Abstract
Lung cancer is a malignant tumor with high incidence and mortality across the world. The use of immune checkpoint inhibitors for lung cancer has improved the prognosis of some lung cancer patients to a greater extent and provided a new direction for the clinical treatment of lung cancer. Immunotherapy still has limitations in terms of its appropriate population and adverse reactions. Particularly for non-small cell lung cancer (NSCLC) patients with epidermal growth factor receptor (EGFR) mutation, there has been no major breakthrough in current immunotherapy. Whether immunotherapy can bring new benefits after drug resistance is induced by tyrosine kinase inhibitor-targeted therapy and whether the combination of immunotherapy with other treatments can improve the prognosis remain to be studied in depth. In this article, we provide a detailed review of the relevant characteristics of the tumor microenvironment of NSCLC with EGFR mutation and the current research on immunotherapy for NSCLC with EGFR mutation.
Key words: Non-small cell lung cancer (NSCLC), Immunotherapy, Epidermal growth factor receptor (EGFR)-sensitive mutations
INTRODUCTION
According to the data of the Global Cancer Observatory (GLOBOCAN2020), the incidence and mortality of lung cancer in China account for 37.0% and 39.8% of those in the world, respectively. According to GLOBOCAN estimates, there were approximately 2.2 million new lung cancer cases worldwide in 2020, accounting for 11.4% of all malignant tumors, and there were approximately 1.8 million deaths, accounting for 18.0% of malignant tumor-related deaths1. According to the data released by the National Cancer Center, 57 per 100,000 people in China had lung cancer in 2019, and approximately 630,000 people die of lung cancer each year2. Lung cancer is also the malignant tumor with the heaviest burden in China3. From 2012 to 2015, the 5-year survival rate of lung cancer in the Chinese population was 19.7%, and most patients were already at an advanced stage when they were diagnosed. With the combined application of chemotherapy, radiotherapy, targeted therapy, and immunotherapy, the prognosis of lung cancer has been improved, but in general, the 5-year survival rate has not been significantly improved4.
Non-small cell lung cancer (NSCLC) accounts for approximately 80%–85% of lung cancer, and the driver gene mostly determines the treatment and prognosis of NSCLC at present. The patients with NSCLC positive for the epidermal growth factor receptor (EGFR) gene have benefited significantly from the EGFR-tyrosine kinase inhibitor (TKI) targeted therapy. The marketed EGFR-TKIs have been continually optimized. The third-generation TKIs have shown a better therapeutic effect, and even the drug resistance problem of the T790M mutation of the first-generation TKIs has been better resolved. However, the discovery of various new mutation sites and the emergence of complex drug resistance targets also pose more challenges for targeted therapy. As research on immune checkpoint inhibitors (ICIs) progresses, can immunotherapy become a new treatment for NSCLC with EGFR-sensitive mutations? Programmed death-1 (PD-1) inhibitors may be less effective at treating NSCLC patients with EGFR mutations5–8. A meta-analysis including five trials (Checkmate 017, 057, Keynote 010, OAK, and POPLAR) showed that treatment with ICIs prolonged the overall survival (OS) in the EGFR wild-type (WT) subgroup [hazard ratio (HR) = 0.67, 95% confidence interval (CI) = 0.60–0.75; p < 0.001] but did not perform well in the EGFR-mutant subgroup (HR = 1.11, 95% CI = 0.80–1.53; p = 0.540)5. A similar analysis confirmed that ICIs did not increase the OS of NSCLC patients with EGFR mutations compared with patients taking docetaxel (HR = 1.09, 95% CI = 0.84–1.41)9. This has aroused the interest of many people, who have explored the treatment efficacy and studied the mechanisms of PD-1/programmed cell death ligand 1 (PD-L1) ICIs in patients with EGFR mutation. In this article, we will review their efforts in detail.
EFFECT OF EGFR MUTATIONS ON THE TUMOR IMMUNE MICROENVIRONMENT
In addition to cancer cells, primary tumors also include a variety of stromal cells, of which T lymphocytes, myeloid cells [myeloid-derived suppressor cells (MDSCs), mesenchymal stem cells (MSCs), mast cells, macrophages, and neutrophils], cytokines, and exosomes constitute the immunomodulatory network of tumors10,11. The tumor microenvironment (TME) is an internal environment for the development and progression of tumor cells and promotes tumor metastasis. Interventions targeting the TME are an important part of tumor immunotherapy strategies10. The TME plays a specific role at different stages of tumor progression, gradually changing from the initial inhibition of tumor development and progression to a state of adaptation and promotion of tumor growth12. T lymphocytes change from having an immune surveillance function to an immune escape function through immunoediting and even exhibit immunosuppression, such as by recruiting regulatory T cells (Tregs) and MDSCs and upregulating the levels of immunosuppressive cells in the TME. Tumor-associated macrophages (TAMs) induce tumor cell invasion by releasing cell colony-stimulating factor 1 (CSF-1) and macrophage-derived epidermal growth factor (EGF). Cancer-associated fibroblasts, inflammatory cells, and various growth factors and immunomodulatory cytokines are involved in tumor progression7–9.
NSCLC with EGFR mutations has a unique TME that is mainly in a noninflammatory state. In this state, the inflammatory response around the tumor cells is weak, lymphocyte infiltration is reduced, and antitumor immunity is lowered. EGFR mutations can regulate potential factors associated with TME status through multiple pathways, such as through tumor-infiltrating lymphocytes (TILs)13–15, Tregs16,17, MDSCs18,19, TAMs, and immunomodulatory cytokines20.
EGFR Mutation and Tregs
Tregs are physiologically involved in maintaining immune tolerance and immune homeostasis. Under pathological conditions, Treg cells are found at a high frequency in various types of cancer and are considered to be a key obstacle to antitumor immunity. Forkhead box P3 (Foxp3) is one of the key transcription factors controlling the development and function of Tregs. Induction of Foxp3 expression in naive T cells in vivo or in vitro can lead to Treg-like immunosuppressive effects21–23. Cytokines such as transforming growth factor-β, interleukin (IL)-10, and IL-35 secreted by Treg cells can create an immunosuppressive environment that actively attenuates and inhibits the antitumor immune response of CD4+ T cells, CD8+ T cells, and natural killer cells9,24,25. On the other hand, Tregs constitutively express inhibitory molecules such as cytotoxic T-lymphocyte antigen 4 (CTLA-4), PD-1, and TIM-3, which bind to specific ligands to facilitate their inhibitory function.
The expression of indoleamine 2,3-dioxygenase (IDO) can upregulate Treg function and induce immune tolerance26,27. Huang et al. found that EGFR-containing exosomes can induce plastic transformation of tolerogenic dendritic cells (DCs) and cause DCs to produce IDO, which plays an important role in converting CD4+CD25− T cells into CD4+CD25+ Treg cells28. Amphiregulin (AREG) is one of the ligands of EGFR, and its higher expression in the plasma of NSCLC patients is associated with a poor prognosis29. In addition, as a specific molecule in the exosomes of tumor cells, amphiregulin plays an important role in promoting tumor progression30. Wang et al. found that amphiregulin can regulate the suppressive function of Treg through the EGFR/GSK-3/Foxp3 axis both in vitro and in vivo31. The EGFR-TKI gefitinib inhibits EGFR activity, restores GSK-3β activity, and attenuates Treg function32. Mascia et al. also showed that knockdown of EGFR expression significantly inhibited tumor cell growth and downregulated Treg infiltration into the TME33.
EGFR Mutation and TILs
TILs are a group of tumor-infiltrating and antigenic cell populations that are present in tumor nests and stroma34. CD8+ T cells act as antitumor immune cells in the TME to destroy malignant tumor cells by releasing cytokines such as interferon-γ, perforin, and granzyme B, and the number of CD8+ T cells determines the tumor cell killing rate. A high degree of infiltration of CD8+ TILs in NSCLC is associated with a good prognosis and treatment outcome35–38.
Teng et al. evaluated the efficacy of immunotherapy by establishing a TME model based on TIL and PD-L1 expression, suggesting that an immune-inflammatory TME (PD-L1+ and TIL+) is most likely to benefit from anti-PD-1/PDL1 therapy39. Some patients with EGFR mutations have lower TIL levels as well as a lower ratio of PD-L1+CD8+ TILs14,15,40. The decrease in CD8+ TIL levels may be related to the low expression of major histocompatibility complex (MHC) molecules. The MHC plays an important role in tumor antigen presentation. The tumor antigens of MHC class I molecules constitute the first signal for cell activation, they activate CD8+ T cells, and they play a role in the antitumor immune effect41.
