primary form of treatment where other forms of treatment described below are only supplementary [68,69,84,98,109,111, 112,124, 135,151,159,169,170,178,179,199,273,348,349,362].
From a patient’s perspective, most felt that synchronous contact with a therapist afforded greater accessibility, independence, and made it easier for them to express themselves, others felt that it was impersonal [231,363], and some patients with schizophrenia and psychosis disorders were not comfortable with the technology, felt monitored or recorded, and refused care [147,232,308,360,361].
For asynchronous communications, there is a time delay between responses (eg, email and text). These methods can be useful in encouraging patients to attend their appointments, take their medications, exercise, relax, complete daily life tasks, and reduce relapse following remission [74,110,157,198,232,274,279,330,361,364-367]. However, asynchronous forms of communication were not as effective as synchronous forms of communication before remission [123,129,142,147,148]. Furthermore, asynchronous communications are rarely tested in emergency situations with patients who are potentially suicidal or violent [29,125,149,179].
Web-Based Peer Support
Mental health support provided by people with lived experience of mental health issues took place via web-based discussion groups (video calls, forums, and social media) where patients with similar disorders can interact. Treatment programs rarely include web-based groups, and few studies explore their role in treatment and adherence; therefore, we retained it as a separate category. Online communities and forums (eg, specific subreddits, forums, discord, and Facebook groups) are prevalent for all mental health conditions since patients can learn more about others’ experiences, learn about their condition, receive peer support, and accept their condition [87,232,304,305]. Online communities have also formed on YouTube where people living with mental health conditions are able to share their lived experience and insights. While there are examples of evidence-based forums and media content on mental health conditions, web-based content is not usually moderated, which may lead to the spread of misinformation. Indeed, unmoderated online communities have lower retention rates [306], suggesting that moderation by a practitioner may be required to reduce potential problems. Nevertheless, patient involvement and interaction on social media platforms provide significant insights, alternative perspectives, and fortitude to the general population, other patients, health care providers, and researchers. Despite their prominence, their use and effectiveness are rarely evaluated.
Web-Based or Computer-Based Therapy Programs
Various types of content delivered on the internet included psychoeducation, self-help therapy, journaling, assessments, topics traditionally covered in workbooks and paper format, reminders to take medication, motivational interventions, and web-based peer support. Web-based and mobile programs delivered with administrative or therapist guidance are as effective as treatment as usual (TAU), while those without guidance show significantly lower effectiveness and variable dropout rates [68,69,84,98,109,111,112,124,135, 151,159,169,170,178,179,199,273,308,348,349,362]. These are well developed for substance use–, mood-, anxiety-, and trauma-related disorders but not bipolar, personality, and sleep-wake disorders (Table 2). Indeed, for the latter disorders these interventions yield mixed results since they primarily treat anxiety and mood symptoms, but not mania or other symptoms [233,323,326].
Mobile-Based Therapy Programs
Mobile apps are a novel way to deliver therapy programs on mobile devices and share similarities to web-based or computer-based therapy programs. Over 2200 mobile apps claim to deliver therapy for several mental health conditions but lack rigorous validation, are not necessarily based on therapeutic principles, are gamified and addictive, or harm recovery [1,43,74,154,180,185,187,194-196,198,200,231,237,280,308,333,356,368]. Furthermore, 38% of trials for mobile apps were uncontrolled (Table 2). Mobile apps were therefore separated from web-based and computerized therapy (Table 2). We also urge caution when selecting mobile apps and provide a list of web-based tools and apps that have previously been validated (Table S1 in Multimedia Appendix 1).
Virtual and Augmented Reality
Virtual and augmented reality provide realistic and immersive experiences with a sense of presence for participants. It is a promising tool for new forms of assessment, treatment, and research to understand psychological processes (eg, psychosis and paranoia) [310]. Virtual reality is easier to implement, perform, and more realistic, motivating, and enjoyable than traditional exposure therapy [65-67,98,115,134,183,205,206,208-210,212-215, 219,222,311,369]. Virtual reality can be used to deliver psychotherapy, education, cognitive therapy, and exposure therapy [65-67,98,115,134, 183,205,206,208-210,212-215,217, 219,222,248,257,292,310,311,369,370]. Experiential cognitive therapy, a combination of virtual and cognitive therapy, has also been successful in treating eating- and weight-related disorders [284,371]. Lastly, virtual reality is valuable as a distraction tool, which leads to reduced pain perception, improved functional ability, and lower stress in patients with various acute and chronic illnesses [81,83,290,291,294,295]. Virtual reality could also provide otherwise inaccessible experiences to individuals with a disability, older individuals, or those living with a chronic illness or disability. Nevertheless, virtual reality should be part of a comprehensive treatment strategy [67].
Initial concerns that virtual reality could induce nausea, headaches, and other negative side effects, which could ultimately worsen phobias and attrition [207] have been assuaged by several improvements in the technology [67,206]. Practitioners should nevertheless use caution and test participants for susceptibility to motion sickness [218]. Some of these concerns may be addressed by using augmented reality where 3D representations of elements are imposed on the user’s native world, but more research is necessary for conclusive evidence of treatment efficacy between virtual reality and augmented reality [184]. Therapists also need to carefully assess for signs of cognitive avoidance in patients where they might treat virtual environment and stimuli as a “game” instead of cognitive immersion [218]. Mobile-based virtual reality treatments may provide new treatment avenues for patients who cannot attend in-person therapy owing to disability, transportation, or health concerns [137,220].
Cognitive Training
Cognitive training includes training exercises, neurofeedback, and games provided over mobile, web-based, or computer devices or virtual reality. These provide greater flexibility and development than pen-and-paper methods. Evidence suggests broad cognitive training is more effective than a narrow focus on a single cognitive modality [61,244,252,316,318]. Additionally, these must also be combined with tailored remediation to extract the greatest benefits in everyday life [58,92,244,252,258,316-318,372]. Cognitive declines are also reported in anxiety, mood, bipolar, and personality disorders, where similarly broad cognitive training could be useful to alleviate cognitive decline, reduce premature brain aging [59-62,64,150,251,252], and increase remission [166,230], and where the success of cognitive training in disorders such as schizophrenia, ADHD, developmental disorders, and dementia could be applied. Cognitive training and virtual reality could also improve broad motor and cognitive functions in patients with neurological disorders such as stroke, traumatic brain injury, Parkinson disease, and multiple sclerosis [61,247]. Attention bias modification appears to be successful in treating negative cognitive and attentional biases in patients with mood and anxiety disorders [163].
Other Technologies
Monitoring technologies (eg, breathalyzer, pill dispenser Wisepill, mobile apps, smart watches) are used to regularly monitor psychological symptoms, heart rate, blood pressure, location, and sleep and to alert practitioners to early signs of relapse, missed doses, or to flag early warning signs of disease [60,232,236,243,251,302,305,306,333,334]. Security systems, call screening technology (for scams), and chatbots can also improve quality of life, but more research is needed [60,243,245,251]. Lastly, transcranial direct current stimulation (tDCS) and similar treatments can be delivered remotely for dementia and schizophrenia [244].
Discussion
Principal Findings
This review found that a majority of studies on digital health interventions are focused on substance use–, anxiety-, mood-, and trauma-related disorders. For patients with these conditions, the greater flexibility, comfort, and routine associated with digital health offered a favorable substitute for in-person visits and retained therapeutic utility. Given this finding, we expect the use of digital health interventions to persist during and after the pandemic owing to the relaxation of insurance and administrative regulations [12,373-377]. The volume and quality of research for these disorders has enabled the discovery of new treatment methods and the refinement of existing digital health tools to improve treatment efficacy.
We also found that the sudden onset of the COVID-19 pandemic led to a rapid shift toward the use of new technology and interventions without the necessary time to train or prepare practitioners and posed challenges for many health care providers. To remedy this, governments, professional organizations, and academics, have created region-specific digital health toolkits [12,378-383] to facilitate and encourage the provision of digital health services. These toolkits are extensive and provide examples of ways in which digital health can be delivered in a meaningful and effective way.
Evidence from this review also suggests that digital health interventions have implications for combatting the dual public health emergencies across North America: the COVID-19 pandemic and the ongoing overdose crisis [11,384]. Findings indicate that there is significant potential for digital health interventions in reducing the harms experienced by people who use substances [32,75,78,96-114,329-339,346-353,385]. Research into digital health interventions for substance use disorders is relatively new and demonstrates the promising use of web-based programs and social media to reach participants instead of relying solely on referrals from practitioners [100,102,111-114,171,339,349,385]. These interventions may offer timely and cost-effective solutions, where texting, moderated forums, validated web-based or computer-based programs, or mobile apps may be used for treatment, psychoeducation, managing ongoing symptoms, and preventing relapse [12,20,25,30, 79,80,85,147,157,175,351] (see Table S1 in Multimedia Appendix 1 for a list of validated tools). Nevertheless, it is important to acknowledge that there are certain instances where in-person contact with a service provider is most suitable. This is particularly important given that many homeless and street-involved populations lack access to and knowledge of technology [386-388].
Similarly, this review found indications that web-based programs in anxiety-, mood-, and trauma-related disorders are poised for similar expansion. Since anxiety and depression symptoms have risen in the general population during the pandemic [10-16], several interventions can be useful for short-term symptom management, such as synchronous communication (videoconferencing or telephone calls) with a therapist [68,96,123-126,129,130,133-139,141,142] and referral to validated web-based [1,30,68,69,84-86,96,118,124, 125,129,130,133-135,137,138,142,145-187], computer-, or mobile-based applications [1,68,96,185-187,193-200] such as those listed in Table S1 in Multimedia Appendix 1. However, we would like to emphasize that interventions were far less successful without practitioner guidance [30,69,73,76,77,155,157,252].
While this review also identified promising developments in digital programs for ADHD, developmental, dementia, eating, schizophrenia, and chronic illness, we found that digital health interventions for these conditions are nascent. Negative findings in sleep-wake and bipolar disorders suggest that significant retooling is necessary for treating these conditions. Furthermore, no reviews on the use of digital health tools for dissociative, elimination, sexual, and personality disorders were identified. The positive outcomes reported for digital health interventions in a wide range of mental health conditions suggest that there may be merit to exploring these interventions in additional clinical contexts during and after the COVID-19 pandemic. Caution is also warranted with patients with schizophrenia, psychosis, or bipolar disorder as technology may be triggering or could exacerbate existing symptoms [147,232,360,361].
Review findings also suggest that synchronous digital contact is an effective substitution for in-person treatment and assessment for many mental health conditions. Considering successes in most mental health conditions, these findings can be generalized to other conditions where less research is available, such as bipolar, sleep-wake–related, and personality disorders. While some health care providers have expressed concerns regarding their ability to build a therapeutic alliance with their patients, research shows that this is not significantly affected by synchronous communication [26,389,390]. Interestingly, synchronous digital health may be beneficial for autism spectrum disorders [269] and social anxiety since it reduces social interaction–related stress, need for eye contact, oversensitivity, and overstimulation. Evidence from this review indicates that synchronous platforms are associated with significant cost and time savings. First, this transition is also beneficial by reducing commutes to work, the ability to organize one’s working day and tasks [391-393], and protects therapists from the risk of physical confrontations [394,395].
Digital health tools have also been found to allow practitioners to reduce the time they spend with each patient, where evidence suggests that spending 10 minutes with patients through synchronous platforms, and providing referrals to asynchronous platforms (eg, web-based, mobile-, or computer-based therapy and cognitive training) is sufficient [30,69,73,76,77,155,157,252,308]. Some patients (eg, children and elderly) may face other barriers to using or accessing technology [396,397], which can be resolved by specific training on using the application [59,62], obtaining help from a caregiver, and could even be accomplished through remote desktop applications (such as Microsoft Teams: Remote Desktop Protocol). Nonetheless, transferring this responsibility to a family member increases caregiver burden and may lead to suboptimal results over the long term. However, the proliferation of untested applications (especially mobile apps) raises concerns around the quality of existing platforms [1,74,154,180,185,187,194-196,198,200,231,237,280,333]. More specifically, these applications often lack validation, reliability, and are not always built on sound psychotherapeutic principles [1,74,154,180,185,187, 194-196,198,200,231,237,280,308,333].
Digital health interventions are also less effective at mitigating the impacts of social isolation, particularly in the context of the COVID-19 pandemic, where public health orders and the requirement of physical distancing is expected to drastically impact peoples’ mental health. Human connection contributes significantly to one’s mental health; therefore, it is important that digital health interventions maintain their human aspect as this is associated with increased efficacy [68,69,84,98,109,111,112, 124,135,151,159,169,170,178,179,199,273,348,349,362]. Findings demonstrate that asynchronous platforms, such as web-based forums, social media, and other digital communities, likely increase patient engagement and adherence to treatment across all mental health conditions [87,232,304,305]. Additionally, preventative education can be disseminated via asynchronous platforms (eg, social media, groups, forums, and schools) for all mental health conditions, as seen in substance use disorders [100,102,111-114,171,339,349]. Owing to increased demand and lack of availability of services during the COVID-19 pandemic, many patients have transitioned to mobile apps and web-based programs without the guidance of a practitioner [13]. Hence, the absence of sufficient research into these venues, their impact on mental health, and the lack of practitioner guidance and support [1,74,154,180,185,187,194-196,198,200,231,237,280,333] raise concerns that these platforms may cause harm. Indeed, government intervention to increase the prominence of validated region-specific tools and resources in web-based and app-related searches may be required.
Another emerging asynchronous technology that can be used for the treatment of mental health conditions are virtual reality tools. Greater accessibility, comfort, and normalcy of the technology will encourage the development of virtual reality interventions on site or at home. Nevertheless, there are also barriers to providing and expanding virtual reality tools. For example, the high cost of equipment acts as a significant barrier, however, lower priced equipment or mobile phones can be used as substitutes [137,220,247]. Additionally, virtual reality tools are based on recent technological advancements, and there is little quality research on the use of industry-standard equipment and even less so for low-cost virtual reality options. Despite these limitations, virtual reality addresses a particular niche of therapeutic tools (eg, exposure therapy) [65-67,98,115,134,183,205,206,208-210,212-215,219,222,311,369] and is an effective tool for pain management [81,83,290,291,294,295], indicating that as technology and research advances, it may become a central component of any comprehensive mental health treatment strategy.
Owing to the social distancing and quarantine requirements posed by the pandemic, patients with mental health disorders already face social isolation in addition to increased stress and anxiety [5-14]. Additionally, patients surviving COVID-19 may experience lingering symptoms and post–intensive care syndrome long after discharge from intensive care units [398,399]. Mental health challenges for these patients include anxiety, depression, posttraumatic stress disorder (PTSD), cognitive decline, and chronic illness [398,399]. Along with previously mentioned interventions to deal with symptoms of anxiety, depression, and posttraumatic stress, virtual reality can be used to reduce stress, distract from pain, and retrain functional movement in patients who experience chronic illness after COVID-19.
Health care providers are also at risk of feeling social and professional isolation as well as burnout [26,394,400], which must be properly managed by managers, the professional organization, and practitioners themselves. Given the anticipated impact of the pandemic on the mental health of health care providers [11,18,401-403], health care organizations will benefit from specialized synchronous, web-based, and mobile therapy and moderated discussion forums to alleviate this burden. Similar interventions have been used with family caregivers [70,88-90] and health care providers [18,401,402,404,405] to treat anxiety, depression, PTSD, and burn out. Therefore, such interventions can help manage health care providers’ mental health.
Future Directions
Over the last two decades, research on the use of digital health interventions to deliver mental health care has increased significantly. Lessons learned from highly studied fields (eg, substance use–, anxiety-, mood-, and trauma-related disorders) can guide the implementation of digital health interventions to treat other mental health conditions. Starting at the most basic level, where practitioner guidance for 10 minutes was essential and often sufficient for the treatment of anxiety-, mood-, and trauma-related disorders, web-based, computer-based, or mobile programs or apps developed for these conditions could be adapted, improved upon, and evaluated to treat other conditions with overlapping symptomatology. For example, one could consider the overlap in symptomatology among mood-related, anxiety, bipolar, sleep-wake–related, and some personality disorders [406]. Thus, digital interventions for the former two conditions could be adapted to include journaling, behavioral modification prompts, and other psychotherapeutic treatments akin to these conditions, and finally be re-evaluated. Nonetheless, for conditions where no treatments exist, the development and digitization of novel treatment strategies is required [233,323,326]. Indeed, the digital nature of these programs enables the collection of regular assessment data, input from patients, and evaluation by health care providers to develop decision trees and machine learning algorithms to instantly improve and personalize treatment plans, require less practitioner time, and provide greater flexibility in treatment delivery.
The rapid pace of technological advancements also poses significant challenges. For example, treatment program implementation has evolved from computerized delivery with CDs to web platforms to mobile apps in the last two decades. Significant technological shifts have forced researchers to completely rebuild the programs despite apparent similarities between these modes of delivery. Many validated programs identified (Table S2 in Multimedia Appendix 1) are outpaced by technological advancements and lack recent updates. First, easy-to-use development and cross-platform tools (eg, React Native and Xamarin) will enable researchers to make, evaluate, and maintain programs despite rapid technological advancements. Second, health care policies and evaluation may need to be modified so that validated tools can evolve over time and across platforms when the underlying therapeutic principles remain consistent.
Existing research on digital interventions rarely covers comorbid conditions, emergency situations, or complex socioeconomic factors. For example, research on people experiencing homelessness is limited to commentaries and policy recommendations based on available research in the general population [32-42]. This is of particular concern when considering that those of lower socioeconomic status or with complex life circumstances show reduced benefits from digital health interventions [148,165,407]. Additional research considering individuals experiencing various psychosocial complexities or comorbid conditions is required.
Further research must endeavor to use appropriate controls and more rigorous design to improve overall study quality assessed in Table 2. Blinding patients to the digital nature of the treatment is difficult, but creative solutions (eg, unrelated cognitive tasks in lieu of treatment) are recommended. Additionally, standardized rating scales (ie, DSM-V criteria) should be used instead of nonstandard assessments or a participant’s opinion on the treatment. Most studies are restricted to treatment duration and lack long-term follow-up (>6 months). Considering digitization of treatments and records, practitioners can automatically request follow-up surveys and assessments via email or text. Follow-up surveys must also consider whether patients have pursued other treatment programs, as these could confound any pertinent treatment effects. Lastly, following successful remission, there is limited research on the use of digital health interventions (eg, email, text, social media, and forums) to prevent relapse, which can be accomplished via email or text [74,110,157,198,232,274,279,330,361,364-367].
Web-based peer support is dependent on human interaction, which can be unpredictable and include uncontrolled variables. For example, since any large number of people can participate in forums for intermittent periods of time, the inevitable turnover can cause cultural shifts. This would therefore require moderation by practitioners. Evaluation is further complicated by the lack of objective and quantifiable pre-post measures in open social media groups and forums. Indeed, practitioner moderated forums or groups may fare better and could automatically request participants to fill out monthly surveys. Further research is needed to address these hypotheses.
Limitations
There are several limitations to this review. First, to rapidly inform health care stakeholders responsible for managing treatment of a broad range of mental health disorders, we took a comprehensive approach. As a result, we limited the scope to secondary literature sources and utilized a systematic methodology designed for meta-reviews [167]. Since we primarily report on the effectiveness, feasibility, and reliability of digital delivery in lieu of face-to-face treatment, we did not attempt to compare different forms of therapy. This included drawing comparisons to nondigital interventions reported within identified studies, when available (27% of primary studies compared digital health interventions to TAU). Owing to the urgency of this endeavor and to limit the already substantial number of references, we focus exclusively on reports obtained from Medline. This is not atypical as many of the included reports use a single database but can miss some reports.
Additionally, the metadata collection procedure described only approximates the state and volume of research. Reliance on secondary research articles implies that we likely missed recent relevant primary research articles. Nevertheless, our correlative analysis (Table S2 and Figure S1 in Multimedia Appendix 1) suggests that metadata and secondary research can be used to estimate the relative amount and reliability of primary research.
Owing to differences in quality and bias reporting between included literature, we could not report this for individual studies and instead relied on the included literature sources to dictate the quality of research in the field. We observed considerable variability in quality assessments between reviews (Table 2). Potential explanations include the specific selection and inclusion or exclusion criteria of reviews or lower stringency in early discovery studies versus later RCTs. Nevertheless, this raises concerns regarding interreview reliability, which we did not assess here. To enable policy makers and researchers to reliably compile all amassed data, reliably rate studies, and reduce time lost to re-evaluating studies we recommend an update to Cochrane and PRISMA requirements to include the adoption of a single consistent bias and quality assessment reporting methodology and consistent reporting of study details in all reviews. In addition to ensuring similar quality and bias assessment between reviewers within a review, we recommend comparison with previous reviews to ensure greater reproducibility of quality and bias assessments between independent reviews. Nevertheless, living systematic reviews are likely to accelerate research and development in digital mental health interventions and may if designed accordingly upend the systematic review process. Living reviews stem from the ability to continuously update web-based articles with the latest developments in the field. These are a way forward for rapid evidence-based development, collaboration, standardization of digital health tools, and a necessary step forward to improve treatment options.
