Abstract
Introduction and importance
Epidermoid cysts are developmental cysts of the retrorectal space. They are benign lesions resulting from ectodermal inclusion during neural tube closure. Generally, they are misdiagnosed given that symptoms are often vague and nonspecific. They have a high infection rate (up to 30%) and can be easily mistaken for perirectal abscesses.
Case presentation
We present a case of an epidermoid cyst in a 58-year-old woman with a retrorectal cyst mistaken for a perianal abscess, which was initially incised and drained and then, after MRI investigation, an anterior resection was performed.
Clinical discussion
Epidermoid cysts have a high infection rate (up to 30%). Infected cysts can be easily mistaken for perirectal abscesses, pilonidal disease, or fistulae in ano. CT (computed tomography) used in conjunction with MRI (Magnetic Resonance Imaging) is the gold standard for establishing the diagnosis. A biopsy is never indicated. Surgery is the best treatment, even for asymptomatic lesions.
Conclusion
Epidermoid cysts are rare and generally misdiagnosed. In fact, symptoms are often vague and nonspecific. Radiologic imaging (especially MRI) is essential for surgical planning and biopsy should be avoided. Once a presacral lesion is diagnosed, even if the patient is asymptomatic, complete resection remains the treatment of choice because of the risk of infection.
Keywords: Abdominal surgery, Epidermal cyst, Histological finding, Magnetic resonance imaging, Case report
Highlights
-
•
Epidermoid cysts have a high infection rate and can be easily mistaken for perirectal abscesses, or fistulae in ano.
-
•
CT (computed tomography) used in conjunction with MRI (Magnetic Resonance Imaging) is the gold standard for the diagnosis.
-
•
A biopsy is never indicated.
-
•
Surgery is the best treatment even for asymptomatic lesions.
1. Introduction and importance
Epidermoid cysts are developmental cysts of the retrorectal space. They are typically benign and unilocular lesions resulting from the failure of ectodermal tube to close [1], [2]. Given the vagueness and non-specificity of symptoms, these lesions are generally misdiagnosed and easily mistaken for perirectal abscesses [3]. In addition to this, They are highly predisposed to infections in up to 30% of cases.
We report a rare case of a retro rectal cyst mistaken for a perianal abscess, which was initially, incised, and drained and then, after MRI investigation, an anterior resection was performed. The patient was operated in an academic teaching hospital.
This case report is reported in line with SCARE guidelines [4].
2. Case presentation
A 58-year-old housewife, right handed, nonsmoker, with no drug history, and unremarkable medical, surgical, family or psychosocial history, was referred by her family physician to our facility with a 5-day history of perianal pain. She had no change in bowel habits, bleeding, or difficulty in defecation.
At presentation she had a BMI (Body Mass Index) of 30 kg/m 2 and a body temperature of 38 °C. Examination of the perirectal region showed a tender and swollen lump with red and warm tissues. The digital rectal exam was refused by the patient.
Her white blood cell count was 10,450 ele/ml and the level of C-reactive protein (CRP) reached 20 mg/L. The renal function analysis was normal.
A perirectal abscess was suspected, and the surgeon performed a surgical incision and drainage, bringing a viscid green-yellow material (Fig. 1).
Fig. 1.
Viscid green-yellow material.
A retrorectal cyst was suspected and the surgeon chose not to start with a CT scan and to directly perform an MRI, which was performed one week later showing a retrorectal cyst of 14 ∗ 10 cm. The cyst was slightly hyperintense to cerebrospinal fluid on T1-weighted images and on T2-weighted images with a thin wall and some thin septation. It had an increased signal intensity on diffusion-weighted Images with a thin peripheral enhancement without any vegetation. The cyst did not have any sign of extension to the rectum or to the vagina (Fig. 2, Fig. 3).
Fig. 2.

Retrorectal cyst of 14 ∗ 10 cm with a thin wall and some thin septation without any vegetation or sign of extension to the rectum or to the vagina (axial view).
Fig. 3.
Retrorectal cyst sagittal view.
