Abstract
Background
Complex regional pain syndrome (CRPS) is a painful and disabling condition that usually manifests in response to trauma or surgery and is associated with significant pain and disability. CRPS can be classified into two types: type I (CRPS I) in which a specific nerve lesion has not been identified and type II (CRPS II) where there is an identifiable nerve lesion. Guidelines recommend the inclusion of a variety of physiotherapy interventions as part of the multimodal treatment of people with CRPS. This is the first update of the review originally published in Issue 2, 2016.
Objectives
To determine the effectiveness of physiotherapy interventions for treating pain and disability associated with CRPS types I and II in adults.
Search methods
For this update we searched CENTRAL (the Cochrane Library), MEDLINE, Embase, CINAHL, PsycINFO, LILACS, PEDro, Web of Science, DARE and Health Technology Assessments from February 2015 to July 2021 without language restrictions, we searched the reference lists of included studies and we contacted an expert in the field. We also searched additional online sources for unpublished trials and trials in progress.
Selection criteria
We included randomised controlled trials (RCTs) of physiotherapy interventions compared with placebo, no treatment, another intervention or usual care, or other physiotherapy interventions in adults with CRPS I and II. Primary outcomes were pain intensity and disability. Secondary outcomes were composite scores for CRPS symptoms, health‐related quality of life (HRQoL), patient global impression of change (PGIC) scales and adverse effects.
Data collection and analysis
Two review authors independently screened database searches for eligibility, extracted data, evaluated risk of bias and assessed the certainty of evidence using the GRADE system.
Main results
We included 16 new trials (600 participants) along with the 18 trials from the original review totalling 34 RCTs (1339 participants). Thirty‐three trials included participants with CRPS I and one trial included participants with CRPS II. Included trials compared a diverse range of interventions including physical rehabilitation, electrotherapy modalities, cortically directed rehabilitation, electroacupuncture and exposure‐based approaches. Most interventions were tested in small, single trials. Most were at high risk of bias overall (27 trials) and the remainder were at 'unclear' risk of bias (seven trials). For all comparisons and outcomes where we found evidence, we graded the certainty of the evidence as very low, downgraded due to serious study limitations, imprecision and inconsistency. Included trials rarely reported adverse effects.
Physiotherapy compared with minimal care for adults with CRPS I
One trial (135 participants) of multimodal physiotherapy, for which pain data were unavailable, found no between‐group differences in pain intensity at 12‐month follow‐up. Multimodal physiotherapy demonstrated a small between‐group improvement in disability at 12 months follow‐up compared to an attention control (Impairment Level Sum score, 5 to 50 scale; mean difference (MD) ‐3.7, 95% confidence interval (CI) ‐7.13 to ‐0.27) (very low‐certainty evidence). Equivalent data for pain were not available. Details regarding adverse events were not reported.
Physiotherapy compared with minimal care for adults with CRPS II
We did not find any trials of physiotherapy compared with minimal care for adults with CRPS II.
Authors' conclusions
The evidence is very uncertain about the effects of physiotherapy interventions on pain and disability in CRPS. This conclusion is similar to our 2016 review. Large‐scale, high‐quality RCTs with longer‐term follow‐up are required to test the effectiveness of physiotherapy‐based interventions for treating pain and disability in adults with CRPS I and II.
Plain language summary
Does physiotherapy improve pain and disability in adults with complex regional pain syndrome?
Key messages
We are very uncertain if physiotherapy treatments improve the pain and disability associated with complex regional pain syndrome (CRPS).
We are very uncertain because the clinical trials we found:
‐ were not conducted or reported as well as they could have been (or both);
‐ included small numbers of patients with CRPS;
‐ tested a large range of different types of physiotherapy treatments; and
‐ because there were a limited number of trials that investigated any particular physiotherapy treatment.
We are very uncertain if physiotherapy treatments cause unwanted side effects; more evidence is required to clarify this.
Good‐quality clinical trials are required to further investigate whether or not physiotherapy treatments improve the pain and disability associated with CRPS.
Treating pain and disability in adults with complex regional pain syndrome
Complex regional pain syndrome is a painful and disabling condition that can occur after trauma or surgery and is associated with significant pain and disability. CRPS can be classified into two types: type I (CRPS I) in which a specific nerve injury has not been identified and type II (CRPS II) where there is an identifiable nerve injury. Guidelines recommend that physiotherapy rehabilitation should be included as part of the treatment for CRPS. Physiotherapy for CRPS could include a range of treatments and rehabilitation approaches, such as exercise, pain management, manual therapy, electrotherapy or advice and education, either used alone or in combination. Physiotherapy is recommended because it is thought that it may improve the pain and disability associated with CRPS.
What did we want to find out?
We wanted to find out if physiotherapy treatments improve pain and disability in adults (aged over 18) with CRPS.
What did we do?
We searched for clinical trials that involved adults with CRPS, which compared physiotherapy treatments to placebo treatments or routine care or which compared different physiotherapy treatments to each other.
We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as trial methods, size and length of follow‐up.
What did we find?
We found 33 clinical trials that involved 1317 people in total with CRPS type I of the upper or lower limb, or both. The trials investigated the effect of a range of physiotherapy treatments. We found only one trial involving 22 people with CRPS type II.
Here we present the findings from comparisons between different physiotherapy treatments and placebo treatments or routine care and for comparisons of different physiotherapy treatments to each other.
Reducing pain
We are uncertain if any of the physiotherapy treatments investigated in the clinical trials we identified help reduce the pain associated with CRPS.
Reducing disability
We are uncertain if any of the physiotherapy treatments investigated in the clinical trials we identified help reduce the disability associated with CRPS.
Side effects
We are uncertain if any of the physiotherapy treatments investigated in the clinical trials we identified cause any unwanted side effects.
What are the limitations of the evidence?
Clinical trials were small and most have been conducted in ways that could introduce errors into their results. This limited our confidence in the evidence.
How up to date is the evidence?
The evidence is up to date to July 2021.
Summary of findings
Summary of findings 1. Physiotherapy compared with minimal care for adults with CRPS I.
| Physiotherapy compared with minimal care for adults with CRPS I | ||||
|
Patient or population: adults with CRPS I Settings: outpatient clinic Intervention: multimodal physiotherapy Comparison: 'social work' (i.e. passive attention, advice) | ||||
| Outcomes | Effect size (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments |
|
Oerlemans 1999 Pain (VAS 0 to 100) |
Not estimable | — | — | — |
|
Oerlemans 1999 Disability as measured by the impairment level sum score (5 to 50) Higher scores indicate greater impairment Measured 12 months post recruitment |
MD ‐3.7 95% CI ‐7.13 to 0.27 |
91 (1) | ⊕⊝⊝⊝ very lowa,b,c |
One study found evidence of a small beneficial effect of physiotherapy compared to 'social work' (i.e. an attention and advice control) intervention |
| Incidence/nature of adverse effects | Not estimable | — | — | Data not reported |
| CI: confidence interval; CRPS I: complex regional pain syndrome type I; MD: mean difference; VAS: visual analogue scale | ||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect; Very low certainty: We have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect. | ||||
aDowngraded once for serious study limitations.
bDowngraded once for inconsistency.
cDowngraded once for imprecision.
Summary of findings 2. Physiotherapy compared with minimal care for adults with CRPS II.
| Physiotherapy compared with minimal care for adults with CRPS II | ||||
|
Patient or population: adults with CRPS II Settings: any Intervention: multimodal physiotherapy Comparison: any eligible comparison | ||||
| Outcomes | Effect size (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments |
| Pain (VAS 0 to 100) | No data | — | — | — |
| Disability | No data | — | — | — |
| Incidence/nature of adverse effects | No data | — | — | — |
| CRPS II: complex regional pain syndrome type II | ||||
CI: confidence interval; CRPS: complex regional pain syndrome; VAS: visual analogue scale
Background
This is the first update of a review of physiotherapy interventions for complex regional pain syndrome originally published in 2016 (Smart 2016).
Description of the condition
Complex regional pain syndrome (CRPS) is a persistent, painful and disabling condition that usually, but not exclusively, manifests in response to acute trauma or surgery (Goebel 2011; Shipton 2009). The International Association for the Study of Pain (IASP) introduced the diagnostic label 'CRPS' in the 1990s in order to standardise inconsistencies in terminology and diagnostic criteria (Merskey 1994). Two sub‐categories of CRPS have been described: CRPS type I (CRPS I) (formerly and variously referred to as reflex sympathetic dystrophy (RSD), algodystrophy, Sudek's atrophy), in which there is no clear evidence of a nerve lesion and CRPS type II (CRPS II) (formerly referred to as causalgia, algoneurodystrophy), in which a co‐existing nerve lesion (as determined by nerve conduction studies or surgical inspection, for example) is present (Coderre 2011; Todorova 2013).
CRPS is characterised by symptoms and signs typically confined to a body region or limb, but which may become more widespread (van Rijn 2011). The diagnostic criteria for CRPS originally proposed by Veldman et al (Veldman 1993) and subsequently by the IASP (Merskey 1994) have since been revised in response to their low specificity and potential to over‐diagnose cases of CRPS. The Budapest criteria proposed by Harden 2010 have enhanced diagnostic accuracy and are now widely accepted (Goebel 2011). The diagnosis of CRPS is clinical and the cardinal features include (Goebel 2011):
continuing pain disproportionate to any inciting event;
the presence of clusters of various symptoms and signs reflecting sensory (e.g. hyperaesthesia, allodynia), vasomotor (e.g. asymmetries of temperature or skin colour, or both), sudomotor (e.g. oedema or altered sweating or both), motor (e.g. reduced range of motion, tremor) or trophic (e.g. altered hair or nails, or both) disturbances; and
the absence of any other medical diagnosis that might better account for an individual's symptoms and signs.
However, a recent international survey of clinical practice found half of health professionals who provided clinical care to patients with CRPS had difficulty in recognising the symptoms of CRPS (Grieve 2019). Symptom profiles can vary between individuals with CRPS (Borchers 2014) and while statistically determined phenotypes (‘central’, ‘peripheral’ and ‘mixed’ phenotypes) have been suggested (Dimova 2020), their clinical significance is as yet unclear.
The pathophysiological mechanisms underlying CRPS are not fully understood (Harden 2010). Current understanding implicates multiple mechanisms including complex contributions from a maladaptive pro‐inflammatory response and a disturbance in sympathetically mediated vasomotor control, together with maladaptive peripheral and central neuronal plasticity (Birklein 2017; Bruehl 2010; Bruehl 2015; Knudsen 2019; Marinus 2011; Parkitny 2013). Furthermore, mechanisms, and in consequence symptoms and signs, may vary between individuals and within individuals over the time course of the disorder, thus heightening the complexity (Marinus 2011).
The incidence of CRPS is not accurately known but population estimates indicate an incidence of somewhere between five and 26 cases per 100,000 person‐years (Marinus 2011). A likely conservative 11‐year period prevalence rate for CRPS of 20.57 per 100,000 people has been reported (Sandroni 2003). CRPS is three to four times more likely to occur in women than in men, and although it may occur at any time throughout the lifespan, it tends to occur more frequently with increasing age (Shipton 2009). Genetic susceptibility may serve as an aetiological risk factor for the development of CRPS (de Rooij 2009). In individuals who develop CRPS after a fracture, intra‐articular fracture, fracture‐dislocation, pre‐existing rheumatoid arthritis, pre‐existing musculoskeletal co‐morbidities (e.g. low‐back pain, arthrosis) (Beerthuizen 2012) and limb immobilisation (Marinus 2011) may increase the risk of its development. A retrospective analysis of risk factors for the development of CRPS I in a large (22,533 patients) 'Nationwide Inpatient Sample' database from 2007 to 2011 in the United States found female gender, Caucasian race, higher median household income, depression, headache and drug abuse to be associated with a higher rate of CRPS I in an inpatient population (Elsharydah 2017). Others have found that psychological traits, such as depression, anxiety, neuroticism and anger, have so far been discounted as risk factors for the development of CRPS (Beerthuizen 2009: Lohnberg 2013), although further prospective studies are required to substantiate this assertion (Harden 2013). However, they may be associated with poorer outcomes once the condition has developed (Bean 2015). Studies into the course of CRPS present contradictory findings. Whilst some studies have reported complete and partial symptom resolution within one year (Sandroni 2003; Zyluk 1998), other studies have indicated more protracted symptoms and impairments lasting from three to nine years (de Mos 2009; Geertzen 1998; Vaneker 2006). Evidence from prognostic studies of CRPS is scarce and contradictory (Wertli 2013).
People with CRPS have been found to have poor knowledge of the condition (Brunner 2010), and experience significant suffering and disability (Bruehl 2010; Lohnberg 2013). It appears that men with CRPS are more likely to experience depression and kinesiophobia and use more passive coping strategies than women (van Velzen 2019). Preliminary data suggest that interference with activities of daily living, sleep, work and recreation is common and further contributes to a diminished quality of life (Galer 2000; Geertzen 1998; Kemler 2000; Sharma 2009). Qualitative data concerning the lived experience of CRPS from the patient's perspective is emerging. Such studies have found that living with CRPS is a daily battle, and that coping with changing symptoms together with the knowledge that there is no known cure can be particularly challenging (Johnston‐Devin 2018). Furthermore, living with CRPS can have a widespread impact on personal and social relationships and intimacy (Packham 2020). Another qualitative study that investigated the informational needs of people living with CRPS found patients wanted honest and accurate information, the opportunity to meet others with the condition and readily available resources with which to facilitate access to local expertise (Grieve 2016a).
Guidelines for the treatment of CRPS recommend an interdisciplinary multimodal approach, comprising pharmacological and interventional pain management strategies together with rehabilitation, psychological therapy and educational strategies (Goebel 2018; Harden 2013; Perez 2010; Stanton‐Hicks 2002), and two international surveys of clinical practice suggest such care is being delivered (Grieve 2019; Miller 2017). However determining the optimal approach to therapy remains clinically challenging (Cossins 2013; O'Connell 2013; Shim 2019).
Description of the intervention
Despite the fact that their effectiveness is not known, guidelines recommend the inclusion of a variety of physiotherapy interventions as part of the multimodal treatment of CRPS (Goebel 2018; Perez 2010; Stanton‐Hicks 2002). Physiotherapy has been defined as "the treatment of disorders with physical agents and methods" (Anderson 2002). For CRPS this could include any of the following interventions employed either as stand‐alone interventions or in combination: manual therapy (e.g. mobilisation, manipulation, massage, desensitisation); therapeutic exercise and progressive loading regimens (including hydrotherapy); electrotherapy (e.g. transcutaneous electrical nerve stimulation (TENS), therapeutic ultrasound, interferential, shortwave diathermy, laser); physiotherapist‐administered education (e.g. pain neuroscience education); as well as cortically directed sensory‐motor rehabilitation strategies (e.g. graded motor imagery (GMI), mirror therapy, sensory‐motor retuning, tactile discrimination training).
How the intervention might work
The precise mechanisms of action through which various physiotherapy interventions are purported to relieve the pain and disability associated with CRPS are not fully understood. Theories underpinning the use of manual therapies to relieve pain include the induction of peripheral or central nervous system‐mediated analgesia, or both (Bialosky 2018). While therapeutic exercise may bring about exercise‐induced analgesia by positively influencing i) central pain processing, via endorphin‐mediated inhibition for example (Nijs 2012), ii) immune system function and iii) the affective aspects of pain (Smith 2019), and improve function, and by extension disability, by restoring range of movement at affected joints and improving neuromuscular function and load tolerance (Kisner 2002). Theories underlying the use of electrotherapy modalities, also known as electrophysical agents, for pain relief variously include spinal cord‐mediated electro‐analgesia, heat‐ or cold‐mediated analgesia and anti‐inflammatory effects (Atamaz 2012; Logan 2017; Robertson 2006). Pain neuroscience education aims to reduce pain and disability by helping individuals to better understand the biological processes underlying their pain in a way that positively changes pain perceptions and attitudes (Moseley 2015). Other rehabilitation strategies, such GMI or mirror therapy, may provide pain relief or increase mobility, or both, by ameliorating maladaptive somatosensory and motor cortex reorganisation (Moseley 2012).
Why it is important to do this review
A number of systematic reviews suggest that physiotherapy interventions (e.g. exercise, GMI, TENS) employed in combination with medical management may be beneficial in reducing the pain and disability associated with CRPS (Daly 2009; Smith 2005). However, the inclusion of non‐randomised clinical trials and case series designs, together with the exclusion of studies involving people with CRPS II as well as those published in a language other than English, may have biased these conclusions. Given the limitations of existing systematic reviews, together with the availability of potentially numerous physiotherapy treatment strategies for CRPS, an up‐to‐date systematic review of the evidence from randomised clinical trials for the effectiveness of these interventions may assist clinicians in their treatment choices and inform future clinical guidelines that may be of use to policymakers and those who commission healthcare for people with CRPS.
Our original Cochrane systematic review of physiotherapy interventions for CRPS found very low‐quality evidence supporting the use of graded motor imagery and mirror therapy for pain and disability in people with CRPS I while evidence of the effectiveness of most other physiotherapeutic interventions was generally absent or unclear. Additionally, we found no eligible trials of physiotherapy interventions for CRPS II (Smart 2016). An update to our original Cochrane systematic review of physiotherapy interventions for CRPS was considered appropriate given the publication of a number of additional clinical trials since the endpoint of our original search (February 2015).
Objectives
To determine the effectiveness of physiotherapy interventions for treating pain and disability associated with CRPS types I and II.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) (including those of parallel, cluster‐randomised and cross‐over design) published in any language. Translators identified by the Managing Editor of the Cochrane Pain, Palliative and Supportive Care Group evaluated studies published in a language other than English. We excluded studies in which participants were not randomised to intervention groups.
While we accept that non‐randomised studies (e.g. case series, quasi‐experimental designs) can provide “proof of concept”‐level evidence for healthcare interventions it is our contention that such evidence should not be used to inform clinical treatment decision‐making because such evidence is less robust and subject to greater risks of bias than RCTs (Shea 2017). Also, given that our original systematic review identified 18 clinical trials we decided there was no justification for including non‐randomised studies on the grounds of an absence of RCT data upon which to inform clinical decision‐making. We accept it could be argued that the exclusion of non‐randomised studies provides an incomplete summary of the potential effects of interventions but we maintain the view that a robust systematic review of the evidence for the effectiveness of physiotherapy interventions for CRPS is best established by the inclusion of RCTs only. We remain open to the fact that developments in the science and methodology of systematic reviews might justify the inclusion of data from non‐randomised studies, such as from large population databases, in the future (Shea 2017). We included published abstracts and where there were insufficient data for analysis in the abstracts, we attempted to locate the full study (e.g. by contacting the study authors). If the data from the full study were unavailable, we added the abstract to ‘Studies awaiting classification’ (see Characteristics of studies awaiting classification table).
Types of participants
We included trials of adults, aged 18 years or older, diagnosed with CRPS I or II, or with an alternative diagnostic label for these conditions (e.g. RSD, causalgia). We grouped trials and analysed data according to diagnosis (i.e. CRPS I and II, or mixed). Since the use of formal diagnostic criteria for CRPS is inconsistent across studies (Reinders 2002), we included trials that used established or validated diagnostic criteria, including the Veldman criteria (Veldman 1993), the International Association for the Study of Pain (IASP) criteria (Merskey 1994), Bruehl criteria (Bruehl 1999), Budapest criteria (Harden 2010), and Atkins criteria (Atkins 2010), as well as studies that either predate these criteria or use non‐standard diagnostic criteria.
Types of interventions
We included all randomised controlled comparisons of physiotherapy interventions, employed in either a stand‐alone fashion or in combination, compared with placebo, no treatment, another intervention or usual care, or of varying physiotherapy interventions compared with each other, which were aimed at treating pain or disability, or both, associated with CRPS. We included trials in which non‐physiotherapists (e.g. occupational therapists) delivered such physiotherapy interventions, as defined in Description of the intervention, and reported the professional discipline of the clinician delivering the intervention. We did not pre‐define any specific comparisons in advance as physiotherapy interventions encompass a broad range of potential therapeutic approaches (e.g. various rehabilitation strategies or electrotherapy modalities). After the publication of our Cochrane protocol (Smart 2013), we decided to exclude studies that evaluated non‐physiotherapy based interventions (e.g. pharmacological) in which all arms received the same physiotherapy intervention (differing only in the application of the non‐physiotherapy component) as they are unlikely to offer any insight into the value of physiotherapy management (see Differences between protocol and review).
Types of outcome measures
Primary outcomes
Pain intensity as measured using a visual analogue scale (VAS), numerical rating scale (NRS), verbal rating scale or Likert scale.
Disability as measured by validated self‐report questionnaires/scales or functional testing protocols.
Secondary outcomes
We planned to analyse the following secondary outcome measures where such data were available:
Composite scores for CRPS symptoms.
Health‐related quality of life (HRQoL) using any validated tool.
Patient global impression of change (PGIC) scales.
Incidence/nature of adverse effects (AEs).
We excluded studies that did not measure the primary or secondary outcomes of interest described above.
Search methods for identification of studies
Electronic searches
For this update we identified relevant RCTs by electronically searching the following databases:
Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library, Issue 7 of 12, 2021;
MEDLINE (OVID) (1966 to 16 July 2021);
EMBASE (OVID) (1974 to 16 July 2021);
CINAHL (EBSCO) (1982 to July 2021);
PsycINFO (OVID) (1806 to July 2021);
LILACS (Bireme) (1982 to July 2021);
PEDro (1929 to July 2021);
Web of Science (ISI) (1945 to July 2021).
The Information Specialist of the Cochrane Pain, Palliative and Supportive Care Group devised the search strategies and added some extra terms to the strategies for this update. She and the review authors ran these searches. We used a combination of controlled vocabulary, i.e. medical subject headings (MeSH) and free‐text terms. The search strategies used for this update and the original review can be found in Appendix 1 and Appendix 2.
Searching other resources
Reference lists
On completion of the electronic searches we searched the reference lists of all eligible studies in order to identify additional relevant studies. In addition we screened the reference lists of previous systematic reviews (Bowering 2013; Daly 2009; O'Connell 2013; Smith 2005).
External experts
We sent the list of included trials to a content expert to help identify any additional relevant studies (November 2020).
Unpublished data
In order to minimise the impact of publication bias we searched the following registers and databases to identify unpublished research as well as research in progress (July to August 2021):
OpenGrey (System for Information on Grey Literature in Europe);
ProQuest Dissertations & Theses Global (formerly Dissertation Abstracts (ProQuest));
National Research Register Archive;
Health Services Research Projects in Progress;
Current Controlled Trials Register (incorporating the meta‐register of controlled trials and the International Standard Randomised Controlled Trial Number);
ClinicalTrials.gov;
International Clinical Trials Registry Platform;
Pan African Clinical Trials Registry;
EU Clinical Trials Register.
Data collection and analysis
Selection of studies
Two review authors (KMS and BMW in the original review and KMS and MCF in this updated review) independently assessed the titles and abstracts of studies we identified by the search strategy for eligibility. If the eligibility of a trial was unclear from the title and abstract, we assessed the full‐text article. We obtained potentially relevant studies identified in the first round of screening in full text and independently assessed these for inclusion using the same process outlined above. We excluded trials that did not match the inclusion criteria (see the Criteria for considering studies for this review section). We resolved any disagreements between review authors regarding a study's inclusion by discussion. If we could not resolve disagreements, a third review author (NOC) assessed relevant studies and we made a majority decision. Trials were not anonymised prior to assessment. We did not apply any language restrictions.
