To the Editor,
The pandemic of Coronavirus disease 2019 (COVID‐19) has had a substantial impact on health of adults among the world. In this context, vaccines are being developed in order to increase population immunity. The ChAdOx1 nCoV‐19 vaccine is based on a replication‐deficient chimpanzee adenoviral vector ChAdOx1, containing the SARS‐CoV‐2 structural surface glycoprotein antigen gene. 1
A 86‐year‐old man presented us with a pruritic and persistent eruption of 3 months duration that had appeared 7 days after his first dose of the COVID‐19 vaccine (ChAdOx1 nCoV‐19, AZ‐FIOCRUZ, Rio de Janeiro, Brazil), and got worse after the second dose of vaccine (ChAdOx1 nCoV‐19, AZ‐ FIOCRUZ, Rio de Janeiro, Brazil), with 12 weeks apart. The lesions had developed in both upper and lower limbs and further disseminated to the trunk and buttocks. Upon physical examination, he showed erythematous squamous psoriasiform plaques in the arms, legs, hands and trunk (Figure 1A). Polarized dermoscopy displayed a network of whitish lines with an orthogonal disposition, compatible with Wickham's striae (Figure 1B). A 4‐mm punch biopsy was performed. The H&E examination showed orthokeratosis, paraceratosis, acanthotic epidermis with hypergranulosis and vacuolar degeneration of basal layer with dyskeratotic keratinocytes (Civatte bodies). A dense lichenoid lymphoid cell infiltrate at the dermal‐epidermal junction was identified, with scattered dermal melanophages (Figure 1C, D).
FIGURE 1.
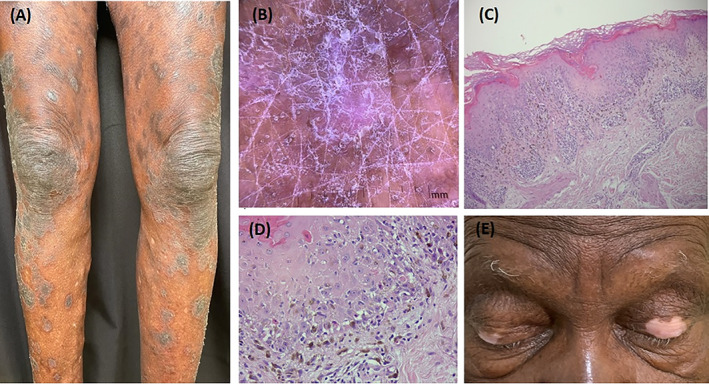
Erythematous squamous psoriasiform plaques in legs (A). A network of whitish lines with an orthogonal disposition, compatible with Wickham striae, noticed with polarized dermoscopy (B). Orthokeratosis, paraceratosis, and vacuolar degeneration of basal layer with Civatte bodies on H&E examination, magnification at ×10 (C) and ×40 (D). Vitiligoid macules on the upper eyelids (E)
In addition to the rash, vitiligoid macules appeared after the second dose of the COVID‐19 vaccine on the upper eyelids with eyelashes poliosis (Figure 1E), in the thenar region of the left hand and in the arm where the biopsy was performed. Polarized dermoscopy displayed areas of altered pigment network. Treatment with halobetasol propionate 0.05% cream was instituted.
Lichen planus (LP) is a cutaneous disorder of unknown origin. Immune dysregulation, environment, drugs, vaccines, genetic factors, and COVID‐19 infection may be involved in the disease's etiology. The classic presentation of LP occurs with a clinical pattern described with the “six P's”: purple, pruritic, polygonal, planar, papules, and plaques. Lichenoid drug eruption (LDE) is a variant of lichen planus in which the skin lesions tend to be more polymorfic and have a desquamation with psoriasiform or eczematous morphology. In the biopsy, eosinophilia is frequently present, what was not seen in this patient. The pathogenesis of LP appears to be related with the activation of the T‐helper‐1 (Th1) response, with the participation of IFN‐γ, TNF‐α, IL‐1α, and IL‐2. This process contributes to the basal keratinocyte apoptosis. 2
Vitiligo is an idiopathic depigmenting disease featured by white spots in the skin due to the selective destruction of melanocytes. There is evidence of autoimmunity and cytokines playing a meaningful role in its pathophysiological mechanism. In vitiligo lesions, the detection of T‐cells indicates the presence of cellular immunity at the pathogenic mechanism, with the promotion of a Th1 response and a consequent production of TNF‐α and IFN‐γ, mediators of innate immunity which inhibit melanocyte activity. 3
The ChAdOx1 nCoV‐19 vaccine activates a Th1 response, with high levels of IL‐2, IFN‐γ, and TNF‐α. 4 These immune dysregulation plays an important role in the pathophysiology of LP and vitiligo. 2 , 3
In this case, the cause–effect relationship is strong, as the eruption had a bimodal timing: it first appeared after the first dose, was remitting, and got worse soon after the second dose. As for the biological plausibility, the vaccine could represent a trigger for the occurrence of LP and vitiligo.
The safety and efficacy of the vaccines against SARS‐CoV‐2 have been shown in clinical trials, but it is important to be aware of the possibility of skin manifestations and worsening of some dermatologic diseases after the COVID‐19 vaccine. Nevertheless, this should not discourage vaccination, as the benefits outweigh the risks.
CONFLICTS OF INTEREST
None of the authors report any conflicts of interest.
PRESENTATION AT A MEETING
This case report was not presented at a meeting.
AUTHOR CONTRIBUTIONS
Shirley Braga Lima Gamonal: Conceptualization; visualization; data curation; writing‐original draft. Aloisio Carlos Couri Gamonal: Conceptualization; visualization; data curation. Nathália Couri Vieira Marques: Conceptualization; writing‐review; edition; submission of the manuscript. Caio Lima Adário: Conceptualization; supervision; editing.
ACKNOWLEDGEMENT
The patient in this manuscript has given written informed consent to the publication of his case details.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Voysey M, Clemens SAC, Madhi AS, et al. Safety and efficacy of the ChAdOx1 nCoV‐19 vaccine (AZD1222) against SARS‐CoV‐2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397:99‐111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tziotzios C, Lee JYW, Brier T, et al. Lichen planus and lichenoid dermatoses: clinical overview and molecular basis. J Am Acad Dermatol. 2018;79:789‐804. [DOI] [PubMed] [Google Scholar]
- 3. Bassiouny DA, Shaker O. Role of interleukin‐17 in the pathogenesis of vitiligo. Clin Exp Dermatol. 2011;36:292‐297. [DOI] [PubMed] [Google Scholar]
- 4. Ewer KJ, Barrett JR, Belij‐Rammerstorfer S. T cell and antibody responses induced by a single dose of ChAdOx1 nCoV‐19 (AZD1222) vaccine in a phase 1/2 clinical trial. Nat Med. 2021;27:270‐278. [DOI] [PubMed] [Google Scholar]
- 5. Sinha A, Kumar R, Singh AR. Implication of mass COVID‐19 vaccination on dermatology practice in 2021. Dermatol Ther. 2021;34:e14765. doi: 10.1111/dth.14765 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


