Abstract
Aims
This study aimed to identify the psycho‐behavioural factors influencing coronavirus disease 2019 (COVID‐19) vaccine hesitancy among Korean adults. We examined the primary effects of eHealth literacy, social responsibility and self‐efficacy on COVID‐19 vaccine hesitancy using the information‐motivation‐behavioural skills (IMB) model. The moderating effect of age on the relationship between psycho‐behavioural factors and COVID‐19 vaccine hesitancy was also examined.
Design
The study used a cross‐sectional survey design.
Methods
An online survey was completed by 500 Korean adults (253 men and 247 women) aged 20–60 years. Data collection took place in May 2021. The constructed hypothetical model for eHealth literacy, social responsibility, self‐efficacy and age was evaluated using partial least squares structural equation modelling (PLS‐SEM).
Results
eHealth literacy, social responsibility and self‐efficacy had significant negative effects on COVID‐19 vaccine hesitancy. Age had a significant moderating effect on COVID‐19 vaccine hesitancy. The moderating effects of age on the relationship between eHealth literacy and COVID‐19 vaccine hesitancy and between social responsibility and COVID‐19 vaccine hesitancy enhanced the explanatory power by high effect size. The overall fitness of the hypothetical model was good. The standardized root mean square residual value was 0.007, which explained 18.5% of the COVID‐19 vaccine hesitancy.
Conclusion
To reduce COVID‐19 vaccine hesitancy among Korean adults, a strategic approach that considers age should be adopted to enhance eHealth literacy, social responsibility and self‐efficacy.
Impact
The findings of this study suggest that providing correct health information online related to the COVID‐19 vaccine is likely to be effective in decreasing COVID‐19 vaccine hesitancy in older individuals, whereas inspiring a sense of social responsibility is more likely to be effective in younger individuals. These strategic nursing interventions could contribute to improving COVID‐19 vaccination rates among Korean adults.
Keywords: age, COVID‐19 vaccines, health literacy, self‐efficacy, social responsibility
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) continues to threaten the global population (World Health Organization, 2019), and national vaccination campaigns are currently underway, in addition to comprehensive quarantine efforts. According to statistics updated daily, 47.3% of the world population has received at least one dose of a COVID‐19 vaccine, 6.61 billion doses have been administered globally and 22.4 million doses have been administered daily as of 14 October 2021 (Our World in Data, 2021). In South Korea, 62.5% of the national population have been fully vaccinated, and 15.9% of Koreans are waiting to receive their second shot of COVID‐19 as of 14 October 2021 (Our World in Data, 2021).
However, in early May 2021, when COVID‐19 vaccination was in progress in Korea, the rate of full vaccination was only 0.82%, and the rate of completion of the first dose was 6.31% (Korea Disease Control and Preventing Agency, 2021). Although vaccination rate can vary depending on supply and demand, unconfirmed news and information about vaccine safety on social media raises public doubts, causing an increase in COVID‐19 vaccine hesitancy (Puri et al., 2020; Wilson & Wiysonge, 2020). In mid‐October 2021, COVID‐19 vaccine hesitancy was confirmed by observing the rate of advance reservations to receive the vaccine among Korean adults. The advance reservation rate for individuals in their 40s and 50s reached 75.7%, while the advance reservation rate for those in their 20s and 30s was only 57.8% (Korea Disease Control and Preventing Agency, 2021). Moreover, a large proportion of young people claimed that they would prefer to continue social distancing rather than receive a vaccine that they believed could cause death (Shin, 2021). According to a global study, younger people report less vaccine hesitancy about seasonal flu vaccines, whereas they have been found to have more vaccine hesitancy about the COVID‐19 vaccine (Sallam, 2021).
Thus, it is important to understand the causal relationship between psycho‐behavioural factors that cause COVID‐19 vaccine hesitancy, which can help control the rapidly changing COVID‐19 pandemic situation, and to understand the unique characteristics of age group. The authors of this study attempted to identify the unique factors by age that affected COVID‐19 vaccine hesitancy among Korean adults, who are widely considered to have been successfully quarantined to decrease the spread of COVID‐19.
1.1. Background and hypothesis
The term ‘vaccination hesitancy’ refers to an individual's state on the continuum between demanding vaccination and a refusal to ever be vaccinated (refusal and no demand). It is a concept that corresponds to a certain degree of acceptance, delay in vaccination, or partial rejection of vaccination, and an individual can change their position on this continuum at any time from hesitancy to demand or full rejection (MacDonald, 2015). To stop the COVID‐19 transmission and improve herd immunity, it is crucial to improve the rate of vaccine acceptance among those with vaccination hesitancy.
Diverse factors have been found to influence COVID‐19 vaccine hesitancy, including characteristics such as age (Daly & Robinson, 2021; Murphy et al., 2021; Troiano & Nardi, 2021); gender (Murphy et al., 2021; Troiano & Nardi, 2021); education level (Daly & Robinson, 2021; Robertson et al., 2021); job status (Troiano & Nardi, 2021); one's sense of social responsibility (Tavolacci et al., 2021); altruistic tendencies (Murphy et al., 2021); confidence in the health management system and healthcare professionals (Murphy et al., 2021; Yan et al., 2021); knowledge of COVID‐19 (Yan et al., 2021); perceived risk disability, benefit or sensitivity (Chen et al., 2021); and motivation and self‐efficacy (Yan et al., 2021). However, most previous studies have focused on identifying factors related to vaccine hesitancy rather than on a theoretical framework. Daly and Robinson (2021) asserted that more studies are needed to explain and predict the unique phenomenon of COVID‐19 vaccination hesitancy by identifying causal relationships between influencing factors based on a theoretical framework.
The information‐motivation‐behavioural (IMB) model is a theoretical framework for explaining human behaviour according to which information (knowledge) and individual motivation (beliefs or attitudes) induce behavioural change (health behaviour or health risk behaviour) mainly through behavioural skills (self‐efficacy) (Fisher & Fisher, 2002). Based on the IMB model, Internet health information literacy (eHealth literacy) could be considered an informational factor (Choi, 2020; Dib et al., 2021), because rapid changes in the public's information‐seeking methods (Internet or social networking services) have changed the public's degree of knowledge, perception and attitudes toward vaccination, while the non‐face‐to‐face environment has been emphasized (Puri et al., 2020). And, social responsibility, which refers to an individual's sense of responsibility or beliefs related to the maintenance and safety of their community, can be a motivational factor (Kim, 2000; Kwok et al., 2021). Lastly, self‐efficacy, which refers to a person's belief that they can successfully perform the actions necessary to obtain the desired result, can be considered a behavioural skill factor in the IMB model (Kwok et al., 2021; Luo et al., 2020). Therefore, the authors attempted to explain and predict COVID‐19 vaccine hesitancy among Korean adults using the aforementioned psycho‐behavioural factors with the IMB model (Fisher & Fisher, 2002), which is increasingly being used as a theoretical framework for explaining health or health risk behaviours (Luo et al., 2021). The present study investigated the causal relationship between eHealth literacy, social responsibility, and self‐efficacy and how they influenced COVID‐19 vaccine hesitancy. We also investigated the moderating effect of age on the relationship between these factors.
