Abstract
Backgroud and Aims
Hypertension (HTN) is a multifactorial chronic disease. Considering the high prevalence rates of this disease, treatment of HTN is necessary, not only to reduce blood pressure (BP) levels but also to prevent the development of cardiovascular, cerebrovascular, and kidney diseases. This treatment can be through medication, which will be determined according to the BP values, obtained either in medical consultations or at home; presence of cardiovascular risk factors, and the presence of target organ damage identified during anamnesis. The aim of this systematic review and meta‐analysis is to summarize the effects of device‐guided slow breathing (DGSB) and nondevice‐guided slow breathing (NDGSB) on BP levels of patients with HTN.
Methods
This study is a systematic review and meta‐analysis of randomized clinical trials, pertaining to hypertensive patients, with or without comorbidity, over 18 years old, of both sexes, and with or without hypertensive medication. The selected studies showed comparisons between groups that performed DGSB and/or NDGSB with control conditions. The primary outcome was the value of systolic blood pressure (SBP) and diastolic blood pressure (DBP) after the interventions.
Results
Twenty‐two studies involving 17,214 participants were included in the quantitative analysis. Considerable heterogeneity was revealed between studies. Using random effect model, it was found that DGSB did not significantly reduce SBP and DBP compared to usual care, both in terms BP values and in relation to their variations (SBP, mean difference [MD]: −2.13 mmHg, (95% confidence interval [CI]: −12.71 to 8.44), 288 individuals; I 2 = 93%, high heterogenity: DBP, MD: −0.90, 95% CI: −3.97 to 2.11, 288 individuals; I 2 = 63%, substantial heterogenity. SBP variations MD: −2.42, 95% CI: −7.24 to 2.40, 443 individuals; I 2 = 85% high heterogenity/DBP variations MD: −1.67, 95% CI: −4.57 to 1.24, 443 individuals; I 2 = 80%, high heterogenity).
Conclusion
Based on these results it appears that DGSB did not reduce BP in hypertensive patients and NDGSB is a new path for the future.
Keywords: breathing exercisese, device‐guided breathing, hypertension, physical therapy modalities, resperate, systematic review
1. INTRODUCTION
Hypertension (HTN) is a multifactorial chronic disease and the main risk factor for the development of cardiovascular diseases (CVDs) and chronic kidney disease. 1 It affects 32% of adults and more than 60% of the elderly, being responsible for half of the deaths from CVD in Brazil. 2 In addition, its complications can lead to decreased work productivity and family income. 1 , 2 In high‐income countries such as Canada, the HTN prevalence has declined; in middle‐income countries, such as Latin America, Asia, the Middle East, and North Africa, detection and treatment of HTN have enhanced, whereas low detection and treatment rates persist in the poorest nations, such as those of sub‐Saharan Africa and Oceania. 1 , 3 , 4
Considering the high prevalence rates of the disease, the treatment of HTN is necessary, not only to reduce blood pressure (BP) levels but also to prevent the development of CVD, cerebrovascular diseases, and kidney diseases. This treatment can be through medication, which will be determined according to the BP values, obtained either in medical consultations or at home, cardiovascular risk factors, and the presence of target organ damage identified during anamnesis.
Nonpharmacological treatment has also been shown to be effective in reducing BP levels in patients with HTN, 1 , 2 , 3 , 4 which includes bodyweight control, establishing healthy eating habits, reducing salt consumption, alcohol consumption control, smoking cessation, stress control, aerobic and isometric physical exercises, and slow breathing guided or not by devices. 1 , 2 , 3 , 4
The physiotherapy prescription for the treatment of HTN may include both exercise and device‐guided slow breathing (DGSB) or nondevice‐guided slow breathing (NDGSB); these breathing exercises consist of slow and deep breathing, 6–10 breathing per minute, and can be performed with or without devices. Concerning the practice of exercises, isometric exercises have been shown to be effective in reducing BP levels, as well as aerobic exercises and dynamic exercises. 4 , 5 , 6 On the other hand, DGSB presents controversies about its application. Since it activates cardiac and pulmonary stretching receptors, decreases sympathetic activity, increases parasympathetic activity and vagal tone, changing heart rate and BP, it would be clinically sound to consider that it reduces BP levels. With the BP reduction, there is an increase in baroreflex sensitivity, which promotes improvements in the autonomic balance of hypertensive patients. 7
The American Heart Association reports that there is no strong evidence on the effectiveness of DGSB, whereas the 8th Brazilian Hypertension Guidelines report the degree of recommendation IIa, level of evidence A. 1 , 4 Already a review of 2016 8 reports that there is currently insufficient evidence of data grouped to recommend the routine use of DGSB in hypertensive patients, even though this device is cleared by the United States Food and Drug Administration and the United Kingdom's National Health Service. Cernes et al. 9 in their review stated that DGSB, as long as it is monitored by a health professional, can be recommended for hypertensive patients who cannot obtain full control of their BP with drug treatment or cannot tolerate potential side effects of treatment. de Barros et al. 10 conducted a controlled clinical study with 15 individuals in the control group and 17 in the experimental group in which they performed DGSB 15–20 min/day, 6–10 breathing/min, and concluded that DGSB, in a long term, did not reduce BP values, catecholamine levels, or muscle sympathetic nerve activity in hypertensive patients. However, this use of DGSB was indicated in the 7th Brazilian Hypertension Guidelines. 11
