Abstract
Wound documentation is integral to effective wound care, health data coding and facilitating continuity of care. This study evaluated the usability and effectiveness of an artificial intelligence application for wound assessment and management from a clinician‐and‐patient user perspective. A quasi‐experimental design was conducted in four settings in an Australian health service. Data were collected from patients in the standard group (n = 166, 243 wounds) and intervention group (n = 124, 184 wounds), at baseline and post‐intervention. Clinicians participated in a survey (n = 10) and focus group interviews (n = 13) and patients were interviewed (n = 4). Wound documentation data were analysed descriptively, and bivariate statistics were used to determine between‐group differences. Thematic analysis of interviews was conducted. Compared with the standard group, wound documentation in the intervention group improved significantly (more than two items documented 24% vs 70%, P < .001). During the intervention, 101 out of 132 wounds improved (mean wound size reduction = 53.99%). Positive evaluations identified improvements such as instantaneous objective wound assessment, shared wound plans, increased patient adherence and enhanced efficiency in providing virtual care. The use of the application facilitated remote patient monitoring and reduced patient travel time while maintaining optimal wound care.
Keywords: artificial intelligence, digital application, documentation, wound, wound care
1. INTRODUCTION
Individuals with wounds can be found across all age groups and all health care specialties. Some causes of wounds include trauma, burns, skin cancers, infections or underlying medical conditions such as diabetes. 1 Wound care is generally considered a comorbid disease, for example, diabetic foot ulcers, venous leg ulcers, pressure injuries, but despite this, patients are treated in the silo of their medical specialty. 1 The impact is that the approaches to wound care may differ between specialities, and currently there is no specialist patient‐centred wound care approach.
Management of all wounds requires good assessment and handover. 2 , 3 Inaccurate wound documentation can affect the determination of the best treatment options and the wound healing process. 4 The careful documentation of wounds should include all variables, such as the wound location and size, the surrounding skin, the presence of undermining and tunnelling and the amount of exudate, odour and/or pain. 5
The Australian Standards for Wound Management highlight the importance of accurate documentation to provide a ‘legal, comprehensive, chronological record of the individual's wound assessment, management and prevention plan’. 6 However, there is a paucity of research that specifically addresses wound documentation—only a few small studies have been published, which indicate deficiencies in this area. 7
A small Australian and Norwegian study 8 using a retrospective review of wound documentation across five health care facilities identified that almost half (45%) of the medical record notes on wounds—specifically, pressure injuries—lacked key details on assessment and intervention. Wound care activities were not described comprehensively. Gillespie and colleagues 9 studied wound documentation by clinicians in 200 medical records in an Australian hospital. They found that less than half (41.4%) of the medical records had completed wound assessment documentation and that wound care documentation was not in line with evidence‐based guidelines.
Similar results have been found in the United States and other countries. In their pilot study conducted in a 560‐bed tertiary hospital, Dan Li and Korniewicz 10 found that wound assessment and management documentation in electronic medical records (eMR) was poorer than in written documentation. Thus, current wound documentation in eMR does not capture the complex needs of patients, and nor does it reflect evidenced‐based practice. 11 A recent stakeholder engagement and forum review conducted by a national group of experts in Australia found a lack of integration of patient records and wound information across the continuum of care. 12
The importance of wound photography for detailed, reliable wound assessment, monitoring and management has been demonstrated in numerous publications. 13 , 14 , 15 , 16 , 17 Increasingly, health services are using photos to assess, manage and document wounds. 16 , 18 , 19 The wound photo can be checked immediately, is readily available for viewing on a computer screen, and can easily be shared among clinicians and printed if required for hard‐copy records.
There are several problems associated with wound assessment and the use of wound photography for assessment. First, the wound assessment process is subjective, given that it is influenced by the clinician's experience. The assessment of wound dimensions varies between clinicians even when a standard tape measure is used because there is often no clear definitive wound edge and the pinpointing of an edge from which to judge width or length is subjective. Second, the type of camera used to capture wound images and the way the camera is positioned can affect the wound picture, creating further variation in wound dimension measures or the ‘look’ of a wound. Last, the steps required to upload and transfer images can breach hospital policy and privacy regulations. 20
Recent advances in wound photography, such as digital wound applications, have improved the accuracy of wound care documentation, leading to improved wound management and patient outcomes. 13 , 14 , 15 , 17 Digital wound applications downloaded to a smartphone are capable of performing real‐time wound analyses and tracking through image capture. Certain applications have algorithms and clinical decision‐support tools to assist in determining the best treatment options, the type of wound products to use, the tracking of the wound healing progression and the next steps to take. These technologies for wound care have been developed and used for a number of years in Europe, the United States, Canada and the United Kingdom. 21 , 22 , 23 , 24 Their use is also understood to be in the Australian context; however, we could not identify any literature reporting digital apps for an extensive range of wound types. Some studies have reported single wound types such as diabetic foot ulcers. 25
A major metropolitan quaternary health service in New South Wales, Australia conducted a market analysis and a review of digital applications for wound management. The Tissue Analytics digital application (TA app) met all requirements necessary to meet the health service's needs including wound image capture, eMR integration, aggregated wound data, telehealth integration and clinical decision‐support capability such as an algorithm that provides clinicians with treatment options. Tissue Analytics application is a machine learning application, which fits under the overall artificial intelligence (AI) umbrella; AI describes any task automated by a machine/computer (eg, a robotic arm executing a simple up‐and‐down movement), whereas machine learning specifically describes software systems that are learning and improving from data. 26 The aim of this study was to evaluate the usability and effectiveness of the TA app to improve wound assessment and management.
2. METHODS
2.1. Study design
This study used a quasi‐experimental design to evaluate the usability and effectiveness of the TA app where clinicians used the TA app for patient wound assessment and managment from June to October 2020, the data were compared with a historical patient group who received standard wound assessment and management (December 2019 to March 2020) (Figure 1). Patients using the TA app at home (patient interface) were assigned in mid July 2020. Owing to the coronavirus disease (COVID‐19) pandemic, the study paused in March 2020 but then restarted immediately after 3 weeks. In addition, patients were not enrolled to use the patient interface until July 2020 because the patient interface software was not available for download in Australia.
FIGURE 1.
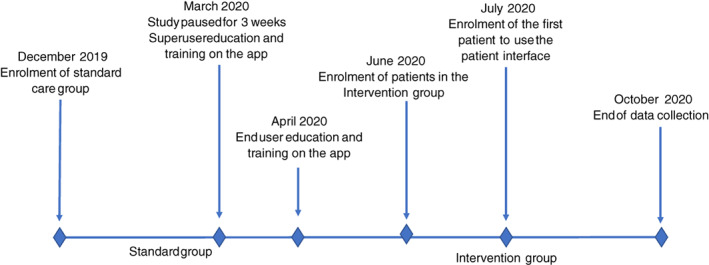
Timeline and study design
2.2. Setting
We conducted this study in four settings in one health service in the state of New South Wales, Australia. The health service is a large urban setting that provides primary, secondary and tertiary care to a local population of 700 000 people. Three study settings were in a quaternary hospital: an aged care ward, a colorectal ward and an outpatient dermatology clinic. The hospital is an 800‐bed major referral hospital that provides services for many specialist areas. The aged care and colorectal ward comprise 28 to 30 beds and have a mean occupancy rate of 93.59% and 98.08%, respectively. The fourth study setting was primary care community services across the health service.