Data extraction and management
Two review authors (KMS and BMW in the original review and KMS and MCF in this updated review) independently extracted data from all included trials. We extracted data using a standardised and piloted form. We resolved any discrepancies and disagreements by consensus. In cases where we could not achieve consensus, a third review author (NOC) assessed the trial and we took a majority decision. We extracted the following data from each included trial:
country of origin;
study design;
study population (including diagnosis, diagnostic criteria used, symptom duration, age range, gender split);
type of noxious initiating event: surgery, fracture, crush injury, projectile, stab injury, other or no event;
type of tissue injured: nerve, soft tissue, bone;
presence of medico‐legal factors (that may influence the experience of pain and the outcomes of therapeutic interventions);
concomitant treatments that may affect outcome: medication, procedures etc.;
sample size: active and control/comparator groups;
intervention (including type, parameters (e.g. frequency, dose, duration), setting and professional discipline of the clinician delivering the therapy);
type of placebo/comparator intervention;
outcomes (primary and secondary) and time points assessed;
adverse effects;
author conflict of interest statements and study funding source;
assessment of risk of bias.
Assessment of risk of bias in included studies
We assessed the overall risk of bias for each included trial on the basis of an evaluation of key domains using a modified version of the Cochrane risk of bias assessment tool. We classified risk of bias as either 'low' (low risk of bias for all key domains), 'unclear' (unclear risk of bias for one or more key domains) or 'high' (high risk of bias for one or more key domains) (items 1 to 8 and 11 below), as outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We also considered experimental design‐specific (e.g. cross‐over study designs) risk of bias issues where appropriate (Higgins 2011b). We also evaluated included trials for the additional sources of bias associated with sample size and duration of follow‐up, as recommended by Moore 2010 (items 9 and 10 below). Small studies are more prone to bias because of their inherent imprecision and due to the effects of publication biases (Dechartres 2013; Moore 2012; Nüesch 2010). Inadequate length of follow‐up may produce an overly positive view of the true clinical effectiveness of interventions, particularly in persistent conditions (Moore 2010). These additional criteria were not considered 'key domains' and therefore did not inform judgements of a trial's overall risk of bias. We assessed the following key and non‐key domains of risks of bias for each included trial using either 'low', 'unclear' or 'high' judgements according to the following criteria:
Random sequence generation (checking for possible selection bias). We assessed the method used to generate the allocation sequence as either: low risk of bias (any truly random process, e.g. random number table; computer random number generator); unclear risk of bias (method used to generate sequence not clearly stated); or high risk of bias (studies on closer inspection using a quasi/non‐random process, e.g. odd or even date of birth; hospital or clinic record number).
Allocation concealment (checking for possible selection bias). The method used to conceal allocation to group prior to assignment determines whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment. We assessed the methods used as: low risk of bias (e.g. telephone or central randomisation; consecutively numbered, sealed, opaque envelopes); unclear risk of bias (method not clearly stated); or high risk of bias (studies that do not adequately conceal allocation, e.g. open list).
Blinding of study participants and personnel (checking for possible performance bias). We assessed the methods used to blind participants and care providers as either: low risk of bias (participants and care providers blinded to allocated intervention and unlikely that blinding broken; or no/incomplete blinding but judged that both intervention arms reflect active interventions of relatively equal credibility delivered with equal enthusiasm); unclear risk of bias (insufficient information provided to permit a judgement of low/high risk of bias); or high risk of bias (participants and care providers not blinded to the allocated intervention and interventions are clearly identifiable as control and experimental; or participants and care providers blinded to the allocated intervention but likely that blinding was broken).
Blinding of outcome assessment (self‐reported outcomes) (checking for possible detection bias). We assessed the methods used to blind study participants self‐reporting outcomes (e.g. pain severity) from knowledge of which intervention a participant received. We assessed the methods as either: low risk of bias (participants blinded to allocated intervention and unlikely that blinding broken; or no/incomplete blinding but judged that both intervention arms reflect active interventions of relatively equal credibility delivered with equal enthusiasm); unclear risk of bias (insufficient information provided to permit a judgement of low/high risk of bias); or high risk of bias (participants not blinded to the allocated intervention and interventions are clearly identifiable as control and experimental; or participants blinded to the allocated intervention but likely that blinding was broken).
Blinding of outcome assessment (investigator‐administered outcomes) (checking for possible detection bias). We assessed the methods used to blind researchers undertaking outcome assessments (e.g. functional testing protocols) from knowledge of which intervention a participant received. We assessed the methods as at either: low risk of bias (researchers blinded to allocated intervention and unlikely that blinding broken); unclear risk of bias (insufficient information provided to permit a judgement of low/high risk of bias); high risk of bias (researchers not blinded to the allocated intervention; or researcher blinded to the allocated intervention but likely that blinding was broken).
Incomplete outcome data (dropout) (checking for possible attrition bias). We first assessed for risk of attrition bias by evaluating participant dropout rates according to judgements based on the following criteria: low risk of bias (less than 20% dropout and appears not to be systematic, with numbers for each group and reasons for dropout reported); unclear risk of bias (less than 20% dropout but appears to be systematic or numbers per group and reasons for dropout not reported); high risk of bias (greater than or equal to 20% dropout).
Incomplete outcome data (method of analysis) (participants analysed in the group to which they were allocated) (checking for possible attrition bias). We further assessed for risk of attrition bias by separately evaluating the appropriateness of the method of analysis employed, using the following criteria: low risk of bias (participants analysed in the group to which they were allocated (intention‐to‐treat (ITT) or as an available case analysis); unclear risk of bias (insufficient information provided to determine if analysis was based on the principle of ITT or per protocol); or high risk of bias (if per protocol analysis used or where available data is not analysed or participant data were included in a group to which they were not originally assigned to).
Selective reporting (checking for possible reporting bias). We assessed studies for selective outcome reporting using the following judgements: low risk of bias (study protocol available and all pre‐specified primary outcomes of interest adequately reported or study protocol not available but all expected primary outcomes of interest adequately reported or all primary outcomes numerically reported with point estimates and measures of variance for all time points); unclear risk of bias (insufficient information provided to permit a judgement of low/high risk of bias); or high risk of bias (incomplete reporting of pre‐specified primary outcomes or point estimates and measures of variance for one or more primary outcome not reported numerically (e.g. graphically only) or one or more primary outcomes reported using measurements, analysis methods or subsets of data that were not pre‐specified or one or more reported primary outcomes were not pre‐specified or results for a primary outcome expected to have been reported were excluded).
Sample size (checking for possible biases confounded by small sample size): we assessed trials as being at low risk of bias (greater than or equal to 200 participants per treatment arm); unclear risk of bias (50 to 199 participants per treatment arm); high risk of bias (less than 50 participants per treatment arm).
Duration of follow‐up (checking for possible biases confounded by a short duration of follow‐up): we assessed trials as being at low risk of bias (follow‐up of greater than or equal to eight weeks); unclear risk of bias (follow‐up of two to seven weeks); or high risk of bias (follow‐up of less than two weeks).
Other bias. We assessed studies for other potential sources of bias. We determined judgements regarding low/unclear/high risk of bias according to the potential confounding influence of identified factors, for example: low risk of bias (appears free of other potentially serious sources of bias e.g. no serious study protocol violations identified); unclear risk of bias (other sources of bias may be present but there is either insufficient information to assess whether an important risk of bias exists or insufficient rationale or evidence regarding whether an identified problem will introduce bias); or high risk of bias (results may have been confounded by at least one potentially serious risk of bias, e.g. a significant baseline imbalance between groups; a serious protocol violation; use of 'last observation carried forward' when dealing with missing data).
Two review authors (KMS and BMW in the original review and KMS and MCF in this updated review) independently undertook the risk of bias assessments, and resolved any disagreements by discussion. If they could not reach an agreement, a third review author (NOC) undertook a risk of bias assessment and we took a majority decision.
Measures of treatment effect
We expressed the size of treatment effect on pain intensity, as measured with a VAS or NRS, using the mean difference (MD) (where all studies utilised the same measurement scale) or the standardised mean difference (SMD) (where studies used different scales) based on the approach described in the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011). Effect sizes were also expressed as a proportion of average baseline values. In order to aid interpretation of the pooled effect size we planned to back‐transform the SMD value to a 0 to 100 mm VAS format on the basis of the mean standard deviation (SD) from trials using a 0 to 100 mm VAS where possible.
We presented and analysed primary outcomes as change on a continuous scale or in a dichotomised format as the proportion of participants in each group who attained a predetermined threshold of improvement. For example, we judged cut‐points from which to interpret the likely clinical importance of (pooled) effect sizes according to provisional criteria proposed in the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) consensus statement (Dworkin 2008). Specifically, we judged reductions in pain intensity compared with baseline as follows:
less than 15%: 'no important change';
15% or more: 'minimally important change';
30% or more: 'moderately important change';
50% or more: 'substantially important change'.
We planned to use the cut‐points for 'minimally', 'moderately' and 'substantially’ important changes to generate dichotomous outcomes, the effect size for which we would have expressed as the risk ratio (or relative risk (RR)) but a lack of data did not permit any such analyses.
The IMMPACT thresholds are based on estimates of the degree of within‐person change from baseline that participants might consider clinically important. In a change to our original protocol (Smart 2013) and systematic review (Smart 2016), we extended our interpretation of changes in outcomes to include between‐group differences (see Differences between protocol and review). There is little consensus or evidence regarding cut‐points from which to interpret the magnitude of clinically important differences in pain intensity (or other patient‐related outcome measures) based on the between‐group difference post‐intervention (Dworkin 2009). For the purpose of this systematic review we adopted the recommendations of the OMERACT 12 group, with a threshold of 10 mm on a 0 mm to 100 mm VAS as being the threshold for minimal importance for average between‐group change (Busse 2015). Busse 2015 also suggests some more nuanced interpretations of between‐group changes, with pooled estimates of i) ≥ 2.0 units suggesting a large treatment effect, ii) 1.0 to 1.9 suggesting an important effect, iii) 0.5 to 1.0 suggesting the treatment may benefit an appreciable number of patients, and iv) ≤ 0.5 suggesting a small to very small effect. We interpreted our estimates of treatment effect according to these thresholds but did so appropriately and cautiously.
We planned to present secondary outcomes as change on a continuous scale or in a dichotomised format but a lack of data did not permit any such analyses.
We analysed the data using Review Manager (RevMan) (RevMan 2014). We plotted the results of each RCT with available data as point estimates with corresponding 95% CIs and displayed them using forest plots. If included trials demonstrated clinical homogeneity we performed a meta‐analysis to quantify the pooled treatment effect sizes using a random‐effects model. We did not perform a meta‐analysis when clinical heterogeneity was present. Similarly we presented secondary outcomes, though we did not consider them for meta‐analysis.
Unit of analysis issues
All included trials randomised participants at the individual participant level. We planned to meta‐analyse estimates of treatment effect (and their standard errors (SE)) from cluster‐RCTs employing appropriate statistical analyses using the generic inverse‐variance method in RevMan (RevMan 2014), as suggested in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). Where we considered such trials to have employed inappropriate analyses, we planned to utilise methods for 'approximately correct analysis' where possible (Higgins 2011b). In addition, we planned to enter cross‐over trials into a meta‐analysis when it was clear that data were free from carry‐over effects, and to combine the results of cross‐over trials with those of parallel trials by imputing the post‐treatment between‐condition correlation coefficient from an included trial that presented individual participant data and use this to calculate the SE of the SMD. These data may be entered into a meta‐analysis using the generic inverse‐variance method (Higgins 2011b).
Dealing with missing data
We attempted to contact the authors of included trials when numerical data were unreported or incomplete. If trial authors only presented data in graphical form, we did not attempt to extract the data from the figures. If SD values were missing from follow‐up assessments but were available at baseline, we used these values as estimates of variance in the follow‐up analyses.
Assessment of heterogeneity
We evaluated the included trials for clinical homogeneity regarding study population, treatment procedure, control intervention, timing of follow‐up and outcome measurement. For trials that were sufficiently clinically homogenous to pool, we formally explored heterogeneity using the Chi² test to investigate the statistical significance of any heterogeneity, and the I² statistic to estimate the amount of heterogeneity. We interpreted I2 values according to the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011):
0% to 40%: heterogeneity might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity.
Assessment of reporting biases
We planned to test for the possible influence of publication bias on trials that utilised dichotomised outcomes by estimating the number of participants in trials with zero effect required to change the number needed to treat (NNT) to an unacceptably high level (defined as an NNT of 10), as outlined by Moore 2008. An absence of relevant data meant that we did not undertake any analyses. Instead, we considered the possible influence of small study/publication biases on review findings as part of our risk of bias assessment (see the Assessment of risk of bias in included studies section) and as part of our Grading of Recommendations Assessment, Development and Evaluation (GRADE) assessments of the certainty of evidence (see the Data synthesis section) (Guyatt 2011a). We may include such analyses in future updates of this Cochrane Review where relevant data are available.
Data synthesis
Where possible, we grouped extracted data according to diagnosis (CRPS types I or II, or mixed), intervention, outcome (i.e. pain, disability) and duration of follow‐up (short‐term: zero to less than two weeks post intervention; mid‐term: two to seven weeks post intervention; and long‐term: eight or more weeks post intervention). Regarding intervention, we planned to pool data from trials that investigated the same single therapy separately for each therapy. We planned to pool trials of multimodal physiotherapy programmes together.
For all analyses, we report the outcome of the risk of bias assessments. Where we found inadequate data to support statistical pooling, we performed a narrative synthesis of the evidence.
Subgroup analysis and investigation of heterogeneity
Where significant heterogeneity (P value < 0.1) was present, we planned to explore subgroup analyses (see the Differences between protocol and review section). We planned to perform subgroup analyses based on the type of CRPS (i.e. I, II or mixed) and its temporal characteristics (i.e. acute (defined as symptoms and signs of CRPS of zero to 12 weeks duration) and chronic (symptoms and signs of CRPS lasting 13 weeks)). However, we did not undertake them due to the insufficient number of included trials.
Sensitivity analysis
We planned to conduct a sensitivity analysis based on risk of bias (investigating the influence of excluding studies classified at high risk of bias).
Summary of findings and assessment of the certainty of the evidence
We conducted a qualitative analysis of all trial findings and used the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach to assess and rank the certainty of evidence (Guyatt 2011a; Guyatt 2011b).
To ensure consistency of GRADE judgements we applied the following assessment criteria:
Serious study limitations: we downgraded once if more than 25% of the participants were from trials we classified as being at overall high risk of bias, as described in the Assessment of risk of bias in included studies section.
Inconsistency: we downgraded once if heterogeneity was statistically significant and the I² statistic value was greater than 40%. When a meta‐analysis was not performed we downgraded once if the trials did not show effects in the same direction.
Indirectness: we downgraded once if more than 50% of the participants were outside the target group.
Imprecision: we downgraded once if there were fewer than 400 participants for continuous data and fewer than 300 events for dichotomous data.
Publication bias: we downgraded once where there was direct evidence of publication bias or if estimates of effect based on small‐scale, industry‐sponsored studies raised a high index of suspicion of publication bias.
Two review authors (KMS and MCF) made the judgement of whether these factors were present or not. We considered single trials to be inconsistent and imprecise, unless more than 400 participants were randomised for continuous outcomes or more than 300 for dichotomous outcomes. We applied the following definitions regarding the certainty of the evidence (Balshem 2011):
High: we are very confident that the true effect lies close to that of the estimate of the effect.
Moderate: we are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low: our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect.
Very low: we have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect.
Summary of findings table
At the time of protocol development we did not specify any key comparisons of interventions (Smart 2013). In light of the wide range of trial interventions identified and the very limited data available we have taken the post hoc decision to present summary of findings tables for our primary outcomes of pain and disability, together with adverse effects, for the comparisons 'Physiotherapy compared to minimal care for adults with CRPS I and CRPS II' and included trials that delivered what we determined to be conventional multimodal physiotherapy, reflective of common clinical practice (Miller 2019).
We have not presented summary of findings tables for all identified comparisons of interventions as these are, we judge, too numerous, most often involving single trials with small samples and minimal to no data presented, and therefore of limited clinical use. However, we have considered the findings from all included trials with respect to all our outcomes of interest in full in the Effects of interventions section.
Results
Description of studies
See the Characteristics of included studies and Characteristics of excluded studies.
Results of the search
Our updated search period extended from February 2015, the time point up to which our original search was conducted, to July 2021. We identified 634 records from the database searches and one additional record from an author whom we contacted with a query. After de‐duplication (n = 149) we screened 486 abstracts from which we assessed 38 full‐text articles for eligibility. A total of 16 studies met our inclusion criteria (see Characteristics of included studies table). We have presented a flow diagram outlining the trial screening and selection process (Figure 1).
1.
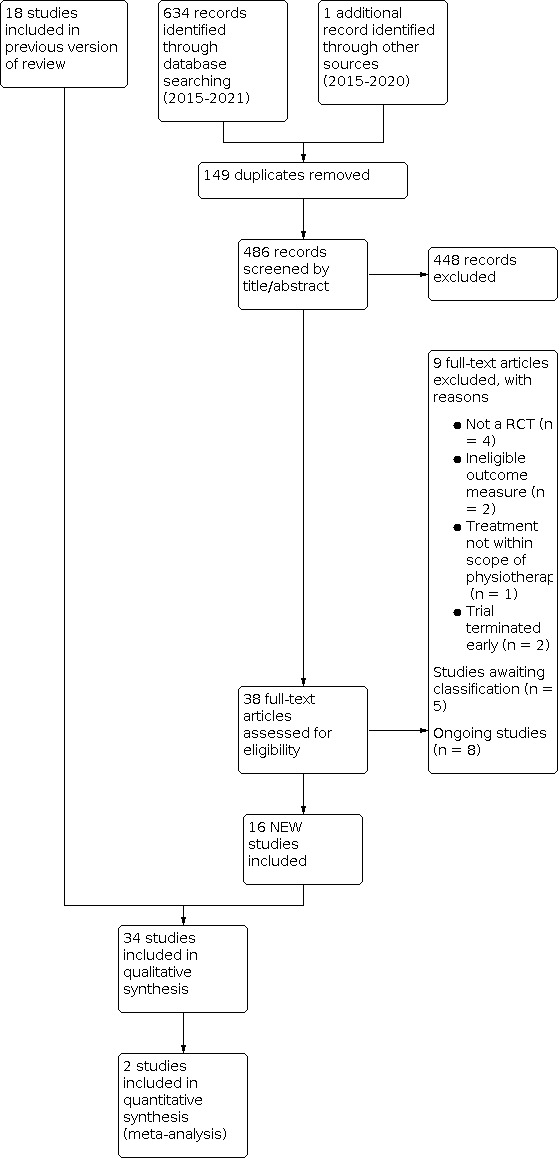
Study flow diagram.
We combined the 16 trials (600 participants) identified in our updated literature search with the 18 trials (739 participants) included within our original review (Smart 2016). From the combined total of 1230 records screened and 80 full‐text reviews across the two searches, we included 34 trials involving 1339 participants in this review.
Included studies
We included 34 trials in this review, 18 from the original review (Smart 2016) (Askin 2014; Aydemir 2006; Cacchio 2009a; Cacchio 2009b; Dimitrijevic 2014; Duman 2009; Durmus 2004; Hazneci 2005; Jeon 2014; Li 2012; Moseley 2004; Moseley 2005; Moseley 2006; Moseley 2009; Mucha 1992; Oerlemans 1999; Schreuders 2014; Uher 2000), and 16 from the updated searches (Barnhoorn 2015; Benedetti 2018; Bilgili 2016; Bϋyϋkturan 2018; den Hollander 2016; Devrimsel 2015; Halicka 2021; Hwang 2014; Lewis 2021; Ozcan 2019; Ryan 2017; Saha 2021; Sarkar 2017; Strauss 2021; Topcuoglu 2015; Vural 2016). We have provided the details of all included trials in the Characteristics of included studies table.
In our original review we contacted 10 authors for missing data (Cacchio 2009b; Jeon 2014; Moseley 2004; Moseley 2005; Moseley 2006; Moseley 2009; Mucha 1992; Oerlemans 1999; Schreuders 2014; Uher 2000). One trial author responded and supplied data for an outcome measure of 'impairment' but we were unable to extract outcome data linked to 'pain intensity' from the supplied data (Oerlemans 1999). One trial author responded, stating that they were unable to supply the relevant data (Schreuders 2014). There was no response from the other trial authors we had contacted. In this updated review, we contacted 10 authors for missing data (den Hollander 2016; Halicka 2021; Hwang 2014; Lewis 2021; Ozcan 2019; Ryan 2017; Sarkar 2017; Strauss 2021; Topcuoglu 2015; Vural 2016). Five authors supplied missing data (den Hollander 2016; Halicka 2021; Ryan 2017; Sarkar 2017; Strauss 2021). One author replied to report that they did not have the data (Vural 2016). One author replied indicating that they would look into our request but did not subsequently supply the data (Ozcan 2019). There was no response from the remaining three authors (Hwang 2014; Lewis 2021; Topcuoglu 2015).
Design
All included trials were RCTs, and 32 essentially used a parallel‐group design. Whilst the selected participants in three trials crossed over from comparator to intervention groups (Cacchio 2009b; Moseley 2004; Mucha 1992), none employed a true randomised cross‐over design and we analysed them up to the point of cross‐over as parallel‐group designs. Two trials employed a within‐subject randomised cross‐over design (Moseley 2009; Strauss 2021). The majority of included trials (26 out of 34) included two intervention arms, seven trials included three arms (Askin 2014; Aydemir 2006; Cacchio 2009b; Hwang 2014; Moseley 2005; Oerlemans 1999; Sarkar 2017), and one study used four arms (Moseley 2009). No cluster‐RCTs met the inclusion criteria of this Cochrane Review.
Setting
Trials were undertaken across a range of geographical locations including: Turkey (n = 11); Australia and the Netherlands (n = 4 each); Germany, Italy and the United Kingdom (n = 3 each), India and South Korea (n = 2 each); China, India and Serbia (n = 1 each). Three (9%) were multi‐centre trials (Halicka 2021; Lewis 2021; Oerlemans 1999), nine (28%) trials did not report whether they were single‐ or multi‐centre (Cacchio 2009b; Devrimsel 2015; Duman 2009; Moseley 2005; Moseley 2006; Moseley 2009; Mucha 1992; Schreuders 2014; Uher 2000), and the remaining 22 (65%) were all single‐centre trials.
Participants
The 34 trials included a total of 1339 participants and the total number of participants per trial ranged from eight (Ryan 2017) to 135 (Oerlemans 1999). Thirty trials included participants with CRPS I using a range of diagnostic criteria, most commonly using those of Bruehl 1999 and Harden 2007; Harden 2010. One trial included participants with CRPS II (Strauss 2021) and one trial included participants with CRPS type I and II but did not report the numbers with each type (Hwang 2014). Two trials did not specify the type of CRPS for their participants (Lewis 2021; Sarkar 2017).
