Abstract
Introduction Tourette syndrome (TS) is a complex neurodevelopmental disorder characterized by chronic motor and vocal tics. While consistently effective treatment is lacking, evidence indicates that the modulation of endocannabinoid system is potentially beneficial. Lu AG06466 (previously ABX-1431) is a highly selective inhibitor of monoacylglycerol lipase, the primary enzyme responsible for the degradation of the endocannabinoid ligand 2-arachidonoylglycerol. This exploratory study aimed to determine the effect of Lu AG06466 versus placebo on tics and other symptoms in patients with TS.
Methods In this phase 1b cross-over study, 20 adult patients with TS on standard-of-care medications were randomized to a single fasted dose of Lu AG06466 (40 mg) or placebo in period 1, followed by the other treatment in period 2. The effects on tics, premonitory urges, and psychiatric comorbidities were evaluated using a variety of scaled approaches at different time points before and after treatment.
Results All scales showed an overall trend of tic reduction, with two out of three tic scales (including the Total Tic Score of the Yale Global Tic Severity Score) showing a significant effect of a single dose of Lu AG06466 versus placebo at various timepoints. Treatment with Lu AG06466 resulted in a significant reduction in premonitory urges versus placebo. Single doses of Lu AG06466 were generally well-tolerated, and the most common adverse events were headache, somnolence, and fatigue.
Conclusion In this exploratory trial, a single dose of Lu AG06466 showed statistically significant positive effects on key measures of TS symptoms.
Key words: Tourette syndrome, endocannabinoid, monoacylglycerol lipase, Lu AG06466
Introduction
Tourette syndrome (TS) is a neurodevelopmental disorder characterized by rapid, recurrent, involuntary movements and vocalizations, manifesting in childhood and often persisting into adulthood 1 . Psychiatric comorbidities such as attention-deficit/hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), anxiety, and depression are common 2 3 . Current treatments are moderately effective; both comprehensive behavioral intervention for tics (CBIT) and pharmacotherapy with atypical antipsychotics (e. g., aripiprazole and risperidone) result in an average tic reduction of 30–50% 4 5 . However, CBIT is hard to access and the atypical antipsychotics are associated with side effects such as sedation and weight gain 4 . Therefore, there is a need for a consistently effective medication that is well-tolerated and, ideally, also helps manage some of the common co-morbidities of TS.
The neurobiological basis of TS remains unclear. Basal ganglia involvement is assumed due to its well-known role in facilitating voluntary and inhibiting involuntary movements, including the control of routine behaviors and habits 6 . A role for the endocannabinoid system (ECS) in TS has, to date, been predominantly supported by clinical evidence indicating a beneficial effect of cannabis-based medicines. Several recent case series 7 8 9 and clinical studies 10 11 have reported that the use of cannabinoids such as tetrahydrocannabinol (THC) improve both tics and psychiatric comorbidities in adults with TS. THC and other exocannabinoids primarily exert their beneficial effects in TS possibly by acting as agonists at the cannabinoid receptor 1 (CB1) receptor which is highly expressed in the basal ganglia 12 . The principal endogenous ligands of the ECS are the lipid transmitters N-arachidonoylethanolamine (also known as anandamide) and 2-arachidonoylglycerol (2-AG), which act on presynaptic CB1 receptors to attenuate neurotransmission, serving an essential feedback function 13 . So, an alternative approach to stimulating central CB1 receptors is to inhibit the degradation of 2-AG into arachidonic acid and glycerol by inhibiting its main catabolizing enzyme monoacylglycerol lipase (MAGL) 14 . Under physiological conditions, 2-AG is released ‘on demand’ and acts as a retrograde messenger to suppress neurotransmitter release via CB1 receptor activation – in effect acting as a system ‘brake’. Thus, in contrast to exocannabinoids, which produce sustained activation of CB1 across all neuronal circuits, MAGL inhibition results in sustained 2-AG signaling through CB1 receptors only in the active synapses.
Lu AG06466 (previously known as ABX-1431) is a highly selective inhibitor of MAGL and is currently under investigation for the treatment of various psychiatric and neurological diseases where modulation of the ECS has been suggested to be of benefit. Its primary active metabolite, Lu AG06988 has a comparable in vitro and in vivo pharmacodynamic profile to Lu AG06466. Lu AG06988 is also a potent and selective MAGL inhibitor and thus may contribute to the overall MAGL inhibitory effect. The primary objective of this exploratory study was to determine the effect of a single dose of Lu AG06466 on tics and comorbid psychiatric symptoms in adult patients with TS. Secondary objectives were to evaluate Lu AG06466 pharmacokinetics (under fasting [Part A] and fed [Part B] conditions), safety, and tolerability in this population.
Methods
Study conduct
This was a phase 1b, randomized, double-blind, placebo-controlled, single-dose, crossover study to evaluate the effects of Lu AG06466 on tics and psychiatric comorbidities in TS. The study was conducted in two parts; part A was a cross-over study conducted under fasting conditions. Part B was a pharmacokinetic extension, added with a protocol amendment, under fed conditions (following a high-fat breakfast) in those patients who tolerated treatment in part A and who agreed to participate within a pre-specified time frame ( Fig. 1 ). The study (Clinicaltrials.gov identifier NCT03058562, EudraCT-No 2016–004294–40) was carried out between February 6, 2017, and September 20, 2017, at the early-phase clinical trial unit at the Clinical Research Center (CRC), Hannover Medical School (MHH), Germany. The trial was conducted in accordance with Good Clinical Practice, following local laws and regulations, and was approved by the local ethics committee at MHH (no. 7285 M) and the Federal Institute for Drugs and Medical Devices (BfArM, no. 4041769). Patients provided written informed consent before entering either part of the study.
