Abstract
Vasectomy is used less often than female sterilization, and many men who do not want more children may lack accurate information about vasectomy. Between May and June 2018, we used a nationally representative online panel to survey U.S. men between 25 and 55 years of age who did not want more children about their vasectomy knowledge. We also asked about interest in undergoing the procedure if it were free or low cost and explored whether a paragraph addressing common misperceptions was associated with interest. We assessed characteristics associated with high vasectomy knowledge (≥3 accurate responses to four questions about vasectomy’s effect on sexual functioning and method efficacy) and vasectomy interest, using chi-square tests and multivariable-adjusted Poisson regression. Of 620 men surveyed, 564 had complete data on the outcomes and covariates of interest. Overall, 51% of respondents demonstrated high vasectomy knowledge. Men who knew someone who had a vasectomy were more likely to have high knowledge (prevalence ratio [PR]: 1.50; 95% CI [1.22, 1.85]). One-third of the sample (35%) said they would consider getting a vasectomy. Men with high (vs. moderate/low) knowledge were more likely (PR: 1.36; 95% CI [1.04, 1.77]) to consider getting a vasectomy. Race/ethnicity, income level, and receiving the informational paragraph were not associated with vasectomy interest. Greater vasectomy knowledge affects men’s interest in the procedure. Given that many U.S. men lack accurate knowledge, efforts are needed to address misinformation and increase awareness about vasectomy to ensure men have the information they need to meet or contribute to reproductive goals.
Keywords: vasectomy, contraception, contraceptive knowledge, United States
Introduction
Vasectomy is a highly effective contraceptive method for people who do not want any or any more children, and, for heterosexual couples who want a permanent method, it poses fewer surgical risks and has a lower failure rate than laparoscopic tubal ligation (Bartz & Greenberg, 2008; Hendrix et al., 1999; Trussell, 2011). In the United States, only 9% of men aged 20 to 49 report vasectomy as their contraceptive method, compared with 21% of women who rely on female sterilization (Daniels & Abma, 2020; National Center for Health Statistics, 2019). Although U.S. men’s reliance on vasectomy increases with age (Zhang & Eisenberg, 2022), the prevalence of vasectomy use is considerably lower than the percentage of men reporting that they do not want more children. In a cross-sectional national study, nearly half (43%) of men between ages 25 and 34 reported that they do not want more children, and the percentage increased to 80% among those in their mid-30s and early 40s (Mitchell et al., 2012). In addition, people of color and those living on low incomes rely on vasectomy less often than female sterilization, indicating that there may be structural barriers to vasectomy use among these groups (Anderson et al., 2012; Daniels & Abma, 2020; Lindberg & Kost, 2014; Martinez et al., 2006; Zhang & Eisenberg, 2022).
There is some evidence that men may be more interested in vasectomy than the current prevalence indicates. A 2005 study of 1,500 U.S. men aged 18 to 50—the majority of whom were married and had children—reported that 35% would consider vasectomy under some circumstances and an additional 12% were currently considering getting one (Heinemann et al., 2005). The study did not assess the characteristics of men most interested in undergoing the procedure and whether these characteristics mirror known demographic differences in vasectomy use (Anderson et al., 2012; Sharma et al., 2013; Zhang & Eisenberg, 2022). In qualitative studies, men who do not want more children often report that they want to take greater responsibility for contraception but lack accurate information about vasectomy and have concerns about the procedure’s effect on sexual functioning (Campbell et al., 2019; Shih et al., 2012, 2013). Identifying and addressing men’s knowledge gaps could support their contraceptive involvement when they have decided they do not want any or any more children.
The purpose of this study was to assess knowledge and interest in vasectomy among U.S. men who do not want any or any more children. Using a nationally representative online panel, we examined men’s knowledge of vasectomy’s effect on sexual functioning and method efficacy and characteristics associated with interest in the procedure. We also assessed whether providing men with medically accurate information about vasectomy was associated with greater interest in having the procedure.
Methods
Data
We used GfK’s (now Ipsos) KnowledgePanel to conduct an online survey of U.S. men regarding their knowledge and attitudes about contraception, including vasectomy. KnowledgePanel is a nationally representative online panel of U.S. households that recruits participants from a probability-based sample of addresses using the U.S. Postal Service’s Delivery Sequence File (GfK, 2018). Randomly selected addresses are sent a series of mailings (in English and Spanish) inviting them to join KnowledgePanel, and follow-up calls are made to non-responders when the address can be matched with a telephone number. To supplement recruitment of Latino households into the sample, GfK uses a random-digit-dialing approach that focuses on telephone exchanges in census blocks where the Latino population density is ≥65% and cell phone numbers in geographic areas with a high concentration of Latinos. Households are selected into the sample if Spanish is spoken in the home at least half of the time. If selected households do not have an internet connection, they are provided a web-enabled device (e.g., tablet) and free internet access.
For this study, male panel members between ages 25 and 55 received up to four emails inviting them to complete a 15-min survey about their knowledge and attitudes about contraception. Men then responded to a series of questions to determine their eligibility. Men were eligible if they did not intend to have (more) children, did not have a vasectomy, had sexual intercourse in the last 3 months with a female partner aged 18 to 49 years, and were able to complete the survey in English or Spanish. We sampled men between 25 and 55 years old because of the large percentage of men in this age range reporting that they do not want more children and to facilitate comparison with prior studies of adult men’s contraceptive attitudes (Campbell et al., 2019; Mitchell et al., 2012; Shih et al., 2012, 2013).
