Abstract
Aim
To explore barriers to and facilitators for supporting communication with and for patients treated with invasive mechanical ventilation in the intensive care unit during the COVID‐19 pandemic.
Design
A qualitative descriptive study reported according to the Consolidated Criteria for Reporting Qualitative Research.
Methods
Adult intensive care unit patients treated with an advanced airway for mechanical ventilation, their family members and healthcare providers (nurses, intensivists and allied health) were recruited for interviews between January and April 2021. Interviews were audio‐recorded, transcribed verbatim and analysed using content analysis methods. Reported communication barriers and facilitators were mapped to the theoretical framework of acceptability to identify potentially modifiable clinical and institutional practices.
Results
We recruited 29 participants (20 healthcare providers, four patients and five family member). Provider communication barriers included isolation procedures, lack of personal protective equipment and inadequate communication tools/training, which reduced perceived communication frequency and effectiveness. Patients and families reported infrequent proactive provision of communication tools, which contributed to a crisis of unmet needs. Reported facilitators included adequate access to personal protective equipment to mitigate the risk of patient proximity and communication tools/training to improve communication effectiveness. Authentic unit leadership helped to assuage pandemic work stressors and encourage humanistic care. Our analysis indicates low acceptability of existing communication practices during the COVID‐19 pandemic and the importance of leadership to reduce the burden of communication through provision of key necessary resources.
Conclusion
COVID‐19 conditions have precipitated a communication crisis in the ICU. The results of this study have practice and policy implications and will be used to co‐design a communication intervention for use during and beyond the COVID‐19 pandemic.
Impact
The study contributes a better understanding of resources necessary to support patient communication. Results apply beyond the pandemic to routine use of infection prevention and control precautions in the intensive care unit.
1. INTRODUCTION
Intensive care unit (ICU) patients and their healthcare providers (HCPs) have persistently reported communication difficulty due to impaired vocalization associated with placement of advanced airways (e.g. endotracheal or tracheostomy tubes) for mechanical ventilation. Globally, ICU survivors have described communication impairment during mechanical ventilation as one of the most stressful and dehumanizing events of hospital admission (Baumgarten & Poulsen, 2015 ; Karlsen et al., 2019 ). Communication difficulty can result in the inability to self‐report major physical (e.g. pain, dyspnea, thirst) and psychological symptoms (e.g. sadness, fear, confusion) of critical illness and its treatment (Choi et al., 2017 ; Radtke et al., 2011 ). Unrelieved symptoms contribute to long‐term patient morbidity including depression, anxiety and post‐traumatic stress disorder, rendering communication an important target for practice improvement (Ijssennagger et al., 2018 ; Inoue et al., 2019 ; Khalaila et al., 2011 ).
ICU nurses most frequently interact with critically ill patients and require pragmatic strategies to address communication impairment. ICU nurses may also be required to guide other HCPs including allied health team members and intensivists about communication strategies and tools that match patient abilities and preferences (Istanboulian et al., 2020 ). Current recommendations include but are not limited to the use of augmentative and alternative communication (AAC). Defined as alternatives to speech, AAC consists of ‘unaided’ strategies (e.g. mouthing words and gesturing) or ‘aided’ strategies such as low‐tech (e.g. picture or word boards) and high‐tech (e.g. computer interface) devices (Augmentative and Alternative Communication, 2019 ). Prospective use of AAC is demonstrated to be effective in reducing patient communication difficulty and improving HCP satisfaction with care (Carruthers et al., 2017 ; Karlsen et al., 2019 ; Ten Hoorn et al., 2016 ; Zaga et al., 2019 ). In support of this evidence, recent research has identified the importance of all ICU HCPs having access to communication tools and training in their use (Happ et al., 2014 ; Istanboulian et al., 2020 ; Trotta et al., 2019 ) to avoid patient and HCP emotional distress (i.e. frustration, anger) over failed communication attempts (Istanboulian et al., 2020 ). The burden associated with failed communication may lead to emotional disengagement and reduced communication frequency by both patients and HCPs (Ijssennagger et al., 2018 ; Istanboulian et al., 2020 ).
In Canada and the US, to date approximately 18–28% of people with confirmed COVID‐19 infection have been reported to require ICU admission (Canada Go, 2022 ; Nguyen et al., 2021 ). Those treated with mechanical ventilation often experience a prolonged ICU admission, thereby increasing the need for consistent and effective communication support (Attaway et al., 2021 ). However to date, infection control conditions, such as those enacted during the COVID‐19 pandemic, have not been the primary context for research informing ICU communication guidance (Istanboulian et al., 2020 ). COVID‐19 infection prevention and control measures including the use of personal protective equipment (PPE) and visiting restrictions may complicate utilization of current guidance to support communication with patients (i.e. AAC) and support of communication for patients (i.e. family education in AAC) in the adult ICU (Freeman‐Sanderson et al., 2020 ; Ontario PH, 2021 ). As the pandemic presents a significant change in the global healthcare landscape, exploratory research is needed to understand barriers to and facilitators for communication among nurses, patients, family and other ICU professional stakeholders to inform practice recommendations (Akgun et al., 2020 ; Barreras‐Espinoza et al., 2021 ; Freeman‐Sanderson et al., 2020 ; Richards et al., 2021 ; Rose et al., 2021 ).
Theoretical frameworks are recommended to explore practice barriers and facilitators, and inform the design and implementation of complex interventions, such as patient communication (O'Cathain et al., 2019 ). The theoretical framework of acceptability (TFA) defines acceptability as a multifaced construct that reflects the cognitive and emotional responses of people delivering or receiving a healthcare intervention (Sekhon et al., 2017 ). The TFA includes seven constructs, namely: affective attitude, burden, ethicality, intervention coherence, opportunity costs, perceived effectiveness and self‐efficacy (Sekhon et al., 2017 ). The TFA posits that patients, families and HCPs form judgements about the acceptability of an intervention, based on anticipated or actual experience, that will impact their engagement with or commitment to the intervention. Because aspects of an intervention can be modified to increase acceptability, an important element of the present study was to identify dimensions of communication that may be amenable to improvement.
2. THE STUDY
2.1. Aim
Our aim was to explore barriers to and facilitators for supporting communication with and for mechanically ventilated adult patients admitted to ICU during the COVID‐19 pandemic according to TFA constructs.