Fig. 1.
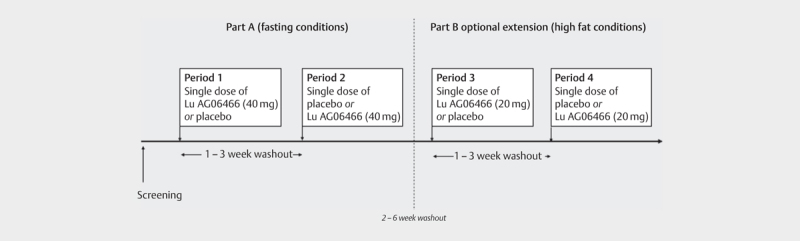
The study design.
Patients
Twenty patients were recruited from the TS outpatient clinic at MHH and also via German TS advocacy groups. Adult (18–65 years) patients with TS according to DSM-5 and a Yale Global Tourette Severity Scale (YGTSS) -Total Tic Score (TTS)>18 [range 0–50] 15 at screening were eligible for inclusion in the study. For≥30 days before the screening visit, patients taking daily medications for tics or psychiatric comorbidities had to be on a stable dose (except cannabis, cannabis extracts, or medical products containing cannabinoids, which were stopped≥4 days prior to study entry and during the study) and were expected to remain on a stable dose during the study. Key exclusion criteria were evidence of alcohol, drug, or chemical abuse (including recreational cannabis use) within one year before the screening, current or previous cannabis dependency, cannabis withdrawal symptoms, history of psychosis or schizophrenia or diagnosis of any unstable psychiatric disorder, or suicidal ideation within 12 months preceding screening; and treatment with potent cytochrome P450 3A4/5 inducers, or strong P450 3A4/5 inhibitors.
Treatment
In part A, patients were randomized by concealed, computer-generated assignment to either a single fasted dose of 40 mg of Lu AG06466 or placebo in Period 1 followed by a 1–3-week washout period and then the other study treatment in Period 2. In each treatment period, patients were hospitalized in the clinical trial unit for up to 48 h, from the night before the start of dosing to enforce abstinence with cannabinoids, fasting, and to allow a timely start in the morning and ending (at the earliest) on the morning after the treatment day. An independent staff member (not otherwise involved in the study) dispensed study medication of identical appearance following the randomized assignments. The investigators, patients, raters, and the sponsor were blinded to treatment during study conduct.
In part B (pharmacokinetic extension), patients were re-randomized to either a single dose of 20 mg of Lu AG06466 or placebo with a high-fat breakfast in period 3, with the other treatment in period 4. The dose with a meal was chosen based on the expectation of higher plasma exposure of the active moiety, Lu AG06466, and the MAGL-selective, CNS-penetrant, active metabolite Lu AG06988. The procedures in part B were the same as in part A, including a 1–3-week washout period between single-day treatments (from period 2–3 and from period 3–4). Patients continued their normal medications, except they discontinued cannabis/cannabinoids for four days prior to each treatment period.
Efficacy and safety assessments
Efficacy was assessed by experts in tic assessment at baseline, 4-, and 8-h post-dose. Key endpoints were the video-based Modified Rush Video Scale (MRVS) 16 , YGTSS-TTS, and the self-assessment Adult Tic Questionnaire (ATQ) 17 , as well as effects on premonitory urges using items 1–9 of the Premonitory Urge for Tic Scale (PUTS) 18 . Standardized video recordings (MRVS) were rated by an independent clinician blinded to treatment, treatment date, and acquisition time relative to dose. The ATQ and PUTS were also assessed at 12 hours post-dose. In addition, YGTSS motor tic (YGTSS-MTS), vocal tic (YGTSS-VTS), and YGTSS global scores (YGTSS-GS) were assessed at 4 h and 8 h. Psychiatric comorbidities were assessed using the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) 19 for OCD; the Conners’ Adult Attention Deficit and Hyperactivity Rating Scale (CAARS) 20 for ADHD; the Beck Anxiety Inventory (BAI) 21 for anxiety; the Beck Depression Inventory (BDI-II) 22 for depression. Effects on overall impairment and improvement were assessed using the Clinical Global Impression of Improvement (CGI-I) and the Clinical Global Impression of Severity (CGI-S) 23 , and patients were asked to guess the treatment sequence they had received. Where needed, assessments were modified for a single-dose study which considered changes from baseline to 4, 8, and 12 h post-dose. Safety was assessed through an adverse event (AE) reporting by an investigator who was not involved in clinical assessments, and by assessments of vital signs, clinical laboratory tests, and ECG.
Pharmacokinetic and Pharmacodynamic assessments
The pharmacokinetic profiles of Lu AG06466 and its metabolite Lu AG06988 were measured by high-performance liquid chroma-tography of the plasma. The pharmacodynamic activity and target engagement of Lu AG06466 were monitored over time by the rate of 2-AG hydrolysis by mass spectrometry in peripheral blood mononuclear cells (PBMC) using a fit-for-purpose assay modified from previously reported methods 14 24 .
Statistics
Effect sizes (the mean difference between treatment and control divided by pooled standard deviation) were computed based on means and between-patient variability estimates from several literature references of relevant drug efficacy studies included those with antipsychotics or THC 10 11 25 . A sample size of 20 patients was estimated to provide 93% power to yield a statistically significant (alpha=0.05, 1-sided) difference between treatments in a 2-period crossover trial for an effect size of 1.0 assuming a within-patient correlations coefficient of 0.5 for efficacy endpoints.