Conclusions
Although digital delivery of mental health treatment has been in clinical use for a long time, the available research on the topic is far from comprehensive or consistent. New guidelines to increase reliability and consistency of reporting, evaluation, and quality and bias assessments would enable faster literature synthesis and increase confidence. Living systematic reviews for bipolar, personality, developmental, dementia, and sleep-wake disorders would also be very useful to guide and organize novel digital treatment strategies.
Overall, digital treatment strategies paired with synchronous practitioner contact are as effective as nondigital alternatives. However, in offering digital treatments, it is essential to consider feasibility of treatment, caregiver burden, patient-specific symptoms (eg, paranoia), and patient-specific parameters. More research is especially needed in marginalized populations who face greater barriers to mental health treatment access. Thus, to maintain treatment quality and efficacy, patients should have the option for face-to-face interventions, despite the challenges posed by the COVID-19 pandemic. Nonetheless, digital treatments offer many benefits such as increased patient engagement, accessibility, and availability paired with reduced practitioner workload. Additionally, the drastic shift to digital health is likely to encourage further developments in treatments for many mental health disorders and expansion into other digital modalities, such as virtual reality, social media, and web-based forums. These developments promise significant advances in mental health treatment via global collaboration and investment.
Acknowledgments
This review was initially conducted to provide comprehensive information about the use of digital health to treat mental health conditions in complex populations for a community clinic and was not funded. Publication of this article was cosponsored by the Journal of Medical Internet Research, the University of British Columbia (Graduate Student Travel and Research Dissemination Fund to TJP), and Simon Fraser University (SFU Central Open Access Fund to KV). We thank the VCHRI Rapid Evidence Synthesis Team and VCH Operations Director, Andy Day, for valuable feedback. All authors discussed and refined the direction and development of this review. TJP, AJ, and MEK carried out research for the Introduction section, which TJP wrote. TJP with guidance from EL and Evan Sterling developed the methodology and search strategy. TJP, NS, and AJ screened articles for inclusion. TJP, NS, and AJ designed the tables and figures and wrote the Results and Discussion sections. AP and KV supervised all stages in equal capacity. All authors approved of and reviewed the final manuscript.
Abbreviations
- ADHD
attention-deficit/hyperactivity disorder
- DSM-5
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- MeSH
Medical Subject Headings
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTSD
post-traumatic stress disorder
- TAU
treatment as usual
Supplementary.
Extracted data for digital health interventions per mental health condition.
Footnotes
Conflicts of Interest: None declared
References
- 1.Sander L, Ebert DD, Baumeister H. [Internet- and Mobile Based Psychotherapy for Depression] Fortschr Neurol Psychiatr. 2017 Jan;85(1):48–58. doi: 10.1055/s-0042-123540. [DOI] [PubMed] [Google Scholar]
- 2.Strike C, Watson TM. Losing the uphill battle? Emergent harm reduction interventions and barriers during the opioid overdose crisis in Canada. Int J Drug Policy. 2019 Sep;71:178–182. doi: 10.1016/j.drugpo.2019.02.005.S0955-3959(19)30057-X [DOI] [PubMed] [Google Scholar]
- 3.Gordon AL, Goodman C, Achterberg W, Barker RO, Burns E, Hanratty B, Martin FC, Meyer J, O'Neill D, Schols J, Spilsbury K. Commentary: COVID in care homes-challenges and dilemmas in healthcare delivery. Age Ageing. 2020 Aug 24;49(5):701–705. doi: 10.1093/ageing/afaa113. http://europepmc.org/abstract/MED/32402088 .5836695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malek J. Senior's care was in crisis before COVID-19. The Council of Canadians. [2020-04-10]. https://canadians.org/analysis/seniors-care-was-crisis-covid-19 .
- 5.Qadir J, Al-Fuqaha A. A Student Primer on How to Thrive in Engineering Education during and beyond COVID-19. Educ Sci. 2020 Sep 05;10(9):236. doi: 10.3390/educsci10090236. [DOI] [Google Scholar]
- 6.Isumi A, Doi S, Yamaoka Y, Takahashi K, Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020 Dec;110(Pt 2):104680. doi: 10.1016/j.chiabu.2020.104680. http://europepmc.org/abstract/MED/32847679 .S0145-2134(20)30335-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muratori P, Ciacchini R. Children and the Covid-19 Transition: Psychological Reflections and Suggestions on Adapting to the Emergency. Clin Neuropsychiatry. 2020 Apr;17(2):131–134. doi: 10.36131/CN20200219. http://europepmc.org/abstract/MED/34908983 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Golberstein E, Wen H, Miller BF. Coronavirus Disease 2019 (COVID-19) and Mental Health for Children and Adolescents. JAMA Pediatr. 2020 Sep 01;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456.2764730 [DOI] [PubMed] [Google Scholar]
- 9.Robinson J, Borgo L, Fennel K, Funahashi T. The Covid-19 Pandemic Accelerates the Transition to Virtual Care. NEJM Catal Innov Care Deliv. 2020 doi: 10.1056/CAT.20.0399. [DOI] [Google Scholar]
- 10.Mendes-Santos C, Andersson G, Weiderpass E, Santana R. Mitigating COVID-19 Impact on the Portuguese Population Mental Health: The Opportunity That Lies in Digital Mental Health. Front Public Health. 2020;8:553345. doi: 10.3389/fpubh.2020.553345. doi: 10.3389/fpubh.2020.553345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020 Mar 14;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. http://europepmc.org/abstract/MED/32112714 .S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torous J, Jän Myrick K, Rauseo-Ricupero N, Firth J. Digital Mental Health and COVID-19: Using Technology Today to Accelerate the Curve on Access and Quality Tomorrow. JMIR Ment Health. 2020 Mar 26;7(3):e18848. doi: 10.2196/18848. https://mental.jmir.org/2020/3/e18848/ v7i3e18848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rauschenberg C, Schick A, Goetzl C, Roehr S, Riedel-Heller SG, Koppe G, Durstewitz D, Krumm S, Reininghaus U. Social isolation, mental health, and use of digital interventions in youth during the COVID-19 pandemic: A nationally representative survey. Eur Psychiatry. 2021 Mar 09;64(1):e20. doi: 10.1192/j.eurpsy.2021.17. http://europepmc.org/abstract/MED/33686930 .S0924933821000171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng J, Morstead T, Sin N, Klaiber P, Umberson D, Kamble S, DeLongis A. Psychological distress in North America during COVID-19: The role of pandemic-related stressors. Soc Sci Med. 2021 Feb;270:113687. doi: 10.1016/j.socscimed.2021.113687.S0277-9536(21)00019-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed O, Ahmed MZ, Alim SMAHM, Khan MDAU, Jobe MC. COVID-19 outbreak in Bangladesh and associated psychological problems: An online survey. Death Stud. 2022;46(5):1080–1089. doi: 10.1080/07481187.2020.1818884. [DOI] [PubMed] [Google Scholar]
- 16.Zhong B, Huang Y, Liu Q. Mental health toll from the coronavirus: Social media usage reveals Wuhan residents' depression and secondary trauma in the COVID-19 outbreak. Comput Human Behav. 2021 Jan;114:106524. doi: 10.1016/j.chb.2020.106524. http://europepmc.org/abstract/MED/32836728 .S0747-5632(20)30276-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hong Y, Lawrence J, Williams D, Mainous I. Population-Level Interest and Telehealth Capacity of US Hospitals in Response to COVID-19: Cross-Sectional Analysis of Google Search and National Hospital Survey Data. JMIR Public Health Surveill. 2020 Apr 07;6(2):e18961. doi: 10.2196/18961. https://publichealth.jmir.org/2020/2/e18961/ v6i2e18961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grover S, Dua D, Sahoo S, Mehra A, Nehra R, Chakrabarti S. Why all COVID-19 hospitals should have mental health professionals: The importance of mental health in a worldwide crisis! Asian J Psychiatr. 2020 Jun;51:102147. doi: 10.1016/j.ajp.2020.102147. http://europepmc.org/abstract/MED/32473537 .S1876-2018(20)30258-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, Ustün TB, Wang PS. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18(1):23–33. doi: 10.1017/s1121189x00001421. http://europepmc.org/abstract/MED/19378696 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whaibeh E, Mahmoud H, Naal H. Telemental Health in the Context of a Pandemic: the COVID-19 Experience. Curr Treat Options Psychiatry. 2020;7(2):198–202. doi: 10.1007/s40501-020-00210-2. http://europepmc.org/abstract/MED/32292687 .210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gates B. Responding to Covid-19 - A Once-in-a-Century Pandemic? N Engl J Med. 2020 Apr 30;382(18):1677–1679. doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- 22.Knopf A. Addiction telemedicine comes into its own with COVID‐19. Alcoholism Drug Abuse Weekly. 2020 Mar 30;32(13):5–6. doi: 10.1002/adaw.32673. [DOI] [Google Scholar]
- 23.Knopf A. Telemental health comes into its own with social distancing. The Brown University Child and Adolescent Behavior Letter. 2020 May;36(5):7–7. doi: 10.1002/cbl.30463. [DOI] [Google Scholar]
- 24.Wind TR, Rijkeboer M, Andersson G, Riper H. The COVID-19 pandemic: The 'black swan' for mental health care and a turning point for e-health. Internet Interv. 2020 Apr;20:100317. doi: 10.1016/j.invent.2020.100317. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(20)30046-4 .S2214-7829(20)30046-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou X, Snoswell CL, Harding LE, Bambling M, Edirippulige S, Bai X, Smith AC. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed J E Health. 2020 Apr;26(4):377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 26.Cowan KE, McKean AJ, Gentry MT, Hilty DM. Barriers to Use of Telepsychiatry: Clinicians as Gatekeepers. Mayo Clin Proc. 2019 Dec;94(12):2510–2523. doi: 10.1016/j.mayocp.2019.04.018.S0025-6196(19)30400-8 [DOI] [PubMed] [Google Scholar]
- 27.Öngür D, Perlis R, Goff D. Psychiatry and COVID-19. JAMA. 2020 Sep 22;324(12):1149–1150. doi: 10.1001/jama.2020.14294.2770856 [DOI] [PubMed] [Google Scholar]
- 28.Sproch LE, Anderson KP. Clinician-Delivered Teletherapy for Eating Disorders. Psychiatr Clin North Am. 2019 Jun;42(2):243–252. doi: 10.1016/j.psc.2019.01.008.S0193-953X(19)30013-9 [DOI] [PubMed] [Google Scholar]
- 29.McGrath P, Wozney L, Bishop A, Curran J, Chorney J, Rathore S. Toolkit for e-Mental Health Implementation. Mental Health Commission of Canada. 2018. [2020-04-20]. https://mentalhealthcommission.ca/wp-content/uploads/2021/05/E_Mental_Health_Implementation_Toolkit_2018_eng.pdf .
- 30.Eells TD, Barrett MS, Wright JH, Thase M. Computer-assisted cognitive-behavior therapy for depression. Psychotherapy (Chic) 2014 Jun;51(2):191–197. doi: 10.1037/a0032406.2013-33235-001 [DOI] [PubMed] [Google Scholar]
- 31.Patel S, Akhtar A, Malins S, Wright N, Rowley E, Young E, Sampson S, Morriss R. The Acceptability and Usability of Digital Health Interventions for Adults With Depression, Anxiety, and Somatoform Disorders: Qualitative Systematic Review and Meta-Synthesis. J Med Internet Res. 2020 Jul 06;22(7):e16228. doi: 10.2196/16228. https://www.jmir.org/2020/7/e16228/ v22i7e16228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaner EF, Beyer FR, Garnett C, Crane D, Brown J, Muirhead C, Redmore J, O'Donnell A, Newham JJ, de Vocht F, Hickman M, Brown H, Maniatopoulos G, Michie S. Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community-dwelling populations. Cochrane Database Syst Rev. 2017 Sep 25;9:CD011479. doi: 10.1002/14651858.CD011479.pub2. http://europepmc.org/abstract/MED/28944453 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robards F, Kang M, Usherwood T, Sanci L. How Marginalized Young People Access, Engage With, and Navigate Health-Care Systems in the Digital Age: Systematic Review. J Adolesc Health. 2018 Apr;62(4):365–381. doi: 10.1016/j.jadohealth.2017.10.018.S1054-139X(17)30861-3 [DOI] [PubMed] [Google Scholar]
- 34.Kannarkat JT, Smith NN, McLeod-Bryant SA. Mobilization of Telepsychiatry in Response to COVID-19-Moving Toward 21 Century Access to Care. Adm Policy Ment Health. 2020 Jul;47(4):489–491. doi: 10.1007/s10488-020-01044-z. http://europepmc.org/abstract/MED/32333227 .10.1007/s10488-020-01044-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mongelli F, Georgakopoulos P, Pato MT. Challenges and Opportunities to Meet the Mental Health Needs of Underserved and Disenfranchised Populations in the United States. Focus (Am Psychiatr Publ) 2020 Jan;18(1):16–24. doi: 10.1176/appi.focus.20190028. http://europepmc.org/abstract/MED/32047393 .FOC_20190028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Whaibeh E, Mahmoud H, Vogt EL. Reducing the Treatment Gap for LGBT Mental Health Needs: the Potential of Telepsychiatry. J Behav Health Serv Res. 2020 Jul;47(3):424–431. doi: 10.1007/s11414-019-09677-1.10.1007/s11414-019-09677-1 [DOI] [PubMed] [Google Scholar]
- 37.Crowe T, Jani S, Jani S, Jani N, Jani R. A pilot program in rural telepsychiatry for deaf and hard of hearing populations. Heliyon. 2016 Mar;2(3):e00077. doi: 10.1016/j.heliyon.2016.e00077. https://linkinghub.elsevier.com/retrieve/pii/S2405-8440(15)30432-1 .S2405-8440(15)30432-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lal S, Abdel-Baki A, Sujanani S, Bourbeau F, Sahed I, Whitehead J. Perspectives of Young Adults on Receiving Telepsychiatry Services in an Urban Early Intervention Program for First-Episode Psychosis: A Cross-Sectional, Descriptive Survey Study. Front Psychiatry. 2020;11:117. doi: 10.3389/fpsyt.2020.00117. doi: 10.3389/fpsyt.2020.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jiménez A, de Léon EM, Sims G, Hiraldo-Lebrón C, Small P, Kamel Boulos MN. Stigma and Prejudice. Cham: Humana Press; 2016. Jun 03, Leveraging Technology for Health Equity; pp. 277–301. [Google Scholar]
- 40.Sandre AR, Newbold KB. Telemedicine: Bridging the Gap between Refugee Health and Health Services Accessibility in Hamilton, Ontario. Refuge. 2016 Nov 23;32(3):108–118. doi: 10.25071/1920-7336.40396. [DOI] [Google Scholar]
- 41.Mantler T, Jackson KT, Walsh EJ. Integration of Primary Health-Care Services in Women's Shelters: A Scoping Review. Trauma Violence Abuse. 2020 Jul;21(3):610–623. doi: 10.1177/1524838018781105. [DOI] [PubMed] [Google Scholar]
- 42.Rhee JY, Chan EJ, Elizondo III PM, Bourgeois JA, Breur JG, Shemuel JK, Dazols L, John MD. Home-Based Telepsychiatry and in-Home CBT for Management of Major Depression in HIV-Positive Adults 50 Years and Older: A Proof-of-Concept Study. Acta Psychopathol. 2017;03(03):A. doi: 10.4172/2469-6676.100096. [DOI] [Google Scholar]
- 43.Baumel A, Torous J, Edan S, Kane JM. There is a non-evidence-based app for that: A systematic review and mixed methods analysis of depression- and anxiety-related apps that incorporate unrecognized techniques. J Affect Disord. 2020 Aug 01;273:410–421. doi: 10.1016/j.jad.2020.05.011.S0165-0327(20)30769-2 [DOI] [PubMed] [Google Scholar]
- 44.Kerst A, Zielasek J, Gaebel W. Smartphone applications for depression: a systematic literature review and a survey of health care professionals' attitudes towards their use in clinical practice. Eur Arch Psychiatry Clin Neurosci. 2020 Mar;270(2):139–152. doi: 10.1007/s00406-018-0974-3.10.1007/s00406-018-0974-3 [DOI] [PubMed] [Google Scholar]
- 45.Hanley T, Prescott J, Gomez KU. A systematic review exploring how young people use online forums for support around mental health issues. J Ment Health. 2019 Oct;28(5):566–576. doi: 10.1080/09638237.2019.1630725. [DOI] [PubMed] [Google Scholar]
- 46.Hargreaves S, Bath PA, Duffin S, Ellis J. Sharing and Empathy in Digital Spaces: Qualitative Study of Online Health Forums for Breast Cancer and Motor Neuron Disease (Amyotrophic Lateral Sclerosis) J Med Internet Res. 2018 Jun 14;20(6):e222. doi: 10.2196/jmir.9709. https://www.jmir.org/2018/6/e222/ v20i6e222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee E, Cooper RJ. Codeine Addiction and Internet Forum Use and Support: Qualitative Netnographic Study. JMIR Ment Health. 2019 Apr 25;6(4):e12354. doi: 10.2196/12354. https://mental.jmir.org/2019/4/e12354/ v6i4e12354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moore D, Drey N, Ayers S. A meta-synthesis of women's experiences of online forums for maternal mental illness and stigma. Arch Womens Ment Health. 2020 Aug;23(4):507–515. doi: 10.1007/s00737-019-01002-1.10.1007/s00737-019-01002-1 [DOI] [PubMed] [Google Scholar]
- 49.Prescott J, Hanley T, Ujhelyi Gomez K. Why do young people use online forums for mental health and emotional support? Benefits and challenges. British Journal of Guidance & Counselling. 2019 May 20;47(3):317–327. doi: 10.1080/03069885.2019.1619169. [DOI] [Google Scholar]
- 50.Prescott J, Hanley T, Ujhelyi K. Peer Communication in Online Mental Health Forums for Young People: Directional and Nondirectional Support. JMIR Ment Health. 2017 Aug 02;4(3):e29. doi: 10.2196/mental.6921. https://mental.jmir.org/2017/3/e29/ v4i3e29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ransom DC, La Guardia JG, Woody EZ, Boyd JL. Interpersonal interactions on online forums addressing eating concerns. Int J Eat Disord. 2010 Mar;43(2):161–170. doi: 10.1002/eat.20629. [DOI] [PubMed] [Google Scholar]
- 52.Smith-Merry J, Goggin G, Campbell A, McKenzie K, Ridout B, Baylosis C. Social Connection and Online Engagement: Insights From Interviews With Users of a Mental Health Online Forum. JMIR Ment Health. 2019 Mar 26;6(3):e11084. doi: 10.2196/11084. https://mental.jmir.org/2019/3/e11084/ v6i3e11084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tighe B, Dunn M, McKay FH, Piatkowski T. Information sought, information shared: exploring performance and image enhancing drug user-facilitated harm reduction information in online forums. Harm Reduct J. 2017 Jul 21;14(1):48. doi: 10.1186/s12954-017-0176-8. https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-017-0176-8 .10.1186/s12954-017-0176-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Widemalm M, Hjärthag F. The forum as a friend: parental mental illness and communication on open Internet forums. Soc Psychiatry Psychiatr Epidemiol. 2015 Oct;50(10):1601–1607. doi: 10.1007/s00127-015-1036-z.10.1007/s00127-015-1036-z [DOI] [PubMed] [Google Scholar]
