Abstract
Purpose
We examined whether financial burdens occurring during the COVID-19 pandemic impacted healthcare utilization among survivors of adolescent and young adult cancers.
Methods
We surveyed survivors enrolled in a patient navigation program to obtain self-reports of delayed/skipped cancer care or other care, changes to medication obtainment, and changes to medication use since the COVID-19 pandemic began. Reported financial burdens were defined as financial toxicity in the past 4 weeks (COmprehensive Score for financial Toxicity [COST] ≤ median 21) and material hardships (range = 4–11) since March 2020. Adjusted logistic regression models calculated associations and effect modification by gender.
Results
Survivors (n = 341) were mostly female (61.3%) and non-Hispanic White (83.3%). Nearly 20% delayed/skipped cancer care, 35.2% delayed/skipped other care, 19.1% changed medication obtainment, and 12.6% changed medication use. Greater material hardships were associated with delayed/skipped cancer care (odds ratio (OR) = 3.13, 95% CI = 1.44–6.81) and other care (OR = 2.17, 95% CI = 1.18–3.98), and changed medication obtainment (OR = 2.72, 95% CI = 1.43–5.18) or use (OR = 4.49, 95% CI = 2.05–9.80). Financial toxicity was associated with delayed/skipped other care (OR = 2.53, 95% CI = 1.31–4.89) and changed medication obtainment (OR = 1.96, 95% CI = 1.01–3.83) and medication use (OR = 3.73, 95% CI = 1.59–8.73). The association of material hardships and any changes in healthcare utilization was greater among female compared to male survivors.
Conclusion
Financial burdens experienced during the pandemic impeded survivors’ ability to utilize necessary healthcare, with worse impacts among female survivors.
Implications for Cancer Survivors
Delayed or skipped healthcare may lead to an increased cancer mortality or severity of therapy-related conditions. Providing resources that enable survivors experiencing financial burdens to continue critical cancer and preventive care during the COVID-19 pandemic is a priority.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11764-022-01214-y.
Keywords: COVID-19, Healthcare utilization, AYA cancers, Survivorship, Financial toxicity
Introduction
The COVID-19 pandemic has taken the lives of over 1,000,000 Americans and strained the capacity of healthcare professionals and systems to care for complex patients [1–3]. Healthcare systems have reduced patient loads to limit in-person contact and preserve resources for COVID-19 care, but these changes have limited capacity for cancer care [4, 5]. Shifting to telehealth has been challenging for cancer patients whose care may require laboratory tests or hands-on examination [4, 5]. While some patients are hesitant to start or continue cancer care during the pandemic, expedient cancer care is still a priority. Even a month-long delay in treatment can increase cancer mortality by between 6 and 23% [6, 7]. Survivors of adolescent and young adult cancers, who were diagnosed between the ages 15 and 39 years (AYA survivors), already had financial and insurance-related barriers to utilizing healthcare before the pandemic [8]. COVID-19-related health care challenges may cause additional barriers for AYA survivors, affecting their treatment, management of late effects, and screening for second cancers [9, 10]. Pandemic-related delays in cancer care have been reported in 40% to 60% of surveyed AYA survivors [11].
Before the pandemic, the financial burden of cancer therapy, employment and education disruption, and inadequate access to health insurance impeded healthcare use among AYA survivors [8]. Distress from financial problems due to cancer therapy, defined as financial toxicity, can continue for years after therapy ends [12]. To cope with financial toxicity and out-of-pocket costs, AYA survivors may engage in cost-coping behaviors such as skipping treatments that likely have adverse impacts on their survival [13]. An estimated 71% of AYA survivors have engaged in at least one cost-coping behavior, and those with the greatest financial toxicity had the highest risk for these behaviors [13]. While health insurance can offset some costs, cancer-related unemployment can create gaps in health insurance coverage and can impede survivors’ ability to build savings [14]. The pandemic appears to have worsened the prevalence of these financial, health insurance, and employment-related barriers to healthcare in AYA survivors [13, 15].
In addition, historic disparities have existed in healthcare utilization according to sociodemographic characteristics like gender, sexual orientation, insurance coverage, and cancer type, that can disproportionately affect AYA survivors [16–19]. These disparities may have widened during the COVID-19 pandemic, but few studies involving young cancer survivors have addressed this topic. In the midst of the COVID-19 pandemic, we surveyed AYA survivors through the Huntsman-Intermountain Adolescent and Young Adult (HIAYA) Cancer Care Program about their healthcare utilization, financial burdens, and changes in employment or school that they experienced during the 2020 calendar year. This exploratory study identifies whether these changes were correlated with survivors’ self-reported healthcare utilization. We captured four dimensions of healthcare utilization: delayed or skipped cancer care, delayed or skipped other care, adaptive behaviors to obtain lower cost medications, and changes in medication use.
Methods
Study design and population
The Utah-based HIAYA program provides AYA cancer survivors with healthcare navigation, access to research studies, and other support. HIAYA serves Utah patients and patients from the neighboring states that utilize Utah’s healthcare network, and patients of community oncology clinics were treated at Intermountain Healthcare. The University of Utah IRB approved this study.
Eligible participants who were enrolled in HIAYA were ≥ 18 years at the time of survey and diagnosed with cancer between 15 and 39 years, and who had an email address in the HIAYA database (n = 675) (Supplemental Fig. 1). A one-time survey was emailed to eligible persons in October 2020, and data collection continued until January 2021. Follow-up emails, texts, and mail notifications occurred between October 2020 and January 2021. Participants received a $20 gift card.
Survey design
We referred to March 2020 as the beginning of the pandemic in the survey. Participants reported demographic items such as age at survey, race, ethnicity, sexual orientation, and gender identity. Diagnosis age was computed from self-reported dates of birth and first cancer diagnosis from medical records. Survey and diagnosis age were grouped by 5-year increments. Race and ethnicity were combined together into White non-Hispanic, Hispanic, and non-Hispanic racial minority. LGBTQ + identity was determined using self-reported sexual orientation and gender identity. Years since diagnosis were computed using the survey date and cancer diagnosis date.
Receipt of cancer therapy was asked in the survey. Participants indicated yes/no if they received cancer-related therapy since March 2020. Participants reported if they specifically received chemotherapy, surgery, radiation, hormone therapy, immunotherapy, or other therapies related to cancer. We reviewed medical records to identify first cancer diagnosis and classified diagnoses by the AYA site recode/WHO 2008 definition [20].
Financial burden and changes in employment or schooling
We measured financial burdens as financial toxicity and material hardship. Financial toxicity in the past 4 weeks was measured using 11 items coded on a 5-point Likert scale from the “COmprehensive Score for financial Toxicity” (COST) [12]. As low scores indicated higher toxicity, we divided participants into “high” or “low” by COST ≤ 21 (median = 21) as done previously [21].