The primary analysis population for efficacy was the Per Protocol population (PP population), which included all randomized patients who completed the treatment periods without a major protocol violation. Safety was assessed in all randomized patients who took the study drug. For key endpoints, the time-weighted average (TWA) of all post-dose differences was compared using a mixed-model repeated-measures analysis including treatment, period, observation time, baseline covariates, interactions as fixed effects as well as random patient effects (see the Supplemental Appendix ). In addition, changes from pre-dose baseline were also compared for treatment effects versus placebo by separate t-tests at each time-point (i. e., 4, 8, and 12 h), with no adjustments for covariates. Lu AG06466-associated changes in clinical symptoms were considered significant versus placebo with p-values<0.05 (one-sided) without correction for multiple endpoints or methods of analysis.
Results
Study flow and patient characteristics
Of the 23 patients screened, 20 patients were enrolled and completed part A ( Fig. 2 ) and one patient was excluded from the PP population due to a protocol violation (taking the CYP3A4 inducer carbamazepine). Seven of the eight patients who agreed to continue study participation in part B completed the extended pharmacokinetic evaluation. One patient taking a placebo in period 3 discontinued due to AEs (headache, nausea, fatigue, vomiting, loss of appetite, and upper abdominal pain). Baseline characteristics for patients entering part A are provided in Table 1 ; patients were predominantly male (n=16 out of 20) and the mean±SD age was 34±11 [18–54] years. The mean±SD YGTSS-GS was 43.7±14.4, with a mean YGTSS-TTS subscore of 27.2±6.4, consistent with moderate-to-severe tics. Eleven of 20 patients (55.0%) regularly used cannabis-based medicines to treat TS.
Fig. 2.
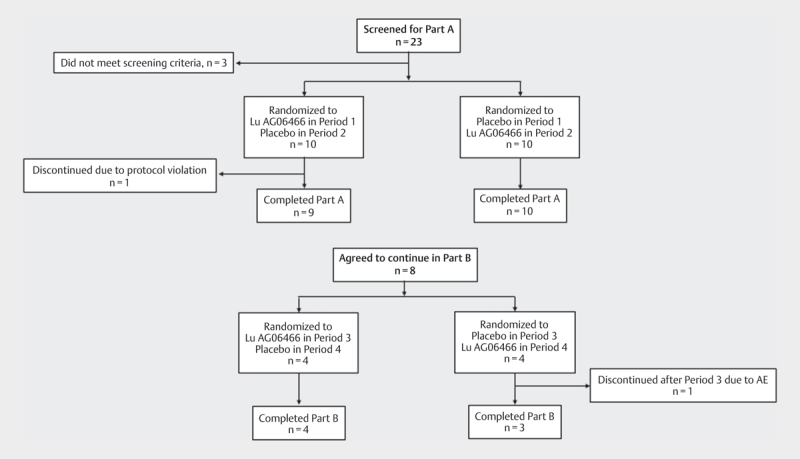
The study flow. Part B was a study extension following a protocol amendment.
Table 1 Baseline demographics of the patients included in the study.
| Characteristic | N=20 | ||
|---|---|---|---|
| Age (years); mean±SD [range] | 33.7±10.5 [18–54] | ||
| Sex (Male/Female); n (%) | 16 (80%)/4 (20%) | ||
| Race (Caucasian); n (%) | 20 (100%)% | ||
| Tics | Age at onset (mean, years) | 6.7 | |
| Severity | YGTSS-TTS (mean±SD | 26.7±6.2 | |
| YGTSS-GS (mean±SD) | 43.6±14.6 | ||
| MRVS (mean±SD) | 12.3±3.8 | ||
| Premonitory urges | PUTS (mean±SD) | 19.8±5.6 | |
| Comorbidities | ADHD*; n (%) | 4 (20%) | |
| OCD*; n (%) | 5 (25%) | ||
| Current treatment of TS | Cannabis/cannabinoid drugs; n (%) | 11 (55%) | |
| Antipsychotics; n (%) | 6 (30%) | ||
| No pharmacological treatment | 4 (20%) | ||
*Patients were assessed for obsessive compulsive disorder (OCD) and attention deficit/hyperactivity disorder (ADHD) at the screening, and were diagnosed according to clinical judgment. MRVS: Modified Rush Video Scale, PUTS: Premonitory Urge for Tic Scale; TS: Tourette Syndrome; YGTSS: Yale Global Tic Severity Scale; YGTSS-GS: Yale Global Tic Severity Scale – Global Score; YGTSS-TTS Yale Global Tic Severity Scale -Total Tic Score.
Efficacy analyses
Despite the small sample size, all scales showed an overall trend of tic reduction during part A of the trial. Placebo-adjusted reductions in tics and premonitory urges following treatment with Lu AG06466 during part A are shown in Table 2 . Although the mean [90% CI] TWA overall treatment effects versus placebo of −0.7 [−2.0, 0.5] for MRVS and −1.1 [−2.7, 0.5] for YGTSS-TTS failed to reach statistical significance, analysis of each time point revealed that the treatment effect on YGTSS-TTS was significant versus placebo at the 8 h time point (−3.0 [−5.4, −0.6], p=0.04) and statistically significant mean placebo-adjusted reductions were also observed for YGTSS-MTS at 4 hours post-dose (−1.5 [−2.8, −0.3], p=0.05). Patients treated with Lu AG06466 also showed a reduction of about 30% in mean tic intensity, as self-assessed by the ATQ, with less robust effects on tic frequency. In addition, motor tic intensity was significantly decreased, relative to placebo, at 4 (−4.6 [−7.4, −1.8], p=0.01), 8 (−4.5 [−7.1, −2.0]; p<0.01), and 12 hours (−3.4 [−5.0, −1.7], p<0.01) after Lu AG06466 treatment. No reductions in ATQ vocal tic intensity were observed, however, treatment with Lu AG06466 did result in a significant placebo-adjusted reduction in premonitory urges as measured by PUTS at 4 and 12 h post-dose, but not at 8 hours.
