Abstract
Background
Although the Coronavirus Disease 2019 (COVID-19) has greatly impacted individuals' mental health and quality of life, network analysis studies of associations between symptoms of common syndromes during the pandemic are lacking, particularly among Macau residents. This study investigated the network structure of insomnia, anxiety, and depression and explored their associations with quality of life in this population.
Method
This online survey was conducted in Macau between August 18 and November 9, 2020. Insomnia, anxiety, depressive symptoms, and quality of life were assessed with the Insomnia Severity Index, Generalized Anxiety Disorder Scale, Patient Health Questionnaire, and World Health Organization Quality of Life-brief version, respectively. Analyses were performed to identify central symptoms and bridge symptoms of this network and their links to quality of life.
Results
975 participants enrolled in this survey. The prevalence of depressive, anxiety and insomnia symptoms were 38.5% (95% confidence interval (CI): 35.5%–41.5%), 28.8% (95%CI: 26.0%–31.7%), and 27.6% (95% CI: 24.8%–30.4%), respectively. “Sleep maintenance” had the highest expected influence centrality, followed by “Trouble relaxing”, “Interference with daytime functioning”, “Irritability”, and “Fatigue”. Five bridge symptoms were identified: “Sleep problems”, “Restlessness”, “Irritability”, “Severity of sleep onset”, and “Motor activity”. The insomnia symptom, “Sleep dissatisfaction”, had the strongest direct relation to quality of life.
Conclusion
Insomnia symptoms played a critical role in the distress symptom network regarding node and bridge centrality as well as associations with quality of life among Macau residents. Close attention to these symptoms may be critical to reducing risk and preventing exacerbations in common forms of distress in this population.
Keywords: Insomnia, Depression, Anxiety, Quality of life, COVID-19, Network analysis
1. Introduction
Coronavirus Disease 2019 (COVID-19) has brought unprecedented challenges to China and the entire world. The Macau Special Administrative Region of China (Macao SAR), located on the west of the Pearl Delta River estuary in southern China, is centered upon the gaming and tourism industries. In 2019, taxation revenue in Macau was US$14.4 billion, of which 85% (i.e., US$12.3 billion) was from casinos (Bamidele, 2019). Public health measures adopted in Macau during the COVID-19 pandemic have been similar to those in mainland China. Since a level III alert (moderate level) was announced on January 5, 2020 in Macau, the Macau government took active, rapid measures to contain the outbreak including suspensions of group tour visas for mainland Chinese visitors to Macao SAR on January 22, 2020, suspensions of licensed casinos and other entertainment venue operations for 15 days from February 5, 2020, and bans of all non-resident workers (except from Mainland China, the region of Taiwan, and Hong Kong SAR) from entering Macao SAR on March 19, 2020 (Loi et al., 2021). These control measures have had negative economic effects on about three quarters of the territory's population who were directly or indirectly employed in casinos and other entertainment venue operations, as well as government tax revenues (Elizabeth et al., 2021).
Recently, a systematic review (Xiong et al., 2020) pointed out that lower or unstable socioeconomic status and unemployment are risk factors for developing psychiatric symptoms (e.g., anxiety symptom, depressive symptom, psychological distress and stress) during the COVID-19 pandemic. From this perspective, many Macau residents may experience serious mental health problems at this particular time. Additionally, a large-scale nationwide study conducted in the general population of China (n = 56,679) reported the prevalence of depressive, anxiety, and insomnia symptoms was 27.9%, 31.6%, and 29.2%, respectively (Wang et al., 2021). And, compared with individuals not in quarantine, those undergoing quarantine had an increased risk for poor psychological outcomes (Chen et al., 2022; Gu et al., 2021; Wang et al., 2021). Moreover, in the general population of other countries, the impact of poor psychological health on quality of life due to COVID-19 pandemic and lockdown has been documented (Epifanio et al., 2021; Ferreira et al., 2021; Kılınçel et al., 2021). However, to date, the absence of studies on the mental health status of Macau residents and its links with quality of life provided us with the impetus to study this issue in this population under pandemic conditions.
During the past few years, network analysis (NA) has been used widely in many fields to understand the interconnectedness of multicomponent systems (Montazeri et al., 2020). NA has been found to be particularly advantageous in psychiatry due to insights it has provided in relation to interactions of symptoms of psychopathology and mental health (Beard et al., 2016). Two important elements - “Nodes” and “Edges” constitute the network graph, which is the core concept in NA (Epskamp et al., 2012). Each node stands for one symptom and each edge represents the partial correlation coefficient between two nodes, after controlling for the effects of other nodes in the model (Epskamp et al., 2012). The goal of this approach is to identify a central node that is highly connected to other nodes and is emphasized due to its potential clinical implications for risk of developing particular syndromes and targeted interventions. This novel approach also has possible utility in understanding psychiatric comorbidities (Cramer et al., 2010b) wherein particular symptoms of one disorder are related to a higher risk of experiencing other disorders. Symptoms that increase the risk of contagion from one disorder to other disorders are called “bridge symptoms” and can be identified in NA (Cramer et al., 2010b). As such, clinicians can target bridge symptoms to treat or prevent comorbidity (Jones et al., 2021).
In NA studies of psychiatric symptoms, researchers have found both common and unique network structures in various samples. For example, in a sample of migrant Filipino workers employed in Macau, “Fatigue” was the most central symptom in the whole network, followed by “Worry too much” and “Depressed mood” (Garabiles et al., 2019). The latter two symptoms were also identified as central symptoms in a psychiatric sample from the United States (Beard et al., 2016). Similarly, symptoms “Fatigue” and “Feeling of worthlessness” were found to be the most influential in the anxiety and depressive symptom (anxiety-depression symptom hereafter) network of nursing students in China (Ren et al., 2021). Another network analysis conducted during and after the peak of the pandemic also found that “Fatigue”, as a bridge symptom, played an important role in the anxiety and depression model after the peak of the pandemic (Wang et al., 2020). Given that fatigue has emerged as a key symptom in various NA studies of anxiety and depression, there may be utility in considering co-morbid syndromes that contribute to fatigue within network models. To this end, insomnia symptoms (insomnia hereafter) characterized by dissatisfaction with sleep quantity or quality that often results in fatigue (American Psychiatric Association, 2013), may be a useful focus in network models of anxiety and depression.