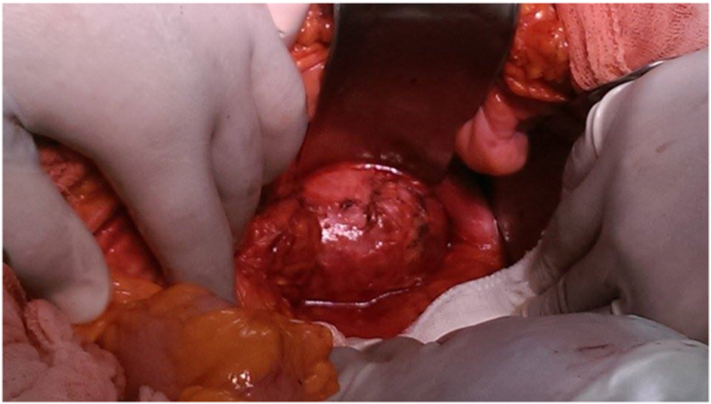
The patient underwent surgery with median incision approach, under general anesthesia and in supine position. Surgical exploration revealed a 14 cm mass bulging in the pouch of Douglas. First, the anterior portion of the lesion was separated from the mesorectum, and then from the presacral fascia, the dissection was easy and there were no rigid adhesions with the mesorectal or presacral wall (Fig. 4). This resection using the anterior (transabdominal) approach was performed by a professor of surgery.
Fig. 4.
Intraoperative view of 14 cm mass bulging in the pouch of Douglas.
After surgery, the patient was placed in the intensive care unit for 48 h and then transferred to the department of surgery. The patient was discharged two days later.
The histopathological examination showed an epidermoid cyst with stratified squamous cells without any skin appendages (Fig. 5).
Fig. 5.
Stratified squamous cells without any skin appendages.
No recurrence was observed at one-year follow-up.
3. Clinical discussion
The retrorectal space is a potential space that only becomes real when a mass grows within it [5]. This region contains structures derived from embryonic neuroectoderm, notochord, and hindgut. A heterogeneous group of both benign and malignant tumors originating from those embryologic remnants can be found in this space [6].
Approximately two thirds of all presacral tumors are congenital, and more than 60% of these are developmental cysts [7].
Developmental cysts are the most common retrorectal cystic lesions in adults, occurring mostly in middle-aged women. They are classified as epidermoid cysts, dermoid cysts, enteric cysts (tailgut cysts and cystic rectal duplication), and neurenteric cysts according to their origin and histopathologic features [8].
Epidermoid cysts are composed of stratified squamous cells. They are typically benign unilocular lesions that do not contain skin appendages. These lesions have a high infection rate (up to 30%), and can be easily mistaken for perirectal abscesses, pilonidal disease, or fistulae in ano. When misdiagnosed and managed as perirectal abscesses, fistula in ano, or pilonidal disease, the secondary infection rate is 30%. [9] When not infected, these cysts tend to be filled with a viscid green-yellow material [10].
They are most diagnosed in females in the fourth and fifth decades of life. The symptoms differ according to the tumor size, location and the presence or not of infection [9]. The clinical presentation of retrorectal developmental cysts is often non-specific and half of them are asymptomatic and are incidentally discovered during routine physical examination [11].
The most frequent symptoms are anal pain and perianal discomfort, difficulty in defecation, tenesmus, changes in bowel habits, bleeding, thin stool, incontinence and a sacrococygeal mass [12].
Currently, CT, used in conjunction with MRI, is the gold standard in diagnosing retrorectal tumors [13]. MRI is very useful for characterizing masses in the presacral space and specifically determining the size, location, and extent of the disease. This information is valuable for patient management, especially for surgical planning [14].
On CT images, epidermoid cysts generally appear as thin walled cystic masses with fluid density and may contain calcification [15].
On MRI, epidermoids are typically isointense or slightly hyperintense to cerebrospinal fluid. Fat-containing portions of dermoids demonstrate increased signal intensity on T1-weighted images and decreased signal on T2-weighted images [14]. Their heterogeneous signal intensity, as seen on both T1- and T2-weighted MR images, is due to keratinous materials [15].