Recommendations for the use of DGSB or NDGSB in clinical practice should be guided by a systematic, high‐quality literature review. Recently, Chaddha et al. 12 published an article that fulfills this requirement. Their review compared DGSB with NDGSB (pranayama, a technique used in yoga) for 4 weeks in prehypertensive and hypertensive patients. The review included 17 studies, and systolic blood pressure (SBP) was reported in 1017 subjects and diastolic blood pressure (DBP) was reported in 964 subjects. Although interesting, it does not cover only hypertensive patients and compares DGSB to pranayama exclusively. Therefore, a systematic review (SR) of the antihypertensive effects of DGSB or NDGSB applied by physical therapists is necessary to provide the best evidence available to clinical physical therapists and hypertensive patients. In addition, it is also important to summarize the evidence on the effectiveness of the DGSB or NDGSB compared to usual care.
This SR was carried out with the objective of summarizing the effects of DGSB or NDGSB on BP levels of hypertensive patients when: compared with the control conditions (such as minimal intervention, usual care, placebo, and no treatment), compared to other interventions, and used as an adjunct to other treatments (medicated). Thus, the research question for this SR with randomized clinical trials (RCTs) was: What are the effects of prolonged use of device‐guided or NDGSB compared to usual care, on the BP values of hypertensive patients?
2. METHODS
2.1. Study design
This SR was inspired by the recommendations of the Cochrane Handbook of Systematic Reviews 13 and the Preferred Reporting Items for Systematic Review and Meta‐Analysis (PRISMA; see eAddenda for Appendix S1). 14
The selected articles met the inclusion criteria according to the type of study, participants, and intervention for SR.
2.2. Type of studies
RCTs published up to January 2020 were included in this SR, without language restriction and year of publication.
2.3. Types of participants
Hypertensive patients, with or without comorbidity, over 18 years old, of both sex, with or without hypertensive medication treatment.
2.4. Types of interventions
Interventions considered had to be DGSB and NDGSB compared to the control conditions (such as minimal intervention—only BP measurement—usual care, placebo, and no treatment); and interventions could be used as an adjunct to other treatments (medication). Any dosage of device‐guided breathing treatment was accepted. Regarding the follow‐up time, 4 and 8‐week studies were considered, and for meta‐analysis, only 8‐week studies were considered (it is the more common time used to treat and reach the BP reduction indicated in studies). 8 , 9
2.5. Exclusion criteria
RCTs that also used other interventions along with DGSB/NDGSB, such as physical activity (aerobic exercises, Tai chi, resistance training, and isometric exercises), salt reduction and salt substitution, stress control techniques that use other types of deep breathing with meditation (e.g., Qigong, Yoga, progressive muscle relaxation and attention‐based stress reduction programs), dietary (dietary approach to stop hypertension, low‐carbohydrate diet, Mediterranean diet, high‐protein diet, low‐fat diet, vegetarian diet, paleolithic diet, and low index glycemic/load) and lifestyle (comprehensive lifestyle modification, smoking cessation, alcohol restriction, sleep, home heating, and weight loss) were excluded since it was not possible to identify the specific effect of DGSB/NDGSB.
2.6. Types of outcomes measures
The primary outcome was the values of SBP and DBP, expressed in mmHg, reached after the interventions, as well as their variations.
The secondary outcome was a reduction in the quantity/dosage of drugs administered to HTN control if the study subjects also used it.
2.7. Identification and selection of studies
A systematic search of all published RCTs on the effects of device and NDGSB on hypertensive patients, without language restriction, was carried out until January 2020 in nine databases: Pubmed/MEDLINE (Medical Literature Analysis and Retrieval System Online), Latin American and Caribbean Health Sciences Literature (LILACS), EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL), Physiotherapy Evidence Database (PEDro), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Scopus, Web of Science, Livivo, as well as searching clinical trial records databases, CT.GOV (Clinical Trials.Gov), and bases for gray OpenGrey literature, Gray Literature Report, and ProQuest Central (Citation, Abstract or Indexing and Dissertations and Theses). In all of these databases, potentially eligible studies were researched, including completed and ongoing RCTs, until January 2020. The complete search strategy used in PubMed/MEDLINE is shown in Appendix S2 (see eAddenda for Appendix S2).