Material hardships that occurred since March 2020 were measured with 11 questions adapted from the Commonwealth tracking survey and other healthcare surveys [22, 23]. We asked participants if their material hardships originated from the COVID-19 pandemic or their cancer treatment and/or side effect costs (Supplemental Fig. 2). We summed the number of material hardships from either cancer or COVID-19 and defined groups as “high” (4–10) or “low” (0–3) by the median (n = 3). We also counted material hardships that were caused due to COVID-19 or cancer separately. These were grouped as “high” (2–9) or “low” (0–1) by the median (n = 1).
Participants reported their employment and/or school enrollment prior to March 2020. Open-ended and multiple-choice questions asked about changes in work hours, employment, or schooling since March 2020. We created four categories to reflect responses: increased hours, reduced hours, no change and unemployed/caregiver, no change and employed.
Healthcare utilization outcomes
Our outcomes were delayed/skipped cancer care, delayed/skipped other care, changes in medication obtainment, and changes in medication use. Participants reported any delayed/skipped care that was related to cancer and unrelated to cancer (other care) since March 2020 [24]. Participants also reported the types of care that were delayed/skipped and reasons for delaying/skipping care, including provider/facility delays or cancelations. The response options for types of care that were skipped/delayed were oncology, primary care, mental health, urgent care, emergency care, and other specialties as a free-response text answer.
Participants reported changes in medication obtainment or use because of the COVID-19 pandemic [22]. Changes to medication obtainment captured adaptive behaviors to find affordable medications, defined as asking physicians for less expensive medication, shopping for lowest priced pharmacies, replacing prescriptions with over-the-counter options, purchasing medication abroad, or obtaining medications through Veterans Affairs. Changes to medication use were defined as taking medications prescribed for others, not filling prescriptions, filling only part of prescriptions, or taking less than the prescribed amount.
Statistical analysis
We described the sample by demographics and outcomes. Chi-squared tests compared differences among the outcomes by therapy, survey age, and cancer diagnosis. Melanoma was chosen as the referent group as it can often be treated with less therapy than the other tumor types included in the survey. Logistic regression models were conducted to examine the associations between the outcomes and demographics separately to avoid collinearity, while adjusting for survey age, race/ethnicity, and gender where appropriate. We also used logistic regression to compute the associations of financial burdens or employment/school changes with our outcomes separately, while adjusting for gender, race/ethnicity, survey age, marital status, and health insurance. Confounders were chosen by their impact on the odds ratio, theoretical merit, and maximization of c ≥ 0.7. For models of delayed/skipped care, we excluded persons with delayed/skipped care due to provider/facility preference (cancer care = 33; other care = 57).
Because of the pandemic’s disproportionate financial impact on women [25], we examined the effect modification of the association of material hardship and our outcomes by gender. To improve power, we aggregated all responses into a single outcome (any change in healthcare utilization) which excluded persons who only reported delayed/skipped care due to provider delays/cancelations (n = 56). We also aggregated the outcome medication obtainment and use (medication obtainment/use) and delayed/skipped cancer and other care (delayed/skipped cancer or other care). Stratified logistic regression models provided the gender-specific odds ratios and confidence intervals while adjusting for survey age, race/ethnicity, education, and health insurance. Separate models with interaction terms provided the p values for the comparison of gender-specific odds ratios. Odds ratios were significant if their 95% confidence intervals excluded the null and interactions were significant if the type 3 test p value < 0.05. We also examined the association between changes in employment and our outcomes stratified by gender and in separate models.
Results
We had 341 (50.5%) survivors who participated in the survey (Supplemental Fig. 1). Participants were largely female (61.3%), married/cohabiting (52.5%), non-Hispanic White (83.3%), 18–29 years old (50.7%), 0–2 years from diagnosis (60.7%), and health insured at the time of survey (79.2%; Table 1). Females composed 83.3% of divorced/widowed/separated persons, 65.9% of married/cohabiting persons, and 79.3% of LGBTQ + survivors. Carcinomas (30.2%) and leukemia/lymphoma (30.5%) were the most common diagnoses and 54.0% reported receiving cancer-related therapy since March 2020. Employment/school hours were reduced for 21.8% and increased for 19.7% of survivors. Only 1.2% lost health insurance and 4.1% enrolled in Medicaid since March 2020.
Table 1.
Characteristics of survivors of adolescent and young adult cancers surveyed from October 2020 to January 2021 (N = 314)
| n | % | ||
|---|---|---|---|
| Female | 209 | 61.3 | |
| Survey age (years) | 18–24 | 99 | 29.0 |
| 25–29 | 74 | 21.7 | |
| 30–34 | 76 | 22.3 | |
| 35–39 | 68 | 19.9 | |
| 40–55 | 24 | 7.0 | |
| Diagnosis age (years) | 15–19 | 51 | 15.0 |
| 20–24 | 97 | 28.5 | |
| 25–29 | 66 | 19.4 | |
| 30–34 | 61 | 17.9 | |
| 35–40 | 60 | 17.6 | |
| Race and ethnicity | Hispanic | 34 | 10.0 |
| Non-Hispanic racial minority | 23 | 6.7 | |
| White, non-Hispanic | 284 | 83.3 | |
| LGBTQ + | 29 | 8.5 | |
| Marital status | Divorced/widowed/separated | 24 | 7.0 |
| Married/cohabiting | 179 | 52.5 | |
| Single | 127 | 37.2 | |
| Education | ≤ High school | 42 | 12.3 |
| Some college | 146 | 42.8 | |
| College | 109 | 32.0 | |
| Graduate school | 43 | 12.6 | |
| Employment or schooling changes during COVID-19 pandemic | Increased hours | 67 | 19.7 |
| Reduced hours | 74 | 21.8 | |
| No change (unemployed/caregiver) | 80 | 23.5 | |
| No change (employed) | 119 | 35.0 | |
| Health insurance | Employer/military/individual | 270 | 79.2 |
| Public and private coverage | 19 | 5.6 | |
| Public | 33 | 9.7 | |
| Uninsured/unknown | 15 | 4.4 | |
| First diagnosis | CNS/other nervous system | 42 | 12.3 |
| Carcinoma | 103 | 30.2 | |
| Gonadal/related tumors | 30 | 8.8 | |
| Leukemia/lymphoma | 104 | 30.5 | |
| Sarcoma | 35 | 10.3 | |
| Melanoma | 20 | 5.9 | |
| Therapy since March 2020 | Yes | 184 | 54.0 |
| Years since diagnosis | 0–2 | 207 | 60.7 |
| 3–10 | 116 | 34.0 | |
| 11–25 | 12 | 3.5 |
Missing N’s: diagnosis age = 6, LGBTQ + = 16, martial status = 11, education = 1, employment = 1, health insurance = 4, first diagnosis = 7, therapy since March 2020 = 4, years since diagnosis = 6
employment includes school enrollment
Delayed/skipped cancer care (19.1%) was less common than delayed/skipped other care (35.2%) (Table 2). Provider/facility preference was responsible for delays/skips in 47.7% of cancer and 44.2% of other care. Oncology (13.8%) was the most commonly delayed/skipped type of cancer care. Primary care (2.1%) and mental health (2.6%) that were related to cancer were the least commonly delayed/skipped cancer care. For other care, primary care (23.8%) was most commonly delayed/skipped. Nearly 20% of survivors changed their medication obtainment and 12.6% changed their medication use. Financial burdens due to cancer (39.9%) or COVID-19 (54.8%) were the most common type of reported material hardship (due to any cause = 77.5%). Other common material hardships included taking money out of savings (due to any cause = 63.2%, COVID-19 = 22.9%, cancer = 32.0%) and spending ≥ 10% of income on medical expenses (due to any cause = 38.4%, COVID-19 = 4.7%, cancer = 31.4%).