EGFR Mutation With TAM and Immunoregulatory Suppressors
Macrophages are an important component in the TME, and it is well established that macrophages can polarize into two states in response to different microenvironmental stimuli, namely, classically activated M1 macrophages and alternatively activated M2 macrophages. The former typically show inflammatory functions, whereas the latter show anti-inflammatory functions. TAMs are thought to more closely resemble M2-polarized macrophages and facilitate tumor growth by inducing immune suppression. For NSCLC with EGFR mutations, whose TME is in a noninflammatory state, Chen et al. showed that EGFR activation can recruit M2 macrophages to suppress antitumor immunity by inducing the expression of ILT442. Wang et al. analyzed data among 515 human lung adenocarcinomas from the TCGA database and found that enumeration of alveolar macrophages (AMS) by CIBERSORT revealed a higher number of AMS in 32 EGFR-mutant tumors compared with 408 EGFR WT/KRAS WT tumors (p = 0.036) and 75 KRAS-mutant tumors. Their study showed that AMS promoted tumor progression in EGFR mutated NSCLC (p = 0.073)43. In addition, activation of the EGFR pathway can induce the release of multiple immunosuppressive factors, including TNF-β [transforming growth factor-β (TGF-β)], IL-10, vascular endothelial growth factor (VEGF), IDO, CC chemokine ligand 2 (CCL-2), arginase (ARG)-1 and adenosine, etc.44. These immunosuppressive agents can directly inhibit the killing of natural killer cells, the maturation of DCs, and the proliferation and function of cytotoxic T cells. Moreover, it can further inhibit the host antitumor immunity by promoting the transformation of CD3+CD4+CD25− cells to CD4+CD25FoxP3+ Tregs, inducing the polarization of TAM into M2 macrophages, and mediating the recruitment and activation of MDSCs45.
EGFR Mutation and MDSCs
MDSC is an immature and dysfunctional myeloid cell group differentiated from immature bone marrow cells (IMCS) under a variety of pathological conditions such as inflammation, infection, and cancer. It has a strong immunosuppressive function. MDSC, Treg, and Tam together constitute the main immunosuppressive cells of TME in patients with lung cancer. It has been reported that MDSC in lung cancer can be divided into two types, namely, monocyte CD33+CD11b+CD14+ MDSCs or granulocyte-like CD33+CD11b+CD14− MDSCs46. In EGFR mutant NSCLC, the activation of EGFR pathway can produce some cytokines (such as IDO and VEGF). These cytokines can induce IMCs to differentiate into MDSC and recruit MDSCs into TME, so as to play the function of immunosuppression. Continuous activation of EGFR signaling pathway in tumor cells can induce the activation of downstream STAT3, which is the main transcription factor regulating MDSC amplification47. However, there is no clear answer to whether EGFR mutation exists in IMC. Generally speaking, the activation of EGFR signaling pathway can lead to the activation of downstream signaling networks that affect multiple processes of cells, which may be the reason why EGFR-mutant NSCLC shows a TME significantly different from EGFR WT lung cancer, and MDSCs are an important participant in the formation of this noninflammatory microenvironment.
EGFR MUTATIONS CAUSE REDUCED IMMUNOGENICITY IN TUMOR CELLS
EGFR Causes Changes in Tumor Mutation Burden (TMB)
TMB is the total number of substitution, insertion, and deletion mutations per megabase in the coding region of tumor genes. It is a good biomarker for predicting the efficacy of immunotherapy. It can quantitatively estimate the total number of mutations in the coding region of tumor genomes. Higher TMB is associated with more neoantigens produced by tumors, easier recognition by immune cells, and long-term clinical responses48.
Cancer cells can produce tumor-specific antigens and tumor-associated antigens, which are processed by antigen presentation machinery to activate effector lymphocytes against them49. Tumor-specific antigens are defined as neoantigens present only on the surface of tumor cells but not on the surface of normal cells that mainly specifically induce the activation of T lymphocytes to produce CTLs and exert antitumor effects. Neoantigens can be generated by mutations of oncogenes or tumor suppressor genes, chromosomal translocations, and viral genes encoding new peptides. When tumors show a greater mutation load, T-cell differentiation may be better stimulated, and T-cell clonal expansion will produce a larger antitumor immune cell bank50. We can measure the value of TMB by the total number of nonsynonymous mutations in each coding region of the tumor genome. The nonsynonymous mutation number is more closely related to TMB than the total exon mutation burden51. For the treatment of NSCLC with ICIs, a higher TMB enables a faster response and better clinical efficacy52,53. In practice, however, the survival rate of patients with high TMB may be worse without ICI treatment52.
Patients with EGFR mutations show lower neoantigen burden and fewer nonsynonymous mutations54, and the latter are negatively correlated with the clonality of T-cell receptor β55. Patients with EGFR mutations have significantly lower TMB than those with WT EGFR, which may be related to the smoking history of EGFR-mutant NSCLC. The number of point mutations in lung cancer patients who smoke is 10 times that of never-smokers, which shows that smoking history is significantly associated with the increase in TMB56. A meta-analysis showed that the chance of having EGFR mutations in never-smokers is significantly higher, while the number of patients with EGFR mutations decreases as the smoking history increases57. Recently, the possibility that traditional chemotherapy can alter TMB has been explored. Studies on EGFR mutation sites have found that TMB may also differ between mutation sites, and tumors with the EGFR L858R mutation have been confirmed to have higher TMB and better response to ICIs58.
EGFR Mutations Cause Changes in the Antigen Presentation Machinery
Mitogen-activated protein kinase (MAPK) signaling inhibits the antigen presentation machinery, while the inhibition of MAPK signaling broadly upregulates it. Brea et al. activated the MAPK pathway by inducing EGFR mutations and found that in addition to inducing the upregulation of immune checkpoint blockade, it caused the inhibition of MHC-1 in vivo. EGFR mutations led to the downregulation of the expression of MHC class I molecules, resulting in weak antigen-presenting ability and low immunogenicity59.
The expression of MHC-I and MHC-II can be achieved through the interferon-γ (IFN-γ) signal transduction pathway and the downstream MEK/ERK signal transduction pathway60–63. Watanabe et al. found that the combination of an EGFR-TKI (irreversible EGFR-TKI afatinib or trametinib) and IFN-γ had an additive effect on HLA expression and the expression of antigen peptide transporter TAP1 and β2-microglobulin64. We can deduce that MHC molecules are expressed more highly when the EGFR pathway is inhibited, further confirming that EGFR mutations are negatively correlated with the expression of MHC molecules.
EGFR MUTATION AND PD-L1 EXPRESSION
Mechanism of PD-L1 Expression
PD-L1 is one of the ligands of T-cell immune checkpoint PD-1 that is widely expressed in hematopoietic and parenchymal cells. It participates in T-cell autoimmune tolerance and prevents itself from being attacked by the immune system under chronic inflammation or infection. In a variety of solid tumors, PD-L1 is overexpressed to protect tumor cells from being damaged by cytotoxic T cells, thereby forming an immunosuppressive TME and promoting tumor progression65,66. The expression mechanisms of PD-L1 in tumor cells can be divided into constitutive oncogene activation expression and cytokine-induced expression, and oncogene activation expression is constitutive and diffuse67. In a variety of tumors, the loss of phosphatase and tensin homolog can constitutively upregulate the expression of PD-L1 on the surface of tumor cells, and dysregulation of the Janus-activated kinase/signal transducer and activator of transcription (STAT) pathway can also lead to oncogene-driven PD-L1 overexpression. Coelho et al. found that KRAS activating mutations can enhance the stability of PD-L1 mRNA through the MEK-ERK signaling pathway68, and multiple different signaling pathways can participate in the regulation of PD-L1. The inflammatory status of the tumor TME plays an important role in the upregulation of PD-L1 expression in the process of cytokine-induced upregulation of PD-L1. In the inflammatory microenvironment, T cells mount a classical inflammatory response and secrete a variety of cytokines to induce PD-L1 expression on tumor cells. Cytokines including IL-1α, IL-6, TNF-α, and IFN-γ promote PD-L1 expression on tumor cells in a dose-dependent and additive manner. Among them, IFN-γ is the main stimulating factor of PD-L169.
Effect of EGFR Mutation on PD-L1 Expression
The EGFR signaling pathway is one of the most important oncogenic pathways in NSCLC70. The activation of EGFR signal transduction not only impacts tumor biology but also can regulate host antitumor immunity, including by driving PD-L1 expression and impeding TIL activation71. The expression level of PD-L1 in NSCLC cell lines with mutated EGFR was found to be significantly higher than that in cells with WT EGFR72. After the activity of EGFR was blocked by EGFR-TKIs, NSCLC cell lines with EGFR mutations downregulated their PD-L1 expression. The transfection of BEAS2B immortalized bronchial epithelial cells with mutated EGFR resulted in increased PD-L1 expression at the mRNA and protein levels. In mouse models, EGFR mutations activated PD-L1 expression and induced immune escape, whereas treatment with EGFR-TKIs downregulated PD-L1 expression73.
