Abstract
The COVID‐19 pandemic caused collateral damage to patients with acute and chronic conditions. In this mono‐centre cross‐sectional study, we sought to evaluate the impact of the COVID‐19 pandemic on patients with hidradenitis suppurativa (HS). In June 2020, we sent an anonymous survey to 109 patients, who were diagnosed with HS in our outpatient clinic from May 2018 to April 2020. Fifty patients (45.9%) completed and returned the survey. Forty‐five participants (90.0%) denied any cancellation of hospitalisation due to the COVID‐19 pandemic. Hospitalisation was postponed in 8% of cases and cancelled in 2%. Compared to prior to the pandemic, fewer patients consulted their primary physician for changing wound dressings and more changed the dressings themselves or were assisted by their family members. 13% of patients avoided doctor visits due to fear of COVID‐19 and 26.1% minimised doctor visits. The Dermatology Life Quality Index showed a moderate to very severe impact on patients' Quality of Life (mean score = 10.06). Only one patient used telemedicine. Due to limited access to primary care and fear of COVID‐19, the pandemic had a detectable impact on the hospital management of patients with HS in our facility. Telemedicine still plays a negligible role in primary wound care.
Keywords: access to health care, public health, quarantine, SARS‐CoV‐2 infection, telemedicine
1. INTRODUCTION
The Coronavirus disease 2019 (COVID‐19) pandemic remains a strong challenge for health care systems around the world. Collateral damage to patients with other conditions, such as myocardial infarction, stroke, hyperglycaemic crisis, 1 , 2 , 3 cancer 4 or even disabilities 5 have been reported.
The management of hidradenitis suppurativa (HS) deserves special consideration in the context of the COVID‐19 pandemic. 6
HS is a chronic, inflammatory, recurrent, debilitating skin disease of the hair follicle in areas rich in apocrine glands. It typically starts in early adulthood with painful, deep‐seated, inflamed lesions, including inflamed nodules, abscesses, pus‐discharging tunnels, and consequent scarring in the intertriginous areas of the body, most commonly the axillae, inguinal and anogenital regions. The estimated prevalence of HS is around 1% in Europe. 7 , 8 , 9
HS is not considered a specific risk factor for COVID‐19, 6 , 10 yet several aspects might potentially increase the risk for severe COVID‐19 and poor outcomes for patients with HS.
First, HS is associated with diabetes and obesity, comorbidities that may predispose to more severe COVID‐19 infections. 9 Second, cigarette smoking is a recognised risk factor for both the development of HS and severe disease, 8 although its exact role in COVID‐19 still needs further elucidation. 11 , 12 Finally, the poor recognition of disease among non‐dermatologists might impact the medical care of HS patients. 6 , 13
In this survey, we sought to evaluate the impact of the COVID‐19 pandemic on HS patients at our institution.
2. METHODS
2.1. Study design and population
Patients diagnosed with HS between May 2018 and April 2020 in the outpatient clinic of the Department of Dermatology and Allergy, University Hospital, LMU (Ludwig Maximilian University) Munich, Germany, were contacted in June 2020 by letter and asked for participation in this questionnaire‐based cross‐sectional study. The ethics committee of the medical faculty at LMU approved the study (permit number: 20‐390 KB), which was performed in accordance with the Helsinki Declaration of 1975.
2.2. Study assessments and measures
An anonymous structured questionnaire was used for data collection. Information on (a) demographics (gender, age, educational background, health insurance); (b) number of medications; (c) treatment for HS; (d) smoking; (e) in‐patient treatments; (f) medical care and condition during the COVID‐19 pandemic were obtained. In addition, this survey included assessment using the Dermatology Life Quality Index (DLQI) score.