We planned to enroll 600 men, half of whom would be presented with a short paragraph that provided medically accurate information about vasectomy (Box) after assessing their baseline knowledge. This sample size would provide 80% statistical power to determine whether there was a 10-percentage-point difference in knowledge (or larger) between those randomized to receive (information group) or not receive (comparison group) the informational paragraph during the survey. Based on estimates from the male sample of the National Survey of Family Growth, we anticipated that 37% of men between ages 25 and 55 would meet the eligibility criteria. We expected a cooperation rate of 57% among eligible men, which is typical of other KnowledgePanel surveys on reproductive health (Grossman et al., 2013; K. White et al., 2016).
Box.
Statements presented to the information group before they answered questions about their interest in getting a vasectomy.
| Vasectomy is done by cutting and blocking the tubes that carry sperm so the sperm cannot get into the semen. A doctor uses medication to numb the scrotum, and the procedure takes about 20 minutes. Men go home the same day and can return to their normal activities in 2 or 3 days. Men still have orgasms, and vasectomy doesn’t affect their desire or ability to have sex. Because vasectomy reversal surgery is very expensive and not always successful, vasectomy is considered permanent birth control. It is the most effective method of birth control. |
Prior to launching the survey, the authors’ research team conducted cognitive interviews with 15 English-speaking men and 10 Spanish-speaking men to ensure men understood the survey items and the informational paragraph describing how vasectomy is performed, its effects on sexual functioning, and method effectiveness. The study authors revised the survey and paragraph based on these interviews.
Between May and June 2018, GfK pretested the survey with 25 English- and Spanish-speaking participants and then fielded the online survey with the larger sample. Men provided informed consent before completing the survey and received reward points redeemable for cash or other prizes (GfK’s standard incentive) for their participation. GfK provided the authors with information on men’s demographic characteristics, including age, race/ethnicity, household income, and family size from the initial profile survey that participants complete upon joining KnowledgePanel. Race/ethnicity was reported as non-Hispanic white, non-Hispanic black, non-Hispanic other race, non-Hispanic more than one race, and Hispanic. The study was approved by the University of Alabama at Birmingham Institutional Review Board (IRB-140721006).
Measures
The 53-item survey collected information on whether men had ever contributed to a pregnancy, number of biological children, reasons for not wanting more children, relationship with their current partner, and current contraceptive use. We also asked men how important it was for them to prevent future pregnancies (very important, somewhat important, a little important, not at all important) and their level of agreement (strongly agree, somewhat agree, neither agree nor disagree, somewhat disagree, strongly disagree) that it is mainly a woman’s responsibility to use birth control to keep from getting pregnant. We based these items on questions used in the National Survey of Family Growth and the National Survey of Reproductive and Contraceptive Knowledge (Kaye et al., 2009; National Center for Health Statistics, 2015).
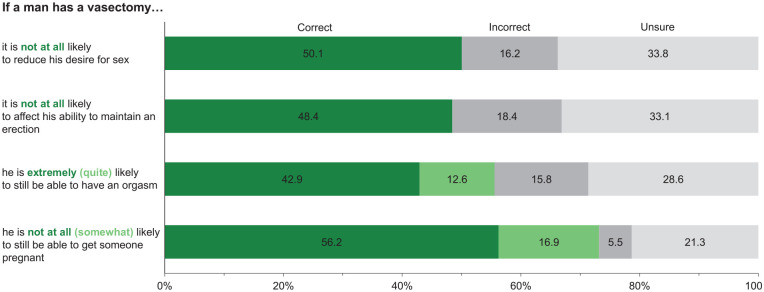
We assessed men’s knowledge of vasectomy by asking them to rate the likelihood (extremely likely, quite likely, somewhat or not at all likely or not sure) that the following would happen if a man had a vasectomy: it will reduce his desire for sex; it will affect his ability to maintain an erection; he will still be able to have an orgasm; and he can still get someone pregnant. These items were based on common misperceptions about vasectomy reported in the literature (Campbell et al., 2019; Landry & Ward, 1997; Shih et al., 2012). Changes in sexual desire and performance due to chronic pain following vasectomy are uncommon (Buchholz et al., 1994; Sharlip et al., 2012). Therefore, we classified men’s answers as accurate if they responded that it was “not at all likely” that vasectomy would affect sexual desire and one’s ability to maintain an erection and “extremely” or “quite likely” that men would still be able to have an orgasm. We considered answers of “not at all” or “somewhat likely” that a man can still get someone pregnant after a vasectomy as accurate given the low failure rate for the procedure (Trussell, 2011). We also asked respondents if they knew anyone who had a vasectomy.
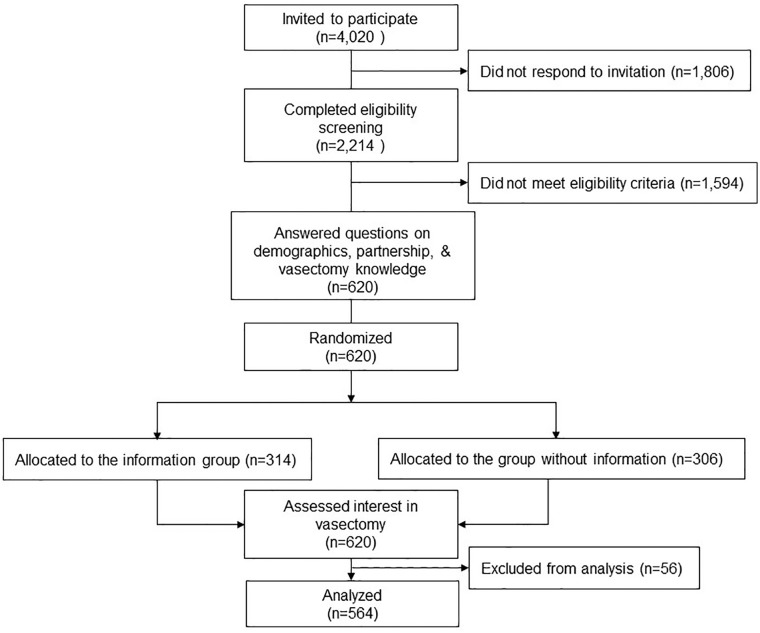
After participants answered the above-described survey items (including the vasectomy knowledge questions), we randomized them to receive or not receive the informational paragraph describing vasectomy (Figure 1). The goal of presenting the paragraph was to correct common misperceptions and determine whether having medically accurate information about vasectomy was associated with interest in the procedure. Then, we asked all respondents to indicate whether they would consider getting a vasectomy if they could do so for free or for a small co-pay, so as to assess interest when potentially high upfront costs are removed (Sonfield, 2015). We asked those who would not consider vasectomy or who responded “unsure” to report the main reason they would not get a vasectomy or were unsure. The response options, developed from prior research (Campbell et al., 2019; Shih et al., 2012), included not wanting a procedure that is permanent; not wanting a procedure on that part of the body; worrying about pain from procedure; worrying about how it would affect your sex life; feeling like less of a man; and satisfaction with current birth control method. Respondents could provide other reasons they would not consider vasectomy. The median time to complete the survey was 12 min.