Table 2.
Changes in healthcare utilization among survivors of adolescent and young adult cancers surveyed from October 2020 to January 2021
| n | % | |
|---|---|---|
| All | 341 | |
| Delayed/skipped cancer care since March 2020 | ||
| No | 276 | 80.9 |
| Yes | 65 | 19.1 |
| Facility/provider delayed or canceled care | 31 | 47.7 |
| Types of delayed/skipped cancer care | ||
| Oncology | 47 | 13.8 |
| Primary care | 7 | 2.1 |
| Mental health | 9 | 2.6 |
| Urgent care | 2 | 0.6 |
| Emergency care | 1 | 0.3 |
| Other specialties | 16 | 4.7 |
| Delayed/skipped other care since March 2020 | ||
| No | 220 | 64.5 |
| Yes | 120 | 35.2 |
| Facility/provider delayed or canceled care | 53 | 44.2 |
| Types of delayed/skipped other care | ||
| Primary care | 81 | 23.8 |
| Mental health | 40 | 11.7 |
| Urgent care | 9 | 2.6 |
| Emergency care | 4 | 1.2 |
| Dental | 18 | 5.3 |
| Other specialties | 33 | 9.7 |
| Changed medication obtainmenta | ||
| No | 208 | 61.0 |
| Yes | 65 | 19.1 |
| Changed medication use | ||
| No | 237 | 69.5 |
| Yes | 43 | 12.6 |
aAdaptive behaviors to find more affordable medications
Missing N’s: therapy = 4, delayed/skipped cancer care = 1, delayed/skipped not cancer care = 1, medication obtainment = 68, medication use = 61, financial toxicity = 2, financial burden = 1, employment = 1
Italics indicate subgroup percentages
Odds ratios for delayed/skipped other care were greater among female survivors (OR = 2.41, 95%CI = 1.26–4.62) compared to males and among married/cohabiting survivors (OR = 2.34, 95% CI = 1.15–4.76) relative to single survivors (Table 3). Changing medication obtainment odds ratios were elevated among divorced/widowed/separated survivors (OR = 3.32, 95% CI = 1.08–10.2) and inverse among survivors with employer/military/individual health insurance (OR = 0.42, 95% CI = 0.21–0.82) relative to their comparison groups. Odds ratios for changes to medication use were elevated among LGBTQ + survivors (OR = 3.51, 95% CI = 1.35–9.11) but inverse among married/cohabiting survivors (OR = 0.31, 95% CI = 0.13–0.73). We found no significant results by cancer diagnosis or self-reported cancer therapy since March 2020.
Table 3.
Multivariable associations of demographic and clinical characteristics of survivors of adolescent and young adult cancers and changes in healthcare utilization during the COVID-19 pandemic
| Models | Delayed/skipped care from March 2020 to January 2021 | Changes to medication obtainment or use because of the COVID-19 pandemic | ||||
|---|---|---|---|---|---|---|
| Cancer care | Other care | Obtainmenta | Use | |||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |||
| 1 | Gender | Female | 0.83 (0.39–1.76) | 2.41 (1.26–4.62)* | 1.17 (0.62–2.20) | 1.49 (0.71–3.15) |
| Male | 1 | 1 | 1 | 1 | ||
| 2 | Marital status | Divorced/widowed/separated | 1.65 (0.37–7.36) | 1.56 (0.42–5.82) | 3.32 (1.08–10.2)* | 0.55 (0.14–2.10) |
| Married/cohabitating | 1.28 (0.54–3.05) | 2.34 (1.15–4.76)* | 0.64 (0.31–1.33) | 0.31 (0.13–0.73)* | ||
| Single | 1 | 1 | 1 | 1 | ||
| 3 | Sexuality | LGBTQ + | 2.25 (0.65–7.80) | 0.64 (0.20–2.10) | 1.72 (0.62–4.73) | 3.51 (1.35–9.11)* |
| Cis-heterosexual | 1 | 1 | 1 | 1 | ||
| 4 | Education | ≤ High school | 0.77 (0.14–4.34) | 0.77 (0.22–2.68) | 2.63 (0.68–10.1) | 0.60 (0.11–3.11) |
| Some college | 1.32 (0.37–4.69) | 0.95 (0.38–2.38) | 1.53 (0.50–4.68) | 1.01 (0.29–3.52) | ||
| College | 0.93 (0.26–3.38) | 1.15 (0.46–2.88) | 1.39 (0.45–4.36) | 0.80 (0.22–2.93) | ||
| Grad school | 1 | 1 | 1 | 1 | ||
| 5 | Health insurance | Employer/military/individual | 0.60 (0.26–1.42) | 0.76 (0.37–1.56) | 0.42 (0.21–0.82)* | 0.50 (0.23–1.08) |
| Public, uninsured, unknown | 1 | 1 | 1 | 1 | ||
| 6 | Diagnosis age (years) | 15–19 | 0.32 (0.02–4.61) | 0.21 (0.03–1.35) | 0.69 (0.11–4.28) | 1.32 (0.15–11.5) |
| 20–24 | 1.38 (0.14–13.5) | 0.24 (0.04–1.32) | 0.85 (0.16–4.66) | 1.19 (0.15–9.65) | ||
| 25–29 | 1.30 (0.16–10.6) | 0.22 (0.05–1.07) | 1.11 (0.23–5.28) | 1.26 (0.18–8.87) | ||
| 30–34 | 2.43 (0.53–11.1) | 0.46 (0.12–1.73) | 1.45 (0.41–5.07) | 1.53 (0.30–7.86) | ||
| 35–40 | 1 | 1 | 1 | 1 | ||
| 7 | Diagnosis | CNS and nervous system | 0.66 (0.16–2.81) | 0.50 (0.12–2.11) | 1.42 (0.24–8.37) | 1.02 (0.08–12.7) |
| Carcinoma | 0.58 (0.15–2.21) | 0.76 (0.23–2.53) | 1.61 (0.30–8.57) | 2.46 (0.28–21.9) | ||
| Gonadal or related tumors | 0.39 (0.06–2.56) | 0.20 (0.03–1.27) | 1.66 (0.24–11.7) | 5.74 (0.51–64.2) | ||
| Leukemia or lymphoma | 0.35 (0.09–1.37) | 1.32 (0.41–4.29) | 1.67 (0.33–8.47) | 2.66 (0.31–22.7) | ||