From these results, we can infer that the transduction of oncogenic EGFR signaling can directly or indirectly drive PD-L1 upregulation. The PI3K–Akt–STAT3/mTOR signaling pathway is involved in EGFR-mediated PD-L1 expression74. The activation of mTOR upregulates the expression of PD-L1 by inducing its translation rather than transcription. IFN-γ-mediated PD-L1 expression also depends on mTOR. Inhibition of Akt or STAT3 activity may downregulate PD-L1 expression even in gefitinib-resistant NSCLC75. There is also evidence that EGFR activation can upregulate PD-L1 through the ERK1/2 pathway76. Contrary to what was expected, patients with mEGFR have tended to have worse remission than those with WT EGFR during anti-PD-1/PD-L1 clinical treatment. The reason for the poor therapeutic effect may be that the upregulation of EGFR-mediated PD-L1 expression induced by the PI3K–Akt–STAT3/mTOR signaling pathway and the mEGFR-induced decrease in IFN-γ occur simultaneously, so it is difficult to estimate whether PD-L1 expression is increased in reality69,70.
This relationship is paradoxical in the clinical analysis of NSCLC patients with EGFR mutations. Tang et al. analyzed the tissues of 170 patients with lung adenocarcinoma by immunohistochemical assays, and the results showed that PD-L1 overexpression may be related to EGFR mutations77. However, two pooled analyses78,79 confirmed that PD-L1 expression was negatively correlated with EGFR mutation. The researchers evaluated the tissue sample data of 3,969 patients by analyzing the immunohistochemical assays of 18 studies and found that EGFR-mutant NSCLC was less likely to be PD-L1 positive than WT EGFR tumors [odds ratio (OR) = 0.59, 95% CI = 0.39–0.92; p < 0.02]80. Liu et al. found that EGFR-WT NSCLC tumors were more likely to be PD-L1 positive than EGFR-mutant tumors (OR = 1.79, 95% CI = 1.10–2.93; p = 0.02)81. In addition, they analyzed the mRNA and protein levels of PD-L1 in the Cancer Genome Atlas and internal database (Guangdong Lung Cancer Institute) and detected lower PD-L1 mRNA and PD-L1 protein expression in EGFR-mutant NSCLC samples than WT tumor samples. These opposing results may be related to the differences in how PD-L1 expression was measured (i.e., immunohistochemical analysis vs. mRNA expression). For now, it remains controversial how EGFR mutations influence PD-L1 expression.
EXPLORATION ON THE COMBINED APPLICATION OF ICIs AND EGFR-TKIs
Effects of EGFR-TKIs on the TME
TKIs can increase IFN secretion to enhance the induction of MHC-I and MHC-II molecules, promote Foxp3 degradation to attenuate the suppressive function of Tregs81, enhance antigen-specific antitumor T-cell responses, reduce T-cell apoptosis, and increase the cytotoxicity of CTLs that can enhance the immune system responses79. Therefore, the combined application of EGFR-TKIs may show some effect in anti-PD-1/PD-L1 treatment.
Effect of Treatment With EGFR-TKIs on PD-L1 Expression
The expression of PD-L1 may be dynamic and may be inhibited during EGFR-TKI treatment, but some patients show increased PD-L1 expression after displaying acquired resistance to EGFR-TKIs. Gainor et al. examined the levels of PD-L1 in paired tumor tissues that were taken either before EGFR-TKI treatment or after the development of resistance to EGFR-TKI, and the results showed that PD-L1 expression was significantly increased in 12 patients (21%)13. The researchers also found that the frequency of PD-L1 expression in patients with EGFR mutations was lower before TKI exposure (16%; PD-L1 ≥ 5%) than after acquired resistance to TKI had occurred (29%; PD-L1 ≥ 5%). Therefore, the authors concluded that the development of primary resistance to EGFR-TKIs in NSCLC patients with EGFR mutations seems to be related to the upregulation of PD-L1 expression on the tumor surface.
Combined Application of TKIs and Immunosuppressive Agents
Some clinical trials have tested the combinations of PD-1 or PD-L1 inhibitors with EGFR TKIs, targeting TKI-pretreated or untreated patients with EGFR mutations. In a phase I clinical trial, the investigators treated 20 NSCLC patients with EGFR mutations who had received TKI therapy with erlotinib in combination with nivolumab, and the results showed an objective response rate of 15% (3/20), but five patients experienced treatment-related grade 3 toxicity events in this study82. TATTON was a phase Ib trial that combined osimertinib (third-generation TKI) with selumetinib (MEK1/2 inhibitor), savolitinib (MET-TKI), or durvalumab (anti-PD-L1 monoclonal antibody) for the treatment of EGFR-mutant NSCLC. Because of the increased incidence of interstitial lung disease in the durvalumab group, this arm of the trial was terminated83.
CAURAL is a phase III randomized trial that was also terminated early due to safety concerns given the high incidence of interstitial lung disease reported in the TATTON trial. In a phase Ib trial, erlotinib was administered in combination with atezolizumab, and the initial results showed an objective response rate of 75% (95% CI = 50.9–91.3) and a median duration of response (DOR) of 16.7 months (range = 4.2–26.0). Although no grade ≥4 adverse events occurred, grade 3 treatment-related adverse events were reported in 43% of patients84. Indeed, toxicity is the main concern of the combination strategy. In the trial on gefitinib combined with durvalumab, grade 3 and grade 4 hypertransaminasemia occurred in 40% and 15% of patients, respectively, and 20% of patients had to discontinue treatment because of treatment-related adverse events85. Clinical trials combining TKIs and ICIs are still ongoing, and most of them still need to assess safety and tolerability. The reason behind the increased toxicity remains unclear, but current studies show that these combinations have no significant advantage in therapeutic efficacy, but they show more severe toxicity and side effects.
EGFR MUTATIONS AND TREATMENT WITH ICIs
We found that patients with EGFR mutations did not respond well to immunotherapy in the Checkmate 017, 057, Keynote 010, OAK, and POPLAR studies, which then raises questions as to whether there are differences between different mutation sites? It is known that EGFR mutations occur at several hotspots between exons 18 and 21. The in-frame deletion in exon 19 (EGFRΔ19) and the L858R point mutation in exon 21 were the most common mutations detected, accounting for 50% and 40% of patient samples, respectively86. Both types of mutations are sensitizing mutations, and tumors with these mutations are sensitive to EGFR TKIs. A special type of EGFR mutation, an in-frame insertion in exon 20, occurs in 3%–7% of NSCLCs, and most tumors with this type of mutation are resistant to treatment with EGFR TKIs87. Hastings et al. treated 126 patients with the most common EGFR gene mutations (EGFRΔ19 and EGFR L858R) with ICIs and compared them with 212 patients with WT EGFR88. The researchers found that patients with EGFRΔ19 had a lower objective response rate than those in the WT EGFR group (p = 0.002), whereas there was no difference between the WT EGFR group and the EGFR L858R group. In terms of OS benefit, there was no difference between WT EGFR and EGFR L858R, whereas shorter OS was found in the EGFRΔ19 group (p = 0.069 and p = 0.03, respectively). Haratani et al. assessed the response of the EGFR resistance mutation T790M to the treatment with ICIs89. The results suggested that treatment with ICIs may provide poorer survival outcomes in this subgroup of patients than in those with nonresistant mutations. The authors suggested that ICIs may achieve certain results in patients whose condition progressed after first-line TKI treatment before they developed the secondary T790M mutation. Yamada et al. retrospectively analyzed 27 patients with advanced NSCLC with EGFR mutations (rare or T790M) whose condition progressed after TKI treatment90. They found that the efficacy and best outcome of immunotherapy were correlated with having a rare EGFR mutation or not having the T790M mutation. This result suggested the possible use of ICIs, such as the later treatment for patients with rare EGFR mutations but not the T790M mutation whose condition progressed after TKI treatment. In addition, data from the ImmunoTarget registry presented at the American Society of Clinical Oncology (ASCO) 2018 meeting showed that NSCLC patients with the T790M mutation or EGFRΔ19 mutation who were treated with ICIs had worse survival than those having other types of mutations91.
In summary, further analysis of the different EGFR mutations is necessary for improved selection of patients with EGFR mutations who may be more responsive to ICIs. At present, it remains unclear as to the therapeutic efficacy of ICIs in NSCLC patients with EGFR mutations whose conditions have progressed after TKI treatment. The key question remains whether ICIs have a definite benefit in NSCLC patients with EGFR mutation. For EGFR-mutant NSCLC, factors leading to weak immunogenicity, such as TME not yet in an inflammatory state, lack of PD-L1+/CD8+ TILs, and low TMB92,93, will limit the antitumor immune response, even in a subgroup of patients with higher PD-L1 expression. Therefore, the clinical application of ICIs in patients with EGFR-mutant NSCLC still needs further study.