2.3. Sample
2.3.1. Patients
Patients with a wound(s) and aged above 18 years were invited to participate in the study to have their wound care managed using the TA app. Patients were excluded if they: (a) had a diagnosed non‐healing wound (eg, palliative, malignant or fungating tumours; and wounds with a blind‐ended track, such as pilonidal sinus); (b) had a wound that required specialised treatment, such as burn/scalds; or (c) had a superficial fast‐healing wound, for example superficial lacerations.
2.3.2. Clinicians
A purposive sample of 13 clinicians—11 nurses and two doctors—were recruited. These 13 clinicians were trained on the TA app and used the app with their patients.
2.3.3. Intervention
The TA app is a cloud‐based application to measure, analyse and treat wounds. The TA app is designed to facilitate patient wound care delivery using artificial intelligence‐based technology to support clinical decision‐making. By capturing an image of the wound, the TA app analyses its dimensions and perimeters, surface area and tissue composition and presents augmented visual images (Figure 2). To facilitate the success of the intervention, we undertook careful planning, and codesigned the clinical model and technology solution through broad collaboration with many key stakeholders, including the TA app developers, system architects and clinicians, as well as consultation with statewide government agencies.
FIGURE 2.
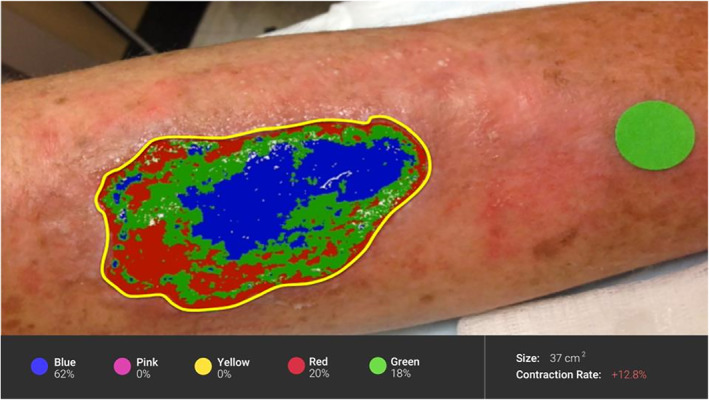
The Tissue Analytics app wound analysis
For this study, we tested a standalone solution that was not integrated with eMR, whereby the image and structured report generated from the TA app were to be uploaded to the eMR via the medical records department. The TA app was available for any smartphone and Android device with an integrated camera. No additional optics or hardware were needed to run the app. The TA app comprises two components, each with a separate login, a clinician interface (Figure 3) and a patient interface (Figure 4). Clinicians used the clinician interface to take photos and document wound assessment and management. The patient interface was used by patients who care for their wound at home and require regular monitoring by clinicians. The patient interface was linked to the clinician interface for oversight.
FIGURE 3.
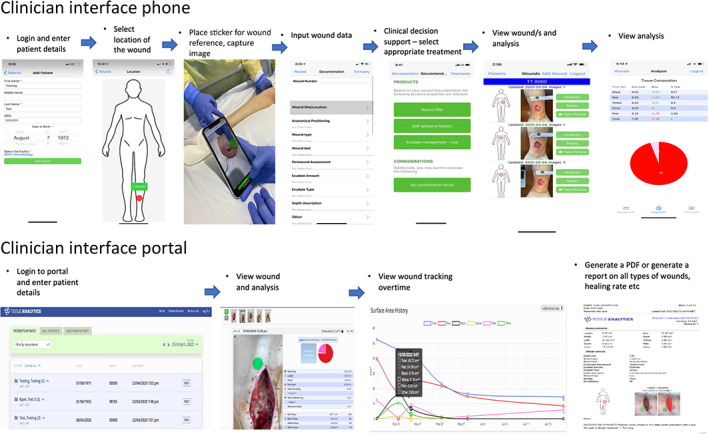
Clinician interface
FIGURE 4.
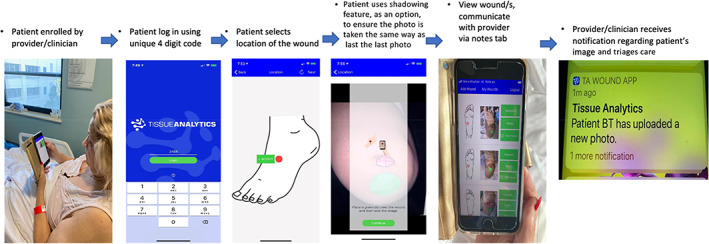
Patient interface
2.4. Standard practice
The health service uses wound iView in the eMR for wound documentation. Wound iView is a platform for wound documentation in the eMR. Wound iView at present has wound documentation fields, such as wound location, colour and exudate, with drop‐down options to document wound assessment. Wound iView does not have inbuilt functionality to store visual images; therefore, the wound information is stored only as text. Clinicians take photos with either a single lens reflex camera or a work mobile device. The photos are then uploaded onto a secure password‐protected drive to which only senior wound care nurse consultants have access. Wound iView in the eMR has the functionality for wound assessment and management documentation for patients with one wound.
2.5. Outcome measures
The outcome measures of this study were: (a) patient and clinician usability, and acceptability of the TA app; (b) reduction in wound size at the point of discharge (inpatient cohort) and at the end of 3 months after enrolment (community and outpatient cohort); (c) completeness of wound‐related documentation determined by the documentation of pain, wound size, exudate, odour and a management schedule.
2.6. Instruments
2.6.1. Clinicians
A clinician survey (APPENDIX 1) was developed by the study investigators (M.B.J., A.J., F.C.) in consultation with researchers and senior clinicians using the REDCap system (a system for building and managing online surveys and research data) hosted by the local health service. 27 The clinician survey included 21 questions regarding user experience in the following categories: usability and easiness (seven items), image capture (four items), benefits to assessment and management (three items), benefits to communication and continuity (three items), benefits to workflow and time to wound assessment (three items) and overall perceived value (one item). The survey used a 10‐point Likert scale, with scores ranging from 0 to 10 (higher scores indicating stronger agreeance), with items 3, 5, 7, 9, 11, 14 and 16 being reverse scored. The survey was reviewed for face validity by wound care expert clinicians and pilot tested on five clinicians. No changes were required. To further explore clinician usability and acceptability, focus group interviews were conducted with clinicians.