The hypothetical model of this study is shown in Figure 1, and the research hypotheses are as follows: eHealth literacy has a positive effect on self‐efficacy (H1), social responsibility has a positive effect on self‐efficacy (H2), eHealth literacy has a negative effect on COVID‐19 vaccine hesitancy (H3), social responsibility has a negative effect on COVID‐19 vaccine hesitancy (H4), self‐efficacy has a negative effect on COVID‐19 vaccine hesitancy (H5), age moderates the positive relationship between eHealth literacy and self‐efficacy (H6), age moderates the positive relationship between social responsibility and self‐efficacy (H7), age moderates the negative relationship between eHealth literacy and COVID‐19 vaccine hesitancy (H8), age moderates the negative relationship between social responsibility and COVID‐19 vaccine hesitancy (H9), and age moderates the negative relationship between self‐efficacy and COVID‐19 vaccine hesitancy (H10).
FIGURE 1.
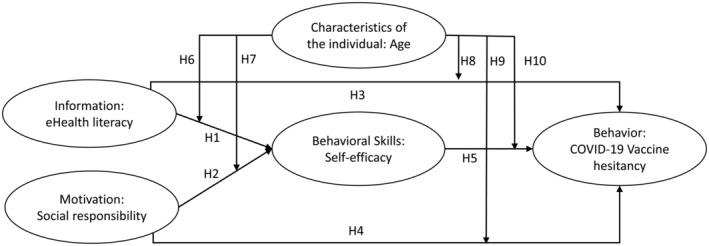
Conceptual framework of this study based on the IMB model
2. THE STUDY
2.1. Aim
This study aimed to explain and predict COVID‐19 vaccine hesitancy among Korean adults using the aforementioned psycho‐behavioural factors with the IMB model and to evaluate the moderating effect of age on the relationship between psycho‐behavioural factors and COVID‐19 vaccine hesitancy.
2.2. Design
This study used a cross‐sectional survey design to investigate the causal relationship between eHealth literacy, social responsibility and self‐efficacy and how they influenced COVID‐19 vaccine hesitancy using partial least squares structural equation modelling (PLS‐SEM). The authors also investigated the moderating effect of age on the relationship between these factors among Korean adults.
2.3. Participants and data collection
The study participants were men and women aged 20–60 years who understood the purpose and methods of this study and agreed to participate in the survey. They were recruited using an online voluntary survey research panel through the Korean Policy & Research Group. Data were collected on 07 May 2021. At the time of data collection, the participants were evenly classified into gender and age groups to enable corresponding sub‐analyses.
The minimum number of participants required was 495, given that 33 variables were measured in this study. A previous study (Yu, 2012) found that at least 15 participants were required for each measured variable when conducting an analysis using a partial least squares structural equation model (PLS‐SEM). The researchers conducted a survey with 500 people, and all of them agreed to participate and responded to the survey. After reviewing the answered questionnaires, we confirmed that all of them were answered completely with no missing responses, and a total of 500 participants were included as the final study participants without any surveys being excluded.
2.4. Ethical considerations
To ensure the safety and privacy of the study participants, the institutional review board of the institution to which the research director belonged reviewed and approved this study (No. CR321025). At the start of the online survey, information about the study, such as the study title, data collection method, and confidentiality of the response data were provided. Participants were allowed to participate in the study by making their own judgements. In addition, it was fully explained that there would be no disadvantages, even if they felt uncomfortable in the course of participating in the survey or decided to stop participating in the research.
2.5. Measures
eHealth literacy refers to the ability to seek, search, understand and evaluate health information online, as well as the ability to apply acquired knowledge to deal with and solve health problems. This study used the eHealth Literacy Scale developed by Norman and Skinner (2006), translated into Korean and validated by Lee et al. (2010). It consists of eight questions on knowledge, ability, evaluation and use of health information found on the Internet. Each item is evaluated using a Likert scale, with 1 point indicating ‘not at all’ and 5 points indicating ‘strongly agree’. The mean item scores were used to compare the variables. The Cronbach's α of the eHealth Literacy Scale was 0.88 in Lee et al.'s (2010) study and 0.91 in this study.
2.5.1. Social responsibility
Social responsibility refers to a person's sense of responsibility toward others for the maintenance and safety of their community (Ko, 2020). This study used the Social Responsibility Scale developed and validated by Ko (2020) consisting of a total of six items, and each item was evaluated using a Likert scale with 1 point indicating ‘not at all’ and 5 points indicating ‘strongly agree’. The mean item scores were used to compare the variables. The Cronbach's α of the tool to measure social responsibility tool was 0.83 in Ko's (2020) study and 0.87 in this study.
2.5.2. Self‐efficacy
Self‐efficacy refers to a person's belief that they can successfully perform the behaviours necessary to achieve the desired result (Bandura, 2010). This study used a version of the self‐efficacy measurement tool developed by Sherer et al. (1982), which was translated into Korean (Kim, 2020). The Korean translated and validated Self‐efficacy Scale by Kim (2020) was also used, consisting of 17 items, and each item was evaluated using a Likert scale with 1 point indicating ‘not at all’ and 5 points indicating ‘strongly agree’. The mean item scores were used to compare the variables. The Cronbach's α of the self‐efficacy tool was 0.86 in Kim's (2020) study and 0.91 in this study.
2.5.3. COVID‐19 vaccine hesitancy
To determine COVID‐19 vaccine hesitancy, the survey asked a single question (‘Are you going to be vaccinated against COVID‐19?’) based on MacDonald (2015) definition of vaccination hesitancy. Responses were recorded using a 5‐point Likert scale, with 1 point indicating ‘I will definitely get the vaccine’, 2 points indicating ‘I will get the vaccine’, 3 points indicating ‘I am hesitant to get the vaccine, so I will think about it’, 4 points indicating ‘I may not get the vaccine’, and 5 points indicating ‘Never, I will not be vaccinated’. Unlike the other variables, COVID‐19 vaccine hesitancy was measured using a single item. This was based on the assumption that a latent variable can be measured as a single item when a multi‐item measurement is highly homogeneous (Cronbach's α > 0.9), or when multiple items are semantically unnecessary (Diamantopoulos et al., 2012).