| Sarcoma | 0.47 (0.09–2.56) | 1.66 (0.42–6.56) | 0.96 (0.14–6.35) | 3.61 (0.36–36.7) | ||
| Melanoma | 1 | 1 | 1 | 1 | ||
| 8 | Therapy since March 2020 | No | 0.88 (0.41–1.89) | 1.42 (0.78–2.60) | 1.37 (0.74–2.52) | 1.74 (0.84–3.62) |
| Yes | 1 | 1 | 1 | 1 | ||
aAdaptive behaviors to find more affordable medications
Models for cancer care exclude n = 33 and other care exclude n = 57 with delayed/skipped care due to provider/facility preference. Persons with no information on medication obtainment (n = 68) or use (n = 61) were excluded
Model 1 controls for survey age and race/ethnicity. Models 2–7 control for gender, survey age, and race/ethnicity
OR, odds ratio; CI, confidence interval. *p < 0.05
Financial burdens had significant impacts on delayed/skipped cancer and other care appointments. Odds of reporting a delayed/skipped cancer care appointment were greater among survivors with high material hardships due to any cause, from COVID-19, and from cancer (any cause, OR = 3.13, 95% CI = 1.44–6.81; COVID-19, OR = 6.09, 95% CI = 2.04–18.10; cancer, OR = 5.36, 95% CI = 1.96–14.70) (Table 4). Delayed/skipped other care appointments were associated with high financial toxicity (OR = 2.53, 95% CI = 1.31–4.89) and high material hardship from any cause, from COVID-19, and from cancer (any cause, OR = 2.17, 95% CI = 1.18–3.98; COVID-19, OR = 2.67, 95% CI = 1.29–5.53; cancer, OR = 2.17, 95% CI = 1.02–4.59).
Table 4.
Multivariable associations of financial burden and employment changes of survivors of adolescent and young adult cancers and changes in healthcare utilization during the COVID-19 Pandemic
| Models | n | Delayed/skipped care from March 2020 to January 2021 | Changes to medication obtainment or use because of the COVID-19 pandemic | ||||
|---|---|---|---|---|---|---|---|
| Cancer care | Other care | Obtainmenta | Use | ||||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||||
| 1 | Financial toxicity | High: COST score ≤ 21 | 168 | 1.75 (0.79–3.91) | 2.53 (1.31–4.89)* | 1.96 (1.01–3.83)* | 3.73 (1.59–8.73)* |
| Low: COST score > 21 | 171 | 1 | 1 | 1 | 1 | ||
| 2 | Material hardship, any cause | High: 4–11 | 136 | 3.13 (1.44–6.81)* | 2.17 (1.18–3.98)* | 2.72 (1.43–5.18)* | 4.49 (2.05–9.80)* |
| Low: 0–3 | 204 | 1 | 1 | 1 | 1 | ||
| 3 | Material hardship due to COVID-19 | High: 2–9 | 106 | 6.09 (2.04–18.10)* | 2.67 (1.29–5.53)* | 3.08 (1.41–6.75)* | 3.63 (1.41–9.35)* |
| Low: 0–1 | 131 | 1 | 1 | 1 | 1 | ||
| 4 | Material hardship due to cancer | High: 2–9 | 90 | 5.36 (1.96–14.70)* | 2.17 (1.02–4.59)* | 3.08 (1.41–6.71)* | 2.93 (1.18–7.27)* |
| Low: 0–1 | 144 | 1 | 1 | 1 | 1 | ||
| 3 | Employment or schooling changes during COVID-19 pandemic | Increased hours | 67 | 0.89 (0.29–2.72) | 0.77 (0.30–1.96) | 1.18 (0.44–3.17) | 4.54 (1.44–14.30)* |
| Reduced hours | 74 | 2.64 (0.98–7.10) | 1.40 (0.58–3.36) | 2.08 (0.88–4.88) | 3.66 (1.23–10.90)* | ||
| No change (unemployed/caregiver) | 80 | 0.39 (0.10–1.62) | 1.44 (0.64–3.20) | 0.60 (0.23–1.59) | 1.06 (0.29–3.85) | ||
| No change (employed) | 119 | 1 | 1 | 1 | 1 | ||
aAdaptive behaviors to find more affordable medications
Models for cancer care exclude n = 33 and other care exclude n = 57 persons with delayed/skipped care due to provider/facility preference. Persons with no information on medication obtainment (n = 68) or use (n = 61) were excluded
All models adjust for gender, survey age, marital status, education, health insurance type, and race/ethnicity
OR, odds ratio; CI, confidence interval
COST, “COmprehensive Score for financial Toxicity”
Missing N = 104 for hardship missing due to COVID-19 and N = 107 responses for hardship due to cancer
*p < 0.05
Odds ratios for changes in medication obtainment were elevated among survivors with high financial toxicity (OR = 1.96, 95% CI = 1.01–3.83) and high material hardship due to any cause, from COVID-19, and from cancer (any cause, OR = 2.72, 95% CI = 1.43–5.18; COVID-19, OR = 3.08, 95% CI = 1.41–6.75; cancer, OR = 3.08, 95% CI = 1.41–6.71). Odd ratios for changing medication use were elevated among survivors with high financial toxicity (OR = 3.73, 95% CI = 1.59–8.73) and high material hardship from any cause, COVID-19, and cancer (any cause, OR = 4.49, 95% CI = 2.05–9.80; COVID-19, OR = 3.63, 95% CI = 1.41–9.35; cancer, OR = 2.93, 95% CI = 1.18–7.27) relative to their comparison groups. Participants whose employment/school hours were increased (OR = 4.54, 95% CI = 1.44–14.30) or reduced (OR = 3.66, 95% CI = 1.23–10.90) had higher odds of changing their medication use relative to employed survivors with no changes.