- 55.Palmer NB, Myers KM, Vander Stoep A, McCarty CA, Geyer JR, Desalvo A. Attention-deficit/hyperactivity disorder and telemental health. Curr Psychiatry Rep. 2010 Oct;12(5):409–417. doi: 10.1007/s11920-010-0132-8. http://europepmc.org/abstract/MED/20625857 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Powell L, Parker J, Harpin V. What is the level of evidence for the use of currently available technologies in facilitating the self-management of difficulties associated with ADHD in children and young people? A systematic review. Eur Child Adolesc Psychiatry. 2018 Nov;27(11):1391–1412. doi: 10.1007/s00787-017-1092-x.10.1007/s00787-017-1092-x [DOI] [PubMed] [Google Scholar]
- 57.Benyakorn S, Riley SJ, Calub CA, Schweitzer JB. Current State and Model for Development of Technology-Based Care for Attention Deficit Hyperactivity Disorder. Telemed J E Health. 2016 Sep;22(9):761–768. doi: 10.1089/tmj.2015.0169. http://europepmc.org/abstract/MED/26985703 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cotelli M, Manenti R, Brambilla M, Gobbi E, Ferrari C, Binetti G, Cappa SF. Cognitive telerehabilitation in mild cognitive impairment, Alzheimer's disease and frontotemporal dementia: A systematic review. J Telemed Telecare. 2019 Feb;25(2):67–79. doi: 10.1177/1357633X17740390. [DOI] [PubMed] [Google Scholar]
- 59.Moussa Y, Mahdanian AA, Yu C, Segal M, Looper KJ, Vahia IV, Rej S. Mobile Health Technology in Late-Life Mental Illness: A Focused Literature Review. Am J Geriatr Psychiatry. 2017 Aug;25(8):865–872. doi: 10.1016/j.jagp.2017.04.003.S1064-7481(17)30280-4 [DOI] [PubMed] [Google Scholar]
- 60.Yousaf K, Mehmood Z, Saba T, Rehman A, Munshi AM, Alharbey R, Rashid M. Mobile-Health Applications for the Efficient Delivery of Health Care Facility to People with Dementia (PwD) and Support to Their Carers: A Survey. Biomed Res Int. 2019;2019:7151475. doi: 10.1155/2019/7151475. doi: 10.1155/2019/7151475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Coyle H, Traynor V, Solowij N. Computerized and virtual reality cognitive training for individuals at high risk of cognitive decline: systematic review of the literature. Am J Geriatr Psychiatry. 2015 Apr;23(4):335–359. doi: 10.1016/j.jagp.2014.04.009.S1064-7481(14)00139-0 [DOI] [PubMed] [Google Scholar]
- 62.García-Casal JA, Loizeau A, Csipke E, Franco-Martín M, Perea-Bartolomé MV, Orrell M. Computer-based cognitive interventions for people living with dementia: a systematic literature review and meta-analysis. Aging Ment Health. 2017 May;21(5):454–467. doi: 10.1080/13607863.2015.1132677. [DOI] [PubMed] [Google Scholar]
- 63.Ten Brinke LF, Davis JC, Barha CK, Liu-Ambrose T. Effects of computerized cognitive training on neuroimaging outcomes in older adults: a systematic review. BMC Geriatr. 2017 Jul 10;17(1):139. doi: 10.1186/s12877-017-0529-x. https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-017-0529-x .10.1186/s12877-017-0529-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Webb SL, Loh V, Lampit A, Bateman JE, Birney DP. Meta-Analysis of the Effects of Computerized Cognitive Training on Executive Functions: a Cross-Disciplinary Taxonomy for Classifying Outcome Cognitive Factors. Neuropsychol Rev. 2018 Jun;28(2):232–250. doi: 10.1007/s11065-018-9374-8.10.1007/s11065-018-9374-8 [DOI] [PubMed] [Google Scholar]
- 65.Benbow AA, Anderson PL. A meta-analytic examination of attrition in virtual reality exposure therapy for anxiety disorders. J Anxiety Disord. 2019 Jan;61:18–26. doi: 10.1016/j.janxdis.2018.06.006.S0887-6185(18)30052-5 [DOI] [PubMed] [Google Scholar]
- 66.Carl E, Stein AT, Levihn-Coon A, Pogue JR, Rothbaum B, Emmelkamp P, Asmundson GJG, Carlbring P, Powers MB. Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials. J Anxiety Disord. 2019 Jan;61:27–36. doi: 10.1016/j.janxdis.2018.08.003.S0887-6185(18)30246-9 [DOI] [PubMed] [Google Scholar]
- 67.Fernández-Álvarez J, Di Lernia D, Riva G. Virtual Reality for Anxiety Disorders: Rethinking a Field in Expansion. Adv Exp Med Biol. 2020;1191:389–414. doi: 10.1007/978-981-32-9705-0_21. [DOI] [PubMed] [Google Scholar]
- 68.Gaebel W, Großimlinghaus I, Mucic D, Maercker A, Zielasek J, Kerst A. EPA guidance on eMental health interventions in the treatment of posttraumatic stress disorder (PTSD) Eur Psychiatry. 2017 Mar;41:140–152. doi: 10.1016/j.eurpsy.2017.01.001.S0924-9338(17)30006-8 [DOI] [PubMed] [Google Scholar]
- 69.Titov N. Internet-delivered psychotherapy for depression in adults. Curr Opin Psychiatry. 2011 Jan;24(1):18–23. doi: 10.1097/YCO.0b013e32833ed18f. [DOI] [PubMed] [Google Scholar]
- 70.McKechnie V, Barker C, Stott J. Effectiveness of computer-mediated interventions for informal carers of people with dementia-a systematic review. Int Psychogeriatr. 2014 Oct;26(10):1619–1637. doi: 10.1017/S1041610214001045. http://journals.cambridge.org/abstract_S1041610214001045 .S1041610214001045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dölemeyer R, Tietjen A, Kersting A, Wagner B. Internet-based interventions for eating disorders in adults: a systematic review. BMC Psychiatry. 2013 Aug 06;13:207. doi: 10.1186/1471-244X-13-207. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-13-207 .1471-244X-13-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aardoom JJ, Dingemans AE, Spinhoven P, Van Furth EF. Treating eating disorders over the internet: a systematic review and future research directions. Int J Eat Disord. 2013 Sep;46(6):539–552. doi: 10.1002/eat.22135. [DOI] [PubMed] [Google Scholar]
- 73.Wilson GT, Zandberg LJ. Cognitive-behavioral guided self-help for eating disorders: effectiveness and scalability. Clin Psychol Rev. 2012 Jun;32(4):343–357. doi: 10.1016/j.cpr.2012.03.001.S0272-7358(12)00030-X [DOI] [PubMed] [Google Scholar]
- 74.Bauer S, Moessner M. Harnessing the power of technology for the treatment and prevention of eating disorders. Int J Eat Disord. 2013 Jul;46(5):508–515. doi: 10.1002/eat.22109. [DOI] [PubMed] [Google Scholar]
- 75.Moreira TDC, Signor L, Figueiró LR, Fernandes S, Bortolon CB, Benchaya MC, Ferigolo M, Barros HM. Non-adherence to telemedicine interventions for drug users: systematic review. Rev Saude Publica. 2014 Jun;48(3):521–531. doi: 10.1590/s0034-8910.2014048005130. https://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-89102014000300521&lng=en&nrm=iso&tlng=en .S0034-89102014000300521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Abuwalla Z, Clark MD, Burke B, Tannenbaum V, Patel S, Mitacek R, Gladstone T, Van Voorhees B. Long-term telemental health prevention interventions for youth: A rapid review. Internet Interv. 2018 Mar;11:20–29. doi: 10.1016/j.invent.2017.11.006. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(17)30065-9 .S2214-7829(17)30065-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shore JH, Yellowlees P, Caudill R, Johnston B, Turvey C, Mishkind M, Krupinski E, Myers K, Shore P, Kaftarian E, Hilty D. Best Practices in Videoconferencing-Based Telemental Health April 2018. Telemed J E Health. 2018 Nov;24(11):827–832. doi: 10.1089/tmj.2018.0237. [DOI] [PubMed] [Google Scholar]
- 78.Gainsbury S, Blaszczynski A. A systematic review of Internet-based therapy for the treatment of addictions. Clin Psychol Rev. 2011 Apr;31(3):490–498. doi: 10.1016/j.cpr.2010.11.007.S0272-7358(10)00177-7 [DOI] [PubMed] [Google Scholar]
- 79.Fisher E, Law E, Palermo TM, Eccleston C. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2015 Mar 23;(3):CD011118. doi: 10.1002/14651858.CD011118.pub2. http://europepmc.org/abstract/MED/25803793 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fisher E, Law E, Dudeney J, Eccleston C, Palermo TM. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2019 Apr 02;4:CD011118. doi: 10.1002/14651858.CD011118.pub3. http://europepmc.org/abstract/MED/30939227 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Garrett B, Taverner T, Masinde W, Gromala D, Shaw C, Negraeff M. A rapid evidence assessment of immersive virtual reality as an adjunct therapy in acute pain management in clinical practice. Clin J Pain. 2014 Dec;30(12):1089–1098. doi: 10.1097/AJP.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 82.Herrador Colmenero L, Perez Marmol JM, Martí-García C, Querol Zaldivar MÁ, Tapia Haro RM, Castro Sánchez AM, Aguilar-Ferrándiz ME. Effectiveness of mirror therapy, motor imagery, and virtual feedback on phantom limb pain following amputation: A systematic review. Prosthet Orthot Int. 2018 Jun;42(3):288–298. doi: 10.1177/0309364617740230. [DOI] [PubMed] [Google Scholar]
- 83.Honzel E, Murthi S, Brawn-Cinani B, Colloca G, Kier C, Varshney A, Colloca L. Virtual reality, music, and pain: developing the premise for an interdisciplinary approach to pain management. Pain. 2019 Sep;160(9):1909–1919. doi: 10.1097/j.pain.0000000000001539. http://europepmc.org/abstract/MED/30817437 .00006396-201909000-00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Charova E, Dorstyn D, Tully P, Mittag O. Web-based interventions for comorbid depression and chronic illness: a systematic review. J Telemed Telecare. 2015 Jun;21(4):189–201. doi: 10.1177/1357633X15571997.1357633X15571997 [DOI] [PubMed] [Google Scholar]
- 85.Vigerland S, Lenhard F, Bonnert M, Lalouni M, Hedman E, Ahlen J, Olén O, Serlachius E, Ljótsson B. Internet-delivered cognitive behavior therapy for children and adolescents: A systematic review and meta-analysis. Clin Psychol Rev. 2016 Dec;50:1–10. doi: 10.1016/j.cpr.2016.09.005. https://linkinghub.elsevier.com/retrieve/pii/S0272-7358(15)30090-8 .S0272-7358(15)30090-8 [DOI] [PubMed] [Google Scholar]
- 86.Wright JH, McCray LW, Eells TD, Gopalraj R, Bishop LB. Computer-Assisted Cognitive-Behavior Therapy in Medical Care Settings. Curr Psychiatry Rep. 2018 Sep 07;20(10):92. doi: 10.1007/s11920-018-0947-2.10.1007/s11920-018-0947-2 [DOI] [PubMed] [Google Scholar]
- 87.Gavin J, Rodham K, Coulson N, Watts L. Health Services and Delivery Research. Southampton: NIHR Journals Library; 2014. Meeting the support needs of patients with complex regional pain syndrome through innovative use of wiki technology: a mixed-methods study. [PubMed] [Google Scholar]
- 88.Deeken F, Rezo A, Hinz M, Discher R, Rapp MA. Evaluation of Technology-Based Interventions for Informal Caregivers of Patients With Dementia-A Meta-Analysis of Randomized Controlled Trials. Am J Geriatr Psychiatry. 2019 Apr;27(4):426–445. doi: 10.1016/j.jagp.2018.12.003.S1064-7481(18)30587-6 [DOI] [PubMed] [Google Scholar]
- 89.Ruggiano N, Brown EL, Li J, Scaccianoce M. Rural Dementia Caregivers and Technology: What Is the Evidence? Res Gerontol Nurs. 2018 Jul 01;11(4):216–224. doi: 10.3928/19404921-20180628-04. [DOI] [PubMed] [Google Scholar]
- 90.Lee E. Do Technology-Based Support Groups Reduce Care Burden Among Dementia Caregivers? A Review. J Evid Inf Soc Work. 2015;12(5):474–487. doi: 10.1080/15433714.2014.930362. [DOI] [PubMed] [Google Scholar]
- 91.Rathnayake S, Moyle W, Jones C, Calleja P. mHealth applications as an educational and supportive resource for family carers of people with dementia: An integrative review. Dementia (London) 2019;18(7-8):3091–3112. doi: 10.1177/1471301218768903. [DOI] [PubMed] [Google Scholar]
- 92.Ferguson J, Craig EA, Dounavi K. Telehealth as a Model for Providing Behaviour Analytic Interventions to Individuals with Autism Spectrum Disorder: A Systematic Review. J Autism Dev Disord. 2019 Feb;49(2):582–616. doi: 10.1007/s10803-018-3724-5. http://europepmc.org/abstract/MED/30155578 .10.1007/s10803-018-3724-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dadds MR, Thai C, Mendoza Diaz A, Broderick J, Moul C, Tully LA, Hawes DJ, Davies S, Burchfield K, Cane L. Therapist-assisted online treatment for child conduct problems in rural and urban families: Two randomized controlled trials. J Consult Clin Psychol. 2019 Aug;87(8):706–719. doi: 10.1037/ccp0000419.2019-33053-001 [DOI] [PubMed] [Google Scholar]
- 94.Parsons D, Cordier R, Vaz S, Lee HC. Parent-Mediated Intervention Training Delivered Remotely for Children With Autism Spectrum Disorder Living Outside of Urban Areas: Systematic Review. J Med Internet Res. 2017 Aug 14;19(8):e198. doi: 10.2196/jmir.6651. https://www.jmir.org/2017/8/e198/ v19i8e198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sheehan R, Hassiotis A. Digital mental health and intellectual disabilities: state of the evidence and future directions. Evid Based Ment Health. 2017 Nov;20(4):107–111. doi: 10.1136/eb-2017-102759.eb-2017-102759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gilmore AK, Wilson SM, Skopp NA, Osenbach JE, Reger G. A systematic review of technology-based interventions for co-occurring substance use and trauma symptoms. J Telemed Telecare. 2017 Sep;23(8):701–709. doi: 10.1177/1357633X16664205.1357633X16664205 [DOI] [PubMed] [Google Scholar]
- 97.Batastini AB, King CM, Morgan RD, McDaniel B. Telepsychological services with criminal justice and substance abuse clients: A systematic review and meta-analysis. Psychol Serv. 2016 Feb;13(1):20–30. doi: 10.1037/ser0000042.2015-31580-001 [DOI] [PubMed] [Google Scholar]
- 98.Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for drug and alcohol abuse and smoking addiction: is human contact necessary for therapeutic efficacy? Clin Psychol Rev. 2011 Feb;31(1):178–186. doi: 10.1016/j.cpr.2010.10.002.S0272-7358(10)00168-6 [DOI] [PubMed] [Google Scholar]
- 99.Song T, Qian S, Yu P. Mobile Health Interventions for Self-Control of Unhealthy Alcohol Use: Systematic Review. JMIR Mhealth Uhealth. 2019 Jan 29;7(1):e10899. doi: 10.2196/10899. https://mhealth.jmir.org/2019/1/e10899/ v7i1e10899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dallery J, Jarvis B, Marsch L, Xie H. Mechanisms of change associated with technology-based interventions for substance use. Drug Alcohol Depend. 2015 May 01;150:14–23. doi: 10.1016/j.drugalcdep.2015.02.036. http://europepmc.org/abstract/MED/25813268 .S0376-8716(15)00139-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Boumparis N, Karyotaki E, Schaub MP, Cuijpers P, Riper H. Internet interventions for adult illicit substance users: a meta-analysis. Addiction. 2017 Sep;112(9):1521–1532. doi: 10.1111/add.13819. http://europepmc.org/abstract/MED/28295758 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Carey KB, Scott-Sheldon LAJ, Elliott JC, Garey L, Carey MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: a meta-analytic review, 1998 to 2010. Clin Psychol Rev. 2012 Dec;32(8):690–703. doi: 10.1016/j.cpr.2012.08.001. http://europepmc.org/abstract/MED/23022767 .S0272-7358(12)00114-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Donoghue K, Patton R, Phillips T, Deluca P, Drummond C. The effectiveness of electronic screening and brief intervention for reducing levels of alcohol consumption: a systematic review and meta-analysis. J Med Internet Res. 2014 Jun 02;16(6):e142. doi: 10.2196/jmir.3193. https://www.jmir.org/2014/6/e142/ v16i6e142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Garnett CV, Crane D, Brown J, Kaner EFS, Beyer FR, Muirhead CR, Hickman M, Beard E, Redmore J, de Vocht F, Michie S. Behavior Change Techniques Used in Digital Behavior Change Interventions to Reduce Excessive Alcohol Consumption: A Meta-regression. Ann Behav Med. 2018 May 18;52(6):530–543. doi: 10.1093/abm/kax029. http://europepmc.org/abstract/MED/29788261 .4827558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kiluk BD, Ray LA, Walthers J, Bernstein M, Tonigan JS, Magill M. Technology-Delivered Cognitive-Behavioral Interventions for Alcohol Use: A Meta-Analysis. Alcohol Clin Exp Res. 2019 Nov;43(11):2285–2295. doi: 10.1111/acer.14189. http://europepmc.org/abstract/MED/31566787 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lin LA, Casteel D, Shigekawa E, Weyrich MS, Roby DH, McMenamin SB. Telemedicine-delivered treatment interventions for substance use disorders: A systematic review. J Subst Abuse Treat. 2019 Jun;101:38–49. doi: 10.1016/j.jsat.2019.03.007.S0740-5472(18)30428-8 [DOI] [PubMed] [Google Scholar]
- 107.Moore BA, Fazzino T, Garnet B, Cutter CJ, Barry DT. Computer-based interventions for drug use disorders: a systematic review. J Subst Abuse Treat. 2011 Apr;40(3):215–223. doi: 10.1016/j.jsat.2010.11.002. http://europepmc.org/abstract/MED/21185683 .S0740-5472(10)00235-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Olmos A, Tirado-Muñoz J, Farré M, Torrens M. The efficacy of computerized interventions to reduce cannabis use: A systematic review and meta-analysis. Addict Behav. 2018 Apr;79:52–60. doi: 10.1016/j.addbeh.2017.11.045.S0306-4603(17)30453-7 [DOI] [PubMed] [Google Scholar]
- 109.Riper H, Hoogendoorn A, Cuijpers P, Karyotaki E, Boumparis N, Mira A, Andersson G, Berman AH, Bertholet N, Bischof G, Blankers M, Boon B, Boß L, Brendryen H, Cunningham J, Ebert D, Hansen A, Hester R, Khadjesari Z, Kramer J, Murray E, Postel M, Schulz D, Sinadinovic K, Suffoletto B, Sundström C, de Vries H, Wallace P, Wiers RW, Smit JH. Effectiveness and treatment moderators of internet interventions for adult problem drinking: An individual patient data meta-analysis of 19 randomised controlled trials. PLoS Med. 2018 Dec;15(12):e1002714. doi: 10.1371/journal.pmed.1002714. https://dx.plos.org/10.1371/journal.pmed.1002714 .PMEDICINE-D-18-01494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rooke S, Thorsteinsson E, Karpin A, Copeland J, Allsop D. Computer-delivered interventions for alcohol and tobacco use: a meta-analysis. Addiction. 2010 Aug;105(8):1381–1390. doi: 10.1111/j.1360-0443.2010.02975.x.ADD2975 [DOI] [PubMed] [Google Scholar]