Uncommonly, the cyst may contain air due to an anorectal fistula [5].
Other imaging techniques that may assist in the diagnosis and management of retrorectal tumors include angiogram and venogram, endorectal ultrasound (ERUS), and fistulograms [13].
In general, a biopsy is never indicated. For resectable lesions, surgical resection is the best diagnostic and therapeutic option [16]. In fact, those lesions are usually benign and there is a risk of secondary infection [17] and the most definitive and effective tissue biopsy is achieved by complete surgical excision [7]. In fact, incomplete removal will increase local recurrence.
Malignant transformation has also been documented in tailgut cysts and epidermoid cysts in only one observation [18].
Surgery is advocated, even for asymptomatic lesions, for several reasons. First, approximately 50% of developmental cysts will become spontaneously infected. Second, although rare, developmental cysts have the potential for malignant degeneration [18]. This has been reported for enteric cysts and tailgut cysts. Last, for women of childbearing age, a presacral mass may complicate vaginal delivery by causing dystocia [7].
CT and MRI will help define the margins of resection and the relationship of the tumor to the sacral level. The common approaches for resection of retrorectal tumors are the anterior (transabdominal), the combined abdominoperineal and the posterior (perineal) approaches [13].
Generally, tumors above the level of S3 will require an anterior or combined approach while small lesions below the level of S3 may be removed utilizing the posterior approach [17].
3.1. Anterior approach (transabdominal)
The anterior approach is performed when the lowest portion of the lesion is above the level of S4. The mesorectum should first be dissected off the anterior portion of the lesion, then the lesion must be separated from the presacral fascia [13].
3.2. Combined approach (abdominoperineal)
A combined approach is reserved for those lesions that are above the S3 vertebrae [19].
3.3. Posterior approach (perineal)
The posterior approach is ideal for small retrorectal tumors that do not extend above the level of S3 [13]. It can be an intersphincteric approach for very low lesion or the parasacrococcygeal approach for deeper or higher lesions.
Overall survival for benign tumors is ≈100% [13]. Recurrence rates vary and are dependent on the extent and completeness of resection. With incomplete resection, the patients are predisposed to higher recurrence rates [20].
4. Conclusion
Retro rectal tumors are rare and heterogeneous. Generally, they are misdiagnosed. In fact, symptoms are often vague and nonspecific. Radiologic imaging (especially MRI) is essential for surgical planning and biopsy should be avoided. Once presacral lesion is diagnosed, even if the patient is asymptomatic, complete resection remains the treatment of choice.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
There were no funding sources for this report.
Ethical approval
It is exempted from ethical approval because it is an observation report.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Dr. Mossaab Ghannouchi: primary author and operating surgeon, Dr. mohamed ben khlifa: coauthor, Dr. karim Nacef, Dr.aminachaka, dr olfa zoukar: involved in the clinical evaluation of the patient, Prof. moez boudhokhan: supervision of report writing.
Research registration
Not applicable.
Guarantor
Mossaab Ghannouchi.
Declaration of competing interest
The authors have no conflicts of interest to declare.
