Abstract
Aims
To examine how weekly rates of emergency department (ED) visits for drug overdoses changed among individuals with a recent history of homelessness (IRHH) and their housed counterparts during the pre‐pandemic, peak, and re‐opening periods of the first wave of the COVID‐19 pandemic, using corresponding weeks in 2019 as a historical control.
Design
Population‐based retrospective cohort study conducted between September 30, 2018 and September 26, 2020.
Setting
Ontario, Canada.
Participants
A total of 38 617 IRHH, 15 022 369 housed individuals, and 186 858 low‐income housed individuals matched on age, sex, rurality, and comorbidity burden.
Measurements
ED visits for drug overdoses of accidental and undetermined intent.
Findings
Average rates of ED visits for drug overdoses between January and September 2020 were higher among IRHH compared with housed individuals (rate ratio [RR], 148.0; 95% CI, 142.7–153.5) and matched housed individuals (RR, 22.3; 95% CI, 20.7–24.0). ED visits for drug overdoses decreased across all groups by ~20% during the peak period (March 17 to June 16, 2020) compared with corresponding weeks in 2019. During the re‐opening period (June 17 to September 26, 2020), rates of ED visits for drug overdoses were significantly higher among IRHH (RR, 1.56; 95% CI, 1.44–1.69), matched housed individuals (RR, 1.25; 95% CI, 1.08–1.46), and housed individuals relative to equivalent weeks in 2019 (RR, 1.07; 95% CI, 1.02–1.11). The relative increase in drug overdose ED visits among IRHH was larger compared with both matched housed individuals (P = 0.01 for interaction between group and year) and housed individuals (P < 0.001) during this period.
Conclusions
Recently homeless individuals in Ontario, Canada experienced disproportionate increases in ED visits for drug overdoses during the re‐opening period of the COVID‐19 pandemic compared with housed people.
Keywords: cohort studies, COVID‐19, drug overdose, emergency department visits, homeless persons, vulnerable populations
INTRODUCTION
Although the direct impacts of the coronavirus disease 2019 (COVID‐19) pandemic have been substantial and well‐documented, concerns have been raised about the numerous indirect impacts of the pandemic. Public health measures such as stay‐at‐home orders, closure of public spaces, and social distancing, although critical for reducing viral transmission, have had negative consequences for mental health [1, 2]. Recent evidence suggests that social isolation, economic strain, and uncertainty about the future during the pandemic have increased psychological distress and loneliness [3]. Substance use has intensified as a result of coping with pandemic‐related stressors [4]. Deaths from drug overdoses and emergency department (ED) visits for substance‐related conditions have all increased significantly during the pandemic among the general population in North America [5, 6, 7, 8]. Morbidity and mortality attributable to substance use have likely been exacerbated by closures and reductions in the availability of treatment facilities and harm reduction services during the pandemic [9, 10]. Because of stay‐at‐home‐orders, fears of being exposed to COVID‐19, and caregiving and occupational responsibilities, many people delayed or avoided seeking necessary health care and supports, reflected in reductions in overall primary care visits and hospital use during the pandemic [11, 12, 13]. However, very little is currently known about the indirect toll of the COVID‐19 pandemic on vulnerable populations such as individuals experiencing homelessness.
A growing body of evidence shows that the burden of COVID‐19 infection has been much larger among the homeless population relative to the general population [14, 15]. Many homeless shelters are high‐risk environments for viral transmission, and rates of health conditions that elevate risk of COVID‐19 mortality are much higher in this population [16, 17]. A recent population‐based study in Ontario, Canada found that rates of COVID‐19 infection, hospitalization, and death among individuals with a recent history of homelessness were several times higher than those of the community‐dwelling population, respectively [18]. The outsized direct impact of the pandemic on the homeless population and their pre‐existing risk factors present concerns about disproportionate indirect impacts, particularly in relation to substance‐related outcomes. Drug overdose is a leading cause of morbidity and mortality in the homeless population and baseline rates of substance use disorders are several‐fold higher among individuals experiencing homelessness compared to their housed counterparts [19, 20, 21]. Individuals experiencing homelessness stand to benefit greatly from substance use treatments and harm reduction services [22]. Yet, this population faces tremendous systemic and structural barriers to health care and supports, which have been further exacerbated by the COVID‐19 pandemic [16].
This study had three main objectives for understanding the indirect impacts of the COVID‐19 pandemic on individuals experiencing homelessness. First, it sought to quantify the relative rates of ED visits for drug overdoses in 2020 among individuals with a recent history of homelessness (IRHH) compared to housed individuals. Second, it aimed to describe how rates of ED visits for drug overdoses changed during the 2020 pandemic among IRHH and their housed counterparts, using 2019 as a historical control. Third, it assessed whether changes in ED visits for drug overdoses between 2019 and 2020 were different between IRHH and housed individuals.
METHODS
Study design and setting
We conducted a retrospective population‐based cohort study in Ontario—the most populous province of Canada with a population of 14.7 million as of 2020—using health administrative data. Ontario has a publicly funded healthcare system that provides universal access to essential medical and hospital services. Datasets were linked using unique encoded identifiers and analyzed at ICES. ICES is an independent, non‐profit research institute whose legal status under Ontario's health information privacy law allows it to collect and analyze health care and demographic data, without consent, for health system evaluation and improvement. This study followed the Reporting of Studies Conducted Using Observational Routinely Collected Data (RECORD) reporting guidelines [23].