- 111.Tait RJ, Christensen H. Internet-based interventions for young people with problematic substance use: a systematic review. Med J Aust. 2010 Jun 07;192(S11):S15–S21. doi: 10.5694/j.1326-5377.2010.tb03687.x.tai10832_fm [DOI] [PubMed] [Google Scholar]
- 112.Vernon ML. A review of computer-based alcohol problem services designed for the general public. J Subst Abuse Treat. 2010 Apr;38(3):203–211. doi: 10.1016/j.jsat.2009.11.001. http://europepmc.org/abstract/MED/20015607 .S0740-5472(09)00184-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.White A, Kavanagh D, Stallman H, Klein B, Kay-Lambkin F, Proudfoot J, Drennan J, Connor J, Baker A, Hines E, Young R. Online alcohol interventions: a systematic review. J Med Internet Res. 2010 Dec 19;12(5):e62. doi: 10.2196/jmir.1479. https://www.jmir.org/2010/5/e62/ v12i5e62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wood SK, Eckley L, Hughes K, Hardcastle KA, Bellis MA, Schrooten J, Demetrovics Z, Voorham L. Computer-based programmes for the prevention and management of illicit recreational drug use: a systematic review. Addict Behav. 2014 Jan;39(1):30–38. doi: 10.1016/j.addbeh.2013.09.010.S0306-4603(13)00269-4 [DOI] [PubMed] [Google Scholar]
- 115.Ghiţă A, Gutiérrez-Maldonado J. Applications of virtual reality in individuals with alcohol misuse: A systematic review. Addict Behav. 2018 Jun;81:1–11. doi: 10.1016/j.addbeh.2018.01.036.S0306-4603(18)30049-2 [DOI] [PubMed] [Google Scholar]
- 116.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015 Jan 01;4:1. doi: 10.1186/2046-4053-4-1. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/2046-4053-4-1 .2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Baum RA, Epstein JN, Kelleher K. Healthcare reform, quality, and technology: ADHD as a case study. Curr Psychiatry Rep. 2013 Jul;15(7):369. doi: 10.1007/s11920-013-0369-0. http://europepmc.org/abstract/MED/23712720 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, Davies EB. Annual Research Review: Digital health interventions for children and young people with mental health problems - a systematic and meta-review. J Child Psychol Psychiatry. 2017 Apr;58(4):474–503. doi: 10.1111/jcpp.12663. [DOI] [PubMed] [Google Scholar]
- 119.Valentine AZ, Hall SS, Young E, Brown BJ, Groom MJ, Hollis C, Hall CL. Implementation of Telehealth Services to Assess, Monitor, and Treat Neurodevelopmental Disorders: Systematic Review. J Med Internet Res. 2021 Jan 20;23(1):e22619. doi: 10.2196/22619. https://www.jmir.org/2021/1/e22619/ v23i1e22619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Emmelkamp PMG, Meyerbröker K. Virtual Reality Therapy in Mental Health. Annu Rev Clin Psychol. 2021 May 07;17:495–519. doi: 10.1146/annurev-clinpsy-081219-115923. [DOI] [PubMed] [Google Scholar]
- 121.Pandian GSB, Jain A, Raza Q, Sahu KK. Digital health interventions (DHI) for the treatment of attention deficit hyperactivity disorder (ADHD) in children - a comparative review of literature among various treatment and DHI. Psychiatry Res. 2021 Mar;297:113742. doi: 10.1016/j.psychres.2021.113742.S0165-1781(21)00039-1 [DOI] [PubMed] [Google Scholar]
- 122.Oldrati V, Corti C, Poggi G, Borgatti R, Urgesi C, Bardoni A. Effectiveness of Computerized Cognitive Training Programs (CCTP) with Game-like Features in Children with or without Neuropsychological Disorders: a Meta-Analytic Investigation. Neuropsychol Rev. 2020 Mar;30(1):126–141. doi: 10.1007/s11065-020-09429-5.10.1007/s11065-020-09429-5 [DOI] [PubMed] [Google Scholar]
- 123.Andersson G, Topooco N, Havik O, Nordgreen T. Internet-supported versus face-to-face cognitive behavior therapy for depression. Expert Rev Neurother. 2016;16(1):55–60. doi: 10.1586/14737175.2015.1125783. [DOI] [PubMed] [Google Scholar]
- 124.Andersson G, Carlbring P. Internet-Assisted Cognitive Behavioral Therapy. Psychiatr Clin North Am. 2017 Dec;40(4):689–700. doi: 10.1016/j.psc.2017.08.004.S0193-953X(17)30071-0 [DOI] [PubMed] [Google Scholar]
- 125.Andrews G, Newby JM, Williams AD. Internet-delivered cognitive behavior therapy for anxiety disorders is here to stay. Curr Psychiatry Rep. 2015 Jan;17(1):533. doi: 10.1007/s11920-014-0533-1. [DOI] [PubMed] [Google Scholar]
- 126.Berryhill MB, Culmer N, Williams N, Halli-Tierney A, Betancourt A, Roberts H, King M. Videoconferencing Psychotherapy and Depression: A Systematic Review. Telemed J E Health. 2019 Jun;25(6):435–446. doi: 10.1089/tmj.2018.0058. [DOI] [PubMed] [Google Scholar]
- 127.Christensen LF, Moller AM, Hansen JP, Nielsen CT, Gildberg FA. Patients' and providers' experiences with video consultations used in the treatment of older patients with unipolar depression: A systematic review. J Psychiatr Ment Health Nurs. 2020 Jun;27(3):258–271. doi: 10.1111/jpm.12574. [DOI] [PubMed] [Google Scholar]
- 128.Guaiana G, Mastrangelo J, Hendrikx S, Barbui C. A Systematic Review of the Use of Telepsychiatry in Depression. Community Ment Health J. 2021 Jan;57(1):93–100. doi: 10.1007/s10597-020-00724-2. http://europepmc.org/abstract/MED/33040191 .10.1007/s10597-020-00724-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Herbst N, Voderholzer U, Stelzer N, Knaevelsrud C, Hertenstein E, Schlegl S, Nissen C, Külz AK. The potential of telemental health applications for obsessive-compulsive disorder. Clin Psychol Rev. 2012 Aug;32(6):454–466. doi: 10.1016/j.cpr.2012.04.005.S0272-7358(12)00068-2 [DOI] [PubMed] [Google Scholar]
- 130.Kruse CS, Atkins JM, Baker TD, Gonzales EN, Paul JL, Brooks M. Factors influencing the adoption of telemedicine for treatment of military veterans with post-traumatic stress disorder. J Rehabil Med. 2018 May 08;50(5):385–392. doi: 10.2340/16501977-2302. https://www.medicaljournals.se/jrm/content/abstract/10.2340/16501977-2302 . [DOI] [PubMed] [Google Scholar]
- 131.Lenferink LIM, Meyerbröker K, Boelen PA. PTSD treatment in times of COVID-19: A systematic review of the effects of online EMDR. Psychiatry Res. 2020 Nov;293:113438. doi: 10.1016/j.psychres.2020.113438. https://linkinghub.elsevier.com/retrieve/pii/S0165-1781(20)31459-1 .S0165-1781(20)31459-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.McLean SA, Booth AT, Schnabel A, Wright BJ, Painter FL, McIntosh JE. Exploring the Efficacy of Telehealth for Family Therapy Through Systematic, Meta-analytic, and Qualitative Evidence. Clin Child Fam Psychol Rev. 2021 Jun;24(2):244–266. doi: 10.1007/s10567-020-00340-2. http://europepmc.org/abstract/MED/33492545 .10.1007/s10567-020-00340-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Olthuis JV, Wozney L, Asmundson GJG, Cramm H, Lingley-Pottie P, McGrath PJ. Distance-delivered interventions for PTSD: A systematic review and meta-analysis. J Anxiety Disord. 2016 Dec;44:9–26. doi: 10.1016/j.janxdis.2016.09.010.S0887-6185(16)30274-2 [DOI] [PubMed] [Google Scholar]
- 134.Paul LA, Hassija CM, Clapp JD. Technological advances in the treatment of trauma: a review of promising practices. Behav Modif. 2012 Nov;36(6):897–923. doi: 10.1177/0145445512450733.0145445512450733 [DOI] [PubMed] [Google Scholar]
- 135.Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev. 2012 Jun;32(4):329–342. doi: 10.1016/j.cpr.2012.02.004.S0272-7358(12)00027-X [DOI] [PubMed] [Google Scholar]
- 136.Roth DE, Ramtekkar U, Zeković-Roth S. Telepsychiatry: A New Treatment Venue for Pediatric Depression. Child Adolesc Psychiatr Clin N Am. 2019 Jul;28(3):377–395. doi: 10.1016/j.chc.2019.02.007.S1056-4993(19)30028-8 [DOI] [PubMed] [Google Scholar]
- 137.Saltzman LY, Solomyak L, Pat-Horenczyk R. Addressing the Needs of Children and Youth in the Context of War and Terrorism: the Technological Frontier. Curr Psychiatry Rep. 2017 Jun;19(6):30. doi: 10.1007/s11920-017-0786-6.10.1007/s11920-017-0786-6 [DOI] [PubMed] [Google Scholar]
- 138.Sloan DM, Gallagher MW, Feinstein BA, Lee DJ, Pruneau GM. Efficacy of telehealth treatments for posttraumatic stress-related symptoms: a meta-analysis. Cogn Behav Ther. 2011;40(2):111–125. doi: 10.1080/16506073.2010.550058.937189374 [DOI] [PubMed] [Google Scholar]
- 139.Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. 2013 Mar;170(3):256–262. doi: 10.1176/appi.ajp.2012.12081064.1655117 [DOI] [PubMed] [Google Scholar]
- 140.Sunjaya AP, Chris A, Novianti D. Efficacy, patient-doctor relationship, costs and benefits of utilizing telepsychiatry for the management of post-traumatic stress disorder (PTSD): a systematic review. Trends Psychiatry Psychother. 2020;42(1):102–110. doi: 10.1590/2237-6089-2019-0024. doi: 10.1590/2237-6089-2019-0024.S2237-60892020000100102 [DOI] [PubMed] [Google Scholar]
- 141.Turgoose D, Ashwick R, Murphy D. Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder. J Telemed Telecare. 2018 Oct;24(9):575–585. doi: 10.1177/1357633X17730443. [DOI] [PubMed] [Google Scholar]
- 142.Wootton BM. Remote cognitive-behavior therapy for obsessive-compulsive symptoms: A meta-analysis. Clin Psychol Rev. 2016 Feb;43:103–113. doi: 10.1016/j.cpr.2015.10.001.S0272-7358(15)00136-1 [DOI] [PubMed] [Google Scholar]
- 143.Weightman M. Digital psychotherapy as an effective and timely treatment option for depression and anxiety disorders: Implications for rural and remote practice. J Int Med Res. 2020 Jun;48(6):300060520928686. doi: 10.1177/0300060520928686. https://journals.sagepub.com/doi/10.1177/0300060520928686?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zhao L, Chen J, Lan L, Deng N, Liao Y, Yue L, Chen I, Wen SW, Xie R. Effectiveness of Telehealth Interventions for Women With Postpartum Depression: Systematic Review and Meta-analysis. JMIR Mhealth Uhealth. 2021 Oct 07;9(10):e32544. doi: 10.2196/32544. https://mhealth.jmir.org/2021/10/e32544/ v9i10e32544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Andersson G, Carlbring P, Titov N, Lindefors N. Internet Interventions for Adults with Anxiety and Mood Disorders: A Narrative Umbrella Review of Recent Meta-Analyses. Can J Psychiatry. 2019 Jul;64(7):465–470. doi: 10.1177/0706743719839381. http://europepmc.org/abstract/MED/31096757 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One. 2010 Oct 13;5(10):e13196. doi: 10.1371/journal.pone.0013196. https://dx.plos.org/10.1371/journal.pone.0013196 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Andrews G, Basu A, Cuijpers P, Craske MG, McEvoy P, English CL, Newby JM. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: An updated meta-analysis. J Anxiety Disord. 2018 Apr;55:70–78. doi: 10.1016/j.janxdis.2018.01.001. https://linkinghub.elsevier.com/retrieve/pii/S0887-6185(17)30447-4 .S0887-6185(17)30447-4 [DOI] [PubMed] [Google Scholar]
- 148.Bayrampour H, Trieu J, Tharmaratnam T. Effectiveness of eHealth Interventions to Reduce Perinatal Anxiety: A Systematic Review and Meta-Analysis. J Clin Psychiatry. 2019 Jan 22;80(1):18r12386. doi: 10.4088/JCP.18r12386. [DOI] [PubMed] [Google Scholar]
- 149.Christensen H, Batterham PJ, O'Dea B. E-health interventions for suicide prevention. Int J Environ Res Public Health. 2014 Aug 12;11(8):8193–8212. doi: 10.3390/ijerph110808193. https://www.mdpi.com/resolver?pii=ijerph110808193 .ijerph110808193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Crabb RM, Cavanagh K, Proudfoot J, Learmonth D, Rafie S, Weingardt KR. Is computerized cognitive-behavioural therapy a treatment option for depression in late-life? A systematic review. Br J Clin Psychol. 2012 Nov;51(4):459–464. doi: 10.1111/j.2044-8260.2012.02038.x. [DOI] [PubMed] [Google Scholar]
- 151.Cuijpers P, Donker T, Johansson R, Mohr DC, van Straten A, Andersson G. Self-guided psychological treatment for depressive symptoms: a meta-analysis. PLoS One. 2011;6(6):e21274. doi: 10.1371/journal.pone.0021274. https://dx.plos.org/10.1371/journal.pone.0021274 .PONE-D-11-00173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Deady M, Choi I, Calvo RA, Glozier N, Christensen H, Harvey SB. eHealth interventions for the prevention of depression and anxiety in the general population: a systematic review and meta-analysis. BMC Psychiatry. 2017 Aug 29;17(1):310. doi: 10.1186/s12888-017-1473-1. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1473-1 .10.1186/s12888-017-1473-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Dèttore D, Pozza A, Andersson G. Efficacy of technology-delivered cognitive behavioural therapy for OCD versus control conditions, and in comparison with therapist-administered CBT: meta-analysis of randomized controlled trials. Cogn Behav Ther. 2015;44(3):190–211. doi: 10.1080/16506073.2015.1005660. [DOI] [PubMed] [Google Scholar]
- 154.Ebert DD, Zarski A, Christensen H, Stikkelbroek Y, Cuijpers P, Berking M, Riper H. Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: a meta-analysis of randomized controlled outcome trials. PLoS One. 2015;10(3):e0119895. doi: 10.1371/journal.pone.0119895. https://dx.plos.org/10.1371/journal.pone.0119895 .PONE-D-14-33759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Griffiths KM, Farrer L, Christensen H. The efficacy of internet interventions for depression and anxiety disorders: a review of randomised controlled trials. Med J Aust. 2010 Jun 07;192(S11):S4–S11. doi: 10.5694/j.1326-5377.2010.tb03685.x.gri10844_fm [DOI] [PubMed] [Google Scholar]
- 156.Grist R, Croker A, Denne M, Stallard P. Technology Delivered Interventions for Depression and Anxiety in Children and Adolescents: A Systematic Review and Meta-analysis. Clin Child Fam Psychol Rev. 2019 Jun;22(2):147–171. doi: 10.1007/s10567-018-0271-8. http://europepmc.org/abstract/MED/30229343 .10.1007/s10567-018-0271-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Iakimova G, Dimitrova S, Burté T. [Can we do therapy without a therapist? Active components of computer-based CBT for depression] Encephale. 2017 Dec;43(6):582–593. doi: 10.1016/j.encep.2016.08.006.S0013-7006(16)30194-4 [DOI] [PubMed] [Google Scholar]
- 158.Karyotaki E, Riper H, Twisk J, Hoogendoorn A, Kleiboer A, Mira A, Mackinnon A, Meyer B, Botella C, Littlewood E, Andersson G, Christensen H, Klein JP, Schröder J, Bretón-López J, Scheider J, Griffiths K, Farrer L, Huibers MJH, Phillips R, Gilbody S, Moritz S, Berger T, Pop V, Spek V, Cuijpers P. Efficacy of Self-guided Internet-Based Cognitive Behavioral Therapy in the Treatment of Depressive Symptoms: A Meta-analysis of Individual Participant Data. JAMA Psychiatry. 2017 Apr 01;74(4):351–359. doi: 10.1001/jamapsychiatry.2017.0044.2604310 [DOI] [PubMed] [Google Scholar]
- 159.Karyotaki E, Kemmeren L, Riper H, Twisk J, Hoogendoorn A, Kleiboer A, Mira A, Mackinnon A, Meyer B, Botella C, Littlewood E, Andersson G, Christensen H, Klein JP, Schröder J, Bretón-López J, Scheider J, Griffiths K, Farrer L, Huibers MJH, Phillips R, Gilbody S, Moritz S, Berger T, Pop V, Spek V, Cuijpers P. Is self-guided internet-based cognitive behavioural therapy (iCBT) harmful? An individual participant data meta-analysis. Psychol Med. 2018 Nov;48(15):2456–2466. doi: 10.1017/S0033291718000648. http://europepmc.org/abstract/MED/29540243 .S0033291718000648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kendall PC, Khanna MS, Edson A, Cummings C, Harris MS. Computers and psychosocial treatment for child anxiety: recent advances and ongoing efforts. Depress Anxiety. 2011 Jan;28(1):58–66. doi: 10.1002/da.20757. [DOI] [PubMed] [Google Scholar]
- 161.Lee EW, Denison FC, Hor K, Reynolds RM. Web-based interventions for prevention and treatment of perinatal mood disorders: a systematic review. BMC Pregnancy Childbirth. 2016 Feb 29;16:38. doi: 10.1186/s12884-016-0831-1. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-016-0831-1 .10.1186/s12884-016-0831-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Loughnan SA, Joubert AE, Grierson A, Andrews G, Newby JM. Internet-delivered psychological interventions for clinical anxiety and depression in perinatal women: a systematic review and meta-analysis. Arch Womens Ment Health. 2019 Dec;22(6):737–750. doi: 10.1007/s00737-019-00961-9.10.1007/s00737-019-00961-9 [DOI] [PubMed] [Google Scholar]
- 163.Lowther H, Newman E. Attention bias modification (ABM) as a treatment for child and adolescent anxiety: a systematic review. J Affect Disord. 2014 Oct;168:125–135. doi: 10.1016/j.jad.2014.06.051.S0165-0327(14)00419-4 [DOI] [PubMed] [Google Scholar]
- 164.Martínez P, Rojas G, Martínez V, Lara MA, Pérez JC. Internet-based interventions for the prevention and treatment of depression in people living in developing countries: A systematic review. J Affect Disord. 2018 Jul;234:193–200. doi: 10.1016/j.jad.2018.02.079.S0165-0327(17)32567-3 [DOI] [PubMed] [Google Scholar]
- 165.Melville KM, Casey LM, Kavanagh DJ. Dropout from Internet-based treatment for psychological disorders. Br J Clin Psychol. 2010 Nov;49(Pt 4):455–471. doi: 10.1348/014466509X472138.bjcp840 [DOI] [PubMed] [Google Scholar]
- 166.Morimoto SS, Wexler BE, Alexopoulos GS. Neuroplasticity-based computerized cognitive remediation for geriatric depression. Int J Geriatr Psychiatry. 2012 Dec;27(12):1239–1247. doi: 10.1002/gps.3776. http://europepmc.org/abstract/MED/22451346 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Peñate W, Fumero A. A meta-review of Internet computer-based psychological treatments for anxiety disorders. J Telemed Telecare. 2016 Jan;22(1):3–11. doi: 10.1177/1357633X15586491.1357633X15586491 [DOI] [PubMed] [Google Scholar]
- 168.Rasing SPA, Stikkelbroek YAJ, Bodden DHM. Is Digital Treatment the Holy Grail? Literature Review on Computerized and Blended Treatment for Depressive Disorders in Youth. Int J Environ Res Public Health. 2019 Dec 24;17(1):153. doi: 10.3390/ijerph17010153. https://www.mdpi.com/resolver?pii=ijerph17010153 .ijerph17010153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Richardson T, Stallard P, Velleman S. Computerised cognitive behavioural therapy for the prevention and treatment of depression and anxiety in children and adolescents: a systematic review. Clin Child Fam Psychol Rev. 2010 Sep;13(3):275–290. doi: 10.1007/s10567-010-0069-9. [DOI] [PubMed] [Google Scholar]
- 170.Shim M, Mahaffey B, Bleidistel M, Gonzalez A. A scoping review of human-support factors in the context of Internet-based psychological interventions (IPIs) for depression and anxiety disorders. Clin Psychol Rev. 2017 Nov;57:129–140. doi: 10.1016/j.cpr.2017.09.003.S0272-7358(17)30097-1 [DOI] [PubMed] [Google Scholar]