Figure 1.
Respondent Eligibility and Survey Flow.
Analysis
We computed the overall distribution of men’s characteristics. We used chi-square tests to compare differences in the distribution of characteristics according to whether or not respondents received the informational paragraph about vasectomy to assess effective random assignment. We then evaluated the accuracy of men’s responses to the individual knowledge items about vasectomy’s effect on sexual functioning and method efficacy, overall and by race/ethnicity and household income ≤200% of the federal poverty level (FPL) or >200% FPL, given prior research noting knowledge differences between these groups.
Next, we summed men’s responses to the four knowledge questions and categorized respondents’ knowledge as low (0 correct answers), moderate (1–2 correct answers), and high (3–4 correct answers). Then, we computed the percentage of respondents who reported high knowledge and used chi-square tests and a multivariable-adjusted Poisson regression model with robust standard errors to assess characteristics associated with high knowledge. We focused on characteristics that may be associated with knowledge of contraception, including age, educational attainment, having biological children, whether they knew other men who had a vasectomy, partner use of permanent contraception, survey language, as well as race/ethnicity, income, and information group assignment. We used Poisson models because the estimates are more reliable than those from logistic regression when the outcome is common (>10%) (Zou, 2004).
We computed the percentage of men who would consider vasectomy if it were free or low cost, according to respondent and partnership characteristics, including respondent age, income, whether they had any biological children, and partner’s age, as well as race/ethnicity given potential sociocultural variation in vasectomy interest. In addition, we included respondents’ educational attainment, baseline vasectomy knowledge (high vs. moderate/low), their information group assignment, whether they knew other men who had undergone vasectomy, and importance of avoiding pregnancy (very/somewhat important versus a little/not at all important) and survey language. We used chi-square tests and estimated multivariable-adjusted Poisson regression models with robust standard errors to assess the association between these factors and vasectomy interest. We also conducted a sensitivity analysis limited to the 444 men whose partner had not undergone a permanent contraceptive procedure (e.g., tubal ligation); because the associations were similar, we present results for the full sample and control for partner use of permanent contraception (Appendix). As a final step, we computed frequencies for the reasons respondents would not consider vasectomy or were unsure.
We conducted all analyses in Stata 15 using the weights provided by GfK. The weights adjusted for the probability of selection into the panel and non-response based on geographic and demographic characteristics that were benchmarked to the 2017 March supplement of the Current Population Survey. The weights also adjusted for the Spanish-language distribution of respondents based on the 2016 American Community Survey.
Results
Of the 4,020 men invited to participate in the study, 2,214 completed the initial screening (55% cooperation rate) and 620 met the inclusion criteria and completed the survey. We later determined that 20 (3%) respondents were ineligible because they reported having had a vasectomy or were sterile (n = 3) or that their only sexual partner was ≥50 years of age (n = 17). After excluding those who were missing information on vasectomy knowledge (n = 19; 3%), vasectomy interest (n = 1) and other covariates (n = 16; 3%), the final analytic sample included 564 respondents.
More than half of men in the sample were 40 years of age or older (n = 344; 58%), had some college education or a college degree (n = 346; 53%), and reported a household income >200% FPL (n = 402; 77%; Table 1). Overall, 57% (n = 328) identified as white, 23% (n = 160) as Hispanic, and 12% (n = 48) as Black. The majority had biological children (n = 423; 75%) and were married or living with a female partner (n = 498; 90%). About half of respondents (n = 323; 56%) knew at least one other man who had a vasectomy and nearly three quarters (n = 415; 73%) stated that it was somewhat or very important to avoid pregnancy. Only 11% (n = 57) agreed that contraception should mainly be a woman’s responsibility. The most common contraceptive methods respondents reported currently using with their main sexual partner were female permanent contraception (n = 120; 22%) and condoms/withdrawal (n = 194; 35%); 16% (n = 94) reported they did not use a method. With the exception of current contraceptive use, there were no statistically significant differences in baseline characteristics between men who did and did not receive the informational paragraph about vasectomy.
Table 1.