2.6. Data analysis
This study adopted a hypothetical model to analyse the main effects of eHealth literacy, social responsibility and self‐efficacy on COVID‐19 vaccine hesitancy among Korean adults, and the moderating effect of age on the relationship between these psycho‐behavioural factors and COVID‐19 vaccine hesitancy. To test the causal relationships and moderating effects of age, we used PLS‐SEM. Unlike the covariance‐based structural equation model, PLS‐SEM is a variance‐based Structural Equation Model (VB‐SEM), which is a non‐parametric statistical technique with a bootstrapping method. It has the advantage of having no constraints on the sample size and the normal distribution of variables and residuals (Fornell & Larcker, 1981). PLS‐SEM is also a statistical procedure that allows testing of non‐straightforward relationships and is therefore well suited to the management of cross‐sectional data for inferential purposes. This enables the simultaneous fit of several multiple linear regressions, and the variables present in the regressions may either be observable or latent (Cohidon et al., 2019; Falissard, 2008).
SPSS version 25.0 (IBM Corp.) and SmartPLS 3 were used to analyse PLS‐SEM. First, a descriptive statistical analysis was performed on the demographic characteristics, health‐related characteristics, COVID‐19‐related characteristics, and causal variables of COVID‐19 vaccine hesitancy. The reliability of the latent variables was evaluated using Cronbach's α and the normality of the sample was confirmed by skewness and kurtosis. Multicollinearity between independent variables was confirmed using the variation inflation factor, correlation coefficient and tolerance limit. Second, hypothesis testing of the research model in the present study was conducted by analysing the measurement model and the structural model of PLS‐SEM. For this purpose, this study tested construct validity using a measurement model and tested the proposed hypotheses using a structural model (Hair et al., 2010).
3. RESULTS
3.1. General characteristics of study participants
In total, 50.6% of the study participants were men and 49.4% were women. The average age of participants was 44.5 years. The majority of participants were college graduates (67.4%), office workers (61.6%) and married (52%). In total, 4.4% of the participants had experienced self‐quarantine due to COVID‐19, and the most common channels for obtaining health‐related information were Internet search engines such as Naver and Google (35.4%), mass media (22.6%), close acquaintances, including family and friends (15.6%) and healthcare workers such as doctors or nurses (14.3%). The mean item scores for eHealth literacy, social responsibility and self‐efficacy were 3.63, 4.14 and 3.33 out of 5 points, respectively. The mean score for COVID‐19 vaccine hesitancy was 2.57 points out of 5 points (Table 1).
TABLE 1.
General and psycho‐behavioural characteristics of participants (N = 500)
| Variables | Categories (range) | n (%) or M (SD) |
|---|---|---|
| Sociodemographic characteristics | ||
| Gender | Male | 253 (50.6) |
| Female | 247 (49.4) | |
| Age group, years | 20–29 | 87 (17.4) |
| 30–39 | 98 (19.6) | |
| 40–49 | 108 (21.6) | |
| 50–59 | 103 (20.6) | |
| ≥60 | 104 (20.8) | |
| 44.5 (12.7) | ||
| Education | ≤ High school | 124 (24.8) |
| Bachelor's degree | 337 (67.4) | |
| ≥ Master's degree | 39 (7.8) | |
| Job | No | 192 (38.4) |
| Yes | 308 (61.6) | |
| Marital status | Single | 208 (41.6) |
| Married | 260 (52.0) | |
| Divorced/Separated | 24 (4.8) | |
| Widowed | 8 (1.6) | |
| Health‐related characteristics | ||
| Diagnosed chronic diseases | No | 392 (78.4) |
| Yes | 108 (21.6) | |
| Experience of self‐quarantine due to COVID‐19 | No | 478 (95.6) |
| Yes | 22 (4.4) | |
| Route of health‐related information gathering† | Web searching (Naver, Google, etc.) | 444 (35.4) |
| Social networking service (Facebook, Kakao, etc.) | 122 (9.7) | |
| TV | 283 (22.6) | |
| Radio | 30 (2.4) | |
| Significant others (family, friends, etc.) | 196 (15.6) | |
| Healthcare provider (doctor, nurse, etc.) | 179 (14.3) | |
| eHealth literacy (1~5) | 3.63 (0.69) | |
| Social responsibility (1~5) | 4.14 (0.61) | |
| Self‐efficacy (1~5) | 3.33 (0.60) | |
| COVID‐19 Vaccination hesitancy (1~5) | 2.57 (1.09) | |
Abbreviation: COVID‐19, coronavirus disease 2019; M, mean; SD, standard deviation.
Multi responses.
3.2. PLS measurement model
Table 2 presents the results of the measurement model analysis. The results of the confirmatory factor analysis of the PLS‐SEM showed that all outer loadings were more than 0.70 for both eHealth literacy (0.78–0.82) and social responsibility (0.74–0.76); thus, these constructs demonstrated convergent validity (p < 0.001) in the measurement model. Self‐efficacy (0.43–0.79) had outer loadings of less than 0.70 for some measurement items; however, all self‐efficacy items for which the content validity had already been verified in previous studies (Kim, 2000) were included in our measurement model, because even measurement items with weaker outer loading values between 0.40 and 0.70 can be retained in a measurement model if the composite reliability is satisfied or the items contribute to content validity (Hair Jr et al., 2021). In addition, the Cronbach's α values for the social responsibility and self‐efficacy constructs composed of reflective indicators were 0.91 and 0.87, respectively, and these constructs satisfied internal consistency. The average variance extracted (AVE) for eHealth literacy was 0.62, and the AVE for social responsibility was 0.61. These constructs met the requirement for convergent validity because they had AVE values of at least 0.50 (Fornell & Larcker, 1981). However, the AVE value for self‐efficacy at 0.41, was less than 0.50, but its composite reliability at 0.92 was higher than 0.60. As a result, the convergent validity of the construct was acceptable (Fornell & Larcker, 1981). Discriminant validity is considered satisfactory when the square root of the extracted AVE value of each latent variable is greater than the correlation coefficient of the other latent variables (Fornell & Larcker, 1981). The discriminant validity of each latent variable in this study was confirmed because all the square root values of the AVE, as shown by the diagonal line in Table 3, were larger than the correlation coefficient values of each latent variable. Therefore, both convergent and discriminant validity were satisfied for all latent variables, and the construct validity of all latent variables was also satisfied.