To date, no network studies have been conducted to explore psychiatric symptoms among Macau residents during the pandemic and research on anxiety-depression symptom networks has tended to ignore salient related syndromes, particularly insomnia. To address these gaps, the current study is the first to use NA to investigate interrelations between symptoms of anxiety, depression and insomnia among Macau residents during the COVID-19 pandemic. Apart from identifying central and bridge symptoms in this study, we also focused on identifying symptoms that are directly related to quality of life as a foundation for developing targeted interventions to improve quality of life among Macau residents.
2. Methods
2.1. Participants and study procedure
This online survey was conducted in Macau between August 18, 2020 and November 9, 2020, using a convenience sampling method. Due to the COVID-19 pandemic, face-to-face assessments were not adopted. Following other studies (Luo et al., 2020; Zhou et al., 2020), an online assessment was conducted using the WeChat-based “Questionnaire Star” program that can be embedded in smartphones. WeChat is a widely used communication program with over 1.2 billion active users in China. A QR code linked to the invitation and assessment forms was generated and delivered to several online platforms (e.g., WhatsApp, WeChat, Facebook). Following previous studies (Di Blasi et al., 2021; Ren et al., 2021; Wang et al., 2020), to understand a fuller spectrum of mental health concerns among Macau residents, dimensional conceptualizations were adopted (National Institute of Mental Health, 2021), i.e., residents with and without symptoms of depression, anxiety, and/or insomnia were recruited so that the full spectrum of functioning related to these issues, from normal to abnormal, could be assessed. Inclusion criteria were the following: (1) Macau residents living in Macau during the COVID-19 pandemic; (2) aged above 18 years; (3) capable to understand the purposes and content of the survey. All participants provided online informed consent. This study was approved by the ethics panel of Beijing Anding Hospital.
2.2. Measures
The Insomnia Severity Index (ISI) questionnaire was used to measure the severity of insomnia symptoms (Morin, 1993). The ISI includes seven items, each rated on a 5-point scale (from 0 to 4), with higher total scores indicating more severe insomnia symptoms. The Chinese version of the ISI has been well validated in Chinese samples (Bai et al., 2018).
Depressive symptoms were assessed with the Chinese version of the nine-item Patient Health Questionnaire (PHQ-9) (Chen et al., 2015; Kroenke et al., 2001). PHQ-9 items are based on the nine Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria for major depressive disorder; each item is scored on a frequency scale from 0 (not at all) to 3 (nearly every day). Higher total PHQ-9 scores indicate more severe depressive symptoms. PHQ-9 total scores of 5, 10, 15, and 20 reflect mild, moderate, moderately severe and severe depressive symptoms, respectively.
Anxiety symptoms were measured with the Chinese version of the seven-item Generalized Anxiety Disorder scale (GAD-7) (He et al., 2010; Spitzer et al., 2006). GAD-7 items are assessed on a 4-point frequency scale with 0, 1, 2, and 3 indicating “not at all”, “several days”, “more than half the days”, and “nearly every day”, respectively. Higher GAD-7 scores indicate more severe anxiety symptoms. Total scores of 5, 10, 15 are regarded as cut-off points for mild, moderate and severe anxiety symptoms, respectively. Global quality of life (QoL) was assessed by summing scores on the first two items of the World Health Organization Quality of Life-brief version (WHOQOL-BREF) (Fang et al., 1999; The WHOQOL Group, 1998; Xia et al., 2012); higher total scores reflected higher reported QoL.
2.3. Data analysis
2.3.1. Network estimation
For data analysis, the R program (R Core Team, 2020) was used to conduct NA. Within a network model, each symptom is viewed as a node, and the association between two nodes is regarded as an edge (Epskamp et al., 2012). Least absolute shrinkage and selection operator (LASSO) and extended Bayesian information criteria (EBIC) were used to shrink edges in the network and choose related tuning parameters so that the symptom network was sparser and easier to interpret (Epskamp et al., 2012). Because mean score distributions on study items were skewed, nonparametric correlations were calculated via nonparanormal transformations (Han et al., 2012). R packages qgraph (version 1.6.9) (Epskamp et al., 2012) and bootnet (version 1.4.3) (Epskamp et al., 2018) were applied to estimate and illustrate the network model visually. Thicker edges indicated stronger associations between two nodes, green edges represented positive associations and red edges represented negative relations.
2.3.2. Centrality and stability
In order to quantify the importance of each node in the network, expected influence was calculate via R package qgraph (Epskamp et al., 2012). This approach is more appropriate for networks that comprise both positive and negative edges compared to the traditional centrality index (i.e., node strength) (Robinaugh et al., 2016). Nodes having higher expected influence in the network mode were considered to be more important. Bridge expected influence was calculated to identify bridge symptoms using the bridge function via R package networktools (version 1.2.3) (Payton, 2020). Bridges having higher expected influence values reflected a greater risk of contagion from one community to other communities compared to bridges with lower expected influence values (Jones et al., 2021). To identify bridge symptoms, we used the 80th percentile of bridge expected influence values as a cutoff (Garabiles et al., 2019). To identify particular symptoms that were directly associated with QoL, the “flow” function in R package qgraph was used (Epskamp et al., 2012). Moreover, R package mgm (version 1.2-12) was used to compute the predictability of each node, an index that reflects controllability of the network model (Haslbeck and Waldorp, 2020). Predictability values represented interconnectedness or the extent to which a node was associated with its neighboring nodes and was expressed as the area in the rings around each node in the layout of the network.
