Abstract
Aim
To determine compression force variation (CFV) during mechanical cardiopulmonary resuscitation (CPR) and its relationship with CPR-related injuries and survival.
Methods
Adult non-traumatic OHCA patients who had been treated with mechanical CPR were evaluated for CPR-related injuries using chest X-rays, thoracic computed tomography or autopsy. The CFV exerted by the LUCAS 2 device was calculated as the difference between the maximum and the minimum force values and was categorised into three different groups (high positive CFV ≥ 95 newton (N), high negative CFV ≤ -95 N, and low variation for intermediate CFV). The CFV was correlated with the CPR injuries findings and survival data.
Results
Fifty-two patients were included. The median (IQR) age was 57 (49–66) years, and 13 (25%) cases survived until hospital admission. High positive CFV was found in 21 (40.4%) patients, high negative CFV in 9 (17.3%) and a low CFV in 22 (42.3%). The median (IQR) number of rib fractures was higher in the high positive and negative CFV groups compared with the low CFV group [7(1–9) and 9 (4–11) vs 0 (0–6) (p = 0.021)]. More bilateral fracture cases were found in the high positive and negative CFV groups [16 (76.2%) and 6 (66.7%) vs 6 (27.3%) (p = 0.004)]. In the younger half of the sample more patients survived until hospital admission in the low CFV group compared with the high CFV groups [5 (41.7%) vs 1 (7.1%) (p = 0.037)].
Conclusions
High CFV was associated with ribcage injuries. In the younger patients low CFV was associated with survival until hospital admission.
Keywords: Cardiopulmonary resuscitation, Thoracic injuries, Out-of-hospital cardiac arrest, Sudden death
Introduction
High quality chest compressions are the cornerstone of the cardiopulmonary resuscitation (CPR), but it is a complex task to find a balance between the benefit of increased compression depth, cardiac output, and the risk of harming the patient.1., 2. Chest injuries caused by CPR have recently been described as an independent factor for 30-day mortality following out-of-hospital cardiac arrest (OHCA).3 The incidence of serious rib cage injuries in these cases ranges between 39.8% and 63.3% and the shape of the thoracic cage and chest mechanics during CPR can be altered.4., 5.
A review to understand the adverse haemodynamic effect of CPR-related serious injuries showed that it could affect both the thoracic pump and the cardiac pump driving flow theories during CPR.6 The pressure–volume curves of the Campbell diagram show how CPR-related injuries affect the thoracic pump. A reduction in lung-thorax compliance lead to a reduction in the negative intrathoracic pressure in the decompression phase, which in turn causes an impairment in the venous return. Regarding the cardiac pump theory, sternum and multiple rib fractures could flatten the anterior thoracic wall, causing dynamic obstruction of the left ventricular outflow tract during chest compression which was associated with poor outcomes in prolonged CPR.7
It has been suggested that the decrease in compression force as CPR progresses is due to CPR-related injuries.8 At the same time in other cases, the compression force has been reported to increase for, as yet, unknown reasons.9
The LUCAS 2 mechanical CPR device (Stryker/Jolife AB, Lund, Sweden) apply the force that is required to reach the compression depth recommended by the guidelines at a constant rate making possible to explore how the compression force varies during a CPR attempt.10 This study aimed to determine the compression force variation (CFV) measured by the LUCAS 2 device and its relationship with chest injuries and patient survival following CPR.
Methods
Study design and setting
The study period was from January 26, 2016 to November 14, 2016. Data were taken from the ReCaPTa Study, an OHCA prospective registry initiated in the Tarragona region (Catalonia, Spain) in 2014, which contains multiple sources of information. The ReCaPTa Study is focused on the study of sudden cardiac death and CPR-related injuries and the details of the design were published previously.11 The present study was approved by the Ethics Committee of Institut d’Investigació Sanitària Pere Virgili (IISPV), Tarragona (Ref: 166/2019), which waived the need for informed consent from participants. Sistema d’Emergències Mèdiques de Catalunya, the emergency medical service (EMS) in Catalonia, covers the whole of the study territory. When a cardiac arrest is suspected, an advanced life support (ALS) team is dispatched. All ALS teams have been equipped with a LUCAS 2 mechanical CPR device since January 2016. Data on clinical variables and the times of CPR have been collected and recorded by the ALS team who attended the patient via an online application. This study was planned in September 2016.