- 171.Siemer CP, Fogel J, Van Voorhees BW. Telemental health and web-based applications in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2011 Jan;20(1):135–153. doi: 10.1016/j.chc.2010.08.012. http://europepmc.org/abstract/MED/21092918 .S1056-4993(10)00076-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Sijbrandij M, Kunovski I, Cuijpers P. Effectiveness of Internet-Delivered Cognitive Behavioral Therapy for Posttraumatic Stress Disorder: A Systematic Review and Meta-Analysis. Depress Anxiety. 2016 Sep;33(9):783–791. doi: 10.1002/da.22533. [DOI] [PubMed] [Google Scholar]
- 173.Sikorski C, Luppa M, Kersting A, König HH, Riedel-Heller SG. [Computer-aided cognitive behavioral therapy for depression] Psychiatr Prax. 2011 Feb;38(2):61–68. doi: 10.1055/s-0030-1248575. [DOI] [PubMed] [Google Scholar]
- 174.So M, Yamaguchi S, Hashimoto S, Sado M, Furukawa TA, McCrone P. Is computerised CBT really helpful for adult depression?-A meta-analytic re-evaluation of CCBT for adult depression in terms of clinical implementation and methodological validity. BMC Psychiatry. 2013 Apr 15;13:113. doi: 10.1186/1471-244X-13-113. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-13-113 .1471-244X-13-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Spurgeon JA, Wright JH. Computer-assisted cognitive-behavioral therapy. Curr Psychiatry Rep. 2010 Dec;12(6):547–552. doi: 10.1007/s11920-010-0152-4. [DOI] [PubMed] [Google Scholar]
- 176.Stefanopoulou E, Lewis D, Taylor M, Broscombe J, Larkin J. Digitally Delivered Psychological Interventions for Anxiety Disorders: a Comprehensive Review. Psychiatr Q. 2019 Mar;90(1):197–215. doi: 10.1007/s11126-018-9620-5.10.1007/s11126-018-9620-5 [DOI] [PubMed] [Google Scholar]
- 177.Vallury KD, Jones M, Oosterbroek C. Computerized Cognitive Behavior Therapy for Anxiety and Depression in Rural Areas: A Systematic Review. J Med Internet Res. 2015 Jun 05;17(6):e139. doi: 10.2196/jmir.4145. https://www.jmir.org/2015/6/e139/ v17i6e139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wells MJ, Owen JJ, McCray LW, Bishop LB, Eells TD, Brown GK, Richards D, Thase ME, Wright JH. Computer-Assisted Cognitive-Behavior Therapy for Depression in Primary Care: Systematic Review and Meta-Analysis. Prim Care Companion CNS Disord. 2018 Mar 01;20(2):17r02196. doi: 10.4088/PCC.17r02196. http://www.psychiatrist.com/pcc/computer-assisted-cbt-for-depression-in-primary-care . [DOI] [PubMed] [Google Scholar]
- 179.Wilks CR, Zieve GG, Lessing HK. Are Trials of Computerized Therapy Generalizable? A Multidimensional Meta-analysis. Telemed J E Health. 2016 May;22(5):450–457. doi: 10.1089/tmj.2015.0129. http://europepmc.org/abstract/MED/26461235 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Wright JH, Mishkind M, Eells TD, Chan SR. Computer-Assisted Cognitive-Behavior Therapy and Mobile Apps for Depression and Anxiety. Curr Psychiatry Rep. 2019 Jun 27;21(7):62. doi: 10.1007/s11920-019-1031-2.10.1007/s11920-019-1031-2 [DOI] [PubMed] [Google Scholar]
- 181.Wright JH, Owen JJ, Richards D, Eells TD, Richardson T, Brown GK, Barrett M, Rasku MA, Polser G, Thase ME. Computer-Assisted Cognitive-Behavior Therapy for Depression: A Systematic Review and Meta-Analysis. J Clin Psychiatry. 2019 Mar 19;80(2):18r12188. doi: 10.4088/JCP.18r12188. http://www.psychiatrist.com/JCP/article/Pages/2019/v80/18r12188.aspx . [DOI] [PubMed] [Google Scholar]
- 182.Ye Y, Zhang Y, Chen J, Liu J, Li X, Liu Y, Lang Y, Lin L, Yang X, Jiang X. Internet-Based Cognitive Behavioral Therapy for Insomnia (ICBT-i) Improves Comorbid Anxiety and Depression-A Meta-Analysis of Randomized Controlled Trials. PLoS One. 2015;10(11):e0142258. doi: 10.1371/journal.pone.0142258. https://dx.plos.org/10.1371/journal.pone.0142258 .PONE-D-15-29392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Kampmann IL, Emmelkamp PMG, Morina N. Meta-analysis of technology-assisted interventions for social anxiety disorder. J Anxiety Disord. 2016 Aug;42:71–84. doi: 10.1016/j.janxdis.2016.06.007.S0887-6185(16)30097-4 [DOI] [PubMed] [Google Scholar]
- 184.Suso-Ribera C, Fernández-Álvarez J, García-Palacios A, Hoffman HG, Bretón-López J, Baños RM, Quero S, Botella C. Virtual Reality, Augmented Reality, and In Vivo Exposure Therapy: A Preliminary Comparison of Treatment Efficacy in Small Animal Phobia. Cyberpsychol Behav Soc Netw. 2019 Jan;22(1):31–38. doi: 10.1089/cyber.2017.0672. http://europepmc.org/abstract/MED/30335525 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Callan JA, Wright J, Siegle GJ, Howland RH, Kepler BB. Use of Computer and Mobile Technologies in the Treatment of Depression. Arch Psychiatr Nurs. 2017 Jun;31(3):311–318. doi: 10.1016/j.apnu.2016.10.002.S0883-9417(16)30317-X [DOI] [PubMed] [Google Scholar]
- 186.Nair U, Armfield NR, Chatfield MD, Edirippulige S. The effectiveness of telemedicine interventions to address maternal depression: A systematic review and meta-analysis. J Telemed Telecare. 2018 Dec;24(10):639–650. doi: 10.1177/1357633X18794332. [DOI] [PubMed] [Google Scholar]
- 187.Søgaard Neilsen A, Wilson RL. Combining e-mental health intervention development with human computer interaction (HCI) design to enhance technology-facilitated recovery for people with depression and/or anxiety conditions: An integrative literature review. Int J Ment Health Nurs. 2019 Feb;28(1):22–39. doi: 10.1111/inm.12527. [DOI] [PubMed] [Google Scholar]
- 188.Fu Z, Burger H, Arjadi R, Bockting CLH. Effectiveness of digital psychological interventions for mental health problems in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry. 2020 Oct;7(10):851–864. doi: 10.1016/S2215-0366(20)30256-X. http://europepmc.org/abstract/MED/32866459 .S2215-0366(20)30256-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Orsolini L, Pompili S, Salvi V, Volpe U. A Systematic Review on TeleMental Health in Youth Mental Health: Focus on Anxiety, Depression and Obsessive-Compulsive Disorder. Medicina (Kaunas) 2021 Jul 31;57(8):793. doi: 10.3390/medicina57080793. https://www.mdpi.com/resolver?pii=medicina57080793 .medicina57080793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Stech EP, Lim J, Upton EL, Newby JM. Internet-delivered cognitive behavioral therapy for panic disorder with or without agoraphobia: a systematic review and meta-analysis. Cogn Behav Ther. 2020 Jul;49(4):270–293. doi: 10.1080/16506073.2019.1628808. [DOI] [PubMed] [Google Scholar]
- 191.Burger F, Neerincx MA, Brinkman W. Technological State of the Art of Electronic Mental Health Interventions for Major Depressive Disorder: Systematic Literature Review. J Med Internet Res. 2020 Jan 20;22(1):e12599. doi: 10.2196/12599. https://www.jmir.org/2020/1/e12599/ v22i1e12599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Roman M, Constantin T, Bostan CM. The efficiency of online cognitive-behavioral therapy for postpartum depressive symptomatology: a systematic review and meta-analysis. Women Health. 2020 Jan;60(1):99–112. doi: 10.1080/03630242.2019.1610824. [DOI] [PubMed] [Google Scholar]
- 193.Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, Sarris J. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry. 2017 Oct;16(3):287–298. doi: 10.1002/wps.20472. doi: 10.1002/wps.20472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Alyami M, Giri B, Alyami H, Sundram F. Social anxiety apps: a systematic review and assessment of app descriptors across mobile store platforms. Evid Based Ment Health. 2017 Aug;20(3):65–70. doi: 10.1136/eb-2017-102664.eb-2017-102664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Bry LJ, Chou T, Miguel E, Comer JS. Consumer Smartphone Apps Marketed for Child and Adolescent Anxiety: A Systematic Review and Content Analysis. Behav Ther. 2018 Mar;49(2):249–261. doi: 10.1016/j.beth.2017.07.008. http://europepmc.org/abstract/MED/29530263 .S0005-7894(17)30084-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Decker V, Valenti M, Montoya V, Sikorskii A, Given CW, Given BA. Maximizing New Technologies to Treat Depression. Issues Ment Health Nurs. 2019 Mar;40(3):200–207. doi: 10.1080/01612840.2018.1527422. [DOI] [PubMed] [Google Scholar]
- 197.Firth J, Torous J, Carney R, Newby J, Cosco TD, Christensen H, Sarris J. Digital Technologies in the Treatment of Anxiety: Recent Innovations and Future Directions. Curr Psychiatry Rep. 2018 May 19;20(6):44. doi: 10.1007/s11920-018-0910-2. http://europepmc.org/abstract/MED/29779065 .10.1007/s11920-018-0910-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Frank E, Pong J, Asher Y, Soares CN. Smart phone technologies and ecological momentary data: is this the way forward on depression management and research? Curr Opin Psychiatry. 2018 Jan;31(1):3–6. doi: 10.1097/YCO.0000000000000382. [DOI] [PubMed] [Google Scholar]
- 199.Loo Gee B, Griffiths KM, Gulliver A. Effectiveness of mobile technologies delivering Ecological Momentary Interventions for stress and anxiety: a systematic review. J Am Med Inform Assoc. 2016 Jan;23(1):221–229. doi: 10.1093/jamia/ocv043. http://europepmc.org/abstract/MED/25997643 .ocv043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Van Ameringen M, Turna J, Khalesi Z, Pullia K, Patterson B. There is an app for that! The current state of mobile applications (apps) for DSM-5 obsessive-compulsive disorder, posttraumatic stress disorder, anxiety and mood disorders. Depress Anxiety. 2017 Jun;34(6):526–539. doi: 10.1002/da.22657. [DOI] [PubMed] [Google Scholar]
- 201.Basit SA, Mathews N, Kunik ME. Telemedicine interventions for medication adherence in mental illness: A systematic review. Gen Hosp Psychiatry. 2020;62:28–36. doi: 10.1016/j.genhosppsych.2019.11.004.S0163-8343(19)30271-3 [DOI] [PubMed] [Google Scholar]
- 202.Jones C, Miguel-Cruz A, Smith-MacDonald L, Cruikshank E, Baghoori D, Kaur Chohan A, Laidlaw A, White A, Cao B, Agyapong V, Burback L, Winkler O, Sevigny PR, Dennett L, Ferguson-Pell M, Greenshaw A, Brémault-Phillips S. Virtual Trauma-Focused Therapy for Military Members, Veterans, and Public Safety Personnel With Posttraumatic Stress Injury: Systematic Scoping Review. JMIR Mhealth Uhealth. 2020 Sep 21;8(9):e22079. doi: 10.2196/22079. https://mhealth.jmir.org/2020/9/e22079/ v8i9e22079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Grossman JT, Frumkin MR, Rodebaugh TL, Lenze EJ. mHealth Assessment and Intervention of Depression and Anxiety in Older Adults. Harv Rev Psychiatry. 2020;28(3):203–214. doi: 10.1097/HRP.0000000000000255. http://europepmc.org/abstract/MED/32310834 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Hidalgo-Mazzei D, Llach C, Vieta E. mHealth in affective disorders: hype or hope? A focused narrative review. Int Clin Psychopharmacol. 2020 Mar;35(2):61–68. doi: 10.1097/YIC.0000000000000302.00004850-202003000-00001 [DOI] [PubMed] [Google Scholar]
- 205.Diemer J, Mühlberger A, Pauli P, Zwanzger P. Virtual reality exposure in anxiety disorders: impact on psychophysiological reactivity. World J Biol Psychiatry. 2014 Aug;15(6):427–442. doi: 10.3109/15622975.2014.892632. [DOI] [PubMed] [Google Scholar]
- 206.Botella C, Fernández-Álvarez J, Guillén V, García-Palacios A, Baños R. Recent Progress in Virtual Reality Exposure Therapy for Phobias: A Systematic Review. Curr Psychiatry Rep. 2017 Jul;19(7):42. doi: 10.1007/s11920-017-0788-4.10.1007/s11920-017-0788-4 [DOI] [PubMed] [Google Scholar]
- 207.Bouchard S. Could virtual reality be effective in treating children with phobias? Expert Rev Neurother. 2011 Feb;11(2):207–213. doi: 10.1586/ern.10.196. [DOI] [PubMed] [Google Scholar]
- 208.Deng W, Hu D, Xu S, Liu X, Zhao J, Chen Q, Liu J, Zhang Z, Jiang W, Ma L, Hong X, Cheng S, Liu B, Li X. The efficacy of virtual reality exposure therapy for PTSD symptoms: A systematic review and meta-analysis. J Affect Disord. 2019 Oct 01;257:698–709. doi: 10.1016/j.jad.2019.07.086.S0165-0327(19)30832-8 [DOI] [PubMed] [Google Scholar]
- 209.Diemer J, Zwanzger P. [Development of virtual reality as an exposure technique] Nervenarzt. 2019 Jul;90(7):715–723. doi: 10.1007/s00115-019-0678-6.10.1007/s00115-019-0678-6 [DOI] [PubMed] [Google Scholar]
- 210.Fernández-Álvarez J, Rozental A, Carlbring P, Colombo D, Riva G, Anderson PL, Baños RM, Benbow AA, Bouchard S, Bretón-López JM, Cárdenas G, Difede J, Emmelkamp P, García-Palacios A, Guillén V, Hoffman H, Kampann I, Moldovan R, Mühlberger A, North M, Pauli P, Peñate Castro W, Quero S, Tortella-Feliu M, Wyka K, Botella C. Deterioration rates in Virtual Reality Therapy: An individual patient data level meta-analysis. J Anxiety Disord. 2019 Jan;61:3–17. doi: 10.1016/j.janxdis.2018.06.005.S0887-6185(17)30611-4 [DOI] [PubMed] [Google Scholar]
- 211.Freeman D, Reeve S, Robinson A, Ehlers A, Clark D, Spanlang B, Slater M. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol Med. 2017 Oct;47(14):2393–2400. doi: 10.1017/S003329171700040X. http://europepmc.org/abstract/MED/28325167 .S003329171700040X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Gerardi M, Cukor J, Difede J, Rizzo A, Rothbaum BO. Virtual reality exposure therapy for post-traumatic stress disorder and other anxiety disorders. Curr Psychiatry Rep. 2010 Aug;12(4):298–305. doi: 10.1007/s11920-010-0128-4. [DOI] [PubMed] [Google Scholar]
- 213.Gonçalves R, Pedrozo AL, Coutinho ESF, Figueira I, Ventura P. Efficacy of virtual reality exposure therapy in the treatment of PTSD: a systematic review. PLoS One. 2012;7(12):e48469. doi: 10.1371/journal.pone.0048469. https://dx.plos.org/10.1371/journal.pone.0048469 .PONE-D-12-18828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Ling Y, Nefs HT, Morina N, Heynderickx I, Brinkman W. A meta-analysis on the relationship between self-reported presence and anxiety in virtual reality exposure therapy for anxiety disorders. PLoS One. 2014;9(5):e96144. doi: 10.1371/journal.pone.0096144. https://dx.plos.org/10.1371/journal.pone.0096144 .PONE-D-13-42501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Maples-Keller JL, Bunnell BE, Kim S, Rothbaum BO. The Use of Virtual Reality Technology in the Treatment of Anxiety and Other Psychiatric Disorders. Harv Rev Psychiatry. 2017;25(3):103–113. doi: 10.1097/HRP.0000000000000138. http://europepmc.org/abstract/MED/28475502 .00023727-201705000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.McCann RA, Armstrong CM, Skopp NA, Edwards-Stewart A, Smolenski DJ, June JD, Metzger-Abamukong M, Reger GM. Virtual reality exposure therapy for the treatment of anxiety disorders: an evaluation of research quality. J Anxiety Disord. 2014 Aug;28(6):625–631. doi: 10.1016/j.janxdis.2014.05.010.S0887-6185(14)00072-3 [DOI] [PubMed] [Google Scholar]
- 217.Morina N, Ijntema H, Meyerbröker K, Emmelkamp PMG. Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments. Behav Res Ther. 2015 Nov;74:18–24. doi: 10.1016/j.brat.2015.08.010.S0005-7967(15)30033-4 [DOI] [PubMed] [Google Scholar]
- 218.Motraghi TE, Seim RW, Meyer EC, Morissette SB. Virtual reality exposure therapy for the treatment of posttraumatic stress disorder: a methodological review using CONSORT guidelines. J Clin Psychol. 2014 Mar;70(3):197–208. doi: 10.1002/jclp.22051. [DOI] [PubMed] [Google Scholar]
- 219.Rizzo A, Parsons TD, Lange B, Kenny P, Buckwalter JG, Rothbaum B, Difede J, Frazier J, Newman B, Williams J, Reger G. Virtual reality goes to war: a brief review of the future of military behavioral healthcare. J Clin Psychol Med Settings. 2011 Jun;18(2):176–187. doi: 10.1007/s10880-011-9247-2. [DOI] [PubMed] [Google Scholar]
- 220.Salehi E, Mehrabi M, Fatehi F, Salehi A. Virtual Reality Therapy for Social Phobia: A Scoping Review. Stud Health Technol Inform. 2020 Jun 16;270:713–717. doi: 10.3233/SHTI200253.SHTI200253 [DOI] [PubMed] [Google Scholar]
- 221.Turner WA, Casey LM. Outcomes associated with virtual reality in psychological interventions: where are we now? Clin Psychol Rev. 2014 Dec;34(8):634–644. doi: 10.1016/j.cpr.2014.10.003.S0272-7358(14)00139-1 [DOI] [PubMed] [Google Scholar]
- 222.Vanni F, Conversano C, Del Debbio A, Landi P, Carlini M, Fanciullacci C, Bergamasco M, Di Fiorino A, Dell'Osso L. A survey on virtual environment applications to fear of public speaking. Eur Rev Med Pharmacol Sci. 2013 Jun;17(12):1561–1568. http://www.europeanreview.org/article/4450 . [PubMed] [Google Scholar]
- 223.Emmelkamp PMG, Meyerbröker K, Morina N. Virtual Reality Therapy in Social Anxiety Disorder. Curr Psychiatry Rep. 2020 May 13;22(7):32. doi: 10.1007/s11920-020-01156-1. http://europepmc.org/abstract/MED/32405657 .10.1007/s11920-020-01156-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Hussain-Shamsy N, Shah A, Vigod SN, Zaheer J, Seto E. Mobile Health for Perinatal Depression and Anxiety: Scoping Review. J Med Internet Res. 2020 Apr 13;22(4):e17011. doi: 10.2196/17011. https://www.jmir.org/2020/4/e17011/ v22i4e17011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Horigome T, Kurokawa S, Sawada K, Kudo S, Shiga K, Mimura M, Kishimoto T. Virtual reality exposure therapy for social anxiety disorder: a systematic review and meta-analysis. Psychol Med. 2020 Nov;50(15):2487–2497. doi: 10.1017/S0033291720003785.S0033291720003785 [DOI] [PubMed] [Google Scholar]
- 226.Anderson PL, Molloy A. Maximizing the impact of virtual reality exposure therapy for anxiety disorders. Curr Opin Psychol. 2020 Dec;36:153–157. doi: 10.1016/j.copsyc.2020.10.001.S2352-250X(20)30197-4 [DOI] [PubMed] [Google Scholar]
- 227.Lognoul M, Nasello J, Triffaux J. [Virtual reality exposure therapy for post-traumatic stress disorders, obsessive-compulsive disorders and anxiety disorders: Indications, added value and limitations] Encephale. 2020 Aug;46(4):293–300. doi: 10.1016/j.encep.2020.01.005.S0013-7006(20)30032-4 [DOI] [PubMed] [Google Scholar]
