Abstract
Dental dams are a barrier method of protection, which may help prevent the spread of sexually transmitted infections during oral-vaginal or oral-anal sex. Despite their relative simplicity of use, data on dental dams are limited and patients infrequently utilize this method of barrier protection because of the lack of awareness, perceived barriers to procurement and accessibility, and unfamiliarity on the part of health educators. Nevertheless, increased knowledge of dental dams may be beneficial especially in high-risk populations, where sexually transmitted infections are more common and remain a significant cause for morbidity. This article aims to increase awareness and knowledge of dental dams, as well as provide an informational guide on their procurement and use that may be helpful to dermatologists when counseling patients.
Keywords: Dental dam, sexually transmitted infection, dermatology
What is known about this subject in regard to women and their families?
Many adolescent and adult patients perceive oral sex as a risk-free act, although it is known that several sexually transmitted infections can be transmitted from nonpenetrative activities.
The majority of adolescents do not use barrier protection during oral sex due to feeling uneducated about both the risks and the types of protection available for use.
There is a lack of awareness about using dental dams as a tool for sexually transmitted infection prevention during oral sex.
The majority of dental dam literature focuses on women who have sex with women; however, the data are quite limited.
What is new from this article as messages for women and their families?
Dental dams can be an invaluable tool for safe oral sex, and it is important for patients to know how to use them properly.
From the authors’ experience, dental dams are infrequently used by their patient population, which could be attributed to the lack of knowledge by the provider.
Dental dams can often be conflated with other forms of barrier protection, such as female condoms, and it is essential to know the differences for the most effective use.
Dental dams can be fashioned out of more common household items, such as gloves or even plastic wrap.
Barrier methods of protection are an invaluable tool to provide physical separation between partners during sexual activities. They are used to reduce the risk of sexually transmitted infections (STIs), prevent pregnancy, and decrease the transmission of other diseases that can be contracted through sexual behaviors—such as the Zika virus.1 The most commonly utilized, publicized, and studied are male condoms. Lesser-known forms of barrier protection include female condoms, gloves, finger cots, and dental dams. In conjunction with the popularity and known effectiveness surrounding the male condom, barrier protection is often discussed in regards to penetrative sexual intercourse involving a male partner. There are less educational efforts surrounding barrier protection and oral sex—including oral-anal and oral-genital sexual behaviors.2 This article discusses the importance of barrier protection during oral sex, specifically highlighting the lesser-known dental dams.
Although the risk of STI transmission is lower during oral sexual behaviors than penetrative intercourse, it certainly still exists.2 Many STIs can be transmitted from nonpenetrative activities including gonorrhea, chlamydia, syphilis, human papillomavirus, herpes simplex virus, and rarely HIV.3 Yet, many adolescents and adults believe oral sex to be a “risk-free” behavior and, therefore, do not utilize protection.4,5 A recent study showed that the majority of youth do not use barrier protection during oral sex because they feel uneducated on the risks and are unaware of which protection methods to use.5
An underutilized method of barrier protection for oral-vaginal and oral-anal sex is the dental dam. Initially developed for oral surgery, the dental dam is a thin square sheet of latex or nitrile that can be used to prevent the transmission of STIs during oral sex. Literature on dental dam use focuses primarily on women who have sex with women. However, the data are quite limited; studies have reported only 10% to 15% of women engaging in oral-vaginal sex have ever used a dental dam,6–8 with even lower numbers among women who have sex exclusively with women.9 Data on dental dam use in men who have sex with men are even scarcer. One study reported dental dams as the least utilized barrier method in this population, with respondents using them more for hygienic purposes rather than for STI prevention.10 Although dental dams have been associated with a reduction in STIs, the lack of statistical significance may thus be explained in part by small sample sizes.11
Dental dams are not a widely utilized method of protection because many roadblocks prevent regular use.7 Primarily, there is a lack of awareness of dental dams and even the small number of individuals that are familiar with them, often do not know that they can be utilized for STI prevention.12 There has been conflation of female condoms with dental dams and the perception that they are not as readily available to purchase as male condoms.3 Additionally, some report decreased pleasure and sensation with a dental dam in place4 and a dislike of the taste.8
The Ronald O. Perelman Department of Dermatology at New York University School of Medicine operates a STI clinic as part of the dermatology services offered at Bellevue Hospital Center. By rotating at this clinic, dermatology residents are able to gain insight into the diverse mucocutaneous manifestations of STIs and learn how to manage conditions, such as anogenital warts, gonorrhea, chlamydia, herpes simplex virus, and syphilis. In line with findings from the aforementioned studies, dental dams are infrequently used by our STI clinic population. One potentially overlooked barrier may be the lack of knowledge on the part of the provider. This article aims to both increase awareness and knowledge of dental dams, and also to provide an informational guide on their procurement and use that may be helpful when counseling patients.