To assess the accuracy and stability of the observed network model, R package bootnet (version 1.4.3) was used (Epskamp et al., 2018) based on 1000 bootstraps performed for each node. The centrality indexes of expected influence and bridge expected influence were assessed using correlation stability (CS)-coefficients; values greater than 0.25 indicated moderate stability while values greater than 0.5 indicating strong stability.
2.3.3. Network comparison
Considering gender differences in depression and several anxiety disorders (Hou et al., 2020), network characteristic differences between participating men and women were examined. Global connectivity and local connectivity were assessed using a Network Comparison Test (NCT) between the two within gender models, using R package NetworkComparisonTest (version 2.2.1) (van Borkulo et al., 2017) with 1000 permutations.
3. Results
A total of 975 Macau residents (634 women, 341 men) was included in this study. Participants had a mean age of 29.91 years (standard deviation (SD = 2.0 years)). Regarding other demographics, 765 (78.5%) received higher education (i.e., undergraduate/college or above), 578 were currently employed (59.3%), and 566 (58.1%) were unmarried. Prevalences of depressive (PHQ-9 ≥ 5), anxiety (GAD-7 ≥ 5) and insomnia symptoms (ISI ≥ 8) were 38.5% (95% confidence interval (CI): 35.5%–41.5%), 28.8% (95%CI: 26.0%–31.7%), and 27.6% (95% CI: 24.8%–30.4%), respectively.
3.1. Network structure
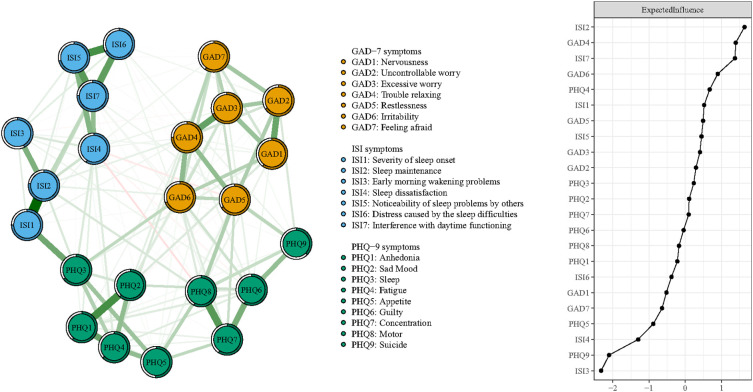
Networks of depressive, anxiety and insomnia symptoms are shown on the left panel of Fig. 1 . Regarding basic characteristics of the final networks, first, 142 of the 253 possible edges (56.1%) were not zero and reflected considerable interconnectedness between symptoms. Second, the top ten strongest edges observed in the model were distributed within respective communities of particular mental health problems (i.e., two edges in the depression community, three edges in the anxiety community, and five edges in the insomnia community).
Fig. 1.
Network structure of insomnia, anxiety, and depressive symptoms in adult residents of Macau during the later stage of the COVID-19 pandemic.
The edge between ISI1 “Severity of sleep onset” (i.e., difficulty falling asleep) and ISI2 “Sleep maintenance” was strongest, followed by edges PHQ1-PHQ2 (Anhedonia- Sad Mood), ISI5-ISI6 (Noticeability of sleep problems by others-Distress caused by sleep difficulties), ISI5-ISI7 (Noticeability of sleep problems by others-Interference with daytime functioning), GAD3-GAD4 (Excessive worry-Trouble relaxing), PHQ1-PHQ4 (Anhedonia-Fatigue), GAD1-GAD2 (Nervousness-Uncontrollable worry), ISI2-ISI3 (Sleep maintenance-Early morning wakening problems), ISI4-ISI5 (Sleep dissatisfaction-Noticeability of sleep problems by others), and GAD4-GAD6 (Trouble relaxing-Irritability) (Fig. 1). Moreover, node predictability values ranged from 37.5% to 77.1% with an average of 62.8%, indicating that, on average, 62.8% of the variance in nodes from the network could be explained by their neighboring nodes (Fig. 1, Table 1 ). Insomnia symptoms, ISI2 “Sleep maintenance” and ISI7 “Interference with daytime functioning”, had the highest predictability in the model, while the depressive symptom, PHQ9 “Suicide ideation”, had the lowest predictability.
Table 1.
Descriptive statistics of measurement items.
| Item abbreviation | Item content | Item mean (SD) | Expected influencea | Predictability |
|---|---|---|---|---|
| ISI1 | Severity of sleep onset | 0.58 (0.86) | 1.027 | 0.748 |
| ISI2 | Sleep maintenance | 0.52 (0.83) | 1.212 | 0.771 |
| ISI3 | Early morning wakening problems | 0.66 (0.92) 662.37 | 0.555 | 0.430 |
| ISI4 | Sleep dissatisfaction | 1.37 (0.94) | 0.724 | 0.586 |
| ISI5 | Noticeability of sleep problems by others | 0.86 (0.97) | 1.015 | 0.711 |
| ISI6 | Distress caused by sleep difficulties | 0.63 (0.87) | 0.877 | 0.673 |
| ISI7 | Interference with daytime functioning | 0.65 (0.88) | 1.168 | 0.755 |
| PHQ1 | Anhedonia | 0.68 (0.76) | 0.904 | 0.600 |
| PHQ2 | Sad Mood | 0.59 (0.70) | 0.958 | 0.615 |
| PHQ3 | Sleep problems | 0.58 (0.79) | 0.979 | 0.650 |
| PHQ4 | Fatigue | 0.75 (0.83) | 1.052 | 0.630 |
| PHQ5 | Appetite | 0.48 (0.73) | 0.794 | 0.508 |
| PHQ6 | Guilt | 0.39 (0.74) | 0.932 | 0.566 |
| PHQ7 | Concentration | 0.38 (0.69) | 0.956 | 0.593 |
| PHQ8 | Motor problems | 0.27 (0.57) | 0.912 | 0.579 |
| PHQ9 | Suicide ideation | 0.15 (0.49) | 0.591 | 0.375 |
| GAD1 | Nervousness | 0.49 (0.66) | 0.854 | 0.611 |
| GAD2 | Uncontrollable worry | 0.37 (0.64) | 0.989 | 0.658 |
| GAD3 | Excessive worry | 0.52 (0.72) | 1.008 | 0.685 |
| GAD4 | Trouble relaxing | 0.50 (0.73) | 1.172 | 0.745 |
| GAD5 | Restlessness | 0.28 (0.57) | 1.022 | 0.661 |
| GAD6 | Irritability | 0.45 (0.70) | 1.089 | 0.693 |
| GAD7 | Feeling afraid | 0.43 (0.66) | 0.834 | 0.595 |
ISI: Insomnia Severity Index; PHQ-9: the 9-item Patient Health Questionnaire; GAD-7: 7-item Generalized Anxiety Disorder Scale; SD, standard deviation.