References
- 1.Stewart R.J.H.W.G., Parks T.G. The presentation and management of presacral tumours. Br. J. Surg. 1986;73(2):153–155. doi: 10.1002/bjs.1800730227. [DOI] [PubMed] [Google Scholar]
- 2.BRW Jao S.W., Jr Spencer R.J., Reiman H.M., Ilstrup D.M. Retrorectal tumors. Mayo clinic experience, 1960-1979. Dis Colon Rectum. 1985;28(9):644–652. doi: 10.1007/BF02553440. [DOI] [PubMed] [Google Scholar]
- 3.Abel M.E.N.R., Prasad M.L., Pearl R.K., Orsay C.P., Abcarian H. Parasacrococcygeal approach for the resection of retrorectal developmental cysts. Dis. Colon Rectum. 1985;28(11):855–858. doi: 10.1007/BF02555492. [DOI] [PubMed] [Google Scholar]
- 4.FT Agha R.A., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. International Journal of Surgery. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Yang B.L., et al. Retrorectal tumors in adults: magnetic resonance imaging findings. World J. Gastroenterol. 2010;16(46):5822–5829. doi: 10.3748/wjg.v16.i46.5822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GPHN S. Rectum and Anus. Quality Medical Publishing; 1999. Retrorectal tumors. Principles and practice of surgery for the colon; pp. 427–445. [Google Scholar]
- 7.Kalady M.F., Ludwig K.A. Presacral developmental cysts. Semin. Colon Rectal Surg. 2004;15(1):12–18. [Google Scholar]
- 8.Dahan H., et al. Retrorectal developmental cysts in adults: clinical and radiologic-histopathologic review, differential diagnosis, and treatment. RadioGraphics. 2001;21(3):575–584. doi: 10.1148/radiographics.21.3.g01ma13575. [DOI] [PubMed] [Google Scholar]
- 9.Bullard Dunn K. Retrorectal tumors. Surg. Clin. North Am. 2010;90(1):163–171. doi: 10.1016/j.suc.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Ludwig K.A.R.H. Retrorectal tumors. Clin Colon Rectal Surg. 2002;15:285–293. [Google Scholar]
- 11.Hayashi M., Tomita S., Fujimori T., Nagata H., Kubota K., Shoda A., et al. Retrorectal epidermoid cyst with unusually elevated serum SCC level, initially diagnosed as an ovarian tumor. Rare Tumors. 2009;1(1) doi: 10.4081/rt.2009.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baek S.W.K.H., Yoon J.Y., et al. Clinical study and review of articles (Korean) about retrorectal developmental cysts in adults. J. Korean Soc. Coloproctol. 2011;27:303–314. doi: 10.3393/jksc.2011.27.6.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neale J.A. Retrorectal tumors. Clin. Colon. Rectal Surg. 2011;24(3):149–160. doi: 10.1055/s-0031-1285999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Malley C.M., Remer E.M., Delaney C. Imaging of the presacral space. Semin. Colon Rectal Surg. 2004;15(1):2–11. [Google Scholar]
- 15.Yang D.M.Y.M., Kim H.S., Kim H.S., Chung S., Chung J.W., et al. CT and MR findings of presacral epidermoid cyst. J. Korean Radiol. Soc. 1999;41:545–547. [Google Scholar]
- 16.Hobson K.G., Ghaemmaghami V., Roe J.P., Goodnight J.E., Khatri V.P. Tumors of the retrorectal space. Dis. Colon Rectum. 2005;48(10):1964–1974. doi: 10.1007/s10350-005-0122-9. [DOI] [PubMed] [Google Scholar]
- 17.Dozois E.J., Jacofsky D.J., Dozois R.R. In: The ASCRS Textbook of Colon and Rectal Surgery. Wolff B.G., Fleshman J.W., Beck D.E., Pemberton J.H., Wexner S.D., Church J.M., et al., editors. New York, NY; Springer, New York: 2007. Presacral Tumors; pp. 501–514. [Google Scholar]
- 18.Yang D.M., Kim H.C., Lee H.L., Lee S.H., Kim G.Y. Squamous cell carcinoma arising from a presacral epidermoid cyst: CT and MR findings. Abdom. Imaging. 2008;33(4):498–500. doi: 10.1007/s00261-007-9287-0. [DOI] [PubMed] [Google Scholar]
- 19.Wolpert A., Beer-Gabel M., Lifschitz O., Zbar A.P. The management of presacral masses in the adult. Tech. Coloproctol. 2002;6(1):43–49. doi: 10.1007/s101510200008. [DOI] [PubMed] [Google Scholar]
- 20.Hobson K.G., Ghaemmaghami V., Roe J.P., Goodnight J.E., Khatri V.P. Tumors of the retrorectal space. Dis. Colon Rectum. 2005;48(10):1964–1974. doi: 10.1007/s10350-005-0122-9. [DOI] [PubMed] [Google Scholar]