ANTIANGIOGENIC DRUGS MAY IMPROVE THE IMMUNE RESPONSE IN PATIENTS WITH EGFR MUTATIONS
Antiangiogenic drugs can directly or indirectly improve the immune microenvironment of tumors. In fact, in the process of tumor progression, the abnormal vascular proliferation around the tumor inhibits the body’s antitumor immunity roughly through the following three aspects: 1) the lack of pericyte coverage, the widening of the endothelial cell gap, and the breakage or loss of the basement membrane of the new blood vessels increase the leakage of blood vessels, resulting in increased interstitial fluid pressure, which hinders the infiltration of T cells; 2) the nascent vasculature often lacks some adhesion molecules, which further inhibits the response of immune cells; and 3) tumor blood vessels are morphologically characterized by tortuosity, distension, high disorder, and uneven thickness, which lead to blood flow disturbances and hypoxia94. The hypoxic environment can help to upregulate some signals that inhibit antitumor immune responses, such as PD-L1, IDO, IL-6, and IL-10, and the hypoxic TME can also promote the polarization of TAMs into an M2-like phenotype95. Therefore, antitumor angiogenic drugs can induce the normalization of tumor blood vessels and induce TAM differentiation into M1-like phenotype by alleviating hypoxia96. There is increasing evidence that appropriate administration of antiangiogenic drugs can induce changes in the state of the TME, that is, from an immunosuppressive state to an improved antitumor immunity state97. Anti-VEGF drugs can also block circulating VEGF-mediated blocking effects that hinder the maturation and differentiation of DCs98. The combined application of ICIs and antiangiogenic drugs has also been studied in clinical trials. NCT00790010 investigated the role of ipilimumab (anti-CTLA-4) and bevacizumab (anti-VEGF) in patients with metastatic melanoma, and the results showed that patients receiving the combined treatment had a better prognosis99. Wallin et al. treated 10 patients with previously untreated metastatic renal cell carcinoma with the combination of atezolizumab (anti-PD-L1) and bevacizumab, and eight of them showed a favorable response100. The Impower150 study is a multicenter, open-label, randomized, phase III study that evaluated the efficacy and safety of atezolizumab plus chemotherapy with or without bevacizumab versus bevacizumab in combination with chemotherapy in patients with nonsquamous NSCLC. The results of IMpower150 showed that immunotherapy combined with antiangiogenic agents and chemotherapy yielded significant benefits in both PFS and OS in first-line treatment of nonsquamous NSCLC. The study was divided into three groups, the treatment regimen of group A was atezolizumab + paclitaxel + carboplatin (ACP), the treatment regimen of group B was atezolizumab + bevacizumab + paclitaxel + carboplatin (ABCP), and the treatment regimen of group C was bevacizumab + paclitaxel + carboplatin (BCP)101. A subgroup analysis of patients with EGFR-sensitive mutations in the Impower150 trial showed that the ABCP regimen also provided significant OS benefits. Median OS was improved by 11.3 months, 29.4 versus 18.1 months, HR = 0.6 (95% Cl = 0.31, 1.14), in ABCP versus BCP. In addition, no OS benefit was observed in the ACP group compared with the BCP group. The incidence of treatment-related grade 3–4 adverse events was 21 (64%) of 33 patients in the ABCP group, 30 (68%) of 44 patients in the ACP group, and 28 (64%) of 44 patients in the BCP group. No patients in the ABCP and ACP groups experienced grade 5 adverse events. One patient in the BCP group experienced a grade 5 adverse event102. In the safety analysis of Impower150, when compared with the three-drug ACP and BCP regimens, the four-drug ABCP regimen has no additional toxicity and are relatively safe and tolerable. The findings of Impower150 provide a new direction and possibility for immunotherapy. It is certain that the normalization of tumor blood vessels has a great promoting effect on antitumor immunity, but whether the combination of ICIs and antiangiogenic drugs can become a new possibility for the treatment of EGFR-mutant NSCLC needs further study103. Please see Figure 1 for a graphical summary of this review.
Figure 1.
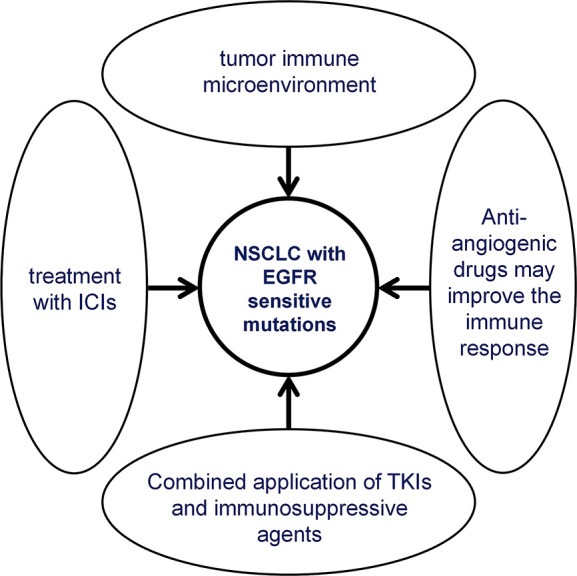
Graphical summary for the text.
OUTLOOK
There is increasing evidence that ICIs provide clinical benefit to cancer patients, and immunotherapy will play an increasingly important role in cancer therapy in the future. For EGFR-mutant NSCLC, it is important to determine whether patients can benefit from ICI treatment. Different types of EGFR mutations may exhibit different responses to ICIs, and it is necessary to explore the mechanism by which patients with EGFR mutations benefit from ICI treatment. Understanding how to improve the immunogenicity of EGFR-mutant NSCLC will provide much-needed evidence for the application of immunosuppressive agents. Therefore, many clinical trials and basic studies are still needed to explore the mechanism, potential influencing factors, and biomarkers of the response to ICIs. It is believed that future studies can clarify or improve the immunotherapy for EGFR-mutant NSCLC and can continue to extend the good prognosis of patients with EGFR-mutant NSCLC.
ACKNOWLEDGMENTS
This work was supported by the Scientific research fund project of Education Department of Liaoning Province (LJKZ0861) and the Dalian Medical Science Research Project (No. 2011012) and the Natural Science Foundation of Liaoning province (Nos. 20180550077 and 20180550937).
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1. Soerjomataram I, Jemal A, Bray F. 2021. Global Cancer Statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 71(3):209–249. [DOI] [PubMed] [Google Scholar]
- 2. Zheng RS, Sun KX, Zhang SW, Zeng HM, Zou XN, Chen R, Gu XY, Wei WW, He J. 2019. [Report of cancer epidemiology in China, 2015]. Zhonghua Zhong Liu Za Zhi. 41(1):19–28 [Chinese]. [DOI] [PubMed] [Google Scholar]
- 3. Zeng H, Chen W, Zheng R, Zhang S, Ji JS, Zou X, Xia C, Sun K, Yang Z, Li H, Wang N, Han R, Liu S, Li H, Mu H, He Y, Xu Y, Fu Z, Zhou Y, Jiang J, Yang Y, Chen J, Wei K, Fan D, Wang J, Fu F, Zhao D, Song G, Chen J, Jiang C, Zhou X, Gu X, Jin F, Li Q, Li Y, Wu T, Yan C, Dong J, Hua Z, Baade P, Bray F, Jemal A, Yu XQ, He J. 2018. Changing cancer survival in China during 2003–15: A pooled analysis of 17 population-based cancer registries. Lancet Glob Health 6(5):e555–e567. [DOI] [PubMed] [Google Scholar]
- 4. He J, Li N, Chen WQ, Wu N, Shen HB, Jiang Y, Li J, Wang F, Tian JH. 2021. Consulting Group of China Guideline for the Screening and Early Diagnosis and Treatment of Lung Cancer; Expert Group of China Guideline for the Screening and Early Diagnosis and Treatment of Lung Cancer; Working Group of China Guideline for the Screening and Early Diagnosis and Treatment of Lung Cancer. [China guideline for the screening and early detection of lung cancer (2021, Beijing)]. Zhonghua Zhong Liu Za Zhi 43(3):243–268. [DOI] [PubMed] [Google Scholar]