Participants and autopsy data
On arrival at the scene, the ALS team decide whether to start mechanical compressions based on his clinical decision and current resuscitation guidelines.12 The LUCAS 2 device is used following the manufacturer's recommendations for correct device placement. Before starting chest compression, the suction cup is manually adjusted down to the chest surface on the lower half of the sternum. The present study includes consecutive adult patients with non-traumatic OHCA who were treated with mechanical CPR. Survivors admitted to the hospital underwent chest-X-Ray and/or thoracic CT, and non-survivors were studied by the Tarragona forensic service of the Institut de Medicina Legal i Ciències Forenses de Catalunya. In Spain a forensic autopsy is required for all sudden and unexpected natural death in non-hospitalized persons. All autopsies were performed prospectively according to a specifically designed protocol for the study of CPR-related injuries.13 Serious damages secondary to CPR were defined as in previous studies.14., 5., 4. Serious ribcage damage was defined as one with sternal fracture and/or involved fractures to > 6 ribs if unilateral or > 4 ribs if at least one rib was bilateral. Serious visceral damage was defined as any of the following injuries: haemopericardium, epicardial contusion, dissection or haematoma of the thoracic aorta, pneumothorax, haemothorax, lung haematoma, hepatic laceration, hepatic subcapsular haematoma, spleen injury. The injuries secondary to CPR in survivor were determined from the radiology and CT scan reports.
Mechanical chest compression device data
Compression depth was measured from the piston start position. The measured force was that exerted by the device at the point of maximum compression depth with a maximum accuracy of ±100 newtons (N). The device automatically applies the force required to achieve a compression depth of 53 mm with an accuracy of ±2 mm. A detailed description of the measurements and performance of the LUCAS 2 device has been presented previously.10 The data was downloaded from the LUCAS 2 internal memory card by a specialist technician using a service software. The treated cases in the ambulance and defibrillator records were correlated with those of the ReCaPTa Study by date, time and CPR duration. Two authors (YA and BMH) reviewed the mechanical device data to identify any anomalous readings or errors in placement of the suction cup. Compression force data of the first minute of the CPR were excluded from the analysis. Data on thoracic height, suction cup return distance, compression depth and force (mean and standard deviation) were averaged each minute throughout the CPR episode for each case.
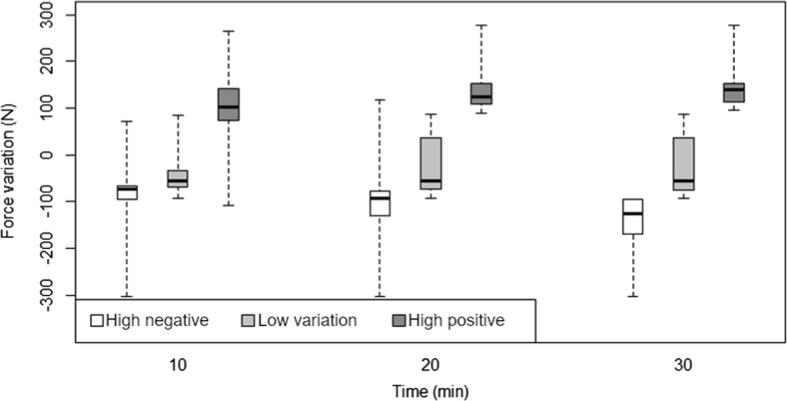
Statistical analysis
CFV was measured as the difference between the maximum and the minimum values of the LUCAS2 device compression force during the first 30 minutes of CPR. The variation was considered positive when the maximum force value was observed after the minimum value along the CPR duration; the variation was considered negative when the maximum value was observed before the minimum value. Thus, for each subject one CFV was determined. To obtain the threshold absolute value for the compression CFV able to predict different injuries with the best trade-off between sensibility and specificity, area under the curve (AUC) of the receiver operating characteristic curves were computed. Following these results, the CFV was categorised in three different groups: high positive CFV for variations with value ≥ 95 N, high negative CFV for variations ≤ -95 N, and low variation for the intermediate CFV. A graphical explanation of the CFV calculation and an analysis of the CFV slope in each case can be found in Figure S2 and S3 of the electronic supplementary material. The quantitative variables were described using the median and the first and third quartiles (IQR), the categorical variables were described using the number of cases and percentages. Group comparisons for quantitative variables were performed using Wilcoxon and Kruskal-Wallis rank-sum tests, and the chi-squared test was used for categorical variables. The association between survival and low CFV was studied both in the total sample and in the younger half of the sample for the effect of age as a confounder. All tests were two-tailed and p < 0.05 was considered statistically significant. All the calculations were made using the R statistical software.
Results
During the study period 210 adult patients with OHCA were treated by the EMS and 110 (52.3%) received mechanical chest compression. Fifty-two patients were included in the final analysis, as shown in the flow chart (Figure S1 of the electronic supplementary material).