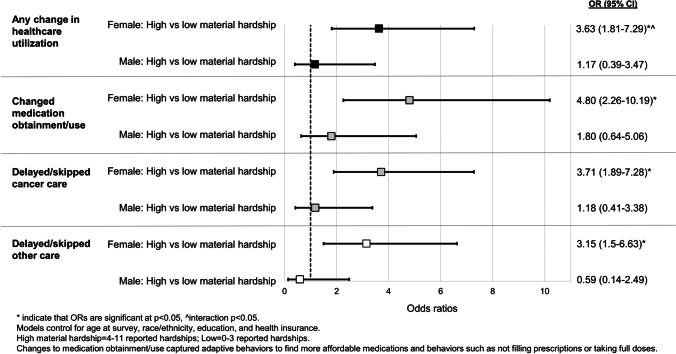
We found significant effect modification of the association of high material hardship and adverse changes in any healthcare utilization by gender (Fig. 1; p value interaction = 0.03). Females with high material hardship had an odds ratio of 3.63 (95% CI =1.81–7.29 of changing any healthcare utilization compared to females with low material hardship, while the odds ratio among males did not significantly differ by material hardship (OR = 1.17, 95% CI = 0.39–3.47). Odds ratios for female-only analyses were consistently elevated and significant for all other outcomes, including changes in medication obtainment/use (OR =4.80, 95% CI = 2.26–10.19) and delayed/skipped cancer or other care (cancer, OR =3.71, 95% CI = 1.89–7.28; other care, OR=3.15, 95% CI=1.50–6.63). We found no significant differences in the effect estimates for the association of changes in employment and our outcomes stratified by gender.
Fig. 1.
Effect modification of the association of material hardship and healthcare utilization by gender among survivors of adolescent and young adult cancers during the COVID-19 pandemic
In a post hoc analysis, we found no significant correlations between demographics and delayed/skipped care among persons with delays/skips that were due to provider/facility preference. We examined the effect modification of the association of material hardship and changes in healthcare utilization by LGBTQ + . The interaction term was significant, but the small sample size and resulting wide confidence intervals indicate that the results are not reliable.
Discussion
The COVID-19 pandemic had adverse impacts on healthcare utilization among survivors of AYA cancer, for whom healthcare is necessary to manage chronic conditions and prevent second neoplasms [9, 10]. We found that survivors of AYA cancers with high financial burdens had nearly threefold increases in their odds of delaying or skipping healthcare appointments. While provider-initiated delays/cancelations were a large reason for delayed/skipped care, our results provide strong support for the role of pandemic-related financial barriers in impeding healthcare utilization. Survivors who were females, married, and LGBTQ + appear to be at risk for pandemic-related decreases in healthcare utilization.
Even before the COVID-19 pandemic, AYA survivors had high rates of treatment nonadherence [26, 27], and financial toxicity was a significant risk factor for nonadherence [14, 22]. In our study, financial toxicity and material hardship had significant impacts on delayed/skipped cancer care. Even a 4-week delay in starting care increases mortality from treatable cancers that are diagnosed among AYAs, including breast, cervical, and colorectal cancer [6, 7]. In this study, financial burdens were the only significant contributing factors to delayed/skipped cancer or other care. Over a third of surveyed survivors delayed/skipped other care while nearly 20% delayed/skipped cancer care, perhaps due to perceptions that cancer care was of greater importance. While receiving timely cancer care is important for cancer survival, primary care is still needed to detect preventable diseases, cancer screenings, and administration of vaccines including COVID-19 vaccines. The lower percent of delayed/skipped cancer care suggests that AYA survivors may have a higher need or feel more pressure to pay for cancer care than other types of healthcare during the COVID-19 pandemic.
Adherence to recommended medication use is necessary as many chemotherapies have transitioned from intravenous administration to oral ingestion [28], and medications may also be needed to manage therapy-related effects [29]. Our results support that pandemic-related financial burdens were major barriers to medication adherence among AYA survivors, increasing the odds of changing medication obtainment by fivefold relative to survivors with fewer financial burdens. Our survey questions about medication obtainment captured adaptive behaviors to find affordable medications. The cost of prescription medications in the USA rose even before the pandemic began, with cancer drugs being among the most expensive [30].
AYA survivors in the USA have limited protections against drug price increases and are responsible for drug costs that may or may not be covered by health insurance policies [30]. As medication costs during the COVID-19 pandemic may increase due to supply chain interruptions [31], adaptations to locate affordable medications may not be effective in the face of global supply problems. These pandemic-related barriers to obtaining and using medications will require more follow-up to document their full impact on AYA survivors.
Patterns in healthcare utilization appear to vary based on relationship status and sexual orientation/gender identity. Married/cohabiting survivors had two-fold odds of reporting delayed/skipped other care, but inverse odds of changing medication use relative to single persons. During the COVID-19 pandemic, women had increased responsibilities due to school and daycare closures [32]. In addition to their regular employment, women were more likely to be tasked with the at-home education and care of children [33, 34]. While many employed women left their jobs to cope with these added pressures [35, 36], nationwide, women were also more likely to be laid off or underemployed during the pandemic [25]. This loss of income may have increased material hardships experienced by the family as a whole while adding to demands on women’s time.
Prior to the pandemic, financial burdens were a risk factor for delayed/skipped healthcare appointments among families with children [37]. The combination of time limitations due to childcare responsibilities and the rise of pandemic-related material hardships may explain why the odds ratio for delayed/skipped other care was greater among married/cohabiting females relative to single persons. The inverse odds of changing medication use among married persons may be due to having a stable caregiver who helps manage medications or supports self-management of medications [38].
Divorced/widowed/separated survivors and LGBTQ + survivors appear to be more vulnerable to pandemic-related changes in medication obtainment and use, respectively. Divorced persons may experience poorer health and greater health expenditures relative to married persons [39, 40]. This may be due to the lack of social support, financial resources, or access to a partner’s health insurance [39, 40]. Greater healthcare expenditures, competing needs of dependents, social isolation, and financial problems brought on by the pandemic may have led to these changes in medication obtainment among divorced/widowed/separated survivors. In our study, divorced/widowed/separated had a three-fold increase in their odds of changing how their medication was obtained, signaling a potential need to obtain medications at a lower cost than prior to the pandemic.
LGBTQ + survivors also faced social and/or financial challenges in forms of social isolation [41], discrimination by employers [42], and greater rates of poverty before and during the pandemic [43]. In addition, LGBTQ + persons have difficulty finding non-stigmatizing and nondiscriminatory cancer care [44, 45]. These multiple forces may have impeded LGBTQ + survivors from using necessary medication, showing nearly fourfold increases in changing medication use relative to cis-heterosexual persons in this study [46, 47].