- 5. Pinto JA, Vallejos CS, Raez LE, Mas LA, Ruiz R, Torres-Roman JS, Morante Z, Araujo JM, Gómez HL, Aguilar A, Bretel D, Flores CJ, Rolfo C. 2018. Gender and outcomes in non-small cell lung cancer: An old prognostic variable comes back for targeted therapy and immunotherapy? ESMO Open 3(3):e000344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee CK, Man J, Lord S, Cooper W, Links M, Gebski V, Herbst RS, Gralla RJ, Mok T, Yang JC. 2018. Clinical and molecular characteristics associated with survival among patients treated with checkpoint inhibitors for advanced non-small cell lung carcinoma: A systematic review and meta-analysis. JAMA Oncol. 4(2):210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Peng W, Chen JQ, Liu C, Malu S, Creasy C, Tetzlaff MT, Xu C, McKenzie JA, Zhang C, Liang X, Williams LJ, Deng W, Chen G, Mbofung R, Lazar AJ, Torres-Cabala CA, Cooper ZA, Chen PL, Tieu TN, Spranger S, Yu X, Bernatchez C, Forget MA, Haymaker C, Amaria R, McQuade JL, Glitza IC, Cascone T, Li HS, Kwong LN, Heffernan TP, Hu J, Bassett RL Jr, Bosenberg MW, Woodman SE, Overwijk WW, Lizée G, Roszik J, Gajewski TF, Wargo JA, Gershenwald JE, Radvanyi L, Davies MA, Hwu P. 2016. Loss of PTEN promotes resistance to T cell-mediated immunotherapy. Cancer Discov. 6(2):202–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Azuma K, Ota K, Kawahara A, Hattori S, Iwama E, Harada T, Matsumoto K, Takayama K, Takamori S, Kage M, Hoshino T, Nakanishi Y, Okamoto I. 2014. Association of PD-L1 overexpression with activating EGFR mutations in surgically resected nonsmall-cell lung cancer. Ann Oncol. 25(10):1935–1940. [DOI] [PubMed] [Google Scholar]
- 9. Syn N, Wang L, Sethi G, Thiery JP, Goh BC. 2016. Exosome-mediated metastasis: From epithelial–mesenchymal transition to escape from immunosurveillance. Trends Pharmacol Sci. 37(7):606–617. [DOI] [PubMed] [Google Scholar]
- 10. Joyce JA, Pollard JW. 2009. Microenvironmental regulation of metastasis. Nat Rev Cancer 9(4):239–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Quail DF, Joyce JA. 2013. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 19(11):1423–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schreiber RD, Old LJ, Smyth MJ. 2011. Cancer immunoediting: Integrating immunity’s roles in cancer suppression and promotion. Science 331(6024):1565–1570. [DOI] [PubMed] [Google Scholar]
- 13. Gainor JF, Shaw AT, Sequist LV, Fu X, Azzoli CG, Piotrowska Z, Huynh TG, Zhao L, Fulton L, Schultz KR, Howe E, Farago AF, Sullivan RJ, Stone JR, Digumarthy S, Moran T, Hata AN, Yagi Y, Yeap BY, Engelman JA, Mino-Kenudson M. 2016. EGFR mutations and ALK rearrangements are associated with low response rates to PD-1 pathway blockade in non-small cell lung cancer: A retrospective analysis. Clin Cancer Res. 22(18):4585–4593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dong ZY, Zhang JT, Liu SY, Su J, Zhang C, Xie Z, Zhou Q, Tu HY, Xu CR, Yan LX, Li YF, Zhong WZ, Wu YL. 2017. EGFR mutation correlates with uninflamed phenotype and weak immunogenicity, causing impaired response to PD-1 blockade in non-small cell lung cancer. Oncoimmunology 6(11):e1356145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mazzaschi G, Madeddu D, Falco A, Bocchialini G, Goldoni M, Sogni F, Armani G, Lagrasta CA, Lorusso B, Mangiaracina C, Vilella R, Frati C, Alfieri R, Ampollini L, Veneziani M, Silini EM, Ardizzoni A, Urbanek K, Aversa F, Quaini F, Tiseo M. 2018. Low PD-1 expression in cytotoxic CD8+ tumor-infiltrating lymphocytes confers an immune-privileged tissue microenvironment in NSCLC with a prognostic and predictive value. Clin Cancer Res. 24(2):407–419. [DOI] [PubMed] [Google Scholar]
- 16. Mascia F, Schloemann DT, Cataisson C, McKinnon KM, Krymskaya L, Wolcott KM, Yuspa SH. 2016. Cell autonomous or systemic EGFR blockade alters the immune-environment in squamous cell carcinomas. Int J Cancer 139(11):2593–2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Huang SH, Li Y, Zhang J, Rong J, Ye S. 2013. Epidermal growth factor receptor-containing exosomes induce tumor-specific regulatory T cells. Cancer Invest. 31(5):330–335. [DOI] [PubMed] [Google Scholar]
- 18. Jia Y, Li X, Jiang T, Zhao S, Zhao C, Zhang L, Liu X, Shi J, Qiao M, Luo J, Liu S, Han R, Su C, Ren S, Zhou C. 2019. EGFR-targeted therapy alters the tumor microenvironment in EGFR-driven lung tumors: Implications for combination therapies. Int J Cancer 145(5):1432–1444. [DOI] [PubMed] [Google Scholar]
- 19. Zhang B, Zhang Y, Zhao J, Wang Z, Wu T, Ou W, Wang J, Yang B, Zhao Y, Rao Z, Gao J. 2014. M2-polarized macrophages contribute to the decreased sensitivity of EGFR-TKIs treatment in patients with advanced lung adenocarcinoma. Med Oncol. 31(8):127. [DOI] [PubMed] [Google Scholar]
- 20. Berraondo P, Sanmamed MF, Ochoa MC, Etxeberria I, Aznar MA, Pérez-Gracia JL, Rodríguez-Ruiz ME, Ponz-Sarvise M, Castañón E, Melero I. 2019. Cytokines in clinical cancer immunotherapy. Br J Cancer 120(1):6–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tosolini M, Kirilovsky A, Mlecnik B, Fredriksen T, Mauger S, Bindea G, Berger A, Bruneval P, Fridman WH, Pagès F, Galon J. 2011. Clinical impact of different classes of infiltrating T cytotoxic and helper cells (Th1, th2, treg, th17) in patients with colorectal cancer. Cancer Res. 71(4):1263–1271. [DOI] [PubMed] [Google Scholar]
- 22. Fontenot JD, Gavin MA, Rudensky AY. 2003. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol. 4(4):330–336. [DOI] [PubMed] [Google Scholar]
- 23. Frydrychowicz M, Boruczkowski M, Kolecka-Bednarczyk A, Dworacki G. 2017. The dual role of Treg in cancer. Scand J Immunol. 86(6):436–443. [DOI] [PubMed] [Google Scholar]
- 24. Chin AR, Wang SE. 2016. Cancer-derived extracellular vesicles: The ‘soil conditioner’ in breast cancer metastasis? Cancer Metastasis Rev. 35(4):669–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Whiteside TL. 2016. Tumor-derived exosomes and their role in tumor-induced immune suppression. Vaccines (Basel) 4(4):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fallarino F, Grohmann U, Puccetti P. 2012. Indoleamine 2,3-dioxygenase: From catalyst to signaling function. Eur J Immunol. 42(8):1932–1937. [DOI] [PubMed] [Google Scholar]
- 27. Ino K. 2011. Indoleamine 2,3-dioxygenase and immune tolerance in ovarian cancer. Curr Opin Obstet Gynecol. 23(1):13–18. [DOI] [PubMed] [Google Scholar]
- 28. Huang SH, Li Y, Zhang J, Rong J, Ye S. 2013. Epidermal growth factor receptor-containing exosomes induce tumor-specific regulatory T cells. Cancer Invest. 31(5):330–335. [DOI] [PubMed] [Google Scholar]
- 29. Chang MH, Ahn HK, Lee J, Jung CK, Choi YL, Park YH, Ahn JS, Park K, Ahn MJ. 2011. Clinical impact of amphiregulin expression in patients with epidermal growth factor receptor (EGFR) wild-type nonsmall cell lung cancer treated with EGFR-tyrosine kinase inhibitors. Cancer 117(1):143–151. [DOI] [PubMed] [Google Scholar]
- 30. Higginbotham JN, Demory Beckler M, Gephart JD, Franklin JL, Bogatcheva G, Kremers GJ, Piston DW, Ayers GD, McConnell RE, Tyska MJ, Coffey RJ. 2011. Amphiregulin exosomes increase cancer cell invasion. Curr Biol. 21(9):779–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wang S, Zhang Y, Wang Y, Ye P, Li J, Li H, Ding Q, Xia J. 2016. Amphiregulin confers regulatory T cell suppressive function and tumor invasion via the EGFR/GSK-3β/Foxp3 axis. J Biol Chem. 291(40):21085–21095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yi T, Lee HL, Cha JH, Ko SI, Kim HJ, Shin HI, Woo KM, Ryoo HM, Kim GS, Baek JH. 2008. Epidermal growth factor receptor regulates osteoclast differentiation and survival through cross-talking with RANK signaling. J Cell Physiol. 217(2):409–422. [DOI] [PubMed] [Google Scholar]