The values of expected influence were raw data generated from the network.
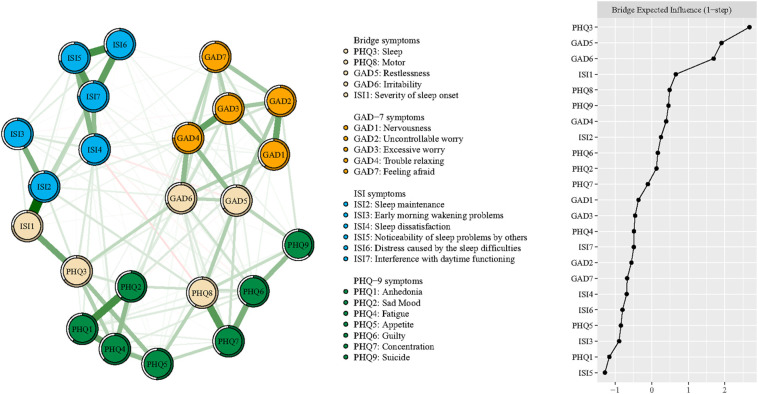
Expected influences within the entire network structure are shown on the right panel of Fig. 1 and in Table 1. ISI2 “Sleep maintenance” had the highest expected influence value, followed by GAD4 “Trouble relaxing”, ISI7 “Interference with daytime functioning”, GAD6 “Irritability”, and PHQ4 “Fatigue”, suggesting that these individual symptoms were the most influential within the entire symptom network model in terms of variance explained. In contrast, other symptoms such as ISI3 “Early morning wakening problems” and PHQ9 “Suicide ideation” had a marginal impact within the network. Regarding bridge symptoms, PHQ3 “Sleep problems”, GAD5 “Restlessness”, GAD6 “Irritability”, ISI1 “Severity of sleep onset”, and PHQ8 “Motor problems” had the highest bridge expected influence values (Fig. 2 ).
Fig. 2.
Network structure of insomnia, anxiety, and depressive symptoms showing bridge symptoms in Macau adult residents during the later stage of the COVID-19 pandemic.
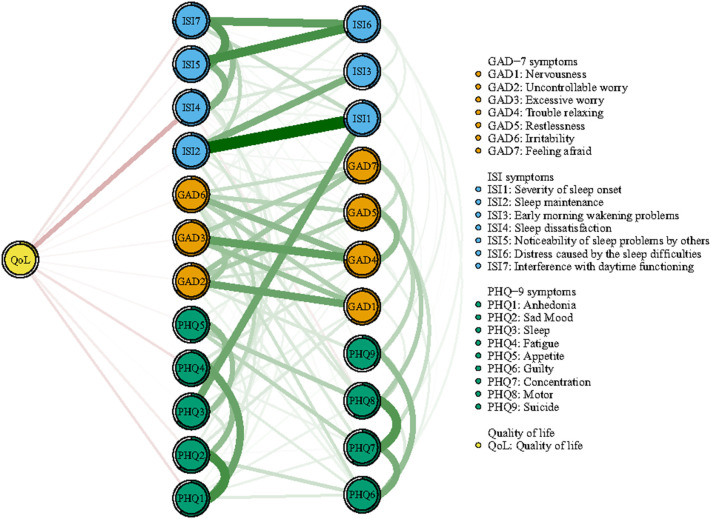
Fig. 3 depicts the flow diagram illustrating connections of “QoL” with depressive, anxiety, and insomnia symptoms in the network. The 12 individual symptoms located in the middle of the figure are directly related to QoL and the rest are indirectly related to QoL. Symptoms with the strongest direct relations to QoL included ISI4 “Sleep dissatisfaction”, PHQ1 “Anhedonia”, PHQ4 “Fatigue”, and ISI7 “Interference with daytime functioning”.
Fig. 3.
Flow network of quality of life.
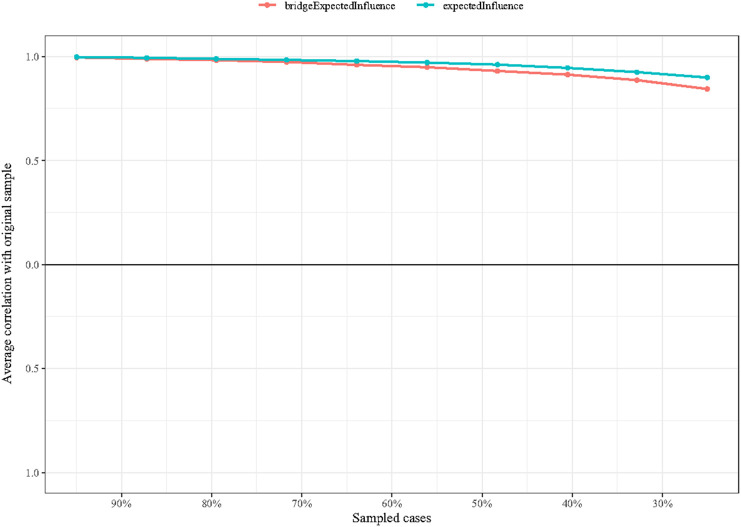
3.2. Network stability
As shown in Fig. 4, both expected influence and bridge expected influence values indicated an excellent level of stability (both CS-coefficients equaled 0.75), suggesting that 75% of participants could be dropped from analyses without significantly changing the network structure. The bootstrapped stability test for expected influence also indicated the central symptoms were significantly different from the other nodes (Fig. S1).