- 228.Kothgassner OD, Felnhofer A. Lack of research on efficacy of virtual reality exposure therapy (VRET) for anxiety disorders in children and adolescents : A systematic review. Neuropsychiatr. 2021 Jun;35(2):68–75. doi: 10.1007/s40211-020-00349-7. http://europepmc.org/abstract/MED/32372291 .10.1007/s40211-020-00349-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Eshuis LV, van Gelderen MJ, van Zuiden M, Nijdam MJ, Vermetten E, Olff M, Bakker A. Efficacy of immersive PTSD treatments: A systematic review of virtual and augmented reality exposure therapy and a meta-analysis of virtual reality exposure therapy. J Psychiatr Res. 2021 Nov;143:516–527. doi: 10.1016/j.jpsychires.2020.11.030. https://linkinghub.elsevier.com/retrieve/pii/S0022-3956(20)31089-X .S0022-3956(20)31089-X [DOI] [PubMed] [Google Scholar]
- 230.Motter JN, Pimontel MA, Rindskopf D, Devanand DP, Doraiswamy PM, Sneed JR. Computerized cognitive training and functional recovery in major depressive disorder: A meta-analysis. J Affect Disord. 2016 Jan 01;189:184–191. doi: 10.1016/j.jad.2015.09.022.S0165-0327(15)30845-4 [DOI] [PubMed] [Google Scholar]
- 231.Aref-Adib G, McCloud T, Ross J, O'Hanlon P, Appleton V, Rowe S, Murray E, Johnson S, Lobban F. Factors affecting implementation of digital health interventions for people with psychosis or bipolar disorder, and their family and friends: a systematic review. Lancet Psychiatry. 2019 Mar;6(3):257–266. doi: 10.1016/S2215-0366(18)30302-X.S2215-0366(18)30302-X [DOI] [PubMed] [Google Scholar]
- 232.Naslund JA, Marsch LA, McHugo GJ, Bartels SJ. Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. J Ment Health. 2015;24(5):321–332. doi: 10.3109/09638237.2015.1019054. http://europepmc.org/abstract/MED/26017625 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Gliddon E, Barnes SJ, Murray G, Michalak EE. Online and mobile technologies for self-management in bipolar disorder: A systematic review. Psychiatr Rehabil J. 2017 Sep;40(3):309–319. doi: 10.1037/prj0000270.2017-25109-001 [DOI] [PubMed] [Google Scholar]
- 234.Hidalgo-Mazzei D, Mateu A, Reinares M, Matic A, Vieta E, Colom F. Internet-based psychological interventions for bipolar disorder: Review of the present and insights into the future. J Affect Disord. 2015 Dec 01;188:1–13. doi: 10.1016/j.jad.2015.08.005.S0165-0327(15)30369-4 [DOI] [PubMed] [Google Scholar]
- 235.Leitan ND, Michalak EE, Berk L, Berk M, Murray G. Optimizing delivery of recovery-oriented online self-management strategies for bipolar disorder: a review. Bipolar Disord. 2015 Mar;17(2):115–127. doi: 10.1111/bdi.12258. [DOI] [PubMed] [Google Scholar]
- 236.Biagianti B, Hidalgo-Mazzei D, Meyer N. Developing digital interventions for people living with serious mental illness: perspectives from three mHealth studies. Evid Based Ment Health. 2017 Nov;20(4):98–101. doi: 10.1136/eb-2017-102765. http://europepmc.org/abstract/MED/29025862 .eb-2017-102765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Nicholas J, Larsen ME, Proudfoot J, Christensen H. Mobile Apps for Bipolar Disorder: A Systematic Review of Features and Content Quality. J Med Internet Res. 2015 Aug 17;17(8):e198. doi: 10.2196/jmir.4581. https://www.jmir.org/2015/8/e198/ v17i8e198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Brearly TW, Shura RD, Martindale SL, Lazowski RA, Luxton DD, Shenal BV, Rowland JA. Neuropsychological Test Administration by Videoconference: A Systematic Review and Meta-Analysis. Neuropsychol Rev. 2017 Jun;27(2):174–186. doi: 10.1007/s11065-017-9349-1.10.1007/s11065-017-9349-1 [DOI] [PubMed] [Google Scholar]
- 239.Sekhon H, Sekhon K, Launay C, Afililo M, Innocente N, Vahia I, Rej S, Beauchet O. Telemedicine and the rural dementia population: A systematic review. Maturitas. 2021 Jan;143:105–114. doi: 10.1016/j.maturitas.2020.09.001.S0378-5122(20)30363-7 [DOI] [PubMed] [Google Scholar]
- 240.Costanzo MC, Arcidiacono C, Rodolico A, Panebianco M, Aguglia E, Signorelli MS. Diagnostic and interventional implications of telemedicine in Alzheimer's disease and mild cognitive impairment: A literature review. Int J Geriatr Psychiatry. 2020 Jan;35(1):12–28. doi: 10.1002/gps.5219. [DOI] [PubMed] [Google Scholar]
- 241.Yi JS, Pittman CA, Price CL, Nieman CL, Oh ES. Telemedicine and Dementia Care: A Systematic Review of Barriers and Facilitators. J Am Med Dir Assoc. 2021 Jul;22(7):1396–1402.e18. doi: 10.1016/j.jamda.2021.03.015.S1525-8610(21)00311-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Gosse PJ, Kassardjian CD, Masellis M, Mitchell SB. Virtual care for patients with Alzheimer disease and related dementias during the COVID-19 era and beyond. CMAJ. 2021 Mar 15;193(11):E371–E377. doi: 10.1503/cmaj.201938. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=33722828 .193/11/E371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Gibson G, Newton L, Pritchard G, Finch T, Brittain K, Robinson L. The provision of assistive technology products and services for people with dementia in the United Kingdom. Dementia (London) 2016 Jul;15(4):681–701. doi: 10.1177/1471301214532643.1471301214532643 [DOI] [PubMed] [Google Scholar]
- 244.Gough N, Brkan L, Subramaniam P, Chiuccariello L, De Petrillo A, Mulsant BH, Bowie CR, Rajji TK. Feasibility of remotely supervised transcranial direct current stimulation and cognitive remediation: A systematic review. PLoS One. 2020;15(2):e0223029. doi: 10.1371/journal.pone.0223029. https://dx.plos.org/10.1371/journal.pone.0223029 .PONE-D-19-21285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Ruggiano N, Brown EL, Roberts L, Framil Suarez CV, Luo Y, Hao Z, Hristidis V. Chatbots to Support People With Dementia and Their Caregivers: Systematic Review of Functions and Quality. J Med Internet Res. 2021 Jun 03;23(6):e25006. doi: 10.2196/25006. https://www.jmir.org/2021/6/e25006/ v23i6e25006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Yousaf K, Mehmood Z, Awan IA, Saba T, Alharbey R, Qadah T, Alrige MA. A comprehensive study of mobile-health based assistive technology for the healthcare of dementia and Alzheimer's disease (AD) Health Care Manag Sci. 2020 Jun;23(2):287–309. doi: 10.1007/s10729-019-09486-0.10.1007/s10729-019-09486-0 [DOI] [PubMed] [Google Scholar]
- 247.Díaz Pérez E, Flórez Lozano JA. Realidad virtual y demencia. RevNeurol. 2018;66(10):344. doi: 10.33588/rn.6610.2017438. [DOI] [PubMed] [Google Scholar]
- 248.Kim O, Pang Y, Kim J. The effectiveness of virtual reality for people with mild cognitive impairment or dementia: a meta-analysis. BMC Psychiatry. 2019 Jul 12;19(1):219. doi: 10.1186/s12888-019-2180-x. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-019-2180-x .10.1186/s12888-019-2180-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Maggio MG, Maresca G, De Luca R, Stagnitti MC, Porcari B, Ferrera MC, Galletti F, Casella C, Manuli A, Calabrò RS. The Growing Use of Virtual Reality in Cognitive Rehabilitation: Fact, Fake or Vision? A Scoping Review. J Natl Med Assoc. 2019 Aug;111(4):457–463. doi: 10.1016/j.jnma.2019.01.003.S0027-9684(18)30346-8 [DOI] [PubMed] [Google Scholar]
- 250.Sitges-Maciá E, Bonete-López B, Sánchez-Cabaco A, Oltra-Cucarella J. Effects of e-Health Training and Social Support Interventions for Informal Caregivers of People with Dementia-A Narrative Review. Int J Environ Res Public Health. 2021 Jul 21;18(15):7728. doi: 10.3390/ijerph18157728. https://www.mdpi.com/resolver?pii=ijerph18157728 .ijerph18157728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Buettner LL, Yu F, Burgener SC. Evidence supporting technology-based interventions for people with early-stage Alzheimer's disease. J Gerontol Nurs. 2010 Oct;36(10):15–19. doi: 10.3928/00989134-20100831-01. [DOI] [PubMed] [Google Scholar]
- 252.Harvey PD, McGurk SR, Mahncke H, Wykes T. Controversies in Computerized Cognitive Training. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018 Nov;3(11):907–915. doi: 10.1016/j.bpsc.2018.06.008. https://linkinghub.elsevier.com/retrieve/pii/S2451-9022(18)30159-9 .S2451-9022(18)30159-9 [DOI] [PubMed] [Google Scholar]
- 253.Aresti-Bartolome N, Garcia-Zapirain B. Technologies as support tools for persons with autistic spectrum disorder: a systematic review. Int J Environ Res Public Health. 2014 Aug 04;11(8):7767–802. doi: 10.3390/ijerph110807767. https://www.mdpi.com/resolver?pii=ijerph110807767 .ijerph110807767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Boisvert M, Lang R, Andrianopoulos M, Boscardin ML. Telepractice in the assessment and treatment of individuals with autism spectrum disorders: A systematic review. Dev Neurorehabil. 2010;13(6):423–432. doi: 10.3109/17518423.2010.499889. [DOI] [PubMed] [Google Scholar]
- 255.Doyen CM, Oreve M, Desailly E, Goupil V, Zarca K, L'Hermitte Y, Chaste P, Bau M, Beaujard D, Haddadi S, Bibay A, Contejean Y, Coutrot M, Crespin L, Frioux I, Speranza M, Francois N, Kaye K. Telepsychiatry for Children and Adolescents: A Review of the PROMETTED Project. Telemed J E Health. 2018 Jan;24(1):3–10. doi: 10.1089/tmj.2017.0041. [DOI] [PubMed] [Google Scholar]
- 256.Gregory P, Alexander J, Satinsky J. Clinical telerehabilitation: applications for physiatrists. PM R. 2011 Jul;3(7):647–656; quiz 656. doi: 10.1016/j.pmrj.2011.02.024.S1934-1482(11)00172-9 [DOI] [PubMed] [Google Scholar]
- 257.Parsons TD, Riva G, Parsons S, Mantovani F, Newbutt N, Lin L, Venturini E, Hall T. Virtual Reality in Pediatric Psychology. Pediatrics. 2017 Nov;140(Suppl 2):S86–S91. doi: 10.1542/peds.2016-1758I.peds.2016-1758I [DOI] [PubMed] [Google Scholar]
- 258.Sutherland R, Trembath D, Roberts J. Telehealth and autism: A systematic search and review of the literature. Int J Speech Lang Pathol. 2018 Jun;20(3):324–336. doi: 10.1080/17549507.2018.1465123. [DOI] [PubMed] [Google Scholar]
- 259.Krysta K, Romańczyk M, Diefenbacher A, Krzystanek M. Telemedicine Treatment and Care for Patients with Intellectual Disability. Int J Environ Res Public Health. 2021 Feb 11;18(4):1746. doi: 10.3390/ijerph18041746. https://www.mdpi.com/resolver?pii=ijerph18041746 .ijerph18041746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Whittingham LM, Coons-Harding KD. Connecting People with People: Diagnosing Persons with Fetal Alcohol Spectrum Disorder Using Telehealth. J Autism Dev Disord. 2021 Apr;51(4):1067–1080. doi: 10.1007/s10803-020-04607-z.10.1007/s10803-020-04607-z [DOI] [PubMed] [Google Scholar]
- 261.Ellison KS, Guidry J, Picou P, Adenuga P, Davis TE. Telehealth and Autism Prior to and in the Age of COVID-19: A Systematic and Critical Review of the Last Decade. Clin Child Fam Psychol Rev. 2021 Sep;24(3):599–630. doi: 10.1007/s10567-021-00358-0. http://europepmc.org/abstract/MED/34114135 .10.1007/s10567-021-00358-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Sivaraman M, Fahmie TA. A systematic review of cultural adaptations in the global application of ABA-based telehealth services. J Appl Behav Anal. 2020 Sep;53(4):1838–1855. doi: 10.1002/jaba.763. [DOI] [PubMed] [Google Scholar]
- 263.Oudshoorn CEM, Frielink N, Nijs SLP, Embregts PJCM. Psychological eHealth interventions for people with intellectual disabilities: A scoping review. J Appl Res Intellect Disabil. 2021 Jul;34(4):950–972. doi: 10.1111/jar.12877. http://europepmc.org/abstract/MED/33704872 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Moon SJ, Hwang J, Hill HS, Kervin R, Birtwell KB, Torous J, McDougle CJ, Kim JW. Mobile device applications and treatment of autism spectrum disorder: a systematic review and meta-analysis of effectiveness. Arch Dis Child. 2020 May;105(5):458–462. doi: 10.1136/archdischild-2019-318258.archdischild-2019-318258 [DOI] [PubMed] [Google Scholar]
- 265.Cavalcante Neto JL, de Oliveira CC, Greco AL, Zamunér AR, Moreira RC, Tudella E. Is virtual reality effective in improving the motor performance of children with developmental coordination disorder? A systematic review. Eur J Phys Rehabil Med. 2019 Apr;55(2):291–300. doi: 10.23736/S1973-9087.18.05427-8. https://www.minervamedica.it/index2.t?show=R33Y2019N02A0291 .S1973-9087.18.05427-8 [DOI] [PubMed] [Google Scholar]
- 266.Wass SV, Porayska-Pomsta K. The uses of cognitive training technologies in the treatment of autism spectrum disorders. Autism. 2014 Nov;18(8):851–871. doi: 10.1177/1362361313499827.1362361313499827 [DOI] [PubMed] [Google Scholar]
- 267.Grynszpan O, Weiss PLT, Perez-Diaz F, Gal E. Innovative technology-based interventions for autism spectrum disorders: a meta-analysis. Autism. 2014 May;18(4):346–361. doi: 10.1177/1362361313476767.1362361313476767 [DOI] [PubMed] [Google Scholar]
- 268.Loo JHY, Bamiou D, Campbell N, Luxon LM. Computer-based auditory training (CBAT): benefits for children with language- and reading-related learning difficulties. Dev Med Child Neurol. 2010 Aug;52(8):708–717. doi: 10.1111/j.1469-8749.2010.03654.x. doi: 10.1111/j.1469-8749.2010.03654.x.DMCN3654 [DOI] [PubMed] [Google Scholar]
- 269.Ploog BO, Scharf A, Nelson D, Brooks PJ. Use of computer-assisted technologies (CAT) to enhance social, communicative, and language development in children with autism spectrum disorders. J Autism Dev Disord. 2013 Feb;43(2):301–322. doi: 10.1007/s10803-012-1571-3. [DOI] [PubMed] [Google Scholar]
- 270.Ramdoss S, Machalicek W, Rispoli M, Mulloy A, Lang R, O'Reilly M. Computer-based interventions to improve social and emotional skills in individuals with autism spectrum disorders: a systematic review. Dev Neurorehabil. 2012;15(2):119–135. doi: 10.3109/17518423.2011.651655. [DOI] [PubMed] [Google Scholar]
- 271.Duncan AB, Velasquez SE, Nelson E. Using videoconferencing to provide psychological services to rural children and adolescents: a review and case example. J Clin Child Adolesc Psychol. 2014;43(1):115–127. doi: 10.1080/15374416.2013.836452. [DOI] [PubMed] [Google Scholar]
- 272.Albano G, Hodsoll J, Kan C, Lo Coco G, Cardi V. Task-sharing interventions for patients with anorexia nervosa or their carers: a systematic evaluation of the literature and meta-analysis of outcomes. Int Rev Psychiatry. 2019 Jun;31(4):367–381. doi: 10.1080/09540261.2019.1588711. [DOI] [PubMed] [Google Scholar]
- 273.Barakat S, Maguire S, Smith KE, Mason TB, Crosby RD, Touyz S. Evaluating the role of digital intervention design in treatment outcomes and adherence to eTherapy programs for eating disorders: A systematic review and meta-analysis. Int J Eat Disord. 2019 Oct;52(10):1077–1094. doi: 10.1002/eat.23131. [DOI] [PubMed] [Google Scholar]
- 274.Loucas CE, Fairburn CG, Whittington C, Pennant ME, Stockton S, Kendall T. E-therapy in the treatment and prevention of eating disorders: A systematic review and meta-analysis. Behav Res Ther. 2014 Dec;63:122–131. doi: 10.1016/j.brat.2014.09.011. https://linkinghub.elsevier.com/retrieve/pii/S0005-7967(14)00162-4 .S0005-7967(14)00162-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Shingleton RM, Richards LK, Thompson-Brenner H. Using technology within the treatment of eating disorders: a clinical practice review. Psychotherapy (Chic) 2013 Dec;50(4):576–582. doi: 10.1037/a0031815. http://europepmc.org/abstract/MED/23527906 .2013-10230-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Machado PPP, Rodrigues TF. Treatment delivery strategies for eating disorders. Curr Opin Psychiatry. 2019 Nov;32(6):498–503. doi: 10.1097/YCO.0000000000000542. [DOI] [PubMed] [Google Scholar]
- 277.Humphreys G, Evans R, Makin H, Cooke R, Jones A. Identification of Behavior Change Techniques From Successful Web-Based Interventions Targeting Alcohol Consumption, Binge Eating, and Gambling: Systematic Review. J Med Internet Res. 2021 Feb 09;23(2):e22694. doi: 10.2196/22694. https://www.jmir.org/2021/2/e22694/ v23i2e22694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Moghimi E, Davis C, Rotondi M. The Efficacy of eHealth Interventions for the Treatment of Adults Diagnosed With Full or Subthreshold Binge Eating Disorder: Systematic Review and Meta-analysis. J Med Internet Res. 2021 Jul 20;23(7):e17874. doi: 10.2196/17874. https://www.jmir.org/2021/7/e17874/ v23i7e17874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Anastasiadou D, Folkvord F, Lupiañez-Villanueva F. A systematic review of mHealth interventions for the support of eating disorders. Eur Eat Disord Rev. 2018 Sep;26(5):394–416. doi: 10.1002/erv.2609. [DOI] [PubMed] [Google Scholar]
- 280.Juarascio AS, Manasse SM, Goldstein SP, Forman EM, Butryn ML. Review of smartphone applications for the treatment of eating disorders. Eur Eat Disord Rev. 2015 Jan;23(1):1–11. doi: 10.1002/erv.2327. http://europepmc.org/abstract/MED/25303148 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Smith KE, Juarascio A. From Ecological Momentary Assessment (EMA) to Ecological Momentary Intervention (EMI): Past and Future Directions for Ambulatory Assessment and Interventions in Eating Disorders. Curr Psychiatry Rep. 2019 Jun 04;21(7):53. doi: 10.1007/s11920-019-1046-8.10.1007/s11920-019-1046-8 [DOI] [PubMed] [Google Scholar]
- 282.Wasil AR, Patel R, Cho JY, Shingleton RM, Weisz JR, DeRubeis RJ. Smartphone apps for eating disorders: A systematic review of evidence-based content and application of user-adjusted analyses. Int J Eat Disord. 2021 May;54(5):690–700. doi: 10.1002/eat.23478. [DOI] [PubMed] [Google Scholar]
- 283.Gutiérrez-Maldonado J, Ferrer-García M, Riva G. VR cue-exposure treatment for bulimia nervosa. Stud Health Technol Inform. 2013;191:21–25. [PubMed] [Google Scholar]
- 284.Koskina A, Campbell IC, Schmidt U. Exposure therapy in eating disorders revisited. Neurosci Biobehav Rev. 2013 Feb;37(2):193–208. doi: 10.1016/j.neubiorev.2012.11.010.S0149-7634(12)00200-X [DOI] [PubMed] [Google Scholar]
- 285.Butler RM, Heimberg RG. Exposure therapy for eating disorders: A systematic review. Clin Psychol Rev. 2020 Jun;78:101851. doi: 10.1016/j.cpr.2020.101851.S0272-7358(20)30039-8 [DOI] [PubMed] [Google Scholar]
- 286.Mikolasek M, Berg J, Witt CM, Barth J. Effectiveness of Mindfulness- and Relaxation-Based eHealth Interventions for Patients with Medical Conditions: a Systematic Review and Synthesis. Int J Behav Med. 2018 Feb;25(1):1–16. doi: 10.1007/s12529-017-9679-7.10.1007/s12529-017-9679-7 [DOI] [PubMed] [Google Scholar]
- 287.Mariano TY, Wan L, Edwards RR, Jamison RN. Online teletherapy for chronic pain: A systematic review. J Telemed Telecare. 2021 May;27(4):195–208. doi: 10.1177/1357633X19871746. [DOI] [PubMed] [Google Scholar]