Table 2 Effects of a single dose of Lu AG06466 (40 mg) on tics and premonitory urges during Part A of the study (periods 1 and 2).
| Outcome | Placebo-adjusted change from baseline | |||||
|---|---|---|---|---|---|---|
| Time period post-dose (t-test) | Time weighted analysis (MMRM) | |||||
| 4 h | 8 h | 12 h | ||||
| MRVS | −1.1 [−3.0, 0.9] | −1.4 [−3.9, 1.1] | N/A | −0.7 [−2.0, 0.5] | ||
| YGTSS | TTS | −2.0 [−4.3, 0.3] | −3.0 [−5.4, −0.6]* | N/A | −1.1 [−2.7, 0.5] | |
| MTS | −1.5 [−2.8, −0.3]* | −1.3 [−2.3, −0.2] | ||||
| VTS | −0.5 [−1.9, 0.9] | −1.4 [−3.1, 0.3] | ||||
| GS | −5.7 [−11.9, 0.5] | −5.8 [−12.7, 1.1] | ||||
| ATQ | Frequency | MT | −2.9 [−7.0, 1.3] | −5.1 [−9.0, −1.1]* | −3.5 [−6.4, −0.6] | −1.7 [−4.0, 0.6] |
| VT | −1.4 [−3.4, 0.5] | −1.6 [−3.2, 0.0] | 1.1 [−2.2, 0.1] | −0.1 [−1.1, 0.8] | ||
| Total | −4.3 [−10.0, 1.4] | −6.6 [−11.8, 1.5]* | −4.6 [−8.0, 1.2]* | −2.6 [−5.4, 0.3] | ||
| Intensity | MT | −4.6 [−7.4, −1.8]* | −4.5 [−7.1, −2.0]* | −3.4 [−5.0, −1.7]* | −3.0 [−4.3, −1.6]* | |
| VT | −1.4 [−2.4, −0.3]* | −1.1 [−2.1, 0.0] | −1.0 [−2.0, 0.0] | −0.7 [−1.1, −0.3]* | ||
| Total | −5.9 [−9.5, −2.4]* | −5.6 [−8.9, −2.3]* | −4.4 [−6.7, −2.0]* | −4.2 [−5.7, −2.6]* | ||
| PUTS | −1.9 [−3.4, −0.4]* | −0.7 [−2.1, 0.6] | −1.3 [−2.2, −0.4]* | −0.8 [−1.5, 0.0] | ||
All post-dose measurements were analyzed by mixed model repeated measures (MMRM) and summarized by time-weighted average (TWA). *Statistical significance was declared by a one-sided p-value≤0.05. ATQ: Adult Tic Questionnaire; GS: Global Score; MT: Motor Tics; MTS: Motor Tic Score; MRVS: Modified Rush Video Scale; PUTS: Premonitory Urge for Tic Scale; TS: Tourette Syndrome; TTS: Total Tic Score; VT: Vocal Tics; VTS: Vocal Tic Score; YGTSS: Yale Global Tic Severity Scale.
Global assessment of change showed significant improvement for Lu AG06466 relative to placebo on CGI-I at 4 hours post-dose (p=0.045) and on CGI-S at 8 hours post-dose (p=0.03). Six patients were assessed as ‘very much better’ or ‘much better’ with Lu AG06466, compared to only two patients after treatment with placebo. There were no significant changes in ADHD, OCD, anxiety, and depression as assessed by CAARS, Y-BOCS, BAI, and BDI-II. Thirteen out of 18 patients guessed their treatment sequence correctly and one patient did not provide a guess.
In the pharmacokinetic extension (part B), tic reductions from baseline were observed on some scales with placebo, but not with Lu AG06466. Patients receiving placebo showed an adjusted mean [90% CI] reduction from baseline of −2.4 [−3.3 to −1.5] points on YGTSS-TTS (TWA), −2.3, [−3.6 to −1.1] points on ATQ number of tics, and 5.1 [−6.4 to −3.9] points on ATQ intensity, but 90% confidence intervals crossed 0 for all other scale parameters and patients receiving Lu AG06466. No significant effects were seen on CGI or scales of psychiatric comorbidity.
Adverse events
Overall, a single dose of Lu AG06466 was well-tolerated with full details of AEs during part A are presented in Table 3 . In part A, more patients reported AEs after treatment with Lu AG06466, compared to placebo, with the most frequently cited being headache, somnolence, and fatigue. In general, AEs were transient and were resolved. No serious AEs occurred. There were no discontinuations due to Lu AG06466-related AEs. In part B, more AEs were reported after placebo (23 events reported by seven patients) compared to Lu AG06466 (three events reported by two patients).