Data sources
We used a number of data sources to define participants, outcomes, and covariates, including: the Discharge Abstract Database and the Same Day Surgery databases; the National Ambulatory Care Reporting System database; the Ontario Mental Health Reporting System database; the ICES Registered Persons Database demographic and postal year databases; the Ontario Health Insurance Plan claims database; and several ICES‐derived population‐surveillance databases, including the Chronic Obstructive Pulmonary Disease Database, the Ontario Asthma Database, the Ontario Diabetes Database, the Congestive Heart Failure Database, the Ontario Hypertension Database, and the Ontario Cancer Registry.
Participants
All participants were followed from September 30, 2018 until September 26, 2020—the latest date, for which complete data were available at the time of analysis. Individuals were excluded if they died or entered long‐term care on or before September 30, 2018 or if they did not have any contact with the healthcare system in the past 9 years (to ensure participants were living in Ontario). We defined three groups of participants. The first group was IRHH, which included all individuals eligible for Ontario Health Insurance Plan (OHIP) coverage and identified to be experiencing homelessness between September 30, 2018 and September 26, 2020 through an established, previously described algorithm [24]. In brief, the algorithm was able to identify IRHH if they were documented to be experiencing homelessness during a hospital‐based health care encounter or had a residential address associated with shelter services during the study period. The second group consisted of all Ontario residents eligible for OHIP coverage and were not identified as having a recent history of homelessness. This group will be referred to as housed individuals for brevity. The third group was created by restricting the second group to those with at least one hospital‐based health care encounter during the study period and living in a neighborhood in the lowest income quintile. This group was also matched 5:1 to the IRHH group based on age (±2 years), sex (exact), level of rurality (exact), and Charlson Comorbidity Index (CCI) score (exact). Greedy matching was used to produce matched samples with balanced covariates by finding the most optimal match for the first record, removing that record from further consideration, and repeating the process until all records have been matched [25]. The CCI score is a widely used and validated measure for comorbidity adjustment with administrative health data [26].
Outcomes
The primary outcome of this study was ED visits for drug overdoses. International Classification of Diseases, 10th Revision codes X40‐X44 and Y10‐Y14 were used to identify ED visits for unintentional drug overdoses and those of undetermined intent in the National Ambulatory Care Reporting System database. Outcomes were ascertained between January 5 and September 26, 2020, along with corresponding weeks in 2019.
Covariates
We obtained sociodemographic characteristics for all groups at the start of the observation window (September 30, 2018), including age, sex, neighborhood income quintile, and level of rurality. To compare comorbidity burden across groups, we ascertained CCI scores (calculated using hospitalization data from the past 2 years), a past diagnosis of asthma or chronic obstructive pulmonary disease (COPD), diabetes, congestive heart failure, hypertension, chronic liver disease, and a recent cancer diagnosis (past 2 years). Additionally, we measured care for psychotic disorders, non‐psychotic mental health disorders, and substance use disorders and the number of outpatient visits in the year before the observation window.
Statistical analysis
One‐way analysis of variance, Kruskal‐Wallis, Cochran‐Armitage, and χ2 tests were used to compare group characteristics at baseline between IRHH and either housed individuals or matched housed individuals. Because IRHH and housed individuals included nearly all Ontarians, we also reported standardized differences between groups, which assess differences between group means as a percentage of the pooled standard deviation. Standardized differences of 0.1 or more were considered meaningful [27].
For descriptive purposes, we first calculated weekly rates (per 100 000 individuals) of ED visits for drug overdoses in each group throughout the study period, using the cohort at risk that week as the denominator. Individuals were censored if they died or entered long‐term care. Weekly rate ratios (RR) were calculated by dividing group weekly rates in 2020 with corresponding weekly rates in 2019.
Three periods of interest in 2020 were defined for this study based on two major events during the first wave of the COVID‐19 pandemic in Ontario. The first event was the initial declaration of a state of emergency and province‐wide lockdown in Ontario, which occurred on March 17, 2020. The second event was the staggered province‐wide re‐opening in Ontario, which began in the middle of June 2020. Therefore, the periods of January 5–March 16, March 17–June 16, and June 17–September 26 were designated as the pre‐pandemic, peak, and re‐opening periods, respectively.
Poisson regression models with population size offsets were fit to compute RRs and 95% CIs for drug overdose ED visits across groups between January 2020 and September 2020. Separate models were then fit for each group and period to compare weekly rates of ED visits for drug overdoses in 2020 to corresponding weekly rates in 2019. An interaction term between group (IRHH vs housed individuals or IRHH vs matched housed individuals) and year (2020 vs 2019) were added to another set of models to evaluate whether changes in ED visits for drug overdoses between 2019 and 2020 were different between groups for each period.
All tests were two‐sided with P < 0.05 defining statistical significance. Analyses were performed using R 4.0.0 and SAS 9.4. This study was approved by the Research Ethics Board of Unity Health Toronto. Analyses were not pre‐registered and, therefore, results presented in this study should be considered exploratory.
RESULTS
We identified a total of 38 617 IRHH, 15 022 369 housed individuals, and 186 858 matched housed individuals (Supporting information Appendix Fig. S1). Compared with housed individuals, IRHH were significantly more likely to be young adults 25 to 39 years old (36.3% vs 21.7%), male (68.0% vs 49.3%), reside in lowest income quintile neighborhoods (41.7% vs 19.6%), have higher CCI scores, have received care in the previous year for psychotic disorders (25.3% vs 1.1%), non‐psychotic mental health disorders (48.3% vs 11.3%), and substance use disorders (40.9% vs 1.3%) and have had more outpatient visits in the past year (median [IQR], 13 [3‐36] vs 4 [1‐10]) (Table 1). Matched housed individuals were more similar to IRHH in terms of age, sex, level of rurality, and overall level of comorbidity. However, IRHH were still more likely to have several chronic conditions, have received care for mental health and substance use disorders and have had more outpatient visits.