Twenty‐four trials included participants with CRPS I of the upper limb (Askin 2014; Aydemir 2006; Bilgili 2016; Bϋyϋkturan 2018; Cacchio 2009a; Cacchio 2009b; Devrimsel 2015; Duman 2009; Durmus 2004; Halicka 2021; Hazneci 2005; Lewis 2021; Li 2012; Moseley 2004; Moseley 2005; Moseley 2009; Mucha 1992; Oerlemans 1999; Ozcan 2019; Ryan 2017; Saha 2021; Schreuders 2014; Topcuoglu 2015; Vural 2016), seven with either upper or lower limb CRPS I (Barnhoorn 2015; Benedetti 2018; den Hollander 2016; Dimitrijevic 2014; Hwang 2014; Moseley 2006; Sarkar 2017), one with CRPS I of the lower limb (Uher 2000) and one trial included participants with either upper, lower, multi‐limb or whole body CRPS I (Jeon 2014). In the trials where the type of CRPS was not specified, one study included participants with upper limb CRPS (Lewis 2021) and one included participants with upper and lower limb CRPS (Sarkar 2017). Participants developed CRPS I linked to a range of aetiologies including onset post fracture, soft‐tissue injuries, stroke, surgery, carpal tunnel syndrome as well as of idiopathic onset.
Participants had acute symptoms (less than or equal to three months) of CRPS I in eight trials (Bϋyϋkturan 2018; Cacchio 2009a; Devrimsel 2015; Dimitrijevic 2014; Durmus 2004; Hazneci 2005; Li 2012; Mucha 1992), chronic symptoms (greater than three months) in 14 trials (Barnhoorn 2015; den Hollander 2016; Duman 2009; Halicka 2021; Hwang 2014; Jeon 2014; Lewis 2021; Moseley 2004; Moseley 2005; Moseley 2006; Moseley 2009; Ryan 2017; Saha 2021; Schreuders 2014), and a mix of acute and chronic symptoms in six trials (Askin 2014; Benedetti 2018; Oerlemans 1999; Sarkar 2017; Topcuoglu 2015; Vural 2016). Five trials involving participants with CRPS I did not report the duration of symptoms (Aydemir 2006; Bilgili 2016; Cacchio 2009b; Ozcan 2019; Uher 2000). Participants had chronic symptoms in the one trial involving those with CRPS II (Strauss 2021).
Interventions and comparators
We have provided a detailed description of the interventions delivered in each included trial in the Characteristics of included studies table. The types of physiotherapy interventions delivered were heterogeneous across the included trials and included various electro‐physical modalities (ultrasound, TENS, laser, interferential therapy, pulsed electromagnetic field therapy, whirlpool baths, neuromuscular electrical stimulation, fluidotherapy, contrast baths), cortically‐directed sensory‐motor rehabilitation strategies (GMI, mirror therapy, virtual body swapping, tactile sensory discrimination training, prism adaptation treatment), exercise (active, active‐assisted, passive, stretching, strengthening, mobilising, functional; supervised and unsupervised), cognitive‐behavioural interventions ('exposure‐based' strategies), manual lymphatic drainage (MLD) and pain management advice. Twelve trials evaluated electro‐physical modalities (Askin 2014; Aydemir 2006; Benedetti 2018; Bilgili 2016; Bϋyϋkturan 2018; Devrimsel 2015; Dimitrijevic 2014; Durmus 2004; Hazneci 2005; Mucha 1992; Ozcan 2019; Ryan 2017), 15 trials evaluated cortically‐directed sensory‐motor rehabilitation strategies (Cacchio 2009a; Cacchio 2009b; Halicka 2021; Hwang 2014; Jeon 2014; Lewis 2021; Moseley 2004; Moseley 2005; Moseley 2006; Moseley 2009; Saha 2021; Sarkar 2017; Schreuders 2014; Strauss 2021; Vural 2016), three trials evaluated aerobic exercise or general rehabilitation therapies (Li 2012; Oerlemans 1999; Topcuoglu 2015), two trials evaluated MLD (Duman 2009; Uher 2000) and two trials evaluated cognitive‐behavioural/exposure‐based interventions (Barnhoorn 2015; den Hollander 2016). Eleven trials directly compared an active and placebo intervention (Askin 2014; Aydemir 2006; Benedetti 2018; Bilgili 2016; Bϋyϋkturan 2018; Cacchio 2009a; Cacchio 2009b; Durmus 2004; Halicka 2021; Lewis 2021; Ryan 2017), and 22 trials compared the experimental intervention to an active comparator. Of these, 11 trials compared the experimental intervention to 'conventional treatment' (Barnhoorn 2015; den Hollander 2016; Duman 2009; Li 2012; Moseley 2004; Moseley 2006; Ozcan 2019; Saha 2021; Schreuders 2014; Topcuoglu 2015; Vural 2016), and 11 trials compared the experimental intervention to various other active comparators (Devrimsel 2015; Dimitrijevic 2014; Hazneci 2005; Hwang 2014; Jeon 2014; Moseley 2005; Moseley 2009; Mucha 1992; Oerlemans 1999; Sarkar 2017; Uher 2000). One cross‐over trial compared the experimental intervention to a waiting list control (Strauss 2021).
Excluded studies
We excluded nine full‐text trial reports from the updated searches, in addition to the 13 excluded from the original review, because they were not RCTs (n = 4), investigated outcome measures that were not of interest (n = 2), were terminated early (n = 2) or tested interventions that fell outside the scope of physiotherapy (n = 1) (see Characteristics of excluded studies).
Studies awaiting classification
Eight trials are awaiting classification (see Characteristics of studies awaiting classification). At the time the searches for the current review update were undertaken (July 2021) four trials had only been published as conference abstracts (Dimitrijevic 2019; Dimitrijevic 2020; Mallikarjunaiah 2015; Patru 2017). We were unable to make contact with the authors of three trials to ascertain their status (ISRCTN39729827; ISRCTN97144266; NCT01944150) and one trial had been delayed (UKCRN ID 12602).
Ongoing studies
We identified seven potentially relevant ongoing studies that are either completed and being analysed (NCT03377504; NCT03887962), ongoing (NCT02395211; NCT02753335), delayed (JPRN‐UMIN000029801), or whose progress is unknown (ChiCTR1900020835; CTRI/2019/01/017272) (see Characteristics of ongoing studies).
Risk of bias in included studies
We have summarised risk of bias results for all included trials in Figure 2 and Figure 3. We judged the overall risk of bias, based on evaluations of key domains (i.e. random sequence generation, allocation concealment, blinding of study participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias) as being 'high' for 27 trials (Askin 2014; Barnhoorn 2015; Bilgili 2016; Bϋyϋkturan 2018; Cacchio 2009b; den Hollander 2016; Dimitrijevic 2014; Duman 2009; Halicka 2021; Jeon 2014; Lewis 2021; Li 2012; Moseley 2004; Moseley 2005; Moseley 2006; Moseley 2009; Mucha 1992; Oerlemans 1999; Ozcan 2019; Ryan 2017; Saha 2021; Sarkar 2017; Schreuders 2014; Strauss 2021; Topcuoglu 2015; Uher 2000; Vural 2016), and 'unclear' for seven trials (Aydemir 2006; Benedetti 2018; Cacchio 2009a; Devrimsel 2015; Durmus 2004; Hazneci 2005; Hwang 2014). We did not judge any of the included trials as having an overall 'low' risk of bias.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included trial.
Allocation
Random sequence generation
We judged 18 trials to be at low risk of bias as the methods used to generate the random sequence were adequately described (Aydemir 2006; Barnhoorn 2015; Benedetti 2018; den Hollander 2016; Dimitrijevic 2014; Durmus 2004; Halicka 2021; Lewis 2021; Li 2012; Moseley 2004; Moseley 2005; Moseley 2006; Oerlemans 1999; Ozcan 2019; Ryan 2017; Schreuders 2014; Topcuoglu 2015; Vural 2016), and 12 to be at unclear risk of bias because insufficient information was provided on the process for random sequence generation (Cacchio 2009a; Cacchio 2009b; Devrimsel 2015; Duman 2009; Hazneci 2005; Hwang 2014; Jeon 2014; Moseley 2009; Mucha 1992; Saha 2021; Strauss 2021; Uher 2000). Four trials used a quasi‐randomisation method and we judged these to be at high risk of bias (Askin 2014; Bilgili 2016; Bϋyϋkturan 2018; Sarkar 2017).
Allocation concealment
We judged 10 trials to be at low risk of bias because the methods for concealing allocation were adequately described (Barnhoorn 2015; den Hollander 2016; Dimitrijevic 2014; Lewis 2021; Li 2012; Moseley 2009; Ryan 2017; Saha 2021; Schreuders 2014; Uher 2000), and 24 to be at unclear risk of bias because insufficient information was provided about how allocation was concealed (Askin 2014; Aydemir 2006; Benedetti 2018; Bilgili 2016; Bϋyϋkturan 2018; Cacchio 2009a; Cacchio 2009b; Devrimsel 2015; Duman 2009; Durmus 2004; Halicka 2021; Hazneci 2005; Hwang 2014; Jeon 2014; Moseley 2004; Moseley 2005; Moseley 2006; Mucha 1992; Oerlemans 1999; Ozcan 2019; Sarkar 2017; Strauss 2021; Topcuoglu 2015; Vural 2016).
Blinding
Blinding of study participants and personnel
We judged 10 trials to be at low risk of bias where participants and personnel were adequately blinded to the intervention or where we considered a lack of blinding to have been unlikely to have biased trial outcomes (Askin 2014; Aydemir 2006; Benedetti 2018; Devrimsel 2015; Dimitrijevic 2014; Durmus 2004; Halicka 2021; Hazneci 2005; Lewis 2021; Moseley 2005), and five to be at unclear risk of bias where there was insufficient information provided to permit a judgement of low/high risk of bias (Bϋyϋkturan 2018; den Hollander 2016; Hwang 2014; Jeon 2014; Moseley 2009). We judged 19 trials to have a high risk of bias because of inadequate or a lack of blinding (Barnhoorn 2015; Bilgili 2016; Cacchio 2009a; Cacchio 2009b; Duman 2009; Li 2012; Moseley 2004; Moseley 2006; Mucha 1992; Oerlemans 1999; Ozcan 2019; Ryan 2017; Saha 2021; Sarkar 2017; Schreuders 2014; Strauss 2021; Topcuoglu 2015; Uher 2000; Vural 2016).
Blinding of outcome assessment (self‐reported outcomes)
We judged 12 trials to be at low risk of bias because they successfully blinded participants who self‐reported outcomes (Askin 2014; Aydemir 2006; Benedetti 2018; Bϋyϋkturan 2018; den Hollander 2016; Devrimsel 2015; Dimitrijevic 2014; Durmus 2004; Halicka 2021; Hazneci 2005; Lewis 2021; Moseley 2005), and three to be at unclear risk of bias where there was insufficient information provided to permit a judgement of low/high risk of bias (Hwang 2014; Jeon 2014; Moseley 2009). We judged 19 trials to have a high risk of bias because of inadequate or a lack of blinding of participants who self‐reported outcomes (Barnhoorn 2015; Bilgili 2016; Cacchio 2009a; Cacchio 2009b; Duman 2009; Li 2012; Moseley 2004; Moseley 2006; Mucha 1992; Oerlemans 1999; Ozcan 2019; Ryan 2017; Saha 2021; Sarkar 2017; Schreuders 2014; Strauss 2021; Topcuoglu 2015; Uher 2000; Vural 2016).
Blinding of outcome assessment (investigator‐administered outcomes)
We judged 20 trials to be at low risk of bias either because they successfully blinded outcome assessors or where the trialists did not employ any investigator‐administered outcomes (Askin 2014; Aydemir 2006; Barnhoorn 2015; Benedetti 2018; Cacchio 2009a; Cacchio 2009b; den Hollander 2016; Durmus 2004; Halicka 2021; Hwang 2014; Jeon 2014; Lewis 2021; Moseley 2004; Moseley 2006; Ozcan 2019; Ryan 2017; Sarkar 2017; Schreuders 2014; Uher 2000; Vural 2016). We judged 13 trials to be at unclear risk of bias where there was insufficient information provided to permit a judgement of low/high risk of bias (Bilgili 2016; Bϋyϋkturan 2018; Devrimsel 2015; Dimitrijevic 2014; Duman 2009; Hazneci 2005; Li 2012; Moseley 2005; Moseley 2009; Mucha 1992; Oerlemans 1999; Strauss 2021; Topcuoglu 2015). We judged one trial to have a high risk of bias because of a lack of blinding of investigator‐administered outcomes (Saha 2021).
Incomplete outcome data (dropout)
Eighteen trials either had no dropouts or a dropout rate of less than 20% and as such we judged them as having a low risk of attrition bias secondary to dropouts (Askin 2014; Barnhoorn 2015; Benedetti 2018; Bϋyϋkturan 2018; Cacchio 2009b; Duman 2009; Durmus 2004; Jeon 2014; Li 2012; Moseley 2004; Moseley 2005; Moseley 2006; Moseley 2009; Mucha 1992; Ozcan 2019; Topcuoglu 2015; Uher 2000; Vural 2016). In 11 trials the risk of attrition bias was unclear either because the dropout rate was not reported (Aydemir 2006; Bilgili 2016; Devrimsel 2015; Hazneci 2005; Hwang 2014; Sarkar 2017), or the dropout rate between groups was unequal or the reasons for dropouts were only partially explained and we were unsure of the impact on the trial's results (Cacchio 2009a; Dimitrijevic 2014; Lewis 2021; Oerlemans 1999; Strauss 2021). Five trials with overall dropout rates of ≥ 20% had a high risk of attrition bias (den Hollander 2016; Halicka 2021; Ryan 2017; Saha 2021; Schreuders 2014).
Incomplete outcome data (participants analysed in the group to which they were allocated)
We judged 13 trials (Barnhoorn 2015; Cacchio 2009a; Cacchio 2009b; den Hollander 2016; Duman 2009; Durmus 2004; Jeon 2014; Li 2012; Moseley 2004; Moseley 2006; Moseley 2009; Mucha 1992; Oerlemans 1999), 11 trials (Aydemir 2006; Benedetti 2018; Bilgili 2016; Bϋyϋkturan 2018; Devrimsel 2015; Hazneci 2005; Hwang 2014; Lewis 2021; Sarkar 2017; Topcuoglu 2015; Vural 2016), and 10 trials (Askin 2014; Dimitrijevic 2014; Halicka 2021; Moseley 2005; Ozcan 2019; Ryan 2017; Saha 2021; Schreuders 2014; Strauss 2021; Uher 2000), respectively as being at 'low', 'unclear' and 'high' risk of attrition bias as a consequence of their adopted method of analysis.
Selective reporting
Seventeen trials either adequately reported outcome data (Askin 2014; Aydemir 2006; Benedetti 2018; Bilgili 2016; Bϋyϋkturan 2018; Cacchio 2009a; Devrimsel 2015; Dimitrijevic 2014; Duman 2009; Hazneci 2005; Li 2012; Moseley 2006; Saha 2021), or the authors supplied missing data (Halicka 2021; Ryan 2017; Sarkar 2017; Strauss 2021), and we judged them as being at low risk of reporting bias. We judged reporting bias to be unclear in one trial (Barnhoorn 2015). We judged a total of 16 trials as being at high risk of reporting bias; nine trials because of inadequate or incomplete reporting of primary outcomes, or both (den Hollander 2016; Durmus 2004; Hwang 2014; Jeon 2014; Oerlemans 1999; Ozcan 2019; Topcuoglu 2015; Uher 2000; Vural 2016), and seven trials because the trial authors presented data in graphical format only, i.e. point estimates with measures of variance were not reported (Cacchio 2009b; Lewis 2021; Moseley 2004; Moseley 2005; Moseley 2009; Mucha 1992; Schreuders 2014).
Sample size
None of the included trials had intervention arms with 200 or more participants per treatment arm. One trial randomised 60 participants to each trial arm and we judged it as being at unclear risk of bias (Li 2012). The remaining 33 trials had fewer than 50 participants per trial arm and we judged them as being at high risk of bias.
Duration of follow‐up
Ten trials employed a follow‐up period of eight or more weeks and we judged them as being at low risk of bias (Barnhoorn 2015; Cacchio 2009a; den Hollander 2016; Duman 2009; Halicka 2021; Li 2012; Moseley 2005; Moseley 2006; Oerlemans 1999; Ryan 2017). Five trials reported a follow‐up period of two to seven weeks (Aydemir 2006; Benedetti 2018; Moseley 2004; Saha 2021; Schreuders 2014), and we judged these as being at unclear risk of bias. Nineteen trials employed a follow‐up period of less than two weeks and we judged them as being at high risk of bias based on this criterion (Askin 2014; Bilgili 2016; Bϋyϋkturan 2018; Cacchio 2009b; Devrimsel 2015; Dimitrijevic 2014; Durmus 2004; Hazneci 2005; Hwang 2014; Jeon 2014; Lewis 2021; Moseley 2009; Mucha 1992; Ozcan 2019; Sarkar 2017; Strauss 2021; Topcuoglu 2015; Uher 2000; Vural 2016).
Other potential sources of bias
We considered four trials to be at high risk of other potential sources of bias: one trial because of differences in descriptions of the trial design and specification of a primary outcome measure between the trial registration and the published trial report (Strauss 2021); one trial because of imbalanced numbers of participants in an already very small group (n = 8) and differences in engagement with a co‐intervention between groups (Ryan 2017); one trial because it did not report the baseline data of three participants excluded from the analysis and because of a likely highly significant baseline imbalance in duration of symptoms between groups (Schreuders 2014); and one trial because violations of the random sequence generation were permitted (Oerlemans 1999). We judged six trials to be at unclear risk of bias: one trial because 27% of patients switched between intervention arms (Barnhoorn 2015); one trial because it was published as a 'Letter to the Editor' and not as a full trial report (Cacchio 2009b); one trial because of baseline imbalances between groups with respect to gender and duration of pain (Hwang 2014); one trial because it did not report participants' baseline pain data (Jeon 2014); one trial because of uncertainty regarding the extent to which a carry‐over effect may have introduced bias in estimates of treatment effect (Moseley 2009); and one because it did not report participants' baseline demographics and characteristics (Sarkar 2017). The 23 other trials appeared to be free of other potential sources of bias.
Effects of interventions
See: Table 1 (Physiotherapy compared with minimal care for adults with CRPS I); Table 2 (Physiotherapy compared with minimal care for adults with CRPS II).
Physiotherapy versus occupational therapy or minimal care for CRPS I
One three‐arm trial with 135 participants, which we judged as being at 'high' risk of bias based on a number of criteria, compared a physiotherapy programme (pain management advice, relaxation exercises, connective tissue massage, transcutaneous electrical nerve stimulation (TENS) and exercise) plus medical treatment according to a fixed pre‐established protocol, to an occupational therapy programme (splinting, de‐sensitisation, functional rehabilitation) plus medical management and to, what we understand is, an attention control intervention, described as 'social work' (SW) (which included attention, advice) plus medical management in participants with CRPS I of the upper limb secondary to mixed aetiologies (Oerlemans 1999). The trial authors did not adequately report details regarding the nature of the interventions and did not standardise the number of treatment sessions given with the intensity and frequency of treatment adjusted to the individual needs of participants. The trial authors did not report the overall duration of the treatment periods for each trial group.
Physiotherapy versus occupational therapy
Pain
Numerical data (i.e. group means and standard deviations (SD) for each time point) for the four self‐reported measures of pain intensity (current pain, pain from effort of use of the affected extremity, least and worst pain experienced in the preceding week) were not reported and the trial authors have not provided these data. Consequently, no further analyses of these measures were possible and we could not determine effect sizes. However, according to the trial report there were no between‐group differences in pain at 12‐month follow‐up (very low‐certainty evidence).
Disability
Numerical data for measures of upper limb disability (Impairment Level Sum score, Radboud Skills Questionnaire, modified Greentest, Radboud Dexterity Test) were not reported and the trial authors have not provided these data. Consequently, no further analyses of these measures were possible and we could not determine effect sizes. However, according to the trial report there were no between‐group differences in disability at 12‐month follow‐up (very low‐certainty evidence).
Other outcomes
The trial authors did not report numerical data from other outcomes of interest, including measures of health‐related quality of life (HRQoL) (Sickness Impact Profile) and adverse effects although the authors state that there were no between‐group differences in well‐being at 12 months follow‐up (Oerlemans 1999) (very low‐certainty evidence).
Certainty of the evidence
We judged the certainty of evidence for outcomes of pain and disability to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether a multimodal physiotherapy intervention improves disability or pain compared to an occupational therapy intervention in the treatment of CRPS I of the upper limb.
Physiotherapy versus minimal care
Pain
According to the trial authors (Oerlemans 1999), physiotherapy was superior to minimal care for reducing pain according to all four measures of pain intensity (current pain, pain from effort of use of the affected extremity, least and worst pain experienced in the preceding week) at three months post‐recruitment, and for reducing pain from effort of use of the affected extremity at six months. However, there were no between‐group differences for any measure of pain intensity at 12 months follow‐up. Numerical data (i.e. group means and standard deviations (SD) for each time point) for the four self‐reported measures of pain intensity were not reported, and the trial authors did not provide these data. Consequently, no further analyses of these measures were possible and we could not determine effect sizes (very low‐certainty evidence).
Disability
Multimodal physiotherapy demonstrated a small between‐group improvement in disability at 12 months follow‐up compared to minimal care (Impairment Level Sum score, 5 to 50 scale (higher scores indicate greater disability); mean difference (MD) ‐3.7, 95% confidence interval (CI) ‐7.13 to ‐0.27, P = 0.03). Numerical data were not reported for other measures of disability (Radboud Skills Questionnaire, modified Greentest, Radboud Dexterity Test) or time points (six weeks, three months, six months), although the authors state that there were no between‐group differences at 12 months follow‐up (Oerlemans 1999) (very low‐certainty evidence).
Other outcomes
The trial authors did not report data on other outcomes of interest, including HRQoL (Sickness Impact Profile) and adverse effects although the authors state that there were no between‐group differences in HRQoL at 12 months follow‐up (Oerlemans 1999) (very low‐certainty evidence).
Certainty of the evidence
We judged the certainty of evidence for outcomes of pain and disability to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether a multimodal physiotherapy intervention improves disability or pain compared to a social work (control) intervention in the treatment of CRPS I of the upper limb (Table 1).
Physiotherapy versus minimal care for CRPS II
No trials found (Table 2).
Upper limb aerobic exercise and physiotherapy versus physiotherapy alone
Topcuoglu 2015 (n = 40) compared aerobic upper limb exercise, using arm crank ergometry, combined with CRPS‐specific (TENS, cold‐packs, massage, contrast baths) and stroke‐specific (various exercise approaches) physiotherapy to CRPS‐ and stroke‐specific physiotherapy alone in participants with post‐stroke upper limb CRPS I. We judged this trial as being at 'high' risk of bias on multiple domains.
Pain
The authors report between‐group differences in favour of upper limb aerobic exercise for shoulder pain (10 cm visual analogue scale (VAS)) (daytime: MD ‐1.9, 95% CI ‐3.23 to ‐0.57; P < 0.005; on movement: MD ‐1.7, 95% CI ‐2.95 to ‐0.45 ; P < 0.007) and wrist pain (daytime: MD ‐1.75, 95% CI ‐2.87 to‐0.63; P < 0.002; night‐time: MD ‐1.3, 95% CI ‐2.48 to‐0.12; P < 0.03, on movement: MD ‐2.05 95% CI ‐3.17 to ‐0.93 ; P < 0.003) immediately post‐intervention. There was no further follow‐up of participants. The trial authors did not report baseline numerical data for measures of pain intensity and they did not supply us with these data. Thus we were unable to perform any further analyses (very low‐certainty evidence).
Disability
The trial authors did not report numerical data on disability.
Other outcomes
The trial authors did not report data on adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence to be very low for pain, downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether upper limb aerobic exercise combined with physiotherapy improves pain in the very short term compared to physiotherapy alone in people with post‐stroke CRPS I.