- 33. Mascia F, Schloemann DT, Cataisson C, McKinnon KM, Krymskaya L, Wolcott KM, Yuspa SH. 2016. Cell autonomous or systemic EGFR blockade alters the immune-environment in squamous cell carcinomas. Int J Cancer 139(11):2593–2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, Van den Eynden G, Baehner FL, Penault-Llorca F, Perez EA, Thompson EA, Symmans WF, Richardson AL, Brock J, Criscitiello C, Bailey H, Ignatiadis M, Floris G, Sparano J, Kos Z, Nielsen T, Rimm DL, Allison KH, Reis-Filho JS, Loibl S, Sotiriou C, Viale G, Badve S, Adams S, Willard-Gallo K, Loi S. 2015. International TILs Working Group 2014. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: Recommendations by an International TILs Working Group 2014. Ann Oncol. 26(2):259–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kamphorst AO, Wieland A, Nasti T, Yang S, Zhang R, Barber DL, Konieczny BT, Daugherty CZ, Koenig L, Yu K, Sica GL, Sharpe AH, Freeman GJ, Blazar BR, Turka LA, Owonikoko TK, Pillai RN, Ramalingam SS, Araki K, Ahmed R. 2017. Rescue of exhausted CD8 T cells by PD-1-targeted therapies is CD28-dependent. Science 355(6332):1423–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Iglesia MD, Parker JS, Hoadley KA, Serody JS, Perou CM, Vincent BG. 2016. Genomic analysis of immune cell infiltrates across 11 tumor types. J Natl Cancer Inst. 108(11):djw144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Brambilla E, Le Teuff G, Marguet S, Lantuejoul S, Dunant A, Graziano S, Pirker R, Douillard JY, Le Chevalier T, Filipits M, Rosell R, Kratzke R, Popper H, Soria JC, Shepherd FA, Seymour L, Tsao MS. 2016. Prognostic effect of tumor lymphocytic infiltration in resectable non-small-cell lung cancer. J Clin Oncol. 34(11):1223–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Simoni Y, Becht E, Fehlings M, Loh CY, Koo SL, Teng KWW, Yeong JPS, Nahar R, Zhang T, Kared H, Duan K, Ang N, Poidinger M, Lee YY, Larbi A, Khng AJ, Tan E, Fu C, Mathew R, Teo M, Lim WT, Toh CK, Ong BH, Koh T, Hillmer AM, Takano A, Lim TKH, Tan EH, Zhai W, Tan DSW, Tan IB, Newell EW. 2018. Bystander CD8+ T cells are abundant and phenotypically distinct in human tumour infiltrates. Nature 557(7706):575–579. [DOI] [PubMed] [Google Scholar]
- 39. Teng MW, Ngiow SF, Ribas A, Smyth MJ. 2015. Classifying cancers based on T-cell Infiltration and PD-L1. Cancer Res. 75(11):2139–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Haratani K, Hayashi H, Tanaka T, Kaneda H, Togashi Y, Sakai K, Hayashi K, Tomida S, Chiba Y, Yonesaka K, Nonagase Y, Takahama T, Tanizaki J, Tanaka K, Yoshida T, Tanimura K, Takeda M, Yoshioka H, Ishida T, Mitsudomi T, Nishio K, Nakagawa K. 2017. Tumor immune microenvironment and nivolumab efficacy in EGFR mutation-positive non-small-cell lung cancer based on T790M status after disease progression during EGFR-TKI treatment. Ann Oncol. 28(7):1532–1539. [DOI] [PubMed] [Google Scholar]
- 41. Pollack BP, Sapkota B, Cartee TV. 2011. Epidermal growth factor receptor inhibition augments the expression of MHC class I and II genes. Clin Cancer Res. 17(13):4400–4413. [DOI] [PubMed] [Google Scholar]
- 42. Chen X, Gao A, Zhang F, Yang Z, Wang S, Fang Y, Li J, Wang J, Shi W, Wang L, Zheng Y, Sun Y. 2021. ILT4 inhibition prevents TAM- and dysfunctional T cell-mediated immunosuppression and enhances the efficacy of anti-PD-L1 therapy in NSCLC with EGFR activation. Theranostics. 11(7):3392–3416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wang DH, Lee HS, Yoon D, Berry G, Wheeler TM, Sugarbaker DJ, Kheradmand F, Engleman E, Burt BM. 2017. Progression of EGFR-mutant lung adenocarcinoma is driven by alveolar macrophages. Clin Cancer Res. 23(3):778–788. [DOI] [PubMed] [Google Scholar]
- 44. Passarelli A, Aieta M, Sgambato A, Gridelli C. 2020. Targeting immunometabolism mediated by CD73 pathway in EGFR-mutated non-small cell lung cancer: A new hope for overcoming immune resistance. Front Immunol. 11:1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Holmgaard RB, Zamarin D, Li Y, Gasmi B, Munn DH, Allison JP, Merghoub T, Wolchok JD. 2015. Tumor-expressed IDO recruits and activates MDSCs in a Treg-dependent manner. Cell Rep. 13(2):412–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Huang A, Zhang B, Wang B, Zhang F, Fan KX, Guo YJ. 2013. Increased CD14(+)HLA-DR (−/low) myeloid-derived suppressor cells correlate with extrathoracic metastasis and poor response to chemotherapy in non-small cell lung cancer patients. Cancer Immunol Immunother. 62(9):1439–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Veglia F, Perego M, Gabrilovich D. 2018. Myeloid-derived suppressor cells coming of age. Nat Immunol. 19(2):108–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yarchoan M, Hopkins A, Jaffee EM. 2017. Tumor mutational burden and response rate to PD-1 inhibition. N Engl J Med. 377(25):2500–2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. McGranahan N, Furness AJ, Rosenthal R, Ramskov S, Lyngaa R, Saini SK, Jamal-Hanjani M, Wilson GA, Birkbak NJ, Hiley CT, Watkins TB, Shafi S, Murugaesu N, Mitter R, Akarca AU, Linares J, Marafioti T, Henry JY, Van Allen EM, Miao D, Schilling B, Schadendorf D, Garraway LA, Makarov V, Rizvi NA, Snyder A, Hellmann MD, Merghoub T, Wolchok JD, Shukla SA, Wu CJ, Peggs KS, Chan TA, Hadrup SR, Quezada SA, Swanton C. 2016. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science 351(6280):1463–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Topalian SL, Taube JM, Anders RA, Pardoll DM. 2016. Mechanism-driven biomarkers to guide immune checkpoint blockade in cancer therapy. Nat Rev Cancer 16(5):275–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, Lee W, Yuan J, Wong P, Ho TS, Miller ML, Rekhtman N, Moreira AL, Ibrahim F, Bruggeman C, Gasmi B, Zappasodi R, Maeda Y, Sander C, Garon EB, Merghoub T, Wolchok JD, Schumacher TN, Chan TA. 2015. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 348(6230):124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rizvi H, Sanchez-Vega F, La K, Chatila W, Jonsson P, Halpenny D, Plodkowski A, Long N, Sauter JL, Rekhtman N, Hollmann T, Schalper KA, Gainor JF, Shen R, Ni A, Arbour KC, Merghoub T, Wolchok J, Snyder A, Chaft JE, Kris MG, Rudin CM, Socci ND, Berger MF, Taylor BS, Zehir A, Solit DB, Arcila ME, Ladanyi M, Riely GJ, Schultz N, Hellmann MD. 2018. Molecular determinants of response to anti-programmed cell death (PD)-1 and anti-programmed death-ligand 1 (PD-L1) blockade in patients with non-small-cell lung cancer profiled with targeted next-generation sequencing. J Clin Oncol. 36(7):633–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Carbone DP, Reck M, Paz-Ares L, Creelan B, Horn L, Steins M, Felip E, van den Heuvel MM, Ciuleanu TE, Badin F, Ready N, Hiltermann TJN, Nair S, Juergens R, Peters S, Minenza E, Wrangle JM, Rodriguez-Abreu D, Borghaei H, Blumenschein GR Jr, Villaruz LC, Havel L, Krejci J, Corral Jaime J, Chang H, Geese WJ, Bhagavatheeswaran P, Chen AC, Socinski MA. 2017. CheckMate 026 Investigators. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer. N Engl J Med. 376(25):2415–2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Cheng ML, Oxnard GR. 2019. Does TMB impact the effectiveness of TKIs in EGFR-mutant NSCLC? Clin Cancer Res. 25(3):899–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Miyauchi E, Matsuda T, Kiyotani K, Low SK, Hsu YW, Tsukita Y, Ichinose M, Sakurada A, Okada Y, Saito R, Nakamura Y. 2019. Significant differences in T cell receptor repertoires in lung adenocarcinomas with and without epidermal growth factor receptor mutations. Cancer Sci. 110(3):867–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lim SM, Choi JW, Hong MH, Jung D, Lee CY, Park SY, Shim HS, Sheen S, Kwak KI, Kang DR, Cho BC, Kim HR. 2019. Indoor radon exposure increases tumor mutation burden in never-smoker patients with lung adenocarcinoma. Lung Cancer. 131:139–146. [DOI] [PubMed] [Google Scholar]
- 57. Chapman AM, Sun KY, Ruestow P, Cowan DM, Madl AK. 2016. Lung cancer mutation profile of EGFR, ALK, and KRAS: Meta-analysis and comparison of never and ever smokers. Lung Cancer 102:122–134. [DOI] [PubMed] [Google Scholar]