2.6.2. Patients
A patient data collection tool was developed by the lead authors (M.B.J., A.J., F.C.) in consultation with wound care expert clinicians and reviewed for face validity by senior registered nurses (RNs) and senior researchers. The tool captured patient demographic data, diagnoses and comorbidities; wound aetiology; wound size percentage decrease; the completeness of wound documentation including data on pain, exudate, odour, size, wound management goal, wound assessment schedule and potential saving in patient travel‐related time. For outcome measures of usability and acceptability, semi‐structured in‐depth interviews were conducted with patients via telephone.
2.7. Procedure
2.7.1. Clinicians
Clinicians were trained by the application vendor on the use of the TA app prior to enrolment. They were instructed to download the TA app on their work smartphone. Two training sessions were held (Box 1). Out of 13 clinicians, one designated Skin Integrity Nurse Consultant (T.L) was assigned as superuser. The lead author was also assigned as the superuser for oversight and coordinatinon. The remaining clinicians were assigned as end users.
BOX 1. Training content for superusers and end users.
| Training on how to | Superuser | End user |
|---|---|---|
| Use administrative tools (create users and passwords) | √ | ‐ |
| Create and generate system, health service reports | √ | ‐ |
| Train the trainer | √ | ‐ |
| Overview of the TA app | √ | √ |
| Understand the TA app functionalities and its scope | √ | √ |
| Use the app and desktop portal | √ | √ |
| Impute and amend wound information | √ | √ |
| Use the clinical decision support | √ | √ |
| Generate a wound report | √ | √ |
| Enrol patients, assist in the use of the patient interface | √ | √ |
The TA app developers conducted a 4‐hour virtual session for superusers and 1‐hour session for end users. The end‐user virtual training sessions were followed by 2‐hour face‐to‐face sessions with the superusers. The investigators assembled a training resource pack, including an information brochure on the TA app for both clinicians and patients, step‐by‐step instructions and a cheat sheet with frequently asked questions. At the end of the training session, clinicians were provided with the training resource pack and were instructed to raise any questions with the investigators, who would then triangulate issues with the TA support team. For progress and monitoring, the investigators set up 15‐minute virtual catchups with clinicians twice a week to discuss progress and raise any issues related to the app and the clinical workflow for the duration of the study.
All clinicians testing the TA app were invited via email to complete the survey online and to participate in the focus groups 4 months after the TA app implementation. They were given a month to complete the survey and were sent two follow‐up emails in this period to remind and encourage them to complete it.
Semi‐structured focus group interviews, which lasted between 20 and 40 minutes, were conducted with clinicians in a quiet location of their choice. They were given the opportunity to share their views on the TA app: its ease of use, its impact on wound documentation, their experience with the TA app, TA app incorporation into the workflow and its effectiveness in assisting with wound management decisions. Focus group interviews were audio‐recorded, professionally transcribed and de‐identified.
2.7.2. Patients
Data on patients were collected via their medical records and were compared with data from standard care patients collected prior to the TA app implementation. All patient data were de‐identified when recorded and entered onto a secure web‐based platform used to store data research (REDCap). 27
The clinician users assisted the patients using the patient interface to download the TA app on their phone and instructed them on the use of the app. The patients were provided with a written information sheet and the contact details of their clinicians for questions. When patients used the patient interface to photograph their wound and input wound information, the treating clinicians received a notification to review the report and triage as appropriate.
All patients using the TA app were invited after discharge, via a follow‐up call from an investigator, to participate in a brief (15‐minute) semi‐structured interview. The interviews were conducted via telephone. Interviews were audio‐recorded, professionally transcribed and de‐identified.
2.7.3. Data analysis
All data were entered and analysed using IBM SPSS Statistics V24 (IBM Corps, 2013, Armonk, NY: IBM Corp). A convenience sampling was used for patients, with no a priori sample size calculation. Patient demographic and clinical data were analysed descriptively using frequencies and percentages, means and standard deviations (SD) and compared using independent t‐tests for continuous data and chi‐square tests of independence for categorical data. Chi‐square tests of independence were conducted to examine whether there was a statistically significant difference between cohorts in wound documentation practice: pain, exudate, odour, size, wound care plan, wound assessment schedule and types of dressing applied. Wound percentage decrease was not able to be compared between groups as this outcome was not measured in the standard care approach. The first and the last wound area measurements were used to calculate the percentage change in area.
Clinician satisfaction with TA was calculated by adding the scores of each question of the survey and then calculating the mean of each category. The higher score reflected greater satisfaction. Transcripts of clinician focus groups and patient individual interviews were uploaded into NVivo 11 software for analysis. Thematic analysis 28 was conducted in six steps: familiarisation with data; generation of initial codes; search for themes; review of themes; definition and naming of themes; and preparation of a written report. Data analysis was undertaken by four team members (M.B.J., F.C., A.F., S.R.) independently to ensure rigour.
The potential travel time of patients was estimated using Google Maps. The patient's address and the hospital's address were used to calculate the time using Google Maps. The time of travel was set at 12 pm. The mean travel time was calculated using the minimum and the maximum travel time provided by Google Maps. The average fuel cost of 122.6 c/L over the period of the study was used to calculate the cost of travel.
2.7.4. Ethical consideration
The study was conducted in accordance with the National Health and Medical Research Council's (NHMRC) National Statement on Ethical Conduct in Human Research. Ethics approval was obtained from the Ethics Review Committee (RPAH Zone) X19‐0307 and 2019/ETH12459. Patient participants who used the app were invited to participate in an interview and clinician participants were invited to participate in an interview and in clinician focus groups. Fully signed consent was obtained from both patient and clinician participants. Confidentiality was ensured by assigning each participant a unique identifier and de‐identifying data when transferred into a secure base. Re‐identifiable coded data were stored on our secure online REDCap database, accessible only by study investigators. Clinicians anonymously completed an electronic satisfaction survey, where the completed return of the survey signified consent.
3. RESULTS
3.1. Demographic and baseline characteristics
A total of 290 patients were enrolled in this study: 166 patients in the standard group and 124 in the intervention group (Figure 5).
FIGURE 5.
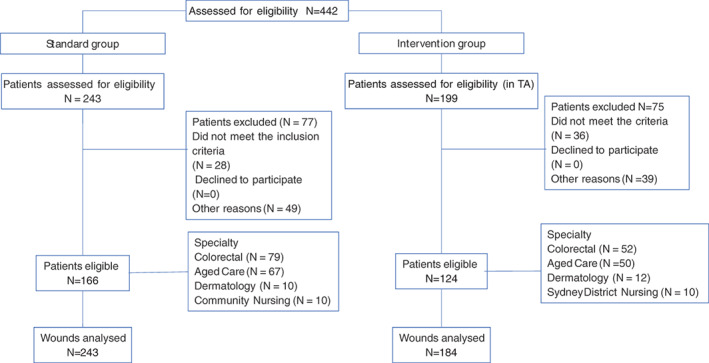
Schema of patient flow in the study
The TA app clinician interface was trialled by 13 clinicians on 124 patients with 184 wounds and the outcomes compared with a standard group of 166 patients with 243 wounds who were treated with standard care. There was no statistically significant difference between the two groups by age, gender or study settings. The standard care group had statistically significant higher proportions of wound types such as blister/abrasion/skin tear and lower proportion of ulcers than the intervention group (based on adjusted standardised residuals >2). The demographic and clinical characteristics of both groups are presented in Table 1.