The median (IQR) age of the sample was 57 (49–66) years, and 19 (36.5%) patients were women. The initial rhythm was shockable in 15 (28.8%) patients, 25 (48.1%) patients received bystander CPR and total CPR duration was 40 (30–52) min. All patients received manual CPR prior to the deployment of the LUCAS 2 device. Twenty-two patients (42.3%) presented a sternal fracture and 33 (63.5%) presented at least one rib fracture secondary to CPR.
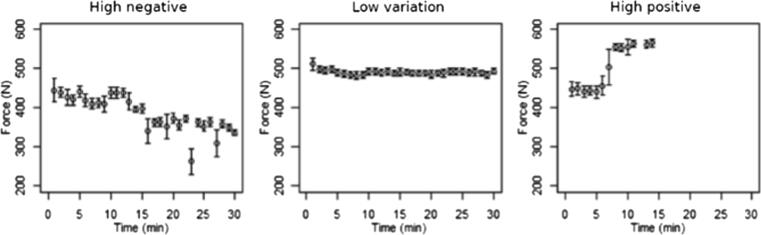
The three types of compression force variation
Detailed examples of the CFV during the mechanical compressions are depicted in Fig. 1. The results of the diagnostic values of the absolute value of the CFV to predict different injuries are shown in Table 1. The optimum threshold of the absolute CFV obtained was 95 N, which predicted sternum fracture, bilateral rib fractures or sternum and bilateral rib fractures with an AUC of 0.74, 0.79 and 0.79, respectively. The three CFV groups are depicted in Fig. 2. Low CFV was found in 22 (42.3%) patients, followed by high positive CFV in 21 (40.4%) patients and high negative CFV in 9 (17.3%) patients. The comparison of the study sample variables according to the type of CFV is shown in Table 2. The mechanical CPR time was significantly lower in the low CFV group (16 min) compared with the high positive CFV group (24 min) and the high negative CFV group (35 min) (p = 0.02). Regarding injuries, the median (IQR) of rib fractures was higher in the group with high positive CFV [9 (4–11)] and with high negative CFV [7 (1–9)] than in the group with low CFV [0 (0–6)] (p = 0.021). The proportion of patients with sternum fractures was higher in the groups with high positive CFV (57.1%) and high negative CFV (66.7%) than the group with low CFV (18.2%) (p = 0.009). The proportion of patients with bilateral fractures was higher in the groups with high positive CFV (76.2%) and high negative CFV (66.7%) than the group with low CFV (27.3%) (p = 0.004).
Fig. 1.
Example cases of chest compression force variation. Case A (9): A 54-year old male received 9 minutes of manual CPR and 107 minutes of mechanical CPR. BMI: 31.2. The median compression force was 330 N with a high negative compression force variation (≤-95 N). The thoracic height at the beginning of CPR was 257 mm and 240 mm at the end. He presented 10 bilateral rib fractures and 1 sternal fracture. Case B (8): A 29-year-old woman received 9 minutes of manual CPR and 41 minutes of mechanical CPR. BMI: 49.5. The median compression force was 490 N with low compression force variation. The thoracic height at the beginning of CPR was 243 mm and 243 mm at the end. There was no thoracic injury secondary to CPR. Case C (5): A 51-year-old male received 27 minutes of manual CPR and 13 minutes of mechanical CPR. BMI: 26.2. The median compression force was 510 N with a high positive compression force variation (≥95 N). The thoracic height at the beginning of CPR was 204 mm and 204 mm at the end. He presented 6 bilateral rib fractures and 1 sternal fracture together with serious visceral injuries. Abbreviations: CPR = cardiopulmonary resuscitation, BMI = body mass index, N = newtons.
Table 1.
Shows the area under the receiver-operating characteristic curve and diagnostic values of the absolute threshold compression force variation predicting different injuries.
| Injuries | AUC | Threshold force variation (N) | Precision | Sensitivity | Specificity | MCC | p-value |
|---|---|---|---|---|---|---|---|
| Any injury | 0.79 | 108 | 1.00 | 0.60 | 1.00 | 0.37 | 0.07 |
| Serious visceral damage | 0.56 | 93 | 0.31 | 0.80 | 0.38 | 0.17 | 0.60 |
| Sternum fracture | 0.74 | 95 | 0.68 | 0.85 | 0.58 | 0.45 | 0.01 |
| Rib fracture | 0.75 | 86 | 0.89 | 0.81 | 0.63 | 0.39 | 0.04 |
| Bilateral rib fractures | 0.79 | 95 | 0.84 | 0.81 | 0.69 | 0.49 | <0.001 |
| Sternum and bilateral rib fractures | 0.79 | 95 | 0.68 | 0.89 | 0.60 | 0.52 | <0.001 |
AUC = area under the curve; N = newton; MCC = Matthews Correlation Coefficient.
Fig. 2.
Compression force variation overtime distributed in three groups (threshold = 95 N).