DLQI is a widely used questionnaire for measuring the impact of skin disease on adult patients' Quality of Life (QoL). The DLQI consists of 10 items covering six basic topics: symptoms and feelings, daily activities, leisure, work or school, personal relationships and treatment, each rated on a 4‐point Likert scale. DLQI is calculated by collecting the sum of the scores of the above‐mentioned questions. Higher scores are associated with greater impairment of QoL. The DLQI score is displayed in percentage ranging from a minimum of ‘0’ to a maximum of ‘30’. 14 , 15
2.3. Statistics
For descriptive statistics, mean with 95% confidence interval was calculated for numerical data, while proportions were calculated for categorical variables. McNemar's Chi‐squared test was applied to test for a difference in the person performing the wound dressing before and during COVID‐19. Whether the transportation time correlates with limited doctor access was tested by calculating Goodman‐Kruskal's gamma. Group differences in the DLQI score were tested by the application of independent samples t‐test. All statistics were performed in R (version 3.6.0, 2010, R Foundation for Statistical Computing, Vienna, Austria). Figures were created by using the R package: ggplot2.
3. RESULTS
A total of 50 patients completed the survey, which corresponds to a return rate of 45.9%. However, not all participants answered every question.
Slightly more participants were female (53.1%). Most patients (37.4%) had general education or visited middle school, and 10 (20.8%) experienced higher education. Fifteen participants (31.3%) have had a vocational training or specialisation, while seven (14.6%) held a university degree. All patients were covered by public health insurance. A complete overview of our sample can be found in Table 1.
TABLE 1.
Demographic and clinical characteristics of the study participants
| n = replies | % | |
|---|---|---|
| Gender | 49 | |
| Female | 26 | 53.1 |
| Male | 23 | 46.9 |
| Age | 49 | |
| <20 | 2 | 4.1 |
| 20‐29 | 8 | 16.3 |
| 30‐39 | 14 | 28.6 |
| 40‐49 | 14 | 28.6 |
| 50 or older | 11 | 22.4 |
| School education | 48 | |
| General education (9 y) | 7 | 14.6 |
| Middle school (10 y) | 9 | 18.8 |
| Higher education (12‐13 y) | 10 | 20.8 |
| Vocational training or specialisation | 15 | 31.3 |
| University degree | 7 | 14.6 |
| Medication per day | 50 | |
| None | 17 | 34.0 |
| 1‐4 | 27 | 54.0 |
| 5‐10 | 6 | 12.0 |
| 10 or more | 0 | 0 |
| HS treatment | 49 | |
| None | 29 | 59.2 |
| Pain medication | 2 | 4.1 |
| Antibiotics | 9 | 18.4 |
| Adalimumab | 2 | 4.1 |
| Other | 7 | 14.3 |
| Smoking behaviour | 49 | |
| Currently smoking | 26 | 53.1 |
| Never smoked | 13 | 26.5 |
| Ex‐smokers | 10 | 20.4 |
| Smoking behaviour in COVID‐19 pandemic | 38 | |
| Non‐smokers | 13 | 34.2 |
| Largely increased | 0 | 0 |
| Moderate increased | 2 | 5.3 |
| No increase | 14 | 36.8 |
| Slightly reduced | 5 | 13.2 |
| Importantly reduced | 4 | 10.5 |
| Hospitalisation within 12 mo prior to study | 50 | |
| None | 29 | 58.0 |
| Once | 12 | 24.0 |
| Twice | 5 | 10.0 |
| Three times | 2 | 4.0 |
| Three times or more | 2 | 4.0 |
| Hospitalisation due to HS within 12 mo prior to study | 50 | |
| None | 29 | 58.0 |
| Once | 12 | 24.0 |
| Twice | 5 | 10.0 |
| Three times | 2 | 4.0 |
| Three times or more | 2 | 4.0 |
| Cancellation of hospitalisation | 50 | |
| Yes, without fixing new appointment | 4 | 8.0 |
| Yes, a new appointment was fixed | 1 | 2.0 |
| No cancellation was made | 45 | 90.0 |