Two reviewers independently analyzed all titles and abstracts retrieved with the search. When there was agreement on a particular record, the study was analyzed in full text by both reviewers, according to the eligibility criteria. In the presence of disagreement between the reviewers, a third reviewer was convened. When additional information was needed, authors of the potentially eligible studies were contacted.
Two reviewers independently extracted the following data from the included trials: author, publication date, country of publication, study type, sample size, participant characteristics (age, gender, use or not of antihypertensive medications, presence of comorbidities, categories of BP, details of intervention (type of device used in the DGSB—whether DGSB was performed with or without load, or how the NDGSB was performed, breaths per minute for DGSB and NDGSB, time of use of the device in a day, and for how many months), details for BP measurement (device used, type of measurement (home or office), protocol used for measurement including preparation), and outcome measures (systolic and diastolic BP). A third reviewer was called in case of disagreement. When necessary, the authors of RCTs included were contacted to provide additional information.
2.8. Assessment of characteristics of studies
The quality assessment of the included studies was conducted using the Cochrane Risk of Bias Tool for Randomized Trials (RoB2), 15 which includes a randomization process, deviations from the intended interventions, conflicting result data, result measurement, selection of the reported result, and biases generally. The same two reviewers performed an independent assessment. Disagreements between reviewers were resolved by discussion and, if necessary, the opinion of a third reviewer was requested. The same two reviewers performed data extraction, using standardized forms regarding the methodological characteristics of the studies, interventions, and results. Disagreements were again resolved by discussion and, if necessary, the opinion of a third reviewer was requested.
2.9. Data analysis
All data from continuous variables referring to BP values in mmHg were synthesized using the mean difference (MD) method, with their respective 95% confidence intervals (CIs). Standard deviations (SDs) for analysis were also extracted.
The effects of interventions on BP values were analyzed separately. The data were evaluated according to the type of intervention (DGSB or NDGSB); however, only studies lasting at least 8 weeks were considered for meta‐analysis (results evaluated after 8 weeks of randomization). Whenever possible, study results, where there was an intention‐to‐treat analysis, were used.
The presence of statistical heterogeneity between RCTs was assessed using the I 2 statistic. The quality of the evidence was considered inconsistent if considerable heterogeneity between the groups (I 2 > 50%) was observed. When sufficient evidence is available, a funnel plot could be used to investigate possible publication bias.
2.10. Data synthesis
The overall quality of the evidence for each outcome was assessed using the Grading of Recommendations, Development and Evaluation (GRADE) 16 system, regardless of whether or not the information was sufficient to summarize the data in quantitative analysis.
The quality of the evidence was categorized as follows: the evidence was of high quality if the results were consistent in ≥75% of the participants, with a low risk of bias, without publication bias, and with consistent direct and accurate data; further research is unlikely to alter the estimate or confidence in such results. The evidence was of moderate quality when only one of the five classification factors above was met; further research can alter the estimated effect and impact on confidence in the effect in this case. The evidence was of poor quality when two of the five classification factors were not met. In this situation, future research is likely to alter the estimated effect and have a significant impact on confidence in the effect. The evidence was of very low quality when three of the five classification factors were not met and, in this case, any estimate of effect is uncertain. 16
2.11. Statistical analysis
The statistics commonly used for meta‐analysis of continuous data are the MD or the standardized mean difference (SMD). Selection of summary statistics for continuous data is determined by whether studies all report the outcome using the same scale (when the MD can be used), as SBP and DBP, or using different scales (when the SMD is usually applied). For the MD approach, the SDs are used together with the sample sizes to compute the weight given to each study. Studies with small SDs are given relatively higher weights while studies with larger SDs are given relatively smaller weights. If the heterogeneity will be present, a CI around the random‐effects summary estimate is wider than a CI around a fixed‐effect summary estimate. This will happen whenever the I 2 statistic is greater than zero, The RevMan will be used for these analyses. 13
3. RESULTS
3.1. The flow of studies throughout the review (Figure 1)
Figure 1.
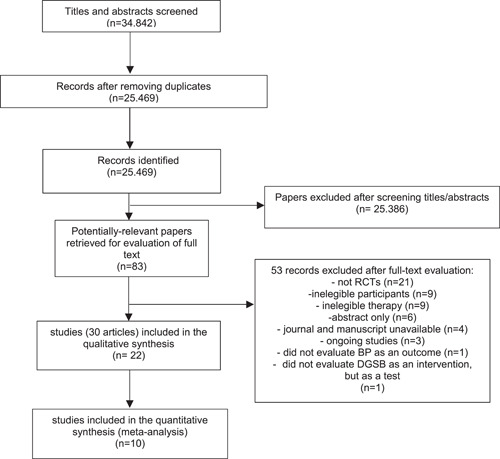
Flowchart of included and excluded studies throughout the review. BP, blood pressure; DGSB, device‐guided slow breathing; RCT, randomized clinical trial.