Table 2.
Shows the comparison of the sample variables according to the type of the compression force variation (CFV).
| Variables | High negative CFV | Low CFV | High positive CFV | p-value |
|---|---|---|---|---|
| N (%) | 9 (17.3) | 22 (42.3) | 21 (40.4) | |
| LUCAS data | ||||
| Initial chest height, mm | 234 (218–255) | 226 (211–238) | 227 (204–244) | 0.69 |
| Compression depth, mm | 51 (50–52) | 51 (49–52) | 51 (49–52) | 0.82 |
| Compression force, Newtons | 430 (410–480) | 425 (380–497.5) | 470 (390–510) | 0.66 |
| No of pauses, (%) | 10 (9–20) | 6 (3–10) | 9 (6–12) | 0.013 |
| Chest compression fraction, % | 77 (74–84) | 89 (82–95) | 84 (78–89) | 0.032 |
| CPR Characteristics | ||||
| Total CPR duration, min | 52 (36–63) | 39 (27–50) | 40 (35–50) | 0.42 |
| Manual CPR time, min | 12 (9–19) | 18 (9–29) | 14 (7–22) | 0.38 |
| Mechanical CPR time, min | 35 (25–43) | 16 (11–22) | 24 (13–38) | 0.02 |
| Bystander CPR | 6 (67) | 10 (45.5) | 9 (43) | 0.46 |
| Ongoing CPR to Hospital | 2 (22.2) | 1 (4.5) | 1 (4.8) | 0.20 |
| ROSC | 4 (44.4) | 8 (36.4) | 5 (23.8) | 0.48 |
| ROSC at Hospital | 1 (11.1) | 8 (36.4) | 4 (19) | 0.24 |
| Discharge alive | 1 (11.1) | 3 (13.6) | 2 (9.5) | 0.91 |
| CPC 1–2 at hospital discharge | 1 (11.1) | 1 (4.5) | 1 (4.8) | 0.49 |
| Cardiac cause of death | 9 (100) | 11 (50) | 12 (57.1) | 0.001 |
| Epidemiological data | ||||
| Age, y | 60 (54–66) | 56 (46–61) | 62 (49–71) | 0.30 |
| Female | 1 (11.1) | 9 (40.9) | 9 (42.9) | 0.22 |
| Damage | ||||
| Sternum fracture | 6 (66.7) | 4 (18.2) | 12 (57.1) | 0.009 |
| Rib fracture | 7 (77.8) | 10 (45.5) | 16 (76.2) | 0.069 |
| Number of rib fractures | 7 (1–9) | 0 (0–6) | 9 (4–11) | 0.021 |
| Bilateral rib fractures | 6 (66.7) | 6 (27.3) | 16 (76.2) | 0.004 |
| Flail chest | 2 (22.2) | 1 (4.5) | 3 (14.3) | 0.33 |
| Sternum and bilateral rib fractures | 6 (66.7) | 3 (13.6) | 12 (57.1) | 0.003 |
| Serious ribcage damage | 6(66.7) | 8(36.4) | 16(76.2) | 0.025 |
| Serious visceral damage | 2 (22.2) | 3 (13.6) | 6 (28.6) | 0.49 |
Data are expressed as median and interquartile range for continuous variables and frequency (N) and percentage for categoric variables. Abbreviations: LUCAS = Lund University Cardiac Arrest System, CFV = Compression force variation, CPR = cardiopulmonary resuscitation, ROSC: return of spontaneous circulation, CPC: cerebral performance category.
Comparison of groups with and without bilateral rib fractures
Table 3 shows the comparison between groups with and without bilateral fractures. Twenty-eight patients (53.8%) had bilateral fractures. The total CPR duration had been longer in subjects with bilateral rib fractures. There were fewer females in the group with bilateral fractures group [13 (54.2%) vs 6 (21.4%) (p = 0.015)].
Table 3.
Shows the comparison of the patients with and without bilateral rib fractures.
| Variables | No bilateral rib fractures | Bilateral rib fracture | p-value |
|---|---|---|---|
| N (%) | 24 (46.2) | 28 (53.8) | |
| Age, y | 58 (46–65) | 57 (50–68) | 0.35 |
| Female | 13 (54.2) | 6 (21.4) | 0.015 |
| Anthropometric variables and autopsy findings* | |||
| BMI, kg/m2 | 30 (27–35) | 30 (27–34) | 0.99 |
| Abdominal perimeter, cm | 102.5 (97.3–108.5) | 105.0 (91.5–112.0) | 0.79 |
| Thorax perimeter, cm | 99.0 (92.0–110.5) | 103.5 (95.3–110.3) | 0.55 |
| Heart weight, g | 343 (277–447) | 495.5 (416.25–569.5) | 0.004 |
| Interventricular cardiac wall, mm | 14 (12–16) | 16 (15–20) | 0.04 |
| Posterior cardiac wall, mm | 15 (12–15) | 16 (15–20) | 0.046 |
| Lungs weight, g | 1064 (1005–1313) | 1422 (1167–1623) | 0.15 |
Data are expressed as median and interquartile range for continuous variables and frequency (N) and percentage for categoric variables. Abbreviations: BMI = body mass index. *Only autopsy data.