TABLE 1.
Demographic and clinical characteristics of patients
| Standard care N = 166 | Intervention N = 124 | Mean Diff a (95% CI) a P value | |
|---|---|---|---|
| Gender | |||
| Male | 85 (51.2%) | 65 (52.4%) | 0.84 b |
| Female | 81 (48.8%) | 59 (47.6%) | |
| Age mean (SD) [range] | 72.01 (18.46) [24‐103] | 69.87 (18.66) [23‐96] | 2.14 c (−2.20, 6.47) 0.33 |
| Clinical area | |||
| Ward | 146 (18.46%) | 102 (82.3%) | .173 b |
| Community and dermatology | 20 (12.0%) | 22 (17.7%) | |
| Type of wound d | |||
| Blister/abrasion/skin tear | 68 (28.0%) e | 24 (13.0%) e | <.001 b |
| Ulcers (arterial, venous, diabetic foot) | 57 (23.5%) f | 88 (47.8%) f | |
| Surgical dehiscence/postoperative | 83 (34.2%) | 48 (26.1%) | |
| Traumatic wound/laceration | 8 (3.3) | 9 (4.9%) | |
| Dermatological condition/cellulitis | 15 (6.2%) | 11 (6.0%) | |
| Other | 12 (4.9%) | 4 (2.2%) | |
For difference in means only.
Chi‐square test.
Independent t‐test.
Total number of wounds: Standard care n = 243; Intervention n = 184.
Difference in proportions between standard and intervention.
Difference in proportions between standard and intervention.
Of the 124 participants in the intervention group, 13 trialled the patient interface, which provided data to calculate the potential travel‐related time, and cost.
3.2. Feasibility, usability and acceptability of the TA app
3.2.1. Clinician survey results
The survey was distributed to the 13 participant clinicians, among whom 10 completed it, yielding a response rate of 77%. Most clinicians strongly agreed that the TA app was easy to learn and to use (Table 2). The highest mean item score was for overall perceived value (8.44) and the lowest was for ease of use (6.92).
TABLE 2.
Clinician survey TA app results
| Category | Mean |
|---|---|
| Image capture | 7.33 |
| Ease of use | 6.92 |
| Benefits to patient assessment and management | 8 |
| Benefits to communication and continuity | 8.19 |
| Benefits to workflow and time to wound assessment | 7.41 |
| Overall perceived value of the TA app | 8.44 |
3.2.2. Clinician focus groups and patient interviews
Data were collected from four patients individually and 13 clinicians in five focus groups. Table 3 gives an overview of participating clinicians' characteristics.
TABLE 3.
Overview of participating clinicians' characteristics
| Colorectal surgery | Acute aged care | Dermatology outpatient | Community nursing | Wound service | |
|---|---|---|---|---|---|
| Registered nurse a | 2 | 3 | 2 | 3 | 1 |
| Doctor b | 2 | ||||
| Male | 2 | 1 | |||
| Female | 2 | 3 | 2 | 3 |
Included senior nursing leads, nurse educators and unit managers.
Included a senior geriatric specialist and a registrar (a doctor receiving advanced training in a specialist field of medicine).
Two major themes emerged from the data: Connecting treatment and continuity of care and Engaging with a new technology.
3.3. Connecting treatment and continuity of care
Patients were unanimous in their belief that the TA app provided benefits to their wound healing and communication with clinicians. The importance of clinician engagement and continuity of care from the hospital to the community was highlighted:
So, we took weekly pictures of it, or whenever I would get it dressed to get a new dressing done. And I found that good, I found it good for like, seeing the progress of it or seeing, like how far the wound had progressed or whatever, in terms of healing. (Patient participant 1)
So it gave me a level of comfort that it's improving, it's improving by a certain percentage. (Patient participant 4)
From the clinician's and the patient's perspective, the use of the TA app increased patients' engagement and their own care and security in knowing that they were in constant contact with their provider:
Every time we change the dressing, the patient will ask, ‘Can I have a look what it looks like now?’. (Focus group 2, RN 4)
I mean, looking at the patient side of things, it really has made a difference in terms of patients' confidence and their sense of security … so they feel confident to go home and do that, basically without having a clinician with them. (Focus group 5, RN 10)
[At home,] I feel like a doctor is right alongside me and they can look at it and analyse it and it's like having a doctor in another room. You don't feel isolated, and you feel that you're not on your own. (Patient participant 2)
The importance of communication and continuity of care was reinforced by all clinicians. Clinicians indicated that using the TA app in practice could improve communication between clinicians, reduce discomfort for the patient and allow the wound to be viewed remotely by the doctor, which reduced the unnecessary early removal of the dressing:
So, it's really good, yeah, if the patient comes from the community into hospital, we can see what the plan was in the community and vice versa. So, yeah, good consistency in that way. (Focus group 1, RN 1)
This remote viewing, according to another clinician participant, not only encourages communication but also reduces resource wastage:
It allows the clinician to actually review the wound remotely … at the moment, the process would be that we would contact the doctor to come and review the wound and, sometimes, they get caught up on a round and are unable to come and review the wound; then, the dressing gets done. (Focus group 2, RN 5)
Clinician participants indicated the valuable role of the TA app in sharing management plans, providing objective wound measurement and ensuring efficient wound documentation. The app allowed them to efficiently document specific information, such as the types of tissues, exudate and the types of dressings applied, in a structured format:
Also looking at wound management, and … the most appropriate dressing. In that sense alone, that's [TA app] very helpful for nursing staff or medical staff as well, both in an inpatient unit and outpatient unit. (Focus group 4, Doctor 1)
Sometimes, it's quite hard to explain what you can see [in the wounds], and then, it's quite hard to remember which word to use to explain tissue type in a wound. Because on the app, everything is pretty much there … (Focus group 2, RN 4)
So, as a doctor using the app, I found it overall useful – a useful way of collecting good data and documenting wounds and adding good photographic documentation as well. (Focus group 5, Doctor 2)
Virtual communication and seeking expert advice were other advantages identified by clinician participants. They suggested that these enhanced efficiency, communication and continuity of care for patients:
It will connect us with community nurses, with GP services and keep us connected with patients if they fall through the loops. For example, we get patients that come here [in hospital], and then, if they discharge and we can't keep track of them, it will help us keep connected with continuing of care with their treatment. (Focus group 3, RN 7)
One clinician participant suggested that the TA app offered health care providers the ability to manage wound‐related liability and dispute by recording an objective wound measurement on discharging or transferring the patient to another facility.