The 53 records excluded by full text are listed in Appendix S3 (see eAddenda for Appendix S3).
3.2. Characteristics of included studies
The characteristics of each study included are shown in Table 1.
Table 1.
Characteristics of included studies.
| Author/year/country | Interventions (experimental group) | Control group (n) | Experimental group (n) | Duration DGSB/NDGSB | Follow‐up | ||
|---|---|---|---|---|---|---|---|
| Schein/2001 7 /Israel | Breathe with interactive music | 29 | – | 32 | 10 min/day | 8 weeks | |
| Schein/2009 17 /Israel | RESPeRATE (10 bpm) | 33 | – | 33 | 15 min/day | 8 weeks | |
| Jones/2010 18 /Thailand | A no loaded breathing (N/A) | B loaded breathing—20 cmH2O (N/A) | 10 | A10 | B10 | 30 min/2x each day | 8 weeks |
| Clemow/2015 19 /USA | A Sham device (13bpm) | B RESPeRATE (6–10 bpm) | 56 | A54 | B101 | 15 min/day | 8 weeks |
| Sangthong/2016 20 /Thailand | A no loaded breathing (6 bpm) | B loaded breathing 18 cmH20 (6 bpm) | 9 | A10 | B10 | 30 min/day | 8 weeks |
| Grossman/2001 21 /Israel | Breathe with interactive music | 15 | – | 18 | 10 min/day | 8 weeks | |
| Yuenyongchaiwat/2019 22 /Thailand | TU‐breath training resistance applied to the waist cuff = 40% of MIP (3 series/10 repetitions) | 20 | – | 20 | One session | ||
| Landman/2013 23 /The Netherlands | RESPeRATE (bpm: <10) | 24 | – | 21 | 15 min/day | 8 weeks | |
| Gusmão/2012 24 /Brazil | RESPeRATE (bpm: <10) | 16 | – | 16 | 15 min/day | 8 weeks | |
| Hering/2013 25 /Poland | RESPeRATE (bpm: <10) | 12 | – | 10 | 15 min/day (≥40 min/week) | 8 weeks | |
| Barros/2017 10 /Brazil | RESPeRATE (bpm: <10) | 15 | – | 17 | 15 min/day | 8 weeks | |
| Elliot/2004 26 /USA | RESPeRATE (bpm: <10) | 60 | – | 89 | 15 min/day | 8 weeks | |
| Mori/2005 27 /Japan | NDGSB 80% of MIP (6 bmp) | 1807a | – | 14,283a | 30 s | ||
| Ferreira/2013 28 /Brazil | Threshold 30% of MIP (15–20 bpm) | 7 | – | 6 | 30 min/day | 8 weeks | |
| Meles/2004 29 /Italy | RESPeRATE (bpm: <10) | 26 | – | 47 | 15 min/day | 8 weeks | |
| Sundaram/2012 30 /India | NDGSB (6 bpm/min) | 20 | – | 20 | 2x/week | 4 weeks | |
| Ping/2018 31 /Malaysia | NDGSB (5 bpm/min) | 41 | – | 39 | 15 min/day | 8 weeks | |
| Logtenberg/2007 32 /The Netherlands | RESPeRATE (bpm: <10) | 15 | – | 15 | 10–15 min/day | 8 weeks | |
| Altena/2009 33 /The Netherlands | RESPeRATE (bpm: <10) | 15 | – | 15 | 15 min/day | 8 weeks | |
| Howorka/2013 34 /Austria | RESPeRATE (bpm: <10) | 16 | – | 16 | 12 min/day | 8 weeks | |
| Santos/2019 35 /The Netherlands | RESPeRATE (bpm: <10) | 18 | – | 17 | 15 min/day | 8 weeks | |
| Pandic/2008 36 /Sweden | RESPeRATE (bpm: <10) | 22 | – | 31 | 15 min/day 3x/week | 8 weeks | |
Abbreviations: 2x, twice; bpm, breaths per minute; DGSB, device‐guided slow breathing; min, minutes; MIP, maximal inspiratory pressure; NDGSB, nondevice‐guided slow breathing.
In this study, data were also collected with normotensive individuals, which were not included in this review.
3.3. Risk of bias
The data relating to the assessment of the risk of bias for each study are shown in Table 2. Most of the articles included presented good methodological quality.
Table 2.