TABLE 2.
Results of the partial least squares measurement model
| Construct | Measurement item | External loading | t | p‐value |
|---|---|---|---|---|
| eHealth Literacy (HL) | HL1 | 0.815 | 42.594 | <0.001 |
| HL2 | 0.801 | 40.611 | <0.001 | |
| HL3 | 0.807 | 39.885 | <0.001 | |
| HL4 | 0.783 | 37.469 | <0.001 | |
| HL5 | 0.838 | 51.718 | <0.001 | |
| HL6 | 0.716 | 25.696 | <0.001 | |
| HL7 | 0.755 | 28.534 | <0.001 | |
| HL8 | 0.779 | 33.295 | <0.001 | |
| Social Responsibility (SR) | SR1 | 0.757 | 29.978 | <0.001 |
| SR2 | 0.784 | 32.193 | <0.001 | |
| SR3 | 0.817 | 40.386 | <0.001 | |
| SR4 | 0.859 | 57.658 | <0.001 | |
| SR5 | 0.728 | 24.045 | <0.001 | |
| SR6 | 0.742 | 27.027 | <0.001 | |
| Self‐efficacy (SE) | SE1 | 0.641 | 23.047 | <0.001 |
| SE2 | 0.486 | 10.139 | <0.001 | |
| SE3 | 0.586 | 17.240 | <0.001 | |
| SE4 | 0.549 | 12.641 | <0.001 | |
| SE5 | 0.724 | 25.145 | <0.001 | |
| SE6 | 0.722 | 26.892 | <0.001 | |
| SE7 | 0.692 | 19.774 | <0.001 | |
| SE8 | 0.432 | 7.390 | <0.001 | |
| SE9 | 0.527 | 12.318 | <0.001 | |
| SE10 | 0.614 | 16.638 | <0.001 | |
| SE11 | 0.654 | 18.825 | <0.001 | |
| SE12 | 0.721 | 26.665 | <0.001 | |
| SE13 | 0.524 | 13.939 | <0.001 | |
| SE14 | 0.762 | 36.565 | <0.001 | |
| SE15 | 0.578 | 15.899 | <0.001 | |
| SE16 | 0.794 | 39.301 | <0.001 | |
| SE17 | 0.713 | 25.066 | <0.001 | |
| Interaction term | Age × Self‐efficacy | 1.045 | 29.389 | <0.001 |
| Age × Social Responsibility | 1.004 | 32.492 | <0.001 | |
| Age × eHealth Literacy | 1.008 | 31.748 | <0.001 | |
| Age | AGE1 | 1 | ||
| COVID‐19 vaccine hesitancy (VH) | VH1 | 1 |
Abbreviation: COVID‐19, coronavirus disease 2019.
TABLE 3.
Square root of the average variance square root and correlations between latent variables
| Latent variable | eHealth literacy | Social responsibility | Self‐efficacy | Age | Age × eHealth literacy | Age × social responsibility | Age × self‐efficacy | COVID‐19 vaccine hesitancy |
|---|---|---|---|---|---|---|---|---|
| AVE | 0.62 | 0.61 | 0.41 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| eHealth Literacy | 0.79 | |||||||
| Social responsibility | 0.35 (<0.001) | 0.78 | ||||||
| Self‐efficacy | 0.37 (<0.001) | 0.31 (<0.001) | 0.64 | |||||
| Age | 0.12 (<0.001) | 0.19 (<0.001) | 0.23 (<0.001) | 1.00 | ||||
| Age × eHealth literacy | 0.04 (<0.001) | −0.01 (<0.001) | −0.01 (<0.001) | −0.06 (<0.001) | 1.00 | |||
| Age × Social responsibility | −0.01 (<0.001) | −0.02 (<0.001) | 0.08 (<0.001) | −0.05 (<0.001) | 0.36 (<0.001) | 1.00 | ||
| Age × Self‐efficacy | −0.01 (<0.001) | 0.08 (<0.001) | −0.13 (<0.001) | −0.04 (<0.001) | 0.35 (<0.001) | 0.23 (<0.001) | 1.00 | |
| COVID‐19 vaccine hesitancy | −0.21 (<0.001) | −0.27 (<0.001) | −0.22 (<0.001) | −0.26 (<0.001) | 0.06 (<0.001) | −0.09 (<0.001) | −0.06 (<0.001) | 1.00 |
Notes. The off‐diagonal elements are the correlations between constructs. Diagonal elements are the square roots of the AVE of each construct.
Abbreviations: AVE, average variance extracted; COVID‐19, coronavirus disease 2019.
3.3. PLS structural model
The overall goodness‐of‐fit of the PLS‐SEM (0.37) was higher than 0.10, thus confirming the overall fit of the model. The standardized root mean square residual (SRMR) value, as an absolute fit index, was 0.01. As an SRMR value of less than 0.10 is generally considered indicative of good fit (Henseler et al., 2014; Hu & Bentler, 1999), the overall fit of the hypothetical model was confirmed. In addition, fitness was also confirmed by the finding that all the Stone‐Geisser Q 2 test statistics related to cross‐validated redundancy showed positive values ranging from 0.08 to 0.13, with an average of 0.10. The average R 2 value of self‐efficacy and COVID‐19 vaccine hesitancy, which indicates the average fit of PLS‐SEM, was 18.5%, confirming that it showed a moderate fit.
The PLS structural model used to evaluate the research hypotheses was assessed by evaluating the significance of the structural path coefficients, as shown in Table 4 and Figure 2. First, for the causal relationships between psycho‐behavioural factors in our proposed research model, eHealth literacy had a significant positive effect on self‐efficacy (H1: path coefficient = 0.30, p < 0.001), and social responsibility had a significant positive effect on self‐efficacy (H2: path coefficient = 0.17, p < 0.001). Second, for the relationships between the psycho‐behavioural factors and COVID‐19 vaccine hesitancy, eHealth literacy had a significant negative effect on COVID‐19 vaccine hesitancy (H3: path coefficient = −0.09, p = 0.034), social responsibility had a significant negative effect on COVID‐19 vaccine hesitancy (H4: path coefficient = −0.17, p = 0.001), and self‐efficacy had a significant negative effect on COVID‐19 vaccine hesitancy (H5: path coefficient = −0.09, p = 0.047).
TABLE 4.