Characteristics of Men Who Do Not Intend to Have (More) Children.
| Total (n = 564) |
Group without information (n = 278) |
Information group (n = 286) |
||
|---|---|---|---|---|
| Respondent characteristics | n (% a ) | n (% a ) | n (% a ) | p value b |
| Age, years | .222 | |||
| 25–29 | 52 (7.4) | 25 (6.3) | 27 (8.4) | |
| 30–39 | 168 (34.1) | 86 (36.7) | 82 (31.6) | |
| 40–44 | 125 (23.0) | 65 (25.1) | 60 (20.9) | |
| 45–55 | 219 (35.5) | 102 (31.8) | 117 (39.1) | |
| Race/ethnicity | .829 | |||
| White, non-Hispanic | 328 (57.5) | 161 (56.7) | 167 (58.3) | |
| Hispanic | 160 (23.3) | 77 (24.5) | 83 (22.1) | |
| Black, non-Hispanic | 48 (12.3) | 25 (12.8) | 23 (11.8) | |
| Other race/more than one race | 28 (6.8) | 15 (5.9) | 13 (7.7) | |
| Educational attainment | .099 | |||
| High school or less | 218 (46.7) | 118 (51.2) | 100 (42.2) | |
| Some college | 179 (27.1) | 79 (23.4) | 100 (30.7) | |
| College degree | 167 (26.2) | 81 (25.4) | 86 (27.1) | |
| Income relative to federal poverty level (FPL) | .334 | |||
| ≤200% FPL | 162 (22.8) | 86 (24.6) | 76 (21.1) | |
| >200% FPL | 402 (77.2) | 192 (75.4) | 210 (78.9) | |
| Number of children | .308 | |||
| 0 | 141 (24.5) | 66 (23.0) | 75 (25.9) | |
| 1 | 105 (18.5) | 56 (20.2) | 49 (16.8) | |
| 2 | 181 (32.6) | 97 (35.3) | 84 (30.0) | |
| ≥3 | 137 (24.4) | 59 (21.5) | 78 (27.2) | |
| Relationship status | .222 | |||
| Married | 411 (75.7) | 205 (76.5) | 206 (75.0) | |
| Living with partner, not married | 87 (14.2) | 40 (13.6) | 47 (14.8) | |
| Not living with partner/single | 66 (10.1) | 33 (9.9) | 33 (10.2) | |
| Partner age, years | .242 | |||
| <30 | 84 (13.4) | 45 (13.5) | 39 (13.4) | |
| 30–39 | 205 (39.1) | 96 (39.0) | 109 (39.3) | |
| 40–44 | 120 (20.9) | 65 (24.2) | 55 (17.7) | |
| 45–49 | 155 (26.5) | 72 (23.3) | 83 (29.6) | |
| Knows other men with vasectomy | .907 | |||
| Yes | 323 (56.2) | 160 (55.9) | 163 (56.5) | |
| No | 241 (43.8) | 118 (44.1) | 123 (43.5) | |
| Importance of avoiding pregnancy | .166 | |||
| Very important | 316 (55.9) | 140 (51.4) | 176 (60.2) | |
| Somewhat important | 99 (17.6) | 51 (18.8) | 48 (16.4) | |
| A little/not at all important/not sure | 149 (26.5) | 87 (29.8) | 62 (23.4) | |
| Contraception is a woman’s responsibility | .407 | |||
| Agree/strongly agree | 57 (10.8) | 26 (9.7) | 31 (11.9) | |
| Neither agree nor disagree | 155 (27.1) | 73 (26.1) | 82 (28.0) | |
| Disagree/strongly disagree | 352 (62.1) | 179 (64.2) | 173 (60.0) | |
| Contraceptive use with main sexual partner | .028 | |||
| Permanent female method | 120 (21.7) | 67 (24.6) | 53 (18.8) | |
| Intrauterine device or implant | 54 (9.4) | 24 (9.3) | 30 (9.5) | |
| Oral contraceptive pills | 80 (13.3) | 30 (9.6) | 50 (17.0) | |
| Injectable contraceptive | 16 (2.8) | 10 (3.7) | 6 (1.2) | |
| Contraceptive patch or ring | 6 (1.7) | 5 (3.1) | 1 (0.3) | |
| Condoms and/or withdrawal | 194 (34.6) | 89 (32.0) | 105 (37.2) | |
| No method | 94 (16.5) | 53 (17.8) | 41 (15.3) | |
| Survey language | .983 | |||
| English | 499 (89.4) | 250 (89.3) | 249 (89.4) | |
| Spanish | 65 (10.6) | 28 (10.7) | 37 (10.6) |
Percentages are weighted to account for the survey design. bDifferences between the information group and group without information were assessed using chi-square tests.
Approximately half of the sample accurately reported that vasectomy did not adversely affect a man’s sexual desire (n = 285; 50%), his ability to maintain an erection (n = 270; 48%), or his ability to have an orgasm (n = 322; 55%); nearly three-quarters (n = 414; 73%) accurately reported that a man with a vasectomy was not at all or only somewhat likely to get someone pregnant (Figure 2). A higher percentage of white men had accurate knowledge about vasectomy’s effect on sexual desire (53%) and his ability to maintain an erection (52%) compared with Black men (sexual desire: 42%; maintain an erection: 44%) and Hispanic men (sexual desire: 39%; maintain an erection: 36%) (all p < .05). In addition, men with incomes >200% FPL were more likely than those with incomes ≤200% FPL to have accurate knowledge about vasectomy’s effect on a man’s sexual desire (53% vs. 39%), his ability to maintain an erection (52% vs. 35%), have an orgasm (60% vs. 42%), and his ability to get someone pregnant (76% vs. 62%; all p < .01).
Figure 2.
Baseline Knowledge of Vasectomy’s Effect on Sexual Functioning and Efficacy Among Men Who Do Not Intend to Have (More) Children.
Overall, 51% of the sample (n = 287) demonstrated high vasectomy knowledge, with ≥3 accurate responses to the four knowledge questions. After multivariable adjustment, respondents who knew someone who had a vasectomy (vs. did not know anyone) had higher vasectomy knowledge (prevalence ratio [PR]: 1.50; 95% CI [1.22, 1.85]; Table 2). Hispanic respondents (PR: 0.67; 95% CI [0.49, 0.92]) and those living on incomes <200% FPL (PR: 0.73; 95% CI [0.55, 0.96]) were less likely to have high vasectomy knowledge than White, non-Hispanic and higher income respondents, respectively.