2.1.1. Design and setting
We conducted a prospective qualitative descriptive study, which is an approach for exploring participants' perceptions of clinical processes and how they might be improved (Doyle et al., 2020 ). We recruited participants from a 17‐bed medical‐surgical ICU in a community teaching hospital in Toronto, Canada (January–April 2021) admitting COVID‐19 patients experiencing hypoxemic respiratory failure. The unit is managed under a closed intensivist model and nurses are assigned to mechanically ventilated patients in a 1:1 or 1:2 ratio. Respiratory therapists (RTs) are also present in the unit to manage ventilator support and weaning. The study unit followed COVID‐19 infection prevention and control standards set by the Government of Ontario, including the use of PPE, isolation of patients with suspected or confirmed infection and restricting family visitors except in the case of imminent death (Ontario PH, 2021 ). The Consolidated Criteria for Reporting Qualitative Research (COREQ) was used as a guide for reporting this research (Tong et al., 2007 ).
2.2. Participants
Eligible participants were: (1) patients (≥18 years of age, discharged from ICU and able to speak English) admitted to the study unit and treated with an advanced airway during the COVID‐19 pandemic; (2) family members (≥18 years of age, discharged from ICU and able to speak English) of patients admitted to the study unit; (3) HCPs including registered nurses, intensivists and allied health team members (i.e. RTs, speech and language therapists [SLP], occupational and physical therapists, registered dietitians, pharmacists, social workers, spiritual care providers) employed in the study unit during the COVID‐19 pandemic. We used convenience sampling in the study setting to recruit participants. This comprised the use of paper and electronic posters advertising the study. Patients and family were identified by HCPs on discharge from ICU and all participants were approached and consented by the principal investigator (LI).
2.2.1. Data collection
Following informed consent, participants took part in one interview exploring their communication experiences using a semi‐structured interview guide ( Material S1 ) previously piloted with an external sample. All interviews were conducted by LI who identifies as a woman and has graduate training in the conduct of semi‐structured interviews. LI works professionally as a nurse practitioner with prior clinical experience caring for mechanically ventilated patients and their families in adult ICUs and a long‐term ventilation and weaning centre in the study site.
Interviews were conducted privately either face to face (in an office), by telephone or video call. Data collection and analysis occurred concurrently and data collection was discontinued when no new information was being identified during interviews (Cope, 2014 ). No one refused participation, no participant dropped out and no repeat interviews were carried out. Interviews were digitally audio‐recorded and transcribed verbatim. Prior to the interview, LI ensured participants understood the rationale for the study and that participation was voluntary and confidential.
2.2.2. Ethical considerations
Ethics approval for the study was given by the Michael Garron Hospital (820‐2010‐Mis‐347) and the University of Toronto Research Ethics Boards (40495). Written informed consent was obtained from all participants prior to interview.
2.2.3. Data analysis and rigour
We completed a team‐based deductive content analysis with author coders working in pairs together, multiple rounds of group discussions and NVIVO 12 software to identify, code and categorize barriers and facilitators to supporting patient communication (Bengtsson, 2016 ). The four stages of content analysis (i.e. decontextualization, recontextualization, categorization and compilation) were used (Bengtsson, 2016 ). In the categorization phase, barriers and facilitators were mapped to the TFA's seven constructs. Definitions for the TFA constructs were adapted to communication with adult ICU patients (Table 1). To enhance credibility of the analysis a code book was constructed and modified using an audit trail through the multiple rounds of coding and discussions among the research team (Cope, 2014 ; De Cuir‐Gunby et al., 2011 ). Further meanings in and across the acceptability constructs and participant groups were elaborated during the compilation stage.
TABLE 1.
Context‐specific definitions for theoretical framework of acceptability (TFA)
| Constructs | Definition |
|---|---|
| Affective attitude | How the individual (HCP or patient/family) describes feeling about communication in the context of infection control practices for COVID‐19 in the adult ICU |
| Burden | The perceived physical, psychological and cognitive effort required of the individual (HCP or patient/family) to engage in communication in the context of infection control practices for COVID‐19 in the adult ICU |
| Ethicality | The extent to which supporting patient communication has a good fit with the individual's (HCP or patient/family) personal or professional values in the context of infection control practices for COVID‐19 in the adult ICU |
| Intervention coherence | The extent to which the individual (HCP or patient/family) understands how to support communication in the context of infection control practices for COVID‐19 in the adult ICU |
| Opportunity costs | The extent to which benefits (e.g. time, money, personal safety) must be given up by the individual (HCP or patient/family) to engage in communication in the context of infection control practices for COVID‐19 in the adult ICU |
| Perceived effectiveness | The extent to which communication is perceived by the individual (HCP or patient/family) to be effective. Strategies that support selecting what is thought to be the most effective intervention in the context of infection control practices for COVID‐19 in the adult ICU |
| Self‐efficacy | The individual's (HCP or patient/family) confidence that they can support communication in the context of infection control practices for COVID‐19 in the adult ICU |
Abbreviations: HCP, healthcare provider; ICU, intensive care unit.
3. FINDINGS
We conducted 29 semi‐structured telephone (15, 52%), face to face (9, 31%) and video call (5, 17%) interviews. Most interviews (23, 79%) were between 30 and 60 min (average 35 min) and six (21%) lasted between 15 and 30 min. Data were collected from nurses and other HCPs (20, 69%) and patients/family (9, 31%). HCPs were primarily women (17, 85%); patient participants were mostly men (3, 75%). Family members largely identified as women (4, 80%) and spouses (2, 40%) and included both members of surviving and deceased ICU patients (Table 2). Patient and family interviews occurred from 11 to 305 days post discharge from ICU, and all participants were able to recall communication experiences in ICU during COVID‐19 pandemic conditions. Patient and family interviews were conducted in dyads (4, 44%) or stand alone when only a patient or family member was available (5, 56%).
TABLE 2.
Participant demographics (N = 29)
| Demographics | n (%) |
|---|---|
| Healthcare providers | 20 (69) |
| Women | 17 (85) |
| Education level | |
| Diploma | 3 (15) |
| Bachelor | 7 (35) |
| Graduate | 10 (50) |
| Profession | |
| Registered Nurse | 9 (45) |
| Allied | 10 (50) |
| Intensivist | 1 (5) |
| Intensive care unit experience | |
| <1 year | 5 (25) |
| 1–10 years | 12 (60) |
| 11–20 years | 2 (10) |
| >20 years | 1 (5) |
| Employment | |
| Full‐time | 11 (55) |
| Patients | 4 (44) |
| Age (range) | 55–71 |
| Gender | |
| Women | 1 (25) |
| Family | 5 (56) |
| Gender | |
| Woman | 4 (80) |
| Relation to patient | |
| Spouse | 2 (40) |
| Sibling | 2 (40) |
| Child | 1 (20) |
| Patient deceased | |
| Yes | 1 (20) |
Though a variety of interview modes were used, each in accordance with participant preference, the quality of data collected afforded by video and face to face methods offered better access to non‐verbal communication for all participants, and in the case of HCPs time constraints in the form of interruptions were observed. Participant checking did not occur after data collection was complete, however, clarification with participants was sought throughout each interview. Participants largely expressed gratitude for the opportunity to share their experiences.