At the moment, we would often send these patients off to other facilities … sometimes, because the documentation was so poor, we do often get a few calls back saying, ‘Well, this wasn't here before. It wasn't as extensive’ … it could be quite useful, particularly if the patient is going on to other facilities … I think it provides us with a sort of evidence of what we've seen as well. (Focus Group 4, RN 8)
Clinicians also reported that that using the TA app increased patient adherence to the wound care plan, which facilitated wound healing:
Yeah, especially with [patient's name] … before, she refused to reposition. … And then, when we showed her how bad it was and then the progression … Since then, she repositioned herself. (Focus group 2, RN 4)
3.4. Engaging with a new technology
Engaging with new technology can be challenging. Given that clinicians and patients were introduced to this new technology at similar times, it was unsurprising that they gave positive feedback as well as identified some problem areas.
Environmental considerations, both for clinicians and patients, need to be explored and understood when engaging with a new technology. Several patient participants commented on the advantages of being in their own home environment, regarding this as a positive element of their recovery:
It was easy for me to do that from home and for my wife to actually do the wound itself … and for us to send those photos … it was very convenient for us, otherwise we would have had to stay in Sydney [metropolitan]. For us being at Dubbo [rural], it made it so convenient for us and I had no issue with carrying it around in my pocket and I reckon it's the best thing that's happened. (Patient participant 3)
The advantages included ease of movement, the opportunity to adhere to their normal meal‐time routines and the ability to have better sleep at home. Most patient participants also believed that using the TA app enabled them to manage their own wound care under supervision, which was convenient and saved them travel time:
I think it probably saves a couple of trips, especially if I was concerned about something. I'd just take a photo, and then send it through, and then he [wound care nurse specialist] can mark notes on it. So, I guess it saves me from going to the doctors … It saves those trips. (Patient participant 3)
However, clinician participants noted difficulties in the community, such as inadequate lighting that inhibited them from obtaining a good‐quality photograph:
We have no control over the dark dingy room or the over‐brightly lit room and trying to reposition people in the right spot and the frustrations that that can develop into. (Focus group 1, RN 1).
They also mentioned problems with the correct positioning of a patient if the wound was in a ‘hard‐to‐reach’ area. Similarly, patients had difficulties photographing their own wound, depending on the part of anatomy:
The clientele that we have are quite elderly, so not a lot of them are tech savvy and depending on where their wound is, they might not be able to get a picture of it themselves or have someone be there to take it. (Focus group 1, RN 2)
Another environmental consideration that several hospital clinician participants highlighted was infection control. Problems were identified with infection control practices and picture clarity when using personal phones; with covering phones with a plastic sleeve for protection; and about the need to take a photo in a room where a patient had an infectious disease:
I try to use the plastic before the sleeve, but it doesn't give you a clear photo. (Focus group 2, RN 5)
I think the other biggest thing for me was infection control, so having the phone in an infectious room as well is another challenge. (Focus group 4, RN 9)
Participants were found to have different expectations, experiences and needs when using the TA app. Patients found the application easy to use, taking little time except when uploading a photo, which was noted to be a bit slow. For clinicians, the process of logging in and inputting patient information was described as, at times, time‐consuming:
I find that it's quite time‐consuming to read the information. Not that it's not good, it's fantastic, but I don't know how well people sit to do that at the point of call. (Focus group 1, RN 3)
It was quite an easy app to actually use in terms of functionality, but it was a bit time‐consuming and then a couple of things also make it a bit … Even just logging in takes a good minute or so because you've got to put in email whatever, and then, it logs out. (Focus group 5, Doctor 2)
Clinicians agreed that the TA app was useful for clinical assessment and for the real‐time tracking and monitoring of wounds; however, participants often did not use the clinical decision support provided by the TA app algorithm because they felt they already had access to expert advice by doctors and wound care specialists. Several clinician participants suggested that the use of the clinical decision support component of the TA app could be beneficial for inexperienced nurses, including new graduate nurses:
There's a lot of new grads in the hospitals, and it [TA] also can help with that. If they haven't got the support, this app also can give you recommendations of what to put on the dressings. It then analyses the wound and can give the nurse the option of dressings to put on that wound. (Focus group 3, RN 7)
They indicated that it could also improve wound management, given that effective care could be initiated immediately rather than waiting for advice from the Wound Clinical Nurse Consultant:
Yes, because it [TA app] gives you advice and recommendations on what sort of dressing. At least something's being done, just putting a simple dressing … because in that short 2 days, there's a lot of things that can happen in that wound. (Focus group 2, RN 4)
3.5. Reduction in wound size
Fifty‐two patients (42%) in the intervention group had multiple wounds. In this group, the size of 132 wounds was measured more than once by using the app; 101 out of 132 wounds over an average of 36.47 days (SD 41.76) improved, with a mean reduction of 54.0% (SD 31.60) in wound size. The breakdown of the wound size percentage change by wound type is presented in Table 4.
TABLE 4.
Wound area percentage decrease or increase by wound type at time of discharge in intervention group
| Improved (n) | Reduction in wound size area (%) a Mean (SD) | Deteriorated (n) | Increase in wound size area (%) a Mean (SD) | |
|---|---|---|---|---|
| Blister/abrasion/skin tear | 7 | 60.23 (36.83) | 1 | 1.13 |
| Pressure injury/ulcers | 44 | 41.99 (29.12) | 14 | 82.21 (81.59) |
| Surgical dehiscence/postoperative | 33 | 66.88 (29.27) | 9 | 86.47 (103.02) |
| Traumatic wound/laceration | 1 | 99.95 | 3 | 26.95 (19.66) |
| Dermatological condition, ASD, cellulitis | 7 | 59.03 (34.63) | 3 | 142.24 (65.29) |
| Miscellaneous/unknown aetiology | 9 | 51.47 (27.85) | 1 | 73.86 |
| Total | 101 | 54.00 (31.61) | 31 | 81.03 (83.17) |
Percentage change calculated as ([Original area measurement − final area measurement]/original measurement) × 100.
3.6. Completeness of wound‐related documentation
The use of the TA app by clinicians significantly increased the completeness of documentation compared with standard care (Table 5). Completeness of the documentation was based on the number of dressing changes.
TABLE 5.
Comparison of completeness of wound documentation a
| Standard care N = 935 a n% | Post (app used) N = 447 a N% | Significance | % Improvement (95% Cl) | |
|---|---|---|---|---|
| Pain | 80 (8.6%) | 185 (41.4%) | P < .001 | 32.8 (28.4, 37.2) |
| Size | 78 (8.3%) | 447 (100.0%) | P < .001 | 91.7 (86.2, 97.2) |
| Exudate | 298 (31.9%) | 390 (87.2%) | P < .001 | 55.2 (49.7, 60.9) |
| Odour | 17 (1.8%) | 181 (40.5%) | P < .001 | 38.7 (34.8, 42.7) |
| Wound management schedule | 278 (30.2%) | 162 (36.3%) | P = .020 | 6.1 (.80, 11.4) |
| ≥2 items documented | 244 (24.0%) | 418 (93.5%) | P < .001 | 69.5 (63.9, 72.1) |
Sample sizes for this outcome are based on the number of dressing changes documented.
In particular, the recording of wound size increased from 8.3% completion rate in the standard care group to 100% completion rate in the intervention group and that for exudate increased from 31.9% in the standard care group to 87.2% with the use of the TA app.