Exposure‐based interventions versus usual physiotherapy
Two trials investigated the effects of contrasting approaches of 'exposure'‐based interventions (Barnhoorn 2015; den Hollander 2016). We did not pool trial data due to substantial differences in therapeutic rationale and the use of outcome measures for pain and function.
Pain exposure physical therapy versus usual physiotherapy
Barnhoorn 2015 compared the effect of 'Pain exposure physical therapy' (PEPT), whereby participants are directly exposed to painful movements and activities (through self‐massage, 'forced' use during activities of daily living, progressive loading exercises, education) and are instructed to ignore the pain, to a conventional 'pain‐contingent' approach (comprising of medication, mild exposure and exercise) in 56 participants with CRPS I of the upper or lower limb. The trial was at high risk of bias on multiple domains.
Pain
Barnhoorn 2015 reported that while both groups improved there was no clear evidence of a difference in pain intensity (1 to 10 VAS (higher scores indicating worse pain), MD 0.61, 95% CI ‐0.70 to 1.92) or in the trial's primary composite outcome measure of pain intensity, range of motion and skin temperature (Impairment Level Sum Score ‐ Restricted Version (ISS‐RV); 4 to 40 scale (higher scores indicate worse pain), MD 0.96, 95% CI ‐1.56 to 3.48) at nine‐month follow‐up (very low‐certainty evidence).
Disability
There were no between‐group differences in pain‐related upper limb disability (Disability of the Arm, Shoulder and Hand; Dutch Language version (DASH‐DLV); 0 to 100 scale (higher scores indicate greater disability), MD 6.47, 95% CI ‐5.97 to 18.90) or lower limb disability (Lower Limb Tasks Questionnaire; 0 to 40 scale (lower scores indicate greater disability), MD 5.11, 95% CI ‐0.45 to 10.68) at nine‐month follow‐up (very low‐certainty evidence).
Other outcomes
There were no between‐group differences in HRQoL (EuroQoL‐5D index (EQ‐5D); maximum 1 (higher scores indicate worse health), MD ‐0.01, 95% CI ‐0.10 to 0.08) at nine‐month follow‐up (very low‐certainty evidence). The authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for outcomes of pain, disability and HRQoL to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether a PEPT approach improves pain or disability compared to conventional treatment in people with CRPS I of the upper or lower limb.
Exposure in vivo versus usual physiotherapy
den Hollander 2016 compared the effect of an exposure intervention targeting pain‐related fear avoidance compared to a 'protective pain‐contingent' treatment as usual approach in 46 participants with CRPS I of the upper or lower limb and moderate to high pain‐related fear. The trial had a high risk of bias secondary to a high dropout rate, some discrepancies in reported outcomes between their published protocol and the trial report, selective reporting of secondary outcomes and a small sample size.
Pain
The authors report additional between‐group differences in favour of the exposure intervention, in reductions in pain intensity (Neuropathic Pain Scale; score range 0 to 10 (higher scores indicate worse pain)) post‐treatment (MD ‐2.04 95% CI ‐3.01 to ‐1.07; P = 0.001) and at six‐month follow‐up (MD ‐2.82, 95% CI ‐4.18 to ‐1.46; P = 0.001), equating to a 36.7% (95% CI 19.2% to 54.1%) and 50.7% (95% CI 26.3% to 75.25%) reduction in baseline pain levels respectively, equivalent to 'moderately important change' and 'substantially important change' respectively (very low‐certainty evidence).
Disability
den Hollander 2016 reported between‐group differences in favour of the exposure intervention, in reductions of self‐reported upper limb disability (Radboud Skills Questionnaire (RASQ), score range 0 to 5 (higher scores indicate greater disability)) post‐treatment (MD ‐1.08, 95% CI ‐1.60 to ‐0.56; P = 0.001) and at six‐month follow‐up (MD ‐1.30, 95% CI ‐1.69 to ‐0.92 ; P = 0.001), and reductions in self‐reported lower limb disability (Walking Ability Questionnaire (WAQ), score range 0 to 10 (higher scores indicate greater disability)) at six‐month follow‐up (MD ‐3.62, 95% CI ‐6.78 to ‐0.47; P = 0.02) but not at the post‐treatment time point (very low‐certainty evidence).
Other outcomes
The authors also report improvements in physical (SF36‐PCS, score range 0 to 100 (lower scores indicate worse physical health)) and emotional HRQoL (SF36‐MCS, score range 0 to 100 (lower scores indicate worse mental health)) at post‐treatment (SF36‐PCS: MD 25.93, 95% CI 15.92 to 35.91; P = 0.001; SF36‐MCS: MD 16.23, 95% CI 6.85 to 25.63; P = 0.001) and six‐month time points (SF36‐PCS: MD 22.64, 95% CI 10.15 to 35.13; P = 0.001; SF36‐MCS: MD 19.63, 95% CI 10.78 to 28.47; P = 0.001) in favour of the exposure intervention, equivalent to 64.9% (95% CI 39.8% to 89.9%), 29.9% (95% CI 11.1% to 42.5%), and 56.7% (95% CI 25.4% to 87.9%), 32.5% (95% CI 17.9% to 47.2%) consistent with a substantially important change in SF36‐PCS score and a moderately important change in SF36‐MCS score (very low‐certainty evidence). The authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for outcomes of pain, disability and HRQoL to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether an exposure in vivo approach targeting pain‐related fear avoidance improves disability, pain or health‐related quality of life compared to a conventional 'protective pain‐contingent' treatment as usual approach in people with CRPS I of the upper or lower limb at short‐ and long‐term follow‐up.
Cortically directed sensory‐motor rehabilitation strategies
Graded motor imagery (GMI)
We included five separate trials of GMI, all of which were small trials (13 to 37 participants) judged to be at 'high' risk of bias.
Graded motor imagery versus standard care
Two trials compared the same GMI protocol to control interventions of standard care (Moseley 2004; Moseley 2006) and one trial compared a different GMI protocol plus conventional treatment (occupational and therapy physiotherapy) to conventional treatment alone (Schreuders 2014).
Moseley 2004 (n = 13) compared a six‐week GMI programme (consisting of two weeks of limb laterality recognition followed by two weeks of imagined movements followed by two weeks of mirror‐box therapy) to 12 weeks of ongoing medical management and usual physiotherapy care in participants with longstanding CRPS I of the upper limb post wrist fracture. Moseley 2006 compared the same GMI programme to physical therapy and usual care in a combined cohort of 14 participants with phantom‐limb pain and 37 participants with CRPS I of the upper or lower limb of mixed aetiologies. Schreuders 2014 (n = 18) compared a different six‐week GMI programme (consisting of one week of limb laterality recognition, followed by one week of imagined movements, followed by four weeks of mirror‐box therapy) plus conventional care (physiotherapy and occupational therapy) to conventional care alone in participants with longstanding CRPS I of the upper limb (aetiology not reported).
Pain
Moseley 2004 reported an improvement in pain intensity, as measured by the Neuropathic Pain Scale (NPS; score range 0 to 10 (higher scores indicate worse pain)) at six weeks post‐treatment, in participants that received GMI compared to ongoing medical management. Moseley 2004 reported a number needed to treat (NNT) to obtain a 50% reduction in the NPS (total score) of three (95% CI 1.4 to 10.1). Moseley 2006 reported improvements in pain intensity, as measured by a 0 to 100 VAS (higher scores indicate worse pain) immediately post‐intervention and at six months post‐treatment for the combined cohort of participants with CRPS I and phantom limb pain. At six weeks post‐treatment, Schreuders 2014 found no between‐group differences on any measure of pain intensity (current, minimum or maximum over last three days).
Moseley 2004, Moseley 2006 and Schreuders 2014 presented data for changes in pain intensity graphically only and did not report numerical data (i.e. group means and standard deviation (SD) values at each time point) for measures of pain intensity. However, 0 to 100 VAS pain data at the post intervention time point were available from Moseley 2004 and the CRPS I participants in Moseley 2006 from a previous overview of systematic reviews of interventions for CRPS (O'Connell 2013). We used these data in this Cochrane Review with the authors' permission. Pooling of these results gave an effect size (mean difference) of ‐14.45 (95% CI ‐23.02 to ‐5.87; P = 0.001, 2 trials, 49 participants; Analysis 1.1) with no significant heterogeneity (I² = 29%). We expressed these data as a percentage of the mean baseline pain levels in the larger trial (58 out of 100), which equated to a 25% (95% CI 10% to 40%) reduction in baseline pain intensity at the end of the treatment period. Moseley 2004 presented outcomes at medium‐term follow‐up (six weeks post‐treatment, n = 13, MD ‐20.00, 95% CI ‐32.13 to ‐7.97; P = 0.001). This equated to an improvement of 34% (95% CI 14% to 55%) of the baseline VAS pain level in the Moseley 2006 trial (average baseline data for pain VAS were not available from the Moseley 2004 trial report). At long‐term follow‐up (six months post‐treatment (n = 36)) in Moseley 2006, the MD was ‐21.00, 95% CI ‐31.17 to ‐10.83; P < 0.001, which equates to an improvement of 36% (95% CI 19% to 54%). The immediate post‐treatment effect was below the threshold for a moderately clinically important difference but exceeded the threshold for a minimally clinically important difference. The medium‐ and long‐term effects met the threshold for a moderately important benefit (very low‐certainty evidence). We were unable to obtain numerical data from Schreuders 2014.
1.1. Analysis.

Comparison 1: Graded motor imagery versus standard care, Outcome 1: Pain intensity (0 to 100 VAS; higher scores indicate worse pain) (post‐treatment)
Disability
Moseley 2006 reported improvements in disability, as measured by a 0 to 10 patient‐specific functional scale (lower scores indicate greater disability), immediately post‐intervention and at six months post‐treatment for the combined cohort of participants with CRPS I and phantom limb pain. At six weeks post‐treatment, Schreuders 2014 found no between‐group differences in function. Moseley 2006 and Schreuders 2014 presented data for changes in disability graphically only and did not report the numerical data (i.e. group means and SD values at each time point). We were unable to obtain numerical data from Schreuders 2014.
As described above, we were able to pool the data on disability from two trials (Moseley 2004 and Moseley 2006; data on CRPS I participants only), which returned a MD of 1.87 (95% CI 1.03 to 2.71; P < 0.001; I² = 41%; 2 trials, 49 participants; Analysis 1.2) at the end of treatment; 2.26 (95% CI 1.42 to 3.10; P < 0.001) at medium‐term follow‐up (Moseley 2004, n = 13); and 2.30 (95% CI 1.12 to 3.48; P < 0.001) at long‐term follow‐up (Moseley 2006, n = 36). This represented a large improvement in function from the baseline function score (0.5) in the control group of the larger trial (Moseley 2006) (very low‐certainty evidence).
1.2. Analysis.

Comparison 1: Graded motor imagery versus standard care, Outcome 2: Disability (0 to 10 patient‐specific functional scale; higher scores indicate better function) (post‐treatment)
Other outcomes
None of these trials reported data about adverse effects or measured any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and disability to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether GMI improves pain or disability compared to standard care for people with CRPS I of the upper limb post wrist fracture or CRPS I of the upper or lower limb of mixed aetiologies at short‐, medium‐ or long‐term follow‐up.
Three graded motor imagery (GMI) protocols compared with each other
In a three‐arm trial, Moseley 2005 (n = 20) compared a six‐week GMI programme with its three components delivered in the 'correct’ order (i.e. two weeks of laterality recognition followed by two weeks of imagined movements followed by two weeks of mirror‐box therapy) to two other GMI programmes with selected components delivered in different orders at odds with its hypothesised mechanism of action, in participants with longstanding CRPS I of the upper limb post wrist fracture.
Pain
Improvements were found in pain intensity in the correctly ordered GMI group compared to both comparison groups, as measured by the NPS at 12 weeks post‐treatment. Moseley 2005 reported that at 12‐week follow‐up, the mean reduction in NPS score for the correctly ordered GMI group was approximately seven and 18 points greater than the mean reductions in the other two groups respectively. The trial did not report numerical data for the outcome of pain intensity and we have been unable to obtain these data from the trial author. Consequently we were unable to perform any further analyses of these measures and we could not determine the effect sizes (very low‐certainty evidence).
Disability
Improvements were found in function in the correctly ordered GMI group compared to both comparison groups, as measured by an 11‐point NRS at 12 weeks post‐treatment. The trial did not report numerical data for the outcome of function, and we have been unable to obtain these data from the trial author. Consequently we were unable to perform any further analyses of these measures and we could not determine the effect sizes (very low‐certainty evidence).
Other outcomes
The trial did not report data concerning adverse effects and did not measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and disability to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether appropriately ordered GMI was more effective at reducing pain and improving disability than inappropriately ordered GMI in people with longstanding CRPS I of the upper limb post wrist fracture.
Graded Motor Imagery versus waiting list control
One two‐arm, two‐period cross‐over trial compared a GMI protocol (identical to that of Moseley 2004; Moseley 2006) to a waiting list control in 22 participants with CRPS II of mixed aetiologies (Strauss 2021). We judged this trial as being at 'high' risk of bias on multiple domains. In addition, there was no washout period to account for potential carry‐over effects, in particular for those people who underwent the wait‐list control intervention after undergoing GMI.
Pain
According to our analyses of the missing outcome data supplied to us by the trial authors, there was no clear evidence of a difference in pain at rest (0 to 10 cm VAS (higher scores indicating more severe pain), MD –0.58, 95% CI –1.94 to 0.78) or pain on movement (0 to 10 cm VAS (higher scores indicating more severe pain), MD –0.7, 95% CI –2.29 to 0.89) (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report numerical data on adverse effects or measure any other outcomes of interest, and they were not able to complete follow‐up measures of participants' CRPS severity scores, which requires investigator‐assessed items, secondary to coronavirus restrictions during the trial. The authors responded to our request for data and reported to us that two participants reported a feeling of swelling of the affected limb during training, 12 participants reported increased pain during the training procedure, and two participants had increased pain levels after completing training.
Certainty of the evidence
We judged the certainty of evidence for pain and adverse effects to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether a six‐week GMI rehabilitation programme improves pain in the very short term compared to a waiting‐list control in people with CRPS II.
Mirror therapy
We included five trials of mirror therapy, four of which included participants with post‐stroke CRPS I of the upper limb (Cacchio 2009a; Cacchio 2009b; Saha 2021; Vural 2016). The type and cause of CRPS was not reported in the other trial (Sarkar 2017).
Mirror therapy plus conventional stroke rehabilitation versus placebo mirror therapy plus conventional stroke rehabilitation
Cacchio 2009a (n = 48) compared four weeks of mirror therapy plus conventional stroke rehabilitation to placebo mirror therapy (covered mirror) plus conventional stroke rehabilitation in participants with CRPS I of the upper limb post‐stroke in a trial judged to be at 'unclear' risk of bias.
Pain
Cacchio 2009a reported improvements in pain intensity and disability, at all post‐treatment time points, in the mirror therapy group compared to the placebo group. Specifically, Cacchio 2009a reported a mean between‐group difference following treatment in pain at rest (0 to 10 VAS (higher scores indicate worse pain)) of ‐2.9 (95% CI ‐4.23 to ‐1.57; P < 0.001) and in pain on movement (shoulder flexion) of ‐3.10 (95% CI ‐4.28 to ‐1.92; P < 0.001). At six‐month follow‐up the differences were still present, ‐3.4 (95% CI ‐4.71 to ‐2.09; P < 0.001) for pain at rest, and ‐3.8 (95% CI ‐4.96 to ‐2.64; P < 0.001) for pain on movement. The post‐treatment and six‐month follow‐up mean differences for pain at rest equated to a 38% (95% CI 21% to 56%) and 45% (95% CI 28% to 62%) reduction in the average baseline pain level respectively, whilst the post‐treatment and six‐month follow‐up mean differences for pain on movement equated to a 36% (95% CI 23% to 50%) and 45% (95% CI 31% to 58%) reduction in the average baseline pain level respectively, consistent with a moderately important benefit (very low‐certainty evidence).
Disability
Regarding disability, Cacchio 2009a also reported between‐group differences in functional limitation, in favour of mirror therapy, as measured by the functional ability subscale of the Wolf Motor Function Test (WMFT, 0 to 5 score range (higher scores indicate greater disability)) of ‐1.9 (95% CI ‐2.36 to ‐1.44, P < 0.001) at the end of treatment and of ‐2.3 (95% CI ‐2.88 to ‐1.72, P < 0.001) at six‐month follow‐up (very low‐certainty evidence).
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and disability to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether mirror therapy plus conventional stroke rehabilitation is more effective at reducing pain and improving disability compared to placebo mirror therapy plus conventional stroke rehabilitation in people with post‐stroke CRPS I of the upper limb.
Mirror therapy versus placebo mirror therapy
In a separate three‐arm trial, judged to be at 'high' risk of bias, Cacchio 2009b (n = 24) compared four weeks of mirror therapy (n = 8) to placebo mirror therapy (covered mirror) (n = 8) in participants with CRPS I of the upper limb post stroke.
Pain
Cacchio 2009b reported that seven out of eight participants in the mirror therapy group reported reduced pain (100 mm VAS; higher scores indicate worse pain) (median change in 0 to 100 VAS of ‐51 mm, range ‐70 to ‐18) compared with one of eight participants in the placebo mirror therapy group. The median change was not reported for the placebo mirror groups. At the end of the treatment period, pain scores were lower in the mirror therapy group compared to the placebo mirror groups. However, the trial authors did not report any further between‐group data and we were unable to obtain these data from the trial authors. Consequently we were unable to perform any further analyses of these measures and we could not determine the effect size (very low‐certainty evidence).
Disability
The trial authors did not report data on disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether mirror therapy is more effective at reducing pain compared to placebo mirror therapy in people with post‐stroke CRPS I of the upper limb.
Mirror therapy versus mental imagery
In the same trial (Cacchio 2009b) (n = 24), the effect of four weeks of mirror therapy (n = 8) was also compared to four weeks of mental imagery training (n = 8) in participants with CRPS I of the upper limb post stroke.
Pain
Cacchio 2009b reported that seven out of eight participants in the mirror therapy group reported reduced pain on movement (median change in zero to 100 VAS of ‐51 mm, range ‐70 to ‐18) compared with two of eight participants in the mental imagery group. The median change was not reported for the mental imagery group. At the end of the treatment period, pain scores were significantly lower in the mirror therapy group compared to the mental imagery group. However, the trial authors did not report any further between‐group data and we were unable to obtain these data from the trial authors. Consequently we were unable to perform any further analyses of these measures and we could not determine the effect size (very low‐certainty evidence).
Disability
The trial authors did not report data on disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether mirror therapy was more effective at reducing pain compared to mental imagery in people with post‐stroke CRPS I of the upper limb.
Mirror therapy plus conventional stroke rehabilitation versus conventional stroke rehabilitation
Two trials investigated the effectiveness of mirror therapy plus conventional stroke rehabilitation compared to conventional stroke rehabilitation alone (Saha 2021; Vural 2016).
Saha 2021 (n = 38) and Vural 2016 (n = 30) both compared four weeks of mirror therapy plus conventional stroke rehabilitation to four weeks of patient‐specific conventional stroke rehabilitation alone in participants with post‐stroke CRPS I of the upper limb. We judged both trials to be at high risk of bias across a number of key domains.
Pain
Saha 2021 reported improvements in pain intensity (0 to 10 numerical rating scale (NRS), higher scores indicating worse pain) in favour of the combined mirror therapy/conventional stroke rehabilitation group compared to the conventional stroke rehabilitation alone group at the post‐intervention (MD ‐1.40, 95% CI ‐2.26 to ‐0.54; P < 0.001) and two‐week (MD ‐1.86, 95% CI ‐2.77 to ‐0.95; P < 0.001) follow‐up time points, equating to a 22.1% (95% CI 8.5% to 35.6%) and 29.3% (95% CI 15.0% to 43.7%) reduction in the average baseline pain level respectively, consistent with minimal clinically important benefits, with the improvement at two weeks falling just short of our threshold for a moderate clinical benefit (very low‐certainty evidence).
According to Vural 2016, improvements in pain intensity (0 to 10 VAS; higher scores indicate worse pain) were greater in the mirror therapy group (median within‐group change of three points) compared to the control group (median within‐group change of one point). The authors did not report mean values with measures of variance and in response to our request reported that they were unable to supply these missing data. Consequently we were unable to perform any further analyses of these measures and we could not determine additional estimates of effect sizes (very low‐certainty evidence).
Disability
Saha 2021 reported improvements in disability (Functional Independence Measure, scoring properties and interpretation assumed to follow standardised methods, i.e. 18 to 126 scale, with lower scores indicating greater disability) in favour of the combined mirror therapy/conventional stroke rehabilitation group compared to the conventional stroke rehabilitation alone group at the post‐intervention (MD 21.95, 95% CI 9.71 to 34.19; P < 0.001) and two‐week (MD 25.82, 95% CI 14.12 to 37.52; P < 0.001) follow‐up time points equating to a 32.4% (95% CI 14.3% to 50.5%) and 38.2% (95% CI 20.9% to 55.4%) improvement in the average baseline disability, consistent with a 'moderate' clinically important benefit (very low‐certainty evidence).
According to Vural 2016, improvements in wrist (Fugl‐Meyer Assessment (FMA); FMA‐Wrist, score range 0 to 10 (lower scores indicate greater disability)) and hand (FMA‐Hand, score range 0 to 14 (lower scores indicate greater disability)) scores were greater in the mirror therapy group (FMA‐Wrist: median within‐group change of 3 points; FMA‐Hand: median within‐group change of 3 points) compared to the control group (FMA‐Wrist: median within‐group change of 0 points; FMA‐Hand: median within‐group change of 0 points) (mean values and measures of variation not reported) (very low‐certainty evidence).
Other outcomes
Saha 2021 and Vural 2016 did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and disability to be very low. We downgraded three times, twice for serious study limitations and once for imprecision. Consequently, we are uncertain whether mirror therapy combined with conventional stroke rehabilitation was more effective at reducing pain or improving disability compared to conventional stroke rehabilitation alone in people with post‐stroke CRPS I of the upper limb.
Mirror visual feedback plus medical management versus contrast baths plus medical management
In a three‐arm trial, Sarkar 2017 compared the effect of four weeks of mirror visual feedback (MVF) plus 900 mg/day gabapentin and 10 mg/day amitriptyline (n = 10) to a control group receiving the same pharmacological treatment plus contrast baths of the affected limb (n = 10) in participants with upper or lower limb CRPS but whose type and cause of CRPS was not reported. The trial was at high risk of bias across multiple domains.
Pain
The authors reported an improvement in both pain at rest (NRS 0 to 10; higher scores indicate worse pain) and pain on movement (NRS 0 to 10) in the MVF group compared to the contrast bath group. The authors supplied missing data, confirmed there were no dropouts and were followed up to the point of intervention completion only. According to our analyses there was a mean difference of ‐2.65 (95% CI ‐3.14 to ‐2.16; P < 0.001) in pain at rest in favour of the MVF group compared to the contrast bath group at the post‐intervention time point, equating to a 53% (95% CI 43.2% to 62.8%) reduction in baseline pain levels, equivalent to 'substantially important change'. There were similar favourable mean differences for pain on movement in the MVF group compared to the contrast bath group (MD ‐3.15, 95% CI ‐3.78 to ‐2.52; P < 0.001) at the post‐intervention time point, equating to a 40% (95% CI 32.0% to 48.0%) reduction in baseline pain levels, equivalent to 'moderately important change' (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether MVF combined with medical management was more effective at reducing pain compared to contrast baths combined with medical management in the treatment of CRPS.