Table 2.
Characteristics Associated With High Baseline Knowledge of Vasectomy Among Men Who Do Not Intend to Have (More) Children a (n = 564).
| Respondent characteristics | % b | PR | 95% CI |
|---|---|---|---|
| All men | 51.1 | — | — |
| Age, years | |||
| 25–29 | 46.1 | 0.94 | [0.66, 1.32] |
| 30–39 | 46.4 | 0.90 | [0.73, 1.11] |
| 40–44 | 52.5 | 0.91 | [0.74, 1.13] |
| 45–55 | 55.9 | 1 | (ref) |
| Race/ethnicity c ** | |||
| White, non-Hispanic | 54.0 | 1 | (ref) |
| Hispanic | 39.3 | 0.67 | [0.49, 0.92] |
| Black, non-Hispanic | 44.6 | 0.93 | [0.65, 1.33] |
| Educational attainment** | |||
| High school or less | 43.3 | 0.86 | [0.69, 1.07] |
| Some college | 53.9 | 0.94 | [0.77, 1.14] |
| College degree | 62.3 | 1 | (ref) |
| Income relative to federal poverty level (FPL)*** | |||
| ≤200% FPL | 34.9 | 0.73 | [0.55, 0.96] |
| >200% FPL | 55.9 | 1 | (ref) |
| Has biological children | |||
| No | 46.6 | 0.91 | [0.72, 1.14] |
| Yes | 52.6 | 1 | (ref) |
| Partner had permanent contraceptive procedure | |||
| No | 49.6 | 1 | (ref) |
| Yes | 56.7 | 1.15 | [0.95, 1.41] |
| Presented with information about vasectomy d | |||
| Did not receive informational paragraph | 52.6 | 1 | (ref) |
| Received informational paragraph | 49.7 | 0.92 | [0.77, 1.08] |
| Knows other men with vasectomy*** | |||
| Yes | 61.4 | 1.49 | [1.21, 1.83] |
| No | 38.0 | 1 | (ref) |
| Survey language | |||
| English | 51.8 | 1 | (ref) |
| Spanish | 45.4 | 1.51 | [0.98, 2.34) |
Note. PR = prevalence ratios from Poisson regression models; CI: confidence interval.
Those with high knowledge correctly answered at least 3 of the 4 knowledge questions related to vasectomy’s effect on sexual desire, maintaining an erection, having an orgasm, and being able to get someone pregnant. bPercentages are weighted to account for the survey design. cThe model also included a term for men who identified as more than one race/other race. dRespondents were assigned to receive (or not receive) an informational paragraph describing how vasectomy is performed, its effects on sexual functioning, and method effectiveness after answering questions about their vasectomy knowledge.
χ2 p values: **p < .01. ***p < .001.
Approximately one-third of the sample (n = 186; 34%) said they would consider getting a vasectomy if it were free or available for a small co-pay (Table 3). In multivariable-adjusted models, men between 30 and 39 years of age (versus ≥45 years), who had children, and whose main sexual partner was between 30 and 39 years old (versus ≥45 years) were more likely to consider vasectomy. In addition, men with high (vs. moderate/low) vasectomy knowledge (PR: 1.36; 95% CI [1.04, 1.77]) and men who knew someone who had a vasectomy (PR: 1.39; 95% CI [1.02, 1.87]) were more likely to consider getting a vasectomy; however, whether a respondent received the informational paragraph about vasectomy during the survey was not significantly associated with interest in vasectomy. Compared with those who reported preventing pregnancy was very important, respondents who reported that it was a little or not at all important to prevent pregnancy were less likely to be interested in vasectomy.
Table 3.
Characteristics Associated With Interest in Vasectomy Among Men Who Do Not Intend to Have (More) Children (n = 564).
| Respondent characteristics | % a | PR | 95% CI |
|---|---|---|---|
| All men | 34.6 | — | — |
| Age, years* | |||
| 25–29 | 33.2 | 1.66 | [0.95, 2.88] |
| 30–39 | 46.0 | 1.78 | [1.20, 2.65] |
| 40–44 | 39.3 | 1.48 | [0.95, 2.31] |
| 45–55 | 21.0 | 1 | (ref) |
| Race/ethnicity b | |||
| White, non-Hispanic | 37.0 | 1 | (ref) |
| Hispanic | 30.4 | 0.97 | [0.71, 1.33] |
| Black, non-Hispanic | 30.5 | 1.11 | [0.70, 1.74] |
| Educational attainment † | |||
| High school or less | 30.0 | 1.01 | [0.74, 1.37] |
| Some college | 35.2 | 0.97 | [0.74, 1.28] |
| College degree | 42.1 | 1 | (ref) |
| Income relative to federal poverty level (FPL) | |||
| ≤200% FPL | 29.0 | 0.94 | [0.68, 1.31] |
| >200% FPL | 36.3 | 1 | (ref) |
| Has children* | |||
| No | 24.8 | 1 | (ref) |
| Yes | 37.8 | 1.77 | [1.25, 2.52] |
| Partner age, years* | |||
| <30 | 36.0 | 1.54 | [0.85, 2.79] |
| 30–39 | 46.5 | 1.92 | [1.13, 3.27] |
| 40–44 | 32.8 | 1.42 | [0.83, 2.42] |
| ≥45 | 17.9 | 1 | (ref) |
| Partner had permanent contraceptive procedure † | |||
| No | 37.0 | 1 | (ref) |
| Yes | 26.0 | 0.73 | [0.51, 1.05] |
| Presented with information about vasectomy c | |||
| Did not receive informational paragraph | 30.5 | 1 | (ref) |
| Received informational paragraph | 38.6 | 1.22 | [0.96, 1.56] |
| High knowledge of vasectomy at baseline* | |||
| No | 26.1 | 1 | (ref) |
| Yes | 42.8 | 1.37 | [1.05, 1.78] |
| Knows other men with vasectomy* | |||
| No | 25.4 | 1 | (ref) |
| Yes | 41.8 | 1.39 | [1.03, 1.89] |
| Importance of avoiding pregnancy* | |||
| Very important | 42.7 | 1 | (ref) |
| Somewhat important | 31.1 | 0.69 | [0.49, 0.97] |
| A little/not at all important/not sure | 19.9 | 0.49 | [0.32, 0.73] |
| Survey language | |||
| English | 35.6 | 1 | (ref) |
| Spanish | 26.7 | 0.84 | [0.46, 1.50] |
Note. PR = prevalence ratio from multivariable-adjusted Poisson regression models; CI = confidence interval.