3.7. Potential travel‐related time avoided
Out of 13 patients who used the TA app, travel related data were collected on 12 patients. Nine patients used the TA app patient interface from their home in the Sydney metropolitan area and three patients used the patient interface from their rural home. Patients used the TA app on average, 11.2 times (range 4‐21 times) over an average period of 45.3 days (range 12‐104 days).
The travel‐related fuel cost to a patient living in metropolitan Sydney was on average $4.54 ($0.42‐$11.78) for every visit to the hospital and for rural patients was on average $72.90 ($16.20‐$124.00) (Table 6).
TABLE 6.
Patient travel time and cost saved
| Average round trip saved | Average travel time saved | Average fuel cost | |
|---|---|---|---|
| Metropolitan patients (n = 9) | |||
| Travel by car (n = 7) | 29.7 kms (Range 4.4‐109.2 kms) | 35.9 minutes (Range 8.15‐68.3 minutes) | $4.54 (Range $0.42‐$11.78) |
| Public transport (n = 2) | Not applicable | 14 minutes | Not applicable |
| Rural patients (n = 3) | |||
| Travel by car (n = 3) | 585 kms (Range 177‐794 kms) | 224 minutes (Range 82.5‐316.5 minutes) | $72.90 (Range $16.20‐$124.00) |
| Potentially a saving of $552.40 (Range $60.91‐$956.13) per month in travel expense | |||
4. DISCUSSION
This study demonstrated a significant improvement in the completeness of wound documentation. This has important clinical implications because it demonstrates improvements in objective and quantitative wound information and consistency of documented care using the TA app. Currently, in our health service, clinicians document their wound assessments in the progress notes section of the eMR, a variable and often inconsistent approach to documentation. The TA app provided standardised key information for all wounds that link to the patient's eMR. In addition, this information was available across both community and inpatient settings.
The TA app performed well on measures of functionality and user experience. Clinicians strongly agreed that the TA app was easy to learn, particularly with respect to assessment, clinical tracking and monitoring of the wound. This finding is consistent with several previous studies testing wound applications to improve wound assessment and monitoring. 29 , 30 , 31 , 32 Currently, across many health services in Australia, there are no databases or systems that allow for monitoring, tracking or benchmarking of wounds. We found the TA app facilitated clinical workflows and improved continuity of patient care and clinician communication.
Accurate wound documentation is an essential part of handover and is important for effective wound management. 33 , 34 Similar to our study, Klinker, Wiesche and Krcmar (2020) found that their wound app prototype had the potential for improving the wound documentation process. 29 Their smart glass wound care app allowed for rapid objective hands‐free wound documentation. In our study, clinicians reported that the TA app provided an instantaneous objective wound size measurement, which gave a reliable and effective record of the patient's wound and was a powerful tool that enabled them to see wound progression or deterioration. Shamloul, Ghias and Khachemoune (2019), in their review on digital technologies, concluded that mobile applications and digital applications potentially lead to prompt, easy and accurate wound assessment for both the clinician and the patient. Accurate and easy assessment facilitates effective wound management, which improves patient wound outcomes. 30 Objective wound documentation also facilitates patient continuity of care, as reported by our clinician participants in this study.
Clinicians and patients in this study valued the TA app providing real‐time information, its ease of use and efficiency in wound assessment and image capture. This enabled patients to view the progress of their wound instantaneously after a photo was taken. Clinicians reported that because of this, patients were more engaged in their care and were more adherent to the wound management regime. Findings from a systematic review on engaging patients to improve quality of care suggest that patients feel empowered by being involved in their care and that it increases their self‐esteem. 35 Further, a recent consensus document by the World Union of Wound Healing Societies on patient engagement and wound care indicated that involving patients in their wound care can positively influence wound healing. 36
Consistent with previous work on virtual health care platforms, 37 , 38 , 39 our study demonstrated that the TA app enabled patient wound care through virtual connection to a clinician. Strong patient satisfaction was reported through interviews. Patients were excited to use the TA app and commented on the advantages of receiving care and being in their own home environment, regarding this as a positive element of their recovery. Further, patients commented on feeling safe, as though the provider was within arm's length should wound help be required. The clinicians perceived that the TA app made it easier to communicate with the patient about their wound care and that the patient did not have to travel to receive the same level of care. Virtual patient care facilitates prompt treatment and has the potential to prevent negative patient outcomes. 37 , 38 , 39
When interventions are implemented in complex settings, such as a health service setting, facilitators and barriers are often encountered, which can directly affect patient health outcomes. 40 , 41 , 42 In this instance, barriers to wound care can potentially lead to wound breakdown or prolonged wound healing. Acknowledging the barriers and facilitators that were reported by clinicians and patients in this study, the intervention (the TA app) did not have any negative impact on patient outcomes or on wound healing. In fact, in this study, the app potentially enabled patients to continue to be treated effectively despite outpatient appointments having to be cancelled because of COVID‐19. Further, patients using the app reported the benefits of the app in facilitating their wound healing. Patients' wounds continued to heal, reducing in percentage size by over half (54%). The approach taken in this study, namely careful planning, and broad collaboration with key stakeholders, ensured the reduction of any unintended negative effects and promoted positive patient experiences.
Although it was not the focus of this paper, the time and cost saved by the patient needs to be noted, especially in the context of prompt access to care. Studies have reported that if a patient cannot access timely wound care owing to costs and delays, it can lead to wound breakdown or prolonged healing. 43 , 44 In this study, virtual care via the TA app led to travel cost savings for patients. Patient also reported the benefits of not having to travel and being able to communicate with wound care nurse specialists, which made care very convenient.
Last, the TA app facilitated wound care during COVID‐19. Most projects in our health service ceased because of COVID‐19 priorities. However, telehealth and telemedicine consults increased during the COVID‐19 pandemic. The TA app during this period allowed for virtual wound care and reduced face‐to‐face visits between staff and patients, as well as clinician face‐to‐face consultations on wound care. The process of setting up the TA app in our health service so that it was more appropriate for our population was an iterative as well as a positive process between our health service and information technology team and the TA team in the United States. The responsiveness to clinician experience in the early part of the implementation was critical to the success of the implementation of the app.
The use of the TA app during COVID has led to the establishment of the Virtual Wound Care Command Centre and further research into this area, expanding on the work of this study. The Virtual Wound Care Command Centre research will investigate the benefits of having a centralised specialist wound care service using a digital wound application for remote timely intervention for patients in the community, to ensure they receive world‐class wound care irrespective of their physical location.
This study has acknowledged limitations. The purposive sampling of 13 clinicians in this study introduces a degree of bias and limits the generalisability of the results. Since we recruited patients from four health settings in one metropolitan health service, future studies involving the recruitment of clinicians and patients from other settings, such as residential aged care facilities and general practice, may assist in determining whether similar benefits are observed in different specialties to expand on this study's findings. The use of a historical control (the standard care group) as a non‐randomised comparator in our study may have introduced bias and increased the type 1 error rate. However, we used matching of study design and demographic parameters to incorporate historical data in a supplementary manner for reducing the number of concurrent control subjects required and the recruitment burden. The retrospective review of medical record notes for patients in the standard group limits our ability to understand whether improvements in wound healing were directly related to the intervention, the TA app. However, over the past decades, with the advent of eMR, considerable investments have been made in high‐quality, curated and trusted clinical data.