Mirror visual feedback plus medical management versus contrast baths and exercise plus medical management
In the same trial the effect of four weeks of mirror visual feedback plus 900 mg/day gabapentin and 10 mg/day amitriptyline (n = 10) was also compared to another control group receiving the same pharmacological treatment plus contrast baths and exercise (n = 10) (Sarkar 2017).
Pain
The authors reported a significant improvement in both pain at rest (NRS 0 to 10) and pain on movement (NRS 0 to 10) in the mirror visual feedback compared to the contrast bath and exercise group. According to our analyses there was a mean difference of ‐2.60 (95% CI ‐3.08 to ‐2.12; P < 0.001) in pain at rest in favour of the mirror visual feedback group compared to the contrast bath and exercise group at the post‐intervention time point, equating to a 52% (95% CI 42.4% to 61.6%) reduction in baseline pain levels, equivalent to 'substantially important change'. There were similar favourable mean differences for pain on movement in the mirror visual feedback group compared to the contrast bath and exercise group (MD ‐3.25, 95% CI ‐3.70 to ‐2.80; P < 0.001) at the post‐intervention time point, equating to a 41.2% (95% CI 35.5% to 47.0%) reduction in baseline pain levels, equivalent to 'moderately important change' (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether MVF combined with medical management was more effective at reducing pain compared to contrast baths and exercise combined with medical management in the treatment of CRPS.
Virtual body swapping
We included two trials of virtual body swapping, which is a method of evoking the perceptual illusion that a virtual body is perceived as one's own body, with mental rehearsal (Hwang 2014; Jeon 2014), and may be thought of as conceptually similar to mirror therapy.
Virtual body swapping with mental rehearsal versus 'watching movement only' (control)
In a three‐arm trial, Hwang 2014 compared a single session of virtual body swapping with mental rehearsal (n = 13) to a ‘watching movement only’ control group (n = 13) in patients with CRPS types I and II of the upper or lower limb. Data regarding the number of participants with CRPS types I and II either in total or per group were not reported. Participants were followed up immediately post‐treatment only. We rated the trial as at high risk of bias for selective outcome reporting and unclear risk of bias for multiple domains, including for random sequence generation and allocation concealment.
Pain
Pain intensity was measured with respect to the 'past week' and 'present'. Hwang 2014 reported that there were no between‐group differences in changes in pain intensity (11‐point Likert scale; higher scores indicate worse pain) but did not specify to which time point this referred to. Published data suggest that pain intensity was unchanged in the virtual body swapping with mental rehearsal group and worsened slightly in the 'watching movement only' control group. The authors did not reply to our requests for missing data. As a result, we could not conduct any further analyses (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the immediate effect of a single session of virtual body swapping with mental rehearsal compared to a ‘watching movement only’ control intervention in the treatment of CRPS.
Virtual body swapping with mental rehearsal versus mental rehearsal only (control)
In the same trial the effect of a single session of virtual body swapping with mental rehearsal (n = 13) was also compared to a ‘mental rehearsal only’ (n = 13) control group (Hwang 2014).
Pain
Hwang 2014 reported that there were no between‐group differences in changes in pain intensity. Published data suggest that pain intensity was unchanged in the virtual body swapping with mental rehearsal group and worsened slightly in the mental rehearsal only control group. The authors did not reply to our requests for missing data. As a result, we could not conduct any further analyses (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the immediate effect of a single session of virtual body swapping with mental rehearsal compared to a mental rehearsal control intervention in the treatment of CRPS.
Virtual body swapping with mental rehearsal versus virtual body swapping alone
Jeon 2014 compared a single session of virtual body swapping with mental rehearsal compared to virtual body swapping alone in a total of 10 participants (number per group not reported) with CRPS I of either the upper or lower limbs, multiple limbs or the whole body, the aetiology of which was not reported. Participants underwent a single session of their allocated intervention with follow‐up immediately post‐treatment only. We rated the trial as at 'unclear' risk of bias for random sequence generation and allocation concealment, and at 'high' risk of bias for selective outcome reporting.
Pain
Jeon 2014 reported that there was no difference between the groups regarding pain intensity, as measured by an 11‐point Likert rating scale ranging from zero (no pain) to 10 (severe pain) immediately post‐treatment. The trial authors did not report numerical data for measures of pain intensity, and we have been unable to obtain these data from the trial authors. As a result, we could not conduct any further analyses and we could not determine the effect size (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other any outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the immediate effect of a single session of virtual body swapping with mental rehearsal compared to virtual body swapping alone in the treatment of CRPS I.
Virtual reality versus sham virtual reality
One two‐arm trial with 45 participants, which we judged as being at high risk of bias secondary to inadequate reporting of outcomes, its small sample size and short‐term follow‐up of participants, compared a virtual reality intervention (n = 23), during which participants visualised a digitally altered image of their affected hand, to a sham virtual reality intervention (n = 22) in participants with CRPS (type(s) not reported) of the upper limb (Lewis 2021).
Pain
Lewis 2021 reported a reduction in pain intensity (11‐point NRS; higher scores indicate worse pain) in the virtual reality group compared to the sham virtual reality (MD 1.2; effect size SMD 0.7; with measures of variation either not explained or not reported) at the post‐intervention time point. This equates to a 22% reduction in the average baseline pain level, consistent with a 'minimally important change'. The trial authors did not fully report numerical data for measures of pain intensity, and we have been unable to obtain these data from them. As a result, we could not conduct any further analyses or confirm the effect size (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain whether virtual reality is more effective at reducing pain compared to sham virtual reality in the treatment of CRPS.
Four tactile discrimination training protocols compared with each other
We included one trial that employed a within‐subject, randomised, cross‐over design, which compared four tactile discrimination training (TDT) protocols with one another (n = 10) in participants with CRPS I of the upper limb from mixed aetiologies (Moseley 2009).
Pain
Moseley 2009 reported that there were no differences in self‐reported pain intensity (0 to 100 VAS; higher scores indicate worse pain) at two‐day follow‐up between the four TDT protocols. The trial authors did not report numerical data for measures of pain intensity, and they have not supplied us with these data. Thus we were unable to perform any further analyses and we could not determine the effect size. We rated the trial at 'high' risk of bias for selective outcome reporting, sample size and duration of follow‐up (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
Regarding adverse effects, three participants reported that the pressure stimuli associated with the TDT occasionally hurt but that this was not enough to necessitate modification or cessation of the TDT training (very low‐certainty evidence). The trial authors did not measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and adverse effects to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of TDT in people with CRPS I of the upper limb at short‐term follow‐up.
Prism adaptation treatment versus sham prism adaptation treatment
We included one trial that compared two weeks of twice‐daily prism adaptation treatment, during which participants perform a pointing task while wearing adapted goggles in an attempt to counter‐lateralise attention bias in attention and spatial representations, with a sham prism adaptation treatment in 49 participants with upper limb CRPS I (Halicka 2021). We judged the trial as being at high risk of bias secondary to a small sample size and high risk of attrition bias secondary to violation of the intention‐to‐treat principle and a high dropout rate at six‐month follow‐up, however we note that the primary endpoint was immediately post‐intervention.
Pain
Halicka 2021 found no clear evidence of benefit of prism adaptation treatment beyond sham for treating the primary outcomes of pain (11‐point NRS; higher scores indicate worse pain) at short‐ or long‐term follow‐up (mean differences and 95% CI not reported) (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
There was no clear evidence of a difference in Patient's Global Impression of Change (1 to 7 scale; lower scores indicate poorer treatment outcomes) at short‐ or long‐term follow‐up (differences in medians with measure of variation not reported) (very low‐certainty evidence). The trial authors did not report data concerning adverse effects or measure other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and Patient's Global Impression of Change to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of prism adaptation treatment in people with CRPS I of the upper limb at short‐term follow‐up.
Electrophysical agents
Ultrasound of the stellate ganglion versus sham ultrasound of the stellate ganglion
One three‐arm trial (n = 45) compared two different doses (3.0 watts and 0.5 watts intensity) of high‐frequency ultrasound to sham ultrasound (Askin 2014). All trial groups also received multimodal conventional treatment that included a course of medication (including vitamin C, gabapentin and prednisolone) and physiotherapy (including TENS, contrast baths, active and passive range of motion exercises and stretching, resistance and mirror box exercises). The participants received treatments daily for 20 days. The trial was small with fewer than 50 participants, and we judged it to be at 'high' or 'unclear' risk of bias based on a number of criteria.
Pain
There was no clear evidence of a difference in pain intensity (10 cm VAS; higher scores indicate worse pain) at the post‐intervention time point and there was no further follow‐up (mean differences with measures of variation not reported) (very low‐certainty evidence).
Disability
There was no clear evidence of a difference in disability (DASH (Turkish language version); score range not reported, higher scores indicating greater disability) at the post‐intervention time point and there was no further follow‐up (mean differences with measures of variation not reported) (very low‐certainty evidence).
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and disability to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of ultrasound to the stellate ganglion compared to a sham intervention in people with CRPS I of the upper limb at short‐term follow‐up.
Stellate ganglion block (SGB) with lidocaine versus SGB with ultrasound versus sham SGB with lidocaine and ultrasound
One three‐arm trial (n = 25) compared stellate ganglion block with lidocaine to blocks with ultrasound and placebo conditions for both interventions. All trial groups received exercises, TENS, contrast baths, compression and oral paracetamol. We judged the trial to be at 'high' or 'unclear' risk of bias based on a number of criteria (Aydemir 2006).
Pain
There was no clear evidence of a difference in pain intensity (0 to 10 VAS; higher scores indicate worse pain) at the post‐intervention (MD 0.08, 95% CI ‐2.11 to 2.27) or one‐month follow‐up time points (MD 0.00, 95% CI ‐1.69 to 1.69) (very low‐certainty evidence).
Disability
Aydemir 2006 measured hand disability using a Functional Hand Scale (0 to 19 scale, higher scores indicating greater disability) and reported improvements in all three trial groups post‐treatment and at one‐month follow‐up. According to our analyses there were greater improvements in the placebo group post‐treatment (MD ‐7.86, 95% CI ‐14.33 to 1.39) and at one‐month follow‐up (MD 6.79, 95% CI 1.19 to 12.34) compared to the SGB with ultrasound group only (very low‐certainty evidence).
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and disability to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of SGB with lidocaine or ultrasound compared to a sham intervention in people with CRPS I of the upper limb at short‐term or one‐month follow‐up.
Ultrasound of the stellate ganglion versus TENS
One trial with 30 participants compared ultrasound of the stellate ganglion to TENS in military recruits with acute (mean duration of symptoms: 44 days) CRPS I of the upper limb secondary to mixed aetiologies (Hazneci 2005). Both groups also received contrast baths and physiotherapist‐prescribed exercises. We judged the trial to be at 'unclear' risk of bias for random sequence generation and allocation concealment.
Pain
In this trial the ultrasound group demonstrated inferior post‐treatment pain scores (0 to 10 VAS (higher scores indicate worse pain), MD 2.13, 95% CI 1.47 to 2.79, P < 0.001), which equates to a potentially clinically important difference of 27% (95% CI 19% to 36%) of the average baseline pain score (very low‐certainty evidence). The trial authors measured pain intensity at the end of the three‐week intervention period only without longer‐term follow‐up.
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of ultrasound of the stellate ganglion compared to TENS in people with acute CRPS I of the upper limb.
(Pulsed) electromagnetic field therapy (PEMF) versus placebo PEMF
Three trials investigated the effectiveness of pulsed electromagnetic field therapy (Durmus 2004; Benedetti 2018; Bϋyϋkturan 2018). One trial with 40 participants compared pulsed electromagnetic field (PEMF) treatment (100 Gauss, 50 Hz, five times weekly for six weeks) plus calcitonin and a stretching exercise routine to placebo PEMF plus calcitonin and stretching in participants with acute (mean duration of symptoms: 52 days) CRPS I of the upper limb following Colles' fracture (Durmus 2004). We rated the trial at 'high' risk of bias for selective outcome reporting, study size and duration of follow‐up and at 'unclear' risk of bias for allocation concealment. Benedetti 2018 (n = 30) compared 10 sessions of PEMF and physiotherapy (education, psychological support, mobilisation, exercise, desensitisation, proprioceptive feedback, gait rehabilitation or occupational therapy as needed) to sham PEMF and physiotherapy in patients with upper and lower limb CRPS I of mixed aetiologies. We judged the trial to be at 'unclear' risk of bias overall secondary to uncertainties concerning their method of allocation concealment and whether or not they employed the 'intention‐to‐treat' principle. The trial was at high risk of bias given the small sample size. Bϋyϋkturan 2018 (n = 42) compared the effectiveness of 30 sessions of electromagnetic field therapy (EMFT) and physiotherapy (stretching, range of motion exercises) to placebo EMFT and physiotherapy in patients with upper limb CRPS I. We judged the trial to be at high risk of selection bias secondary to the use of a pseudo‐randomisation procedure, the small sample size and follow‐up limited to the post‐intervention point only.
Pain
At the end of treatment, Durmus 2004 found no clear evidence of a difference in pain intensity (10 cm VAS; higher scores indicate worse pain) at rest or on activity (null effect size data could not be estimated because the authors did not report the number of participants in each group). Benedetti 2018 reported improvements in pain intensity (10 cm VAS; higher scores indicate worse pain) in favour of the PEMF group compared to sham at the post‐intervention (MD ‐2.2, 95% CI ‐2.41 to ‐1.99; P < 0.001) and one‐month (MD ‐2.5, 95% CI ‐2.79 to ‐2.21; P < 0.001) follow‐up time points equating to a 46.3% (95% CI 41.9% to 50.7%) and 52.6% (95% CI 46.5% to 58.7%) reduction in the average baseline pain level, consistent with a 'moderate' and 'substantial' clinically important benefits, respectively. Bϋyϋkturan 2018 found an improvement in pain intensity (average pain over the last week using a 10 cm VAS; higher scores indicate worse pain) in the EMFT compared to the placebo EMFT group at the post‐intervention time point. According to our analyses there was a mean difference of ‐1.6 (95% CI ‐2.37 to ‐0.83; P < 0.001) in favour of the EMFT group compared to the placebo EMFT group, equating to a 29.1% (95% CI 15.1% to 43.1%) reduction in baseline pain levels, falling just short of the threshold of a 'moderately important change'. We were unable to pool the data from these trials secondary to reporting limitations (e.g. Durmus 2004 did not report the number of participants in each trial arm) and study heterogeneity (very low‐certainty evidence).
Disability
Benedetti 2018 reported an improvement in a self‐reported composite measure of lower limb pain/disability in the participants with lower limb CRPS I (n = 18) (Maryland Foot Score (MFS) 0 to 100) in favour of the PEMF group compared to sham at both post‐intervention (MD 14.4, 95% CI 11.36 to 17.44; P < 0.001) and one‐month (MD 14.9, 95% CI 11.34 to 18.46) time points equating to a 19.6% (95% CI 15.5% to 23.8%) and 20.3% (95% CI 15.4% to 25.1%) improvement in average baseline pain/disability, consistent with 'minimally' important change. There was no benefit from PEMF according to a self‐reported composite measure of upper limb function/pain in the participants with upper limb CRPS I (n = 12) (Disabilities of the Arm, Shoulder, and Hand (DASH) 0 to 100), where there was in fact a significant improvement in favour of the sham PEMF group at both post‐intervention (MD ‐14.0, 95% CI ‐23.59 to ‐4.41; P < 0.004) and one‐month (MD ‐23.3, 95% CI ‐29.52 to ‐17.08) time points, equating to a 17.2% (95% CI 5.4% to 29.0%) and 28.6% (95% CI 21.0% to 36.3%) improvement in average baseline pain/disability, consistent with 'minimally' important change. Bϋyϋkturan 2018 found no clear evidence of a difference in disability (Quick Disabilities of the Arm, Shoulder and Hand (Q‐DASH); 0 to 100 range; higher scores indicate greater disability; MD 2, 95% CI ‐3.91 to 7.91) at the post‐intervention time point (very low‐certainty evidence).
Other outcomes
Bϋyϋkturan 2018 and Durmus 2004 did not report data concerning adverse effects or measure other outcomes of interest. Benedetti 2018 reported that none of the participants presented with adverse effects (very low‐certainty evidence) and they did not measure other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain, disability and adverse effects to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of PEMF compared to placebo PEMF in the treatment of CRPS I.
Transcutaneous electrical nerve stimulation (TENS) versus sham TENS
Two trials investigated the effectiveness of TENS (Bilgili 2016; Ryan 2017). Bilgili 2016 compared 15 sessions of TENS plus conventional physiotherapy (contrast bath, whirlpool bath, exercise programme) to sham TENS plus physiotherapy in 30 participants with upper limb CRPS I. We rated the trial as being at high risk of bias across a number of key domains as well as secondary to a small sample size and follow‐up limited to the post‐intervention point only. Ryan 2017 compared (what we assume was) 21 sessions of TENS plus physiotherapy (advice, education, exercise, motor imagery, desensitisation, hydrotherapy) (n = 6) to sham TENS plus physiotherapy (n = 2) in a small‐scale feasibility trial that included participants with CRPS I of the upper limb. The trial was at high risk of bias across a number of key domains as well as secondary to a small sample size. Given the particularly small sample size, violation of the intention‐to‐treat principle and the 50% dropout rate we did not undertake any further analyses of the missing data the authors supplied as we did not think it would be possible to derive any clinically meaningful effect estimates for pain and function outcomes.
Pain
There was no clear evidence of a difference in pain (100 mm VAS; higher scores indicating worse pain; MD ‐9.0, 95%CI ‐18.5 to 0.5, p=0.074) (Bilgili 2016 ) (very low‐certainty evidence).
Disability
There was no clear evidence of a difference in hand disability (Duruöz Hand Index; scale scoring properties not adequately reported, higher scores indicate greater disability; MD ‐3.6, 95% CI ‐13.38 to 6.18) (Bilgili 2016) (very low‐certainty evidence).
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and disability to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of TENS on pain and disability compared to sham TENS in the treatment of CRPS I of the upper limb.
Laser therapy versus Interferential therapy
One trial with 50 participants compared 20 sessions of low‐level laser therapy with interferential current therapy in participants with post‐traumatic CRPS I of the upper or lower limb (Dimitrijevic 2014). Both trial groups also received kinesitherapy that consisted of individualised active and active assisted exercises, strictly dosed up to pain threshold. We rated the trial at 'high' risk of bias for incomplete outcome data, trial size and duration of follow‐up.
Pain
Dimitrijevic 2014 reported an improvement in pain at rest (0 to 100 VAS) of ‐8.6 (95% CI ‐16.27 to ‐0.93, P = 0.03) in favour of laser therapy at the post‐intervention time point. This equates to a difference of 14% (95% CI 1.5% to 26%) from the mean baseline pain score of the two groups, which falls below our criteria for a minimal clinically important difference. There was no clear evidence of a difference with respect to pain with movement of the affected wrist or ankle according to our analysis (MD 10.2, 95% CI 0.17 to 20.24) (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors reported that there were no adverse effects of therapy recorded (very low‐certainty evidence). The trial authors did not measure other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and adverse effects to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of laser compared to interferential therapy in the treatment of CRPS I of the upper or lower limb.
CO2 bath therapy and exercise versus exercise
One trial with 40 participants compared carbon dioxide (CO2) baths in addition to exercise therapy with exercise therapy alone in participants with post‐traumatic CRPS I of the hand (Mucha 1992). Neither intervention is clearly described in the paper though the baths were administered in 12‐minute sessions five times a week for four weeks. We rated the study at 'high' risk of bias on five separate criteria.
Pain
Mucha 1992 reported that there was an improvement in pain at rest, pain with movement and night pain (measurement properties not described) in favour of the CO2 bath group. The trial authors did not report numerical data, and we have been unable to obtain these data from the trial authors. Consequently, we were unable to perform any further analyses of these measures and could not determine an effect size (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of CO2 baths combined with exercise compared to exercise alone in the treatment of CRPS I of the hand.
Whirlpool baths versus neuromuscular electrical stimulation
Devrimsel 2015 (n = 60), compared the effects of 15 sessions of a whirlpool bath intervention to 15 sessions of neuromuscular electrical stimulation (NMES) in a two‐arm trial of participants with upper limb CRPS I. Both groups also received underwater ultrasound and exercise therapies. We rated the trial as being at 'unclear' or 'low' risk of bias across all key domains, and at high risk of bias secondary to a small size and follow‐up limited to the post‐intervention point only.
Pain
Devrimsel 2015 reported improvements in pain intensity (10 cm VAS; higher scores indicate worse pain) favouring the whirlpool bath group at the post‐intervention time point, although according to our analysis a MD of ‐0.65 (95% CI ‐1.03 to ‐0.27; P < 0.001), equating to a 9.8% (95% CI 4.1% to 15.6%) reduction in the average baseline level of pain is probably clinically unimportant (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors reported that none of the participants experienced any 'treatment‐associated complications' (which we assume to mean adverse effects) (very low‐certainty evidence) and they did not measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and adverse effects to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of whirlpool baths compared to NMES in the treatment of CRPS I of the upper limb.
Fluidotherapy plus conventional stroke rehabilitation versus conventional stroke rehabilitation
Ozcan 2019 (n = 32) compared the effectiveness of 15 sessions of fluidotherapy, a dry heat modality, combined with conventional rehabilitation to conventional rehabilitation alone in participants with post‐stroke upper limb CRPS I. The trial was at high risk of bias on multiple key domains and secondary to a small size and follow‐up limited to the post‐intervention point only.
Pain
Ozcan 2019 reported no clear evidence of a difference in pain intensity (10 cm VAS; higher scores indicate worse pain) at the post‐intervention time point (mean scores with measures of variance not reported) (very low‐certainty evidence).
Disability
There was no clear evidence of a difference in disability (Functional Independence Measure (FIM) motor items; 1 to 7 scale, lower scores indicate greater disability) at the post‐intervention time point (mean scores with measures of variance not reported) (very low‐certainty evidence).
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain and disability to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of fluidotherapy combined with conventional rehabilitation compared to conventional rehabilitation alone in people with post‐stroke upper limb CRPS I.
Other interventions
Manual lymphatic drainage (MLD) therapy versus conventional care
Two trials investigated the effectiveness of adding MLD therapy to rehabilitation (Duman 2009; Uher 2000). Duman 2009 (n = 34) compared the addition of MLD massage to conventional care (nonsteroidal anti‐inflammatory drugs and physical therapy) to conventional care alone in participants with CRPS I of the upper limb of mixed aetiology. Uher 2000 (n = 40) compared the addition of MLD in addition to exercise therapy to exercise therapy alone in participants with CRPS I of the lower limb of mixed aetiology. We rated both trials as being at 'high' risk of bias on multiple criteria.
Pain
Both trials showed no clear evidence of an effect from the addition of MLD on pain intensity. We were unable to extract accurate data from either study and so no further analyses were possible (very low‐certainty evidence).
Disability
The trial authors did not measure disability.
Other outcomes
The trial authors did not report data concerning adverse effects or measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain to be very low. We downgraded three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of MLD combined with conventional care compared to conventional care alone for the treatment of CRPS I.
Electro‐acupuncture and massage versus rehabilitation
One trial (n = 120) compared 30 sessions of electro‐acupuncture combined with upper limb massage therapy to 30 sessions of rehabilitation in participants with post‐stroke shoulder‐hand syndrome (Li 2012). Rehabilitation consisted of active‐assisted scapular movements, Bobath exercises to clench the fist, functional transfer training and proprioceptive neuromuscular facilitation (PNF) exercise. We rated the trial at 'high' risk of bias for blinding of participants and at 'unclear' risk of bias for sample size.