The pandemic had disproportionate adverse financial and employment impacts on women [25], and these financial issues appear to have impacted female survivors’ healthcare utilization based on the degree of their material hardship. None of these patterns was seen among male survivors. Financial burdens from COVID-19 and cancer played a large role in our findings, but social pressures may have also contributed to the associations. In our study, women composed nearly the entire group of divorced/widowed/separated and LGBTQ + persons, as well as a large percent of married survivors. Because we saw significant differences in healthcare utilization among survivors in these groups, the differential impacts of material hardships experienced by females may also be explained by marital status and LGBTQ + identity.
Our findings differ from a prior national survey reporting that 60% of AYA survivors had delayed cancer care [11], potentially because the HIAYA patient navigation services may have had a protective effect and/or due to differences in the geographic scope of the surveys. Despite access to patient navigation services, one-fifth of AYAs in our sample still reported that the COVID-19 pandemic had severe effects on their finances and ability to utilize healthcare. Our study provides strong support for the profound impacts that the COVID-19 pandemic had on delayed/skipped healthcare utilization among AYA survivors that may not be able to be addressed through patient navigation services alone. The HIAYA participants were predominantly non-Hispanic White, for whom the impact of the COVID-19 pandemic was less generally severe than racial and ethnic minorities [48]. Thus, we can infer that impacts on healthcare utilization among minority AYA survivors likely have been more severe than reported by our sample.
Socioeconomic disparities in healthcare utilization are not new, but the results of our study suggest that the COVID-19 pandemic heightened these disparities. Prior to the pandemic, AYA survivors already experienced systematic inequalities in health insurance coverage, cancer care delivery and healthcare access, and employment discrimination that influence their health outcomes [49, 50]. During the pandemic, AYAs from historically marginalized groups (e.g., women, LGBTQ +) appeared to be the most vulnerable to the financial impacts of the pandemic and disruptions in healthcare. Thus, addressing the challenges posed by COVID-19 for these groups requires a systematic approach that considers and addresses the fundamental causes of socioeconomic disparities in the US healthcare system, such as lack of insurance access.
Some of the COVID-19 economic policies, such as the federal stimulus checks and other financial aids, were passed to provide households with some relief from the financial impacts of the pandemic [51]. These policies may have lessened the socioeconomic disparities in cancer health outcomes among AYA survivors. Understanding how financial assistance like the stimulus checks was used by AYAs during the COVID-19 pandemic can shed light on how to implement financial interventions in future pandemics.
As pandemics of infectious diseases are expected to increase in frequency with climate change [52], steps should be taken to intervene and provide support to these marginalized groups during future pandemics. Since females were most affected by the financial impacts of the pandemic, ensuring that women are able to secure an income and continuity of services that enable employment or alleviate stress among women (e.g., childcare) may be critical pieces to supporting their healthcare access. Medication use among LGBTQ AYAs was the most impacted during the pandemic. While this suggests that ensuring continuous access to providers, pharmacies, and prescriptions during pandemics may be a challenge for this group, more studies are needed in this population.
Limitations of the study included our small sample for LGBTQ + survivors and limited information about active treatment for cancer late effects. We did not ask participants about their stage of cancer at diagnosis. While stage may be correlated with healthcare utilization [53–56], we were primarily interested in how the pandemic affected patients currently in treatment versus not in treatment. We also do not have information about the number of dependents belonging to each participant, nor more detailed information about their work history or household income prior to the pandemic. But we do have detailed information about their reported financial burdens and the origin of those financial burdens. Like all cross-sectional studies, the causal nature of these associations between financial burdens relative to the changes in healthcare utilization cannot be determined due to temporality. Nonetheless, this study reports important associations that shed light on the COVID-19 pandemic’s impact on AYA cancer survivors’ use of healthcare.
Our strengths include our sample recruited from a multisite, health systems–based AYA patient navigation program, and highly detailed questionnaire about healthcare utilization.
Conclusion
Financial problems originating from the COVID-19 pandemic had adverse impacts on healthcare utilization among AYA survivors, with female, divorced/widowed/separated, and LGBTQ + survivors having elevated risk.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank and acknowledge the efforts of the HIAYA staff and study participants. This project was funded by the Huntsman Cancer Institute/Intermountain Healthcare Grand Challenges Grant and the National Cancer Institute’s Cancer Center Support Grant. Dr. Ou is a member of Huntsman Cancer Institute’s Cancer Biostatistics (CB) Shared Resource.
Author contribution
Judy Ou conducted the analyses, contributed to the study aims, and was the primary writer. Austin Waters and Heydon Kaddas conducted data cleaning and management and contributed to the analysis. Austin Waters, Perla Vaca Lopez, and Karely Mann distributed the survey. Karely Mann, Perla Vaca Lopez, Echo Warner, John Anderson, Nicole Ray, Douglas Fair, and Tomoko Tsukamoto contributed to the survey creation and manuscript review. David Gill and Lauri Linder reviewed the manuscript. Anne Kirchhoff was the principal investigator and was responsible for overseeing the study activities and for financial support for all activities.
Funding
This project was funded by the Huntsman Cancer Institute/Intermountain Healthcare Grand Challenges Grant and the National Cancer Institute’s Cancer Center Support Grant.