Results of hypothetical model evaluation
| Hypothesis | Path | Path coefficient | SE | t | p |
|---|---|---|---|---|---|
| H1 | eHealth literacy → Self‐efficacy | 0.30 | 0.04 | 6.88 | <0.001 |
| H2 | Social responsibility → Self‐efficacy | 0.17 | 0.05 | 3.51 | <0.001 |
| H3 | eHealth literacy → COVID‐19 vaccine hesitancy | −0.09 | 0.05 | 1.83 | 0.034 |
| H4 | Social responsibility → COVID‐19 vaccine hesitancy | −0.17 | 0.05 | 3.22 | 0.001 |
| H5 | Self‐efficacy → COVID‐19 vaccine hesitancy | −0.09 | 0.05 | 1.68 | 0.047 |
| H6 | Age × eHealth literacy → Self‐efficacy | −0.05 | 0.05 | 1.11 | 0.269 |
| H7 | Age × Social responsibility → Self‐efficacy | 0.11 | 0.05 | 2.27 | 0.023 |
| H8 | Age × eHealth literacy → COVID‐19 vaccine hesitancy | 0.12 | 0.05 | 2.47 | 0.014 |
| H9 | Age × Social responsibility → COVID‐19 vaccine hesitancy | −0.12 | 0.05 | 2.24 | 0.026 |
| H10 | Age × Self‐efficacy → COVID‐19 vaccine hesitancy | −0.08 | 0.05 | 1.60 | 0.111 |
Abbreviations: COVID‐19, coronavirus disease 2019; SE, standard error.
FIGURE 2.
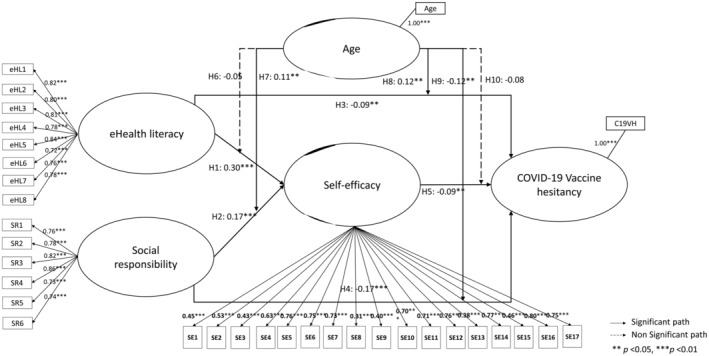
Results of significance testing using the partial least squares (PLS) structural equation model. CV19VH, COVID‐19 vaccine hesitancy; eHL1–8, eHealth literacy; SE1–17, self‐efficacy; SR1–6, social responsibility
Third, age did not have a significant moderating effect on the positive relationship between eHealth literacy and self‐efficacy (H6: path coefficient = −0.05, p = 0.269), but it did have a significant positive moderating effect on the relationship between social responsibility and self‐efficacy (H7: path coefficient = 0.11, p = 0.023), indicating that there was a significant positive interaction between age and social responsibility. In other words, the influence of social responsibility on self‐efficacy was higher for older participants than for younger participants (Figure 3a). Age also showed a significant positive moderating effect on the negative relationship between eHealth literacy and COVID‐19 vaccine hesitancy (H8: path coefficient = 0.12, p = 0.014). This indicates that the interaction between age and eHealth literacy was significantly positive. Figure 3b shows that the relationship between eHealth literacy and COVID‐19 vaccine hesitancy was negative for younger participants and positive for older ones. Age also showed a significant negative moderating effect on the relationship between social responsibility and COVID‐19 vaccine hesitancy (H9: path coefficient = −0.12, p = 0.026), indicating that the interaction between age and eHealth literacy was significantly negative. This result indicates that social responsibility had a greater negative effect on COVID‐19 vaccine hesitancy in older participants than in younger participants (Figure 3c). However, age did not have a significant moderating effect on the relationship between self‐efficacy and COVID‐19 vaccine hesitancy (H10: path coefficient = −0.08, p = 0.111).
FIGURE 3.
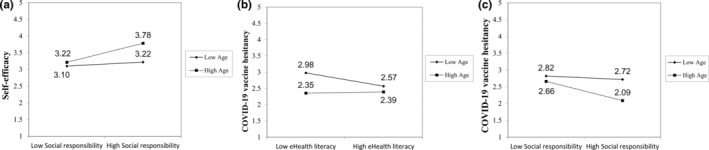
The moderating effect of age on the relationship between psycho‐behavioural factors and COVID‐19 vaccine hesitancy. (a) The moderating effect of age on the relationship between social responsibility and self‐efficacy; (b) The moderating effect of age on the relationship between eHealth literacy and COVID‐19 vaccine hesitancy; (c) The moderating effect of age on the relationship between social responsibility and COVID‐19 vaccine hesitancy
In addition, this study evaluated the overall effect size as f 2 [=R 2(included) − R 2(excluded)]/[1 − R 2(included)] from the main effect model and interaction effect model for the interaction. The R 2 value was 0.20 for self‐efficacy and 0.13 for COVID‐19 vaccine hesitancy in the main effect model of PLS‐SEM without the presence of a moderating effect, whereas the R 2 value was 0.21 for self‐efficacy and 0.16 for COVID‐19 vaccine hesitancy in the interaction effect model of PLS‐SEM. Accordingly, the difference between the R 2 values in the main effect model and the interaction effect model was 0.02 for self‐efficacy and 0.03 for COVID‐19 vaccine hesitancy. Thus, the effect size (f 2) was 0.02 for the moderating effect of age on the relationship between social responsibility and self‐efficacy and 0.04 for the moderating effect of age on both the relationships between eHealth literacy and COVID‐19 vaccine hesitancy and between social responsibility and COVID‐19 vaccine hesitancy. According to Kenny (Kenny, 2018), the effect size indicated by the f 2 value can be classified as low (0.005), moderate (0.01) or high (0.025), based on the minimum value. Therefore, the moderating effect of age on the relationship between social responsibility and self‐efficacy was considered moderate, and the moderating effects of age on the relationship between eHealth literacy and COVID‐19 vaccine hesitancy, and between social responsibility and COVID‐19 vaccine hesitancy were considered high.
4. DISCUSSION
This study identified the degree of COVID‐19 vaccine hesitancy among Korean adults. It was also confirmed that COVID‐19 vaccine hesitancy in individuals with high degrees of eHealth literacy and social responsibility could be reduced by increasing their self‐efficacy. From the perspective of the IMB model, information (eHealth literacy), motivation (social responsibility) and behavioural skills (self‐efficacy) explained the unhealthy behaviour of COVID‐19 vaccine hesitancy at a statistically significant level. This study aimed to confirm the appropriateness of the IMB model as a theoretical framework for explaining the human health‐related behaviour of COVID‐19 vaccination. The results of this study will support the development of strategies to promote COVID‐19 vaccination.