HCPs described using a range of communication strategies with patients individualized to each person's level of consciousness and functional capacities. The primary method described was lip reading/gesture interpretation. Examples of AAC use for awake patients included alphabet boards found online and printed locally or a clipboard and paper if available. For patients who were not awake, some HCP participants described explaining procedures, that is, step‐by‐step guidance. Patient participants recalled more extensive communication efforts by individual providers as the exception rather than the norm. Communication strategies for patients in the context of visitor restrictions included facilitating telephone and video calls between patients and family members (Figure 1).
FIGURE 1.
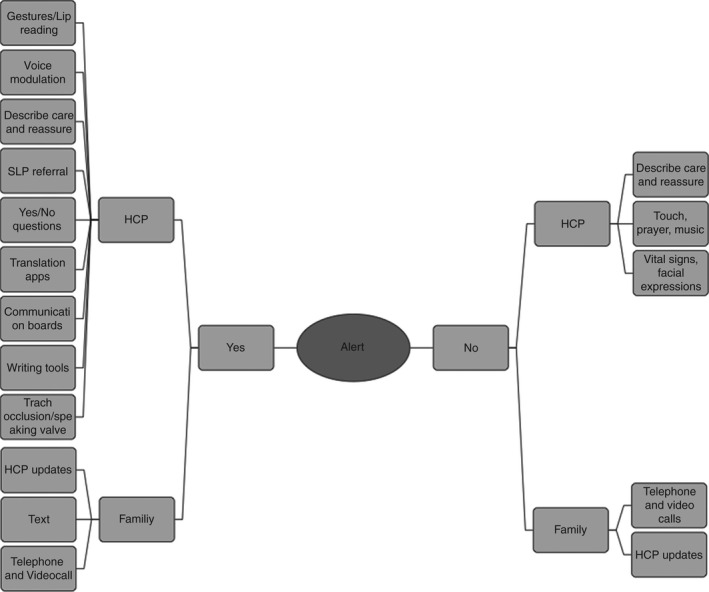
Summary of HCP reported communication strategies. Abbreviations: HCP, health care provider; SLP, speech and language pathologist
Overall participants described communication with and for mechanically ventilated patients in the context of the COVID‐19 pandemic as being significantly constrained, inconsistent, frequently ineffective and unacceptable, thereby contributing to a crisis of communication. Reported barriers and facilitators associated with communication interventions spanned all TFA constructs. The following results are organized by barrier (Table 3) and facilitator (Table 4) categories and described with theoretical concepts from the TFA (identified by italics). In the barrier and facilitator categories, HCP results are separated from patient and family results, permitting comparison across these groups. The source of HCP quotes from members of the allied team were not separated by profession to protect the privacy of participants for whom there were one or few from each class in the study setting. Additional quotes are included as Table S1A–D ).
TABLE 3.
Summary of HCP and patient/family reported barriers to supporting communication with and for patients according to the TFA (Rose et al., 2021 )
| Construct | HCP | Patient/family |
|---|---|---|
| Affective attitude | Negative feelings about distal or insufficient communication | Anger and frustration with failed communication |
| Burden |
Shortage of PPE Physical discomfort of PPE Fear of spreading infection Insufficient time Perceived futility Emotional and cognitive load |
Fear to see patient sick Physical weakness Confusion about situation Loss of family presence |
| Ethicality | Lack of proximity and time | Strategies not supportive of patient humanity and autonomy |
| Intervention coherence | Insufficient tools and training |
Inconsistent availability of tools Inconsistent HCP skill |
| Opportunity costs |
Risk of infection Other priorities in ICU |
|
| Perceived effectiveness |
Patient decreased level of consciousness and weakness PPE impedes verbal and non‐verbal messages |
Decreased level of consciousness PPE blocks verbal and non‐verbal messages |
| Self‐efficacy | HCP lack of skill | HCP and family lack of skill |
Abbreviations: HCP, healthcare provider; PPE, Personal protective equipment; TFA, theoretical framework of acceptability.
TABLE 4.
Summary of HCP and patient/family reported facilitators for supporting communication with and for patients according to the TFA (Rose et al., 2021 )
| Construct | HCP | Patient/family |
|---|---|---|
| Affective attitude | Feeling good with successful communication | |
| Burden |
PPE availability Voice modulation Exaggerate gestures Mental health support Spiritual support Leadership support |
Trust in HCP Connecting patients and family |
| Ethicality |
Empathy Professional values |
Strategies that support patient humanity and autonomy |
| Intervention coherence | Access to tools and training |
Access to tools Coaching from HCP |
| Opportunity costs | Flexibility with timing of video calls | |
| Perceived effectiveness |
Communication assessment and treatment algorithm |
Increased level of consciousness |
| Self‐efficacy |
Abbreviations: HCP, Healthcare provider; PPE, personal protective equipment; TFA, Theoretical framework of acceptability.
3.1. Communication barriers
3.1.1. HCP barriers
Participants described patient proximity as a prerequisite for assessing mechanically ventilated patient communication needs and executing collaborative strategies such as lip reading, symbol/word boards or reading handwritten messages. Impaired patient proximity under isolation procedures led several HCPs to reported negative affective attitudes concerning patient communication. For example, one participant described having to communicate from outside the glass door of the patient's room using a telephone as ‘awful’ (Allied). This HCP explained that communication at a distance was required to reduce excess consumption of PPE, due to shortages at the onset of the pandemic. Conservation of PPE added to the burden of communication, whereby essential communication opportunities were constrained or ineffective at a distance, resulting in concerns about the ethicality of care.