- 58. Hastings K, Yu HA, Wei W, Sanchez-Vega F, DeVeaux M, Choi J, Rizvi H, Lisberg A, Truini A, Lydon CA, Liu Z, Henick BS, Wurtz A, Cai G, Plodkowski AJ, Long NM, Halpenny DF, Killam J, Oliva I, Schultz N, Riely GJ, Arcila ME, Ladanyi M, Zelterman D, Herbst RS, Goldberg SB, Awad MM, Garon EB, Gettinger S, Hellmann MD, Politi K. 2019. EGFR mutation subtypes and response to immune checkpoint blockade treatment in non-small-cell lung cancer. Ann Oncol. 30(8):1311–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Brea EJ, Oh CY, Manchado E, Budhu S, Gejman RS, Mo G, Mondello P, Han JE, Jarvis CA, Ulmert D, Xiang Q, Chang AY, Garippa RJ, Merghoub T, Wolchok JD, Rosen N, Lowe SW, Scheinberg DA. 2016. Kinase regulation of human MHC class I molecule expression on cancer cells. Cancer Immunol Res. 4(11):936–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Im JS, Herrmann AC, Bernatchez C, Haymaker C, Molldrem JJ, Hong WK, Perez-Soler R. 2016. Immune-modulation by epidermal growth factor receptor inhibitors: Implication on anti-tumor immunity in lung cancer. PLoS One 11(7):e0160004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kumai T, Matsuda Y, Oikawa K, Aoki N, Kimura S, Harabuchi Y, Celis E, Kobayashi H. 2013. EGFR inhibitors augment antitumour helper T-cell responses of HER family-specific immunotherapy. Br J Cancer 109(8):2155–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Venugopalan A, Lee MJ, Niu G, Medina-Echeverz J, Tomita Y, Lizak MJ, Cultraro CM, Simpson RM, Chen X, Trepel JB, Guha U. 2016. EGFR-targeted therapy results in dramatic early lung tumor regression accompanied by imaging response and immune infiltration in EGFR mutant transgenic mouse models. Oncotarget 7(34):54137–54156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Garrido G, Rabasa A, Garrido C, López A, Chao L, García-Lora AM, Garrido F, Fernández LE, Sánchez B. 2014. Preclinical modeling of EGFR-specific antibody resistance: Oncogenic and immune-associated escape mechanisms. Oncogene 33(24):3129–3139. [DOI] [PubMed] [Google Scholar]
- 64. Watanabe S, Hayashi H, Haratani K, Shimizu S, Tanizaki J, Sakai K, Kawakami H, Yonesaka K, Tsurutani J, Togashi Y, Nishio K, Ito A, Nakagawa K. 2019. Mutational activation of the epidermal growth factor receptor down-regulates major histocompatibility complex class I expression via the extracellular signal-regulated kinase in non-small cell lung cancer. Cancer Sci. 110(1):52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Taube JM, Klein A, Brahmer JR, Xu H, Pan X, Kim JH, Chen L, Pardoll DM, Topalian SL, Anders RA. 2014. Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy. Clin Cancer Res. 20(19):5064–5074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Parsa AT, Waldron JS, Panner A, Crane CA, Parney IF, Barry JJ, Cachola KE, Murray JC, Tihan T, Jensen MC, Mischel PS, Stokoe D, Pieper RO. 2007. Loss of tumor suppressor PTEN function increases B7-H1 expression and immunoresistance in glioma. Nat Med. 13(1):84–88. [DOI] [PubMed] [Google Scholar]
- 67. Patel SP, Kurzrock R. 2015. PD-L1 Expression as a predictive biomarker in cancer immunotherapy. Mol Cancer Ther. 14(4):847–856. [DOI] [PubMed] [Google Scholar]
- 68. Coelho MA, de Carné Trécesson S, Rana S, Zecchin D, Moore C, Molina-Arcas M, East P, Spencer-Dene B, Nye E, Barnouin K, Snijders AP, Lai WS, Blackshear PJ, Downward J. 2017. Oncogenic RAS signaling promotes tumor immunoresistance by stabilizing PD-L1 mRNA. Immunity. 47(6): 1083–1099.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Lu W, Lu L, Feng Y, Chen J, Li Y, Kong X, Chen S, Li X, Chen Q, Zhang P. 2013. Inflammation promotes oral squamous carcinoma immune evasion via induced programmed death ligand-1 surface expression. Oncol Lett. 5(5):1519–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Tebbutt N, Pedersen MW, Johns TG. 2013. Targeting the ERBB family in cancer: Couples therapy. Nat Rev Cancer 13(9):663–673. [DOI] [PubMed] [Google Scholar]
- 71. Li X, Lian Z, Wang S, Xing L, Yu J. 2018. Interactions between EGFR and PD-1/PD-L1 pathway: Implications for treatment of NSCLC. Cancer Lett. 418:1–9. [DOI] [PubMed] [Google Scholar]
- 72. Azuma K, Ota K, Kawahara A, Hattori S, Iwama E, Harada T, Matsumoto K, Takayama K, Takamori S, Kage M, Hoshino T, Nakanishi Y, Okamoto I. 2014. Association of PD-L1 overexpression with activating EGFR mutations in surgically resected nonsmall-cell lung cancer. Ann Oncol. 25(10):1935–1940. [DOI] [PubMed] [Google Scholar]
- 73. Akbay EA, Koyama S, Carretero J, Altabef A, Tchaicha JH, Christensen CL, Mikse OR, Cherniack AD, Beauchamp EM, Pugh TJ, Wilkerson MD, Fecci PE, Butaney M, Reibel JB, Soucheray M, Cohoon TJ, Janne PA, Meyerson M, Hayes DN, Shapiro GI, Shimamura T, Sholl LM, Rodig SJ, Freeman GJ, Hammerman PS, Dranoff G, Wong KK. 2013. Activation of the PD-1 pathway contributes to immune escape in EGFR-driven lung tumors. Cancer Discov. 3(12):1355–1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Chen N, Fang W, Zhan J, Hong S, Tang Y, Kang S, Zhang Y, He X, Zhou T, Qin T, Huang Y, Yi X, Zhang L. 2015. Upregulation of PD-L1 by EGFR activation mediates the immune escape in EGFR-driven NSCLC: Implication for optional immune targeted therapy for NSCLC patients with EGFR mutation. J Thorac Oncol. 10(6):910–923. [DOI] [PubMed] [Google Scholar]
- 75. Abdelhamed S, Ogura K, Yokoyama S, Saiki I, Hayakawa Y. 2016. AKT-STAT3 pathway as a downstream target of EGFR signaling to regulate PD-L1 expression on NSCLC cells. J Cancer 7(12):1579–1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Dominguez C, Tsang KY, Palena C. 2016. Short-term EGFR blockade enhances immune-mediated cytotoxicity of EGFR mutant lung cancer cells: Rationale for combination therapies. Cell Death Dis. 7(9):e2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Tang Y, Fang W, Zhang Y, Hong S, Kang S, Yan Y, Chen N, Zhan J, He X, Qin T, Li G, Tang W, Peng P, Zhang L. 2015. The association between PD-L1 and EGFR status and the prognostic value of PD-L1 in advanced non-small cell lung cancer patients treated with EGFR-TKIs. Oncotarget 6(16):14209–14219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Kumai T, Matsuda Y, Oikawa K, Aoki N, Kimura S, Harabuchi Y, Celis E, Kobayashi H. 2013. EGFR inhibitors augment antitumour helper T-cell responses of HER family-specific immunotherapy. Br J Cancer 109(8):2155–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Garrido G, Rabasa A, Garrido C, López A, Chao L, García-Lora AM, Garrido F, Fernández LE, Sánchez B. 2014. Preclinical modeling of EGFR-specific antibody resistance: Oncogenic and immune-associated escape mechanisms. Oncogene 33(24): 3129–3139. [DOI] [PubMed] [Google Scholar]
- 80. D’Incecco A, Andreozzi M, Ludovini V, Rossi E, Capodanno A, Landi L, Tibaldi C, Minuti G, Salvini J, Coppi E, Chella A, Fontanini G, Filice ME, Tornillo L, Incensati RM, Sani S, Crinò L, Terracciano L, Cappuzzo F. 2015. PD-1 and PD-L1 expression in molecularly selected non-small-cell lung cancer patients. Br J Cancer 112(1):95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Liu SY, Dong ZY, Wu SP, Xie Z, Yan LX, Li YF, Yan HH, Su J, Yang JJ, Zhou Q, Zhong WZ, Tu HY, Yang XN, Zhang XC, Wu YL. 2018. Clinical relevance of PD-L1 expression and CD8+ T cells infiltration in patients with EGFR-mutated and ALK-rearranged lung cancer. Lung Cancer 125:86–92. [DOI] [PubMed] [Google Scholar]
- 82. Gettinger S, Hellmann MD, Chow LQM, Borghaei H, Antonia S, Brahmer JR, Goldman JW, Gerber DE, Juergens RA, Shepherd FA, Laurie SA, Young TC, Li X, Geese WJ, Rizvi N. 2018. Nivolumab plus erlotinib in patients with EGFR-mutant advanced NSCLC. J Thorac Oncol. 13(9):1363–1372. [DOI] [PubMed] [Google Scholar]