Table 3 Adverse events (AE) during Part A of the study.
| Number of patients (%) | |||
|---|---|---|---|
| Placebo (N=19) | 40 mg Lu AG06466 (N=20) | Overall (N=20) | |
| Any AEs | 8 (42.1%) | 13 (65.0%) | 15 (75.0%) |
| AEs (Preferred term) reported in>2 patients | |||
| Dizziness | 1 (5.3%) | 2 (10.0%) | 3 (15.0%) |
| Headache | 2 (10.5%) | 7 (35.0%) | 9 (45.0%) |
| Somnolence | 1 (5.3%) | 5 (25.0%) | 5 (25.0%) |
| Fatigue | 1 (5.3%) | 3 (15.0%) | 4 (20.0%) |
Pharmacokinetics and Pharmacodynamics
Evidence of systemic plasma exposure to Lu AG06466 was observed in all Lu AG06466-treated patients following single oral administrations in the fasted state (40 mg) or the fed state (20 mg). Under fasting conditions, plasma exposure of Lu AG06466 and its active metabolite Lu AG06988 measured over time, reached peak concentrations 2 to 4 h post-dose ( Fig. 3a , Supplemental Table e1 ). Consistent with plasma exposures, MAGL activity was reduced by 80.5% following administration of Lu AG06466 by 4 hours, inhibition was maintained through 8 hours, and activity returned to near baseline levels by 24 h post-dose ( Fig. 3b ). In part B, mean exposure values for Lu AG06466 were about 2-fold higher following a high-fat meal compared to the fasted state, although the Lu AG06466 dose administered was 2-fold lower ( Supplemental Table e2 ). However, unlike the parent molecule, mean exposure values for the metabolite Lu AG06988 were lower in part B than in part A. Following an administration of 20 mg in the fed state, mean MAGL activity was reduced by 87% at 8 h post-dose administration.
Fig. 3.
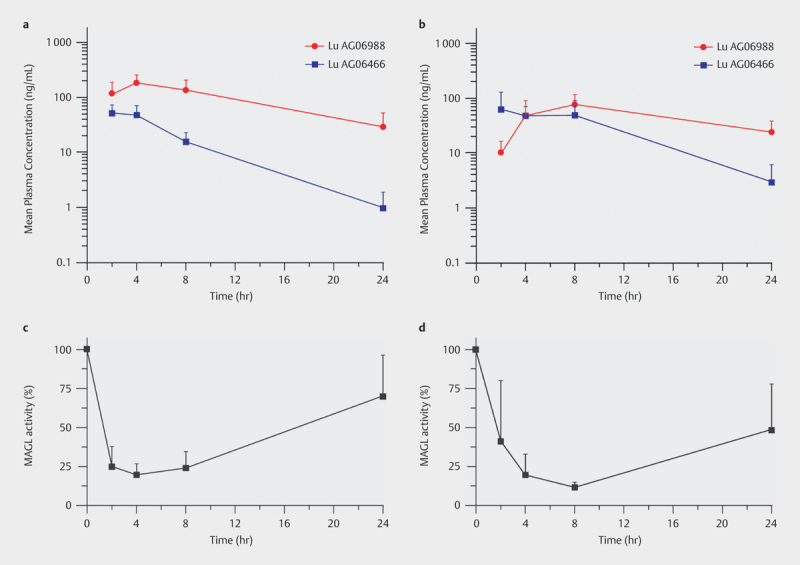
Mean plasma exposure of Lu AG06466 (40 mg) and its active metabolite Lu AG06988 under ( a ) fasting conditions (n=19) and ( b ) fed conditions (n=7). Target engagement measured as MAGL activity inhibition in peripheral blood mononuclear cells after administration of Lu AG06466 (40 mg) in ( c ) fasting conditions (n=19) and ( d ) fed conditions (n=7).
Discussion
This randomized, double-blind, placebo-controlled phase 1b trial indicates that modulation of the ECS with the highly selective MAGL inhibitor Lu AG06466 affects a relevant tic reduction, as assessed by the YGTSS-TTS and the self-assessment ATQ. A reduction in premonitory urges preceding the tics was also observed using the PUTS. Clinical global assessment of change supported a generally well-tolerated and positive impact of treatment with single-doses of Lu AG06466.
In this exploratory study, three different approaches to tic assessment were used to explore pharmacodynamic efficacy on tic severity. We decided on this multi-assessment approach, because (i) all tic severity rating scales suffer from limitations, (ii) tic self-assessment may differ from results obtained from examiner assessments, (iii) our study design required modifications of the YGTSS-TTS as the gold standard for tic assessment and the self-assessment ATQ, and (iv) the assumed advantage of the video-based assessment MRVS to capture short-term fluctuations of tics 26 . However, while the YGTSS-TTS and the ATQ demonstrated significant tic reductions, the MRVS did not reveal efficacy. This discrepancy in our findings might be explained by the fact that the MRVS, although theoretically the ideal instrument to capture short-term tic fluctuations, is also more vulnerable to other influences such as stress than the YGTSS-TTS and the ATQ. Correlation between the MRVS and the YGTSS is unclear since high as well as a poor correlation has been reported 27 28 29 30 . Currently, a revision of the MRVS is in process. On the other hand, both the YGTSS-TTS and the ATQ had to be adapted to the single-dose study design and used several times within a short period instead of tic assessment based on information from the previous week as instructed in the original versions. Furthermore, although the YGTSS has only recently been revised 31 further limitations of the YGTSS have been identified 32 . The ATQ shows a strong correlation with the YGTSS 32 ; however, it has not yet been widely used and further validation is missing 26 .
It is noteworthy that we also found a significant improvement of premonitory urges after treatment with Lu AG06466. This is in line with data obtained from recent studies using different exocannabinoids also reporting improvement of premonitory urges 33 . This finding is of paramount importance since it is believed that premonitory urges may represent the key element of TS; accordingly, patients often describe that a tic is only performed to relieve this preceding sensation 34 . As such, the improvements of tics and premonitory urges demonstrated after a single oral dose of Lu AG06466 adds to the accumulating evidence supporting ECS involvement in the pathobiology of TS. However, this evidence is mainly based on data from open uncontrolled case series using different exocannabinoids, two small randomized, placebo-controlled studies using pure THC 7 8 9 10 11 , and elevated cerebrospinal fluid levels of endocannabinoids in TS 35 . To the best of our knowledge, there is currently no medication for tics available with efficacy also on premonitory urges.