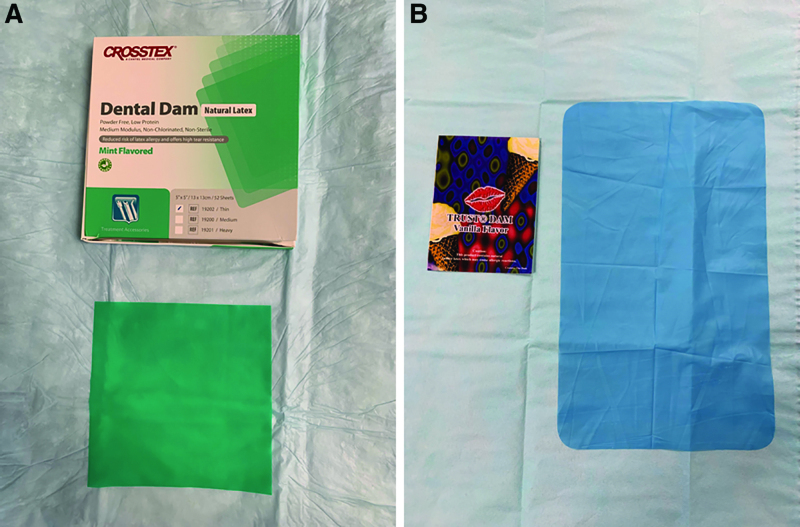
From experience with patients in the STI clinic, the authors advise purchasing dental dams made specifically for oral sex because these are thinner than even the thinnest dental dams available for oral surgery. Dental dams made for oral sex are sold in individually wrapped packages and can be purchased online or in sexual health stores. Pertinently, dental dams sold for oral surgery are sold in larger quantities and will not be individually wrapped (Fig. 1). If a dental dam is able to be purchased, the protective sheet should be placed on the sexual partner’s anus or vulva without stretching the material, to avoid creating tears. The dental dam should be large enough to cover the entire area to prevent oral contact with bodily fluids. Water- or silicone-based lubricant may be utilized, and the lubricated side should face the vulva or anus to aid in adhesion and improvement of sensation.4 Oil-based lubricants, in contrast, may damage the dental dam and are not recommended. Tears in the material necessitate replacement before resuming oral activities. If there are interruptions during sexual activities, a new dental dam is recommended to avoid incorrect replacement on the mucocutaneous surfaces, which may expose an individual to bodily fluids. After one usage, the dental dam should be disposed of to prevent reuse with other partners.1 It is critical to educate about the differences between dental dams and female condoms because using a dental dam rather than a female condom for intercourse is not a sufficient seal to protect from STIs.3 Female condoms consist of 2 rings—an outer ring that stays outside of the body against the vulva and an inner ring, which is inserted inside of the vagina and is placed against the cervix.1 Female condoms serve as a barrier during penetrative intercourse. Dental dams, on the other hand, are completely outside of the body and sit against the vulva. They are a flat sheet of latex or polyurethane and are used as barrier protection for oral sex.
Fig. 1.
(A) Dental dams designed for use in dental practice. (B) Dental dams designed for use in sexual practice.
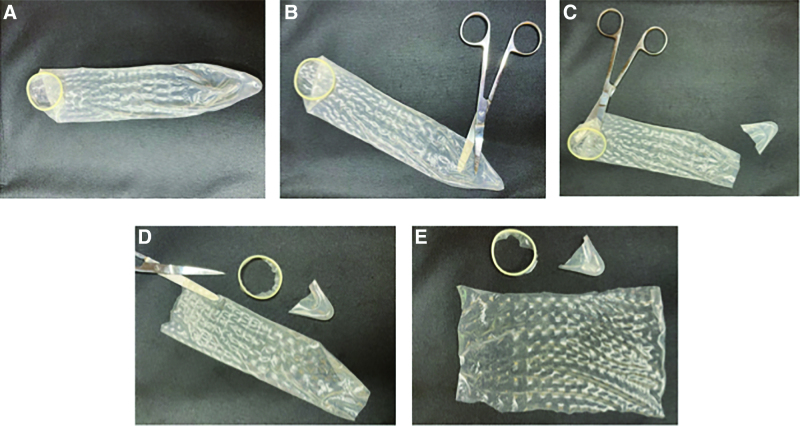
The perceived inaccessibility of dental dams presents a major barrier to use. To help rectify this widespread sentiment, providers and patients should be made aware that dental dams can be fashioned from other barrier methods, especially the more ubiquitous male condom. Removal of the tip and rolled end of the male condom with scissors followed by a perpendicular cut can create a homemade dental dam ready for use during oral sex (Fig. 2). It is important to ensure that the condom is made from latex or polyurethane for optimum protection.1 Additionally, similar results can be obtained by taking a latex or nitrile glove and opening it to increase the surface area. Although lesser advised, a further reported option is to use plastic wrap.4 This is a widely accessible item, yet there are many drawbacks including a significant chance of tearing and slipping.