Subjects with bilateral rib fractures had a higher heart weight, interventricular cardiac wall and posterior wall thickness [495.5 gr vs 343 gr (p = 0.004); 16 mm vs 14 mm (p = 0.04) and 16 mm vs 15 mm (p = 0.046) respectively]. CPR characteristic, CA-location and other variables are shown in Table S1 of the electronic supplementary material.
Comparison of groups in relation to survival until hospital admission
Among the 52 patients studied, 13 patients (25%) presented survival until hospital admission. The variables in the total study population and the comparison in relation to survival until hospital admission are shown in Table 4. The mechanical CPR time was shorter in the group of survivors [13.0 min vs 24.0 min (p = 0.026)]. Injuries were fewer in the group of survivors until hospital admission. LUCAS2 data, CA-location and other variables are given in Table S2 of the electronic supplementary material.
Table 4.
Shows the comparison of the study sample variables in relation to survival at hospital admission.
| Variables | Total | Survival at hospital admission | No survival | p-value |
|---|---|---|---|---|
| N | 52 (100) | 13 (25) | 39 (75) | |
| Age, y | 57 (48–67) | 65 (48–73) | 56 (49–66) | 0.71 |
| Female | 19 (36.5) | 5 (38.5) | 14 (35.9) | 0.87 |
| CPR Characteristics | ||||
| Total CPR duration, min | 40 (30–52) | 38 (16–42) | 44 (35–57) | 0.03 |
| Manual CPR time, min | 14 (9–26) | 11 (8–29) | 15 (9–24) | 0.97 |
| Mechanical CPR time, min | 22 (13–36) | 13 (12–21) | 24 (16–41) | 0.026 |
| Bystander CPR | 25 (48.1) | 7 (53.8) | 18 (46.2) | 0.63 |
| Ongoing CPR to Hospital | 4 (7.7) | 0 (0) | 4 (10.3) | 0.23 |
| Cardiac cause of death | 32 (61.5) | 10 (76.9) | 22 (56.4) | 0.38 |
| Damages | ||||
| Sternum fracture | 22 (42.3) | 1 (7.7) | 21 (53.8) | 0.004 |
| Rib fractures | 33 (63.5) | 2 (15.4) | 31 (79.5) | <0.001 |
| Number of rib fractures | 6 (0–10) | 0 (0–0) | 7 (1–10) | <0.001 |
| Bilateral rib fractures | 28 (53.8) | 2 (15.4) | 26 (66.7) | 0.001 |
| Sternum and bilateral rib fractures | 21 (40.4) | 1 (7.7) | 20 (51.3) | 0.006 |
| Flail chest | 6 (11.5) | 2 (15.4) | 4 (10.3) | 0.62 |
| Serious visceral damage | 11 (21.2) | 1 (7.7) | 10 (25.6) | 0.17 |
Data are expressed as median and interquartile range for continuous variables and frequency (N) and percentage for categorical variables. Abbreviations: CPR = cardiopulmonary resuscitation.
In the total study population 22 (42.3%) patients presented low CFV and 30 (57.7%) patients high positive or negative CFV. Among the low CFV group, 8 (36.6%) patients survived until hospital admission and among the high positive and negative CFV groups together, 5 (16.7%) patients survived until hospital admission (p = 0.105). In the younger half of the sample (n = 26), 12 (46.2%) patients presented low CFV and 14 patients (53.8%) presented high positive or negative CFV. In this younger sample, the survival until hospital admission was higher in the low CFV group compared with the high positive or negative groups [5 (41.7%) vs 1 (7.1%) p = 0.037].