4.1. Psycho‐behavioural factors associated with COVID‐19 vaccine hesitancy
Comparing the differences in mean values from the main study variables and previous studies conducted on Koreans of a similar age using the same measurements as in this study, the eHealth literacy (mean = 3.63) in this study was higher than the results of Lee et al. (2010) (mean = 3.11); social responsibility (mean = 4.14) was also higher than that of Ko (2020) (mean = 3.88); self‐efficacy (mean = 3.33) showed a similar mean value to that of Kim's (2020) (2020) (mean = 3.20). The high mean value of eHealth literacy in this study could be due to participants being recruited from survey panels who were familiar with the online survey. And, the high mean value of social responsibility could be due to the Korean government and the Korea Centers for Disease Control and Prevention, which have been successful in preventing COVID‐19 and have been continuously broadcasting and emphasizing the necessity of realizing a healthy community through COVID‐19 vaccination through various mass media such as news, web‐posting, SNS, brochure, text messages et cetera (Shin, 2021). These results may indicate a high level of interest in COVID‐19 response among the Korean population and it reflects their unique characteristics as responsible members of society desirous of overcoming the pandemic. Therefore, it would be meaningful to examine the possible causal relationships between the study variables of Korean adults with these specific characteristics.
4.2. Modelling of COVID‐19 vaccine hesitancy
Adults with high eHealth literacy had a higher sense of self‐efficacy related to COVID‐19 than those with low eHealth literacy, thereby reducing their COVID‐19 vaccine hesitancy. This supports the results of previous studies (Choi, 2020; Dib et al., 2021), which found that the ability to understand Internet health information and a high degree of self‐efficacy corresponded to an increased uptake of healthy behaviours. These findings highlight the need for strategic approaches to improve eHealth literacy to increase self‐efficacy and the rate of COVID‐19 vaccination. In particular, due to the ongoing pandemic, during which there is a lack of accurate information about COVID‐19, unverified information about the COVID‐19 vaccine can be distributed in real time through the Internet or social networking services, resulting in the rapid spread of misinformation or exaggerated information about the risk of vaccines (Dib et al., 2021; Puri et al., 2020). This suggests that the eHealth literacy of Korean adults should be improved to increase their COVID‐19 vaccination rate. In addition, eHealth literacy is a basic ability to accurately interpret information, and it is a necessary skill that should be cultivated throughout life, regardless of one's age (Dib et al., 2021). To improve eHealth literacy, healthcare providers and public health institutions should make efforts to disseminate accurate and reliable information about COVID‐19 vaccination on the Internet.
Second, adults with a high sense of social responsibility, which refers to an individual's belief in ensuring community safety, had high self‐efficacy related to COVID‐19, thereby reducing their vaccine hesitancy. Social responsibility was identified as the factor that had the greatest influence on COVID‐19 vaccine hesitancy. These results are similar to those of previous studies that found that people with a strong sense of group responsibility (Kwok et al., 2021) or people with strong altruistic tendencies (Murphy et al., 2021) showed less hesitation about COVID‐19 vaccination. Therefore, these findings indicate that one's sense of social responsibility and psychological power (Ko, 2020) of people to prevent the spread of COVID‐19 and end the pandemic quickly enhances self‐efficacy for managing COVID‐19‐related health behaviours, including vaccination, thereby reducing vaccine hesitancy.
Third, adults with high self‐efficacy related to COVID‐19 management had less hesitancy toward the COVID‐19 vaccine. These results are similar to those of a Chinese study (Luo et al., 2020) and indicate that self‐efficacy can enhance individuals' ability to realize health‐promoting behaviours related to COVID‐19 and plays an important role in deciding whether to receive the COVID‐19 vaccine. Therefore, trustworthy healthcare providers or popular public figures sharing their experiences with the COVID‐19 vaccine to promote positive COVID‐19‐related health behaviours will improve self‐efficacy concerning COVID‐19 management and, in turn, decrease COVID‐19 vaccine hesitancy.
4.3. Moderating role of age on COVID‐19 vaccine hesitancy
The moderating effect of age on the relationships among eHealth literacy, social responsibility, self‐efficacy and COVID‐19 vaccine hesitancy can be discussed as follows: First, the effect of social responsibility on self‐efficacy and COVID‐19 vaccine hesitancy was greater for older participants than for younger participants (Figure 3a,c). This result confirms the critical importance of efforts to increase social responsibility among young Koreans so that they understand that COVID‐19 infection can pose a serious risk not only to their own health, but also to the health of others, and to address the problem of COVID‐19 vaccine hesitancy. The rapid spread and asymptomatic nature of COVID‐19 can cause significant harm to public health. Therefore, younger Koreans must be motivated to exercise social responsibility to influence them to comply with quarantine guidelines and to participate more actively in COVID‐19 vaccination. Second, the effect of eHealth literacy on COVID‐19 vaccine hesitancy shows contradictory results according to age. That is, eHealth literacy and COVID‐19 vaccine hesitancy were negatively related for younger participants but positively related for older participants (Figure 3b). This means that H3 was supported for younger participants but not for older participants. This reverse relationship may be due to an increased number of Internet and social media users selectively adopting and accepting distorted information that aligns with their pre‐existing beliefs, inclinations and interests as the ages of such users increase (Del Vicario et al., 2016; Puri et al., 2020). In particular, older participants may tend to have a bias during information collection, influenced by strong individual values or a firm belief system (Chen et al., 2021). In other words, for older participants, COVID‐19 vaccine hesitancy may have increased because of their greater susceptibility to responding to and accepting exaggerated or distorted claims related to COVID‐19. It is possible that with age, individuals may become more sensitive to negative information about health risks than to positive information about health benefits. Therefore, it is very important that trustworthy healthcare providers mitigate vaccine‐related concerns of the older people by providing accurate and reliable information about the COVID‐19 vaccine through the Internet and social media (Murphy et al., 2021; Puri et al., 2020). Anti‐vaccine groups are also active on social media and spread misinformation, which also influences the willingness to vaccinate, a common phenomenon worldwide (Murphy et al., 2021; Sallam, 2021; Shin, 2021). Therefore, aggressive interventional methods, such as identifying opportunities for healthcare providers to modify incorrect health information related to the COVID‐19 vaccine, should be considered.