Declarations
Ethics approval
The University of Utah IRB approved this study.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention. COVID Data Tracker. Atlanta, GA: US Department of Health and Human Services, CDC; 2022 [cited 2022 May 11]. Available from: https://covid.cdc.gov/covid-data-tracker
- 2.Boserup B, McKenney M, Elkbuli A. The financial strain placed on America’s hospitals in the wake of the COVID-19 pandemic. Am J Emerg Med. 2021; Jul(45): 530–531. Published online 2020 Jul 9. [DOI] [PMC free article] [PubMed]
- 3.Warner MA. Stop doing needless things! Saving healthcare resources during COVID-19 and beyond. J Gen Intern Med. 2020;35(7):2186–2188. doi: 10.1007/s11606-020-05863-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20(1):1193. doi: 10.1186/s12889-020-09301-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wood SM, Pickel J, Phillips AW, Baber K, Chuo J, Maleki P, Faust HL, Petsis D, Apple DE, Dowshen N, Schwartz LA. Acceptability, feasibility, and quality of telehealth for adolescent health care delivery during the COVID-19 pandemic: cross-sectional study of patient and family experiences. JMIR Pediatr Parent. 2021;4(4):e32708. doi: 10.2196/32708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hartman HE, Sun Y, Devasia TP, Chase EC, Jairath NK, Dess RT, Jackson WC, Morris E, Li P, Hochstedler KA, Abbott MR, Kidwell KM, Walter V, Wang M, Wang X, Zaorsky NG, Schipper MJ, Spratt DE. Integrated survival estimates for cancer treatment delay among adults with cancer during the COVID-19 pandemic. JAMA Oncol. 2020;6(12):1881–1889. doi: 10.1001/jamaoncol.2020.5403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, Harvey-Jones E, O’Sullivan DE, Booth CM, Sullivan R, Aggarwal A. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087. doi: 10.1136/bmj.m4087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keegan THM, Tao L, DeRouen MC, Wu X-C, Prasad P, Lynch CF, Shnorhavorian M, Zebrack BJ, Chu R, Harlan LC, Smith AW, Parsons HM, Group AHSC Medical care in adolescents and young adult cancer survivors: what are the biggest access-related barriers? J Cancer Surviv. 2014;8(2):282–292. doi: 10.1007/s11764-013-0332-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ryder-Burbidge C, Diaz RL, Barr RD, Gupta S, Nathan PC, McKillop SJ, Fidler-Benaoudia MM. The burden of late effects and related risk factors in adolescent and young adult cancer survivors: a scoping review. Cancers (Basel) 2021;13(19):4870. doi: 10.3390/cancers13194870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bright CJ, Reulen RC, Winter DL, Stark DP, McCabe MG, Edgar AB, Frobisher C, Hawkins MM. Risk of subsequent primary neoplasms in survivors of adolescent and young adult cancer (Teenage and Young Adult Cancer Survivor Study): a population-based, cohort study. Lancet Oncol. 2019;20(4):531–545. doi: 10.1016/S1470-2045(18)30903-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller KA, Kagramanov D, Cohen-Cutler S, Nadim B, Weng Z, Gallagher P, Kaslander JN, Freyer DR, Barzi A, Lenz HJ. Impacts of the SARS-CoV-2 pandemic on young adult colorectal cancer survivors. J Adolesc Young Adult Oncol. 2021 doi: 10.1089/jayao.2021.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Souza JA, Yap BJ, Hlubocky FJ, Wroblewski K, Ratain MJ, Cella D, Daugherty CK. The development of a financial toxicity patient-reported outcome in cancer: the COST measure. Cancer. 2014;120(20):3245–3253. doi: 10.1002/cncr.28814. [DOI] [PubMed] [Google Scholar]
- 13.Thom B, Benedict C, Friedman DN, Watson SE, Zeitler MS, Chino F. Economic distress, financial toxicity, and medical cost-coping in young adult cancer survivors during the COVID-19 pandemic: Findings from an online sample. Cancer. 2021;127(23):4481–4491. doi: 10.1002/cncr.33823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salsman JM, Bingen K, Barr RD, Freyer DR. Understanding, measuring, and addressing the financial impact of cancer on adolescents and young adults. Pediatr Blood Cancer. 2019;66(7):e27660-e. doi: 10.1002/pbc.27660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meernik C, Kirchhoff AC, Anderson C, Edwards TP, Deal AM, Baggett CD, Kushi LH, Chao CR, Nichols HB. Material and psychological financial hardship related to employment disruption among female adolescent and young adult cancer survivors. Cancer. 2021;127(1):137–148. doi: 10.1002/cncr.33190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gibson AW, Radix AE, Maingi S, Patel S. Cancer care in lesbian, gay, bisexual, transgender and queer populations. Future Oncol. 2017;13(15):1333–1344. doi: 10.2217/fon-2017-0482. [DOI] [PubMed] [Google Scholar]
- 17.Zheng Z, Han X, Zhao J, Banegas MP, Tucker-Seeley R, Rai A, Fedewa SA, Song W, Jemal A, Yabroff KR. Financial hardship, healthcare utilization, and health among US cancer survivors. Am J Prev Med. 2020;59(1):68–78. doi: 10.1016/j.amepre.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 18.Treanor C, Donnelly M. An international review of the patterns and determinants of health service utilisation by adult cancer survivors. BMC Health Serv Res. 2012;12(1):1–20. doi: 10.1186/1472-6963-12-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kirchhoff AC, Lyles CR, Fluchel M, Wright J, Leisenring W. Limitations in health care access and utilization among long-term survivors of adolescent and young adult cancer. Cancer. 2012;118(23):5964–5972. doi: 10.1002/cncr.27537. [DOI] [PubMed] [Google Scholar]
- 20.Barr RD, Holowaty EJ, Birch JM. Classification schemes for tumors diagnosed in adolescents and young adults. Cancer. 2006;106(7):1425–1430. doi: 10.1002/cncr.21773. [DOI] [PubMed] [Google Scholar]
- 21.Wheeler S, Rodriguez-O’Donnell J, Rogers C, Fulcher J, Deal A, Manning M, Gellin M, Padilla N, Rosenstein D. Reducing cancer-related financial toxicity through financial navigation: results from a pilot intervention. Cancer Epidemiol Biomark Prev. 2020;29(3):694. doi: 10.1158/1055-9965.Epi-20-0067. [DOI] [Google Scholar]
- 22.Zafar SY, Peppercorn JM, Schrag D, Taylor DH, Goetzinger AM, Zhong X, Abernethy AP. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381–390. doi: 10.1634/theoncologist.2012-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yabroff KR, Dowling EC, Guy GP, Jr, Banegas MP, Davidoff A, Han X, Virgo KS, McNeel TS, Chawla N, Blanch-Hartigan D, Kent EE, Li C, Rodriguez JL, de Moor JS, Zheng Z, Jemal A, Ekwueme DU. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259–267. doi: 10.1200/JCO.2015.62.0468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Cancer Society. Survey: COVID-19 affecting patients’ access to cancer care 2021 [cited 2021 Nov 30, 2021]. Available from: https://www.fightcancer.org/releases/survey-covid-19-affecting-patients%E2%80%99-access-cancer-care.
- 25.Alon T, Doepke M, Olmstead-Rumsey J, Tertilt M. This time it’s different: the role of women’s employment in a pandemic recession. National Bureau of Economic Research, 2020.
