Abstract
Schwannomas are benign nerve sheath tumors that are generally encapsulated and commonly detected in the head, neck, and mediastinal regions. Schwannomas localizing in the pelvis are extremely rare and tend to be asymptomatic initially due to slow growth rate. Schwannomas may be misdiagnosed as urologic or gynecologic tumors. Pelvic schwannomas are typically solitary, large, and well-circumscribed masses in the retroperitoneum or presacral areas. Other imaging characteristics are cystic degeneration, repeated hemorrhages, and calcifications. Calcification patterns can be punctate, speckled, curvilinear, or along the walls of the masses. We report a young man with a pelvic schwannoma with typical imaging features.
Keywords: Computed tomography, neurilemmoma, pelvic tumor, peripheral nerve sheath tumor, schwannoma
Introduction
Schwannomas (also known as neurilemmomas) are benign tumors that arise from well-differentiated Schwann cells (glial cells) of peripheral nerve sheaths. These tumors originate in cranial, peripheral, or visceral nerves at all anatomical locations. 1 Head, neck, mediastinum, retroperitoneal, and extremities are the most common places for schwannomas to grow. In contrast, they rarely occur in the pelvis with a reported incidence of 1–3% and typically associated with neurofibromatosis type 1 (von Recklinghousen disease), less than 0.5%.2,3 Patients usually present in the 2nd and 5th decades without significant sex predilection. Schwannomas are nonaggressive, slow-growing, solitary masses with a low rate of malignant transformation and a low risk of recurrence after resection.3,4 We present a rare case of a left pelvic schwannoma identified on ultrasound, CT, and MRI; and the final diagnosis was confirmed by surgery and histopathology.
Case report
A 37-year-old male was admitted to the hospital because of a mass in the pelvic space detected by abdominal ultrasound. He reported lower left abdominal pain, a palpable mass in the left iliac fossa, and edema in his leg within about the last one month. He had no past or family medical history. There are no symptoms of nervous system disorders. Laboratory tests including complete blood count, complete metabolic profile, and tumor marker CEA were within normal limits. Ultrasound images showed a mixed mass with multiple septa inside the cystic component in the left hemipelvis (Figure 1). CT images showed a well-defined, heterogeneously enhancing mass with cystic areas, hemorrhage, and small foci of calcifications in the left lateral pelvic space measuring 6 x 7 x 10 cm (Figure 2). MRI revealed a mass with heterogeneous low signal intensity on T1-weighted image and high signal intensity on T2-weighted image. There were high signal intensity areas indicating hemorrhage on the T1-weighted image and focal high signal intensity areas indicating cystic components on the T2-weighted image. Contrast-enhanced images showed heterogeneous enhancement of the internal septa and solid components (Figure 3).
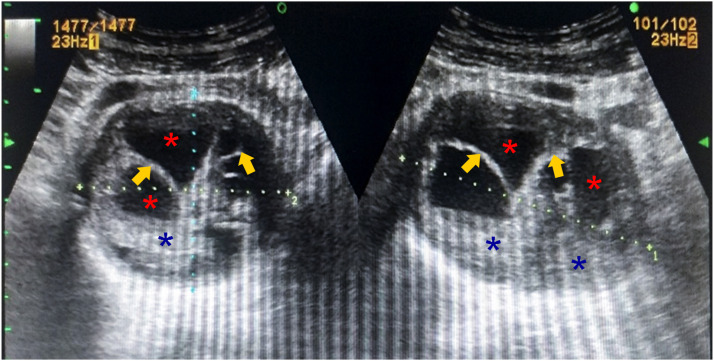
Figure 1.
Ultrasound images show a complex cystic lesion with internal septa (arrows), cystic (red asterisks), and solid (blue asterisks) components in the left hemipelvis.
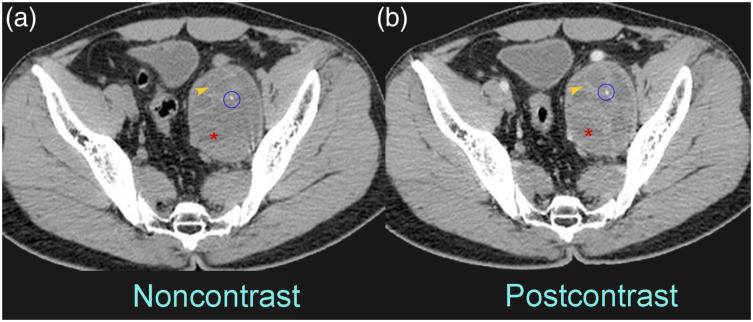
Figure 2.