4.4. Limitations
First, the findings of this study are limited because data were collected through an online survey using a panel registered with a research group owing to the limited opportunity for face‐to‐face contact to prevent the spread of COVID‐19. Therefore, the results of this study should be generalized with caution, as the beliefs of those who were not registered with the panel or who had poor access to the internet were not sufficiently reflected. Second, although this study used a structural model using PLS‐SEM to assess possible causal relationships, it was a cross‐sectional study. Therefore, our results have limitations in determining causal relationships. Future studies should identify causal relationships using longitudinal data.
4.5. Implication for nursing
Although eHealth literacy, social responsibility and self‐efficacy can be considered as influencing factors of COVID‐19 vaccination hesitancy limited to Korean adults, considering the huge adverse health effects of COVID‐19 on the public and the successful case of prevention in Korea, the results of this study will have significant implications for the world. In particular, when nurses encounter individuals who are hesitant to get vaccinated, strategic interventions considering their age (e.g., enhancing social responsibility in younger adults and providing correct information to older adults) should be provided. Nursing interventions that enhance eHealth literacy, social responsibility and self‐efficacy to reduce COVID‐19 vaccine hesitancy in adults are expected to bring positive outcomes in overcoming COVID‐19 worldwide.
5. CONCLUSION
This study investigated the causal effect of eHealth literacy, social responsibility and self‐efficacy on COVID‐19 vaccine hesitancy among Korean adults, and further analysed the moderating effect of age on the relationships between these constructs. This study attempted to provide evidence for the development of specific intervention strategies to reduce COVID‐19 vaccine hesitancy and promote participation in COVID‐19 vaccination. The results showed that eHealth literacy and social responsibility not only had a direct negative effect on COVID‐19 vaccine hesitancy, but also indirectly had a negative effect on COVID‐19 vaccine hesitancy through the improvement of self‐efficacy. In addition, age had a moderating effect on the relationships between social responsibility and self‐efficacy, eHealth literacy and COVID‐19 vaccine hesitancy, and between social responsibility and COVID‐19 vaccine hesitancy. According to the results of this study, to reduce the COVID‐19 vaccine hesitancy, healthcare providers and authorities must actively monitor and manage the spread of unreliable health information on the internet related to COVID‐19 vaccination. In addition, to encourage COVID‐19 vaccination, a strategic approach should be adopted that considers the age of the target population. In particular, for older members of the general public, strategies to enhance the spread of reliable information related to the COVID‐19 vaccine on the Internet and social media should be undertaken. For younger people, strategies should be undertaken to increase their sense of social responsibility and promote the belief that members of a society must actively respond together in the midst of a pandemic rather than responding as individuals.
CONFLICT OF INTEREST
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work in this paper.
AUTHOR CONTRIBUTIONS
All authors have agreed on the final version and meet at least one of the following criteria. Study conception and design acquisition‐ KGY, CJH and SYJ; Data collection‐ KGY and CJH; Analysis and interpretation of the data‐STS and CJH; Drafting and critical revision of the manuscript‐ KGY, CJH and SYJ.
IRB APPROVAL NUMBER
Wonju Severance Christian Hospital IRB, No. CR321025.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15273.
ACKNOWLEDGEMENTS
The authors thank all the older adults who participated in the study.
Kim, G. Y. , Shin, T. , Son, Y‐J & Choi, J. (2022). Psycho‐behavioural factors influencing COVID‐19 vaccine hesitancy among Korean adults: The moderating role of age. Journal of Advanced Nursing, 00, 1–12. 10.1111/jan.15273
Funding information
This study received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors.
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions.
REFERENCES
- Bandura, A. (2010). Self‐efficacy. 10.1002/9780470479216.corpsy0836 [DOI]
- Chen, H. , Li, X. , Liu, X. , Mao, Y. , Wang, R. , Dai, J. , Gao, J. , Fu, H. , Zheng, P. , Xiao, Q. , & Jia, Y. (2021). Health belief model perspective on the control of COVID‐19 vaccine hesitancy and the promotion of vaccination in China: Web‐based cross‐sectional study. Journal of Medical Internet Research, 23(9), e29329. 10.2196/29329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, M. (2020). Association of eHealth use, literacy, informational social support, and health‐promoting behaviors: Mediation of health self‐efficacy. International Journal of Environmental Research and Public Health, 17(21), 7890. 10.3390/ijerph17217890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohidon, C. , Wild, P. , & Senn, N. (2019). A structural equation model of the family physicians attitude towards their role in prevention: A cross‐sectional study in Switzerland. Family Practice, 36(3), 297–303. 10.1093/fampra/cmy063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly, M. , & Robinson, E. (2021). Willingness to vaccinate against COVID‐19 in the US: Representative longitudinal evidence from April to October 2020. American Journal of Preventive Medicine, 60(6), 766–773. 10.1016/j.amepre.2021.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Vicario, M. , Bessi, A. , Zollo, F. , Petroni, F. , Scala, A. , Caldarelli, G. , Stanley, H. E. , & Quattrociocchi, W. (2016). The spreading of misinformation online. Proceedings of the National Academy of Sciences of the United States of America, 113(3), 554–559. 10.1073/pnas.1517441113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamantopoulos, A. , Sarstedt, M. , Fuchs, C. , Wilczynski, P. , & Kaiser, S. (2012). Guidelines for choosing between multi‐item and single‐item scales for construct measurement: A predictive validity perspective. Journal of the Academy of Marketing Science, 40(3), 434–449. 10.1007/s11747-011-0300-3 [DOI] [Google Scholar]
- Dib, F. , Mayaud, P. , Chauvin, P. , & Launay, O. (2021). Online mis/disinformation and vaccine hesitancy in the era of COVID‐19: Why we need an eHealth literacy revolution. Human Vaccines & Immunotherapeutics, 18, 1–3. 10.1080/21645515.2021.1874218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falissard, B. (2008). Mesurer la subjectivité en santé: perspective méthodologique et statistique (2nd ed.). Elsevier. [Google Scholar]
- Fisher, J. D. , & Fisher, W. A. (2002). The information‐motivation‐behavioral skills model. In DiClemente R. J., Crosby R. A., & Kegler M. C. (Eds.), Emerging theories in health promotion practice and research: Strategies for improving public health (Vol. 1, pp. 40–70). Wiley. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11950108 [Google Scholar]
- Fornell, C. , & Larcker, D. F. (1981). Structural equation models with unobservable variables and measurement error: Algebra and statistics. Sage Publications. [Google Scholar]
- Hair, J. F. , Black, W. C. , Barry, B. B. , Babin, B. J. , & Anderson, R. E. (2010). Multivariate data analysis: A global perspective (7th ed.). Pearson Education. [Google Scholar]
- Hair, J. F., Jr. , Hult, G. T. M. , Ringle, C. M. , & Sarstedt, M. (2021). A primer on partial least squares structural equation modeling (PLS‐SEM) (3rd ed.). Sage Publications. [Google Scholar]
- Henseler, J. , Dijkstra, T. K. , Sarstedt, M. , Ringle, C. M. , Diamantopoulos, A. , Straub, D. W. , Ketchen, D. J. , Hair, J. F. , Hult, G. T. M. , & Calantone, R. J. (2014). Common beliefs and reality about partial least squares: Comments on Rönkkö and Evermann (2013). Organizational Research Methods, 17(2), 182–209. 10.1177/1094428114526928 [DOI] [Google Scholar]
- Hu, L. T. , & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Kenny, D. A. (2018). Moderator variables. Retrieved from http://davidakenny.net/cm/moderation.htm
- Kim, D. H. (2020). Association between self‐efficacy, violence experiences, health behaviors and depression in graduate students: Based on Bandura's reciprocal determinism [Unpublished Master's thesis, Inha University]. Incheon, Korea.