Risk of bias in studies included according to Cochrane Risk of Bias Tool for Randomized Trials (RoB2).
| Study (author, year) | Randomization process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported result | Overall bias |
|---|---|---|---|---|---|---|
| Schein (2001) 7 | Low | Some concerns | Low | Low | Some concerns | Some concerns |
| Schein (2009) 17 | High | High | Low | High | High | High |
| Jones (2010) 18 | Low | Low | Low | Low | High | High |
| Clemow (2015) 19 | Low | Low | Low | Low | Low | Low |
| Sangthong (2016) 20 | Low | Low | Low | Low | High | High |
| Grossman (2001) 21 | Low | Low | Low | Low | Low | Low |
| Yuenyongchaiwat (2019) 22 | High | Some concerns | Low | Low | Low | High |
| Landman (2013) 23 | Low | Low | Low | Low | Low | Low |
| Gusmão (2012) 24 | High | Low | Low | Low | Low | High |
| Hering (2013) 25 | Low | Low | Low | Low | Low | Low |
| Barros (2017) 10 | Low | Low | Low | Low | Low | Low |
| Elliot (2004) 26 | Low | Low | Low | Low | Low | Low |
| Mori (2005) 27 | High | Low | Low | Low | Low | High |
| Ferreira (2013) 28 | Low | Low | Low | Low | Low | Low |
| Meles (2004) 29 | Low | Low | Low | Low | Low | Low |
| Sundaram (2012) 30 | Low | Low | Low | Low | Low | Low |
| Ping (2018) 31 | Low | Low | Low | Low | Low | Low |
| Logtenberg (2007) 32 | Low | Low | Low | Low | Low | Low |
| Altena (2009) 33 | Low | Low | Low | Low | Low | Low |
| Howorka (2013) 34 | Low | Low | Low | Low | Some concerns | Some concerns |
| Santos (2019) 35 | Some concerns | High | Low | High | Some concerns | High |
| Pandic (2008) 36 | Low | Low | Low | Low | Low | Low |
3.3.1. Summary of results (see Figures 2, 3, 4, 5)
Figure 2.
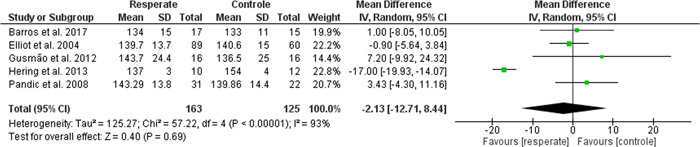
Forest plot of comparison: primary outcome: the effect of DGSB compared to control over postintervention systolic blood pressure. CI, confidence interval; DGSB, device‐guided slow breathing.
Figure 3.
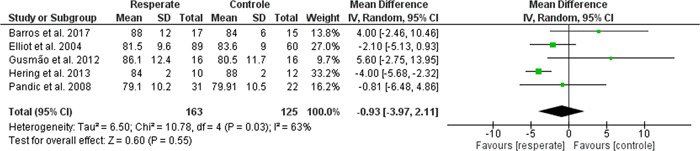
Forest plot of comparison: the effect of DGSB compared to control over postintervention diastolic blood pressure. CI, confidence interval; DGSB, device‐guided slow breathing.
Figure 4.
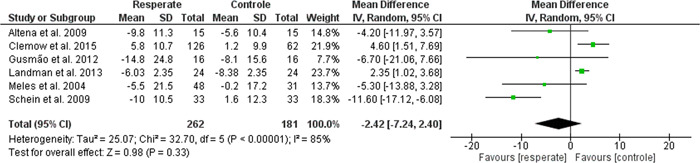
Forest plot of comparison: the effect of DGSB compared to control over the changes in systolic blood pressure. CI, confidence interval; DGSB, device‐guided slow breathing.
Figure 5.
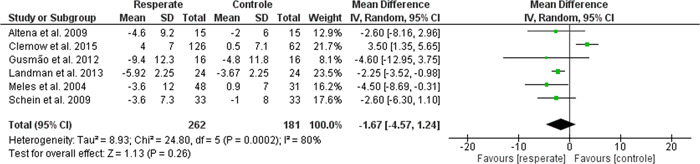
Forest plot of comparison: the effect of DGSB compared to control over the changes in diastolic blood pressure. CI, confidence interval; DGSB, device‐guided slow breathing.
4. DISCUSSION
High BP is associated with many diseases, like obesity and its insulin resistence, 38 pre‐emclampsia 39 and obstructive sleep apnea, 40 so it is necessary to approach new types of treatment HTN, inclusive non‐pharmacological treatments, like DGSB or NDGSB, provided that their risks be smaller than their benefits for hypertensive patients.
The DGSB RCTs 7 , 17 , 19 , 21 , 22 , 23 , 24 , 25 , 26 , 29 , 32 , 33 , 34 , 35 , 36 showed a minimal and not statistically significant reduction in the post/change SBP of −2.13/−2.42 mmHg and in the post/change DBP of −0.93/−1.67 mmHg. Meta‐analyzes identified that the DGSB did not significantly reduce BP compared to the control. These findings do not corroborate the data by Chaddha et al., 12 who reported a modest BP reduction, both for hypertensive and pre‐hypertensive participants. However, these authors compared DGSB with NDGSB (pranayama) for 4 weeks and not for 8 weeks, as well as involved the NDGSB of Yoga (pranayama), both of which were exclusion criteria from this study. In addition, among the participants, there were pre‐hypertensive patients, considered exclusion criteria in this study.
