Abstract
Backgrounds
The COVID‐19 pandemic presents ongoing challenges for healthcare. Stay at Home orders (‘lockdowns’) and community fears have been suggested to create reluctance to seek healthcare. We aimed to determine whether the rates of perforated appendicitis and negative appendicectomy have been affected by the pandemic, and to analyse the effect of lockdowns on the management of acute appendicitis in Victoria.
Methods
We conducted a retrospective audit of emergency appendicectomies performed under adult General Surgery units at Monash Health in Victoria from January 2019 to September 2021, including 242 days of lockdown.
Results
2459 patients were included. Fewer patients had perforated appendicitis during the second lockdown (6.3% versus 10.7% baseline; p = 0.027). The rate of negative appendicectomy was reduced during the first lockdown (4.1% versus 14.9% baseline; p = 0.002) and during intervals between lockdown in 2021 (9.8%; p = 0.010). There was no difference in the rate of perforated appendicitis or negative appendicectomy at other times. Time to surgery and number of appendicectomies performed were also not significantly different. Fewer appendicectomies were performed after hours during lockdowns and in 2021 more generally compared to baseline (p < 0.05).
Conclusion
The lower negative appendicectomy rate during the first lockdown may reflect increased pre‐operative imaging or clinical observation for undifferentiated presentations. There was a reduction in perforated appendicitis during the second lockdown, and no significant difference at other times. Contrary to other studies, lockdowns associated with the COVID‐19 pandemic may not create a reluctance to seek healthcare in all regions.
Keywords: appendicitis, COVID‐19, pandemics, public health, time‐to‐treatment
Comparison of perforated appendicitis rates during COVID‐19 pandemic.
Introduction
The COVID‐19 pandemic has generated an international health crisis and has forced the implementation of restrictions within and between countries globally. Despite relatively low case numbers, the COVID‐19 pandemic has presented unique challenges for the delivery of healthcare within Australia. Restrictions on individual movement, known as ‘lockdowns’, have been enforced around Australia intermittently throughout the pandemic to limit the spread of the COVID‐19 virus. Healthcare delivery and systems have been altered and services prioritized to prevent overwhelming burden on the system, however, these prioritisations and the encouragement of self‐isolation could prevent timely and effective care of patients with non‐COVID disease.
It has been theorized that lockdowns, in combination with fear of entering the healthcare setting due to COVID‐19, have resulted in a reluctance to seek healthcare by community members in Australia. 1 The existing literature supports this, where there have been fewer presentations to metropolitan Emergency Departments during COVID‐19 lockdowns in Melbourne, 2 Sydney, 3 South Australia 4 and New Zealand. 5 Victoria has been the most affected state in Australia by the COVID‐19 pandemic, with multiple extended periods of lockdown during 2020 and 2021.
We conducted a retrospective audit to examine the effect of the COVID‐19 pandemic on the presentation of appendicitis managed by General Surgical teams at Monash Health. We aimed to determine whether the rates of perforated appendicitis and negative appendicectomy have been affected by the COVID‐19 pandemic, as well as to analyse the effect of lockdowns on the management of acute appendicitis in these centres in Victoria.
We examined whether COVID‐19 related protocols, as well as reductions in elective surgery bookings, affected time from initial presentation to surgery, the volume of appendicectomies performed or the proportion of operations performed after hours. The analysis hopes to provide information that may assist in the management of hospital and government responses during the ongoing COVID‐19 pandemic as well as future epidemics.
Methods
We performed a retrospective audit of adult patients who underwent emergency appendicectomy at Monash Health, a metropolitan health network in Victoria, from January 2019 to September 2021 for suspected appendicitis. Monash Health includes three acute General Surgery units (Monash Medical Centre, Dandenong Hospital and Casey Hospital). We defined the COVID‐19 pandemic as beginning with the initial declaration of a State of Emergency in Victoria on 16th March 2020, and lockdowns as being those times during which ‘Stay at Home’ orders were imposed. These ‘Stay at Home’ orders required individuals to remain at home apart from specified purposes, such as seeking medical care, obtaining essential supplies, or work in an authorized industry.