Part B was primarily designed as a pharmacokinetic extension to understand if there is a food effect on drug absorption with the tested formulation, although safety and efficacy measures were also included. Lu AG06466 has fast absorption and elimination kinetics with t max in the range of 2–4 h and t ½ in the range of 3–5 h. It was hypothesized that administration of 20 mg Lu AG06466 with a high-fat meal would increase the exposure of Lu AG06466 and the major active metabolite, Lu AG06988; the meal was also expected to reduce pharmacokinetic variability between patients. In reality, however, while administration with a high-fat meal increased the exposure to Lu AG06466, there was lower plasma exposure of the active metabolite. From a pharmacological point of view, levels of MAGL-inhibition were similar in part A and part B. While the part B extension was not designed to further assess efficacy (limiting any efficacy conclusions from this part), the lack of separation from placebo in terms of tic reduction may reflect a mix of factors including the small sample size and expectation bias (as all patients in part B had already completed tic outcomes, including the YGTSS-TTS, several times in part A). We also cannot rule out the effect of a slightly lower dose (and thus lower plasma exposure) in part B.
Single doses of Lu AG06466 were generally well-tolerated, with an AE profile similar to that seen in single-dose and multiple-dose studies in healthy volunteers 36 . There were no serious AEs and no patient discontinuations due to Lu AG06466–related AEs. The most commonly observed AEs were transient and included headache, somnolence, and fatigue. Since a single dose of 40 mg of Lu AG06466 was well-tolerated, it can be anticipated that maintenance treatment with Lu AG06466 will be even better tolerated when treatment is started with a lower dose – comparable to the general recommendation for cannabis-based medicines according to the principle “start low und go slow.”
This exploratory study has several limitations, most notably the single-dose design which is likely to have limited our ability to detect any impact on comorbid psychiatric symptoms including ADHD, OCD, depression, and anxiety. In addition, patients were hospitalized in an unfamiliar environment in the clinical trial unit for two nights, which might have an impact on overall well-being and may, therefore, have influenced tics and psychiatric symptoms. On the other hand, it is remarkable that we were able to demonstrate significant improvement of tics against this background since stress is regarded as the main environmental factor that worsens tics. While patients were generally representative of the adult TS target population, relatively few patients in this study suffered from typical comorbidities, and a large proportion had used cannabis or cannabis-based agents previously for their TS symptoms. Although cannabis-based medication had to be stopped only≥4 days prior to study entry, we do not believe that results were influenced by cannabis withdrawal syndrome, since in the context of medicinal use, even abrupt withdrawal from long-term treatment causes only mild and transient disturbances in a minority of patients but no withdrawal syndrome 37 . Furthermore, the number of patients included was small (including only four females) and insufficient to look for potential age and sex differences suggested by other studies 38 39 40 . The per-protocol population (patients with complete data and no major protocol violations) was chosen as the most scientifically valid sample for evaluating the proof-of-concept hypotheses.
In summary, this single-dose trial elucidated the first clinical evidence for a positive pharmacodynamic effect of the selective MAGL inhibitor Lu AG06466 for the treatment of tics and premonitory urges in adult patients with TS. However, despite these promising results, efficacy was not replicated in a subsequent, larger phase II study 41 .
Author Contributions
KMV, CB, and CS participated in the study design, research, and data collection and contributed to the first draft of the manuscript. KMV, CF, CB, JI, HL, and CS contributed to the analysis and interpretation of data, writing, review, and approval of the manuscript for its publication.
Acknowledgements
The authors wish to thank all the patients who participated in the study. We also thank Alan Ezekovic of Abide Therapeutics for his unwavering support as well as Nathalie C. Franc (Franc Consulting, San Diego, CA, funded by Abide Therapeutics), Julianne A. Hunt (Abide Therapeutics), Aundrea R. Coppola (Abide Therapeutics) and Anita Chadha-Patel (ACP Clinical Communications Ltd, funded by H.Lundbeck A/S) for support in the preparation, revisions and editing of this paper.
Funding Statement
Funding This study was sponsored by Abide Therapeutics, USA. Funding for editorial support was provided by H. Lundbeck A/S, Denmark.
Footnotes
Conflict of Interest KMV reports financial or material research support from the EU (FP7-HEALTH-2011 No. 278367, FP7-PEOPLE-2012-ITN No. 316978), the German Research Foundation (DFG: GZ MU 1527/3–1), the German Ministry of Education and Research (BMBF: 01KG1421), the National Institute of Mental Health (NIMH), the Tourette Gesellschaft Deutschland e.V., the Else-Kröner-Fresenius-Stiftung, and Abide Therapeutics, Almirall Hermal GmbH, GW pharmaceuticals, Lundbeck, Syneos Health, and Therapix Biosciences Ltd. She has received consultant’s honoraria from Abide Therapeutics, Allmiral, Boehringer Ingelheim International GmbH, Bionorica Ethics GmbH, CannaMedical Pharma GmbH, Canopy Grouth, Columbia Care, CTC Communications Corp., Eurox Deutschland GmbH, Global Praxis Group Limited, IMC Germany, Lundbeck, Resalo Vertrieb GmbH, Sanity Group, STADAPHARM GmbH, Synendos Therapeutics AG, and Tilray. She is/was a consultant or advisory board member for Abide Therapeutics, The Academy of Medical Cannabis Limited, Alirio, Aphria Deutschland GmbH, CannaMedical Pharma GmbH, Bionorica Ethics GmbH, CannaXan GmbH, Canopy Growth, Columbia Care, CTC Communications Corp., IMC Germany, Leafly Deutschland GmbH, Lundbeck, Nuvelution TS Pharma Inc., Resalo Vertrieb GmbH, Sanity Group, Syqe Medical Ltd., Therapix Biosciences Ltd., Tilray, Wayland Group, and CTC Communications Corporation. She has received speaker’s fees from Aphria Deutschland GmbH, Cogitando GmbH, Emalex, Eurox Deutschland GmbH, EVER pharma GmbH, PR Berater, Spectrum Therapeutics GmbH, Tilray, and Wayland Group; she has received royalties from Medizinisch Wissenschaftliche Verlagsgesellschaft Berlin, Elsevier, and Kohlhammer. CF was an investigator in the study and has no conflict of interest; CB was employed by Abide Therapeutics at the time of study and reports consultancy for Lundbeck; JI and HL are employed by H. Lundbeck A/S; CS acted as deputy PI and has no conflict of interest.