TABLE 1.
Cohort characteristics at index
| Characteristics | IRHH a (n = 38 617) | Housed Ontarians (n = 15 022 369) | Matched housed group b (n = 186 858) | STD difference (IRHH vs housed) | P value (IRHH vs housed) | STD difference (IRHH vs matched) | P value (IRHH vs matched) |
|---|---|---|---|---|---|---|---|
| Age group, n (%) | |||||||
| Youth (<25 y) | 7429 (19.2%) | 4 117 377 (27.4%) | 36 311 (19.4%) | 0.19 | <0.001 | 0.01 | 0.008 |
| Young adults (25‐39 y) | 14 021 (36.3%) | 3 254 132 (21.7%) | 66 192 (35.4%) | 0.33 | 0.02 | ||
| Older adults (40‐64 y) | 14 557 (37.7%) | 5 108 358 (34.0%) | 71 300 (38.2%) | 0.08 | 0.01 | ||
| Seniors (65+ y) | 2610 (6.8%) | 2 542 502 (16.9%) | 13 055 (7.0%) | 0.32 | 0.01 | ||
| Female, n (%) | 12 346 (32.0%) | 7 620 547 (50.7%) | 61 569 (32.9%) | 0.39 | <0.001 | 0.02 | <0.001 |
| Income quintile c | |||||||
| Quintile 1 (lowest) | 16 091 (41.7%) | 2 942 457 (19.6%) | 186 858 (100.0%) | 0.49 | <0.001 | N/A | N/A |
| Quintile 2 | 8126 (21.0%) | 2 923 710 (19.5%) | 0 (0.0%) | 0.04 | |||
| Quintile 3 | 7130 (18.5%) | 3 176 456 (21.1%) | 0 (0.0%) | 0.07 | |||
| Quintile 4 | 3807 (9.9%) | 2 983 780 (19.9%) | 0 (0.0%) | 0.28 | |||
| Quintile 5 (highest) | 3463 (9.0%) | 2 995 966 (19.9%) | 0 (0.0%) | 0.32 | |||
| Level of rurality, n (%) | |||||||
| Large CMA (>500 K) | 22 004 (57.0%) | 9 184 393 (61.1%) | 107 068 (57.3%) | 0.08 | <0.001 | 0.01 | <0.001 |
| Medium CMA (100‐500 K) | 10 237 (26.5%) | 3 060 852 (20.4%) | 49 275 (26.4%) | 0.15 | 0 | ||
| Small CMA (10‐100 K) | 2963 (7.7%) | 1 013 810 (6.7%) | 14 487 (7.8%) | 0.04 | 0 | ||
| Non‐CMA regions | 2343 (6.1%) | 1 291 557 (8.6%) | 11 579 (6.2%) | 0.10 | 0.01 | ||
| Unknown or missing | 1070 (2.8%) | 471 757 (3.1%) | 4449 (2.4%) | 0.02 | 0.02 | ||
| Charlson Comorbidity Index score, n (%) d | |||||||
| No hospitalizations | 28 658 (74.2%) | 13 612 789 (90.6%) | 142 877 (76.5%) | 0.44 | <0.001 | 0.05 | <0.001 |
| 0 | 6647 (17.2%) | 1 028 454 (6.8%) | 28 502 (15.3%) | 0.32 | 0.05 | ||
| 1 | 1699 (4.4%) | 161 215 (1.1%) | 7789 (4.2%) | 0.20 | 0.01 | ||
| 2+ | 1613 (4.2%) | 219 911 (1.5%) | 7690 (4.1%) | 0.16 | 0 | ||
| Specific comorbidities, n (%) | |||||||
| Asthma or COPD | 8799 (22.8%) | 2 256 288 (15.0%) | 34 994 (18.7%) | 0.20 | <0.001 | 0.1 | <0.001 |
| Diabetes | 4142 (10.7%) | 1 422 309 (9.5%) | 22 929 (12.3%) | 0.04 | <0.001 | 0.05 | <0.001 |
| Congestive heart failure | 841 (2.2%) | 253 322 (1.7%) | 4179 (2.2%) | 0.04 | <0.001 | 0 | 0.481 |
| Hypertension | 5793 (15.0%) | 3 041 309 (20.2%) | 35 948 (19.2%) | 0.14 | <0.001 | 0.11 | <0.001 |
| Chronic liver disease | 4547 (11.8%) | 322 277 (2.1%) | 8836 (4.7%) | 0.39 | <0.001 | 0.26 | <0.001 |
| Recent cancer diagnosis d | 209 (0.5%) | 127 320 (0.8%) | 2717 (1.5%) | 0.04 | <0.001 | 0.09 | <0.001 |
| Care for mental health disorders, n (%) e | |||||||
| Psychotic disorders | 9782 (25.3%) | 168 340 (1.1%) | 7002 (3.7%) | 0.77 | <0.001 | 0.64 | <0.001 |
| Non‐psychotic disorders | 18 666 (48.3%) | 1 704 326 (11.3%) | 37 315 (20.0%) | 0.88 | <0.001 | 0.63 | <0.001 |
| Substance use disorders | 15 810 (40.9%) | 198 616 (1.3%) | 11 932 (6.4%) | 1.11 | <0.001 | 0.89 | <0.001 |
| No. of outpatient visits, median (IQR) e | 13 (3–36) | 4 (1–10) | 7 (2–17) | 0.62 | <0.001 | 0.36 | <0.001 |
STD = standardized, CMA = census metropolitan area, COPD = chronic obstructive pulmonary disease, IQR = interquartile range.
Individuals with a recent history of homelessness (IRHH).