Masks and visors also negatively impacted perceived effectiveness of communication through reduced transmission of verbal and non‐verbal messages. This warranted additional time spent communicating in discomforting conditions:
Also, sometimes you're wearing an N95 mask and you're wearing a shield on top of that, and you know, and you're wearing a gown and hairnet and everything, you have to speak really loudly. And, and your words don't come out as clear. Nurse
HCPs described communication with mechanically ventilated patients as a time‐intensive endeavour under normal or non‐pandemic circumstances. This is because a process of trial and error is required to identify modes of communication best suited to each patient's level of consciousness and functional capacities. The opportunity costs of supporting patient communication in a pandemic context included having to balance patient care needs, infection risk for themselves, as well as physical discomfort and a time‐compressed work environment. One participant explained:
I mean, it's not just a coincidence that we leave the room without saying ‘Do you need anything else.’ We're trying to get out so that we can get to the next person. Allied
HCPs described volatile emotions such as sadness as a significant communication burden in this context. Some participants speculated that strong emotions might negatively impact the willingness of HCPs to participate in patient communication interventions. For example, the increased proportion of patient deaths due to COVID‐19 led to what some described as an overriding feeling of futility:
…And no matter what you do, sometimes it just doesn't work. They die …. And then, here comes another one, you know, like, and again, the same presentation. Allied.
The emotional, physical and psychological demands of this work were well exemplified by accounts of facilitated communication for patients and families via video call at the time of death. Some family members asked HCPs to perform extended acts of patient intimacy such as ‘holding their hand’ (Nurse). These encounters placed HCPs in sustained contact with dying patients and grieving family members adding to the emotional burden of communication.
Many HCP reported a lack of ready access to communication tools contributing to the burden of communication with mechanically ventilated patients. Lack of access to communication tools, particularly in isolation rooms was frequently reported. One participant stated:
So, I usually have to open the door and be like, “Can I please have a clipboard? paper? Anything? A pen? pencil?” Allied
Others described low intervention coherence and self‐efficacy leading to frequent communication failures. Resolution of such difficulty required time‐consuming workarounds, such as ‘calling a colleague for help’, which increased the opportunity costs of communication (Nurse). Furthermore, while SLPs were available for communication consultation at the study site, there was variable awareness of their services among staff.
In summary, HCP barriers for communicating with mechanically ventilated patients emerged from isolation requirements and PPE shortage, which impeded the proximity required for communication support. PPE impediments to message transmission and limited access to communication tools further complicated this work. The opportunity costs of supporting patient communication in a pandemic context included having to balance patient needs, infection risk, physical discomfort and a time‐compressed work environment. The cumulative physical, emotional and psychological barriers contributed to negative affective attitudes, low intervention coherence and self‐efficacy, reduced ethicality and high burden of communication with and for patients.
3.1.2. Patient and family barriers
Like HCP, patients and families described barriers to communication with respect to visiting restrictions and the deployment of telephone and video calls, which did not uniformly meet their needs. For example, some families did not characterize facilitated telephone or video calls with the patient as ‘real communication’:
Well, I couldn't communicate with xxx because I couldn't be there. Family
In this instance, proximity to the mechanically ventilated patient was considered essential for meaningful expression of verbal (i.e. comforting words) and non‐verbal messages (i.e. physical touch). The limitations of video call methods were made particularly clear in instances where the patient was sedated or comatose:
He was unconscious … the first while so there was no real communicating with him. Family
The non‐responsive nature of sedated or comatose mechanically ventilated patients during some video calls aroused discomfort for some participants and added to the emotional burden of communication and reduced intervention coherence. Some participants felt ill prepared for these encounters:
She's gonna be scarred forever from that first view of the ICU and seeing her dad like that. Family
When reflecting back on their inability to communicate verbally during mechanical ventilation, most patients described negative affective attitudes including frustration with their non‐verbal status and clinicians who they perceived as unable to understand them when they mouthed words:
I couldn't [speak], nothing would come out. It was frustrating for me. I'm trying to talk and then I would get very upset because why isn't she listening to me? Why isn't she understanding me? Patient
Family members confirmed how few HCPs were able to lip read, leading to frequent communication failures:
Because there was one, I remember who was really good at lip reading, but the rest of them weren't. Family
In rare instances, family members reported HCPs introducing low‐tech strategies such as communication boards when lip reading was unsuccessful. However, barriers to their use included patient functional deficits, which negatively impacting perceived effectiveness of this strategy:
He'd play with the [word] boards, and those would get frustrating … Family
Patients confirmed infrequent provision of tools such as communication boards and writing instruments, despite their interest in using them. For most, this culminated in a lack of ethicality related to expectations for communication support:
Did anyone ever bring you an alphabet board? Interviewer
No. Never. Patient
Patients emphasized how unresolved communicate barriers during mechanical ventilation left them vulnerable and afraid in isolation rooms, compromising their feelings of autonomy and humanity (ethicality). For example, one patient repeatedly struggled to capture the attention of HCPs, who often appeared distracted or rushed during their encounters. In addition to the negative impact on their feelings of humanity, these events left patients in a state of crisis:
Well, when you have absolutely no voice [it] is little things that just can bring a little control. They turn around, they walk out. So, I'm waving at a back. […] I have no idea whether they even saw me. Patient
Like HCP, patient and family participants reported impaired verbal and non‐verbal message transmission with PPE, but also described difficulty in identifying which HCP they were communicating with and understanding general information about the treatment plan. On PPE and perceived effectiveness of communication, one family member who was able to visit the ICU stated:
So much of our communication is nonverbal, as you know … And if you've got that taken away, it's very, very, very difficult to really absorb what's going on. Family
In summary, patient and family participants reported communication barriers during mechanical ventilation such as isolation procedures, functional deficits, HCP skill and PPE use as contributing to low intervention coherence and negative affective attitudes. Patients and family also reported a high emotional burden of communication via video calls without adequate preparation as well as confusion about HCP identity. An overall gap in the provision of proactive and effective communication support compromised the ethicality of care and left some participants in a state of crisis.
3.2. Communication facilitators
3.2.1. HCP facilitators
Several strategies were reported to manage the challenges of working with PPE and mechanically ventilated patients managed in isolation. Reduced verbal and non‐verbal message transmission while wearing masks and visors was mitigated through exaggerated gestures and voice modulation.