- 26.Butow P, Palmer S, Pai A, Goodenough B, Luckett T, King M. Review of adherence-related issues in adolescents and young adults with cancer. J Clin Oncol. 2010;28(32):4800–4809. doi: 10.1200/jco.2009.22.2802. [DOI] [PubMed] [Google Scholar]
- 27.Hughes N, Stark D. The management of adolescents and young adults with cancer. Cancer Treat Rev. 2018;67:45–53. doi: 10.1016/j.ctrv.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 28.Bhattacharyya GS. Oral systemic therapy: Not all “win-win”. Indian J Med Paediatr Oncol. 2010;31(1):1–3. doi: 10.4103/0971-5851.68844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chao C, Xu L, Bhatia S, Cooper R, Brar S, Wong FL, Armenian SH. Cardiovascular disease risk profiles in survivors of adolescent and young adult (AYA) cancer: the Kaiser Permanente AYA Cancer Survivors Study. J Clin Oncol. 2016;34(14):1626–1633. doi: 10.1200/jco.2015.65.5845. [DOI] [PubMed] [Google Scholar]
- 30.Leighl NB, Nirmalakumar S, Ezeife DA, Gyawali B. An arm and a leg: the rising cost of cancer drugs and impact on access. Am Soc Clin Oncol Educ Book. 2021;41:e1–12. doi: 10.1200/edbk_100028. [DOI] [PubMed] [Google Scholar]
- 31.Ismail H, Marshall VD, Patel M, Tariq M, Mohammad RA. The impact of the COVID-19 pandemic on medical conditions and medication adherence in people with chronic diseases. J Am Pharm Assoc (2003). 2021. 10.1016/j.japh.2021.11.013. [DOI] [PMC free article] [PubMed]
- 32.Petts RJ, Carlson DL, Pepin JR. A Gendered pandemic: childcare, homeschooling, and parents’ employment during COVID-19. Gend Work Organ. 2021;28(S2):515–534. doi: 10.1111/gwao.12614. [DOI] [Google Scholar]
- 33.Aldossari M, Chaudhry S. Women and burnout in the context of a pandemic. Gend Work Organ. 2021;28(2):826–834. doi: 10.1111/gwao.12567. [DOI] [Google Scholar]
- 34.Carli LL. Women, Gender equality and COVID-19. Gend Manag: Int J. 2020.
- 35.Power K. The COVID-19 pandemic has increased the care burden of women and families. Sustain: Sci Pract Policy. 2020;16(1):67–73. 10.1080/15487733.2020.1776561.
- 36.Kalluri N, Kelly C, Garg A. Child care during the COVID-19 pandemic: a bad situation made worse. Pediatrics. 2021;147(3). [DOI] [PubMed]
- 37.Wisk LE, Witt WP. Predictors of delayed or forgone needed health care for families with children. Pediatrics. 2012;130(6):1027–1037. doi: 10.1542/peds.2012-0668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schulman-Green D, Feder SL, Dionne-Odom JN, Batten J, En Long VJ, Harris Y, Wilpers A, Wong T, Whittemore R. Family caregiver support of patient self-management during chronic, life-limiting illness: a qualitative metasynthesis. J Fam Nurs. 2021;27(1):55–72. doi: 10.1177/1074840720977180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Joung IMA. Marital status and health problems*. In: Fink G, editor. Encyclopedia of stress. 2. New York: Academic Press; 2007. pp. 653–659. [Google Scholar]
- 40.Meulman I. Differences in healthcare expenditure related to becoming divorced or widowed 2020.
- 41.Salerno JP, Williams ND, Gattamorta KA. LGBTQ populations: psychologically vulnerable communities in the COVID-19 pandemic. Psychol Trauma Theory Res Pract Policy. 2020;12(S1):S239–S242. doi: 10.1037/tra0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sears B, Mallory C. Employment discrimination against LGBT people: existence and impact 2014.
- 43.Badgett M, Choi SK, Wilson B. LGBT poverty in the United States. Los Angeles: The Williams Institute and American Foundation for Suicide; 2019. [Google Scholar]
- 44.Boehmer U, Miao X, Ozonoff A. Cancer survivorship and sexual orientation. Cancer. 2011;117(16):3796–3804. doi: 10.1002/cncr.25950. [DOI] [PubMed] [Google Scholar]
- 45.Waters AR, Tennant K, Cloyes KG. Cultivating LGBTQ+ competent cancer research: recommendations from LGBTQ+ cancer survivors, care partners, and community advocates. Semin Oncol Nurs. 2021;37(6):151227. doi: 10.1016/j.soncn.2021.151227. [DOI] [PubMed] [Google Scholar]
- 46.Wallach S, Garner A, Howell S, Adamson T, Baral S, Beyrer C. Address exacerbated health disparities and risks to LGBTQ+ individuals during COVID-19. Health Hum Rights. 2020;22(2):313–316. [PMC free article] [PubMed] [Google Scholar]
- 47.Lehman JR, Diaz K, Ng H, Petty EM, Thatikunta M, Eckstrand K. The equal curriculum: the student and educator guide to LGBTQ health. Springer Nature; 2019. [Google Scholar]
- 48.Gonzalez D, Karpman M, Kenney GM, Zuckerman S. Hispanic adults in families with noncitizens disproportionately feel the economic fallout from COVID-19. Washington: Urban Institute; 2020. p. 13. [Google Scholar]
- 49.Stone DS, Ganz PA, Pavlish C, Robbins WA. Young adult cancer survivors and work: a systematic review. J Cancer Surviv. 2017;11(6):765–781. doi: 10.1007/s11764-017-0614-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moke DJ, Tsai K, Hamilton AS, Hwang A, Liu L, Freyer DR, Deapen D. Emerging cancer survival trends, disparities, and priorities in adolescents and young adults: a California Cancer Registry-based study. JNCI Cancer Spectrum. 2019;3(2). 10.1093/jncics/pkz031. [DOI] [PMC free article] [PubMed]
- 51.Garner TI, Safir A, Schild J. Receipt and use of stimulus payments in the time of the Covid-19 pandemic. Beyond the numbers: prices and spending, Bureau of Labor Statistics. 2020;9(10):1–18.
- 52.The LM. Climate change: fires, floods, and infectious diseases. Lancet Microbe. 2021;2(9):e415. doi: 10.1016/S2666-5247(21)00220-2. [DOI] [PubMed] [Google Scholar]
- 53.Kaye DR, Min HS, Herrel LA, Dupree JM, Ellimoottil C, Miller DC. Costs of cancer care across the disease continuum. Oncologist. 2018;23(7):798–805. doi: 10.1634/theoncologist.2017-0481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Otto AK, Soriano EC, Siegel SD, LoSavio ST, Laurenceau J-P. Assessing the relationship between fear of cancer recurrence and health care utilization in early-stage breast cancer survivors. J Cancer Surviv. 2018;12(6):775–785. doi: 10.1007/s11764-018-0714-8. [DOI] [PubMed] [Google Scholar]
- 55.Starr LT, Ulrich CM, Corey KL, Meghani SH. Associations among end-of-life discussions, health-care utilization, and costs in persons with advanced cancer: a systematic review. Am J Hosp Palliat Med®. 2019;36(10):913–26. 10.1177/1049909119848148. [DOI] [PMC free article] [PubMed]
- 56.Mausbach BT, Irwin SA. Depression and healthcare service utilization in patients with cancer. Psychooncology. 2017;26(8):1133–1139. doi: 10.1002/pon.4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.