Community‐dwelling Ontarians living in income quintile 1 neighborhoods with recent contact with the healthcare system who are matched to individuals with a recent history of homelessness (5:1) on age, sex, level of rurality, and Charlson Comorbidity Index score.
Dissemination area level income quintile, derived from 2016 Census data. Missing and unknown values were recoded to income quintile 3.
Occuring or calculated in the past 2 years.
Occuring in the past year.
Rates (per 100 000 individuals) of ED visits for drug overdoses among IRHH, matched housed individuals, and housed individuals are shown in Supporting information Appendix Figure S2. Average rates between January 2020 and September 2020 were 281.3 among IRHH, 12.6 among matched housed individuals, and 1.9 among housed individuals (Table 2). Compared to housed individuals, rates of ED visits for drug overdoses among IRHH were substantially higher (RR, 148.0; 95% CI, 142.7–153.5). After matching, rates of ED visits for drug overdoses remained higher among IRHH compared to matched housed individuals (RR, 22.3; 95% CI, 20.7–24.0).
TABLE 2.
Events, average rates, and rate ratios of emergency department visits for drug overdoses across groups, January 2020 to September 2020
| Group | Events | Average rate (per 100 000) | Rate ratio vs matched (95% CI) | Rate ratio vs housed (95% CI) |
|---|---|---|---|---|
| IRHH | 3945 | 281.3 | 22.3 (20.7–24.0) | 148.0 (142.7–153.5) |
| Matched a | 879 | 12.6 | Ref | – |
| Housed | 10 721 | 1.9 | – | Ref |
Housed Ontarians residing in lowest income quintile neighborhoods with a recent hospital‐based health care encounter matched to IRHH (5:1) on age, sex, level of rurality, and Charlson Comorbidity Index score. IRHH = individuals with a recent history of homelessness.
Weekly RRs of ED visits for drug overdoses in 2020 versus 2019 for IRHH, matched housed individuals, and housed individuals are shown in Figure 1. During the pre‐pandemic period in 2020 (January 5–March 16), rates of ED visits for drug overdoses among IRHH were significantly higher compared to equivalent 2019 weeks (RR, 1.13; 95% CI, 1.04–1.24) (Table 3 ). No significant changes were observed for matched housed individuals and housed individuals. During the peak period in 2020 (March 17–June 16), ED visits for drug overdoses were significantly lower across IRHH (RR, 0.82; 95% CI, 0.76–0.88), matched housed individuals (RR, 0.84; 95% CI, 0.71–0.97), and housed individuals (RR, 0.79; 95% CI, 0.76–0.83). During the re‐opening period in 2020 (June 17–September 26), rates of ED visits for drug overdoses were markedly higher among IRHH (RR, 1.56; 95% CI, 1.44–1.69), modestly higher among matched housed individuals (RR, 1.25; 95% CI, 1.08–1.46), and marginally higher among housed individuals (RR, 1.07; 95% CI, 1.02–1.11) relative to corresponding weeks in 2019.
FIGURE 1.
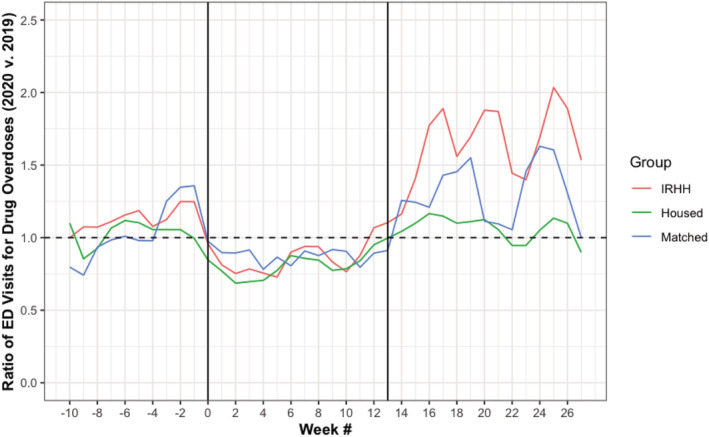
Weekly rate ratios of emergency department visits for drug overdoses by group (2020 vs 2019). Weeks −10, 0, and 27 refer to the weeks of January 5, March 15, and September 20 in 2020, respectively. The first vertical line marks the end of the pre‐pandemic period and beginning of the peak period. The second vertical line marks the end of the peak period and beginning of the re‐opening period. IRHH = individuals with a recent history of homelessness
TABLE 3.
Changes in emergency department visits for drug overdoses by group and pandemic period (2020 vs 2019)
| Group | Pre‐pandemic a | Peak b | Re‐opening c | |||
|---|---|---|---|---|---|---|
| Rate ratio (95% CI) | Interaction P value e | Rate ratio (95% CI) | Interaction P value e | Rate ratio (95% CI) | Interaction P value e | |
| IRHH | 1.13 (1.04–1.24)* | Ref | 0.82 (0.76–0.88)* | Ref | 1.56 (1.44–1.69)* | Ref |
| Matched d | 1.01 (0.84–1.22) | 0.279 | 0.84 (0.71–0.97)* | 0.790 | 1.25 (1.08–1.46)* | 0.01* |
| Housed | 1.01 (0.96–1.07) | 0.03* | 0.79 (0.76–0.83)* | 0.476 | 1.07 (1.02–1.11)* | <0.001* |
*Results are significant at the P < 0.05 level. IRHH = individuals with a recent history of homelessness.
Pre‐pandemic period: January 5, 2020 to March 16, 2020 versus equivalent 2019 weeks.
Peak pandemic period: March 17, 2020 to June 16, 2020 versus equivalent 2019 weeks.
