Abstract
Purpose
To evaluate the response and safety of an inactivated vaccine (Sinovac Life Sciences Co., Ltd., Beijing, China) for coronavirus disease 2019 (COVID-19) in liver transplant (LTx) recipients from China.
Patients and Methods
Thirty-five recipients post LTx from the First Affiliated Hospital of Zhejiang University School of Medicine who received inactivated vaccine from June to October 2021 were screened. Information regarding vaccine side effects and clinical data were collected.
Results
Thirty-five LTx recipients were enrolled, with a mean age of 46 years, and most patients were male (30, 85.71%). All the participants had a negative history of COVID-19 infection. Predictors for negative response in the recipients were interleukin-2 receptor (IL-2R) induction during LTx, shorter time post LTx and application of a derivative from mycophenolate acid (MPA). No serious adverse events were observed during the progress of vaccination or after the vaccination.
Conclusion
LTx recipients have a substantially partial immunological response to the inactivated vaccine for COVID-19. IL-2R induction during LTx, a shorter time post LTx and the application of a derivative from MPA seem to be predictors for a negative serological immunoglobulin G (IgG) antibody response in recipients. The findings require booster vaccination in these LTx recipients.
Keywords: liver transplantation, 2019-nCoV vaccination, SARS-CoV-2 infection, disease control, epidemiology, immune responses
Introduction
Three waves of world wild emerging severe infectious disease pandemics have been presented during this century because of the coronavirus. The severe acute respiratory syndrome (SARS) outbreak in southern China since 2002 has spread to 8096 cases from 29 countries, with a mortality of 9.6%.1 Middle East respiratory syndrome (MERS), an outbreak in Saudi Arabia that became a pandemic since 2012, has spread to 1728 cases from 27 countries, with a mortality of 36.1%.1,2 The third epidemic is coronavirus disease 2019 (COVID-19), notified as unexplained pneumonia at the end of 2019, spreading to the world with 364 million cases updated daily, and the mortality is nearly 1.5%.3 This unprecedented epidemic urges the greatest efforts to develop preventive vaccines for COVID-19. The inactivated vaccine has been produced by companies in China and has become a global platform for vaccination to control irradiation with COVID-19.4
Recently, a weak seroconversion rate (10.8–47.5%) with the inoculation of mRNA vaccine was reported in an immunocompromised population.5,6 However, there is still a lack of reports of the same population with the inoculation of inactivated vaccine. Therefore, we tried to estimate the response and safety of inactivated vaccines for COVID-19 in LTx recipients from the First Affiliated Hospital, Zhejiang University School of Medicine, which owns the National Center for Infectious Diseases and is one of the largest transplant centers in China.
The response and safety of the inactivated vaccine have been evaluated.4,7 However, liver transplant (LTx) recipients, as a group under the immunocompromised with increased infection risk and decreased efficacy of the vaccine, should be given more attention by clinical and preventive doctors. LTx recipients have worse outcomes from COVID-19 than those without liver disease. Therefore, many societies have recommended vaccination of this highly vulnerable population.
Materials and Methods
Patients
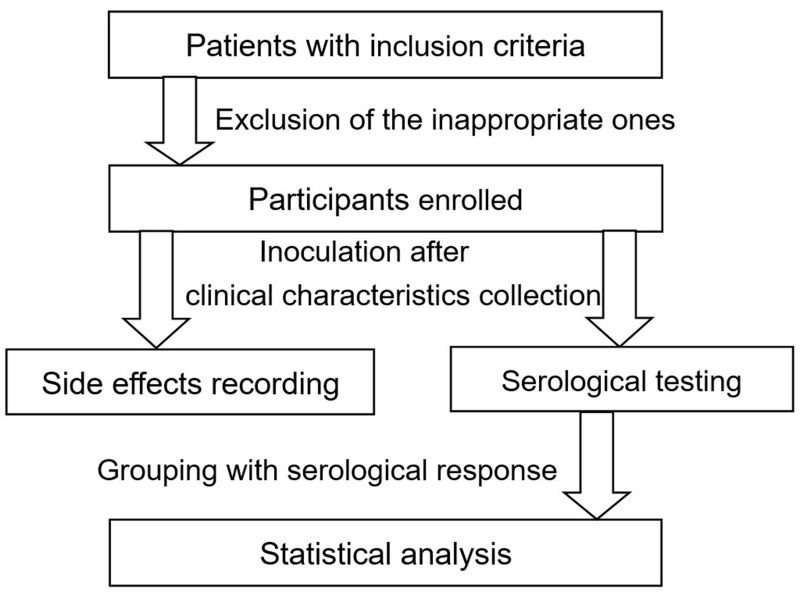
Thirty-five LTx recipients who underwent liver transplantation with the grafts voluntarily donated all from written informed consent during the period of 2010–2020 were followed up in our hospital. The inclusion criteria included patients aged 18–69 years old who had stable liver or kidney function and immunosuppressor concentrations. Exclusion criteria included patients 1) with fever and active malignancy, 2) being pregnant and in lactation, 3) hospitalized less than one month, 4) transplanted less than one year, 5) transplanted ABO incompatible, 6) with a history of COVID-19 infection in the record of the government, 7) positive serum human immunodeficiency virus or 8) unable to provide informed consent. The estimated glomerular filtration rate (eGFR) was calculated with the MDRD formula. The flow chart of the evaluation is shown in Figure 1.