- Kim, J. S. (2000). The impact of youth service learning on the development of personal and social responsibility [Unpublished Doctoral Dessertation, Myongji University]. Seoul, Korea.
- Ko, D. W. (2020). What makes people overcome COVID‐19 pandemic? Vulnerable or tolerable characteristics. Korean Journal of Consumer and Advertising Psychology, 21(3), 399–424. 10.21074/kjlcap.2020.21.3.399 [DOI] [Google Scholar]
- Korea Disease Control and Preventing Agency . (2021). Status of immunization performance. Retrieved from https://ncv.kdca.go.kr/
- Kwok, K. O. , Li, K. K. , Tang, A. , Tsoi, M. T. F. , Chan, E. Y. Y. , Tang, J. W. T. , Wong, A. , Wei, W. I. , & Wong, S. Y. S. (2021). Psychobehavioral responses and likelihood of receiving COVID‐19 vaccines during the pandemic, Hong Kong. Emerging Infectious Diseases, 27(7), 1802–1810. 10.3201/eid2707.210054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, B. K. , Byoun, W. J. , & Lim, J. L. (2010). The influence of individual's e‐health literacy on doctor‐patient communication. Journal of Cybercommunication Academic Society, 27(3), 89–125. [Google Scholar]
- Luo, Y. , Yao, L. , Zhou, L. , Yuan, F. , & Zhong, X. (2020). Factors influencing health behaviours during the coronavirus disease 2019 outbreak in China: An extended information‐motivation‐behaviour skills model. Public Health, 185, 298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, Z. , Zhu, X. , Deng, J. , Gong, K. , & Zhu, X. (2021). High‐value utilization of mask and heavy fraction of bio‐oil: From hazardous waste to biochar, bio‐oil, and graphene films. Journal of Hazardous Materials, 420, 126570. 10.1016/j.jhazmat.2021.126570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald, N. E. (2015). Vaccine hesitancy: Definition, scope and determinants. Vaccine, 33(34), 4161–4164. 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- Murphy, J. , Vallières, F. , Bentall, R. P. , Shevlin, M. , McBride, O. , Hartman, T. K. , McKay, R. , Bennett, K. , Mason, L. , Gibson‐Miller, J. , Levita, L. , Martinez, A. P. , Stocks, T. V. A. , Karatzias, T. , & Hyland, P. (2021). Psychological characteristics associated with COVID‐19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nature Communications, 12(1), 29. 10.1038/s41467-020-20226-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman, C. D. , & Skinner, H. A. (2006). eHEALS: The eHealth literacy scale. Journal of Medical Internet Research, 8(4), e27. 10.2196/jmir.8.4.e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Our World in Data (2021). Coronavirus (COVID‐19) vaccinations. Retrieved from https://ourworldindata.org/covid‐vaccinations
- Puri, N. , Coomes, E. A. , Haghbayan, H. , & Gunaratne, K. (2020). Social media and vaccine hesitancy: New updates for the era of COVID‐19 and globalized infectious diseases. Human Vaccines & Immunotherapeutics, 16(11), 2586–2593. 10.1080/21645515.2020.1780846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson, E. , Reeve, K. S. , Niedzwiedz, C. L. , Moore, J. , Blake, M. , Green, M. , Katikireddi, S. V. , & Benzeval, M. J. (2021). Predictors of COVID‐19 vaccine hesitancy in the UK household longitudinal study. Brain, Behavior and Immunity, 94, 41–50. 10.1016/j.bbi.2021.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallam, M. (2021). COVID‐19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccine, 9(2), 160. 10.3390/vaccines9020160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherer, M. , Maddux, J. E. , Mercandante, B. , Prentice‐Dunn, S. , Jacobs, B. , & Rogers, R. W. (1982). The self‐efficacy scale: Construction and validation. Psychological reports, 51(2), 663–671. 10.2466/pr0.1982.51.2.663 [DOI] [Google Scholar]
- Shin, J. H. (2021). “I was worried about the side effects… ” 20–30 Hesitating to Vaccinate . Retrieved from http://news.heraldcorp.com/view.php?ud=20210814000115
- Tavolacci, M. P. , Dechelotte, P. , & Ladner, J. (2021). COVID‐19 vaccine acceptance, hesitancy, and resistancy among university students in France. Vaccine, 9(6), 654. 10.3390/vaccines9060654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano, G. , & Nardi, A. (2021). Vaccine hesitancy in the era of COVID‐19. Public Health, 194, 245–251. 10.1016/j.puhe.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, S. L. , & Wiysonge, C. (2020). Social media and vaccine hesitancy. BMJ Global Health, 5(10), 004206. 10.1136/bmjgh-2020-004206, e004206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2019). Ten threats to global health in 2019. Retrieved from https://www.who.int/news‐room/spotlight/ten‐threats‐to‐global‐health‐in‐2019
- Yan, E. , Lai, D. W. L. , & Lee, V. W. P. (2021). Predictors of intention to vaccinate against COVID‐19 in the general public in Hong Kong: Findings from a population‐based, cross‐sectional survey. Vaccine, 9(7), 696. 10.3390/vaccines9070696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, J. P. (2012). Structural equation models: Concepts and understanding. Hannarae Publishing. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to privacy/ethical restrictions.