This meta‐analysis is the first to assess NDGSB unrelated to pranayama in the BP of hypertensive patients, since this type of intervention is used routinely in the physiotherapist's clinical practice, in a totally different way from Yoga. However, studies that do not involve Yoga but exclusively the NDGSB of the physiotherapist's practice are still scarce in the literature, which made it impossible to meta‐analyze these studies, 27 , 30 , 31 although two of them 27 , 30 have shown that there was a reduction of the BP values with the technique. Another study 31 concluded that both NDGSB associated with listening to music and listening to music only can reduce BP levels in the same way.
This SR had methodological strengths, such as a punctual review issue, a comprehensive and systematic search for records, both published and unpublished, and the collaboration of a multidisciplinary team of researchers, who used reproducible eligibility criteria as well as the protocol was registered in PROSPERO and published too. 41
In addition, studies were found that reported the use of a different technique than DGSB in which a load (Threshold) 18 , 20 , 28 is associated, which allowed to identify a new path for future research in the area, both for new RCTs, or for another SR.
This study had some limitations. First, the heterogeneity observed in tests with DGSB was high, without being able to identify an explanation for this. Then, the RCTs included consist of an 8‐week follow‐up, and there are already studies, but in smaller quantities, with a 16‐week follow‐up. Although NDGSB may have reduced BP, this information is based on a small number of studies since only three studies with NDGSB were included 18 , 20 , 28 in the qualitative analysis.
Thus, long‐term follow‐up RCTs are needed to better assess the effect of slow breathing (both by device and nondevice‐guided breathing) on BP values and whether these effects are sustained. Tests with loaded DGSB, both using threshold and using the waist cuff, are also necessary.
Based on the five studies included in the post‐SBP and DBP meta‐analysis, according to GRADE, 16 there is low clinical certainty that the DGSB reduces the SBP and DBP of hypertensive patients compared to minimal intervention, or with the usual care, or placebo, or no treatment (SBP after MD: −2.13, 95% CI: −12.71 to 8.44, 288 individuals; I 2 = 93%/DBP after MD: −0.90, 95% CI: −3, 97 to 2.11, 288 individuals; I 2 = 63%). Based on the six studies included in the meta‐analysis of the SBP and DBP delta, according to GRADE, 16 there is low clinical certainty that the DGSB reduces the SBP and DBP of hypertensive patients compared to minimal intervention, or with care usual or with placebo and with no treatment (SBP change DM: −2.42, 95% CI: −7.24 to 2.40, 443 individuals; I 2 = 85%/DBP change DM: −1.67, 95% CI: − 4.57–1.24, 443 individuals; I 2 = 80%).
TRANSPARENCY STATEMENT
All authors have read and approved the final version of the manuscript. Kamila S. de Freitas Gonçalves had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis. All authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
AUTHOR CONTRIBUTIONS
Kamila S. de Freitas Gonçalves: Conceptualization, methodology, investigation, resources, data curation, writing – original draft, visualization, project administration. Ana C. Queiroz Godoy Daniel: Investigation, writing – review and editing. José L. Tatagiba Lamas: writing – review and editing, formal analysis. Henrique C. Oliveira: Formal analysis. Renata C. De Campos Pereira Silveira: Methodology. Lyne Cloutier: Writing – review and editing. Eugenia V. Veiga: Conceptualization, investigation, writing – review and editing, supervision, project administration.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Supporting information
Supporting information.
Supporting information.
Supporting information.
Supporting information.
de Freitas Gonçalves KS, Queiroz Godoy Daniel AC, Tatagiba Lamas JL, et al. Device and nondevice‐guided slow breathing to reduce blood pressure in hypertensive patients: a systematic review and meta‐analysis. Health Sci Rep. 2022;5:e636. 10.1002/hsr2.636
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article (and/or) its Supporting Information Materials.