Fig. 4.
The stability of centrality and bridge centrality indices using case-dropping bootstrap.
3.3. Network comparisons of women versus men
The network structures generated from the two genders are shown in Fig. S2. Comparisons of networks generated for women versus men did not find significant differences in network global strength (Women: 10.903 vs Men: 10.941; S = 0.038, p = 0.841), or the network structure-distribution of edge weights (M = 0.151, p = 0.906) (Fig. S3).
4. Discussion
This was the first study to document the network structure of insomnia, depression and anxiety symptoms among Macau residents during the COVID-19 pandemic. In this network, we found that the strongest edges were all within particular mental disorder communities rather than between different disorders, consistent with the findings of previous network research (Beard et al., 2016; Garabiles et al., 2019; Groen et al., 2020). The strongest edge in the whole network was between insomnia symptoms ISI1 “Severity of sleep onset” and ISI2 “Sleep maintenance”. This diverges from results of a related population study from the Netherlands exploring relations between insomnia symptoms and personality traits wherein the edge ISI2-ISI3 (Sleep maintenance - Early morning wakening problems) was strongest (Dekker et al., 2017). This discrepancy may be due, in part, to differences in the focus of these surveys. Specifically, our research was conducted in the presence of the COVID-19 pandemic which has contributed to more widespread difficulties falling asleep and maintaining sleep due infection fears (Ahorsu et al., 2020) and anxiety emanating from worries about personal economic losses (Huang et al., 2020). Consequently, risks and consequences of COVID-19 may have contributed to the comparatively strong relationship between ISI1 “Severity of sleep onset” and ISI2 “Sleep maintenance” relative to other symptoms in the network. The second strongest edge to emerge in our sample was between PHQ1 “Anhedonia” and PHQ2 “Sad Mood”, a novel link that has not been documented previously. Once again, this association may be unique to this specific sample in the context of the COVID-19 pandemic, though consequent pandemic-based studies are needed to verify or refute this hypothesis. Other strong edges in present network were often between insomnia symptoms, indicating that sleep problems in Macau residents during the COVID-19 pandemic are prominent and should be assessed as a matter of course in local referrals for mental health services.
Expected influence centrality of nodes performed well in identifying specific symptoms that contributed most strongly to the overall psychopathology symptom network in this sample. Specifically, an insomnia symptom, ISI2 “Sleep maintenance”, had the highest centrality value, indicating that this symptom plays the most critical role in maintaining the entire symptom network. Consequently, it can be hypothesized that interventions targeting improvements in maintenaning adequate amounts and quality of sleep have the potential to relieve other symptoms in the anxiety-depression-insomnia symptom network (McElroy and Patalay, 2019). Although the particular sleep symptom differed from that of Dekker et al. (2017) who found item ISI4 “Sleep dissatisfaction” was the most influential symptom in their insomnia-personality network model, it is notable that specific insomnia symptoms were most critical across different network models. According to the DSM-V (American Psychiatric Association, 2013), impaired sleep maintenance is a consequence of multiple or prolonged nocturnal awakenings. Previous reviews have concluded that cognitive behavior therapy for insomnia (CBT-I) is effective in targeting and reversing behavioral and cognitive processes that perpetuate insomnia as well as related symptoms such as worry and fatigue in adult samples (e.g., van der Zweerde et al., 2019), including older adults who often have medical comorbidities (Lovato et al., 2016; Lovato et al., 2014; Mitchell et al., 2019). Certain psychosocial interventions such as CBT-I are viewed as the first line of intervention due to their low risk of adverse effects and effectiveness (van der Zweerde et al., 2019). In addition, pharmacologic strategies including the use of sedative-hypnotic drugs are an alternative treatment for sleep disturbances that may be useful over relatively brief periods. Agents such as benzodiazepines (e.g., Estazolam, Temazepam) (Gooneratne and Vitiello, 2014; Qaseem et al., 2016; Schroeck et al., 2016) and nonbenzodiazepines (e.g., eszopiclone) (Smagula et al., 2016) are effective in improving sleep-maintenance insomnia in this context.
Another insomnia symptom, ISI7 “Interference with daytime functioning”, was identified as a central symptom, in part, because it is a consequence of sleep disruptions related to insomnia. Other central symptoms, GAD4 “Trouble relaxing”, GAD6 “Irritability”, and PHQ4 “Fatigue”, were also identified in line with previous research conducted on Macau Filipino domestic workers and Chinese nursing students (Garabiles et al., 2019; Ren et al., 2021). Interventions targeting these anxiety and depressive symptoms may be effective in reducing the severity of related symptoms in the entire network (Cramer et al., 2010a). All identified central symptoms had high predictability values that accounted for 62.8% of the variance in average predictability for all nodes in the network. That is, much of the variance for nodes in the network could be explained by overlaps with neighboring nodes. As such, symptoms examined in this study were highly salient to participating Macau residents' overall psychiatric status and warrant inclusion within assessment protocols of those seeking mental health care.