- 288.Tang W, Zhang L, Ai Y, Li Z. Efficacy of Internet-delivered cognitive-behavioral therapy for the management of chronic pain in children and adolescents: A systematic review and meta-analysis. Medicine (Baltimore) 2018 Sep;97(36):e12061. doi: 10.1097/MD.0000000000012061. doi: 10.1097/MD.0000000000012061.00005792-201809070-00028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Vugts MAP, Joosen MCW, van der Geer JE, Zedlitz AMEE, Vrijhoef HJM. The effectiveness of various computer-based interventions for patients with chronic pain or functional somatic syndromes: A systematic review and meta-analysis. PLoS One. 2018;13(5):e0196467. doi: 10.1371/journal.pone.0196467. https://dx.plos.org/10.1371/journal.pone.0196467 .PONE-D-17-26362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Ahmadpour N, Randall H, Choksi H, Gao A, Vaughan C, Poronnik P. Virtual Reality interventions for acute and chronic pain management. Int J Biochem Cell Biol. 2019 Sep;114:105568. doi: 10.1016/j.biocel.2019.105568.S1357-2725(19)30145-1 [DOI] [PubMed] [Google Scholar]
- 291.Chi B, Chau B, Yeo E, Ta P. Virtual reality for spinal cord injury-associated neuropathic pain: Systematic review. Ann Phys Rehabil Med. 2019 Jan;62(1):49–57. doi: 10.1016/j.rehab.2018.09.006. https://linkinghub.elsevier.com/retrieve/pii/S1877-0657(18)31453-2 .S1877-0657(18)31453-2 [DOI] [PubMed] [Google Scholar]
- 292.Chirico A, Lucidi F, De Laurentiis M, Milanese C, Napoli A, Giordano A. Virtual Reality in Health System: Beyond Entertainment. A Mini-Review on the Efficacy of VR During Cancer Treatment. J Cell Physiol. 2016 Feb;231(2):275–287. doi: 10.1002/jcp.25117. [DOI] [PubMed] [Google Scholar]
- 293.Gates M, Hartling L, Shulhan-Kilroy J, MacGregor T, Guitard S, Wingert A, Featherstone R, Vandermeer B, Poonai N, Kircher J, Perry S, Graham TAD, Scott SD, Ali S. Digital Technology Distraction for Acute Pain in Children: A Meta-analysis. Pediatrics. 2020 Feb;145(2):e20191139. doi: 10.1542/peds.2019-1139.peds.2019-1139 [DOI] [PubMed] [Google Scholar]
- 294.Pourmand A, Davis S, Marchak A, Whiteside T, Sikka N. Virtual Reality as a Clinical Tool for Pain Management. Curr Pain Headache Rep. 2018 Jun 15;22(8):53. doi: 10.1007/s11916-018-0708-2.10.1007/s11916-018-0708-2 [DOI] [PubMed] [Google Scholar]
- 295.Scapin S, Echevarría-Guanilo ME, Boeira Fuculo Junior PR, Gonçalves N, Rocha PK, Coimbra R. Virtual Reality in the treatment of burn patients: A systematic review. Burns. 2018 Sep;44(6):1403–1416. doi: 10.1016/j.burns.2017.11.002.S0305-4179(17)30602-2 [DOI] [PubMed] [Google Scholar]
- 296.Smith V, Warty RR, Sursas JA, Payne O, Nair A, Krishnan S, da Silva Costa F, Wallace EM, Vollenhoven B. The Effectiveness of Virtual Reality in Managing Acute Pain and Anxiety for Medical Inpatients: Systematic Review. J Med Internet Res. 2020 Nov 02;22(11):e17980. doi: 10.2196/17980. https://www.jmir.org/2020/11/e17980/ v22i11e17980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Chuan A, Zhou JJ, Hou RM, Stevens CJ, Bogdanovych A. Virtual reality for acute and chronic pain management in adult patients: a narrative review. Anaesthesia. 2021 May;76(5):695–704. doi: 10.1111/anae.15202. [DOI] [PubMed] [Google Scholar]
- 298.Ding L, Hua H, Zhu H, Zhu S, Lu J, Zhao K, Xu Q. Effects of virtual reality on relieving postoperative pain in surgical patients: A systematic review and meta-analysis. Int J Surg. 2020 Oct;82:87–94. doi: 10.1016/j.ijsu.2020.08.033.S1743-9191(20)30636-1 [DOI] [PubMed] [Google Scholar]
- 299.Chow H, Hon J, Chua W, Chuan A. Effect of Virtual Reality Therapy in Reducing Pain and Anxiety for Cancer-Related Medical Procedures: A Systematic Narrative Review. J Pain Symptom Manage. 2021 Feb;61(2):384–394. doi: 10.1016/j.jpainsymman.2020.08.016.S0885-3924(20)30695-3 [DOI] [PubMed] [Google Scholar]
- 300.Austin PD, Siddall PJ. Virtual reality for the treatment of neuropathic pain in people with spinal cord injuries: A scoping review. J Spinal Cord Med. 2021 Jan;44(1):8–18. doi: 10.1080/10790268.2019.1575554. http://europepmc.org/abstract/MED/30707649 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Zasadzka E, Pieczyńska A, Trzmiel T, Hojan K. Virtual Reality as a Promising Tool Supporting Oncological Treatment in Breast Cancer. Int J Environ Res Public Health. 2021 Aug 19;18(16):8768. doi: 10.3390/ijerph18168768. https://www.mdpi.com/resolver?pii=ijerph18168768 .ijerph18168768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Bonet L, Izquierdo C, Escartí MJ, Sancho JV, Arce D, Blanquer I, Sanjuan J. Use of mobile technologies in patients with psychosis: A systematic review. Rev Psiquiatr Salud Ment. 2017;10(3):168–178. doi: 10.1016/j.rpsm.2017.01.003.S1888-9891(17)30023-X [DOI] [PubMed] [Google Scholar]
- 303.Kasckow J, Felmet K, Appelt C, Thompson R, Rotondi A, Haas G. Telepsychiatry in the assessment and treatment of schizophrenia. Clin Schizophr Relat Psychoses. 2014 Apr;8(1):21–27A. doi: 10.3371/CSRP.KAFE.021513. http://europepmc.org/abstract/MED/23428781 .9684Q297P151LW04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.van der Krieke L, Wunderink L, Emerencia AC, de Jonge P, Sytema S. E-mental health self-management for psychotic disorders: state of the art and future perspectives. Psychiatr Serv. 2014 Jan 01;65(1):33–49. doi: 10.1176/appi.ps.201300050.1755817 [DOI] [PubMed] [Google Scholar]
- 305.Gaebel W, Großimlinghaus I, Kerst A, Cohen Y, Hinsche-Böckenholt A, Johnson B, Mucic D, Petrea I, Rössler W, Thornicroft G, Zielasek J. European Psychiatric Association (EPA) guidance on the quality of eMental health interventions in the treatment of psychotic disorders. Eur Arch Psychiatry Clin Neurosci. 2016 Mar;266(2):125–137. doi: 10.1007/s00406-016-0677-6.10.1007/s00406-016-0677-6 [DOI] [PubMed] [Google Scholar]
- 306.Biagianti B, Quraishi SH, Schlosser DA. Potential Benefits of Incorporating Peer-to-Peer Interactions Into Digital Interventions for Psychotic Disorders: A Systematic Review. Psychiatr Serv. 2018 Apr 01;69(4):377–388. doi: 10.1176/appi.ps.201700283. http://europepmc.org/abstract/MED/29241435 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Chivilgina O, Wangmo T, Elger BS, Heinrich T, Jotterand F. mHealth for schizophrenia spectrum disorders management: A systematic review. Int J Soc Psychiatry. 2020 Nov;66(7):642–665. doi: 10.1177/0020764020933287. [DOI] [PubMed] [Google Scholar]
- 308.Chivilgina O, Elger BS, Jotterand F. Digital Technologies for Schizophrenia Management: A Descriptive Review. Sci Eng Ethics. 2021 Apr 09;27(2):25. doi: 10.1007/s11948-021-00302-z. http://europepmc.org/abstract/MED/33835287 .10.1007/s11948-021-00302-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Rus-Calafell M, Garety P, Sason E, Craig TJK, Valmaggia LR. Virtual reality in the assessment and treatment of psychosis: a systematic review of its utility, acceptability and effectiveness. Psychol Med. 2018 Feb;48(3):362–391. doi: 10.1017/S0033291717001945.S0033291717001945 [DOI] [PubMed] [Google Scholar]
- 310.Valmaggia LR, Day F, Rus-Calafell M. Using virtual reality to investigate psychological processes and mechanisms associated with the onset and maintenance of psychosis: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2016 Jul;51(7):921–936. doi: 10.1007/s00127-016-1245-0.10.1007/s00127-016-1245-0 [DOI] [PubMed] [Google Scholar]
- 311.Veling W, Moritz S, van der Gaag M. Brave new worlds--review and update on virtual reality assessment and treatment in psychosis. Schizophr Bull. 2014 Nov;40(6):1194–1197. doi: 10.1093/schbul/sbu125. http://europepmc.org/abstract/MED/25193975 .sbu125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Brun G, Verdoux H, Couhet G, Quiles C. [Computer-assisted therapy and video games in psychosocial rehabilitation for schizophrenia patients] Encephale. 2018 Sep;44(4):363–371. doi: 10.1016/j.encep.2017.12.009.S0013-7006(18)30025-3 [DOI] [PubMed] [Google Scholar]
- 313.Bisso E, Signorelli MS, Milazzo M, Maglia M, Polosa R, Aguglia E, Caponnetto P. Immersive Virtual Reality Applications in Schizophrenia Spectrum Therapy: A Systematic Review. Int J Environ Res Public Health. 2020 Aug 22;17(17):6111. doi: 10.3390/ijerph17176111. https://www.mdpi.com/resolver?pii=ijerph17176111 .ijerph17176111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Gainsford K, Fitzgibbon B, Fitzgerald PB, Hoy KE. Transforming treatments for schizophrenia: Virtual reality, brain stimulation and social cognition. Psychiatry Res. 2020 Jun;288:112974. doi: 10.1016/j.psychres.2020.112974.S0165-1781(19)32486-2 [DOI] [PubMed] [Google Scholar]
- 315.Kruk D, Mętel D, Gawęda Ł, Cechnicki A. Implementation of virtual reality (VR) in diagnostics and therapy of nonaffective psychoses. Psychiatr Pol. 2020 Oct 31;54(5):951–975. doi: 10.12740/PP/OnlineFirst/113437. doi: 10.12740/PP/OnlineFirst/113437.113437 [DOI] [PubMed] [Google Scholar]
- 316.Chan JYC, Hirai HW, Tsoi KKF. Can computer-assisted cognitive remediation improve employment and productivity outcomes of patients with severe mental illness? A meta-analysis of prospective controlled trials. J Psychiatr Res. 2015 Sep;68:293–300. doi: 10.1016/j.jpsychires.2015.05.010.S0022-3956(15)00151-X [DOI] [PubMed] [Google Scholar]
- 317.Fisher M, Herman A, Stephens DB, Vinogradov S. Neuroscience-informed computer-assisted cognitive training in schizophrenia. Ann N Y Acad Sci. 2016 Feb;1366(1):90–114. doi: 10.1111/nyas.13042. [DOI] [PubMed] [Google Scholar]
- 318.Grynszpan O, Perbal S, Pelissolo A, Fossati P, Jouvent R, Dubal S, Perez-Diaz F. Efficacy and specificity of computer-assisted cognitive remediation in schizophrenia: a meta-analytical study. Psychol Med. 2011 Jan;41(1):163–173. doi: 10.1017/S0033291710000607.S0033291710000607 [DOI] [PubMed] [Google Scholar]
- 319.Prikken M, Konings MJ, Lei WU, Begemann MJH, Sommer IEC. The efficacy of computerized cognitive drill and practice training for patients with a schizophrenia-spectrum disorder: A meta-analysis. Schizophr Res. 2019 Feb;204:368–374. doi: 10.1016/j.schres.2018.07.034.S0920-9964(18)30479-1 [DOI] [PubMed] [Google Scholar]
- 320.Vass E, Fekete Z, Simon V, Simon L. Interventions for the treatment of theory of mind deficits in schizophrenia: Systematic literature review. Psychiatry Res. 2018 Sep;267:37–47. doi: 10.1016/j.psychres.2018.05.001.S0165-1781(17)31658-X [DOI] [PubMed] [Google Scholar]
- 321.Yeh P, Yu L, Guo N, Lin W, Wu C. Observation and Imitation of Social Emotions Are Essential for Improving Cognitive and Affective Theory of Mind in Schizophrenia: A Meta-analysis. J Nerv Ment Dis. 2019 Jun;207(6):474–481. doi: 10.1097/NMD.0000000000000996.00005053-201906000-00010 [DOI] [PubMed] [Google Scholar]
- 322.Cheng SK, Dizon J. Computerised cognitive behavioural therapy for insomnia: a systematic review and meta-analysis. Psychother Psychosom. 2012;81(4):206–216. doi: 10.1159/000335379.000335379 [DOI] [PubMed] [Google Scholar]
- 323.Drerup ML, Ahmed-Jauregui S. Online Delivery of Cognitive Behavioral Therapy-Insomnia: Considerations and Controversies. Sleep Med Clin. 2019 Jun;14(2):283–290. doi: 10.1016/j.jsmc.2019.02.001.S1556-407X(19)30014-1 [DOI] [PubMed] [Google Scholar]
- 324.Kay-Stacey M, Attarian H. Advances in the management of chronic insomnia. BMJ. 2016 Jul 06;354:i2123. doi: 10.1136/bmj.i2123. [DOI] [PubMed] [Google Scholar]
- 325.Seyffert M, Lagisetty P, Landgraf J, Chopra V, Pfeiffer PN, Conte ML, Rogers MAM. Internet-Delivered Cognitive Behavioral Therapy to Treat Insomnia: A Systematic Review and Meta-Analysis. PLoS One. 2016;11(2):e0149139. doi: 10.1371/journal.pone.0149139. https://dx.plos.org/10.1371/journal.pone.0149139 .PONE-D-15-47789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Ye Y, Chen N, Chen J, Liu J, Lin L, Liu Y, Lang Y, Li X, Yang X, Jiang X. Internet-based cognitive-behavioural therapy for insomnia (ICBT-i): a meta-analysis of randomised controlled trials. BMJ Open. 2016 Nov 30;6(11):e010707. doi: 10.1136/bmjopen-2015-010707. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=27903557 .bmjopen-2015-010707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Hsieh C, Rezayat T, Zeidler MR. Telemedicine and the Management of Insomnia. Sleep Med Clin. 2020 Sep;15(3):383–390. doi: 10.1016/j.jsmc.2020.05.004.S1556-407X(20)30044-8 [DOI] [PubMed] [Google Scholar]
- 328.Frase L, Duss SB, Gieselmann A, Penzel T, Wetter TC, Pollmächer T. [Internet-based cognitive behavioral therapy of insomnia and nightmare disorder] Nervenarzt. 2020 Jul;91(7):617–623. doi: 10.1007/s00115-019-00803-0.10.1007/s00115-019-00803-0 [DOI] [PubMed] [Google Scholar]
- 329.Benavides-Vaello S, Strode A, Sheeran BC. Using technology in the delivery of mental health and substance abuse treatment in rural communities: a review. J Behav Health Serv Res. 2013 Jan;40(1):111–120. doi: 10.1007/s11414-012-9299-6. [DOI] [PubMed] [Google Scholar]
- 330.Blalock DV, Calhoun PS, Crowley MJ, Dedert EA. Telehealth Treatment for Alcohol Misuse: Reviewing Telehealth Approaches to Increase Engagement and Reduce Risk of Alcohol-Related Hypertension. Curr Hypertens Rep. 2019 Jun 17;21(8):59. doi: 10.1007/s11906-019-0966-3.10.1007/s11906-019-0966-3 [DOI] [PubMed] [Google Scholar]
- 331.Young LB. Telemedicine interventions for substance-use disorder: a literature review. J Telemed Telecare. 2012 Jan;18(1):47–53. doi: 10.1258/jtt.2011.110608.jtt.2011.110608 [DOI] [PubMed] [Google Scholar]
- 332.Keoleian V, Polcin D, Galloway GP. Text messaging for addiction: a review. J Psychoactive Drugs. 2015;47(2):158–176. doi: 10.1080/02791072.2015.1009200. http://europepmc.org/abstract/MED/25950596 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Quanbeck A, Chih M, Isham A, Gustafson D. Mobile Delivery of Treatment for Alcohol Use Disorders: A Review of the Literature. Alcohol Res. 2014;36(1):111–122. http://europepmc.org/abstract/MED/26259005 . [PMC free article] [PubMed] [Google Scholar]
- 334.Tofighi B, Abrantes A, Stein MD. The Role of Technology-Based Interventions for Substance Use Disorders in Primary Care: A Review of the Literature. Med Clin North Am. 2018 Jul;102(4):715–731. doi: 10.1016/j.mcna.2018.02.011. http://europepmc.org/abstract/MED/29933825 .S0025-7125(18)30015-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Marsch LA. Leveraging technology to enhance addiction treatment and recovery. J Addict Dis. 2012;31(3):313–318. doi: 10.1080/10550887.2012.694606. http://europepmc.org/abstract/MED/22873192 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Marsch LA, Dallery J. Advances in the psychosocial treatment of addiction: the role of technology in the delivery of evidence-based psychosocial treatment. Psychiatr Clin North Am. 2012 Jun;35(2):481–493. doi: 10.1016/j.psc.2012.03.009. http://europepmc.org/abstract/MED/22640767 .S0193-953X(12)00026-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Suffoletto B, Scaglione S. Using Digital Interventions to Support Individuals with Alcohol Use Disorder and Advanced Liver Disease: A Bridge Over Troubled Waters. Alcohol Clin Exp Res. 2018 Jul;42(7):1160–1165. doi: 10.1111/acer.13771. http://europepmc.org/abstract/MED/29750368 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Sugarman DE, Campbell ANC, Iles BR, Greenfield SF. Technology-Based Interventions for Substance Use and Comorbid Disorders: An Examination of the Emerging Literature. Harv Rev Psychiatry. 2017;25(3):123–134. doi: 10.1097/HRP.0000000000000148. http://europepmc.org/abstract/MED/28475504 .00023727-201705000-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Kazemi DM, Borsari B, Levine MJ, Li S, Lamberson KA, Matta LA. A Systematic Review of the mHealth Interventions to Prevent Alcohol and Substance Abuse. J Health Commun. 2017 May;22(5):413–432. doi: 10.1080/10810730.2017.1303556. http://europepmc.org/abstract/MED/28394729 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Oesterle TS, Kolla B, Risma CJ, Breitinger SA, Rakocevic DB, Loukianova LL, Hall-Flavin DK, Gentry MT, Rummans TA, Chauhan M, Gold MS. Substance Use Disorders and Telehealth in the COVID-19 Pandemic Era: A New Outlook. Mayo Clin Proc. 2020 Dec;95(12):2709–2718. doi: 10.1016/j.mayocp.2020.10.011. http://europepmc.org/abstract/MED/33276843 .S0025-6196(20)31195-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Silang K, Sanguino H, Sohal PR, Rioux C, Kim HS, Tomfohr-Madsen LM. eHealth Interventions to Treat Substance Use in Pregnancy: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021 Sep 22;18(19):9952. doi: 10.3390/ijerph18199952. https://www.mdpi.com/resolver?pii=ijerph18199952 .ijerph18199952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Kim S, Tesmer O. Employing telehealth strategies for opioid addiction during COVID-19: implications for social work health care. Soc Work Health Care. 2021 Aug 09;60(6-7):499–508. doi: 10.1080/00981389.2021.1953207. [DOI] [PubMed] [Google Scholar]
- 343.Li R, Zhao M. Maintaining treatment and prevention programs for opioid use disorders during the coronavirus disease 2019 pandemic. Curr Opin Psychiatry. 2021 Jul 01;34(4):369–375. doi: 10.1097/YCO.0000000000000708. http://europepmc.org/abstract/MED/33859127 .00001504-900000000-99044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Kazemi DM, Troutman-Jordan M, Whitfield JE, Pappa EV. Effectiveness of eHealth Technology-Based Interventions in Reducing Substance Misuse Among Older Adults: A Systematic Review. J Gerontol Nurs. 2021 Oct;47(10):23–29. doi: 10.3928/00989134-20210908-04. [DOI] [PubMed] [Google Scholar]
- 345.Cole TO, Robinson D, Kelley-Freeman A, Gandhi D, Greenblatt AD, Weintraub E, Belcher AM. Patient Satisfaction With Medications for Opioid Use Disorder Treatment via Telemedicine: Brief Literature Review and Development of a New Assessment. Front Public Health. 2020;8:557275. doi: 10.3389/fpubh.2020.557275. doi: 10.3389/fpubh.2020.557275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Das S, Tonelli M, Ziedonis D. Update on Smoking Cessation: E-Cigarettes, Emerging Tobacco Products Trends, and New Technology-Based Interventions. Curr Psychiatry Rep. 2016 May;18(5):51. doi: 10.1007/s11920-016-0681-6.10.1007/s11920-016-0681-6 [DOI] [PubMed] [Google Scholar]