Figure 1.
Flow chart of the evaluation.
The study was approved by the Clinical Research Ethics Committee of The First Affiliated Hospital, Zhejiang University School of Medicine (Reference Number 2021-IIT-f487), following the Declaration of Helsinki and the Declaration of Istanbul. Vaccine insurance was offered by the researcher for the participants. Informed consent was obtained from all the study participants prior to study commencement.
All the participants received two injections with an interval time of 3 to 4 weeks of inactivated vaccine (SinoVac Biotech Co., Ltd., Beijing, China) 3 μg/0.5 mL at the community health center from June to October 2021, following the guidelines of the local government.
Data Collection
We collected clinical characteristics (age, sex, BMI), information on LTx, comorbidities (diabetes, hypertension, chronic obstructive pulmonary disease, heart failure, chronic kidney disease, malignancy, smoking history and ongoing alcoholism) and concomitant medications of all patients who were eligible for vaccination, grouped by serological response, as shown in Table 1.
Table 1.
Baseline Characteristics of LTx Recipients and Comparison According to Serological Response
| Characteristics | Entire (n=35) | Seronegative (n=29) | Seropositive (n=6) | P value | Missing |
|---|---|---|---|---|---|
| Age, years | 47 (40–53) | 47 (41–53) | 47 (31–55) | 0.685 | 0 |
| Male sex | 30 (85.7) | 26 (89.6) | 4 (66.7) | 0.143 | 0 |
| BMI, kg/m2 | 23.8 (20.8–25.6) | 23.9 (21.9–25.7) | 20.4 (18.9–24.4) | 0.124 | 0 |
| Time since LT | 2.4 (2.0–5.5) | 2.3 (1.9–4.0) | 6.3 (2.3–8.6) | 0.025 | 0 |
| IL-2R Induction | 31 (88.5%) | 28 (96.5%) | 3 (50%) | 0.011 | 0 |
| Immunosuppressant | 0.897 | 0 | |||
| Tacrolimus | 28 | 23 | 5 | 0 | |
| Cyclosporin | 1 | 1 | 0 | 0 | |
| Sirolimus | 6 | 5 | 1 | 0 | |
| MPA | 15 (42.8%) | 15 (52.7%) | 0 (0%) | 0.027 | 0 |
Abbreviations: LTx, liver transplant; BMI, body mass index; IL-2R, interleukin-2 receptor; MPA, derivatives from mycophenolic acid.
Safety
The enrolled recipients were followed up within 3 days after inoculation. The following adverse events were reported: systemic (dizziness, fever, chills, headache, fatigue, myalgia, arthralgia, nausea, vomiting, and diarrhea) and/or local (pain, redness, swelling, and lymphadenopathy) on a scale (score of 0–5, as free of side effect, side effect without need of drugs, need of drugs but without hospitalization, hospitalized but without intensive care, hospitalized with intensive care, and death).
Serological Testing
The serological data were collected from participants’ blood tests 1 month after the last vaccination. All the participants were checked for a negative history of COVID-19 before the vaccination. The serological antibodies containing immunoglobulin G (IgG) and immunoglobulin M (IgM) to COVID-19, liver and kidney function, routine blood examination, and immunosuppressor concentration were assessed at approximately 1 month after the secondary inoculation as a completion, with a mean interval of 35 days.