REFERENCES
- 1. Rabi DM, McBrien KA, Sapir‐Pichhadze R, et al. Hypertension Canada's 2020 Comprehensive Guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can J Cardiol. 2020;36(5):596‐624. [DOI] [PubMed] [Google Scholar]
- 2. Barroso WKS, Rodrigues CIS, Bortolotto LA, et al. Diretrizes Brasileiras de Hipertensão Arterial. Arq Bras Cardiol. 2021;116 (3):516‐658. 10.36660/abc.20201238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. NCD Risk Factor Collaboration (NCD‐RisC) . Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population‐representative studies with 104 million participants. Lancet. 2021;398(10304):957‐980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):e127‐e248. 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 5. Hansen D, Dendale P, Coninx K, et al. The European Association of Preventive Cardiology Exercise Prescription in Everyday Practice and Rehabilitative Training (EXPERT) tool: a digital training and decision support system for optimized exercise prescription in cardiovascular disease. Concept, definitions and construction methodology. Eur J Prev Cardiol. 2017;24(10):1017‐1031. 10.1177/2047487317702042 [DOI] [PubMed] [Google Scholar]
- 6. Pescatello LS, MacDonald HV, Ash GI, et al. Assessing the existing professional exercise recommendations for hypertension: a review and recommendations for future research priorities. Mayo Clin Proc. 2015;90(6):801‐812. 10.1016/j.mayocp.2015.04.008 [DOI] [PubMed] [Google Scholar]
- 7. Schein M, Gavish B, Herz M, et al. 1 Treating hypertension with a device that slows and regularises breathing: a randomised, double‐blind controlled study. J Human Hypertens. 2001;15(4):271‐278. [DOI] [PubMed] [Google Scholar]
- 8. Mahtani KR, Beinortas T, Bauza K, Nunan D. Device‐guided breathing for hypertension: a summary evidence review. Curr Hypertens Rep. 2016;18(4):33. [DOI] [PubMed] [Google Scholar]
- 9. Cernes R, Zimlichman R. Role of paced breathing for treatment of hypertension. Curr Hypertens Rep. 2017;19(6):45. 10.1007/s11906-017-0742-1 [DOI] [PubMed] [Google Scholar]
- 10. de Barros S, da Silva GV, de Gusmão JL, et al. Effects of long term device‐guided slow breathing on sympathetic nervous activity in hypertensive patients: a randomized open‐label clinical trial. Blood Press. 2017;26(6):359‐365. 10.1080/08037051.2017.1357109 [DOI] [PubMed] [Google Scholar]
- 11. Malachias MVB. 7th Brazilian guideline of arterial hypertension: presentation. Arq Bras Cardiol. 2016;107(suppl 3):1‐83. 10.5935/abc.20160140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chaddha A, Modaff D, Hooper‐Lane C, Feldstein DA. Device and non‐device‐guided slow breathing to reduce blood pressure: a systematic review and meta‐analysis. Complement Ther Med. 2019;45:179‐184. 10.1016/j.ctim.2019.03.005 [DOI] [PubMed] [Google Scholar]
- 13. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. The Cochrane Collaboration; 2011. [Google Scholar]
- 14. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 16. Schünemann H, Brożek J, Guyatt G, et al. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. The GRADE Working Group; 2013. [Google Scholar]
- 17. Schein MH, Gavish B, Baevsky T, et al. Treating hypertension in type II diabetic patients with device‐guided breathing: a randomized controlled trial. J Human Hypertens. 2009;23(5):325‐331. [DOI] [PubMed] [Google Scholar]
- 18. Jones CU, Sangthong B, Pachirat O An inspiratory load enhances the antihypertensive effects of home‐based training with slow deep breathing: a randomised trial. J Physiother. 2010;56(3):179‐186. [DOI] [PubMed] [Google Scholar]
- 19. Clemow LP, Simmons T, Roemheld‐Hamm B. Both device‐guided breathing and a relaxation control condition reduce ambulatory BP in hypertensives: Report of an RCT. Psychosom Med. 2015;77(3):A17. [Google Scholar]
- 20. Sangthong B, Ubolsakka‐Jones C, Pachirat O, Jones DA. Breathing training for older patients with controlled isolated systolic hypertension. Med Sci Sports Exerc. 2016;48(9):1641‐1647. [DOI] [PubMed] [Google Scholar]
- 21. Grossman E, Grossman A, Schein MH, et al. Breathing‐control lowers blood pressure. J Hum Hypertens. 2001;15(4):263‐269. [DOI] [PubMed] [Google Scholar]
- 22. Yuenyongchaiwat K, Thanawattano C, Buranapuntalug S, Pongpanit K, Saengkrut P. Development and application of a respiratory device on blood pressure in adults with high blood pressure. Interv Med Appl Sci. 2019;11(1):21‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Landman GW, Drion I, Van Hateren KJ, et al. Device‐guided breathing as treatment for hypertension in type 2 diabetes mellitus a randomized, double‐blind, sham‐controlled trial. JAMA Intern Med. 2013;173(14):1346‐1350. [DOI] [PubMed] [Google Scholar]