| Performance of wound dressing before COVID‐19 | 46 | |
| No wound dressing performed | 0 | 0 |
| Wound dressing performed personally or by relatives | 33 | 71.7 |
| In ambulatory care | 1 | 2.2 |
| By primary care physician | 9 | 19.6 |
| In wound center | 3 | 6.5 |
| Performance of wound dressing during COVID‐19 | 43 | |
| No wound dressing performed | 4 | 9.3 |
| Wound dressing performed personally or by relatives | 33 | 76.7 |
| In ambulatory care | 1 | 2.3 |
| By primary care physician | 2 | 4.7 |
| In wound center | 3 | 7.0 |
| Travel time to the treating physician | 47 | |
| Less than 15 min | 11 | 23.4 |
| 15‐30 min | 13 | 27.7 |
| 30‐60 min | 18 | 38.3 |
| More than 60 min | 5 | 10.6 |
| Medical consultations | 46 | |
| Yes, as usual | 25 | 54.3 |
| Yes, less frequently | 12 | 26.1 |
| Yes, domiciliary visit | 0 | 0 |
| Yes, via telemedicine | 1 | 2.2 |
| No, prohibited by my doctor or hospital | 2 | 4.3 |
| No, by fear of getting infected by COVID‐19 | 6 | 13.0 |
| Home office | 50 | |
| Yes | 12 | 24.0 |
| No | 30 | 60.0 |
| Not applicable | 8 | 16.0 |
| Fear of getting infected by COVID‐19 due to HS or HS therapy | 50 | |
| Yes | 9 | 18.0 |
| No | 28 | 56.0 |
| Do not know | 13 | 26.0 |
| Fear of becoming severely affected by COVID‐19 due to HS or HS therapy | 50 | |
| Yes | 9 | 18.0 |
| No | 24 | 48.0 |
| Do not know | 17 | 34.0 |
Note: Demographic and clinical characteristics of study population are shown with partial and total number of replies (n) in absolute and percentage value.
Twenty‐one participants (42.0%) were hospitalised at least once in the previous 12 months, in 30% of cases due to HS.
As to influence of the COVID‐19 pandemic on work conditions, 12 patients (24%) worked remotely during the lockdown and 30 patients (60%) went to work as usual, while for 8 patients (16%) the question was not applicable.
Forty‐five (90.0%) participants denied any cancellation of hospitalisation due to the COVID‐19 pandemic. With regard to the restricted access to medical services for HS patients, the data indicated an increase in the number of patients who could or did not perform wound dressing during the pandemic (9.3%), in comparison to 0% before the pandemic. Similarly, the amount of wound dressing performed by a primary care physician decreased from 9 (19.6%) prior to the pandemic to two (4.7%) during the first lockdown.
Wound care performed in wound centres or ambulatory care, performed by nursing personnel, remained stable. Differences were detected in the person performing wound dressing before and after the implementation of public lockdown. The number of patients in which wound dressing was performed by patients themselves or by relatives increased, while the number of patients in which changes of wound dressing were performed by primary care physicians dropped dramatically. Results are shown in Figure 1.
FIGURE 1.
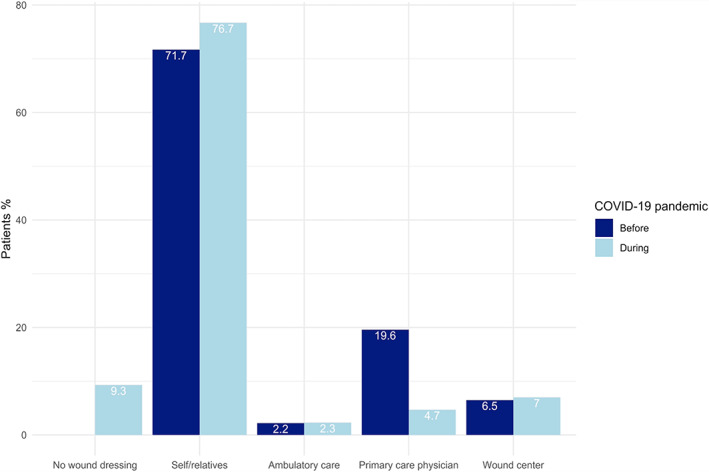
Wound dressing performance in hidradenitis suppurativa (HS) patients before and during the COVID‐19 pandemic. While the number of changes of wound dressing remained stable in ambulatory care and hospital‐based wound centers, the amount of wound dressing performed by patients themselves or by relatives increased, and the number of changes of wound dressing by primary care physicians dropped dramatically
We further assessed whether the frequency of doctor visits may have been impacted by the pandemic (Figure 2) and if the use of public transport or travel time may have had an influence.