There was no change to institutional protocols regarding the management of patients with suspected appendicitis during the pandemic, and surgical appendicectomy continued to be performed as clinically, biochemically or radiologically indicated, unless patients tested positive for COVID‐19. During lockdown periods, patients were routinely swabbed for COVID‐19 pre‐operatively and surgery delayed until a negative result was returned, unless time critical. Time critical operations or operations for patients with COVID‐19 were able to proceed with use of full personal protective equipment.
We analysed rates of perforated appendicitis, negative appendicectomies, number of appendicectomies performed, proportion of operations performed after hours, and time to surgery during lockdowns and intervening periods outside of lockdown since the beginning of the COVID‐19 pandemic. Lockdowns 1, 2 and 6 were analysed individually (duration 43, 111 and 57 days, respectively), whilst shorter lockdowns 3, 4 and 5 in 2021 (maximum 14 days duration) were combined and analysed as a single lockdown period. Intervals between lockdowns were combined and analysed according to year.
Given that this is a retrospective audit, exemption from formal ethics approval was obtained and this study was registered institutionally as a Quality Assurance activity. Patients eligible for inclusion in the study were all patients aged 16 years or over who had an emergency appendicectomy between January 2019 and September 2021. There were no exclusion criteria for the study. Data were collected using Monash Health electronic medical records (Cerner) and online pathology results (Monash Pathology). Cases were identified using operative records and theatre booking data. Operations commenced before 7 am or after 7 pm were considered ‘after hours’, and time to surgery was defined as time from initial presentation to the Emergency Department to the surgical start time. Histopathology results were reviewed to identify perforated appendicitis and negative appendicectomy, which was defined as the absence of any finding on histopathology for which appendicectomy would be indicated. Data were deidentified after extraction from electronic medical records, stored in a password protected Microsoft Excel database and accessed only by research investigators.
Statistical analysis was performed using IBM SPSS (version 27). Pairwise comparisons of lockdown periods and intervals between lockdown to the baseline of prior to the COVID‐19 pandemic were made using Fisher's exact test for dichotomous outcomes. One‐way analysis of variance with Tukey post hoc testing was conducted to compare time from initial presentation to surgery and number of appendicectomies performed per day. A two‐tailed p < 0.05 was considered statistically significant.
Results
We identified 2459 patients who underwent emergency appendicectomy from January 2019 to September 2021. 1390 patients presented during the pandemic (including 608 presenting during lockdowns) and 1069 patients in the preceding period. Lockdown orders were in place for 242 days during the study period (Table 1).
Table 1.
Lockdown dates
| Days | Dates | |
|---|---|---|
| Prior to COVID‐19 pandemic | 440 | 1/1/2019–15/3/2020 |
| Prior to first lockdown | 15 | 16/3/2020–30/3/2020 |
| During first lockdown | 43 | 31/3/2020–12/5/2020 |
| Between first and second lockdowns | 57 | 13/5/2020–8/7/2020 |
| During second lockdown | 111 | 9/7/2020–27/10/2020 |
| Between second and third lockdowns | 108 | 28/10/2020–12/2/2021 |
| During third lockdown | 5 | 13/2/2021–17/2/2021 |
| Between third and fourth lockdowns | 99 | 18/2/2021–27/5/2021 |
| During fourth lockdown | 14 | 28/5/2021–10/6/2021 |
| Between fourth and fifth lockdowns | 35 | 11/6/2021–15/7/2021 |
| During fifth lockdown | 12 | 16/7/2021–27/7/2021 |
| Between fifth and sixth lockdowns | 8 | 28/7/2021–4/8/2021 |
| During sixth lockdown | 57 | 5/8/2021–30/9/2021 |
The rate of perforated appendicitis was reduced during the second lockdown (6.3% versus 10.7% prior to the pandemic; p = 0.027), but there was no significant difference in rates of perforated appendicitis during other lockdowns or periods outside of lockdown (Table 2; Fig. 1). The rate of negative appendicectomy was reduced during the first lockdown (4.1%; p = 0.002) and during intervals between lockdowns in 2021 (9.8%; p = 0.010) compared to prior to the pandemic (14.9%) (Table 3; Fig. 2). There was no statistically significant difference in mean number of appendicectomies per day (Table 4) or median time from initial presentation to surgery (Table 5) during lockdowns or intervals between lockdowns compared to baseline. A lower proportion of operations were conducted after hours during each of the lockdowns, as well as during periods outside of lockdown during 2021 (p < 0.05) compared to baseline (Table 6).