Re‐opening period: June 17, 2020 to September 26, 2020 versus equivalent 2019 weeks.
Housed Ontarians residing in lowest income quintile neighborhoods with a recent hospital‐based health care encounter matched to IRHH (5:1) on age, sex, level of rurality, and Charlson Comorbidity Index score.
Interaction between group and year (2020 vs 2019).
During the pre‐pandemic period, the relative increase in ED visits for drug overdoses between 2019 and 2020 was larger for IRHH compared to housed individuals (P = 0.03 for interaction between group and year). During the re‐opening period, the relative increase in ED visits for drug overdoses between 2019 and 2020 was larger for IRHH compared to both matched housed individuals (P = 0.01) and housed individuals (P < 0.001).
DISCUSSION
In Ontario, average rates of ED visits for drug overdoses between January and September 2020 were considerably higher among IRHH compared to their housed counterparts. Rates of ED visits for drug overdoses declined by ~20% across all groups during the 2020 peak period relative to equivalent weeks in 2019. However, housed individuals, matched housed individuals, and IRHH experienced 7%, 25%, and 56% increases, respectively, in ED visits for drug overdoses during the 2020 re‐opening period relative to equivalent weeks in 2019. The increase among IRHH was significantly more pronounced compared to both matched housed individuals and housed individuals.
Although it is already known that the direct toll of COVID‐19 has been substantial among individuals experiencing homelessness [14, 15, 18], the marked increases in ED visits for drug overdoses during the re‐opening period of the pandemic indicate that this population has also been disproportionately harmed by the indirect effects of the pandemic. Outcomes were comparably worse among recently homeless individuals even in comparison with more medically and socially vulnerable housed individuals, suggesting that the experience of homelessness presented unique challenges during the re‐opening period of the pandemic. Closures and decreased accessibility and availability of treatment facilities and harm reduction services have reduced access to care, pharmacotherapy, and social support, likely contributing to increases in hospitalizations for drug overdoses [10, 28, 29]. These disruptions may have resulted in particularly negative consequences for individuals experiencing homelessness. The burden of drug overdoses was already much larger among the homeless population before the pandemic given higher rates of substance use disorders, greater obstacles to substance use treatment, and harsher circumstances associated with the day‐to‐day experiences of homelessness [21, 22, 30]. This population also continues to contend with other structural barriers to care, such as lack of insurance coverage, competing priorities, and provider‐level stigma [31, 32, 33]. Telehealth and virtual care have filled some gaps in the treatment of substance‐related disorders during the pandemic, but access to these services still remains a challenge for unhoused individuals [34, 35]. Our findings demonstrate an unequivocal need for more accessible and tailored harm reduction, treatment, and recovery support services for the homeless population.
This study also found that increases in ED visits for drug overdoses occurred during the pre‐pandemic period among recently homeless individuals. The rise in overdoses before and during the re‐opening period of the pandemic may be attributable, in part, to an increasingly tainted and toxic unregulated drug supply in Ontario and other jurisdictions, with reported contaminants including synthetic opioids and novel benzodiazepines [36, 37]. Recent studies of characteristics of drug overdose deaths occurring just before and during the COVID‐19 pandemic in Rhode Island and Illinois reported many more fatalities because of synthetic opioids such as fentanyl [38, 39]. Usage of high‐potency and adulterated illicit drugs has been further fueled by pandemic‐related disruptions in regular drug supplies and sources across Canada [40].
Greater supports are urgently needed for individuals experiencing homelessness given substantially higher rates and larger increases in ED visits for drug overdoses among this population before and during the re‐opening period of the COVID‐19 pandemic. Programs and services such as supervised consumption facilities, low‐barrier opioid agonist therapies, and tailored office‐based addiction treatments have been shown to reduce drug‐related morbidity and mortality in the homeless population [22, 41, 42]. The high dual burden of substance use and mental health disorders in this population also necessitates more comprehensive interventions including on‐site and trauma‐informed case management and psychiatric services [21, 43]. One relevant model of care during the pandemic was developed by the City and County of San Francisco, combining hotel‐based COVID‐19 isolation and quarantine with on‐site case management, harm reduction services, pharmacotherapy, telemedicine addiction consultations, and behavioral health supports [44]. Perhaps most importantly, reducing the persistently higher burden of substance‐related difficulties in this population during and beyond the pandemic will require addressing fundamental risk factors such as homelessness and socioeconomic inequities [45, 46].
Further research is needed to understand factors contributing to the reductions in ED visits for drug overdoses during the peak period and subsequent increases during the re‐opening period. These patterns have also been reported in the United States among the general population [7, 47]. One potential contributor is that avoidance of hospital‐based care was highest during the peak period because of social distancing policies and fears of contracting COVID‐19 [13]. Emerging evidence demonstrates significantly higher rates of refusing transportation to the ED for drug overdoses during the peak period [48, 49]. This is also consistent with the 40%–60% reductions in overall ED visits and hospital admissions observed during the first wave [11, 50]. Relative reductions during the peak period in this study were smaller, but this is likely because many substance‐related emergency department visits are precipitated by medical emergencies rather than discretionary care‐seeking [51]. A second potential contributor is that the unregulated drug supply may have continued to become more toxic as the pandemic progressed, resulting in more severe overdoses for which care could not be deferred [36, 40]. One final potential contributor is the movement of individuals experiencing homelessness into temporary housing facilities during the pandemic given high risk of viral transmission in congregate shelters [52]. This may have reduced overdoses given the strong link between the experience of homelessness and drug overdoses [19, 53, 54]. The rebound observed in the re‐opening period may be explained by movement of residents out of such temporary housing facilities or a decline in the potential protective effects of housing on overdoses over time—especially in the absence of additional wraparound supports [55].