You have to talk in short sentences loudly and we have to be very clear and concise because … the mask and the shields. Nurse
Adequate availability of PPE was a reported facilitator that increased the acceptability of supporting patient communication during the COVID‐19 pandemic. As the PPE supply increased and rationing was lessened, clinicians were able to spend more time at the patient bedside:
And we feel a little bit more liberal with our PPE than we did previously. So, I think the actual hands on with the patients enhance the communication with the patient; [it] is a little bit better. Intensivist
Greater time spent in ‘hands on’ care at the bedside enabled more frequent communication opportunities and aligned with ethical tenets of professional practice. For example, one participant explained how PPE enabled them to better fulfil their role in emotionally and psychologically safeguarding patients:
But that's what you're there for. You're there to keep them alive. But you want to reassure them; too, it's just part of the job. Allied
Balancing opportunity costs of patient care needs, infection risk and the physical discomfort of PPE was facilitated through supportive acknowledgement of care stressors by unit leaders (e.g. daily staff‐leadership huddles) and access to the spiritual care team who helped to process feelings of burden for HCPs. Intervention coherence for facilitating communication with and for patients was advanced by communication tool availability and training of staff to assist in appropriate tool selection and implementation:
I think there's room for a structured process in terms of “if this doesn't work, try this. If it doesn't work, try this, this doesn't work try this”. Allied
Choosing the appropriate strategy for mechanically ventilated patients based on communication assessments was a suggestion to reduce frustration associated with communication failure. Recommendations included a decisional algorithm to improve perceived effectiveness of communication interactions.
In summary, HCPs acknowledged the importance of adequate PPE and communication tools/training to support the intervention coherence and sustained proximity required for communication work with mechanically ventilated patients. They also described examples of unit leadership mitigating some of the emotional burden and opportunity costs of supporting patient communication in the pandemic context. Improvements in perceived effectiveness through individual workarounds such as accentuating gestures and speaking louder were described, as was the suggestion to use an assessment‐based communication algorithm.
3.2.2. Patient and family facilitators
Some patients described positive affective attitudes in response to the proactive facilitation of communication needs during mechanical ventilation. For example, a few patients recalled proactive provision of writing instruments. The time HCPs invested in facilitating and reviewing written communication was described as reducing the burden of voicelessness during mechanical ventilation:
Yeah. I said why I have no voice. Thank God there's a pen and paper. Patient
Like I have to be able to write something and then have the person actually take the time to read it […]. And ask you about it. Do you mean this? Yes or no? Patient
Similarly, a patient aligned the proactive application of a speaking valve to their tracheostomy tube with positive affective attitudes about their treatment and recovery:
Yeah, I remember the day I got [the speaking valve]. And I just said a few words. And I just felt so good. Patient
Patients also described the provision of technology for telephone and video calls as reducing the emotional burden of isolation and advancing the ethicality of care, as it facilitated a connection with family members, who offered emotional support and reassurance.
… if it wasn't for the actual iPad that was provided from the hospital, yeah, they would literally have no means of communication whatsoever. Zero. Patient
With respect to preparation for communication with a non‐verbal mechanically ventilated patient, one family member shared how coaching from a speech language pathologist in the ICU improved the coherence and perceived effectiveness of video call communication:
And she [SLP] actually spent some time with xxx coaching him on different things to do. She also coached me in terms of, you know, I'm used to asking open ended questions. Family
In summary, patients and family participants reported proactive provision of communication tools/training and associated use of technology as therapeutic during mechanical ventilation. Such support improved perceived effectiveness in communication and advanced perceptions of role self‐efficacy, care ethicality and reducing the burden of communication barriers.
4. DISCUSSION
The aim of this qualitative study was to explore barriers to and facilitators for supporting communication with and for mechanically ventilated adult patients admitted to ICU during the COVID‐19 pandemic according to TFA constructs. To our knowledge, this is the first study to explore ICU patient communication needs in ICU during pandemic conditions. Study results revealed substantial gaps in support for patients and a practice context fraught with unanticipated challenges, often culminating in a crisis of communication. Stakeholder reported communication barriers and facilitators spanned all constructs of the TFA and comprised potentially modifiable clinical and institutional practices including proactive and systematic provision of communication tools, training, emotional/spiritual support, as well as leadership practices that may encourage effective and timely communication with and for mechanically ventilated patients.
4.1. Communication barriers
Patients, family members and HCPs reported how isolation precautions contributed to negative affective attitudes and burden, as they counteracted the proximity and time required for successful communication support during mechanical ventilation. Negative affective attitudes were described by patients who were frustrated by abbreviated or non‐existent communication encounters and family members who experienced distress in their attempts to communicate with non‐responsive patients. HCPs also reported feeling badly about insufficient or ineffective communication interventions, such as those conducted from a distance or under time‐compressed circumstances. Sustained proximity, for example when using a communication board, tablet for video calls, or lip reading was described, but HCPs explained they often did so with fear of contracting COVID‐19 from patients and infecting their own family members at home. These pandemic‐related reported risks add to known moral difficulties associated with the patient proximal nature of nursing work (Peter & Liaschenko, 2004 ). The high opportunity costs of patient care were similarly reported in a prospective cross‐sectional survey from an Australian ICU, where 90% of responding nurses shared the fear of contracting and transmitting COVID‐19 (Lord et al., 2021 ). Furthermore, prior research suggests HCPs exposed to high patient acuity, advanced technology, families in crisis and morally distressing situations are at high risk of burnout and depersonalization (Epp, 2012 ). These issues may impede the proximity need to identity patient communication needs and provide effective support.
Described shortages of essential resources (e.g. PPE, time, communication tools) and the physical challenges of wearing PPE contributed to perceived ineffective communication, and ethical‐moral conflict for HCPs balancing professional accountability and personal safety. While the lack of available PPE reduced bedside communication encounters, its use often negatively influenced perceived communication effectiveness. Other authors have described impaired verbal and non‐verbal message transmission due to PPE and shortages in supply as major communication barriers in care settings outside of ICU (Knollman‐Porter & Burshnic, 2020 ; Richards et al., 2021 ). Masks and visors inhibit what SLPs call the ‘speech chain’; the listener's ability to simultaneously hear, lip read and interpret facial expressions (Reidy et al., 2020 ). In addition to muffling voices, masks and visors render recognition of clinicians, and therefore their purpose at the bedside, difficult for patients. These challenges may contribute to communication breakdown, increased frustration and decreased quality of care.
As in previous studies, a lack of uniform awareness of local communication experts, such as SLPs, lack of easily accessible communication tools and limited family presence negatively impacted communication encounters and perceived empathic care by mechanically ventilated patients (Istanboulian et al., 2020 ). Insufficient training and ready access to communication tools, such as video call tablets, were reported as barriers to supporting patient communication with family members. A UK multicentre survey of how communication between families, patients and the ICU team was enabled during the pandemic similarly reported insufficient staff time, rapid implementation of and unequal availability of video call technology as well as some centres restricting their use at end‐of‐life (Rose et al., 2021 ). Our study describes the immense emotional nature of end‐of‐life video supported communication on HCPs. The negative psychological effects of remote‐only communication for family of ICU patients during the COVID‐19 pandemic have been recently described (Cattelan et al., 2021 ). Family participants in our study, though appreciative of video calls, suggested the need for better preparation and emotional support for technology‐mediated patient encounters.