CT images before (a) and after (b) contrast administration show a well-defined, heterogeneously enhancing mass with cystic areas (asterisks), hemorrhage (arrowheads), and small foci of calcification (circles) in the left lateral pelvis space.
Figure 3.
MRI on T2-weighted image (a) and T1-weighted image (b) shows a well-defined, complex cystic lesion with hemorrhage (arrowheads), internal septa (arrows), and solid components (blue asterisks) in the left hemipelvis, and fat-saturated T1-weighted postcontrast (c) reveals heterogeneous enhancement of the internal septa and solid components.
We suspected that it was a neurogenic tumor with cystic degeneration, mainly suspecting schwannoma. However, it was difficult to determine the origin of the tumor. An exploratory laparotomy was performed utilizing a lower midline abdominal incision. There was a hard solid mass which displaced the left external iliac vessels anterior and caused a mass effect on the left iliopsoas muscle. It was carefully freed by a combination of blunt and sharp dissection, allowing the mass to be completely removed from the pelvis. The ureteral continuity was identified by palpation at the end of the procedure. The mass was sent to pathology for routine staining and sectioning (Figure 4). The pathology report showed a spindle-cell lesion most consistent with Schwannoma. Histological staining was strongly positive for S100 and vimentin, but negative for CD117, CD34, ACTIN, and EMA.
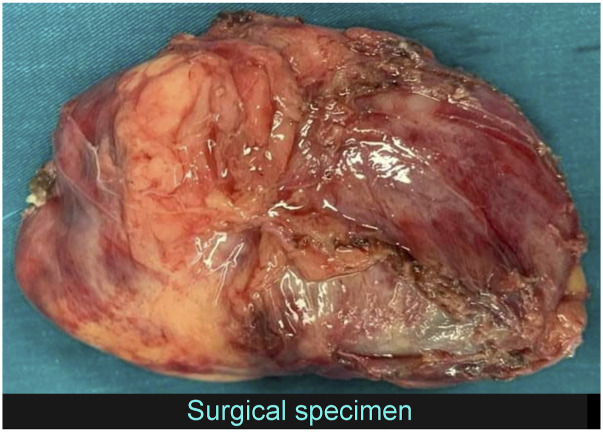
Figure 4.
Photograph of the gross specimen.
Discussion
Pelvic schwannomas originate from peripheral nerve sheath of sacral nerve or hypogastric plexus; nonetheless, only a small amount of them is reported. Almost all cases are benign, and transformation to malignant peripheral nerve sheath tumors is extremely rare. Tumors involving the peripheral nerves are usually asymptomatic, while tumors involving spinal nerve roots commonly present with radicular pain and nerve compression syndromes.1,3 Histologically, they appear as encapsulated masses with a soft tan-white appearance with or without focal areas of cystic degenerative changes of Antoni A (hypercellular) areas and Antoni B (hypocellular) areas, respectively. In immunohistochemistry, the presence of S100 protein is a classic marker for diagnostic confirmation.2–4
The radiological examinations are essential to define the morphological tumor features such as well-circumscribed margin, cystic or connective tissue tumor. CT, or MRI, or PET plays an important role for better characterization of the mass and its relationship with the neighboring structures, as well as any evidence of distant metastatic or adjacent organ invasion. MRI is a modality of choice for preoperative imaging that classically reveals a well-circumscribed T1 iso-/hypointense and T2 hyperintense nodular intradural mass most often arising from peripheral nerve sheath of sacral nerve or hypogastric plexus; post-contrast images show intense enhancement mass. As cystic degeneration tends to occur with larger schwannomas, heterogeneous signal intensity and ringlike enhancement are common in these cases. 5 Typical imaging features include well-circumscribed masses without direct invasion, often containing cystic areas owing to degeneration and sometimes hemorrhage; calcifications are uncommon but have been reported. Intense homogeneous enhancement could be seen in small lesions, while larger lesions enhance heterogeneously.3,6 In our case report, a large schwannoma in the left lateral pelvis revealed a well-defined, heterogeneously enhancing mass with cystic areas, hemorrhage, and small foci of calcification on both CT and MRI imaging. However, radiologists can sometimes confuse pelvic schwannoma with other pelvic lesions (such as abscess, adnexal mass, fibrosarcoma, ganglioneuroma, hydatid cyst, liposarcoma, and hematoma); therefore, biopsy is recommended for definitive diagnosis in some atypical cases.5–7