Percentages are weighted to account for the survey design. bThe model also included a term for men who identified as more than one race/other race. cRespondents were assigned to receive (or not receive) an informational paragraph describing how vasectomy is performed, its effects on sexual functioning, and method effectiveness prior to answering the question about whether they would consider getting a vasectomy.
χ2 p values: †p < .10. *p < .05.
One-third of respondents who would not consider vasectomy or were unsure (n = 123) indicated that they were satisfied with their current birth control method (Table 4); among these men, the most commonly used methods were partner’s tubal ligation or hysterectomy (n = 45; 36%) and condoms and/or withdrawal (n = 35; 31%); 14% (n = 17) reported they were not using a method with their main sexual partner. In addition, 23% of respondents who were not interested in vasectomy (n = 89) stated they did not want a procedure on that part of their body, and 14% (n = 48) indicated that they were not interested in a permanent method. Few men (<5%) reported that they were concerned about how vasectomy would affect their sex life (n = 15) or that it would make them feel like less than a man (n = 9).
Table 4.
Main Reason Men Reported They Are Not Interested in Vasectomy (n = 375).
| Reasons respondents were not interested in vasectomy | n | % a |
|---|---|---|
| Satisfied with current birth control method | 123 | 33.0 |
| Do not want a procedure on that part of my body | 89 | 22.9 |
| Do not want a permanent procedure | 48 | 14.0 |
| Worried about pain from procedure | 26 | 7.4 |
| Still need more information about vasectomy | 29 | 6.8 |
| Worried about how it will affect my sex life | 15 | 3.8 |
| Would feel like less of a man | 9 | 2.9 |
| Other b | 36 | 9.2 |
Percentages are weighted to account for the survey design. bOther reasons included partner had a tubal ligation, hysterectomy or is unable to get pregnant (n = 13); not interested or not needed (n = 8); does not want any form of surgery (n = 2).
Discussion
In this racially and ethnically diverse sample of U.S. men who do not want any or any more children, only half of respondents had accurate knowledge of vasectomy, as assessed by the items in our survey. Respondents demonstrated more accurate knowledge about not being able to get a sexual partner pregnant after undergoing vasectomy than about vasectomy’s effect on sexual functioning. These results are consistent with prior qualitative studies and recent survey findings of vasectomy knowledge in U.S. South (Campbell et al., 2019; Shih et al., 2012; A. L. White et al., 2020). Erroneous perceptions about the impacts of vasectomy on sexual functioning may be related to men’s limited awareness about how vasectomy is performed and the biological processes involved in sexual functioning (Campbell et al., 2019; Shih et al., 2012). Like other studies (Hubert et al., 2016; A. L. White et al., 2020), men in our sample who knew others who had a vasectomy were more knowledgeable about the procedure. Thus, these social connections may be able to dispel common myths and misinformation, even if men themselves do not have detailed knowledge of the procedure, and may reduce stigma surrounding vasectomy use (Shih et al., 2012).
In addition, more than one-third of respondents indicated that they would consider getting a vasectomy if it was available for free or a small co-payment. This level of interest is similar to that reported in older studies and notably higher than the percentage of U.S. men who rely on vasectomy for contraception (Heinemann et al., 2005; Hubert et al., 2016; Zhang & Eisenberg, 2022), indicating that structural barriers may preclude many men from seeking a desired procedure. We also were able to identify several sub-groups of men among whom interest was greater: those indicating a strong desire to avoid pregnancy, who were in their 30s, and who had a female sexual partner in her 30s. This latter finding may be related to couples’ reluctance to use hormonal contraception (and experience of side effects) or less effective male methods (e.g., condoms) for extended periods after deciding they do not want more children (Mumford, 1983). Men in their 30s are less likely than younger men to receive contraceptive counseling (Chabot et al., 2011), which may reflect provider bias about men’s age-specific sexual and reproductive health needs but not men’s lack of interest. By proactively assessing men’s desires to avoid future pregnancies, attitudes about contraceptive responsibility, and partnership characteristics, health care providers could better support men’s contraceptive involvement throughout the reproductive lifecourse.
Our study adds to the literature on differences in vasectomy use by race/ethnicity and income. These well-documented differences have often been attributed to lack of knowledge and interest in the procedure (Borrero et al., 2009; Sharma et al., 2013). Black, Hispanic, and low-income respondents demonstrated less accurate knowledge than white men and those with higher incomes. This may be related to social inequities in access to health information and education, given prior research showing that these factors play an important mediating role in men’s vasectomy knowledge (Hubert et al., 2016; Huether et al., 1984; Marván et al., 2017; A. L. White et al., 2020). There was limited variation in vasectomy interest by race/ethnicity and income in our sample. These results suggest that observed differences in vasectomy use may instead be related to larger structural factors, such as differences in insurance coverage, access to vasectomy providers, and provider bias about men’s interest, that could impede those who want the procedure from getting it (Borrero et al., 2010; K. White et al., 2017).