4.2. Communication facilitators
Authentic leadership, with its attributes of transparency, honesty and mutual respect, may play an important role in creating work environments that promote humanistic care, including communication support through reducing staff moral distress (Spence Laschinger & Fida, 2015 ). Key facilitators reported in this study included the role leadership played in reducing the burden of communication with mechanically ventilated patients through ensuring adequate provision of PPE and transparent policy information. Tabah and colleagues previously identified an association between shortage of PPE and low HCP confidence in the adequacy of protection from COVID infection (Tabah et al., 2020 ). Likewise, a recent US study reported a reduction in moral distress among nurses during COVID‐19 when leadership provided clear communication and adequate PPE supplies (Lake et al., 2021 ). Adequacy of PPE and clear communication from unit leadership may increase confidence in personal safety, thereby enabling more time spent in direct patient care supporting communication interventions.
While provision of PPE was an institutional responsibility, strategies to overcome other communication resource gaps were most often left to the individual HCP to resolve. Clinicians frequently employed time‐intensive workarounds, such as trial and error, to manage patient communication impairment during mechanical ventilation. Resource gaps are known to contribute to HCPs feeling time compressed, which is a predictor of patient communication omission (Ausserhofer et al., 2014 ). Systemic efforts to place communication tools for staff to use in or near patient rooms (i.e. communication cart), and provide just‐in‐time training, may potentially reduce the burden of communication (Happ et al., 2014 ; Trotta et al., 2019 ). Access to evidence‐based tools and training may improve intervention coherence, perceived effectiveness and self‐efficacy in communication efforts and decrease long‐term negative outcomes of communication impairment (Happ et al., 2014 , 2015 ; Radtke et al., 2011 ; Simeone et al., 2021 ; Vento‐Wilson et al., 2015 ).
While evidence‐based communication treatment algorithms exist for use in the adult ICU, none consider telephone and video calls as optional supports for mechanically ventilated patients treated under infection control precautions (Happ, 2013 ; Ten Hoorn et al., 2016 ). Facilitating communication for patients and family through telephone and video calls was reported by HCPs, patients and family members in this study. The endorsement of these communication adjuncts (e.g. telephones and tablets) in communication guidance may be important in expanding communication opportunities for mechanically ventilated patients in pandemic and other infection control contexts. The use of tablet and video call technology in this and other ICUs has become an emerging practice to connect patients and family members when in‐person visiting is restricted (Negro et al., 2020 ; Rose et al., 2021 ). Standardized access to institution tablets, sufficient wireless technology, secure video call programs and accessories such as charging cables and mounting structures may facilitate intervention coherence and the acceptability of these communication practices in the ICU.
4.3. Acceptability
Our analysis indicates low acceptability of existing communication practices for mechanically ventilated patients in the adult ICU during COVID‐19 restrictions from the perspective of diverse ICU stakeholders. Barriers aligned with the TFA constructs burden, affective attitudes, effectiveness, ethicality and intervention coherence suggest a need to address the physical safety and emotional needs of ICU nurses and other HCPs to allow them to maintain proximity to and time with patients to support their communication needs. Many facilitators were also reported and were aligned with the TFA constructs burden, intervention coherence, self‐efficacy, opportunity costs, ethicality and effectiveness suggesting a need for consistent availability of communication tools, staff training and awareness of support roles such as SLP, spiritual care and unit leadership to improve cognitive and emotional responses to communication in pandemic and other infection control conditions.
Looking beyond the COVID‐19 pandemic, critically ill patients will continue to require treatment with advanced airways for mechanical ventilation, ICU nurses and other HCPs will need to wear PPE for infection control purposes, and family members may not be available to attend the patient's bedside. Accurate patient‐HCP communication is essential to providing safe and effective care. The communication challenges experienced during the COVID‐19 pandemic identify the need to expand current guidance to address communication challenges during infection control and prevention precautions. Future research should explore implementation of communication interventions under infection prevention and control precautions and evaluate outcomes using TFA domains.
4.4. Strengths and limitations
Strengths of this study include the use of a theoretical framework and the inclusion of patient, family and professionally diverse stakeholders. The TFA provided a systematic and multilevel approach to exploring acceptability that may inform the design and implementation of communication interventions. In addition, we employed an interprofessional team approach to analysis to expand interpretive insights and implications. Limitations include a single study site and limited numbers of patients, which may impact transferability of the results. Time constraints in the pandemic context contributed to some shorter interviews for some HCPs. The researcher conducing the interviews is an NP working in the same institution, which may have influenced stakeholder reporting during interviews.
5. CONCLUSION
COVID‐19 conditions have precipitated a communication crisis in the ICU. The TFA was a useful framework to analyse reported barriers to and facilitators for supporting communication with and for patients treated with invasive mechanical ventilation in the intensive care unit during the COVID‐19 pandemic. Aligning reported barriers and facilitators to the TFA constructs unveiled multiple dimensions of unacceptability of current communication practices in the COVID‐19 ICU context. The results of this study can be used to inform ICU practice as well as communication and visiting policies that can be used during and beyond the COVID‐19 pandemic. The results will be used to co‐develop with patient, family and clinician stakeholders, an intervention for this context that will undergo further acceptability evaluation.
AUTHOR CONTRIBUTIONS
LI, LR, YY, CD: made substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15212.
Supporting information
DataS 1
TableS 1
ACKNOWLEDGEMENT
The authors thank the patients, families and healthcare provider participants of this study for their generous participation.
Istanboulian, L. , Rose, L. , Yunusova, Y. & Dale, C. (2022). Barriers to and facilitators for supporting patient communication in the adult ICU during the COVID‐19 pandemic: A qualitative study. Journal of Advanced Nursing, 78, 2548–2560. 10.1111/jan.15212
Funding informationThis study is supported by the Canadian Nurses Foundation, the Bertha Rosenstadt Health Research Fund, the Bluma Appel and Jeannie Butler Graduate Award in Nursing, the Mary Kathleen King Graduate Awards, the Staples Family Graduate Student Award in Nursing and the Michael Garron Hospital TD Community Health Fund Solutions for COVID‐19 Research Grant.