- 24. De Gusmão JL, Carminatte DA. Device‐guided slow breathing reduces the poshemodialysis blood pressure in hypertensive patients with chronic kidney disease. J Hypertens. 2012;30:e141. [Google Scholar]
- 25. Hering D, Kucharska W, Kara T, et al. Effects of acute and long‐term slow breathing exercise on muscle sympathetic nerve activity in untreated male patients with hypertension. J Hypertens. 2013;31(4):739‐746. [DOI] [PubMed] [Google Scholar]
- 26. Elliot WJ, Izzo JL Jr., White WB, et al. Graded blood pressure reduction in hypertensive outpatients associated with use of a device to assist with slow breathing. J Clin Hypertens. 2004;6(10):553‐559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mori H, Yamamoto H, Kuwashima M, et al. How does deep breathing affect office blood pressure and pulse rate? Hypertens Res. 2005;28(6):499‐504. https://www.ncbi.nlm.nih.gov/pubmed/16231755 [DOI] [PubMed] [Google Scholar]
- 28. Ferreira JB, Plentz RD, Stein C, Casali KR, Arena R, Lago PD. Inspiratory muscle training reduces blood pressure and sympathetic activity in hypertensive patients: a randomized controlled trial. Int J cardiol. 2013;166(1):61‐67. [DOI] [PubMed] [Google Scholar]
- 29. Meles E, Giannattasio C, Failla M, Gentile G, Capra A, Mancia G. Nonpharmacologic treatment of hypertension by respiratory exercise in the home setting. Am J Hypertens. 2004;17(4):370‐374. http://www.ncbi.nlm.nih.gov/pubmed/15062893 [DOI] [PubMed] [Google Scholar]
- 30. Sundaram B, Maniyar PJ, Varghese JP, et al. Slow breathing training on cardiorespiratory control and exercise capacity in persons with essential hypertension—a randomized controlled trial. Ind J Physiother Occupat Ther. 2012;6(2):17‐21. [Google Scholar]
- 31. Ping KF, Bakar A, Subramaniam S, et al. The impact of music guided deep breathing exercise on blood pressure control—a participant blinded randomised controlled study. Med J Malays. 2018;73(4):233‐238. [PubMed] [Google Scholar]
- 32. Logtenberg SJ, Kleefstra N, Houweling ST, Groenier KH, Bilo HJ. Effect of device‐guided breathing exercises on blood pressure in hypertensive patients with type 2 diabetes mellitus: a randomized controlled trial. J Hypertens. 2007;25(1):241‐246. [DOI] [PubMed] [Google Scholar]
- 33. Altena MR, Kleefstra N, Logtenberg SJ, Groenier KH, Houweling ST, Bilo HJ. Effect of device‐guided breathing exercises on blood pressure in patients with hypertension: a randomized controlled trial. Blood Press. 2009;18(5):273‐279. [DOI] [PubMed] [Google Scholar]
- 34. Howorka K, Pumprla J, Tamm J, et al. 65 Effects of guided breathing on blood pressure and heart rate variability in hypertensive diabetic patients. Auton Neurosc Basic Clin. 2013;179(1):131‐137. [DOI] [PubMed] [Google Scholar]
- 35. Santos ACV, Gusmão JL, Araújo PDP, et al. mpact of guided breathing exercise on blood pressure and sleep quality of hypertensive smokers. Sleep Sci. 2019;12:78. [Google Scholar]
- 36. Pandic S, Ekman I, Nord L, et al. Device‐guided breathing exercises in the treatment of hypertension—perceptions and effects. CVD Prevent Control. 2008;3(3):163‐169. [Google Scholar]
- 37. GRADEpro GDT . GRADEpro Guideline Development Tool [Software]. McMaster University, (developed by Evidence Prime, Inc.). 2020. gradepro.org.
- 38. Al‐Taie M, Baban R, Hamed M. The correlation between serum resistin and toll‐like receptor‐4 with insulin resistance in hypertensive subjects with or without type 2 diabetes mellitus. Bag J Biochem Appl Biol Sciences. 2021;2(04):203‐217. [Google Scholar]
- 39. Nasser NA, Baban RS, Al‐Habib MF, et al. Serum placental growth factor (PLGF) and soluble fms‐like tyrosine kinase‐1 (sFLT‐1) in preeclamptic women at their third trimester of pregnancy. Bag J Biochem Appl Biol Sciences. 2020;1(01):39‐45. [Google Scholar]
- 40. Susanto AD, Harahap RA, Antariksa B, Basalamah MA, Nurwidya F. The prevalence and related risk factors of obstructive sleep apnea in heart failure patients at the indonesian referral hospital for respiratory diseases. J Nat Sci Biol Medicine. 2020;11(2):164. [Google Scholar]
- 41. de Freitas Gonçalves KS, Queiroz Godoy Daniel AC, Tatagiba Lamas JL, et al. Device‐ and nondevice‐guided slow breathing to reduce blood pressure in patients with hypertension: protocol for a systematic review and meta‐analysis. JMIR Res Protoc. 2022;11(3):e33579. 10.2196/33579 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article (and/or) its Supporting Information Materials.