Within the derived insomnia-anxiety-depressive symptom network, the top bridge symptom based on node bridge expected influence was the depressive symptom, PHQ3 “Sleep problems”. This symptom refers to trouble falling or staying asleep, or difficulties with sleeping too much (Kroenke et al., 2001). Notably, this symptom was strongly connected with another bridge symptom, ISI1 “Severity of sleep onset”, indicating that aside from sleep-maintenance insomnia, sleep-onset insomnia may be another symptom critical to maintaining the entire network and an important target for intervention. Certain medications (e.g., Triazolam, Zolpidem, Zaleplon, Ramelteon) have been found to be effective in improving sleep onset (Zheng et al., 2020). Moreover, meta-analyses have found that psychological interventions also improve sleep onset latency and total sleep time (Cheung et al., 2019; Wu et al., 2015). Other bridge symptoms, GAD5 “Restlessness”, GAD6 “Irritability”, and PHQ8 “Motor problems” in this network have also been identified in previous network studies (Ren et al., 2021; Wang et al., 2020). In general, these findings suggest that bridge symptoms in different mental disorder communities contribute to psychiatric comorbidity and warrant attention as targets in treatment studies designed to identify particular symptoms most critical for decreasing risk of contagion between psychiatric syndromes within network models (Jones et al., 2021).
Epidemiological studies have reported that the COVID-19 pandemic has negative effects on individuals' mental health as well as their QoL (Xiong et al., 2020). Within the current network model, we explored which symptoms most directly associated with QoL. The insomnia symptom, “Sleep dissatisfaction”, emerged as the most prominent correlate. The influence of insomnia on residents' QoL is consistent with the prominence of insomnia symptoms within the entire symptom network (i.e., most critical central and bridge symptoms emerged from the insomnia symptom community). Though the prevalence of insomnia (27.6%) in Macau residents was lower than rates of anxiety (28.8%) and depressive symptoms (38.5%), the essential role of insomnia symptoms on overall mental health status and QoL cannot be ignored based on NA results. Once again, analyses of bridge symptoms underscore how interventions specifically targeting insomnia symptoms within this population may have far-reaching implications for alleviating residents' overall levels of insomnia, anxiety, and depression in tandem with improving their QoL.
To the best of our knowledge, this was the first study to explore insomnia-anxiety-depression symptom networks (1) in the context of the COVID-19 pandemic and (2) among residents of Macau, China. Aside from its novel foci, a strength of this study was the reliability of its main results within the entire sample as well as within each gender. Strengths aside, several limitations should be acknowledged. First, due to the cross-sectional study design, causal links related to symptom changes over time could not be assessed. Second, due to restrictions related to managing the pandemic, symptoms were assessed solely on the basis of self-report measures that can be susceptible to response biases such as those related to recall and social desirability. Third, on average, participants were young adults (mean age = 29.91 years) so findings may not generalize equally well to all age groups in Macau. Finally, although the present findings provide potential insights related to psychiatric symptoms that are most prominent within a particular population during an era-defining pandemic, findings may not generalize to other populations or non-pandemic living conditions.
In conclusion, symptoms related to insomnia and sleep disturbances were identified as those most critical within an anxiety-depression-insomnia network model in terms of node and bridge centrality as well as their associations with QoL among Macau residents assessed during the COVID-19 pandemic. As such, specific insomnia symptoms warrant attention both within assessment protocols of those seeking help for psychiatric disturbances and as potential targets for interventions designed to alleviate or prevent common, frequently co-occurring psychiatric syndromes and improve QoL among Macau residents living through the pandemic.
The following are the supplementary data related to this article.
Bootstrapped stability test for ‘expected influence’.
Note: Bootstrapped difference tests between expected influence of insomnia, anxiety, and depressive symptoms. Gray boxes indicate nodes that do not significantly differ from one-another. Black boxes represent nodes that differ significantly from one another (α = 0.05). White boxes show the values of expected influence.
Network comparison of insomnia, anxiety, depressive symptoms between genders.
Comparison of network properties between females and males.
Note: There were no significant differences in network global strength (Female: 10.903 vs Male: 10.941; S = 0.038, p = 0.841), network structure-distribution of edge weights (M = 0.151, p = 0.906).
CRediT authorship contribution statement
Study Design: Yu-Tao Xiang, Si-Man Lei, Grace K.I. Lok, Ines H.I. Chow.
Collection, analyses and interpretation of data: Wei Bai, Yan-Jie Zhao, Hong Cai,Sha Sha, Ling Zhang.
Drafting of the manuscript: Wei Bai, Teris Cheung, Zhaohui Su, Yu-Tao Xiang.
Critical revision of the manuscript: Todd Jackson.
Approval of the final version for publication: All the authors.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgments
Acknowledgements
None.
Role of the funding source
The study was supported by the National Science and Technology Major Project for Investigational New Drug (2018ZX09201-014), the Beijing Municipal Science and Technology Commission (No. Z181100001518005), and the University of Macau (MYRG2019-00066-FHS).