Table 2.
Rate of perforated appendicitis
| % (n) | Comparison versus prior to COVID‐19 pandemic | |
|---|---|---|
| Prior to COVID‐19 pandemic | 10.7% (114/1069) | Baseline |
| First lockdown | 12.2% (12/98) | p = 0.609 |
| Second lockdown | 6.3% (19/301) | p = 0.027 |
| Third, fourth and fifth lockdowns | 15.8% (12/76) | p = 0.180 |
| Sixth lockdown | 12.0% (16/133) | p = 0.656 |
| Intervals between lockdown 2020 | 12.1% (45/373) | p = 0.442 |
| Intervals between lockdown 2021 | 12.7% (52/409) | p = 0.268 |
Fig. 1.
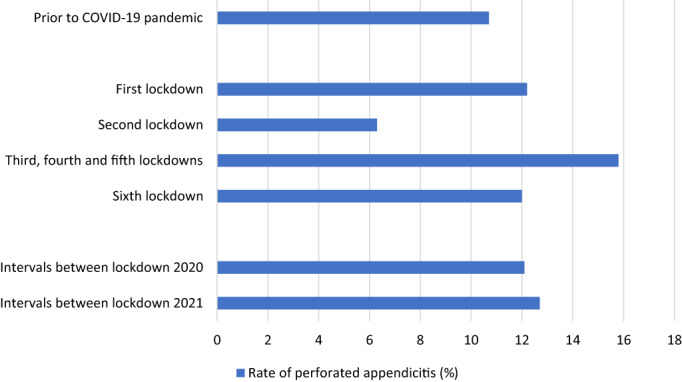
Comparison of perforated appendicitis rates during COVID‐19 pandemic.
Table 3.
Rate of negative appendicectomy
| % (n) | Comparison versus prior to COVID‐19 pandemic | |
|---|---|---|
| Prior to COVID‐19 pandemic | 14.9% (159/1069) | Baseline |
| First lockdown | 4.1% (4/98) | p = 0.002 |
| Second lockdown | 13.6% (41/301) | p = 0.644 |
| Third, fourth and fifth lockdowns | 15.8% (12/76) | p = 0.868 |
| Sixth lockdown | 14.3% (19/133) | p = 1.000 |
| Intervals between lockdown 2020 | 12.1% (45/373) | p = 0.196 |
| Intervals between lockdown 2021 | 9.8% (40/409) | p = 0.010 |
Fig. 2.
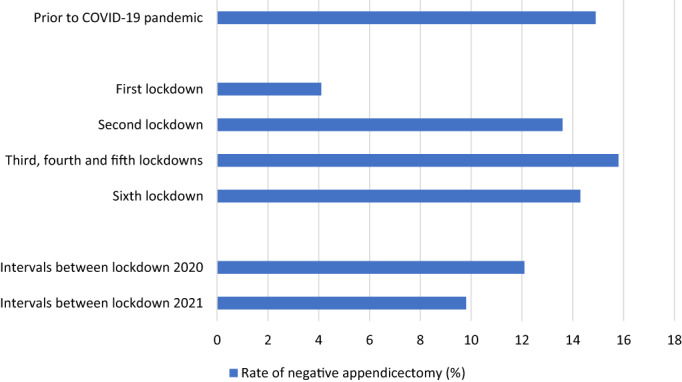
Comparison of negative appendicectomy rates during COVID‐19 pandemic.
Table 4.