Discussion
The majority of the included OHCA cases had a high CFV during the first 30 minutes of mechanical CPR. The groups with high CFV were associated with a higher incidence of CPR-related injuries. There was an association between survival outcomes in the younger half of the study population and low CFV where fewer CPR-related injuries were found. Similar results have been recently reported describing CPR-related fractures as an independent factor for 30-day mortality after OHCA.3
Age, gender, duration of CPR and incidence of rib fractures in our study were similar compared to the ARREST trial, which assessed the effectiveness of Extracorporeal CPR in OHCA, which also carries out mechanical compression during transfer to the hospital and cannulation of the patient.15 The results of the present study can therefore be extrapolated to similar studies that report prolonged CPR. Tomlinson et al. reported an increase in the compression force and thus chest stiffness in 18% of patients at a shallower compression depth and shorter CPR duration than in our sample.8 Russell et al. reported that only 24% of patients receiving prolonged manual CPR guided by a feedback device presented an increase in chest stiffness.9 In this study, the percentage of patients reaching the recommended guideline depth of 50 mm and the incidence of complete sternal return was lower in the stiffer chest quintile, highlighting the deterioration of the mechanical properties of the chest in this group of patients. The rescuer can adapt the depth of compression during manual CPR if the stiffness of the chest increases whereas the mechanical chest compression devices apply a fixed depth that can be more forceful in some cases, which might explain our findings.16., 17.
As the chest wall materials fatigue after repeated loading, there is a loss of structural integrity of the materials, which can lead to fractures. Regarding the elastoplastic behaviour of the ribs, the fractures result in a loss of the elastic component and a drop in the elastic secant stiffness leading to a more unpredictable response to loads.18 The loss of the chest wall elasticity during CPR has been associated with worse survival outcomes which might explain our association between low CFV and survival.19 Basically, the main forces involved in thoracic biomechanics during CPR are the elastic force exerted by the osseous-cartilaginous system of the rib cage and the damping force exerted by the intrathoracic viscera.20 In the case of negative CFV, the elastic force falls as a result of the deterioration in the materials of the ribcage, but the damping force remains unchanged. However, in the case of positive CFV, we hypothesise that the elastic force falls equally, but there is an increase in the damping force that could be the result of two factors. Firstly, the moulding and loss of the elastic component of the chest secondary to ribcage injuries lead to the sternum falling down over the anterior face of the heart, thus gradually increasing the effect of the cardiac damping. Secondly, the stone heart phenomenon and the increasing thickness of the heart walls during prolonged CPR may also result in an increase in the damping force.21
In the present study, the patients with bilateral fractures had significantly larger hearts than those without, which might suggest higher initial chest stiffness and a lower fracture threshold due to the increased initial damping force exerted by the intrathoracic viscera and especially by the heart, highlighting its key role in the CPR chest mechanics. This can be seen in a previously published 4D simulation.22
Regarding the clinical implications of this study, high positive or negative CFV can occur gradually or suddenly, as shown in Fig. 1, and could be caused by rib fractures. The depth of compression and duration of CPR are responsible for the fatigue of rib cage materials and are the two main risk factors for CPR injuries.23 Preventing high positive or negative CFV may help to maintain the elastic properties of the thorax and improve haemodynamics. Taking into account that it has been found maximum survival in the depth interval of 40.3 to 55.3 mm adapting the depth of compression during prolonged mechanical CPR might therefore be beneficial in some cases, although this remains speculative.24 In addition, we must keep in mind that the CPR injuries risk factors not only depend on a deterioration in the biological materials that occurs with ageing but also might depend on the geometry of the rib cage. Based on that theory, there might be two phenotypes that are more likely to present injuries, elderly women and men with a large chest, so we could expect worse survival outcomes in these patients after prolonged CPR.6 That said, the higher risk of CPR injuries in females has not been seen in this study, which might be due to the relatively young age of the sample. A successful, prolonged CPR in a young woman with a low incidence of CPR injuries supports the suggestion of good chest mechanics performance in these cases.25 Consider the preservation of the chest biomechanical properties among the elements of the high quality compressions in prolonged CPR may initiate a new field of research into avoidable CPR-related injuries and personalised CPR.
Our study has several limitations. One was the small sample size. The association found between the low CFV and survival will need to be studied in a larger population. The use of X-ray as an imaging test may underestimate the diagnosis of CPR injuries comparing with autopsies and with thoracic CT.26., 27. Part of the patients treated with mechanical CPR who were declared dead in the field were not autopsied. All patients had received manual compression prior to the mechanical compression and no data on the manual CPR depth of compression was available so not all the injuries found can definitively be attributed to the mechanical compression alone. Only the variation in force during the first thirty minutes of mechanical CPR was studied, therefore several cases were not studied for the total CPR time. It cannot be ruled out that small variations in compression force might have occurred due to movement of the mechanical compressor piston on the chest. The CFV not only occurs as a result of thoracic cage fractures but might also be due to ligament distension or luxations that frequently occur in the sternal-costal joint, but this was not evaluated in this study.
Conclusion
In summary, high CFV was presented in most of the cases and was associated with a high incidence of CPR-related injuries compared with those with low variation CFV. The high CFV can have a positive or negative sign depending on whether the compression force increases or decreases during CPR. Patients younger than 57 years predominantly had low CFV and this was associated with survival until hospital admission. The high variation in compression force could be a marker of loss of chest wall elasticity and warrants further studies to move towards a more personalised CPR.
