Dear Editor,
An otherwise healthy 49‐year‐old Italian man presented to our clinic for a cutaneous, pruriginous eruption on his trunk and limbs. The signs appeared 11 days after receiving the second dose of SARS‐CoV‐2 Adenoviral vector Vaxevria (Astrazaneca) vaccine.
He did not report any additional symptoms. The past medical history is silent, and he has not taken drugs in chronic nor in a discontinuous manner in the last year.
When examined, the patient presented erythematous papules on the upper and lower limbs, while on the feet formed small plaques with a keratotic centre. No other lesions were found on oral and genital mucosa (Figure 1A and B). The rash started with an intense itch, reported on a numeric scale of 7/10. 1 A thorough examination with Dermoscopy showed the presence of thin keratotic stripes, also called Whichkam striae (Figure 1C).
FIGURE 1.
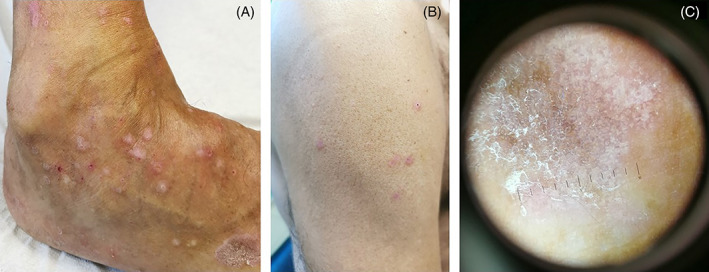
(A) detail of the Lichen of the right foot; (B) Papules of the right arm; (C) Whickam striae, characteristics of lichen planus, observed at Dermoscopy
Clinical and dermoscopic signs, together with the histological examination of a 5‐mm punch biopsy taken from the right arm, led to the eruptive Lichen Planus (LP) diagnosis. Subsequential blood tests were unremarkable, showing no signs of viral hepatitis or possible autoimmune‐related disease as thyroiditis, autoimmune gastritis or antinuclear antibodies positivity (ANA).
We started therapy with topical steroids and systemic antihistamines. After 1 month, the lesions had virtually disappeared, showing only mild erythema and complete remission of the itch.
The clinical signs and the intense itching related to other cases reported in literature 2 , 3 , 4 and the temporal association with the vaccine administration led us to diagnose “Eruptive Lichen Ruber Planus”, according to Naranjo Scale. 5
Numerous skin reactions have been described as elicited by SARS‐COV‐2 and its vaccines, and most of these are considered self‐limiting. Still, others are caused by an autoimmune substrate, leading to chronic skin diseases. Among the possible conditions are described psoriasis, 6 cutaneous lupus erythematosus and LP. LP is a T cell‐mediated chronic inflammatory tissue reaction that results in a cytotoxic response against basal epithelial cells of the skin. 7
The onset of LP after vaccination in our patient may have multiple pathogenetic mechanisms. Among these, we believe that T‐cells play an essential role in the immune response against the cells of the basal layer of the skin in predisposed patients due to the increase in circulating pro‐inflammatory cytokines induced by the vaccine response. 8 Another mechanism may be reconducted to ACE‐2 receptors in the skin. 9 Spike proteins generated by the vaccine may link to the cutaneous cells presenting this receptor and start an immune response by recruiting CD4+ lymphocytes, eventually causing LP in predisposed subjects.
While considering that any inflammatory stimulus, such as vaccinations, can act as a potential trigger of autoimmune disease, such LP in predisposed subjects, data currently do not contraindicate future Anti‐Sars‐Cov2 vaccinations of any type in this kind of patients.
We conclude with a reminder for dermatologists and practitioners to continue investigating any onset of clinical signs concerning the administration of vaccines during vaccination campaigns.
CONFLICT OF INTEREST
The authors have no conflict of interest to declare.
INFORMED CONSENT
The patients in this manuscript have given written informed consent to the publication of their case details.
FUNDING STATEMENT
This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Phan NQ, Blome C, Fritz F, et al. Assessment of pruritus intensity: prospective study on validity and reliability of the visual analogue scale, numerical rating scale and verbal rating scale in 471 patients with chronic pruritus. Acta Derm Venereol. 2012;92(5):502‐507. [DOI] [PubMed] [Google Scholar]
- 2. Hiltun I, Sarriugarte J, Martínez‐de‐Espronceda I, et al. Lichen planus arising after COVID‐19 vaccination. J Eur Acad Dermatol Venereol. 2021;35(7):e414‐e415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diaz‐Guimaraens B, Dominguez‐Santas M, Suarez‐Valle A, Fernandez‐Nieto D, Jimenez‐Cauhe J, Ballester A. Annular lichen planus associated with coronavirus SARS‐CoV‐2 disease (COVID‐19). Int J Dermatol. 2021;60(2):246‐247. [DOI] [PubMed] [Google Scholar]
- 4. Tatu AL, Nadasdy T, Nwabudike LC. Koebner phenomenon with lichen planus in an area of previous vitiligo after COVID‐19 vaccination and the creation of a locus minoris resistentiae. J Eur Acad Dermatol Venereol [Internet]. 2022;n/a:n/a. Accessed January 18, 2022. doi: 10.1111/jdv.17864 [DOI] [PubMed] [Google Scholar]
- 5. Adverse Drug Reaction Probability Scale (Naranjo) in Drug Induced Liver Injury. LiverTox: Clinical and Research Information on Drug‐Induced Liver Injury [Internet]. National Institute of Diabetes and Digestive and Kidney Diseases; 2012. Accessed January 18, 2022. http://www.ncbi.nlm.nih.gov/books/NBK548069/ [PubMed] [Google Scholar]
- 6. Krajewski PK, Matusiak Ł, Szepietowski JC. Psoriasis flare‐up associated with second dose of Pfizer‐BioNTech BNT16B2b2 COVID‐19 mRNA vaccine. J Eur Acad Dermatol Venereol. 2021;35(10):e632‐e634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Aghamajidi A, Raoufi E, Parsamanesh G, et al. The attentive focus on T cell‐mediated autoimmune pathogenesis of psoriasis, lichen planus and vitiligo. Scand J Immunol. 2021;93(4):e13000. [DOI] [PubMed] [Google Scholar]
- 8. Pietschke K, Holstein J, Meier K, et al. The inflammation in cutaneous lichen planus is dominated by IFN‐ϒ and IL‐21—a basis for therapeutic JAK1 inhibition. Exp Dermatol. 2021;30(2):262‐270. [DOI] [PubMed] [Google Scholar]
- 9. Xue X, Mi Z, Wang Z, Pang Z, Liu H, Zhang F. High expression of ACE2 on keratinocytes reveals skin as a potential target for SARS‐CoV‐2. J Invest Dermatol. 2021. Jan;141(1):206‐209.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