Mean number of appendicectomies performed per day
| n | Comparison versus prior to COVID‐19 pandemic | |
|---|---|---|
| Prior to COVID‐19 pandemic | 2.4 | Baseline |
| First lockdown | 2.3 | p = 0.998 |
| Second lockdown | 2.7 | p = 0.626 |
| Third, fourth and fifth lockdowns | 2.5 | p = 1.000 |
| Sixth lockdown | 2.3 | p = 1.000 |
| Intervals between lockdown 2020 | 2.7 | p = 0.482 |
| Intervals between lockdown 2021 | 2.2 | p = 0.775 |
Table 5.
Time from initial presentation to surgery
| Median, IQR (hours) | Comparison versus prior to COVID‐19 pandemic | |
|---|---|---|
| Prior to COVID‐19 pandemic | 22.3 (IQR 14.7–28.7) | Baseline |
| First lockdown | 20.0 (IQR 9.8–24.5) | p = 0.397 |
| Second lockdown | 24.2 (IQR 19.6–31.8) | p = 0.187 |
| Third, fourth and fifth lockdowns | 20.6 (IQR 13.9–25.1) | p = 0.998 |
| Sixth lockdown | 21.8 (IQR 17.5–26.2) | p = 0.952 |
| Intervals between lockdown 2020 | 23.0 (IQR 16.8–30.0) | p = 0.567 |
| Intervals between lockdown 2021 | 21.2 (IQR 14.7–26.5) | p = 1.000 |
Table 6.
Operations undertaken after hours
| % (n) | Comparison versus prior to COVID‐19 pandemic | |
|---|---|---|
| Prior to COVID‐19 pandemic | 18.1% (194/1069) | Baseline |
| First lockdown | 9.2% (9/98) | p = 0.025 |
| Second lockdown | 9.0% (27/301) | p < 0.001 |
| Third, fourth and fifth lockdowns | 6.6% (5/76) | p = 0.007 |
| Sixth lockdown | 9.0% (12/133) | p = 0.007 |
| Intervals between lockdown 2020 | 22.5% (84/373) | p = 0.079 |
| Intervals between lockdown 2021 | 9.3% (38/409) | p < 0.001 |
Discussion
Interestingly, we found that the incidence of perforated appendicitis was lower during the second COVID‐19 related lockdown. Given that there was no clinically significant difference in time from initial presentation to surgery, we suggest that patients may have presented earlier in their disease course during this period and hypothesise that individuals may have been more likely to seek timely medical care in the absence of work or other commitments. This effect was not seen during other lockdowns, or at other times during the pandemic. This result is discordant with other Australian studies, with increased rates of complicated appendicitis reported at a major paediatric tertiary centre in Queensland during the pandemic, despite improved availability of emergency operating theatres. 6 Internationally, similar findings of increased rates of complicated appendicitis have been reported in paediatric patients in Italy, 7 and in both paediatric 8 and adult cohorts 9 in Germany where appendicitis was used in these studies as a proxy for the investigation of delayed presentation to hospital more generally. Our findings suggest there may not be a similar reluctance to seek healthcare in Victoria despite extended periods of lockdown and stay at home orders. Clear public health advice that seeking medical care is an acceptable reason for individual movement during lockdowns may have abated any tendencies to delay seeking medical treatment.
The decreased rate of negative appendicectomy during the first lockdown is an additional unexpected finding. This may reflect a predisposition to obtain imaging or observe patients with undifferentiated pain rather than proceeding to laparoscopy during the early phase of the pandemic, in an effort to avoid unnecessary operations and reduce potential exposure of healthcare staff to COVID‐19. The lower negative appendicectomy rate during intervals between lockdown in 2021, although clinically significant, is less marked, and the cause for this is unclear. The reduction in the volume of appendicectomies performed after hours is consistent with reductions in planned elective surgery in the Victorian healthcare system and hence, increased operating theatre availability for emergency cases during business hours.
While our study was limited by its retrospective nature and its focus on appendicitis particularly, future research could consider multi‐centre analysis of emergency surgical presentations in other states in Australia for a more thorough investigation. Further research could also include comparison of appendicitis managed non‐operatively, as well as whether there was any increase in pre‐operative imaging during the pandemic.