- 83. Oxnard GR, Yang JC, Yu H, Kim SW, Saka H, Horn L, Goto K, Ohe Y, Mann H, Thress KS, Frigault MM, Vishwanathan K, Ghiorghiu D, Ramalingam SS, Ahn MJ. 2020. TATTON: A multi-arm, phase Ib trial of osimertinib combined with selumetinib, savolitinib, or durvalumab in EGFR-mutant lung cancer. Ann Oncol. 31(4):507–516. [DOI] [PubMed] [Google Scholar]
- 84. Créquit P, Chaimani A, Yavchitz A, Attiche N, Cadranel J, Trinquart L, Ravaud P. 2017. Comparative efficacy and safety of second-line treatments for advanced non-small cell lung cancer with wild-type or unknown status for epidermal growth factor receptor: A systematic review and network meta-analysis. BMC Med. 15(1):193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Creelan BC, Yeh TC, Kim SW, Nogami N, Kim DW, Chow LQM, Kanda S, Taylor R, Tang W, Tang M, Angell HK, Roudier MP, Marotti M, Gibbons DL. 2021. A phase 1 study of gefitinib combined with durvalumab in EGFR TKI-naive patients with EGFR mutation-positive locally advanced/metastatic non-small-cell lung cancer. Br J Cancer 124(2):383–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Shigematsu H, Lin L, Takahashi T, Nomura M, Suzuki M, Wistuba II, Fong KM, Lee H, Toyooka S, Shimizu N, Fujisawa T, Feng Z, Roth JA, Herz J, Minna JD, Gazdar AF. 2005. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst. 97(5):339–346. [DOI] [PubMed] [Google Scholar]
- 87. Wu JY, Wu SG, Yang CH, Gow CH, Chang YL, Yu CJ, Shih JY, Yang PC. 2008. Lung cancer with epidermal growth factor receptor exon 20 mutations is associated with poor gefitinib treatment response. Clin Cancer Res. 14(15):4877–4882. [DOI] [PubMed] [Google Scholar]
- 88. Hastings K, Yu HA, Wei W, Sanchez-Vega F, DeVeaux M, Choi J, Rizvi H, Lisberg A, Truini A, Lydon CA, Liu Z, Henick BS, Wurtz A, Cai G, Plodkowski AJ, Long NM, Halpenny DF, Killam J, Oliva I, Schultz N, Riely GJ, Arcila ME, Ladanyi M, Zelterman D, Herbst RS, Goldberg SB, Awad MM, Garon EB, Gettinger S, Hellmann MD, Politi K. 2019. EGFR mutation subtypes and response to immune checkpoint blockade treatment in non-small-cell lung cancer. Ann Oncol. 30(8):1311–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Haratani K, Hayashi H, Tanaka T, Kaneda H, Togashi Y, Sakai K, Hayashi K, Tomida S, Chiba Y, Yonesaka K, Nonagase Y, Takahama T, Tanizaki J, Tanaka K, Yoshida T, Tanimura K, Takeda M, Yoshioka H, Ishida T, Mitsudomi T, Nishio K, Nakagawa K. 2017. Tumor immune microenvironment and nivolumab efficacy in EGFR mutation-positive non-small-cell lung cancer based on T790M status after disease progression during EGFR-TKI treatment. Ann Oncol. 28(7):1532–1539. [DOI] [PubMed] [Google Scholar]
- 90. Yamada T, Hirai S, Katayama Y, Yoshimura A, Shiotsu S, Watanabe S, Kikuchi T, Hirose K, Kubota Y, Chihara Y, Harada T, Tanimura K, Takeda T, Tamiya N, Kaneko Y, Uchino J, Takayama K. 2019. Retrospective efficacy analysis of immune checkpoint inhibitors in patients with EGFR-mutated non-small cell lung cancer. Cancer Med. 8(4):1521–1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Mazieres J, Drilon A, Lusque A, Mhanna L, Cortot AB, Mezquita L, Thai AA, Mascaux C, Couraud S, Veillon R, Van den Heuvel M, Neal J, Peled N, Früh M, Ng TL, Gounant V, Popat S, Diebold J, Sabari J, Zhu VW, Rothschild SI, Bironzo P, Martinez-Marti A, Curioni-Fontecedro A, Rosell R, Lattuca-Truc M, Wiesweg M, Besse B, Solomon B, Barlesi F, Schouten RD, Wakelee H, Camidge DR, Zalcman G, Novello S, Ou SI, Milia J, Gautschi O. 2019. Immune checkpoint inhibitors for patients with advanced lung cancer and oncogenic driver alterations: Results from the IMMUNOTARGET registry. Ann Oncol. 30(8):1321–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, Gadgeel SM, Hida T, Kowalski DM, Dols MC, Cortinovis DL, Leach J, Polikoff J, Barrios C, Kabbinavar F, Frontera OA, De Marinis F, Turna H, Lee JS, Ballinger M, Kowanetz M, He P, Chen DS, Sandler A, Gandara DR. 2017. OAK Study Group. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): A phase 3, open-label, multicentre randomised controlled trial. Lancet 389(10066):255–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Gebhardt C, Sevko A, Jiang H, Lichtenberger R, Reith M, Tarnanidis K, Holland-Letz T, Umansky L, Beckhove P, Sucker A, Schadendorf D, Utikal J, Umansky V. 2015. Myeloid cells and related chronic inflammatory factors as novel predictive markers in melanoma treatment with ipilimumab. Clin Cancer Res. 21(24):5453–5459. [DOI] [PubMed] [Google Scholar]
- 94. Fukumura D, Kloepper J, Amoozgar Z, Duda DG, Jain RK. 2018. Enhancing cancer immunotherapy using antiangiogenics: Opportunities and challenges. Nat Rev Clin Oncol. 15(5):325–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Movahedi K, Laoui D, Gysemans C, Baeten M, Stangé G, Van den Bossche J, Mack M, Pipeleers D, In’t Veld P, De Baetselier P, Van Ginderachter JA. 2010. Different tumor microenvironments contain functionally distinct subsets of macrophages derived from Ly6C(high) monocytes. Cancer Res. 70(14):5728–5739. [DOI] [PubMed] [Google Scholar]
- 96. Huang Y, Yuan J, Righi E, Kamoun WS, Ancukiewicz M, Nezivar J, Santosuosso M, Martin JD, Martin MR, Vianello F, Leblanc P, Munn LL, Huang P, Duda DG, Fukumura D, Jain RK, Poznansky MC. 2012. Vascular normalizing doses of antiangiogenic treatment reprogram the immunosuppressive tumor microenvironment and enhance immunotherapy. Proc Natl Acad Sci USA 109(43):17561–17566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Wang Q, Gao J, Di W, Wu X. 2020. Anti-angiogenesis therapy overcomes the innate resistance to PD-1/PD-L1 blockade in VEGFA-overexpressed mouse tumor models. Cancer Immunol Immunother. 69(9):1781–1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Jain RK, Martin JD, Stylianopoulos T. 2014. The role of mechanical forces in tumor growth and therapy. Annu Rev Biomed Eng. 16:321–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Huang H, Langenkamp E, Georganaki M, Loskog A, Fuchs PF, Dieterich LC, Kreuger J, Dimberg A. 2015. VEGF suppresses T-lymphocyte infiltration in the tumor microenvironment through inhibition of NF-κB-induced endothelial activation. FASEB J. 29(1):227–238. [DOI] [PubMed] [Google Scholar]
- 100. Wallin JJ, Bendell JC, Funke R, Sznol M, Korski K, Jones S, Hernandez G, Mier J, He X, Hodi FS, Denker M, Leveque V, Cañamero M, Babitski G, Koeppen H, Ziai J, Sharma N, Gaire F, Chen DS, Waterkamp D, Hegde PS, McDermott DF. 2016. Atezolizumab in combination with bevacizumab enhances antigen-specific T-cell migration in metastatic renal cell carcinoma. Nat Commun. 7:12624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, Rodríguez-Abreu D, Moro-Sibilot D, Thomas CA, Barlesi F, Finley G, Kelsch C, Lee A, Coleman S, Deng Y, Shen Y, Kowanetz M, Lopez-Chavez A, Sandler A, Reck M. 2018. IMpower150 Study Group. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 378(24):2288–2301. [DOI] [PubMed] [Google Scholar]
- 102. Socinski MA, Nishio M, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, Rodríguez-Abreu D, Moro-Sibilot D, Thomas CA, Barlesi F, Finley G, Kong S, Lee A, Coleman S, Zou W, McCleland M, Shankar G, Reck M. 2021. IMpower150 final overall survival analyses for atezolizumab plus bevacizumab and chemotherapy in first-line metastatic nonsquamous NSCLC. J Thorac Oncol. 16(11):1909–1924. [DOI] [PubMed] [Google Scholar]
- 103. Reck M, Wehler T, Orlandi F, Nogami N, Barone C, Moro-Sibilot D, Shtivelband M, González Larriba JL, Rothenstein J, Früh M, Yu W, Deng Y, Coleman S, Shankar G, Patel H, Kelsch C, Lee A, Piault E, Socinski MA. 2020. Safety and patient-reported outcomes of atezolizumab plus chemotherapy with or without bevacizumab versus bevacizumab plus chemotherapy in non-small-cell lung cancer. J Clin Oncol. 38(22):2530–2542. [DOI] [PMC free article] [PubMed] [Google Scholar]