Statistical Analysis
Data were expressed as the means and standard deviations (SD) or median with interquartile range (IQR) in the case of continuous variables. Continuous variables were tested for normal distribution using the Kolmogorov–Smirnov test and then compared by Student’s t-test and the Mann–Whitney U-test if they were abnormally distributed. In the case of categorical variables, data are presented as frequencies and proportions, which were compared using the χ2 test or Fisher’s exact test as appropriate. A P<0.05 was considered statistically significant for all analyses. All statistics were analysed using IBM SPSS Statistics for Windows, version 22 (IBM Corp., Armonk, NY, USA).
Results
Participants’ Characteristics
In our study, 35 LTx recipients completed the vaccination and were included in the analysis. The mean age was 46 years, and 30 patients (85.71%) were male. The mean time from LTx to the first inoculation was 3.8 years. Among the 35 patients, calcineurin inhibitors (CNIs) (28 cases of tacrolimus and 1 case of cyclosporine) were used as the dominating immunosuppressor in 29 patients (82.9%), and sirolimus was used in 6 patients (17.1%). Derivative from mycophenolate acid (MPA) was given in 15 (44.8%) recipients, of them, in combination with CNIs in 13 participants and with sirolimus in 2 participants (33.3%). The remaining 10 recipients were treated with a single immunosuppressor.
The mean eGFR was 94 (75–105) mL/min. All patients had stable liver or kidney function before vaccination.
Vaccination Seroconversion
All the participants were detected for COVID-19 IgG antibodies 1 month after vaccination, and only 6 (17.14%) LTx recipients were seropositive for IgG antibodies against COVID-19.
All the participants’ data are presented in Table 1. Compared LTx recipients with negative seroconversion with those with positive seroconversion, there was a significantly higher proportion of recipients having interleukin-2 receptor (IL-2R) induction peri-operation (96.5% vs 50%, p=0.011), shorter posttransplant time (2.3 years vs 6.3 years, p=0.025), and a higher proportion of recipients receiving MPA during the vaccination (52.7% vs 0%, p=0.027).
Comparison of age did not yield statistically significant differences in seroconversion, sex or body mass index.
Vaccination Side Effects
Good tolerance was presented, and no severe adverse events were recorded in any of the vaccinated participants, as shown in Table 2. Systemic side effects were presented in 4 LTx recipients (2 cases of dizziness combined with poor appetite, 1 case of fatigue, and 1 case of chest distress) without any local side effects. During the follow-up period (1 month after the vaccination), no severe side effects (rejection, fatal hypersensitivity, cardiac or neurological events) occurred in the participants who needed extra drugs or hospitalization.
Table 2.
The Side Effects and Blood Tests After Vaccination
| Characteristics | Entire (n=35) | Seronegative (n=29) | Seropositive (n=6) | P value | Missing |
|---|---|---|---|---|---|
| Side effects | 4 | 2 | 2 | 0 | |
| Dizziness with poor appetite | 2 | 1 | 1 | ||
| Fatigue | 1 | 0 | 1 | ||
| Chest distress | 1 | 1 | 0 | ||
| Total bilirubin | 14.0 (8.9–19.5) | 14.0 (9.8–19.0) | 15.2 (6.4–25.6) | 0.933 | 3 |
| Serum creatinine | 82 (66–94) | 83 (67–100) | 75 (63–87) | 0.334 | 3 |
| eGFR | 94 (75–105) | 94 (72–105) | 90 (85–118) | 0.438 | 4 |
| WBC | 5.1 (4.1–6.0) | 5.1 (4.2–5.8) | 5.3 (2.8–6.6) | 0.638 | 3 |
Abbreviations: eGFR, estimated glomerular filtration rate; WBC, white blood cell.
Discussion
It has been reported that solid organ transplant (SOT) recipients are at high risk of mortality from COVID-19, ranging from 13% to 39%.8–10 Consequently, the health authorities of numerous countries have prioritized this vulnerable population for vaccination with mRNA vaccines.
However, little is known about the response and safety of inactivated vaccines in LTx recipients under immunosuppression who were excluded from Phase 3 trials for the vaccine. Our study was the first to investigate the response and safety of inactivated vaccines in LTx recipients. Our study indicated that the immune response to the inactivated vaccine for COVID-19 among LTx recipients was generally low, which was consistent with previous reports showing inferior vaccination seroconversion in SOT recipients in general.5,6,11 However, no graft rejection or other major adverse events to the inactivated vaccine were recorded in this study.