Contributor Information
Laura Istanboulian, Email: laura.istanboulian@utoronto.ca, @Laura_lista.
Craig Dale, @Craig_dale1.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Akgun, K. M. , Shamas, T. L. , Feder, S. L. , & Schulman‐Green, D. (2020). Communication strategies to mitigate fear and suffering among COVID‐19 patients isolated in the ICU and their families. Heart & Lung, 49(4), 344–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attaway, A. H. , Scheraga, R. G. , Bhimraj, A. , Biehl, M. , & Hatipoglu, U. (2021). Severe covid‐19 pneumonia: Pathogenesis and clinical management. BMJ, 372, n436. [DOI] [PubMed] [Google Scholar]
- Augmentative and Alternative Communication . Augmentative and Alternative Communication [June 21, 2019]. Available from: http://www.asha.org/public/
- Ausserhofer, D. , Zander, B. , Busse, R. , Schubert, M. , De Geest, S. , Rafferty, A. M. , et al. (2014). Prevalence, patterns and predictors of nursing care left undone in European hospitals: Results from the multicountry cross‐sectional RN4CAST study. BMJ Quality and Safety, 23(2), 126–135. [DOI] [PubMed] [Google Scholar]
- Barreras‐Espinoza, J. A. , Leyva‐Moraga, F. A. , Leyva‐Moraga, E. , Leyva‐Moraga, F. , Soualhi, A. , Juanz‐Gonzalez, A. , et al. (2021). Communication in the ICU during the COVID‐19 pandemic. European Journal of Anaesthesiology, 38(10), 1009–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgarten, M. , & Poulsen, I. (2015). Patients' experiences of being mechanically ventilated in an ICU: A qualitative metasynthesis. Scandinavian Journal of Caring Sciences, 29(2), 205–214. [DOI] [PubMed] [Google Scholar]
- Bengtsson, M. (2016). How to plan and perform a qualitative study using content analysis. NursingPlus Open, 2, 8–14. [Google Scholar]
- Canada Go . COVID‐19 daily epidemiology update 2022. [Available from: https://health‐infobase.canada.ca/src/data/covidLive/Epidemiological‐summary‐of‐COVID‐19‐cases‐in‐Canada‐Canada.ca.pdf.
- Carruthers, H. , Astin, F. , & Munro, W. (2017). Which alternative communication methods are effective for voiceless patients in intensive care units? A systematic review. Intensive & Critical Care Nursing, 42, 88–96. [DOI] [PubMed] [Google Scholar]
- Cattelan, J. , Castellano, S. , Merdji, H. , Audusseau, J. , Claude, B. , Feuillassier, L. , Cunat, S. , Astrié, M. , Aquin, C. , Buis, G. , Gehant, E. , Granier, A. , Kercha, H. , Le Guillou, C. , Martin, G. , Roulot, K. , Meziani, F. , Putois, O. , & Helms, J. (2021). Psychological effects of remote‐only communication among reference persons of ICU patients during COVID‐19 pandemic. Journal of Intensive Care, 9(1), 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, J. , Campbell, M. L. , Gelinas, C. , Happ, M. B. , Tate, J. , & Chlan, L. (2017). Symptom assessment in non‐vocal or cognitively impaired ICU patients: Implications for practice and future research. Heart & Lung, 46(4), 239–245. [DOI] [PubMed] [Google Scholar]
- Cope, D. G. (2014). Methods and meanings: Credibility and trustworthiness of qualitative research. Oncology Nursing Forum, 41(1), 89–91. [DOI] [PubMed] [Google Scholar]
- De Cuir‐Gunby, J. T. , Marshall, P. L. , & McCulloch, A. W. (2011). Developing and using a codebook for the analysis of interview data: An example from a professional development research project. Field Methods, 23(2), 136–155. [Google Scholar]
- Doyle, L. , McCabe, C. , Keogh, B. , Brady, A. , & McCann, M. (2020). An overview of the qualitative descriptive design within nursing research. Journal of Research in Nursing, 25(5), 443–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epp, K. (2012). Burnout in critical care nurses: A literature review. Dynamics (Pembroke, Ont.), 23(4), 25–31. [PubMed] [Google Scholar]
- Freeman‐Sanderson, A. , Rose, L. , & Brodsky, M. B. (2020). Coronavirus disease 2019 (COVID‐19) cuts ties with patients' outside world. Australian Critical Care, 33(5), 397–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Happ MB. 2013. SPEACS – 2 Communication Training Program 2013. Available from: https://nucleus.con.ohio‐state.edu/media/speacs2/speacs.htm.
