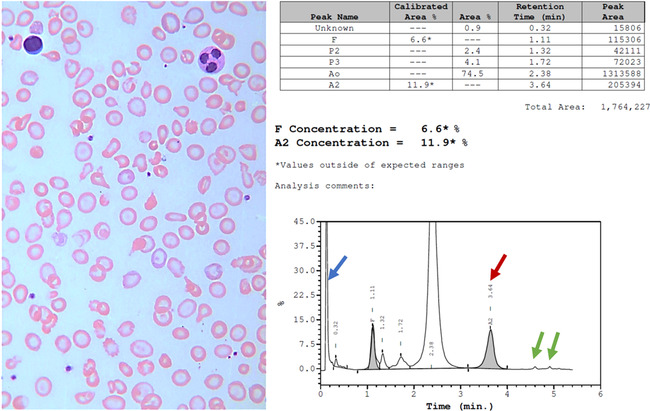
A 20‐year‐old male presented to the Emergency Department with a 2‐day history of fever, fatigue and dark urine. His past medical history included chronic non‐transfusion‐dependent anaemia. The patient had received the ChAdOx1‐S/nCoV‐19 vaccine approximately 6 h earlier. Physical examinations showed temperature 38.6°C, marked pallor and icteric sclerae. Splenic percussion indicated splenomegaly. Laboratory studies showed a haemoglobin concentration of 51 g/l with an MCV of 60 fl and normal white cell and platelet counts. Liver function tests showed an unconjugated bilirubin level of 7.14 mg/dl (normal range 0.2–1.2). A peripheral blood film showed bite cells, blister cells and ghost cells on a background of thalassaemic red cells, polychromasia and nucleated red blood cells (left ×100 objective; Wright‐Giemsa stain). Howell–Jolly bodies were also observed. Glucose‐6‐phosphate dehydrogenase (G6PD) during the haemolytic crisis was decreased (2.1 U/gHb, reference >4.6 U/gHb). After 2 days of supportive treatment and packed red cell transfusion, his fever and symptoms of anaemia resolved. Blood cultures were negative. High performance liquid chromatography (HPLC) of a pretransfusion sample (right) showed haemoglobins A, E (red arrow), Bart's (blue arrow) and Constant Spring (green arrows) indicating EABart's disease, a thalassaemic condition resulting from co‐inheritance of haemoglobin E and the genotype of haemoglobin H disease. All laboratory tests had returned to baseline by 2 weeks.The patient has two genetic diseases, thalassaemia and G6PD deficiency, that are prevalent in South‐east Asia. The acute haemolysis can be attributed to oxidant stress due to COVID‐19 vaccination in a patient with G6PD deficiency.