A previous study on mRNA vaccines for COVID-19 showed that the time from transplant, induction treatment, MPA and serum creatinine showed statistical significance to the response of kidney transplant recipients.6 Age, renal function and immunosuppressive medications showed statistical significance to the response of the liver transplant recipients.5 In our research, time from transplant, induction treatment and MPA application also played obvious roles in the response to the inactivated vaccine, except serum creatinine or age. This discrepancy is supposed to be due to the difference in vaccine platforms or the lack of participants in our research.
In addition, the limitations of this study include the leakage of follow-up time points and the unavailability of the method to quantitate the antibody against the spike protein of COVID-19.
The COVID-19 pandemic continues to put immunosuppressed patients at high risk of severe disease and death. Currently, the booster vaccination is advocated by the government of mainland China. Real-world studies on the infection rate, morbidity and mortality of COVID-19 following vaccination in immunocompromised individuals are warranted in the future.
Conclusion
LTx recipients have a substantially partial immunological response to the inactivated vaccine for COVID-19. IL-2R induction during LTx, a shorter time post LTx and the application of a derivative from MPA seem to be predictors for a negative serological IgG antibody response in recipients. The findings require booster vaccination in these LTx recipients.
Acknowledgments
This work was supported by the program of the Provincial Key Research and Development Program of Zhejiang (2019C03019) and the Zhejiang Provincial Traditional Chinese Medicine Key Discipline Project (2017-XK-A38). The funders did not play any role in the study design, data collection and analysis, decisions regarding data release or manuscript preparation. The authors acknowledge Shui-Ying Lei and Rong-Rong Wang for the contributions to professional proofreading.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Emmie de W, Neeltje van D, Darryl F, et al. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14(8):523–534. doi: 10.1038/nrmicro.2016.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim KH, Tandi TE, Choi JW, et al. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in South Korea, 2015: epidemiology, characteristics and public health implications. J Hosp Infect. 2017;95(2):207–213. doi: 10.1016/j.jhin.2016.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Coronavirus disease (COVID-19) pandemic; 2022. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed May 10, 2022.
- 4.Zhang XY, Guo J, Wan X, et al. Biochemical and antigenic characterization of the structural proteins and their posttranslational modifications in purified SARS-CoV-virions of an inactivated vaccine candidate. Emerg Microbes Infect. 2020;9(1):2653–2662. doi: 10.1080/22221751.2020.1855945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rabinowich L, Grupper A, Baruch R, et al. Low immunogenicity to SARS-CoV-2 vaccination among liver transplant recipients. J Hepatol. 2021;75(2):435–438. doi: 10.1016/j.jhep.2021.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benotmane I, Gautier-Vargas G, Cognard N, et al. Weak anti-SARS-CoV-2 antibody response after the first injection of an mRNA COVID-19 vaccine in kidney transplant recipients. Kidney Int. 2021;99(6):1487–1489. doi: 10.1016/j.kint.2021.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang YJ, Zeng G, Pan HX, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18–59 years: a randomized, double-blind, placebo-controlled, Phase 1/2 clinical trial. Lancet Infect Dis. 2021;21(2):181–192. doi: 10.1016/S1473-3099(20)30843-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azzi Y, Bartash R, Scalea J, et al. COVID-19 and solid organ transplantation: a review article. Transplantation. 2021;105(1):37–55. doi: 10.1097/TP.0000000000003523 [DOI] [PubMed] [Google Scholar]
- 9.Azzi Y, Parides M, Alani O, et al. COVID-19 infection in kidney transplant recipients at the epicenter of pandemics. Kidney Int. 2020;98(6):1559–1567. doi: 10.1016/j.kint.2020.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dumortier J, Duvoux C, Roux O, et al. COVID-19 in liver transplant recipients: the French SOT COVID registry. Clin Res Hepatol Gastroenterol. 2021;45(4):101639. doi: 10.1016/j.clinre.2021.101639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grupper A, Rabinowich L, Schwartz D, et al. Reduced humoral response to mRNA SARS-CoV-2 BNT162b2 vaccine in kidney transplant recipients without prior exposure to the virus. Am J Transplant. 2021;21(8):2719–2726. doi: 10.1111/ajt.16615 [DOI] [PMC free article] [PubMed] [Google Scholar]