References
- Ahorsu D.K., Lin C.Y., Pakpour A.H. The association between health status and insomnia, mental health, and preventive behaviors: the mediating role of fear of COVID-19. Gerontol. Geriatr. Med. 2020;6 doi: 10.1177/2333721420966081. 2333721420966081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . American Psychiatric Publishing; Arlington: 2013. Diagnostic and Statistical Manual of Mental Disorders : DSM-5. [Google Scholar]
- Bai C.J., Ji D.H., Chen L.X., Li L., Wang C.X. Reliability and validity of insomnia severity index in clinical insomnia patients (in Chinese) Chin. J. Pract. Nurs. 2018;34:2182–2186. [Google Scholar]
- Bamidele J. 2019. Macau Raises 2019 Gaming Tax Budget by 12.9% to Almost mop $100 Billion, December. [Google Scholar]
- Beard C., Millner A.J., Forgeard M.J., Fried E.I., Hsu K.J., Treadway M.T., Leonard C.V., Kertz S.J., Björgvinsson T. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol. Med. 2016;46:3359–3369. doi: 10.1017/S0033291716002300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M.M., Sheng L., Shan Q.U. Diagnostic test of screening depressive disorders in general hospital with the patient health questionnaire (in Chinese) Chin. Ment. Health J. 2015;29:241–245. [Google Scholar]
- Chen W.-C., Chen S.-J., Zhong B.-L. Sense of alienation and its associations with depressive symptoms and poor sleep quality in older adults who experienced the lockdown in Wuhan, China, during the COVID-19 pandemic. J. Geriatr. Psychiatry Neurol. 2022;35:215–222. doi: 10.1177/08919887221078564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung J.M.Y., Jarrin D.C., Ballot O., Bharwani A.A., Morin C.M. A systematic review of cognitive behavioral therapy for insomnia implemented in primary care and community settings. Sleep Med. Rev. 2019;44:23–36. doi: 10.1016/j.smrv.2018.11.001. [DOI] [PubMed] [Google Scholar]
- Cramer A.O., Waldorp L.J., van der Maas H.L., Borsboom D. Comorbidity: a network perspective. Behav. Brain Sci. 2010;33:137–150. doi: 10.1017/S0140525X09991567. [DOI] [PubMed] [Google Scholar]
- Cramer A.O.J., Waldorp L.J., van der Maas H.L.J., Borsboom D. Complex realities require complex theories: refining and extending the network approach to mental disorders. Behav. Brain Sci. 2010;33:178–193. [Google Scholar]
- Dekker K., Blanken T.F., Van Someren E.J. Insomnia and personality-a network approach. Brain Sci. 2017:7. doi: 10.3390/brainsci7030028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Blasi M., Gullo S., Mancinelli E., Freda M.F., Esposito G., Gelo O.C.G., Lagetto G., Giordano C., Mazzeschi C., Pazzagli C., Salcuni S., Lo Coco G. Psychological distress associated with the COVID-19 lockdown: a two-wave network analysis. J. Affect. Disord. 2021;284:18–26. doi: 10.1016/j.jad.2021.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elizabeth A., Adam I., Dayour F., Badu Baiden F. Perceived impacts of COVID-19 on risk perceptions, emotions, and travel intentions: evidence from Macau higher educational institutions. Tour. Recreat. Res. 2021:1–17. [Google Scholar]
- Epifanio M.S., Andrei F., Mancini G., Agostini F., Piombo M.A., Spicuzza V., Riolo M., Lavanco G., Trombini E., La Grutta S. The impact of COVID-19 pandemic and lockdown measures on quality of life among italian general population. J. Clin. Med. 2021;10 doi: 10.3390/jcm10020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Cramer A.O.J., Waldorp L.J., Schmittmann V.D., Borsboom D. Qgraph: network visualizations of relationships in psychometric data. J. Stat. Softw. 2012;1(4):2012. [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Methods. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang J.Q., Hao Y.T., Li C.X. Reliability and validity for chinese version of WHO quality of life scale (in Chinese) Chin. Ment. Health J. 1999;13:203–209. [Google Scholar]
- Ferreira L.N., Pereira L.N., da Fé Brás M., Ilchuk K. Quality of life under the COVID-19 quarantine. Qual. Life Res. 2021;30:1389–1405. doi: 10.1007/s11136-020-02724-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garabiles M.R., Lao C.K., Xiong Y., Hall B.J. Exploring comorbidity between anxiety and depression among migrant filipino domestic workers: a network approach. J. Affect. Disord. 2019;250:85–93. doi: 10.1016/j.jad.2019.02.062. [DOI] [PubMed] [Google Scholar]
- Gooneratne N.S., Vitiello M.V. Sleep in older adults: normative changes, sleep disorders, and treatment options. Clin. Geriatr. Med. 2014;30:591–627. doi: 10.1016/j.cger.2014.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groen R.N., Ryan O., Wigman J.T.W., Riese H., Penninx B., Giltay E.J., Wichers M., Hartman C.A. Comorbidity between depression and anxiety: assessing the role of bridge mental states in dynamic psychological networks. BMC Med. 2020;18:308. doi: 10.1186/s12916-020-01738-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Y., Zhu Y., Xu F., Xi J., Xu G. Factors associated with mental health outcomes among patients with COVID-19 treated in the fangcang shelter hospital in China. Asia Pac. Psychiatry. 2021;13 doi: 10.1111/appy.12443. [DOI] [PubMed] [Google Scholar]
- Han L., Fang H., Ming Y., John L., Larry W. High-dimensional semiparametric gaussian copula graphical models. Ann. Stat. 2012;40:2293–2326. [Google Scholar]
- Haslbeck J.M.B., Waldorp L.J. Mgm: estimating time-varying mixed graphical models in high-dimensional data. J. Stat. Softw. 2020;1 [Google Scholar]
- He X.Y., Li C.B., Qian J., Cui H.S., Wu W.Y. Study on the reliability and validity of generalized anxiety scale in general hospitals (in Chinese) Shanghai Arch. Psychiatry. 2010;22:200–203. [Google Scholar]