Pain
Li 2012 reported greater reductions in pain intensity (in the shoulder when moved passively to 90º; measurement properties not reported) in favour of the electro‐acupuncture and massage group at the end of the six‐week treatment period (MD ‐1.70, 95% CI ‐2.09 to ‐1.31, P = 0.01), which were sustained at 12‐week follow‐up (MD ‐1.40, 95% CI ‐1.78 to ‐1.02, P < 0.001). The post‐treatment and 12‐week follow‐up MD values equated to a 21% (95% CI 16% to 26%) and 18% (95% CI 13% to 22%) reduction in the average baseline pain level respectively. These were below the threshold for a moderately clinically important difference but the point estimates exceeded the IMMPACT threshold (15%) for a minimally important benefit (very low‐certainty evidence).
Disability
Li 2012 reported no difference in hand disability (Fugl‐Meyer evaluation of functional movement of the hand; 0 to 14 scale, lower scores indicate greater disability) between the two trial groups, but a difference in upper limb function (as measured by the Fugl‐Meyer evaluation of functional movement of the upper limb; 0 to 66 score, lower scores indicate greater disability) in favour of the electro‐acupuncture and massage group at the end of treatment (MD 4.5, 95% CI 0.85 to 8.15, P = 0.05) but not at the 12‐week follow‐up time point (very low‐certainty evidence).
Other outcomes
The trial authors reported that there were no adverse effects associated with the interventions in either trial group. They did not measure any other outcomes of interest.
Certainty of the evidence
We judged the certainty of evidence for pain, disability and adverse effects to be very low. We downgraded each three times, once for serious study limitations, once for inconsistency and once for imprecision. Consequently, we are uncertain of the effects of electro‐acupuncture combined with upper limb massage therapy compared to a stroke rehabilitation intervention for the treatment of post‐stroke shoulder‐hand syndrome. We also have some concerns regarding the diagnostic equivalence of 'shoulder‐hand syndrome' and CRPS I and whether the control intervention was directed towards the management of the shoulder‐hand syndrome explicitly or if it was a general rehabilitation programme aimed at addressing the impairments related to the stroke, both of which may have implications for the generalisability of this trial's findings.
Discussion
Summary of main results
The evidence arising from the clinical trials included in this review is very uncertain. As such, we cannot draw any firm conclusions regarding the effectiveness or harmfulness of a broad range of physiotherapy interventions for treating the pain and disability associated with CRPS I in adults.
One included trial provided very low‐certainty evidence that a multimodal physiotherapy programme may provide a small, long‐term improvement in impairment compared to a minimal intervention of ‘social work’, but the magnitude of this effect is of questionable clinical significance. We could not determine its effect on a range of pain‐related outcomes (Oerlemans 1999).
Two trials of cognitive‐behavioural approaches that employed differing forms of exposure interventions, compared to a conventional 'pain‐contingent' approach, provided contrasting evidence (Barnhoorn 2015; den Hollander 2016). One trial found that exposure through 'forced' limb use does not improve pain, functional disability or health‐related quality of life in the medium‐ or longer‐term (Barnhoorn 2015), while another found that 'graded' exposure targeting pain‐related fear avoidance may provide 'moderate' to 'substantial' improvements in pain, disability and health‐related quality of life at short‐ and long‐term follow‐up (den Hollander 2016). The difference in findings between these two 'exposure‐based' interventions may reflect differences in their theoretical basis and therapeutic approach. In the approach used by Barnhoorn 2015 patients are directly exposed to painful activities and instructed to ignore the pain in order to attain their personal goals, whereas in the trial by den Hollander 2016 patients with moderate to high pain‐related fear are repeatedly exposed to feared movements and activities in order to adjust their expectancies regarding the association of activities and increased pain, reduce their fear and subsequently their disability. But given the very low‐certainty of this evidence further trials of 'exposure' based interventions are warranted.
Evidence that supports the use of cortically directed sensory‐motor rehabilitation strategies was mixed. Our findings suggest that graded motor imagery (GMI) may provide clinically meaningful medium‐ and long‐term improvements in both pain and disability in people with CRPS I and that mirror therapy may provide short‐ and possibly long‐term clinically meaningful improvements in pain and function in people with CRPS I following stroke. We also identified one trial of mirror therapy that was terminated early secondary to difficulties in recruiting participants and an interim analysis of which found an apparent lack of treatment effect (NCT02667717). The effectiveness of mirror therapy in broader participant populations with CRPS I (e.g. post‐trauma) remains unknown. The results from these trials were all from very low‐certainty studies and were inconsistent, and so should be treated with caution.
We also found very low‐certainty evidence that more novel interventions such as virtual body swapping with/without mental rehearsal (Hwang 2014; Jeon 2014), tactile discrimination training (TDT) (Moseley 2009), and prism adaptation treatment (Halicka 2021) do not provide any short‐term benefits in pain for people with CRPS I, and that a virtual reality intervention may provide minimal clinically significant benefits in pain in the short term (Lewis 2021).
Trials that investigated the use of other physiotherapy interventions provide mixed results. Overall we found no clear evidence of clinical effectiveness for upper limb aerobic exercise, ultrasound over the stellate ganglion, pulsed electromagnetic field therapy, TENS, CO2 bath therapy, fluidotherapy, and manual lymphatic drainage combined with and/or compared to either sham or other active interventions (very low‐certainty evidence). Laser therapy, whirlpool baths and electro‐acupuncture combined with massage may provide small clinically insignificant, short‐ to medium‐term improvements in pain intensity compared to various active comparators in adults with CRPS I (very low‐certainty evidence). We are generally uncertain of the effects of any of these interventions on pain and disability in adults with CRPS I. Details regarding adverse events were generally not reported.
Very low‐certainty evidence indicates that manual lymphatic drainage (MLD) is not beneficial for pain in people with CRPS I compared to other active interventions (Duman 2009; Uher 2000).
We found very low‐certainty evidence from one trial that electro‐acupuncture and massage were superior to a stroke rehabilitation programme for pain on passive shoulder movement in shoulder‐hand syndrome post stroke at longer‐term follow‐up. However, the magnitude of this effect was unlikely to be clinically important and both the reliability and validity of the outcome measure used are questionable (Li 2012).
Only five trial reports, four related to electrophysical modalities (Benedetti 2018; Devrimsel 2015; Dimitrijevic 2014; Ryan 2017), and one to TDT (Moseley 2009), commented on the presence or absence of adverse effects and reported no serious effects.
We found only one trial that included people with CRPS II exclusively (Strauss 2021).
Overall, we identified a lack of high‐ or moderate‐certainty evidence with which to inform or guide rehabilitation practice in people with CRPS I or II. Based on the current body of evidence, we cannot draw any accurate conclusions regarding the effectiveness or safety of any of the physiotherapy interventions identified in this Cochrane Review.
Overall completeness and applicability of evidence
The evidence base for the use of physiotherapy interventions in CRPS is incomplete, although this reflects a broader problem for all intervention research in CRPS (O'Connell 2013). Most included trials (29/34) used established diagnostic criteria to identify participants with CRPS I. However, as might be expected given the development history of such criteria in CRPS, there was some variation in the criteria used between included trials. Beyond various issues relating to risk of bias and study size (see Quality of the evidence) there are few instances where more than one included trial tested a specific intervention. Furthermore, 22 (65%) trials were single‐centre trials and the number of trial sites was unreported in nine (26%) trials. Single‐centre RCTs have been shown to exhibit larger treatment effects, and while the cause of this is unknown, authors and users of randomised controlled trials (RCTs), systematic reviews and meta‐analyses should consider this when reporting and interpreting effect sizes (Bafeta 2012; Deschartes 2011; Unverzagt 2013). Two trials specifically recruited participants from military populations (Aydemir 2006; Hazneci 2005). As such, it is possible that contextual factors specific to that participant group and environment may limit the applicability of those results to civilian clinical practice. Eighteen trials (53%) measured outcomes immediately at the end of treatment only, with no longer‐term follow‐up, and 24 (71%) of the included trials followed up their participants for less than three months. Such trials offer limited information about the genuine clinical utility of interventions for a condition that is commonly persistent. The broad heterogeneity of interventions assessed in the included trials, together with the poor reporting of the interventions, afforded us limited opportunities to pool data.
The aim of this Cochrane Review was to investigate the effectiveness of physiotherapy interventions for pain and disability in people with CRPS I or II. We used a deliberately inclusive definition in an attempt to include evidence on any intervention that might reasonably be delivered within a physiotherapy context for people with CRPS. As a result, the included trials varied considerably but most were designed to test the specific effectiveness of individual modalities either alone, when added to other treatments or compared to other treatments. While these trials offered information about the specific or additional clinical benefits of those modalities, they are less informative about the effectiveness of physiotherapy programmes that incorporate multiple treatment modalities, but are more likely to reflect physiotherapy as it is delivered in clinical practice. Only one included trial took the pragmatic approach of testing a multimodal physiotherapy programme against a minimal treatment control group (Oerlemans 1999). Notably, this trial pre‐dates substantial developments in the pathophysiological models of CRPS and it is possible that a modern multimodal physiotherapy programme might differ substantially. For example, we included 'pain education' within our search strategy but found no RCTs with pain neuroscience education (PNE) as the primary intervention. The 'pain exposure physical therapy' intervention in the trial by Barnhoorn 2015 appeared to contain some elements of the PNE approach and we know of one published case study where PNE was combined with GMI and graded functional exposure (Shepherd 2018). In addition, few of the included trials reported on adverse effects (five out of 34 trials) and it is unclear whether or not this represents an absence of adverse effects or a failure to report them. Only nine of the 34 included trials employed medium‐ to long‐term follow‐up of trial participants (Barnhoorn 2015; Cacchio 2009a; den Hollander 2016; Halicka 2021; Li 2012; Moseley 2005; Moseley 2006; Oerlemans 1999; Ryan 2017). The general lack of long‐term follow‐up of trial participants also limits the applicability of the evidence.
While we categorised these interventions under the label 'physiotherapy' in this Cochrane Review, we recognise that rehabilitation therapies may be delivered by a range of different professionals, including occupational therapists and nurses. Also, our main outcomes of interest were pain and disability. We did not assess outcomes related to emotional wellbeing, which we acknowledge are an important dimension of people's pain experience. Such outcomes were generally not measured in the included trials but could be included in future clinical trials and systematic reviews of interventions for CRPS.
Quality of the evidence
As reflected by the GRADE ratings, the overall certainty of the evidence in this Cochrane Review was very low. This reflects the fact that most included trials were at unclear or high risk of bias for criteria included under the standard domains of the Cochrane risk of bias tool, and under the additional risk of bias criteria of study size and duration included in this review. The included trials studied a broad range of interventions, which afforded us limited opportunity to pool data and that, coupled with study size, led to issues of imprecision and inconsistency. We were only able to combine trials through meta‐analysis for one type of intervention (GMI) because of poor standards of reporting, insufficient data and clinical heterogeneity.
It is likely that small study effects, wherein there is a propensity for smaller published studies to report inflated effect sizes (Dechartres 2013; Moore 2012; Nüesch 2010), might lead to an overly positive picture for some interventions, particularly in a field with such a limited evidence base. A review of meta‐analyses has demonstrated that trials with fewer than 50 participants, which reflects most trials (28/34) included in this Cochrane Review, returned effect estimates that were on average 48% larger than the largest trials and 23% larger than estimates from studies with sample sizes of more than 50 participants (Dechartres 2013). A recent Cochrane systematic review of psychological therapies for the management of chronic pain excluded studies with 19 or fewer participants in each trial arm because of the risk of bias associated with small sample sizes in RCTs (Williams 2020). This exclusion criterion has been recommended for systematic reviews of clinical trials involving patient populations with chronic pain (Busse 2015). Applying the same exclusion criterion would have resulted in the exclusion of over half of the trials (20/34) included in this review.
We did not downgrade any of the GRADE judgements on the basis of publication bias, as there can be no direct evidence with so few trials for any given intervention. Moreover, it is accepted that existing approaches to detecting publication bias are unsatisfactory. To an extent our GRADE judgements reflect this risk through the assessment of imprecision and the limitations of included trials. Conversely, the issue of small study size combined with low number of trials for any single comparison raises the possibility of false negatives through lack of statistical power (Button 2013). Many of the comparisons we included in this review did not demonstrate clear evidence of benefit of the index intervention.
The quality of reporting in many included trials was problematic. There was a lack of detailed descriptions of some interventions, which impedes judgements concerning the replicability and generalisability of some trials. To improve this, we recommend that trialists follow the Template for Intervention Description and Replication guidelines for better reporting of interventions (Hoffman 2014). In addition, a number of included trials did not present key numerical outcome data for all time points (19/34 trials) or insufficiently reported the scoring properties of their outcome measures for pain intensity (10/34 trials). The quality of reporting of pain‐related outcome measures in clinical trials and observational studies is frequently insufficient (Smith 2015). In a systematic review assessing the quality of pain intensity reporting in three prominent pain journals, Smith 2015 found that nearly one‐quarter of published studies inadequately reported the type of pain intensity measure employed. The choice of outcome measures for pain and function/disability varied across the trials included in this review, a finding consistent with a recent systematic review evaluating the use of outcome measures in clinical trials of pain management, rehabilitation and psychological interventions for CRPS (Grieve 2016b). Recommendations for a first core outcome measurement set in clinical trials for complex regional pain syndrome have recently been proposed (Grieve 2017) which, if adopted, would facilitate more valid comparisons between trials as well as the pooling of data for meta‐analyses in order to obtain more precise estimates of treatment effect.
To our knowledge, only six of the 16 new trials included in this updated review were either registered or were associated with a published trial protocol (Barnhoorn 2015; den Hollander 2016; Halicka 2021; Lewis 2021; Ryan 2017; Strauss 2021). This fact, together with the poor standards of reporting that we observed in many of the unregistered studies included in this review, raises serious concerns regarding the validity of the majority of these unregistered trials, and their findings, as well as the potential for publication bias (Viergever 2014). This also shows that there are still academic journals willing to publish RCTs without prospective registration. We respectfully urge all trialists investigating physiotherapy interventions for CRPS to prospectively register their trial and publish a trial protocol in accordance with the SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) guidelines (Chan 2013). We also invite journal editors to give serious consideration to this issue before publishing unregistered trials (ICMJE 2019).
Potential biases in the review process
We conducted extensive and sensitive literature searches and included trials regardless of the language of publication. The choice to use the IMMPACT thresholds to determine the clinical importance of effect sizes is potentially controversial. What exactly constitutes an important difference on any given outcome measure remains contentious as the construct of a generic importance thresholds for a variety of interventions fails to reflect that patient satisfaction might differ substantially between interventions given their risks, costs and inconvenience, the point in the care pathway at which the participant arrives, and a range of other possible factors. Moreover, the IMMPACT thresholds are based on estimates of the degree of within‐person change from baseline that participants might consider to be clinically important, whereas the effect sizes focused on in this review reflect the average change between intervention‐groups following the interventions. It is possible that a small average between‐group effect size might reflect that a proportion of participants responded very well to the intervention tested but equally it might reflect that most participants experienced a small effect. While we planned to include the results of ‘responder analyses’, which compare the proportion of participants achieving a clinically important improvement from baseline in the treatment and control groups, no studies reported these data.
Since the publication of our original protocol for this review (Smart 2013), the OMERACT 12 group reported recommendations for minimally important difference for pain outcomes (Busse 2015). The group recommends a threshold of 10 mm on a 0 to 100 visual analogue scale (VAS) as the threshold for minimal importance for average between‐group change, though stress that this should be interpreted with caution as it remains possible that estimates that fall closely below this point may still reflect a treatment that benefits an appreciable number of participants. Using this largely more lenient threshold would not alter our conclusions regarding clinical importance. The OMERACT thresholds present similar problems to those associated with all generic thresholds and it seems likely that the discussion around what constitutes clinical importance will continue. Arguably, the thresholds used in this Cochrane Review of a 15% or 30% improvement in baseline levels of pain that are specifically attributable to the interventions do not represent unreasonably high thresholds.
Agreements and disagreements with other studies or reviews
The results of this updated systematic review remain largely consistent with the findings of a Cochrane overview of systematic reviews of all interventions for CRPS (O'Connell 2013), which drew its conclusions mainly based on two non‐Cochrane reviews of physiotherapy interventions for CRPS (Daly 2009; Smith 2005). Daly 2009 concluded that there was good to very good‐quality evidence to support the use of GMI for CRPS. Smith 2005 concluded that there was some evidence that exercise, acupuncture, TENS, relaxation techniques, mirror therapy, GMI and combined treatment programmes may be helpful and that it was not possible to determine the effectiveness of individual treatments for CRPS I. A subsequent systematic review of GMI for chronic pain (of which review author NOC was a co‐author) concluded that there was limited evidence to suggest that GMI may be effective for CRPS (Bowering 2013). In O'Connell 2013, we concluded that there was low‐quality evidence for the effectiveness of GMI. In this Cochrane Review we downgraded the GRADE rating for the certainty of evidence related to GMI to very low, largely due to the inconsistency introduced by the inclusion of Schreuders 2014. In Schreuders 2014, the trial authors adjusted the treatment schedule compared to the schedules delivered by Moseley 2004 and Moseley 2006, though it was based on the same theoretical model. A more recent systematic review of treatments for CRPS identified a potential therapeutic role for mirror therapy, aerobic exercise and virtual body swapping (Duong 2018). Our analyses somewhat concur with those of Duong 2018 with respect to mirror therapy and aerobic exercise in that we found very low‐certainty evidence in support of these interventions but larger, more robust trials of these interventions with longer follow‐up are required in order to provide more accurate and clinically meaningful estimates of their treatment effect. We found low‐certainty evidence from two small studies at high risk of bias that a single session of virtual body swapping does not improve pain in CRPS.
Recent clinical guidelines from the USA and the UK have placed rehabilitation therapies as first‐line treatments for people with CRPS (Goebel 2018; Harden 2013). Both guidelines describe and recommend an extensive range of possible physiotherapy modalities that might be employed. In making their recommendations, these guidelines (unlike this Cochrane Review) draw on evidence from non‐randomised studies, panel consensuses and expert opinion. This Cochrane Review highlights the fragility of the evidence underpinning these recommendations. The optimal approach to physiotherapy for people with CRPS and the true extent of potential benefits and risks remain uncertain. Also, there may be substantial redundancy within the broad range of therapies described or recommended in the guidelines.
Authors' conclusions
Implications for practice.
For adults with complex regional pain syndrome (CRPS)
The evidence is very uncertain about the effects of any of the physiotherapy interventions identified in this review, including multimodal physiotherapy, exposure‐based interventions and graded motor imagery, on the pain and disability of CRPS I at short‐, medium‐ or long‐term follow‐up when compared to various active control interventions. Despite the uncertainty, it is likely that, in line with contemporary clinical guidelines, physiotherapy and rehabilitation‐based interventions will continue to be recommended as first‐line treatments for people with CRPS.
For clinicians
There is insufficient evidence to draw any conclusions regarding the effectiveness of any of the physiotherapy interventions for CRPS I identified in this review. Multimodal physiotherapy, aerobic exercise, graded motor imagery, mirror therapy, virtual reality, TENS and 'exposure in vivo' may reduce pain and/or disability for people with CRPS I when compared to various active control interventions but the evidence is very uncertain. These effects were mainly only apparent at short‐term follow‐up. However, we have very little confidence in the current evidence. In light of the uncertainty we encourage clinicians to remain up to date with the evidence and consider ways to present this information in meaningful ways to patients that enables them to make informed decisions regarding their care. In this knowledge vacuum clinicians' treatment selection is extremely challenging and is likely to be based on their training, access to relevant expertise and support and personal preferences. Well designed, executed and reported randomised controlled trials (RCTs) are critical to better guide future patient care. We are unable to draw any conclusions regarding physiotherapy interventions for CRPS II since we found only one small clinical trial for people with CRPS II exclusively.
For policy makers and funders of interventions
The results of this review highlight the uncertainty regarding the effectiveness of any physiotherapy interventions for CRPS I or II. Despite the substantial uncertainty, clinical guidelines recommend rehabilitation therapies as a core treatment for CRPS. The challenge lies in an inability to specifically recommend any one or combined therapeutic approach. Such recommendations remain entirely contingent on the availability of data from future well‐designed and implemented clinical trials. We can say with certainty that the current state of the evidence supports the allocation of research funding for further clinical trials of physiotherapy for CRPS.
Implications for research.
General implications
Overall, given the existing limitations within the current body of evidence, there is a clear need for further research into physiotherapy interventions in people with CRPS but many challenges remain in addressing this problem. Given the relatively low incidence of CRPS, it is likely to be difficult to recruit adequate numbers of participants to clinical trials. It seems likely that the best chance of addressing this challenge is through multicentre, collaborative research projects aimed at recruiting participants from potentially larger pools of clinical populations. The use of telehealth/telerehabilitation trials could facilitate this. It seems unlikely that it will be possible to generate sufficient evidence to support the many individual modalities currently applied to people with CRPS. In this instance there remains a case for taking a pragmatic approach to developing contemporary multi‐modal, individually tailored 'best practice' models of physiotherapy care and prioritising trials of these programmes against usual or minimal care. Such trials might provide pragmatic estimates of effectiveness that best reflect the value of guideline recommended practice. Larger replication trials of graded motor imagery (GMI) and mirror therapy in particular would also be useful in order to provide more accurate estimates of treatment effect for these interventions, which current evidence suggests could offer meaningful clinical benefit.
Design implications
Large, high‐quality randomised controlled trials, with cost‐effectiveness analyses, are needed to investigate the effectiveness of physiotherapy interventions for CRPS. Where such sample sizes are not attainable, future RCTs should, at the very least, be prospectively registered and have a published trial protocol (in accordance with the SPIRIT guidelines; Chan 2013). Future trials should adhere to CONSORT guidance, including that related to the reporting of the development and evaluation of complex interventions (Möhler 2015). There should be a clear rationale outlining the mechanisms that underpin the intervention's effects and how the intervention might affect the outcomes of interest. Mechanism‐specific rehabilitation strategies, whereby treatment selection is based on clinical assessment findings that are thought to reflect the underlying mechanisms of a given patient's CRPS, have been suggested (Packham 2018). Furthermore, trialists should use established diagnostic criteria, clearly report the type and aetiology of CRPS under investigation and adequately describe interventions (according to the TIDieR guidelines; Hoffman 2014). It is our observation that rehabilitation‐based interventions for CRPS often require the ongoing active participation of patients, in the clinic, at home or both. They also have the potential to worsen patients' pain. We invite trialists to accurately report reasons for dropouts from trial arms in an attempt to record and quantify the potential burdensomeness and/or unacceptability of interventions to patients. Accurately reporting reasons for dropout might help rank treatments of apparently equivalent efficacy (or with similarly lacking evidence of efficacy) in terms of what is practicable and least likely to harm. Recommendations for the design of clinical trials of pain interventions are available (Busse 2015; Dworkin 2008; Dworkin 2009; Dworkin 2010; Turk 2008a; Turk 2008b). Finally, when therapeutic exercise is the main or significant component of an intervention, trialists could consider self‐assessing the therapeutic quality of the exercise programme included in their trial using the i‐CONTENT tool, for example (Hoogeboom 2020).