Fig. 2.
Creating a dental dam from a male condom.
At this time, it is unclear if dental dams play a statistically significant role in decreasing incidence and transmission of STIs based on the current literature11; this may be accounted for by factors, such as a paucity of data, infrequent use due to sparse patient education, perceived barriers to procurement and accessibility, and unfamiliarity on the part of providers. Condoms have repeatedly been shown to decrease STI risk; it is likely that dental dams will decrease risk as well when extrapolating the aforementioned data on condoms. Yet, there is a clear need for more provisional research on dental dams to ascertain their usage, perceived barriers, and efficacy in STI prevention.
Nevertheless, we feel that this method of barrier protection has a role in certain high-risk populations, where STIs are more common and remain a significant cause for morbidity—including prisoners, sex workers, and individuals who frequently engage in oral-anal or oral-vaginal sex with many new partners of unknown sexual history—as well as in low-risk populations, where oral transmission of STIs such as herpes simplex virus can still occur.
Conflicts of interest
None.
Funding
None.
Study approval
This article is exempt from Institutional Review Board approval.
Author contributions
D.G. conceived ideas of the study, drafted the article, and provided revisions to article content. A.T. provided revisions to article content. AS. drafted the article and provided revisions to article content. M.K.P. conceived ideas of the study, provided revisions to article content, and principal investigator.
References
- 1.Centers for Disease Control and Prevention. Condom effectiveness. 2021. [cited September 10, 2021]. Available from: https://www.cdc.gov/condomeffectiveness/index.html.
- 2.Halpern-Felsher BL, Cornell JL, Kropp RY, Tschann JM. Adolescents and oral sex: perceptions, attitudes, and behavior. J Adolesc Health 2005;36:109–110. [Google Scholar]
- 3.Muzny CA, Harbison HS, Pembleton ES, Hook EW, Austin EL. Misperceptions regarding protective barrier method use for safer sex among African-American women who have sex with women. Sex Health 2013;10:138–141. [DOI] [PubMed] [Google Scholar]
- 4.Saini R, Saini S, Sharma S. Oral sex, oral health and orogenital infections. J Glob Infect Dis 2010;2:57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strome A, Moore-Petinak N, Waselewski M, Chang T. Youths’ knowledge and perceptions of health risks associated with unprotected oral sex. Ann Fam Med 2022;20:72–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bailey JV, Farquhar C, Owen C, Whittaker D. Sexual behaviour of lesbians and bisexual women. Sex Transm Infect 2003;79:147–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richters J, Prestage G, Schneider K, Clayton S. Do women use dental dams? Safer sex practices of lesbians and other women who have sex with women. Sex Health 2010;7:165–169. [DOI] [PubMed] [Google Scholar]
- 8.Yap L, Richters J, Butler T, Schneider K, Kirkwood K, Donovan B. Sexual practices and dental dam use among women prisoners–a mixed methods study. Sex Health 2010;7:170–176. [DOI] [PubMed] [Google Scholar]
- 9.Rufino AC, Madeiro A, Trinidad A, Santos R, Freitas I. Sexual practices and health care of women who have sex with women: 2013-2014. Epidemiol Serv Saude 2018;27:e2017499. [DOI] [PubMed] [Google Scholar]
- 10.Hunt AJ, Weatherburn P, Hickson FC, Davies PM, McManus TJ, Coxon AP. Changes in condom use by gay men. AIDS Care 1993;5:439–448. [DOI] [PubMed] [Google Scholar]
- 11.Bailey JV, Farquhar C, Owen C, Mangtani P. Sexually transmitted infections in women who have sex with women. Sex Transm Infect 2004;80:244–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Downing-Matibag TM, Geisinger B. Hooking up and sexual risk taking among college students: a health belief model perspective. Qual Health Res 2009;19:1196–1209. [DOI] [PubMed] [Google Scholar]