FIGURE 2.
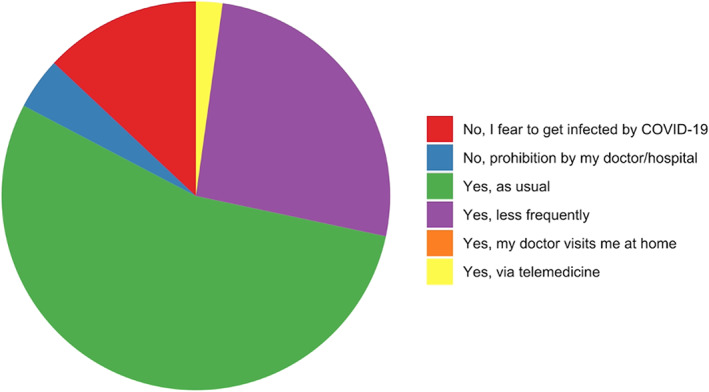
Medical consultations during the COVID‐19 pandemic
54.3% of participants reported visiting their physician as usual, while 26.1% visited their physician less frequently than usual. 4.3% could not see their physician due to pandemic‐related restrictions and 13% decided not to visit the doctor due to fear of exposure to COVID‐19. No patient was visited by doctors at home and telemedicine was used in only one case.
The mean DLQI of our patients who responded to the survey was 10.06, corresponding to a moderate to large effect on patients' QoL. Only 14% of patients declared that HS had no effect on their lives. For 28% of the patients the effect was small and for 18% moderate. For the remaining patients (40%), HS had a major impact: 28% declaring a very large and 12% an extremely large impact on their QoL (Table 2).
TABLE 2.
Effect of the COVID‐19 pandemic on DLQI of study participants (mean 10.06 [95% confidence interval: 8.02, 12.10; SD = 7.17])
| n = replies | % | |
|---|---|---|
| All study participants | 50 | 100 |
| No effect at all on patient's QoL (DLQI 0‐1) | 7 | 14 |
| Small effect on patient's QoL (DLQI 2‐5) | 14 | 28 |
| Moderate effect on patient's QoL (DLQI 6‐10) | 9 | 18 |
| Very large effect on patient's QoL (DLQI 11‐20) | 14 | 28 |
| Extremely large effect on patient's QoL (DLQI 21‐30) | 6 | 12 |
Note: Dermatology Life Quality Index (DLQI) in study population. DLQI values range from 0 to 30 (mean 10.06 [95% confidence interval: 8.02, 12.10; SD = 7.17]).
Moreover, we investigated if working remotely, limitation in access to physician's consultation or in access to professional wound dressing, cancellation of hospitalisation, smoking (Figure 3) or gender differences influenced the DLQI. An independent samples t‐test showed no significant difference among all criteria above.
FIGURE 3.