- Hou F., Bi F., Jiao R., Luo D., Song K. Gender differences of depression and anxiety among social media users during the COVID-19 outbreak in China:a cross-sectional study. BMC Public Health. 2020;20:1648. doi: 10.1186/s12889-020-09738-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Wang Y., Zeng L., Yang J., Song X., Rao W., Li H., Ning Y., He H., Li T., Wu K., Chen F., Wu F., Zhang X. Prevalence and correlation of anxiety, insomnia and somatic symptoms in a chinese population during the COVID-19 epidemic. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.568329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones P.J., Ma R., McNally R.J. Bridge centrality: a network approach to understanding comorbidity. Multivar. Behav. Res. 2021;56:353–367. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- Kılınçel Ş., Kılınçel O., Muratdağı G., Aydın A., Usta M.B. Factors affecting the anxiety levels of adolescents in home-quarantine during COVID-19 pandemic in Turkey. Asia Pac. Psychiatry. 2021;13 doi: 10.1111/appy.12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loi K.I., Lei W.S., Lourenço F. Understanding the reactions of government and gaming concessionaires on COVID-19 through the neo-institutional theory - the case of Macao. Int. J. Hosp. Manag. 2021;94 doi: 10.1016/j.ijhm.2020.102755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovato N., Lack L., Wright H., Kennaway D.J. Evaluation of a brief treatment program of cognitive behavior therapy for insomnia in older adults. Sleep. 2014;37:117–126. doi: 10.5665/sleep.3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovato N., Lack L., Kennaway D.J. Comparing and contrasting therapeutic effects of cognitive-behavior therapy for older adults suffering from insomnia with short and long objective sleep duration. Sleep Med. 2016;22:4–12. doi: 10.1016/j.sleep.2016.04.001. [DOI] [PubMed] [Google Scholar]
- Luo H., Lie Y., Prinzen F.W. Surveillance of COVID-19 in the general population using an online questionnaire: report from 18,161 respondents in China. JMIR Public Health Surveill. 2020;6 doi: 10.2196/18576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy E., Patalay P. In search of disorders: internalizing symptom networks in a large clinical sample. J. Child Psychol. Psychiatry Allied Discip. 2019;60:897–906. doi: 10.1111/jcpp.13044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell L.J., Bisdounis L., Ballesio A., Omlin X., Kyle S.D. The impact of cognitive behavioural therapy for insomnia on objective sleep parameters: a meta-analysis and systematic review. Sleep Med. Rev. 2019;47:90–102. doi: 10.1016/j.smrv.2019.06.002. [DOI] [PubMed] [Google Scholar]
- Montazeri F., de Bildt A., Dekker V., Anderson G.M. Network analysis of behaviors in the depression and autism realms: inter-relationships and clinical implications. J. Autism Dev. Disord. 2020;50:1580–1595. doi: 10.1007/s10803-019-03914-4. [DOI] [PubMed] [Google Scholar]
- Morin C.M. Guilford Press; New York: 1993. Insomnia, Psychological Assessment and Management. [Google Scholar]
- National Institute of Mental Health . 2021. Research Domain Criteria (RDoC) [Google Scholar]
- Payton J. 2020. Tools for Identifying Important Nodes in Networks. [Google Scholar]
- Qaseem A., Kansagara D., Forciea M.A., Cooke M., Denberg T.D. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 2016;165:125–133. doi: 10.7326/M15-2175. [DOI] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A Language and Environment for Statistical Computing. [Google Scholar]
- Ren L., Wang Y., Wu L., Wei Z., Cui L.B., Wei X., Hu X., Peng J., Jin Y., Li F., Yang Q., Liu X. Network structure of depression and anxiety symptoms in chinese female nursing students. BMC Psychiatry. 2021;21:279. doi: 10.1186/s12888-021-03276-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinaugh D.J., Millner A.J., McNally R.J. Identifying highly influential nodes in the complicated grief network. J. Abnorm. Psychol. 2016;125:747–757. doi: 10.1037/abn0000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeck J.L., Ford J., Conway E.L., Kurtzhalts K.E., Gee M.E., Vollmer K.A., Mergenhagen K.A. Review of safety and efficacy of sleep medicines in older adults. Clin. Ther. 2016;38:2340–2372. doi: 10.1016/j.clinthera.2016.09.010. [DOI] [PubMed] [Google Scholar]
- Smagula S.F., Stone K.L., Fabio A., Cauley J.A. Risk factors for sleep disturbances in older adults: evidence from prospective studies. Sleep Med. Rev. 2016;25:21–30. doi: 10.1016/j.smrv.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- The WHOQOL Group Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol. Med. 1998;28:551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- van Borkulo C.D., Boschloo L., Kossakowski J.J., Tio P., Schoevers R.A., Borsboom D., Waldorp L.J. 2017. Comparing Network Structures on Three Aspects: A Permutation Test. [DOI] [PubMed] [Google Scholar]
- van der Zweerde T., Bisdounis L., Kyle S.D., Lancee J., van Straten A. Cognitive behavioral therapy for insomnia: a meta-analysis of long-term effects in controlled studies. Sleep Med. Rev. 2019;48 doi: 10.1016/j.smrv.2019.08.002. [DOI] [PubMed] [Google Scholar]
- Wang Y., Hu Z., Feng Y., Wilson A., Chen R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol. Psychiatry. 2020;25:3140–3149. doi: 10.1038/s41380-020-00881-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Shi L., Que J., Lu Q., Liu L., Lu Z., Xu Y., Liu J., Sun Y., Meng S., Yuan K., Ran M., Lu L., Bao Y., Shi J. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol. Psychiatry. 2021:1–10. doi: 10.1038/s41380-021-01019-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J.Q., Appleman E.R., Salazar R.D., Ong J.C. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: a meta-analysis. JAMA Intern. Med. 2015;175:1461–1472. doi: 10.1001/jamainternmed.2015.3006. [DOI] [PubMed] [Google Scholar]
- Xia P., Li N., Hau K.T., Liu C., Lu Y. Quality of life of chinese urban community residents: a psychometric study of the mainland chinese version of the WHOQOL-BREF. BMC Med. Res. Methodol. 2012;12:37. doi: 10.1186/1471-2288-12-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng X., He Y., Yin F., Liu H., Li Y., Zheng Q., Li L. Pharmacological interventions for the treatment of insomnia: quantitative comparison of drug efficacy. Sleep Med. 2020;72:41–49. doi: 10.1016/j.sleep.2020.03.022. [DOI] [PubMed] [Google Scholar]
- Zhou J., Liu L., Xue P., Yang X., Tang X. Mental health response to the COVID-19 outbreak in China. Am. J. Psychiatry. 2020;177:574–575. doi: 10.1176/appi.ajp.2020.20030304. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Bootstrapped stability test for ‘expected influence’.
Note: Bootstrapped difference tests between expected influence of insomnia, anxiety, and depressive symptoms. Gray boxes indicate nodes that do not significantly differ from one-another. Black boxes represent nodes that differ significantly from one another (α = 0.05). White boxes show the values of expected influence.
Network comparison of insomnia, anxiety, depressive symptoms between genders.
Comparison of network properties between females and males.
Note: There were no significant differences in network global strength (Female: 10.903 vs Male: 10.941; S = 0.038, p = 0.841), network structure-distribution of edge weights (M = 0.151, p = 0.906).