- 347.Muench F. The Promises and Pitfalls of Digital Technology in Its Application to Alcohol Treatment. Alcohol Res. 2014;36(1):131–142. http://europepmc.org/abstract/MED/26259008 . [PMC free article] [PubMed] [Google Scholar]
- 348.Holmes NA, van Agteren JE, Dorstyn DS. A systematic review of technology-assisted interventions for co-morbid depression and substance use. J Telemed Telecare. 2019 Apr;25(3):131–141. doi: 10.1177/1357633X17748991. [DOI] [PubMed] [Google Scholar]
- 349.Boumparis N, Loheide-Niesmann L, Blankers M, Ebert DD, Korf D, Schaub MP, Spijkerman R, Tait RJ, Riper H. Short- and long-term effects of digital prevention and treatment interventions for cannabis use reduction: A systematic review and meta-analysis. Drug Alcohol Depend. 2019 Jul 01;200:82–94. doi: 10.1016/j.drugalcdep.2019.03.016. https://linkinghub.elsevier.com/retrieve/pii/S0376-8716(19)30149-8 .S0376-8716(19)30149-8 [DOI] [PubMed] [Google Scholar]
- 350.Hser Y, Mooney LJ. Integrating Telemedicine for Medication Treatment for Opioid Use Disorder in Rural Primary Care: Beyond the COVID Pandemic. J Rural Health. 2021 Jan;37(1):246–248. doi: 10.1111/jrh.12489. http://europepmc.org/abstract/MED/32579751 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Nair NK, Newton NC, Shakeshaft A, Wallace P, Teesson M. A Systematic Review of Digital and Computer-Based Alcohol Intervention Programs in Primary Care. Curr Drug Abuse Rev. 2015;8(2):111–118. doi: 10.2174/1874473708666150916113538.CDAR-EPUB-70445 [DOI] [PubMed] [Google Scholar]
- 352.Ondersma SJ, Ellis JD, Resko SM, Grekin E. Technology-Delivered Interventions for Substance Use Among Adolescents. Pediatr Clin North Am. 2019 Dec;66(6):1203–1215. doi: 10.1016/j.pcl.2019.08.009.S0031-3955(19)30117-8 [DOI] [PubMed] [Google Scholar]
- 353.Zhang MW, Ying JB, Song G, Fung DSS, Smith HE. Recent Advances in Attention Bias Modification for Substance Addictions. Int J Environ Res Public Health. 2018 Apr 04;15(4):676. doi: 10.3390/ijerph15040676. https://www.mdpi.com/resolver?pii=ijerph15040676 .ijerph15040676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Hutton A, Prichard I, Whitehead D, Thomas S, Rubin M, Sloand E, Powell TW, Frisch K, Newman P, Goodwin Veenema T. mHealth Interventions to Reduce Alcohol Use in Young People: A Systematic Review of the Literature. Compr Child Adolesc Nurs. 2020 Sep;43(3):171–202. doi: 10.1080/24694193.2019.1616008. http://europepmc.org/abstract/MED/31192698 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Colbert S, Thornton L, Richmond R. Smartphone apps for managing alcohol consumption: a literature review. Addict Sci Clin Pract. 2020 May 07;15(1):17. doi: 10.1186/s13722-020-00190-x. https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-020-00190-x .10.1186/s13722-020-00190-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Ghassemlou S, Marini C, Chemi C, Ranjit YS, Tofighi B. Harmful smartphone applications promoting alcohol and illicit substance use: a review and content analysis in the United States. Transl Behav Med. 2020 Oct 12;10(5):1233–1242. doi: 10.1093/tbm/ibz135. http://europepmc.org/abstract/MED/33044528 .5921061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Carreiro S, Newcomb M, Leach R, Ostrowski S, Boudreaux ED, Amante D. Current reporting of usability and impact of mHealth interventions for substance use disorder: A systematic review. Drug Alcohol Depend. 2020 Oct 01;215:108201. doi: 10.1016/j.drugalcdep.2020.108201. http://europepmc.org/abstract/MED/32777691 .S0376-8716(20)30366-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Staiger PK, O'Donnell R, Liknaitzky P, Bush R, Milward J. Mobile Apps to Reduce Tobacco, Alcohol, and Illicit Drug Use: Systematic Review of the First Decade. J Med Internet Res. 2020 Nov 24;22(11):e17156. doi: 10.2196/17156. https://www.jmir.org/2020/11/e17156/ v22i11e17156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Kazemi DM, Li S, Levine MJ, Auten B, Granson M. Systematic Review of Smartphone Apps as a mHealth Intervention to Address Substance Abuse in Adolescents and Adults. J Addict Nurs. 2021;32(3):180–187. doi: 10.1097/JAN.0000000000000416.00060867-202107000-00003 [DOI] [PubMed] [Google Scholar]
- 360.Evangelatos G, Andrew Valasquez G, Hilty DM. Lessons Learned on Telehealth in Inpatient Psychiatric Facilities: Quality, Continuity, and Models of Care. J Technol Behav Sci. 2018 May 23;3(4):221–225. doi: 10.1007/s41347-018-0056-4. [DOI] [Google Scholar]
- 361.Lawes-Wickwar S, McBain H, Mulligan K. Application and Effectiveness of Telehealth to Support Severe Mental Illness Management: Systematic Review. JMIR Ment Health. 2018 Nov 21;5(4):e62. doi: 10.2196/mental.8816. https://mental.jmir.org/2018/4/e62/ v5i4e62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Mogoașe C, Cobeanu O, David O, Giosan C, Szentagotai A. Internet-Based Psychotherapy for Adult Depression: What About the Mechanisms of Change? J Clin Psychol. 2017 Jan;73(1):5–64. doi: 10.1002/jclp.22326. [DOI] [PubMed] [Google Scholar]
- 363.Bauer MS, Krawczyk L, Miller CJ, Abel E, Osser DN, Franz A, Brandt C, Rooney M, Fleming J, Godleski L. Team-Based Telecare for Bipolar Disorder. Telemed J E Health. 2016 Oct;22(10):855–864. doi: 10.1089/tmj.2015.0255. [DOI] [PubMed] [Google Scholar]
- 364.Barceló-Soler A, Baños RM, López-Del-Hoyo Y, Mayoral F, Gili M, García-Palacios A, García-Campayo J, Botella C. Interventions of computerized psychotherapies for depression in Primary Care in Spain. Actas Esp Psiquiatr. 2019 Nov;47(6):236–246. https://www.actaspsiquiatria.es/repositorio//21/122/ENG/21-122-ENG-236-46-459497.pdf . [PubMed] [Google Scholar]
- 365.Capon H, Hall W, Fry C, Carter A. Realising the technological promise of smartphones in addiction research and treatment: An ethical review. Int J Drug Policy. 2016 Oct;36:47–57. doi: 10.1016/j.drugpo.2016.05.013.S0955-3959(16)30167-0 [DOI] [PubMed] [Google Scholar]
- 366.Fichter MM, Quadflieg N, Nisslmüller K, Lindner S, Voderholzer U, Wünsch-Leiteritz W, Osen B, Huber T, Zahn S, Meermann R, Irrgang V, Bleichner F. [Internet-based approaches in the therapy of eating disorders] Nervenarzt. 2011 Sep;82(9):1107–1117. doi: 10.1007/s00115-010-3228-9. [DOI] [PubMed] [Google Scholar]
- 367.Gustafson DH, Boyle MG, Shaw BR, Isham A, McTavish F, Richards S, Schubert C, Levy M, Johnson K. An e-health solution for people with alcohol problems. Alcohol Res Health. 2011;33(4):327–337. http://europepmc.org/abstract/MED/23293549 . [PMC free article] [PubMed] [Google Scholar]
- 368.Huguet A, Rao S, McGrath PJ, Wozney L, Wheaton M, Conrod J, Rozario S. A Systematic Review of Cognitive Behavioral Therapy and Behavioral Activation Apps for Depression. PLoS One. 2016;11(5):e0154248. doi: 10.1371/journal.pone.0154248. https://dx.plos.org/10.1371/journal.pone.0154248 .PONE-D-15-42879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Stetz MC, Folen RA, Yamanuha BK. Technology complementing military behavioral health efforts at tripler army medical center. J Clin Psychol Med Settings. 2011 Jun;18(2):188–195. doi: 10.1007/s10880-011-9246-3. [DOI] [PubMed] [Google Scholar]
- 370.Riva G, Wiederhold BK, Mantovani F. Neuroscience of Virtual Reality: From Virtual Exposure to Embodied Medicine. Cyberpsychol Behav Soc Netw. 2019 Jan;22(1):82–96. doi: 10.1089/cyber.2017.29099.gri. http://europepmc.org/abstract/MED/30183347 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Wiederhold BK, Riva G, Gutiérrez-Maldonado J. Virtual Reality in the Assessment and Treatment of Weight-Related Disorders. Cyberpsychol Behav Soc Netw. 2016 Feb;19(2):67–73. doi: 10.1089/cyber.2016.0012. [DOI] [PubMed] [Google Scholar]
- 372.Gwynette MF, Sidhu SS, Ceranoglu TA. Electronic Screen Media Use in Youth With Autism Spectrum Disorder. Child Adolesc Psychiatr Clin N Am. 2018 Apr;27(2):203–219. doi: 10.1016/j.chc.2017.11.013.S1056-4993(17)30137-2 [DOI] [PubMed] [Google Scholar]
- 373.Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, Cannon M, Correll CU, Byrne L, Carr S, Chen EYH, Gorwood P, Johnson S, Kärkkäinen H, Krystal JH, Lee J, Lieberman J, López-Jaramillo C, Männikkö M, Phillips MR, Uchida H, Vieta E, Vita A, Arango C. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020 Sep;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. http://europepmc.org/abstract/MED/32682460 .S2215-0366(20)30307-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Smith K, Ostinelli E, Macdonald O, Cipriani A. COVID-19 and Telepsychiatry: Development of Evidence-Based Guidance for Clinicians. JMIR Ment Health. 2020 Aug 28;7(8):e21108. doi: 10.2196/21108. https://mental.jmir.org/2020/8/e21108/ v7i8e21108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Samuels EA, Clark SA, Wunsch C, Jordison Keeler LA, Reddy N, Vanjani R, Wightman RS. Innovation During COVID-19: Improving Addiction Treatment Access. J Addict Med. 2020;14(4):e8–e9. doi: 10.1097/ADM.0000000000000685. http://europepmc.org/abstract/MED/32404652 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 Pandemic and Rapid Implementation of Adolescent and Young Adult Telemedicine: Challenges and Opportunities for Innovation. J Adolesc Health. 2020 Aug;67(2):164–171. doi: 10.1016/j.jadohealth.2020.05.006. http://europepmc.org/abstract/MED/32410810 .S1054-139X(20)30225-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Chen JA, Chung W, Young SK, Tuttle MC, Collins MB, Darghouth SL, Longley R, Levy R, Razafsha M, Kerner JC, Wozniak J, Huffman JC. COVID-19 and telepsychiatry: Early outpatient experiences and implications for the future. Gen Hosp Psychiatry. 2020;66:89–95. doi: 10.1016/j.genhosppsych.2020.07.002. http://europepmc.org/abstract/MED/32750604 .S0163-8343(20)30103-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Hoffman L, Wisniewski H, Hays R, Henson P, Vaidyam A, Hendel V, Keshavan M, Torous J. Digital Opportunities for Outcomes in Recovery Services (DOORS): A Pragmatic Hands-On Group Approach Toward Increasing Digital Health and Smartphone Competencies, Autonomy, Relatedness, and Alliance for Those With Serious Mental Illness. J Psychiatr Pract. 2020 Mar;26(2):80–88. doi: 10.1097/PRA.0000000000000450. http://europepmc.org/abstract/MED/32134881 .00131746-202003000-00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Hoffman, Liza J. Vaidyam, Aditya. Wisniewski, Hannah. Henson, Phil. Hays, Ryan. Hendel, Victoria. Keshavan, Matcheri. Torous, John B. Digital Opportunities for Outcomes in Recovery Services. Beth Israel Deaconess Medical Center. [2020-04-23]. https://uploads-ssl.webflow.com/5d321d55bdb594133bc03c07/5db8f45e6f2f7660f86437c1_190924%20DOORS%20Manual-compressed.pdf . [DOI] [PMC free article] [PubMed]
- 380.Practice Standard: Telemedicine. College of Physicians and Surgeons of British Columbia. [2020-04-23]. https://www.cpsbc.ca/files/pdf/PSG-Virtual-Care.pdf .
- 381.Virtual Care Toolkit. Doctors Technology Office. [2020-04-19]. https://www.doctorsofbc.ca/sites/default/files/dto_virtual_care_toolkit.pdf .
- 382.Ganapathy K. Telemedicine and Neurological Practice in the COVID-19 Era. Neurol India. 2020;68(3):555–559. doi: 10.4103/0028-3886.288994. http://www.neurologyindia.com/article.asp?issn=0028-3886;year=2020;volume=68;issue=3;spage=555;epage=559;aulast=Ganapathy .ni_2020_68_3_555_288994 [DOI] [PubMed] [Google Scholar]
- 383.Virtual care in Canada: Discussion paper. Canadian Medical Association. [2020-04-20]. https://www.cma.ca/virtual-care-canada-discussion-paper .
- 384.Overdose Deaths Accelerating During COVID-19. Centers for Disease Control and Prevention. 2020. [2020-04-21]. https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html .
- 385.Shams F, Wong JSH, Nikoo M, Outadi A, Moazen-Zadeh E, Kamel MM, Song MJ, Jang KL, Krausz RM. Understanding eHealth Cognitive Behavioral Therapy Targeting Substance Use: Realist Review. J Med Internet Res. 2021 Jan 21;23(1):e20557. doi: 10.2196/20557. https://www.jmir.org/2021/1/e20557/ v23i1e20557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Lawrie K, Charow R, Giuliani M, Papadakos J. Homelessness, Cancer and Health Literacy: A Scoping Review. J Health Care Poor Underserved. 2020;31(1):81–104. doi: 10.1353/hpu.2020.0010.S154868692010010X [DOI] [PubMed] [Google Scholar]
- 387.Parker S, Prince A, Thomas L, Song H, Milosevic D, Harris MF, IMPACT Study Group Electronic, mobile and telehealth tools for vulnerable patients with chronic disease: a systematic review and realist synthesis. BMJ Open. 2018 Aug 29;8(8):e019192. doi: 10.1136/bmjopen-2017-019192. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=30158214 .bmjopen-2017-019192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Stone B, Dowling S, Cameron A. Cognitive impairment and homelessness: A scoping review. Health Soc Care Community. 2019 Jul;27(4):e125–e142. doi: 10.1111/hsc.12682. http://europepmc.org/abstract/MED/30421478 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Lopez A, Schwenk S, Schneck CD, Griffin RJ, Mishkind MC. Technology-Based Mental Health Treatment and the Impact on the Therapeutic Alliance. Curr Psychiatry Rep. 2019 Jul 08;21(8):76. doi: 10.1007/s11920-019-1055-7.10.1007/s11920-019-1055-7 [DOI] [PubMed] [Google Scholar]
- 390.Henry BW, Block DE, Ciesla JR, McGowan BA, Vozenilek JA. Clinician behaviors in telehealth care delivery: a systematic review. Adv Health Sci Educ Theory Pract. 2017 Oct;22(4):869–888. doi: 10.1007/s10459-016-9717-2.10.1007/s10459-016-9717-2 [DOI] [PubMed] [Google Scholar]
- 391.Chan S, Li L, Torous J, Gratzer D, Yellowlees PM. Review of Use of Asynchronous Technologies Incorporated in Mental Health Care. Curr Psychiatry Rep. 2018 Aug 28;20(10):85. doi: 10.1007/s11920-018-0954-3.10.1007/s11920-018-0954-3 [DOI] [PubMed] [Google Scholar]
- 392.Hilty DM, Chan S, Hwang T, Wong A, Bauer AM. Advances in Mobile Mental Health: Opportunities and Implications for the Spectrum of E-Mental Health Services. Focus (Am Psychiatr Publ) 2018 Jul;16(3):314–327. doi: 10.1176/appi.focus.16301. http://europepmc.org/abstract/MED/32015712 .FOC_16301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Hilty DM, Randhawa K, Maheu MM, McKean AJS, Pantera R, Mishkind MC, Rizzo A. A Review of Telepresence, Virtual Reality, and Augmented Reality Applied to Clinical Care. J Technol Behav Sci. 2020 Feb 20;5(2):178–205. doi: 10.1007/s41347-020-00126-x. [DOI] [Google Scholar]
- 394.Vogt EL, Mahmoud H, Elhaj O. Telepsychiatry: Implications for Psychiatrist Burnout and Well-Being. Psychiatr Serv. 2019 May 01;70(5):422–424. doi: 10.1176/appi.ps.201800465. [DOI] [PubMed] [Google Scholar]
- 395.Gardner KL, Thrivikraman KV, Lightman SL, Plotsky PM, Lowry CA. Early life experience alters behavior during social defeat: focus on serotonergic systems. Neuroscience. 2005;136(1):181–191. doi: 10.1016/j.neuroscience.2005.07.042.S0306-4522(05)00813-4 [DOI] [PubMed] [Google Scholar]
- 396.Langarizadeh M, Tabatabaei MS, Tavakol K, Naghipour M, Rostami A, Moghbeli F. Telemental Health Care, an Effective Alternative to Conventional Mental Care: a Systematic Review. Acta Inform Med. 2017 Dec;25(4):240–246. doi: 10.5455/aim.2017.25.240-246. http://europepmc.org/abstract/MED/29284913 .AIM-25-240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Hilty DM, Seritan AL, Rabinowitz T. Inpatient Geriatric Psychiatry. Cham: Springer; 2019. Telemedicine and IT: Use of Digital Technology on Inpatient Units; pp. 373–392. [Google Scholar]
- 398.Biehl M, Sese D. Post-intensive care syndrome and COVID-19 - Implications post pandemic. Cleve Clin J Med. 2020 Aug 05; doi: 10.3949/ccjm.87a.ccc055. https://www.ccjm.org/cgi/pmidlookup?view=long&pmid=32759175 .ccjm.87a.ccc055 [DOI] [PubMed] [Google Scholar]
- 399.Jaffri A, Jaffri UA. Post-Intensive care syndrome and COVID-19: crisis after a crisis? Heart Lung. 2020;49(6):883–884. doi: 10.1016/j.hrtlng.2020.06.006. http://europepmc.org/abstract/MED/32690219 .S0147-9563(20)30266-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Haimi M, Brammli-Greenberg S, Waisman Y, Baron-Epel O. Physicians' experiences, attitudes and challenges in a Pediatric Telemedicine Service. Pediatr Res. 2018 Nov;84(5):650–656. doi: 10.1038/s41390-018-0117-6.10.1038/s41390-018-0117-6 [DOI] [PubMed] [Google Scholar]
- 401.El-Hage W, Hingray C, Lemogne C, Yrondi A, Brunault P, Bienvenu T, Etain B, Paquet C, Gohier B, Bennabi D, Birmes P, Sauvaget A, Fakra E, Prieto N, Bulteau S, Vidailhet P, Camus V, Leboyer M, Krebs M, Aouizerate B. [Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: What are the mental health risks?] Encephale. 2020 Jun;46(3S):S73–S80. doi: 10.1016/j.encep.2020.04.008. http://europepmc.org/abstract/MED/32370984 .S0013-7006(20)30076-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, He L, Sheng C, Cai Y, Li X, Wang J, Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020 Apr;7(4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X. http://europepmc.org/abstract/MED/32085839 .S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020 Jun;288:112936. doi: 10.1016/j.psychres.2020.112936. http://europepmc.org/abstract/MED/32276196 .S0165-1781(20)30585-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Pignatiello A, Stasiulis E, Solimine C, Ayad O, Boydell KM. Lessons Learned in a Physician Referral to Pediatric Telemental Health Services Program. J Can Acad Child Adolesc Psychiatry. 2019 Nov;28(3):99–104. http://europepmc.org/abstract/MED/31798648 . [PMC free article] [PubMed] [Google Scholar]
- 405.Drissi N, Ouhbi S, Ghogho M, Janati IM. Connected Mental Health Solutions to Assist Healthcare Workers with their Mental Health during COVID-19: A Literature Review. JMIR Preprints. doi: 10.2196/preprints.20917. Preprint posted online 2020. [DOI] [Google Scholar]
- 406.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 407.Odibo IN, Wendel PJ, Magann EF. Telemedicine in obstetrics. Clin Obstet Gynecol. 2013 Sep;56(3):422–433. doi: 10.1097/GRF.0b013e318290fef0.00003081-201309000-00003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary.
Extracted data for digital health interventions per mental health condition.