Macroscopically, schwannomas are solitary, well-circumscribed, encapsulated tumors. Histologically, schwannomas are characterized by the presence of Antoni A and Antoni B bodies. Antoni A bodies represent a disposition in the Verocay body, and Antoni B tissue is a loose hypocellular myxoid region of microcysts. Immunohistochemistry is positive for S-100, vimentin, and neuron-specific enolase but negative for SMA and CD117.3,4,7
Furthermore, pathologists can report the type of schwannoma based on histological findings after tumor resection. Based on that, clinicians can accurately determine whether the tumor is benign or malignant. If a malignant tumor is resistant to chemotherapy, there is a higher rate of recurrence.3,6,8
Few previous case reports have marked the clinical significance and timely management of schwannomas. Haleh Pak et al. 1 reported a large retroperitoneal schwannoma displacing of the colon and attaching to the presacral region of the spine; successful resection of schwannoma was achieved following the diagnosis. In a recent report, Xu Hao et al. 9 reported a successful removal of 16-cm retroperitoneal schwannoma in an elderly patient; however, the evidence of excessive bleeding was seen in this case. Similarly, in a recent report by Wang Yun et al., 10 a pediatric case of a painless schwannoma near the right lumbar region was presented; however, after successful removal of the tumor, one month later, recurrence was seen. A schwannoma can often be removed without associated deficits, and the nerve axons are not disrupted in the course of the procedure.8–10
In conclusion, schwannomas are rarely located in the pelvis or retroperitoneum. It can be challenging to make an accurate preoperative diagnosis. Ultrasound, computed tomography, and magnetic resonance imaging can be utilized to make a diagnosis preoperatively. Surgery is the initial treatment for retroperitoneal schwannoma. The disease usually has a good prognosis and can be completely cured without sequelae after surgery.
Footnotes
Author Contributions: The authors contributed equally.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: This report was prepared in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki Declaration. Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Written informed consent was obstained from the patient for publication of this case report.
ORCID iD
Van Trung Hoang https://orcid.org/0000-0001-7857-4387
References
- 1.Pak H, Haji Maghsoudi L. Pelvic Schwannoma: in light of a case report. Clin Case Rep 2019; 7: 2488–2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakashima T, Tsurumaru D, Nishimuta Y, et al. A case of pelvic schwannoma presenting prominent eggshell-like calcification. Case Rep Radiol 2013; 2013: 825078–825084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Machairiotis N, Zarogoulidis P, Stylianaki A, et al. Pelvic schwannoma in the right parametrium. Int J Gen Med 2013; 6: 123–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jindal T, Mukherjee S, Kamal MR, et al. Cystic schwannoma of the pelvis. Ann R Coll Surg Engl 2013; 95: e1–e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hughes MJ, Thomas JM, Fisher C, et al. Imaging features of retroperitoneal and pelvic schwannomas. Clin Radiol 2005; 60: 886–893. [DOI] [PubMed] [Google Scholar]
- 6.Padmanaban N, Chandrabose PS, Esakki M, et al. Gynaecological perspective of schwannoma: a rare pelvic tumour. J Clin Diagn Res 2016; 10: QD03–QD05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deboudt C, Labat JJ, Riant T, et al. Pelvic schwannoma: robotic laparoscopic resection. Neurosurgery 2013; 72: 2–5. [DOI] [PubMed] [Google Scholar]
- 8.Maneschg C, Rogatsch H, Bartsch G, et al. Treatment of giant ancient pelvic schwannoma. Tech Urol 2001; 7: 296–298. [PubMed] [Google Scholar]
- 9.Xu H, Sha N, Li HW, et al. A giant pelvic malignant schwannoma: a case report and literature review. Int J Clin Exp Pathol 2015; 8: 15363–15368. [PMC free article] [PubMed] [Google Scholar]
- 10.Wang J, Yu M, Zhu H, et al. Retroperitoneal malignant schwannoma in a child. J Int Med Res 2018; 46: 4315–4322. [DOI] [PMC free article] [PubMed] [Google Scholar]