Conflicts of interest.
None.
CRediT authorship contribution statement
Youcef Azeli: Conceptualization, Methodology, Investigation, Validation, Project administration, Data curation, Writing – original draft. Eneko Barbería: Conceptualization, Investigation, Writing – review & editing. Alberto Fernandez: Investigation, Formal analysis, Writing – review & editing. Silvia García-Vilana: Investigation, Formal analysis, Writing – review & editing. Alfredo Bardají: Conceptualization, Investigation, Resources, Writing – review & editing. Bjarne Madsen Hardig: Conceptualization, Methodology, Investigation, Validation, Data curation, Writing – review & editing.
Acknowledgments
Acknowledgements
We would like to thank the research team of the Institute of Legal Medicine and Forensic Science of Catalonia involved in the ReCaPTa study for their collaboration: Inés Landin, Pilar Torralba, Cristina Amaya, Carlos Laguna and Ruth Alvarez.
Grants/Funding
The Jolife AB/Stryker company provided the program to extract the LUCAS 2 data and contributed to the costs for the data download from the device but had no influence on the interpretation of the results. The ReCaPTa study received a grant from the Catalan Resuscitation Council.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2022.100242.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Handley A.J. Press hard – But perhaps not too hard. Resuscitation. 2014;85:153–154. doi: 10.1016/j.resuscitation.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 2.Cone D.C. Push hard, push fast, do not stop—optimal chest compression rate and depth. JAMA Cardiol. 2019;4:908. doi: 10.1001/jamacardio.2019.2838. [DOI] [PubMed] [Google Scholar]
- 3.Karasek J., Slezak J., Stefela R., Topinka M., Blankova A., Doubková A., et al. CPR-related injuries after non-traumatic out-of-hospital cardiac arrest: survivors versus non-survivors. Resuscitation. 2022;171:90–95. doi: 10.1016/j.resuscitation.2021.12.036. [DOI] [PubMed] [Google Scholar]
- 4.Azeli Y., Barbería E., Jiménez-Herrera M., Ameijide A., Axelsson C., Bardají A. Serious injuries secondary to cardiopulmonary resuscitation: incidence and associated factors. Emergencias. 2019;31:327–334. [PubMed] [Google Scholar]
- 5.Koster R.W., Beenen L.F., van der Boom E.B., Spijkerboer A.M., Tepaske R., van der Wal A.C., et al. Safety of mechanical chest compression devices AutoPulse and LUCAS in cardiac arrest: a randomized clinical trial for non-inferiority. Eur Heart J. 2017;38:3006–3013. doi: 10.1093/eurheartj/ehx318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azeli Y., Lorente Olazabal J.V., Monge García M.I., Bardají A. Understanding the adverse hemodynamic effects of serious thoracic injuries during cardiopulmonary resuscitation: a review and approach based on the Campbell diagram. Front Physiol. 2019;10:6. doi: 10.3389/fphys.2019.01475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Catena E., Ottolina D., Fossali T., Rech R., Borghi B., Perotti A., et al. Association between left ventricular outflow tract opening and successful resuscitation after cardiac arrest. Resuscitation. 2019;138:8–14. doi: 10.1016/j.resuscitation.2019.02.027. [DOI] [PubMed] [Google Scholar]
- 8.Tomlinson A.E., Nysaether J., Kramer-Johansen J., Steen P.A., Dorph E. Compression force–depth relationship during out-of-hospital cardiopulmonary resuscitation. Resuscitation. 2007;72:364–370. doi: 10.1016/j.resuscitation.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 9.Russell J.K., González-Otero D.M., Leturiondo M., Ruiz de Gauna S., Ruiz J.M., Daya M.R. Chest stiffness dynamics in extended continuous compressions cardiopulmonary resuscitation. Resuscitation. 2021;162:198–204. doi: 10.1016/j.resuscitation.2021.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Beesems S.G., Hardig B.M., Nilsson A., Koster R.W. Force and depth of mechanical chest compressions and their relation to chest height and gender in an out-of-hospital setting. Resuscitation. 2015;91:67–72. doi: 10.1016/j.resuscitation.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 11.Azeli Y., Barbería E., Jiménez-Herrera M., Bonet G., Valero-Mora E., Lopez-Gomariz A., et al. The ReCaPTa study - a prospective out of hospital cardiac arrest registry including multiple sources of surveillance for the study of sudden cardiac death in the Mediterranean area. Scand J Trauma Resusc Emerg Med. 2016;24(1) doi: 10.1186/s13049-016-0309-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soar J., Nolan J.P., Böttiger B.W., Perkins G.D., Lott C., Carli P., et al. European resuscitation council guidelines for resuscitation 2015. Resuscitation. 2015;95:100–147. doi: 10.1016/j.resuscitation.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 13.Azeli Y., Barbería E., Landín I., Torralba P., Amaya C., Laguna C. Lesiones por reanimación cardiopulmonar en autopsias forenses: protocolo del Registro Clínico-Patológico de Tarragona (ReCaPTa) Rev Esp Med Leg. 2016;42:120–125. [Google Scholar]