Zusätzliches Material
References
- 1.Bloch M H, Leckman J F. Clinical course of Tourette syndrome. J Psychosom Res. 2009;67:497–501. doi: 10.1016/j.jpsychores.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martino D, Ganos C, Pringsheim T M. Tourette syndrome and chronic tic disorders: The clinical spectrum beyond tics. Int Rev Neurobiol. 2017;134:1461–1490. doi: 10.1016/bs.irn.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 3.Hirschtritt M E, Lee P C, Pauls D L et al. Lifetime prevalence, age of risk, and genetic relationships of comorbid psychiatric disorders in Tourette syndrome. JAMA Psychiatry. 2015;72:325–333. doi: 10.1001/jamapsychiatry.2014.2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quezada J, Coffman K A. Current approaches and new developments in the pharmacological management of Tourette syndrome. CNS drugs. 2018;32:33–45. doi: 10.1007/s40263-017-0486-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pringsheim T, Holler-Managan Y, Okun M S et al. Comprehensive systematic review summary: Treatment of tics in people with Tourette syndrome and chronic tic disorders. Neurology. 2019;92:907–915. doi: 10.1212/wnl.0000000000007467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganos C. Tics and Tourette’s: update on pathophysiology and tic control. Curr Opin Neurol. 2016;29:513–518. doi: 10.1097/wco.0000000000000356. [DOI] [PubMed] [Google Scholar]
- 7.Müller-Vahl K R, Kolbe H, Schneider U et al. Cannabinoids: Possible role in patho-physiology and therapy of Gilles de la Tourette syndrome. Acta Psychiatr Scand. 1998;98:502–506. doi: 10.1111/j.1600-0447.1998.tb10127.x. [DOI] [PubMed] [Google Scholar]
- 8.Abi-Jaoude E, Chen L, Cheung P et al. Preliminary evidence on cannabis effectiveness and tolerability for adults with Tourette syndrome. J Neuropsychiatry Clin Neurosci. 2017;29:391–400. doi: 10.1176/appi.neuropsych.16110310. [DOI] [PubMed] [Google Scholar]
- 9.Thaler A, Arad S, Schleider L B et al. Single center experience with medical cannabis in Gilles de la Tourette syndrome. Parkinsonism Relat Disord. 2019;61:211–213. doi: 10.1016/j.parkreldis.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Müller-Vahl K R, Schneider U, Koblenz A et al. Treatment of Tourette’s syndrome with Delta 9-tetrahydrocannabinol (THC): a randomized crossover trial. Pharmacopsychiatry. 2002;35:57–61. doi: 10.1055/s-2002-25028. [DOI] [PubMed] [Google Scholar]
- 11.Müller-Vahl K R, Schneider U, Prevedel H et al. Delta 9-tetrahydrocannabinol (THC) is effective in the treatment of tics in Tourette syndrome: a 6-week randomized trial. J Clin Psychiatry. 2003;64:459–465. doi: 10.4088/jcp.v64n0417. [DOI] [PubMed] [Google Scholar]
- 12.Howlett A C. The cannabinoid receptors. Prostaglandins Other Lipid Mediat. 2002;68-69:619–631. doi: 10.1016/s0090-6980(02)00060-6. [DOI] [PubMed] [Google Scholar]
- 13.Alger B E, Kim J. Supply and demand for endocannabinoids. Trends Neurosci. 2011;34:304–315. doi: 10.1016/j.tins.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blankman J L, Cravatt B F. Chemical probes of endocannabinoid metabolism. Pharmacol Rev. 2013;65:849–871. doi: 10.1124/pr.112.006387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leckman J F, Riddle M A, Hardin M T et al. The Yale Global Tic Severity Scale: Initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry. 1989;28:566–573. doi: 10.1097/00004583-198907000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Goetz C G, Pappert E J, Louis E D et al. Advantages of a modified scoring method for the Rush Video-Based Tic Rating Scale. Mov Disord. 1999;14:502–506. doi: 10.1002/1531-8257(199905)14:3<502::aid-mds1020>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 17.Abramovitch A, Reese H, Woods D W et al. Psychometric properties of a self-report instrument for the assessment of tic severity in adults with tic disorders. Behav Ther. 2015;46:786–796. doi: 10.1016/j.beth.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McGuire J F, McBride N, Piacentini J et al. The premonitory urge revisited: An individualized premonitory urge for tics scale. J Psychiatr Res. 2016;83:176–183. doi: 10.1016/j.jpsychires.2016.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodman W K, Price L H, Rasmussen S A et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 20.Walls B D, Wallace E R, Brothers S L et al. Utility of the Conners’ Adult ADHD Rating Scale validity scales in identifying simulated attention-deficit hyperactivity disorder and random responding. Psychol Assess. 2017;29:1437–1446. doi: 10.1037/pas0000530. [DOI] [PubMed] [Google Scholar]
- 21.Beck A T, Epstein N, Brown G et al. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 22.Beck A, Steer R A, Gregory K. BDI-II, Beck Depression Inventory: Manual San Antonio, Tex. Psychological Corp. :1196. [Google Scholar]