Although this sample was limited to men who did not want any or any more children, the majority was not interested in vasectomy, primarily citing satisfaction with their current contraceptive method and not wanting to use a permanent method. Many were relying on condoms and withdrawal, and this may reflect their limited knowledge about the effectiveness of these methods relative to other contraceptives, concerns about sexually transmitted infections, their or their partner’s preferences, or fluctuating desires about having children related to potentially shifting financial or relationship circumstances (Campbell et al., 2019). Notably, respondents provided with additional information on how vasectomy is performed and recovery from the procedure did not express greater interest in undergoing vasectomy. More interactive approaches that include values clarification exercises and help men reflect on any concerns about permanently ending fertility, along with visual displays showing how vasectomy is performed and comparing the risk and effectiveness of vasectomy relative to other male methods and female permanent contraception, would support informed and value-concordant decision making. In turn, this may affect men’s subsequent pursuit of this method.
This study has several limitations. Only 55% of age-eligible men responded to the survey invitation, and although this cooperation rate is somewhat low, it is typical of other online panel surveys about health (Grossman et al., 2013; Nyhan et al., 2014; K. White et al., 2016). In addition, our knowledge assessment focused on a limited set of items based on common concerns reported in other studies, but men may have limited knowledge about other aspects of vasectomy that were not assessed, including misperceptions about pain and recovery from the procedure that could be examined in other studies (Campbell et al., 2019; Shih et al., 2012). Men responding to the survey may have been more interested in contraception than those who did not respond. Therefore, men’s interest in vasectomy in this sample may not reflect that of all U.S. men who do not want any or any more children. Men’s interest in vasectomy may not predict their eventual use of the method. Factors such as men’s certainty about their fertility desires and relationship stability, gendered norms around the work of pregnancy prevention, as well as insurance coverage and access to a vasectomy provider, may affect men’s intentions and use of the method. Future studies should assess the relationship between these factors and the percentage of interested men who subsequently get a vasectomy.
Despite these limitations, our study is strengthened by our use of a sample derived from a nationally representative panel of U.S. households and a systematic exploration of the characteristics of men who may be interested in vasectomy. Our findings identify a potentially unrecognized interest in vasectomy among U.S. men who do not want any or any more children, including groups that previously have been viewed as having limited interest in the method. The characteristics of men who demonstrated less accurate knowledge and who expressed interest in vasectomy point to the need for approaches to provide salient and high-quality information to facilitate uptake of vasectomy, thereby contributing to greater male involvement in family planning and increasing reliance on this effective contraceptive method.
Supplemental Material
Supplemental material, sj-docx-1-jmh-10.1177_15579883221098574 for Vasectomy Knowledge and Interest Among U.S. Men Who Do Not Intend to Have More Children by Kari White, Macarena Martínez Órdenes, David K. Turok, Jessica D. Gipson and Sonya Borrero in American Journal of Men’s Health
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by grant K01HD079563, and Dr. Turok received support from grant K24HD087436, both from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The funder played no role in the design and conduct of the study; interpretation of the data; or preparation, review, or approval of the manuscript for publication.
ORCID iD: Kari White  https://orcid.org/0000-0001-6463-8626
https://orcid.org/0000-0001-6463-8626
Supplemental material: Supplemental material for this article is available online.
References
- Anderson J. E., Jamieson D. J., Warner L., Kissin D. M., Nangia A. K., Macaluso M. (2012). Contraceptive sterilization among married adults: National data on who chooses vasectomy and tubal sterilization. Contraception, 85(6), 552–557. [DOI] [PubMed] [Google Scholar]
- Bartz D., Greenberg J. A. (2008). Sterilization in the United States. Reviews in Obstetrics and Gynecology, 1(1), 23–32. [PMC free article] [PubMed] [Google Scholar]
- Borrero S., Moore C., Creinin M., Ibrahim S. (2010). Low rates of vasectomy among minorities: A result of differential receipt of counseling? American Journal of Men’s Health, 4(3), 243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrero S., Schwarz E. B., Reeves M. F., Bost J. E., Creinin M. D., Ibrahim S. A. (2009). Does vasectomy explain the difference in tubal sterilization rates between black and white women? Fertility and Sterility, 91(5), 1642–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchholz N.-P., Weuste R., Mattarelli G., Woessmer B., Langwitz W. (1994). Post-vasectomy erectile dysfunction. Journal of Psychosomatic Research, 38(7), 759–762. [DOI] [PubMed] [Google Scholar]
- Campbell A. D., Turok D. K., White K. (2019). Fertility intentions and perspectives on contraceptive involvement among low-income men aged 25 to 55. Perspectives on Sexual and Reproductive Health, 51(3), 125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabot M. J., Lewis C., Thiel de, Bocanegra H., Darney P. (2011). Correlates of receiving reproductive health care services among US men aged 15 to 44 years. American Journal of Men’s Health, 5(4), 358–366. [DOI] [PubMed] [Google Scholar]
- Daniels K., Abma J. C. (2020). Current contraceptive status among women aged 15–49: United States, 2017–2019. National Center of Health Statistics. https://www.cdc.gov/nchs/data/databriefs/db388-H.pdf [PubMed] [Google Scholar]