Limitations
This study has several important limitations. First, we relied on linked health administrative data, which follows the entire Ontario population eligible for OHIP coverage. Although coverage is near universal in Ontario, OHIP eligibility does not extend to certain groups, including Indigenous persons living on reserves and refugee claimants who do not meet the definition of the 1951 Geneva Convention. Because both of these groups are overrepresented in the homeless population in Canada, results of this study should only be generalized to individuals experiencing homelessness with provincial coverage [56]. Second, the case definition for individuals with a recent history of homelessness mainly relies on recent interaction with hospital‐based health care. Previous work has shown that this method of identifying homelessness is highly specific (>99.9%), but relatively insensitive [24]. Therefore, our cohort of individuals with a recent history of homelessness represents a subgroup of the entire Ontario homeless population. However, we created a matched group of medically and socially vulnerable housed individuals based on a similar requirement of recent interaction with hospital‐based health care, thereby allowing for more accurate comparisons. Third, this study did not assess specific drugs and circumstances surrounding overdose events among the homeless population during the COVID‐19 pandemic and this remains an important area of future research. Finally, only overdoses presenting to EDs were ascertained in this study. The increasing number of fatal overdoses occurring at private and unsupervised settings during the pandemic was likely not captured [38].
CONCLUSIONS
Compared to their housed counterparts, recently homeless individuals had substantially higher rates of emergency department visits for drug overdoses. During the re‐opening period of the COVID‐19 pandemic, increases in rates of drug overdose ED visits were most pronounced among IRHH, even in comparison to more medically and socially vulnerable housed individuals. Our findings indicate that individuals experiencing homelessness have been disproportionately harmed by the direct and indirect impacts of the pandemic. Implementing meaningful public health and policy interventions—such as permanent supportive housing and increased access to health care and substance use services—should be made priorities to protect and promote the health of this vulnerable population during and beyond the COVID‐19 pandemic.
DECLARATION OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Michael Liu: Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; validation; visualization. Lucie Richard: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; software; validation. Michael Campitelli: Data curation; formal analysis; investigation; methodology; project administration. Rosane Nisenbaum: Formal analysis; investigation; methodology. Naheed Dosani: Writing ‐ review & editing‐Supporting. Irfan Dhalla: Supervision. Rishi Wadhera: Supervision. Salimah Shariff: Conceptualization; funding acquisition; investigation; methodology; project administration; supervision. Stephen Hwang: Conceptualization; funding acquisition; investigation; methodology; project administration; supervision.
Supporting information
Data S1 Appendix Figure S1 Flow diagram for cohort build
Appendix Figure S2 Rates of emergency department visits for drug overdoses across groups
ACKNOWLEDGEMENTS
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long‐Term Care (MLTC). This work is also supported by the Ontario Health Data Platform (OHDP), a Province of Ontario initiative to support Ontario's ongoing response to COVID‐19 and its related impacts. This study was completed at the ICES Western site, where core funding is provided by the Academic Medical Organization of Southwestern Ontario, the Schulich School of Medicine and Dentistry, Western University, and the Lawson Health Research Institute. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI) and Cancer Care Ontario (CCO). The conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of ICES, the OHDP, the funding or data sources; no endorsement is intended or should be inferred.
Liu M, Richard L, Campitelli MA, Nisenbaum R, Dosani N, Dhalla IA, et al. Drug Overdoses During the COVID‐19 Pandemic Among Recently Homeless Individuals. Addiction. 2022;117:1692–1701. 10.1111/add.15823
Michael Liu and Lucie Richard contributed equally to this work
Funding information Ontario Health Data Platform; Ontario Ministries of Health and Long‐Term Care
REFERENCES
- 1. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID‐19 and physical distancing: The need for prevention and early intervention. JAMA Intern Med. 2020;180(6):817–8. 10.1001/jamainternmed.2020.1562 [DOI] [PubMed] [Google Scholar]
- 2. Santomauro DF, Herrera AMM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID‐19 pandemic. Lancet. 2021;398(10312):1700–12. 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. Jama. 2020;324(1):93–4. 10.1001/jama.2020.9740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pollard MS, Tucker JS, Green HD. Changes in adult alcohol use and consequences during the COVID‐19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. 10.1001/JAMANETWORKOPEN.2020.22942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gomes T, Kitchen SA, Murray R. Measuring the burden of opioid‐related mortality in Ontario, Canada, during the COVID‐19 pandemic. JAMA Netw Open. 2021;4(5):e2112865. 10.1001/JAMANETWORKOPEN.2021.12865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Appa A, Rodda LN, Cawley C, et al. Drug overdose deaths before and after shelter‐in‐place orders during the COVID‐19 pandemic in San Francisco. JAMA Netw Open. 2021;4(5):e2110452. 10.1001/jamanetworkopen.2021.10452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Holland KM, Jones C, Vivolo‐Kantor AM, Idaikkadar N, Zwald M, Hoots B, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID‐19 pandemic. JAMA Psychiat. 2021;78(4):372–9. 10.1001/jamapsychiatry.2020.4402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Faust JS, Du C, Mayes KD, et al. Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides during the pandemic, march‐august 2020. Jama. 2021;326(1):84–86. 10.1001/jama.2021.8012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Canadian Centre on Substance Use and Addiction . Impacts of the COVID‐19 Pandemic on Substance Use Treatment Capacity in Canada. 2020. https://www.ccsa.ca/impacts-covid-19-pandemic-substance-use-treatment-capacity-canada. Accessed May 18, 2021.