- 23.Guy W. Rockville, MD: Department of Health, Education, and Welfare, Washington, DC; 1976. Clinical global impressions. In: ECDEU Assessment Manual for Psychopharmacology; pp. 218–222. [Google Scholar]
- 24.Clapper J R, Henry C L, Niphakis M J et al. Monoacylglycerol lipase inhibition in human and rodent systems supports clinical evaluation of endocannabinoid modulators. J Pharmacol Exp Ther. 2018;367:494–508. doi: 10.1124/jpet.118.252296. [DOI] [PubMed] [Google Scholar]
- 25.Evans J, Seri S, Cavanna A E. The effects of Gilles de la Tourette syndrome and other chronic tic disorders on quality of life across the lifespan: a systematic review. Eur Child Adolesc Psychiatry. 2016;25:939–948. doi: 10.1007/s00787-016-0823-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martino D, Pringsheim T M, Cavanna A E et al. Systematic review of severity scales and screening instruments for tics: Critique and recommendations. Mov Disord. 2017;32:467–473. doi: 10.1002/mds.26891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Franzkowiak S, Pollok B, Biermann-Ruben K et al. Motor-cortical interaction in Gilles de la Tourette syndrome. PLoS One. 2012;7:e27850. doi: 10.1371/journal.pone.0027850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gerasch S, Kanaan A S, Jakubovski E et al. Aripiprazole improves associated comorbid conditions in addition to tics in adult patients with Gilles de la Tourette syndrome. Front Neurosci. 2016;10:416. doi: 10.3389/fnins.2016.00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kanaan A S, Jakubovski E, Muller-Vahl K. Significant tic reduction in an otherwise treatment-resistant patient with Gilles de la Tourette syndrome following treatment with nabiximols. Brain Sci. 2017:7. doi: 10.3390/brainsci7050047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maling N, Hashemiyoon R, Foote K D et al. Increased thalamic gamma band activity correlates with symptom relief following deep brain stimulation in humans with Tourette’s syndrome. PLoS One. 2012;7:e44215. doi: 10.1371/journal.pone.0044215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGuire J F, Piacentini J, Storch E A et al. A multicenter examination and strategic revisions of the Yale Global Tic Severity Scale. Neurology. 2018;90:e1711–e1719. doi: 10.1212/WNL.0000000000005474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haas M, Jakubovski E, Fremer C et al. Yale Global Tic Severity Scale (YGTSS): Psychometric quality of the gold standard for tic assessment based on the large-scale EMTICS Study. Front Psychiatry. 2021;12:626459. doi: 10.3389/fpsyt.2021.626459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Milosev L M, Psathakis N, Szejko N et al. Treatment of Gilles de la Tourette syndrome with cannabis-based medicine: Results from a retrospective analysis and online survey. Cannabis Cannabinoid Res. 2019;4:265–274. doi: 10.1089/can.2018.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cavanna A E, Black K J, Hallett M et al. Neurobiology of the premonitory urge in Tourette’s syndrome: Pathophysiology and treatment implications. J Neuropsych Clin Neurosci. 2017;29:95–104. doi: 10.1176/appi.neuropsych.16070141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Muller-Vahl K R, Bindila L, Lutz B et al. Cerebrospinal fluid endocannabinoid levels in Gilles de la Tourette syndrome. Neuropsychopharmacology. 2020;45:1323–1329. doi: 10.1038/s41386-020-0671-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fraser I P, Blankman J, Clapper J.Preclinical characterization and first-in-human administration of a selective monoacylglycerol lipase inhibitor, ABX-1431 Conference Abstract: EUFEMED 2017 10.3389/conf.fphar.2017.62.00011Front Pharmacol 2019 [DOI] [Google Scholar]
- 37.Robson P. Abuse potential and psychoactive effects of delta-9-tetrahydrocannabinol and cannabidiol oromucosal spray (Sativex), a new cannabinoid medicine. Expert Opin Drug Saf. 2011;10:675–685. doi: 10.1517/14740338.2011.575778. [DOI] [PubMed] [Google Scholar]
- 38.Tabatadze N, Huang G, May R M et al. Sex differences in molecular signaling at inhibitory synapses in the hippocampus. J Neurosci. 2015;35:11252–11265. doi: 10.1523/jneurosci.1067-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Craft R M, Marusich J A, Wiley J L. Sex differences in cannabinoid pharmacology: A reflection of differences in the endocannabinoid system? Life Sci. 2013;92:476–481. doi: 10.1016/j.lfs.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Struik D, Sanna F, Fattore L. The modulating role of sex and anabolic-androgenic steroid hormones in cannabinoid sensitivity. Front Behav Neurosci. 2018;12:249. doi: 10.3389/fnbeh.2018.00249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Müller-Vahl KR, Fremer C, Beals C, Ivkovic J, Loft H, Schindler C. Monoacylglycerol Lipase Inhibition in Tourette Syndrome: A 12-Week, Randomized, Controlled Study. Mov Disord. 2021 Oct; 36(10):2413- 2418. doi:10.1002/mds.28681 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