- Happ, M. B. , Garrett, K. L. , Tate, J. A. , DiVirgilio, D. , Houze, M. P. , Demirci, J. R. , George, E. , & Sereika, S. M. (2014). Effect of a multi‐level intervention on nurse‐patient communication in the intensive care unit: Results of the SPEACS trial. Heart & Lung, 43(2), 89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Happ, M. B. , Seaman, J. B. , Nilsen, M. L. , Sciulli, A. , Tate, J. A. , Saul, M. , & Barnato, A. E. (2015). The number of mechanically ventilated ICU patients meeting communication criteria. Heart & Lung, 44(1), 45–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ijssennagger, C. , Ten Hoorn, S. , Van Wijk, A. , Van den Broek, J. M. , Girbes, A. R. , & Tuinman, P. R. (2018). Caregivers' perceptions towards communication with mechanically ventilated patients: The results of a multicenter survey. Journal of Critical Care, 48, 263–268. [DOI] [PubMed] [Google Scholar]
- Inoue, S. , Hatakeyama, J. , Kondo, Y. , Hifumi, T. , Sakuramoto, H. , Kawasaki, T. , Taito, S. , Nakamura, K. , Unoki, T. , Kawai, Y. , Kenmotsu, Y. , Saito, M. , Yamakawa, K. , & Nishida, O. (2019). Post‐intensive care syndrome: Its pathophysiology, prevention, and future directions. Acute Medicine and Surgery, 6(3), 233–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Istanboulian, L. , Rose, L. , Gorospe, F. , Yunusova, Y. , & Dale, C. M. (2020). Barriers to and facilitators for the use of augmentative and alternative communication and voice restorative strategies for adults with an advanced airway in the intensive care unit: A scoping review. Journal of Critical Care, 57, 168–176. [DOI] [PubMed] [Google Scholar]
- Karlsen, M. W. , Olnes, M. A. , & Heyn, L. G. (2019). Communication with patients in intensive care units: A scoping review. Nursing in Critical Care, 24(3), 115–131. [DOI] [PubMed] [Google Scholar]
- Khalaila, R. , Zbidat, W. , Anwar, K. , Bayya, A. , Linton, D. M. , & Sviri, S. (2011). Communication difficulties and psychoemotional distress in patients receiving mechanical ventilation. American Journal of Critical Care, 20(6), 470–479. [DOI] [PubMed] [Google Scholar]
- Knollman‐Porter, K. , & Burshnic, V. L. (2020). Optimizing effective communication while wearing a mask during the COVID‐19 pandemic. Journal of Gerontological Nursing, 46(11), 7–11. [DOI] [PubMed] [Google Scholar]
- Lake, E. T. , Narva, A. M. , Holland, S. , Smith, J. G. , Cramer, E. , Rosenbaum, K. E. F. , French, R. , Clark, R. R. S. , & Rogowski, J. A. (2021). Hospital nurses' moral distress and mental health during COVID‐19. Journal of Advanced Nursing, 78, 799–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord, H. , Loveday, C. , Moxham, L. , & Fernandez, R. (2021). Effective communication is key to intensive care nurses' willingness to provide nursing care amidst the COVID‐19 pandemic. Intensive & Critical Care Nursing, 62, 102946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negro, A. , Mucci, M. , Beccaria, P. , Borghi, G. , Capocasa, T. , Cardinali, M. , Pasculli, N. , Ranzani, R. , Villa, G. , & Zangrillo, A. (2020). Introducing the video call to facilitate the communication between health care providers and families of patients in the intensive care unit during COVID‐19 pandemia. Intensive & Critical Care Nursing, 60, 102893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen, N. , Chinn, J. , Nahmias, J. , Yuen, S. , Kirby, K. , Hohmann, S. , et al. (2021). Outcomes and mortality among adults hospitalized with COVID‐19 at US medical centres. JAMA Network Open, 4(3), e210417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Cathain, A. , Croot, L. , Duncan, E. , Rousseau, N. , Sworn, K. , Turner, K. M. , Yardley, L. , & Hoddinott, P. (2019). Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open, 9(8), e029954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ontario PH . 2021. IPAC Recommendations for Use of Personal Protective Equipment for Care of Individuals with Suspect or Confirmed COVID‐19 2021 [Available from: https://www.publichealthontario.ca/‐/media/documents/ncov/updated‐ipac‐measures‐covid‐19.pdf?la=en.
- Peter, E. , & Liaschenko, J. (2004). Perils of proximity: A spatiotemporal analysis of moral distress and moral ambiguity. Nursing Inquiry, 11(4), 218–225. [DOI] [PubMed] [Google Scholar]
- Radtke, J. V. , Baumann, B. M. , Garrett, K. L. , & Happ, M. B. (2011). Listening to the voiceless patient: Case reports in assisted communication in the intensive care unit. Journal of Palliative Medicine, 14(6), 791–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reidy, J. , Brown‐Johnson, C. , McCool, N. , Steadman, S. , Heffernan, M. B. , & Nagpal, V. (2020). Provider perceptions of a humanizing intervention for health care workers‐a survey study of PPE portraits. Journal of Pain and Symptom Management, 60(5), e7–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards, D. A. , Sugg, H. V. , Cockcroft, E. , Cooper, J. , Cruickshank, S. , Doris, F. , et al. (2021). COVID‐NURSE: Evaluation of a fundamental nursing care protocol compared with care as usual on experience of care for noninvasively ventilated patients in hospital with the SARS‐CoV‐2 virus‐protocol for a cluster randomised controlled trial. BMJ Open, 11(5), e046436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose, L. , Yu, L. , Casey, J. , Cook, A. , Metaxa, V. , Pattison, N. , Rafferty, A. M. , Ramsay, P. , Saha, S. , Xyrichis, A. , & Meyer, J. (2021). Communication and virtual visiting for families of patients in intensive care during COVID‐19: A UKNational Survey. Annals of the American Thoracic Society, 18, 1685–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekhon, M. , Cartwright, M. , & Francis, J. J. (2017). Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Services Research, 17(1), 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simeone, I. M. , Berning, J. N. , Hua, M. , Happ, M. B. , & Baldwin, M. R. (2021). Training chaplains to provide communication‐board‐guided spiritual care for intensive care unit patients. Journal of Palliative Medicine, 24(2), 218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence Laschinger, H. K. , & Fida, R. (2015). Linking nurses' perceptions of patient care quality to job satisfaction: The role of authentic leadership and empowering professional practice environments. The Journal of Nursing Administration, 45(5), 276–283. [DOI] [PubMed] [Google Scholar]
- Tabah, A. , Ramanan, M. , Laupland, K. B. , Buetti, N. , Cortegiani, A. , Mellinghoff, J. , Conway Morris, A. , Camporota, L. , Zappella, N. , Elhadi, M. , Povoa, P. , Amrein, K. , Vidal, G. , Derde, L. , Bassetti, M. , Francois, G. , Ssi Yan Kai, N. , de Waele, J. J. , & PPE‐SAFE contributors . (2020). Personal protective equipment and intensive care unit healthcare worker safety in the COVID‐19 era (PPE‐SAFE): An international survey. Journal of Critical Care, 59, 70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ten Hoorn, S. , Elbers, P. W. , Girbes, A. R. , & Tuinman, P. R. (2016). Communicating with conscious and mechanically ventilated critically ill patients: A systematic review. Critical Care, 20(1), 333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. [DOI] [PubMed] [Google Scholar]
- Trotta, R. L. , Hermann, R. M. , Polomano, R. C. , & Happ, M. B. (2019). Improving nonvocal critical care patients' ease of communication using a modified SPEACS‐2 program. Journal for Healthcare Quality, 42, e1–e9. [DOI] [PubMed] [Google Scholar]
- Vento‐Wilson, M. T. , McGuire, A. , & Ostergren, J. A. (2015). Role of the speech‐language pathologist: Augmentative and alternative communication for acute care patients with severe communication impairments. Dimensions of Critical Care Nursing, 34(2), 112–119. [DOI] [PubMed] [Google Scholar]
- Zaga, C. , Berney, S. , & Vogel, A. (2019). The feasibility, utility, and safety of communication interventions with mechanically ventilated intensive care unit patients: A systematic review. American Journal of Speech‐Language Pathology, 28, 1335–1255. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
DataS 1
TableS 1
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