- 10. O'Donoghue AL, Biswas N, Dechen T, Anderson TS, Talmor N, Punnamaraju A, et al. Trends in filled naloxone prescriptions before and during the COVID‐19 pandemic in the United States. JAMA Heal Forum. 2021;2(5):e210393. 10.1001/jamahealthforum.2021.0393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID‐19 pandemic on hospital admissions in the United States. Health Aff. 2020;39(11):2010–7. 10.1377/hlthaff.2020.00980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Glazier RH, Green ME, Wu FC, Frymire E, Kopp A, Kiran T. Shifts in office and virtual primary care during the early COVID‐19 pandemic in Ontario, Canada. CMAJ. 2021;193(6):E200–10. 10.1503/cmaj.202303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or avoidance of medical care because of COVID‐19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–7. 10.15585/MMWR.MM6936A4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Baggett TP, Keyes H, Sporn N, Gaeta JM. Prevalence of SARS‐CoV‐2 infection in residents of a large homeless shelter in Boston. Jama. 2020;323(21):2191–2. 10.1001/jama.2020.6887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roederer T, Mollo B, Vincent C, Nikolay B, Llosa AE, Nesbitt R Seroprevalence and risk factors of exposure to COVID‐19 in homeless people in Paris, France: A cross‐sectional study. Lancet Public Health 2021;6: e202–9. 10.1016/s2468-2667(21)00001-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liu M, Hwang SW. Health care for homeless people. Nat Rev Dis Primers. 2021;7(1):5. 10.1038/s41572-020-00241-2 [DOI] [PubMed] [Google Scholar]
- 17. Perri M, Dosani N, Hwang SW. COVID‐19 and people experiencing homelessness: Challenges and mitigation strategies. CMAJ. 2020;192(26):E716–9. 10.1503/cmaj.200834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Richard L, Booth R, Rayner J, Clemens KK, Forchuk C, Shariff SZ. Testing, infection and complication rates of COVID‐19 among people with a recent history of homelessness in Ontario, Canada: A retrospective cohort study. C Open. 2021;9(1):E1–9. 10.9778/cmajo.20200287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fine DR, Dickins KA, Adams LD, et al. Drug overdose mortality among people experiencing homelessness, 2003 to 2018. JAMA Netw Open. 2022;5(1):e2142676. 10.1001/JAMANETWORKOPEN.2021.42676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Baggett TP, Hwang SW, O'Connell JJ, et al. Mortality among homeless adults in Boston: Shifts in causes of death over a 15‐year period. JAMA Intern Med. 2013;173(3):189–95. 10.1001/jamainternmed.2013.1604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gutwinski S, Schreiter S, Deutscher K, Fazel S. The prevalence of mental disorders among homeless people in high‐income countries: An updated systematic review and meta‐regression analysis. PLoS Med. 2021;18(8):e1003750. 10.1371/JOURNAL.PMED.1003750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pottie K, Kendall CE, Aubry T, et al. Clinical guideline for homeless and vulnerably housed people, and people with lived homelessness experience. CMAJ. 2020;192(10):E240–54. 10.1503/cmaj.190777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies conducted using observational routinely‐collected health data (RECORD) statement. PLoS Med. 2015;12(10):1001885. 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Richard L, Hwang SW, Forchuk C, et al. Validation study of health administrative data algorithms to identify individuals experiencing homelessness and estimate population prevalence of homelessness in Ontario, Canada. BMJ Open. 2019;9(10):30221. 10.1136/bmjopen-2019-030221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stuart EA. Matching methods for causal inference: A review and a look forward. Stat Sci. 2010;25(1):1–25. 10.1214/09-STS313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82. 10.1093/AJE/KWQ433 [DOI] [PubMed] [Google Scholar]
- 27. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228–34. 10.1080/03610910902859574 [DOI] [Google Scholar]
- 28. Volkow ND. Collision of the COVID‐19 and addiction epidemics. Ann Intern Med. 2020;173(1):61–2. 10.7326/M20-1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Radfar SR, De Jong CAJ, Farhoudian A, et al. Reorganization of substance use treatment and harm reduction services during the COVID‐19 pandemic: A global survey. Front Psych. 2021;12:1–16. 10.3389/FPSYT.2021.639393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Upshur CC, Jenkins D, Weinreb L, Gelberg L, Orvek EA. Homeless women's service use, barriers, and motivation for participating in substance use treatment. Am J Drug Alcohol Abuse. 2018;44(2):252–262. 10.1080/00952990.2017.1357183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. Jama. 2001;285(2):200–6. 10.1001/jama.285.2.200 [DOI] [PubMed] [Google Scholar]
- 32. Baggett TP, O'Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: A national study. Am J Public Health. 2010;100(7):1326–33. 10.2105/AJPH.2009.180109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Campbell DJT, O'Neill BG, Gibson K, Thurston WE. Primary healthcare needs and barriers to care among Calgary's homeless populations. BMC Fam Pract. 2015;16:1–10. 10.1186/s12875-015-0361-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Molfenter T, Roget N, Chaple M, Behlman S, Cody O, Hartzler B, et al. Use of telehealth in substance use disorder services during and after COVID‐19: Online survey study. JMIR Ment Heal. 2021;8(2): 1–11. 10.2196/25835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lin LA, Fernandez AC, Bonar EE. Telehealth for substance‐using populations in the age of coronavirus disease 2019: Recommendations to enhance adoption. JAMA Psychiat. 2020;77(12):1209–10. 10.1001/jamapsychiatry.2020.1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gomes T, Murray R, Kolla G, et al. Changing Circumstances Surrounding Opioid‐Related Deaths in Ontario during the COVID‐19 Pandemic. 2021. https://odprn.ca/wp-content/uploads/2021/05/Changing-Circumstances-Surrounding-Opioid-Related-Deaths.pdf. Accessed May 19, 2021.