5. CONCLUSION
This is the first Australian study to report a wide‐ranging wound care service using a digital application that provides real‐time wound data with an interface for communication between the patient and the clinician, and clinicians in a hospital, community and outpatient setting. The use of the TA app demonstrated positive documentation and data management of wound care, clinician‐and‐patient communication and patient travel time and costs. This study demonstrated the feasibility of the use of the TA app in acute, community and outpatient settings. The TA app facilitated remote monitoring via telemedicine for patients, thus reducing face‐to‐face visits and travel time. As an innovative application that supports clinicians and patients in wound care, the TA app has the potential to improve patient wound outcomes. The findings of this study will be used to guide further application in other settings and scale up across the health service and eventually the state.
CONFLICT OF INTEREST
The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
ACKNOWLEDGEMENTS
We thank all the healthcare staff who were part of the study for their time, effort and enthusiasm in adopting this new application to improve wound care. In particular, Gina Tsaprounis, System Architect, Sydney Local Health District and John Sheedy, eHealth. We wish to thank our Executive Sponsor, Ivanka Komusanac for her ongoing support of this project. We thank Tissue Analytics for subsidising the cost of the application and providing ongoing product training, an overwhelming amount of support and troubleshooting. Tissue Analytics did not have any input into the design, conduct, analysis or write‐up of this study. This study was supported by a grant from eHealth New South Wales, which is the electronic management of health information. eHealth NSW has been established as a statewide organisation within the New South Wales Ministry of Health to provide statewide leadership on the shape, delivery and management of ICT‐led and digital healthcare.
APPENDIX 1. CLINICIAN SATISFACTION SURVEY
| Item | Question | Domain |
|---|---|---|
| 1 | I would imagine that most people would learn to use the Tissue Analytics digital application easily | Usability and easiness |
| 2 | Taking an image of the wound with the mobile app is a simple task | Image capture |
| 3 | It is difficult to use the ‘retrace feature’ on the Tissue Analytics desktop portal to correct wound demarcation on the image | Usability and easiness |
| 4 | It is straightforward to use the ‘shadowing feature’ on the phone app to ensure | Image capture |
| 5 | The ‘clinical decision support’ feature to assist with wound product selection is not easy to use consistent image taking | Usability and easiness |
| 6 | To input information about the wound on the app, for example, odour and exudate, is a simple task | Usability and easiness |
| 7 | Generating a wound report in a PDF format is complicated | Usability and easiness |
| 8 | I can efficiently navigate the Tissue Analytics desktop portal | Usability and easiness |
| 9 | I do not think that the Tissue Analytics app improves my wound management workflow | Benefits to workflow and time to wound assessment |
| 10 | The Tissue Analytics app supports my clinical assessment of the wound | Benefits to assessment and management |
| 11 | Tissue Analytics does not play a role in improving continuity of care | Benefits for communication and continuity |
| 12 | Tissue Analytics does not guide my decision‐making for various wound types | Benefits to assessment and management |
| 13 | Tissue Analytics always saves the wound image and information I recorded without any technical issue | Benefits to workflow and time to wound assessment |
| 14 | I experienced issues with using the phone camera flash while taking a wound image | Image capture |
| 15 | The wound image and wound descriptions displayed on the mobile app screen were clear to view and read | Usability and easiness |
| 16 | Tissue Analytics does not improve my communication with other clinicians | Benefits to communication and continuity |
| 17 | Tissue Analytics assisted with my communication with the patient about their wound issues | Benefits to communication and continuity |
| 18 | Tissue Analytics freezes often | Image capture |
| 19 | Tissue Analytics allowed timely expert consultation | Benefits to workflow and time to wound assessment |
| 20 | Tissue Analytics assisted with real‐time tracking and monitoring of the wound | Benefits to assessment and management |
| 21 | Tissue Analytics is overall a valuable tool for wound assessment and management | Overall perceived value |
Barakat‐Johnson M, Jones A, Burger M, et al. Reshaping wound care: Evaluation of an artificial intelligence app to improve wound assessment and management amid the COVID‐19 pandemic. Int Wound J. 2022;19(6):1561-1577. doi: 10.1111/iwj.13755
[Correction added on 07 June 2022 after first online publication: Bora Kim was removed from the acknowledgement and has been added to the author byline due to his significant contribution to the article.]
Funding information eHealth NSW Grant
DATA AVAILABILITY STATEMENT
Author elects to not share data.
REFERENCES
- 1. Sen CK. Human wounds and its burden: an updated compendium of estimates. Adv Wound Care (New Rochelle). 2019;8(2):39‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gillespie BM, Chaboyer W, St John W, Morley N, Nieuwenhoven P. Health professionals' decision‐making in wound management: a grounded theory. J Adv Nurs. 2015;71:1238‐1248. [DOI] [PubMed] [Google Scholar]
- 3. Keast DH, Bowering CK, Evans AW, Mackean GL, Burrows C, D'Souza L. MEASURE: a proposed assessment framework for developing best practice recommendations for wound assessment. Wound Repair Regen. 2004;12(3 Suppl):S1‐S17. [DOI] [PubMed] [Google Scholar]
- 4. Coleman S, Nelson EA, Vowden P, et al. Development of a generic wound care assessment minimum data set. J Tissue Viability. 2017;26(4):226‐240. [DOI] [PubMed] [Google Scholar]
- 5. Hampton S. Wound management 4: accurate documentation and wound measurement. Nurs Times. 2015;111(48):16‐19. [PubMed] [Google Scholar]
- 6. Wounds Australia . Standards for Wound Prevention and Management. 3rd ed. Australia: Cambridge Media on behalf of Wounds Australia; 2016. [Google Scholar]
- 7. Gillespie BM, Walker R, Lin F, et al. Wound care practices across two acute care settings: a comparative study. J Clin Nurs. 2020;29(5–6):831‐839. doi: 10.1111/jocn.15135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hansen RL, Fossum M. Nursing documentation of pressure ulcers in nursing homes: comparison of record content and patient examinations. Nurs Open. 2016;3(3):159‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gillespie BM, Chaboyer W, Kang E, et al. Postsurgery wound assessment and management practices: a chart audit. J Clin Nurs. 2014;23(21‐22):3250‐61. doi: 10.1111/jocn.12574. Epub 2014 Mar 8. PMID: 24606529. [DOI] [PubMed] [Google Scholar]
- 10. Li D, Korniewicz DM. Determination of the effectiveness of electronic health records to document pressure ulcers. Medsurg Nurs. 2013;22(1):17‐25. [PubMed] [Google Scholar]