Measurement implications
The wide variety of outcome measures used together with the poor quality of reporting of trial data in a number of studies included in our review highlights the need for trialists to use core outcome sets (Grieve 2016b), adequately report their scoring properties and interpretation, report point estimates with measures of variation for all outcomes at all time points and follow up participants over clinically meaningful lengths of time. Doing so would facilitate comparisons across studies and the statistical pooling of outcome data. A core set of standardised outcome measures for use in CRPS clinical research that might enhance consistency of use and standards of reporting has been developed (Grieve 2017). There is a pressing need to improve the measurement and reporting of adverse effects in this field. In the absence of any consensus or evidence regarding cut‐points from which to interpret the magnitude of clinically important differences in pain intensity based on between‐group differences at post‐intervention time points (Dworkin 2009), trialists, clinicians, policymakers and funders may choose to follow IMMPACT or OMERACT guidance (Busse 2015; Dworkin 2008) until such time as further evidence to guide such decision‐making becomes available.
What's new
| Date | Event | Description |
|---|---|---|
| 8 August 2022 | Amended | Correction to the data reported for the comparison: Transcutaneous electrical nerve stimulation (TENS) versus sham TENS. |
History
Protocol first published: Issue 11, 2013 Review first published: Issue 2, 2016
| Date | Event | Description |
|---|---|---|
| 27 September 2021 | New citation required but conclusions have not changed | We have added 16 trials (600 participants) to this update. Our conclusions remain unchanged. |
| 27 September 2021 | New search has been performed | This review has been updated with the results of a new search in July 2021. |
| 11 March 2016 | Amended | Minor amendment to Analysis 1.2. |
Notes
Acknowledgements
We thank the editors and staff of the Cochrane Pain, Palliative and Supportive Care Review Group for their support with the review specifically Kerry Harding and Anna Erskine.
We would like to thank Information Specialist Joanne Abbott (Cochrane Pain, Palliative and Supportive Care Review Group) for running updated searches.
We would like to thank Prof. Lorimer Moseley (Professor of Clinical Neurosciences & Foundation Chair in Physiotherapy, University of South Australia) for reviewing the list of included studies in our original review and Prof. Norman Harden (Professor Emeritus of Physical Medicine and Rehabilitation, Northwestern Medicine, Feinberg School of Medicine) for reviewing our updated list of included studies.
We also thank Prof Dr Nazan Bilgel (Uludağ University, Turkey) for checking the eligibility and subsequent translation of the two papers published in Turkish, Andrea Wand for checking the eligibility and subsequent translation of the two papers published in German and an anonymous professional for checking the eligibility and subsequent translation of one paper published in Chinese. We are also grateful to three anonymous professionals for checking the eligibility of studies that were not published in the English language and subsequently excluded.
Cochrane Review Group funding acknowledgement: this project was funded by the National Institute for Health Research (NIHR) via Cochrane Infrastructure funding to the Cochrane Pain, Palliative and Supportive Care Review Group (PaPaS). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
The authors are grateful to the following peer reviewers for their time and comments: Victoria Abbott‐Fleming, Diarmuid Denneny and Eugenie Johnson.
Editorial and peer‐review contribution
The Cochrane Pain, Palliative and Supportive Care Review Group (PaPaS) supported the authors in the development of this review.
The following people conducted the editorial process for this article:
Sign‐off Editor (final editorial decision): Christopher Eccleston, Centre for Pain Research, The University of Bath, UK
Managing Editor (provided editorial guidance to authors, edited the article): Anna Erskine (Oxford University Hospitals (OUH) NHS Foundation Trust, Oxford, UK)
Assistant Managing Editor (selected peer reviewers, collated peer‐reviewer comments, conducted editorial checks and supported editorial team): Kerry Harding (Oxford University Hospitals (OUH) NHS Foundation Trust, Oxford, UK)
Contact Editor (editorial and methods guidance): Amanda Williams, University College London, London, UK
Information Specialist (searching support): Joanne Abbott (Oxford University Hospitals (OUH) NHS Foundation Trust, Oxford, UK)
Copy‐editing (initial copy‐edit and final proofread): Jenny Bellorini, Cochrane Copy‐edit Support
Peer‐reviewers (provided comments and recommended an editorial decision): Victoria Abbott‐Fleming, MBE, Founder and Chair of Burning Nights CRPS Support, UK (consumer review), Diarmuid Denneny (clinical review), Eugenie Johnson, Population Health Sciences Institute, Newcastle University, UK (clinical review),
Appendices
Appendix 1. Search strategies 2015
CENTRAL, DARE and HTA strategy
#1 MeSH descriptor: [Complex Regional Pain Syndromes] explode all trees
#2 "complex regional pain syndrome*":ti,ab,kw (Word variations have been searched)
#3 crps:ti,ab,kw (Word variations have been searched)
#4 (Post traumatic near/1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome)):ti,ab,kw (Word variations have been searched)
#5 "Minor causalgia":ti,ab,kw (Word variations have been searched)
#6 "Transient migratory osteoporosis":ti,ab,kw (Word variations have been searched)
#7 "Peripheral trophneurosis":ti,ab,kw (Word variations have been searched)
#8 ((Major or mitchell*) near/1 causalgia):ti,ab,kw (Word variations have been searched)
#9 "Neurovascular dystrophy":ti,ab,kw (Word variations have been searched)
#10 "Sudecks Osteodystrophy":ti,ab,kw (Word variations have been searched)
#11 Sympathalgia:ti,ab,kw (Word variations have been searched)
#12 Chronic traumatic oedema:ti,ab,kw (Word variations have been searched)
#13 Sympathetic dystrophy syndrome:ti,ab,kw (Word variations have been searched)
#14 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13
#15 MeSH descriptor: [Physical Therapy Modalities] explode all trees
#16 physiotherap*:ti,ab,kw (Word variations have been searched)
#17 "physical therap*":ti,ab,kw (Word variations have been searched)
#18 manual therapy:ti,ab,kw (Word variations have been searched)
#19 manipulative therapy:ti,ab,kw (Word variations have been searched)
#20 ((therapeutic or therapy) near/2 exercise):ti,ab,kw (Word variations have been searched)
#21 MeSH descriptor: [Electric Stimulation Therapy] explode all trees
#22 (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy " or "heat therapy" or cryotherapy):ti,ab,kw (Word variations have been searched)
#23 graded motor imagery:ti,ab,kw (Word variations have been searched)
#24 mirror therapy:ti,ab,kw (Word variations have been searched)
#25 MeSH descriptor: [Musculoskeletal Manipulations] explode all trees
#26 tactile sensory discriminatory training:ti,ab,kw (Word variations have been searched)
#27 sensory‐motor integration:ti,ab,kw (Word variations have been searched)
#28 sensory‐motor re‐tuning:ti,ab,kw (Word variations have been searched)
#29 hydrotherapy:ti,ab,kw (Word variations have been searched)
#30 (pain near/3 (advice or education)):ti,ab,kw (Word variations have been searched)
#31 (manipulation or massage or de‐sensiti?ation or mobili?ation):ti,ab,kw (Word variations have been searched)
#32 #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31
#33 #14 and #32
MEDLINE search strategy
1. exp Complex Regional Pain Syndromes/
2. "complex regional pain syndrome*".tw.
3. crps.tw.
4. (Post traumatic adj1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome)).tw.
5. "Minor causalgia".tw.
6. "Transient migratory osteoporosis".tw.
7. "Peripheral trophneurosis".tw.
8. "Sudeck’s Osteodystrophy".tw.
9. "Neurovascular dystrophy".tw.
10. ((Major or mitchell*) adj1 causalgia).tw.
11. Sympathalgia.tw.
12. Chronic traumatic oedema.tw.
13. Sympathetic dystrophy syndrome.tw.
14. or/1‐13
15. exp Physical Therapy Modalities/
16. physiotherap*.tw.
17. "physical therap*".tw.
18. manual therapy.tw.
19. manipulative therapy.tw.
20. ((therapeutic or therapy) adj2 exercise).tw.
21. exp Electric Stimulation Therapy/
22. (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy " or "heat therapy" or cryotherapy).tw.
23. graded motor imagery.tw.
24. mirror therapy.tw.
25. exp Musculoskeletal Manipulations/
26. tactile sensory discriminatory training.tw.
27. sensory‐motor integration.tw.
28. sensory‐motor re‐tuning.tw.
29. hydrotherapy.tw.
30. (pain adj3 (advice or education)).tw.
31. (manipulation or massage or de‐sensiti#ation or mobili#ation).tw.
32. or/15‐31
33. 14 and 32
34 randomized controlled trial.pt.
35 controlled clinical trial.pt.
36 randomized.ab.
37 placebo.ab.
38 drug therapy.fs.
39 randomly.ab.
40 trial.ab.
41 or/34‐40
42 exp animals/ not humans.sh.
43 41 not 42
44 33 and 43
Embase search strategy
1. exp Complex Regional Pain Syndromes/
2. "complex regional pain syndrome*".tw.
3. crps.tw.
4. (Post traumatic adj1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome)).tw.
5. "Minor causalgia".tw.
6. "Transient migratory osteoporosis".tw.
7. "Peripheral trophneurosis".tw.
8. "Sudeck’s Osteodystrophy".tw.
9. "Neurovascular dystrophy".tw.
10. ((Major or mitchell*) adj1 causalgia).tw.
11. Sympathalgia.tw.
12. Chronic traumatic oedema.tw.
13. Sympathetic dystrophy syndrome.tw.
14. or/1‐13
15. exp Physical Therapy Modalities/
16. physiotherap*.tw.
17. "physical therap*".tw.
18. manual therapy.tw.
19. manipulative therapy.tw.
20. ((therapeutic or therapy) adj2 exercise).tw.
21. exp Electric Stimulation Therapy/
22. (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy " or "heat therapy" or cryotherapy).tw.
23. graded motor imagery.tw.
24. mirror therapy.tw.
25. exp Musculoskeletal Manipulations/
26. tactile sensory discriminatory training.tw.
27. sensory‐motor integration.tw.
28. sensory‐motor re‐tuning.tw.
29. hydrotherapy.tw.
30. (pain adj3 (advice or education)).tw.
31. (manipulation or massage or de‐sensiti#ation or mobili#ation).tw.
32. or/15‐31
33. 14 and 32
34 random$.tw.
35 factorial$.tw.
36 crossover$.tw.
37 cross over$.tw.
38 cross‐over$.tw.
39 placebo$.tw.
40 (doubl$ adj blind$).tw.
41 (singl$ adj blind$).tw.
42 assign$.tw.
43 allocat$.tw.
44 volunteer$.tw.
45 Crossover Procedure/
46 double‐blind procedure.tw.
47 Randomized Controlled Trial/
48 Single Blind Procedure/
49 or/34‐48 (1433702)
50 (animal/ or nonhuman/) not human/
51 49 not 50
52 33 and 51
PsycINFO search strategy
1. exp "Complex Regional Pain Syndrome (Type I)"/
2. "complex regional pain syndrome*".tw.
3. crps.tw.
4. (Post traumatic adj1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome)).tw.
5. "Minor causalgia".tw.
6. "Transient migratory osteoporosis".tw.
7. "Peripheral trophneurosis".tw.
8. "Sudeck’s Osteodystrophy".tw.
9. "Neurovascular dystrophy".tw.
10. ((Major or mitchell*) adj1 causalgia).tw.
11. Sympathalgia.tw.
12. Chronic traumatic oedema.tw.
13. Sympathetic dystrophy syndrome.tw.
14. or/1‐13
15. exp Physical Therapy/
16. physiotherap*.tw.
17. "physical therap*".tw.
18. manual therapy.tw.
19. manipulative therapy.tw.
20. ((therapeutic or therapy) adj2 exercise).tw.
21. exp Electrical Stimulation/
22. (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy " or "heat therapy" or cryotherapy).tw.
23. graded motor imagery.tw.
24. mirror therapy.tw.
25. tactile sensory discriminatory training.tw.
26. sensory‐motor integration.tw.
27. sensory‐motor re‐tuning.tw.
28. hydrotherapy.tw.
29. (pain adj3 (advice or education)).tw.
30. (manipulation or massage or de‐sensiti#ation or mobili#ation).tw.
31. or/15‐30
32. 14 and 31
33. clinical trials/
34. (randomis* or randomiz*).tw.
35. (random$ adj3 (allocat$ or assign$)).tw.
36. ((clinic$ or control$) adj trial$).tw.
37. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
38. (crossover$ or "cross over$").tw.
39. random sampling/
40. Experiment Controls/
41. Placebo/
42. placebo$.tw.
43. exp program evaluation/
44. treatment effectiveness evaluation/
45. ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw.
46. or/33‐45
47. 32 and 46
CINAHL search strategy
S43 S33 AND S42
S42 S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41
S41 (allocat* random*)
S40 (MH "Quantitative Studies")
S39 (MH "Placebos")
S38 placebo*
S37 (random* allocat*)
S36 (MH "Random Assignment")
S35 (Randomi?ed control* trial*)
S34 (singl* blind* ) or (doubl* blind* ) or (tripl* blind* ) or (trebl* blind* ) or (trebl* mask* ) or (tripl* mask* ) or
(doubl* mask* ) or (singl* mask* )
S33 S14 AND S32
S32 S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31
S31 (manipulation or massage or de‐sensiti?ation or mobili?ation)
S30 (pain N3 (advice or education))
S29 hydrotherapy
S28 sensory‐motor re‐tuning
S27 sensory‐motor integration
S26 tactile sensory discriminatory training
S25 (MH "Manual Therapy+")
S24 mirror therapy
S23 graded motor imagery
S22 (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy " or "heat therapy" or cryotherapy)
S21 (MH "Transcutaneous Electrical Nerve Stimulation (Iowa NIC)")
S20 ((therapeutic or therapy) N2 exercise)
S19 manipulative therapy
S18 manual therapy
S17 "physical therap*"
S16 physiotherap*
S15 (MH "Physical Therapy+")
S14 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13
S13 Sympathetic dystrophy syndrome
S12 Chronic traumatic oedema
S11 Sympathalgia
S10 ((Major or mitchell*) N1 causalgia)
S9 "Neurovascular dystrophy"
S8 "Sudeck’s Osteodystrophy"
S7 "Peripheral trophneurosis"
S6 "Transient migratory osteoporosis"
S5 "Minor causalgia"
S4 (Post traumatic N1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome))
S3 crps
S2 "complex regional pain syndrome*"
S1 (MH "Complex Regional Pain Syndromes+")
LILACS search strategy
1. "crps"
2. "physiotherapy"
3. "clinical trial"
PEDro search strategy
1. "complex regional pain syndrome"
2. "reflex sympathetic dystrophy"
3. "causalgia"
4. "sudeks'"
5. "sympathetic pain"
6. "clinical trial"
Web of Science search strategy
1. "crps"
2. "physiotherapy"
3. "orthopaedic rehabilitation"
4. "articles"
Appendix 2. Update search strategies (February 2015 to July 2020)
CENTRAL search strategy
#1 MeSH descriptor: [Complex Regional Pain Syndromes] explode all trees
#2 "complex regional pain syndrome*":ti,ab,kw (Word variations have been searched)
#3 crps:ti,ab,kw (Word variations have been searched)
#4 (Posttraumatic near/1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome)):ti,ab,kw (Word variations have been searched)
#5 "Minor causalgia":ti,ab,kw (Word variations have been searched)
#6 "Transient migratory osteoporosis":ti,ab,kw (Word variations have been searched)
#7 "Peripheral trophneurosis":ti,ab,kw (Word variations have been searched)
#8 ((Major or mitchell*) near/1 causalgia):ti,ab,kw (Word variations have been searched)
#9 "Neurovascular dystrophy":ti,ab,kw (Word variations have been searched)
#10 "Sudecks Osteodystrophy":ti,ab,kw (Word variations have been searched)
#11 Sympathalgia:ti,ab,kw (Word variations have been searched)
#12 Chronic traumatic oedema:ti,ab,kw (Word variations have been searched)
#13 Sympathetic dystrophy syndrome:ti,ab,kw (Word variations have been searched)
#14 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13
#15 MeSH descriptor: [Physical Therapy Modalities] explode all trees
#16 physiotherap*:ti,ab,kw (Word variations have been searched)
#17 "physical therap*":ti,ab,kw (Word variations have been searched)
#18 manual therapy:ti,ab,kw (Word variations have been searched)
#19 manipulative therapy:ti,ab,kw (Word variations have been searched)
#20 ((therapeutic or therapy) near/2 exercise):ti,ab,kw (Word variations have been searched)
#21 MeSH descriptor: [Electric Stimulation Therapy] explode all trees
#22 (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy" or "heat therapy" or cryotherapy):ti,ab,kw (Word variations have been searched)
#23 graded motor imagery:ti,ab,kw (Word variations have been searched)
#24 mirror therapy:ti,ab,kw (Word variations have been searched)
#25 MeSH descriptor: [Musculoskeletal Manipulations] explode all trees
#26 tactile sensory discriminatory training:ti,ab,kw (Word variations have been searched)
#27 sensory‐motor integration:ti,ab,kw (Word variations have been searched)
#28 sensory‐motor re‐tuning:ti,ab,kw (Word variations have been searched)
#29 hydrotherapy:ti,ab,kw (Word variations have been searched)
#30 (pain near/3 (advice or education)):ti,ab,kw (Word variations have been searched)
#31 (manipulation or massage or de‐sensiti?ation or mobili?ation):ti,ab,kw (Word variations have been searched)
#32 MeSH descriptor: [Implosive Therapy] explode all trees
#33 ("Bio‐Electro‐Magnetic‐Energy‐Regulation"):ti,ab,kw (Word variations have been searched)
#34 (neuromuscular electrical stimulation):ti,ab,kw (Word variations have been searched)
#35 (Electromagnetic Field Therapy):ti,ab,kw (Word variations have been searched)
#36 (Virtual body swapping):ti,ab,kw (Word variations have been searched)
#37 ("Action observation"):ti,ab,kw (Word variations have been searched)
#38 (Mental visuali*ation):ti,ab,kw (Word variations have been searched)
#39 ("Pain‐contingent treatment*"):ti,ab,kw (Word variations have been searched)
#40 MeSH descriptor: [Transcranial Direct Current Stimulation] this term only
#41 (Transcranial direct current stimulation):ti,ab,kw (Word variations have been searched)
#42 MeSH descriptor: [Desensitization, Psychologic] explode all trees
#43 (Desensiti*ation):ti,ab,kw (Word variations have been searched)
#44 #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43
#45 #14 and #44 with Cochrane Library publication date Between Feb 2015 and Jul 2020, in Trials
MEDLINE and MEDLINE in process search strategies
1 exp Complex Regional Pain Syndromes/ (5534)
2 "complex regional pain syndrome*".tw. (2996)
3 crps.tw. (2313)
4 (Post traumatic adj1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome)).tw. (51)
5 "Minor causalgia".tw. (8)
6 "Transient migratory osteoporosis".tw. (7)
7 "Peripheral trophneurosis".tw. (0)
8 "Sudeck’s Osteodystrophy".tw. (7)
9 "Neurovascular dystrophy".tw. (25)
10 ((Major or mitchell*) adj1 causalgia).tw. (6)
11 Sympathalgia.tw. (17)
12 Chronic traumatic oedema.tw. (0)
13 Sympathetic dystrophy syndrome.tw. (223)
14 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 (7267)
15 exp Physical Therapy Modalities/ (152617)
16 physiotherap*.tw. (25431)
17 "physical therap*".tw. (22290)
18 manual therapy.tw. (2024)
19 manipulative therapy.tw. (831)
20 ((therapeutic or therapy) adj2 exercise).tw. (5752)
21 exp Electric Stimulation Therapy/ (79793)
22 (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy " or "heat therapy" or cryotherapy).tw. (34642)
23 graded motor imagery.tw. (53)
24 mirror therapy.tw. (339)
25 exp Musculoskeletal Manipulations/ (16656)
26 tactile sensory discriminatory training.tw. (0)
27 sensory‐motor integration.tw. (295)
28 sensory‐motor re‐tuning.tw. (0)
29 hydrotherapy.tw. (958)
30 (pain adj3 (advice or education)).tw. (1707)
31 (manipulation or massage or de‐sensiti#ation or mobili#ation).tw. (159532)
32 exp Implosive Therapy/ (1277)
33 "Bio‐Electro‐Magnetic‐Energy‐Regulation".tw. (5)
34 neuromuscular electrical stimulation.tw. (1220)
35 Electromagnetic Field Therapy.tw. (136)
36 Virtual body swapping.tw. (3)
37 "Action observation".tw. (1169)
38 Mental visuali#ation.tw. (32)
39 "Pain‐contingent treatment*".tw. (2)
40 Transcranial Direct Current Stimulation/ (2610)
41 Transcranial direct current stimulation.tw. (4216)
42 exp Desensitization, Psychologic/ (3597)
43 Desensiti#ation.tw. (23332)
44 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 (443161)
45 14 and 44 (1120)
46 randomized controlled trial.pt. (509322)
47 controlled clinical trial.pt. (93750)
48 randomized.ab. (485366)
49 placebo.ab. (209221)
50 drug therapy.fs. (2218451)
51 randomly.ab. (336638)
52 trial.ab. (511833)
53 or/46‐52 (3199899)
54 exp animals/ not humans.sh. (4715958)
55 53 not 54 (2864561)
56 45 and 55 (305)
57 (201502* or 201503* or 201504* or 201505* or 201506* or 201507* or 201508* or 201509* or 201510* or 201511* or 201512* or 2016* or 2017* or 2018* or 2019* or 2020*).ed. (5490256)
58 56 and 57 (92)
Embase search strategy
1 exp Complex Regional Pain Syndromes/ (8973)
2 "complex regional pain syndrome*".tw. (4356)
3 crps.tw. (3714)
4 (Post traumatic adj1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome)).tw. (40)
5 "Minor causalgia".tw. (5)
6 "Transient migratory osteoporosis".tw. (11)
7 "Peripheral trophneurosis".tw. (0)
8 "Sudeck’s Osteodystrophy".tw. (4)
9 "Neurovascular dystrophy".tw. (18)
10 ((Major or mitchell*) adj1 causalgia).tw. (4)
11 Sympathalgia.tw. (9)
12 Chronic traumatic oedema.tw. (0)
13 Sympathetic dystrophy syndrome.tw. (260)
14 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 (10515)
15 exp Physical Therapy Modalities/ (83424)
16 physiotherap*.tw. (43543)
17 "physical therap*".tw. (32013)
18 manual therapy.tw. (2817)
19 manipulative therapy.tw. (868)
20 ((therapeutic or therapy) adj2 exercise).tw. (7641)
21 exp Electric Stimulation Therapy/ (229342)
22 (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy " or "heat therapy" or cryotherapy).tw. (41207)
23 graded motor imagery.tw. (86)
24 mirror therapy.tw. (559)
25 exp Musculoskeletal Manipulations/ (3181)
26 tactile sensory discriminatory training.tw. (0)
27 sensory‐motor integration.tw. (383)
28 sensory‐motor re‐tuning.tw. (0)
29 hydrotherapy.tw. (1197)
30 (pain adj3 (advice or education)).tw. (2456)
31 (manipulation or massage or de‐sensiti#ation or mobili#ation).tw. (190293)
32 exp Implosive Therapy/ (151)
33 "Bio‐Electro‐Magnetic‐Energy‐Regulation".tw. (8)
34 neuromuscular electrical stimulation.tw. (1585)
35 Electromagnetic Field Therapy.tw. (168)
36 Virtual body swapping.tw. (3)
37 "Action observation".tw. (1354)
38 Mental visuali#ation.tw. (41)
39 "Pain‐contingent treatment*".tw. (3)
40 Transcranial Direct Current Stimulation/ (7038)
41 Transcranial direct current stimulation.tw. (6207)
42 exp Desensitization, Psychologic/ (76)
43 Desensiti#ation.tw. (28151)
44 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 (598234)
45 14 and 44 (2534)
46 random$.tw. (1533554)
47 factorial$.tw. (37636)
48 crossover$.tw. (74476)
49 cross over$.tw. (31451)
50 cross‐over$.tw. (31451)
51 placebo$.tw. (303445)
52 (doubl$ adj blind$).tw. (203145)
53 (singl$ adj blind$).tw. (24789)
54 assign$.tw. (391068)
55 allocat$.tw. (152083)
56 volunteer$.tw. (250549)
57 Crossover Procedure/ (63463)
58 double‐blind procedure.tw. (202)
59 Randomized Controlled Trial/ (605488)
60 Single Blind Procedure/ (39339)
61 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 (2296773)
62 (animal/ or nonhuman/) not human/ (5591375)
63 61 not 62 (2032509)
64 45 and 63 (317)
65 (201502* or 201503* or 201504* or 201505* or 201506* or 201507* or 201508* or 201509* or 201510* or 201511* or 201512* or 2016* or 2017* or 2018* or 2019* or 2020*).dd. (4258933)
66 64 and 65 (60)
PsycINFO search strategy
S55 S45 AND S53 Limiters ‐ Publication Year: 2015‐2020
S54 S45 AND S53
S53 S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52
S52 (singl* OR doubl* OR trebl* OR tripl*) N3 (blind* OR mask*)
S51 clinical N3 trial* OR research N3 design OR evaluat* N3 stud* OR prospectiv* N3 stud*
S50 placebo* OR random* OR "comparative stud*"
S49 DE "Followup Studies"
S48 DE "Placebo"
S47 DE "Treatment Outcomes" OR DE "Psychotherapeutic Outcomes" OR DE "Side Effects (Treatment)" OR DE "Treatment Compliance" OR DE "Treatment Duration" OR DE "Treatment Refusal" OR DE "Treatment Termination" OR DE "Treatment Withholding"
S46 DE "Treatment Effectiveness Evaluation"
S45 S14 AND S44
S44 S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43
S43 desensitization
S42 (MH "Desensitization, Psychologic+")
S41 Transcranial direct current stimulation
S40 (MH "Transcranial Direct Current Stimulation")
S39 "Pain‐contingent treatment*"
S38 "Mental visuali?ation"
S37 "Action observation"
S36 "Virtual body swapping"
S35 "Electromagnetic Field Therapy"
S34 neuromuscular electrical stimulation
S33 "Bio‐Electro‐Magnetic‐Energy‐Regulation"
S32 (MH "Behavior Therapy+")
S31 (manipulation or massage or de‐sensiti?ation or mobili?ation)
S30 (pain N3 (advice or education))
S29 hydrotherapy
S28 sensory‐motor re‐tuning
S27 sensory motor integration
S26 tactile sensory discriminatory training
S25 (MH "Manual Therapy+")
S24 mirror therapy
S23 graded motor imagery
S22 (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy " or "heat therapy" or cryotherapy)
S21 (MH "Transcutaneous Electrical Nerve Stimulation (Iowa NIC)")
S20 ((therapeutic or therapy) N2 exercise)
S19 manipulative therapy
S18 manual therapy
S17 "physical therap*"
S16 physiotherap*
S15 (MH "Physical Therapy+")
S14 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13
S13 Sympathetic dystrophy syndrome
S12 Chronic traumatic oedema
S11 Sympathalgia
S10 ((Major or mitchell*) N1 causalgia)
S9 "Neurovascular dystrophy"
S8 "Sudeck’s Osteodystrophy"
S7 "Peripheral trophneurosis"
S6 "Transient migratory osteoporosis"