- 37. Centre on Drug Policy Evaluation . What's in Toronto's Drug Supply? Results from Samples Checked by Toronto's Drug Checking Service October 10, 2019 ‐ March 31, 2020.; 2020.
- 38. Macmadu A, Batthala S, Gabel AMC, et al. Comparison of characteristics of deaths from drug overdose before vs during the COVID‐19 pandemic in Rhode Island. JAMA Netw Open. 2021;4(9):e2125538. 10.1001/JAMANETWORKOPEN.2021.25538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kim HS, Feinglass J, McCarthy DM, Lank PM, Mason M. Unintentional opioid overdose death characteristics in Illinois before and during the COVID‐19 era, 2017 to 2020. JAMA Heal Forum. 2021;2(11):e213699–9. 10.1001/JAMAHEALTHFORUM.2021.3699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ali F, Russell C, Nafeh F, Rehm J, LeBlanc S, Elton‐Marshall T. Changes in substance supply and use characteristics among people who use drugs (PWUD) during the COVID‐19 global pandemic: A national qualitative assessment in Canada. Int J Drug Policy. 2021;93:103237. 10.1016/J.DRUGPO.2021.103237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Magwood O, Salvalaggio G, Beder M, et al. The effectiveness of substance use interventions for homeless and vulnerably housed persons: A systematic review of systematic reviews on supervised consumption facilities, managed alcohol programs, and pharmacological agents for opioid use disorder. PLoS One. 2020;15(1):e0227298. 10.1371/JOURNAL.PONE.0227298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Fine DR, Lewis E, Weinstock K, Wright J, Gaeta JM, Baggett TP. Office‐based addiction treatment retention and mortality among people experiencing homelessness. JAMA Netw Open. 2021;4(3):e210477. 10.1001/JAMANETWORKOPEN.2021.0477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Coldwell CM, Bender WS. The effectiveness of assertive community treatment for homeless populations with severe mental illness: A meta‐analysis. Am J Psychiatry. 2007;164(3):393–399. 10.1176/ajp.2007.164.3.393 [DOI] [PubMed] [Google Scholar]
- 44. Fuchs JD, Carter HC, Evans J, et al. Assessment of a hotel‐based COVID‐19 isolation and quarantine strategy for persons experiencing homelessness. JAMA Netw Open. 2021;4(3):e210490. 10.1001/jamanetworkopen.2021.0490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kashner TM, Rosenheck R, Campinell AB, et al. Impact of work therapy on health status among homeless, substance‐dependent veterans: A randomized controlled trial. Arch Gen Psychiatry. 2002;59(10):938–944. 10.1001/archpsyc.59.10.938 [DOI] [PubMed] [Google Scholar]
- 46. Padgett DK, Stanhope V, Henwood BF, Stefancic A. Substance use outcomes among homeless clients with serious mental illness: Comparing housing first with treatment first programs. Community Ment Health J. 2011;47(2):227–232. 10.1007/S10597-009-9283-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Pines JM, Zocchi MS, Black BS, et al. How emergency department visits for substance use disorders have evolved during the early COVID‐19 pandemic. J Subst Abuse Treat. 2021;129:108391. 10.1016/J.JSAT.2021.108391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Harrison NE, Ehrman RR, Curtin A, et al. Factors associated with voluntary refusal of emergency medical system transport for emergency Care in Detroit during the early phase of the COVID‐19 pandemic. JAMA Netw Open. 2021;4(8):e2120728–8. 10.1001/JAMANETWORKOPEN.2021.20728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID‐19 from emergency medical services data. Drug Alcohol Depend. 2020;214:108176. 10.1016/J.DRUGALCDEP.2020.108176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Jeffery MM, D'Onofrio G, Paek H, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID‐19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328–1333. 10.1001/jamainternmed.2020.3288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lebenbaum M, Chiu M, Vigod S, Kurdyak P. Prevalence and predictors of involuntary psychiatric hospital admissions in Ontario, Canada: A population‐based linked administrative database study. BJPsych Open. 2018;4(2):31–8. 10.1192/bjo.2017.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Huggett TD, Tung EL, Cunningham M, et al. Assessment of a hotel‐based protective housing program for incidence of SARS‐CoV‐2 infection and Management of Chronic Illness among Persons Experiencing Homelessness. JAMA Netw Open. 2021;4(12):e2138464–4. 10.1001/JAMANETWORKOPEN.2021.38464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Yamamoto A, Needleman J, Gelberg L, Kominski G, Shoptaw S, Tsugawa Y. Association between homelessness and opioid overdose and opioid‐related hospital admissions/emergency department visits. Soc Sci Med. 2019;242:112585. 10.1016/J.SOCSCIMED.2019.112585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Riggs KR, Hoge AE, DeRussy AJ, et al. Prevalence of and risk factors associated with nonfatal overdose among veterans who have experienced homelessness. JAMA Netw Open. 2020;3(3):e201190. 10.1001/JAMANETWORKOPEN.2020.1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bardwell G, Collins AB, McNeil R, Boyd J. Housing and overdose: An opportunity for the scale‐up of overdose prevention interventions? Harm Reduct J. 2017;14(1):1–4. 10.1186/S12954-017-0203-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Government of Canada . Everyone Counts 2018: Highlights ‐ Report.; 2020. https://www.canada.ca/en/employment-social-development/programs/homelessness/reports/highlights-2018-point-in-time-count.html. Accessed September 5, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1 Appendix Figure S1 Flow diagram for cohort build
Appendix Figure S2 Rates of emergency department visits for drug overdoses across groups