- 11. Topaz M, Ronquillo C, Peltonen LM, et al. Nurse informaticians report low satisfaction and multi‐level concerns with electronic health records: results from an international survey. AMIA Annu Symp Proc. 2016;2016:2016‐2025. [PMC free article] [PubMed] [Google Scholar]
- 12. Pacella RE, Tulleners R, Cheng Q, et al. Solutions to the chronic wounds problem in Australia: a call to action. Wound Pract Res. 2018;26(2):84‐98. [Google Scholar]
- 13. Khoo R, Jansen S. The evolving field of wound measurement techniques: a literature review. Wounds. 2016;28(6):175‐181. [PubMed] [Google Scholar]
- 14. Sirazitdinova E, Deserno TM. 3D documentation of chronic wounds using low‐cost mobile devices. Stud Health Technol Inform. 2017;245:1237. [PubMed] [Google Scholar]
- 15. Aldaz G, Shluzas LA, Pickham D, et al. Hands‐free image capture, data tagging and transfer using Google glass: a pilot study for improved wound care management. PLoS One. 2015;10(4):e0121179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang L, Pedersen PC, Strong DM, Tulu B, Agu E, Ignotz R. Smartphone‐based wound assessment system for patients with diabetes. IEEE Trans Biomed Eng. 2015;62(2):477‐488. [DOI] [PubMed] [Google Scholar]
- 17. Wang SC, Anderson JAE, Evans R, et al. Point‐of‐care wound visioning technology: reproducibility and accuracy of a wound measurement app. PLoS One. 2017;12(8):e018313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Li D, Mathews C. Automated measurement of pressure injury through image processing. J Clin Nurs. 2017;26(21–22):3564‐3575. [DOI] [PubMed] [Google Scholar]
- 19. Bavuso KM, Mar PL, Rocha RA, et al. Gap analysis and refinement recommendations of skin alteration and pressure ulcer enterprise reference models against nursing flowsheet data elements. AMIA Annu Symp Proc. 2017;2017:421‐429. [PMC free article] [PubMed] [Google Scholar]
- 20. Stevenson P, Finnane AR, Soyer HP. Teledermatology and clinical photography: safeguarding patient privacy and mitigating medico‐legal risk. Med J Aust. 2016;204(5):198‐200. [DOI] [PubMed] [Google Scholar]
- 21. Do Khac A, Jourdan C, Fazilleau S, et al. A mHealth app for pressure ulcer wound assessment in patients with spinal cord injury: clinical validation study. JMIR. 2021;9(2):e26443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang SC, Anderson JAE, Evans R, et al. Point‐of‐care wound visioning technology: reproducibility and accuracy of a wound measurement app. PLoS One. 2017;12(8):e0183139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Patel A, Irwin SL, Allam D. Developing and implementing a wound care app to support best practice for community nursing. Wounds UK. 2019;15(1):90‐95. [Google Scholar]
- 24. Moore Z, Angel D, Bjerregaard J, et al. eHealth in wound care – overview and key is‐sues to consider before implementation. Journal of Wound Care. 2015;24(5):S1‐S44. [DOI] [PubMed] [Google Scholar]
- 25. Kuang B, Pena G, Szpak Z, et al. Assessment of a smartphone‐based application for diabetic foot ulcer measurement. Wound Repair Regen. 2021;29(3):460‐465. doi: 10.1111/wrr.12905 [DOI] [PubMed] [Google Scholar]
- 26. Clark CR, Wilkins CH, Rodriguez JA, et al. Health care equity in the use of advanced analytics and artificial intelligence technologies in primary care. J Gen Intern Med. 2021;36(10):3188‐3193. doi: 10.1007/s11606-021-06846-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377‐381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Braun V, Clarke V. What can ‘thematic analysis’ offer health and wellbeing researchers? Int J Qual Stud Health Well‐Being. 2014;9(1):26152. doi: 10.3402/qhw.v9.26152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Klinker K, Wiesche M, Krcmar H. Digital transformation in health care: augmented reality for hands‐free service innovation. Inf Syst Front. 2020;22:1419‐1431. doi: 10.1007/s10796-019-09937-7 [DOI] [Google Scholar]
- 30. Shamloul N, Ghias MH, Khachemoune A. The utility of smartphone applications and technology in wound healing. Int J Low Extrem Wounds. 2019;18(3):228‐235. [DOI] [PubMed] [Google Scholar]
- 31. Naderi ZA. The use of online applications to improve chronic wound care in primary care; a literature review [internet]. 2020. DNP Qualifying Manuscripts 37. https://repository.usfca.edu/dnp_qualifying/37
- 32. Dong W, Nie LJ, Wu MJ, et al. WoundCareLog APP – a new application to record wound diagnosis and healing. Chinese J Traumatol. 2019;22(5):296‐299. doi: 10.1016/j.cjtee.2019.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ding S, Lin F, Gillespie BM. Surgical wound assessment and documentation of nurses: an integrative review. J Wound Care. 2016;25:232‐240. [DOI] [PubMed] [Google Scholar]
- 34. World Union of Wound Healing Societies . Position Document. Advances in Wound Care: the Triangle of Wound Assessment [Internet]. London: Wounds International. 2016. http://bit.ly/2Brk2uw. Accessed December 01, 2017.
- 35. Bombard Y, Baker GR, Orlando E, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13:98. doi: 10.1186/s13012-018-0784-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. World Union of Wound Healing Societies . Optimising Wound Care through Patient Engagement [Internet]. London: Wounds International. 2020. www.woundsinternational.com
- 37. Hutchings OR, Dearing C, Jagers D, et al. Virtual health care for community management of patients with COVID‐19 in Australia: observational cohort study. J Med Internet Res. 2021;23(3):e21064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ramaswamy A, Yu M, Drangsholt S, et al. Patient satisfaction with telemedicine during the COVID‐19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22(9):e20786. doi: 10.2196/20786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers' satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients' health. PLoS One. 2019;14(8):e0221848. doi: 10.1371/journal.pone.0221848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Monaghesh E, Hajizadeh A. The role of telehealth during COVID‐19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20:1193. doi: 10.1186/s12889-020-09301-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Geerligs L, Rankin NM, Shepherd HL, Butow P. Hospital‐based interventions: a systematic review of staff‐reported barriers and facilitators to implementation processes. Implement Sci. 2018;13(1):36. doi: 10.1186/s13012-018-0726-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gugglberger L. Can health promotion also do harm? Health Promot Int. 2018;33(4):557‐560. doi: 10.1093/heapro/day060 [DOI] [PubMed] [Google Scholar]
- 43. Randall S, Avramidis P, James N, Vincent A, Barakat‐Johnson M. Getting lower leg ulcer evidence into primary health care nursing practice: a case study. Wound Pract Res. 2019;27(2):78‐85. [Google Scholar]
- 44. Lindsay E, Renyi R, Wilkie P, et al. Patient‐centred care: a call to action for wound management. J Wound Care. 2017;26(11):662‐677. doi: 10.12968/jowc.2017.26.11.662 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Author elects to not share data.