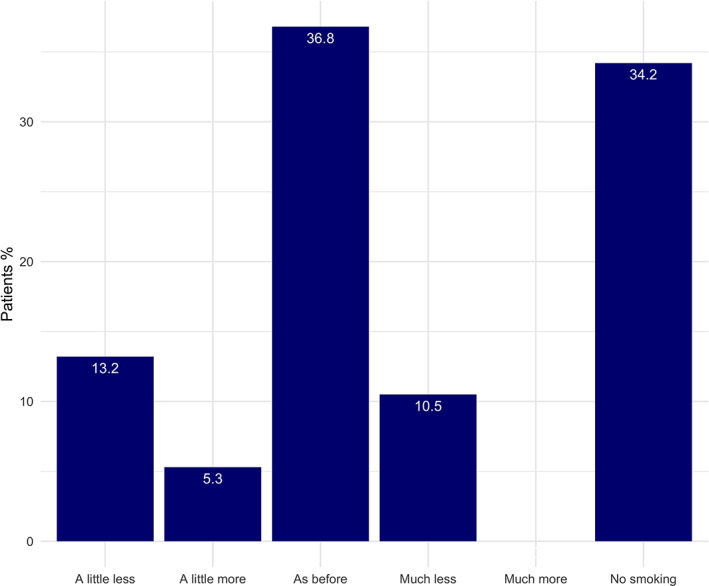
Smoking behaviour in HS patients prior and during the COVID‐19 pandemic. The exact amount of smoked cigarettes has not been quantified
Furthermore, we assessed the sensation of fear associated with the COVID‐19 pandemic in relationship to HS and its therapy. Nine respondents (19%) admitted fear of infection with COVID‐19 due to HS or HS treatment. Similarly, nine patients (18%) claimed to fear a severe course of COVID‐19 due to HS or HS treatment.
4. DISCUSSION
This cross‐sectional study provides evidence of the impact of the COVID‐19 pandemic on patients with HS in a university‐based medical facility in Germany.
Our data revealed a significant decline in access to primary care physicians and, to a lesser extent, a reduced hospitalisation rate of HS patients during the pandemic. However, access to nursing home care and wound centres was not affected. The use of telemedicine did not significantly increase among our patient sample. There was a strong impact of the pandemic on patients' QoL. A significant number of participants feared SARS‐CoV‐2 infection or a severe course of COVID‐19 due to HS or HS treatment.
Indeed, HS patients often have risk factors, that are associated with a severe course of COVID‐19, such as diabetes, obesity 9 and cigarette smoking. 8 , 11 , 12 In addition, biologic treatment with adalimumab may expose HS patients to an additional risk for severe infection. However, the role of biologic treatment during infection with COVID‐19 remains controversial. 16 , 17 Given the uncertainty and fear of HS patients concerning risks of infection with COVID‐19 under HS treatment, close patient follow‐up and counselling are crucial. Telemedicine may be a useful and practicable option, in order to minimise the risk of SARS‐CoV‐2 infection of vulnerable HS patients, maintain physician contact to HS patients, and thus, maintain optimal management of HS patients.
However, our data shows that telecommunication in management of HS remains uncommon in our setting, in contrast to a growing interest in North America. 18 , 19 Most of all, this may be due to the lack of established telemedicine systems or even technical resources and know‐how.
The QoL of our patients was lower compared to HS patients of studies prior to the pandemic. 20 On the one hand, this may be due to lockdown‐related restrictions in daily life that also affect other parts of society. However, based on our data, the QoL in HS patients may additionally be impacted by the particular fear of infection with SARS‐CoV‐2, the limited access to primary care, the increased need to perform wound care without professional help and cancellation of hospitalisation, allegedly leading to worsening of HS lesions. Thus, remote patient counselling could be useful in order to counteract the decrease in the QoL of HS patients during the pandemic.
A limitation of this survey is the sample size of 50 patients recruited from a single institution. In addition, not all participants answered every question. However, the return rate of 50% was remarkably high. The high participation rate may further reflect the significant disease burden or impact of COVID‐19 that our data shows.
5. CONCLUSION
This survey provides evidence that, so far, the COVID‐19 pandemic in our medical facility had a moderate to very large impact on patients with HS.
Despite its clear advantages, especially with respect to the pandemic, telemedicine still plays a negligible role in the management of HS patients. The final impact of the COVID‐19 pandemic on HS patients depends on the course of the pandemic and remains subject of future research.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ETHICS STATEMENT
This study has been approved by the local ethics committee (ethics committee University Hospital, LMU Munich, Germany, Ref.‐No. 20‐390 KB).
ACKNOWLEDGEMENTS
The authors received no financial support for the research, authorship and/or publication of this article.