- GfK. (2018). KnowledgePanel Design Summary. Ipsos (formerly GfK). https://www.ipsos.com/sites/default/files/18-11-53_Overview_v3.pdf
- Grossman D., Grindlay K., Li R., Potter J. E., Trussell J., Blanchard K. (2013). Interest in over-the-counter access to oral contraception among women in the United States. Contraception, 88(4), 544–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinemann K., Saad F., Wiesemes M., Whilte S., Heinemann L. (2005). Attitudes toward male fertility control: Results from a multinational survey on four continents. Human Reproduction, 20(2), 549–556. [DOI] [PubMed] [Google Scholar]
- Hendrix N., Chauhan S., Morrison J. C. (1999). Sterilization and its consequences. Obstetrical and Gynecological Survey, 54(12), 766–777. [DOI] [PubMed] [Google Scholar]
- Hubert C., White K., Hopkins K., Grossman D., Potter J. E. (2016). Latino men’s interest in vasectomy in El Paso, Texas. Journal of Health Care for the Poor and Underserved, 27, 762–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huether C., Howe S., Kelaghan J. (1984). Knowledge, attitudes and practice regarding vasectomy among residents of Hamilton county, Ohio, 1980. American Journal of Public Health, 74(1), 79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye K., Suellentrop K., Sloup C. (2009). The Fog Zone: How misperceptions, magical thinking, and ambivalence put young adults at risk for unplanned pregnancy. Power to Decide (formerly the National Campaign to Prevent Teen and Unplanned Pregnancy). https://powertodecide.org/what-we-do/information/resource-library/fog-zone
- Landry E., Ward V. (1997). Perspectives from couples on the vasectomy decision: A six-country study. In Ravindran T. K. S., Berer M., Cottingham J. (Eds.), Beyond acceptability: Users’ perspectives on contraception (pp. 58–67). Reproductive Health Matters. [Google Scholar]
- Lindberg L. D., Kost K. (2014). Exploring US men’s birth intentions. Maternal and Child Health Journal, 18(3), 625–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez G. M., Chandra A., Abma J. C., Jones J., Mosher W. D. (2006). Fertility, contraception and fatherhood: Data on men and women from Cycle 6 (2002 of the National Survey of Family Growth). Vital Health Stat, 23(26), 1–142. [PubMed] [Google Scholar]
- Marván M. L., Ehrenzweig Y., Hernández-Aguilera D. (2017). Mexican men’s view of vasectomy. American Journal of Men’s Health, 11(3), 610–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell E. W., Levis D. M., Prue C. E. (2012). Preconception health: Awareness, planning and communication among a sample of US men and women. Maternal and Child Health Journal, 16(1), 31–39. [DOI] [PubMed] [Google Scholar]
- Mumford S. D. (1983). The vasectomy decision-making process. Studies in Family Planning, 14(3), 83–88. [PubMed] [Google Scholar]
- National Center for Health Statistics. (2015). National survey of family growth, 2013-2015 [Data set]. https://www.cdc.gov/nchs/nsfg/nsfg_2013_2015_puf.htm
- National Center for Health Statistics. (2019). National Survey of Family Growth, male respondent file 2017-2019 [Data set]. https://www.cdc.gov/nchs/nsfg/nsfg_2017_2019_puf.htm
- Nyhan B., Reifler J., Richey S., Freed G. L. (2014). Effective messages in vaccine promotion: A randomized trial. Pediatrics, 133(4), e835–e842. [DOI] [PubMed] [Google Scholar]
- Sharlip I. D., Belker A. M., Honig S., Labrecque M., Marmar J. L., Ross L. S., . . . Sokal D. C. (2012). Vasectomy: AUA guideline. The Journal of Urology, 188(6 Supplement), 2482–2491. [DOI] [PubMed] [Google Scholar]
- Sharma V., Le B. V., Sheth K. R., Zargaroff S., Dupree J. M., Cashy J., Brannigan R. E. (2013). Vasectomy demographics and postvasectomy desire for future children: Results from a contemporary national survey. Fertility and Sterility, 99(7), 1880–1885. [DOI] [PubMed] [Google Scholar]
- Shih G., Dubé K., Dehlendorf C. (2013). “We never thought of a vasectomy”: A qualitative study of men and women’s counseling around sterilization. Contraception, 88(3), 376–381. [DOI] [PubMed] [Google Scholar]
- Shih G., Dubé K., Sheinbein M., Borrero S., Dehlendorf C. (2012). He’s a real man: A qualitative study of the social context of couple’s vasectomy decisions among a racially diverse population. American Journal of Men’s Health, 7(3), 206–213. [DOI] [PubMed] [Google Scholar]
- Sonfield A. (2015). Rounding out the contraceptive coverage guarantee: Why “male” contraceptive methods matter for everyone. Guttmacher Policy Review, 18(2), 34–39. [Google Scholar]
- Trussell J. (2011). Contraceptive failure in the United States. Contraception, 83(5), 397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A. L., Davis R. E., Billings D. L., Mann E. S. (2020). Men’s vasectomy knowledge, attitudes, and information-seeking behaviors in the Southern United States: Results from an exploratory survey. American Journal of Men’s Health, 14(4), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K., Campbell A., Hopkins K., Grossman D., Potter J. E. (2017). Barriers to offering vasectomy at publicly funded family planning organizations in Texas. American Journal of Men’s Health, 11(3), 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K., Potter J. E., Stevenson A. J., Fuentes L., Hopkins K., Grossman D. (2016). Women’s knowledge of and support for abortion restrictions in Texas: Findings from a statewide representative survey. Perspectives on Sexual and Reproductive Health, 48(4), 189–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Eisenberg M. L. (2022). Vasectomy utilization in men aged 18–45 declined between 2002 and 2017: Results from the United States National Survey for Family Growth data. Andrology, 10(1), 137–142. [DOI] [PubMed] [Google Scholar]
- Zou G. (2004). A modified Poisson regression approach to prospective studies with binary data. American Journal of Epidemiology, 159(7), 702–706. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jmh-10.1177_15579883221098574 for Vasectomy Knowledge and Interest Among U.S. Men Who Do Not Intend to Have More Children by Kari White, Macarena Martínez Órdenes, David K. Turok, Jessica D. Gipson and Sonya Borrero in American Journal of Men’s Health