Conclusion
Our findings did not illustrate a significant increase in the rate of perforated appendicitis associated with lockdown periods in Victoria during the COVID‐19 pandemic. This suggests that the pandemic may not create a reluctance to seek healthcare in all regions, as has previously been hypothesised. This study draws attention to the importance of providing timely healthcare for non‐COVID diseases despite challenges of the pandemic. With appropriate public health advice of the importance of seeking medical care even during periods of lockdown, timely provision of healthcare for non‐COVID related diseases can continue to be delivered despite the disruption associated with the COVID‐19 pandemic.
Conflict of interest
None declared.
Author contributions
Ashray Rajagopalan: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; writing – original draft; writing – review & editing. Blake Roschach: Data curation; formal analysis; investigation; methodology. Katherine Mary Kerr Grant: Conceptualization; writing – review and editing. Jasprit Singh: Conceptualization. Marek Bak: Data curation; investigation. Marjorie Burgess: Data curation; investigation. Kerry Liu: Data curation; investigation. Nevin Chen: Data curation; investigation. Jack Menzie: Data curation; investigation. Sarah Chew: Data curation; investigation. Namankit Gupta: Data curation; investigation. Naomi Frederick: Data curation; investigation. Lachlan Hegarty: Data curation; investigation. Carina Chan: Data curation; investigation. Samuel Penfold: Data curation; investigation. Anysha Walia: Data curation; investigation. Daniel Croagh: Conceptualization; supervision.
Acknowledgments
Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
A. Rajagopalan MBBS; B. Roschach MD; K. Grant MBBS; J. Singh MBBS; M. Bak MBBS; M. Burgess MBBS; K. Liu MBBS; N. Chen MBBS; J. Menzie MD; S. Chew MBBS; N. Gupta MD; N. Frederick MD; L. Hegarty MD; C. Chan MD; S. Penfold MD; Anysha Walia MD; D. Croagh MBBS, FRACS.
The corresponding author is not a recipient of a research scholarship.
References
- 1. Lange PW, Gazzard M, Walker S et al. Where are our patients? Retrospective cohort study of acute medical unit admissions during and prior to the COVID‐19 pandemic. Intern. Med. J. 2020; 50: 1132–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Collyer TA, Athanosopoulos G, Srikanth V et al. Impact of COVID‐19 lockdowns on hospital presentations and admissions in the context of low community transmission: evidence from time series analysis in Melbourne, Australia. J. Epidemiol. Community Health 2021; 76: 1–9. [DOI] [PubMed] [Google Scholar]
- 3. Kam AW, Chaudhry SH, Gunasekaran N, White AJR, Vukasovic M, Fung AT. Fewer presentations to metropolitan emergency departments during the COVID‐19 pandemic. Med. J. Aust. 2020; 213: 370–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boyle LM, Mackay M, Bean N, Roughan M. Impact of the COVID‐19 pandemic on South Australia's emergency departments: evidence from two lockdowns. Aust. Health Rev. 2021; 45: 533. [DOI] [PubMed] [Google Scholar]
- 5. Allen MT, Thompson BC, Atkinson B et al. Emergency department presentations in the Southern District of New Zealand during the 2020 COVID‐19 pandemic lockdown. Emerg. Med. Australas. 2021; 33: 534–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee‐Archer P, Blackall S, Campbell H, Boyd D, Patel B, McBride C. Increased incidence of complicated appendicitis during the COVID‐19 pandemic. J. Paediatr. Child Health 2020; 56: 1313–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bellini T, Rotulo GA, Carlucci M, Fiorenza V, Piccotti E, Mattioli G. Complicated appendicitis due to diagnosis delay during lockdown period in Italy. Acta Paediatr. 2021; 110: 1959–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schafer FM, Meyer J, Kellnar S et al. Increased incidence of perforated appendicitis in children during COVID‐19 pandemic in a Bavarian multi‐center study. Front. Pediatr. 2021; 9: 401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Willms AG, Oldhafer KJ, Conze S et al. Appendicitis during the COVID‐19 lockdown: results of a multicenter analysis in Germany. Langenbecks Arch. Surg. 2021; 406: 367–75. [DOI] [PMC free article] [PubMed] [Google Scholar]