Fiocco Z, Schlager JG, Kendziora B, et al. Impact of the COVID‐19 pandemic on patients with hidradenitis suppurativa. Int Wound J. 2022;19(7):1686‐1692. doi: 10.1111/iwj.13772
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Lange SJ, Ritchey MD, Goodman AB, et al. Potential indirect effects of the COVID‐19 pandemic on use of emergency departments for acute life‐threatening conditions ‐ United States, January‐May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):795‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Reinstadler SJ, Reindl M, Lechner I, et al. Effect of the COVID‐19 pandemic on treatment delays in patients with ST‐segment elevation myocardial infarction. J Clin Med. 2020;9(7):2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diegoli H, Magalhães PSC, Martins SCO, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID‐19 era. Stroke. 2020;51(8):2315‐2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sud A, Jones ME, Broggio J, et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID‐19 pandemic. Ann Oncol. 2020;31(8):1065‐1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Negrini S, Grabljevec K, Boldrini P, et al. Up to 2.2 million people experiencing disability suffer collateral damage each day of COVID‐19 lockdown in Europe. Eur J Phys Rehabil Med. 2020;56(3):361‐365. [DOI] [PubMed] [Google Scholar]
- 6. Naik HB, Alhusayen R, Frew J, et al. Global hidradenitis suppurativa COVID‐19 registry: a registry to inform data‐driven management practices. Br J Dermatol. 2020;183(4):780‐781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zouboulis CC, Desai N, Emtestam L, et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol. 2015;29(4):619‐644. [DOI] [PubMed] [Google Scholar]
- 8. Jemec GB. Clinical practice. Hidradenitis suppurativa. N Engl J Med. 2012;366(2):158‐164. [DOI] [PubMed] [Google Scholar]
- 9. Sabat R, Jemec GBE, Matusiak Ł, Kimball AB, Prens E, Wolk K. Hidradenitis suppurativa. Nat Rev Dis Primers. 2020;6(1):18. [DOI] [PubMed] [Google Scholar]
- 10. Lima XT, Cueva MA, Alora MB. COVID‐19 in patients with hidradenitis suppurativa. Br J Dermatol. 2021;184(1):182‐184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patanavanich R, Glantz SA. Smoking is associated with COVID‐19 progression: a meta‐analysis. Nicotine Tob Res. 2020;22(9):1653‐1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Leung JM, Sin DD. Smoking, ACE‐2 and COVID‐19: ongoing controversies. Eur Respir J. 2020;56(1):2001759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Saunte DM, Boer J, Stratigos A, et al. Diagnostic delay in hidradenitis suppurativa is a global problem. Br J Dermatol. 2015;173(6):1546‐1549. [DOI] [PubMed] [Google Scholar]
- 14. Finlay AY, Salek MS, Abeni D, et al. Why quality of life measurement is important in dermatology clinical practice: an expert‐based opinion statement by the EADV Task Force on Quality of Life. J Eur Acad Dermatol Venereol. 2017;31(3):424‐431. [DOI] [PubMed] [Google Scholar]
- 15. ICR . IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp; 2019. [Google Scholar]
- 16. Marzano AV, Moltrasio C, Genovese G, et al. Hidradenitis suppurativa and adalimumab in the COVID‐19 era. Eur J Dermatol. 2020;30(6):748‐749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Molinelli E, Diotallevi F, Simonetti O, et al. Management of patients with hidradenitis suppurativa during the COVID‐19 pandemic: risk and benefit of immunomodulatory therapy. Dermatol Ther. 2020;33(6):e14256. [DOI] [PubMed] [Google Scholar]
- 18. Kang NC, Hsiao J, Shi V, Naik HB, Lowes MA, Alavi A. Remote management of hidradenitis suppurativa in a pandemic era of COVID‐19. Int J Dermatol. 2020;59(9):e318‐e320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hong YR, Lawrence J, Williams D Jr, Mainous IA. Population‐level interest and telehealth capacity of US hospitals in response to COVID‐19: cross‐sectional analysis of Google search and National Hospital Survey Data. JMIR Public Health Surveill. 2020;6(2):e18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. von der Werth JM, Jemec GB. Morbidity in patients with hidradenitis suppurativa. Br J Dermatol. 2001;144(4):809‐813. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