- 14.Krischer J.P., Fine E.G., Davis J., Nagel E.L. Complications of cardiac resuscitation. Chest. 1987;92:287–291. doi: 10.1378/chest.92.2.287. [DOI] [PubMed] [Google Scholar]
- 15.Yannopoulos D., Bartos J., Raveendran G., Walser E., Connett J., Murray T.A., et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. The Lancet. 2020;396:1807–1816. doi: 10.1016/S0140-6736(20)32338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smekal D., Lindgren E., Sandler H., Johansson J., Rubertsson S. CPR-related injuries after manual or mechanical chest compressions with the LUCASTM device: a multicentre study of victims after unsuccessful resuscitation. Resuscitation. 2014;85:1708–1712. doi: 10.1016/j.resuscitation.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 17.Gao Y., Sun T., Yuan D., Liang H., Wan Y., Yuan B., et al. Safety of mechanical and manual chest compressions in cardiac arrest patients: a systematic review and meta-analysis. Resuscitation. 2021;169:124–135. doi: 10.1016/j.resuscitation.2021.10.028. [DOI] [PubMed] [Google Scholar]
- 18.Kieser J.A., Weller S., Swain M.V., Neil Waddell J., Das R. Compressive rib fracture: Peri-mortem and post-mortem trauma patterns in a pig model. Leg Med. 2013;15:193–201. doi: 10.1016/j.legalmed.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Beger S., Sutter J., Vadeboncoeur T., Silver A., Hu C., Spaite D.W., et al. Chest compression release velocity factors during out-of-hospital cardiac resuscitation. Resuscitation. 2019;145:37–42. doi: 10.1016/j.resuscitation.2019.09.024. [DOI] [PubMed] [Google Scholar]
- 20.Jalali A., Simpao A.F., Nadkarni V.M., Berg R.A., Nataraj C. A novel nonlinear mathematical model of thoracic wall mechanics during cardiopulmonary resuscitation based on a porcine model of cardiac arrest. J Med Syst. 2017;41:20. doi: 10.1007/s10916-016-0676-1. [DOI] [PubMed] [Google Scholar]
- 21.Bartos J.A., Grunau B., Carlson C., Duval S., Ripeckyj A., Kalra R., et al. Improved survival with extracorporeal cardiopulmonary resuscitation despite progressive metabolic derangement associated with prolonged resuscitation. Circulation. 2020;141:877–886. doi: 10.1161/CIRCULATIONAHA.119.042173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hansen K., Machin R., James J., Coats T., Rutty G.N. A look inside cardiopulmonary resuscitation: A 4D computed tomography model of simulated closed chest compression. A proof of concept. Resuscitation. 2020;153:149–153. doi: 10.1016/j.resuscitation.2020.05.037. [DOI] [PubMed] [Google Scholar]
- 23.Ram P., Menezes R.G., Sirinvaravong N., Luis S.A., Hussain S.A., Madadin M., et al. Breaking your heart—a review on CPR-related injuries. Am J Emerg Med. 2018;36(5):838–842. doi: 10.1016/j.ajem.2017.12.063. [DOI] [PubMed] [Google Scholar]
- 24.Stiell I.G., Brown S.P., Nichol G., Cheskes S., Vaillancourt C., Callaway C.W., et al. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. 2014;130:1962–1970. doi: 10.1161/CIRCULATIONAHA.114.008671. [DOI] [PubMed] [Google Scholar]
- 25.Riera J., Argudo E., Ruiz-Rodríguez J.C., Rodríguez-Lecoq R., Ferrer R. Full neurological recovery 6 h after cardiac arrest due to accidental hypothermia. The Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30751-0. [DOI] [PubMed] [Google Scholar]
- 26.Lederer W., Mair D., Rabl W., Baubin M. Frequency of rib and sternum fractures associated with out-of-hospital cardiopulmonary resuscitation is underestimated by conventional chest X-ray. Resuscitation. 2004;60:157–162. doi: 10.1016/j.resuscitation.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 27.Kim E.Y., Yang H.J., Sung Y.M., Cho S.H., Kim J.H., Kim H.S., et al. Multidetector CT findings of skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation. 2011;82:1285–1288. doi: 10.1016/j.resuscitation.2011.05.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.