S5 "Minor causalgia"
S4 (Post traumatic N1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome))
S3 crps
S2 "complex regional pain syndrome*"
S1 (MH "Complex Regional Pain Syndromes+")
CINAHL search strategy
(+RCT filter)
S45 S14 AND S44
S44 S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43
S43 desensitization
S42 (MH "Desensitization, Psychologic+")
S41 Transcranial direct current stimulation
S40 (MH "Transcranial Direct Current Stimulation")
S39 "Pain‐contingent treatment*"
S38 "Mental visuali?ation"
S37 "Action observation"
S36 "Virtual body swapping"
S35 "Electromagnetic Field Therapy"
S34 neuromuscular electrical stimulation
S33 "Bio‐Electro‐Magnetic‐Energy‐Regulation"
S32 (MH "Behavior Therapy+")
S31 (manipulation or massage or de‐sensiti?ation or mobili?ation)
S30 (pain N3 (advice or education))
S29 hydrotherapy
S28 sensory‐motor re‐tuning
S27 sensory motor integration
S26 tactile sensory discriminatory training
S25 (MH "Manual Therapy+")
S24 mirror therapy
S23 graded motor imagery
S22 (electrotherapy or TENS or "transcutaneous electrical nerve stimulation" or "therapeutic ultrasound" or interferential or "shortwave diathermy" or "laser therapy " or "heat therapy" or cryotherapy)
S21 (MH "Transcutaneous Electrical Nerve Stimulation (Iowa NIC)")
S20 ((therapeutic or therapy) N2 exercise)
S19 manipulative therapy
S18 manual therapy
S17 "physical therap*"
S16 physiotherap*
S15 (MH "Physical Therapy+")
S14 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13
S13 Sympathetic dystrophy syndrome
S12 Chronic traumatic oedema
S11 Sympathalgia
S10 ((Major or mitchell*) N1 causalgia)
S9 "Neurovascular dystrophy"
S8 "Sudeck’s Osteodystrophy"
S7 "Peripheral trophneurosis"
S6 "Transient migratory osteoporosis"
S5 "Minor causalgia"
S4 (Post traumatic N1 (algodystrophy or dystrophy or neurodystrophy or osteoporosis or pain syndrome))
S3 crps
S2 "complex regional pain syndrome*"
S1 (MH "Complex Regional Pain Syndromes+")
PEDro search strategy
1. "complex regional pain syndrome"
2. "reflex sympathetic dystrophy"
3. "causalgia"
4. "sudeks'"
5. "sympathetic pain"
6. "clinical trial"
LILACS search strategy
1. “crps”
2. “physiotherapy”
3. “clinical trial”
Web of Science search strategy
1. "complex regional pain syndrome"
2. "articles"
3. "proceedings"
4. "randomized controlled trial"
Data and analyses
Comparison 1. Graded motor imagery versus standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Pain intensity (0 to 100 VAS; higher scores indicate worse pain) (post‐treatment) | 2 | 49 | Mean Difference (IV, Random, 95% CI) | ‐14.45 [‐23.02, ‐5.87] |
| 1.2 Disability (0 to 10 patient‐specific functional scale; higher scores indicate better function) (post‐treatment) | 2 | 49 | Mean Difference (IV, Random, 95% CI) | 1.87 [1.03, 2.71] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Askin 2014.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 3‐arm, single‐blind RCT Setting: outpatient hospital clinic (Turkey; dates not reported) Interventions: conventional care plus low‐dose, high‐frequency ultrasound therapy (0.5 watts/cm²) for stellate ganglion blockade or conventional care plus low‐dose, high‐frequency ultrasound therapy (3.0 watts/cm²) for stellate ganglion blockade or conventional care plus placebo ultrasound therapy Sample size calculation: not reported |
|
| Participants |
Number of participants: 45 (15 in each group) Type of noxious initiating event: mixed (fracture of the distal radius (n = 17), tendon injury (n = 10), hand contusion (n = 5), postsurgery for carpal tunnel syndrome (n = 4), fracture of the elbow (n = 2), fracture of the humerus (n = 1), fracture of the finger (n = 1)) (upper limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in all 3 groups received conventional care including:
Conventional care plus low‐dose, high‐frequency ultrasound therapy (0.5 watts/cm²) (n = 15) Components of intervention: using a Enraf Nonius Sonopuls (590 model) therapeutic ultrasound of the stellate ganglion was applied by placing the 1 cm² ultrasound head at the level of transverse process of the 7th vertebra and 3 cm to 4 cm above the sternoclavicular joint, using a 1 MHz frequency and pulsed pattern of 1:4 Dosage: 0.5 watts/cm², for 5 minutes Frequency of administration: not reported (5 times per week for 4 weeks (20 sessions)) (Askin, personal communication). Provider: not reported Conventional care plus low‐dose, high‐frequency ultrasound therapy (3.0 watts/cm²) (n = 15) Components of intervention: ultrasound procedure as described above Dosage: 3.0 watts/cm², for 5 minutes Frequency of administration: 5 times per week for 4 weeks (20 sessions) Provider: not reported Conventional care plus placebo ultrasound therapy (n = 15) Components of intervention: ultrasound procedure as described above, with the machine turned off |
|
| Outcomes | Time points at which outcomes were measured were not explicitly specified in the trial report. Outcomes were assessed at baseline and on completion of the intervention period (4 weeks post recruitment) (Askin, personal communication). The trial authors did not state any primary outcome.
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients were randomly divided into 3 groups by picking cards in different colours. First, three groups of cards (each group consisted of 15 cards) in 3 different colours (blue for 3 watts/cm2, pink for 0.5 watts/cm2, yellow for placebo) were prepared. Participants were asked to choose a card before starting the treatment. The US dose was determined according to the colour of the selected card and it was recorded. The randomisation process was performed by another physician". Comment: the trial authors used a non‐random sequence generation process. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "No information was given to patients and to the physician who will make assessments and US application about the randomisation process until the end of the study". Comment: the participants were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Quote: "No information was given to patients and to the physician who will make assessments and US application about the randomisation process until the end of the study". |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "No information was given to patients and to the physician who will make assessments and US application about the randomisation process until the end of the study". |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "Thirteen patients from group I, 13 patients from group II and 14 patients from group III, a total of 40 patients completed the study". Comment: an overall dropout rate of 11% is unlikely to have biased the results. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Quote: "Two patients from group I, 2 patients from group II and 1 patient from group III who did not come to therapy sessions regularly were excluded". Comment: the trial authors excluded 5 participants in violation of the ITT principle. |
| Selective reporting (reporting bias) | Low risk | Comment: outcome data were fully reported for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "Fourty‐five patients with CRPS type I were randomly allocated into three groups". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "Before and after the treatment the severity of the pain experienced at rest was assessed". Comment: outcomes were re‐measured on completion of the intervention period only and were not measured over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Aydemir 2006.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 3‐arm, double‐blind RCT Setting: Department of Physical Medicine and Rehabilitation Clinic, Gulhane Military Medical Academy (Turkey; dates not reported) Interventions: stellate ganglion block (SGB) with lidocaine and sham SGB with ultrasound (US) or SGB with US and sham SGB with lidocaine or sham SGB with lidocaine and sham SGB with US Sample size calculation: not reported |
|
| Participants |
Number of participants: 25 (SGB with lidocaine (n = 9); SGB with US (n = 9); sham SGB with lidocaine and sham SGB with US (n = 7)) Type of noxious initiating event: mixed (trauma n = 12, fracture n = 11, idiopathic n = 2) (upper limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in all 3 groups received 21 sessions of exercise (active, active assisted, passive exercises for the wrist and fingers, twice daily supervised by the same physiotherapist), contrast baths (extremities were put in 38 °C hot water, 4 °C cold water for 4 minutes hot and 1 minute cold, 4 minutes cold and 1 minute hot and 4 minutes cold (total time 14 minutes)), transcutaneous electrical nerve stimulation (Enraf Nonius Endomed 582 instrument; for a period of 20 minutes with a frequency of 100 Hz), external pneumatic compression (involved extremity was compressed by a pressure of 50 mmHg for a period of 60 seconds and then pressure was released for 20 seconds and this compression and release procedure was repeated for 15 minutes, for participants who could not tolerate the 50 mmHg pressure a lower level pressure was used) and paracetamol (500 mg orally every 4 hours, maximum dosage of 3 g/daily was given if it is needed). Stellate ganglion block with lidocaine (n = 9) Components of intervention:
Dosage: 10 mL of 1% lidocaine Frequency of administration: not reported Provider: anaesthetist (other providers not reported) Stellate ganglion block with ultrasound (n = 9) Components of intervention:
Dosage: 3 watt/cm² for 5 minutes Frequency of administration: not reported Provider: anaesthetist (other providers not reported) Sham stellate ganglion block with lidocaine and ultrasound (n = 7) Components of intervention:
Dosage: n/a Frequency of administration: not reported Provider: anaesthetist (other providers not reported) |
|
| Outcomes | Outcomes assessed at baseline, after treatment and 1 month post‐treatment:
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised by envelope method and 3 groups were established". Comment: "Treatment orders were made online..." Comment: it is likely that the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomised by envelope method and 3 groups were established". Comment: the trial authors did not adequately report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The study was designed as a double blind study. Treatment orders were made online and except the personnel who were involved in the therapy nobody even the doctor was aware of the selected method". Comment: participants were likely to have been adequately blinded. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Quote: "The study was designed as a double blind study. Treatment orders were made online and except the personnel who were involved in the therapy nobody even the doctor was aware of the selected method". Comment: participants who completed self‐reported outcome measures were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "Treatment orders were made online and except the personnel who were involved in the therapy nobody even the doctor was aware of the selected method". Comment: the outcome assessor was blinded to the treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Comment: the dropout rate was not reported. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the method of analysis (ITT versus per protocol) was not reported. |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "Twenty‐five patients were divided into three groups". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Unclear risk | Quote: "These evaluations were performed before and after treatment and one month later". Comment: the clinical relevance of a 1‐month follow‐up of outcomes is uncertain. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Barnhoorn 2015.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, single‐blind RCT Setting: university hospital (Level 1 trauma centre) in a rural area of The Netherlands (The Netherlands; from 9 January 2009 to 7 March 2012) Interventions: pain exposure physical therapy (PEPT) or conventional treatment Sample size calculation: 62 patients (31 per group) were required based on an α of 0.05 and a power of 80% for a one‐sided Chi2 test, and based on an expected proportion of responders of 80% in the experimental group and 50% in the control group |
|
| Participants |
Number of participants: 56 (28 in each group) Type of noxious initiating event: not reported (upper and lower limb) Diagnostic criteria:Harden 2007 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
PEPT (n = 28) A functional form of physical therapy combined with a cognitive behavioural form of treatment. Components of intervention:
Dosage: 40 minutes per session Frequency of administration: maximum of 5 treatment sessions, with varying intervals between the sessions depending on the progression and personal needs of the patient Provider: physical therapists Conventional treatment (n = 28) Components of intervention:
Dosage: not reported Frequency of administration: no predefined limits, on average 15 to 20 sessions Provider: anaesthesiologist, physical therapist, rehabilitation physician |
|
| Outcomes | Outcomes assessed at baseline and at 3, 6 and 9 months post randomisation
|
|
| Notes |
Source of funding: The Netherlands Organisation for Health Research and Development sponsored this study (grant number 170991004). The sponsor had no role in the study design, data collection, data analysis, data interpretation or writing of the report. Statement regarding declarations of interest: the authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A statistician who had no clinical involvement in the trial designed a computerised randomisation program". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Low risk | Quote: "An independent person allocated patients to one of the two treatment groups...in a 1:1 ratio using the randomisation program". Comment: the trial authors probably used an acceptable method to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Given the nature of the interventions, it was not possible to blind the patients and the therapists". Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. VAS for pain). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "The trained research nurse (TT) who performed all assessments prior to randomisation and during follow‐up was blinded to the treatment allocation". Comment: the outcome assessor of investigator‐administered outcomes was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "One patient in the PEPT group dropped out after two treatment sessions because of complete recovery. One patient in the CONV group was not confident about the treatment and was lost to follow‐up. Another patient in the CONV group stopped without offering a reason". Comment: a small dropout rate is unlikely to have biased the results. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Quote: "We conducted the statistical analysis following the intention‐to‐treat principle (ITT): patients were analysed in the groups to which they were allocated". Comment: the trial authors analysed participants in the group to which they were allocated. |
| Selective reporting (reporting bias) | Unclear risk | Comment: the primary outcome measure was reported in accordance with the published protocol but there are a number of discrepancies in reported outcome measures between the published protocol and the trial report. |
| Sample size | High risk | Quote: "The resulting 56 patients were randomly allocated to either PEPT (n=28) or [conventional treatment] (n=28)" Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Low risk | Quote: "Further measurements are taken during the course of the treatment at three months (T1) and at the end of the treatment at six months (T2). Follow up is at nine months (T3) after inclusion". Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | Unclear risk | Quote: "This trial was prospectively registered at http://www.clinicaltrials.gov, NCT0081 7128". Quote: "The study protocol and rationale of both treatment strategies have been published elsewhere". Comment: the trial was prospectively registered and a trial protocol published. Quote: "Prior to treatment initiation, four patients (14%) in the PEPT group and 11 patients (39%) in the [conventional treatment] group opted out of their assigned treatment and switched groups". Quote: "During the course of the trial, three additional patients switched from [conventional treatment] to PEPT due to insufficient results with their treatment". Comment: a total of 14 (50% of the conventional treatment group) patients voluntarily switched groups, which may have compromised the internal validity of the study. |
Benedetti 2018.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, double‐blind pilot RCT Setting: level‐2 public outpatient clinic for orthopaedic rehabilitation (Italy; patients attending between 2013 to 2016 were considered eligible; exact trial dates not reported) Interventions: rehabilitation plus Bio‐Electro‐Magnetic‐Energy‐Regulation (BEMER) or rehabilitation plus placebo BEMER Sample size calculation: "Sample size (15 patients per group) was established a priori, based on a standard deviation of 1, a minimal clinically significant difference of 3 cm in the VAS between pre‐ and post‐treatment, a significance of 0.05, and a power of > 0.8 using G*Power 3.1.9.2." |
|
| Participants |
Number of participants: 30 (15 in each group) Type of noxious initiating event: mixed (post fracture n = 23, soft‐tissue injury/condition n = 2, post surgery n = 4, postraumatic talar bone oedema n = 1 (upper or lower limb) Diagnostic criteria: "Budapest criteria" (Harden 2007) (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in both groups received rehabilitation for 2 hours per day, for 10 consecutive days, delivered by a physiotherapist, including:
Rehabilitation plus BEMER (n = 15) Components of intervention: Make and model of the device used to deliver BEMER not reported. Patients were treated with "total body" stimulation supplied by a flexible panel (180 × 50 cm) placed underneath the patient laying in supine position, and a local stimulation supplied by a flexible pad (50 × 15cm) positioned depending on the anatomical distribution of CRPS‐I. The BEMER signal is made up of a sequence of PEMF induced by flat and flexible electric coils, with low frequency (< 33.3 Hz) and very low intensity (total body: 7 to 35 microTesla, local pad: 60 to 100 microTesla). The signal starts from lower values of intensity and increases by few microTesla at each pulse. In this way, the initial value of each pulse is higher than the previous one and the deviation from zero increases gradually up to the maximal values. After that, the value decreases every 30 ms until it goes back to zero. After 2 minutes, the magnetic field changes its polarity. Dosage: 20 minutes per session Frequency of administration: once per day for 10 days Provider: physiatrists, physiotherapists Rehabilitation plus placebo BEMER (n = 15) Components of intervention: participants were positioned in the same way, the device was turned on but the treatment was not delivered Dosage: 20 minutes per session Frequency of administration: once per day for 10 days Provider: physiatrists, physiotherapists |
|
| Outcomes | Outcomes assessed at baseline, at the end of the 10‐day treatment period and 1 month post‐treatment
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: the authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Simple randomization was formulated a priori using a system of computer‐generated random numbers". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "According to the sequence of numbers obtained, patients were allocated in two groups". Comment: the trial authors did not adequately report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Since BEMER therapy does not give patients any sensation (e.g., feeling of warmth or tingling), patients were not aware of the difference and they were unaware of the group they belonged". Comment: the participants were blinded to treatment allocation. Comment: the trial authors did not report the procedure for blinding of care providers. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Quote: "Since BEMER therapy does not give patients any sensation (e.g., feeling of warmth or tingling), patients were not aware of the difference and they were unaware of the group they belonged". Comment: the participants who completed self‐reported outcome measures were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "Assessment data were collected by a physiotherapist, and then analyzed by the statistician, blinded to the groups’ assignment. Comment: the outcome assessor was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "Thirty patients accepted to participate to the study and completed the follow‐up assessment, 15 in each group". Comment: all randomly assigned participants completed the study. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the trial authors did not report the method of analysis (ITT versus per protocol). |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "Thirty patients accepted to participate to the study and completed the follow‐up assessment". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Unclear risk | Quote: "Study participants were assessed at the beginning of treatment (T0), at the end of treatment (T1), and at follow‐up (T2, 1 month after T1)". Comment: the trial authors did not measure outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Bilgili 2016.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT Setting: Physical Therapy and Rehabilitation Outpatient Clinic of Antalya Education and Research State Hospital (Turkey; recruitment from 2012 to 2013) Interventions: transcutaneous electrical nerve stimulation (TENS) plus standard physical therapy or sham TENS plus standard physical therapy Sample size calculation: not reported |
|
| Participants |
Number of participants: 30 (15 in each group) Type of noxious initiating event: mixed (fracture of the distal radius (n = 21), excision of cystic mass from soft tissue (n= 2), fracture of the radial corpus (n = 1), fracture of the 1st metacarpal bone (n = 1), fracture of the radial head (n = 1), fracture of the scaphoid (n = 1), fracture of the olecranon and triceps tendon rupture (n = 1), ligament injury in the 5th proximal interphalangeal joint (n = 1), (1 case unaccounted for)) (upper limb) Diagnostic criteria:Merskey 1994 (Stage I or Stage II CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in both groups received standard physical therapy, including contrast bath for 20 minutes; whirlpool bath for 15 minutes; assisted active and passive range of motion, and static stretching exercises up to the pain threshold (15 sessions). Participants were allowed to use paracetamol according to their pain status (maximum dose 4g/day). TENS (n = 15) Components of intervention: TENS was applied using a CHATTANOGA Intelect Mobile Stim 2777. Two carbon electrodes (6 × 8 cm in size) were placed on the involved extremity using wet pads, with the active electrode on the dorsal aspect of the forearm and the passive electrode on the dorsal aspect of the hand. Dosage: frequency 100 Hz, pulse duration, 50 ms to 100 ms; and amplitude that did not cause discomfort to the patient or muscle contraction Frequency of administration: not reported (total of 15 sessions) Provider: not reported Sham TENS (n = 15) Components of intervention: the electrodes were placed on the involved extremity in a similar manner. The TENS device was operated but no current was given. Frequency of administration: not reported (total of 15 sessions) Provider: not reported |
|
| Outcomes | Outcomes assessed at baseline and on completion of the intervention period.
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: the authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Randomization was performed by a physician who did not participate in the study. Thirty cards with two distinct colors were prepared. The patients were asked to choose a card, which was then used to allocate the patient to one of the treatment groups." Comment: the trial authors used a non‐random sequence generation process. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Thirty cards with two distinct colors were prepared. The patients were asked to choose a card, which was then used to allocate the patient to one of the treatment groups. The patients and physicians were blinded to the randomization". Comment: the trial authors did not adequately report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Sham TENS: The electrodes were placed on the involved extremity in a similar manner. The TENS device was operated but no current was given". Comment: given the nature of the intervention and our knowledge of TENS, we judge that the sham intervention did not control for the auditory and/or sensory characteristics of the real intervention and as such participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. VAS for pain). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Quote: "The patients and physicians were blinded to the randomization". Comment: the trial authors did not provide a statement of procedures regarding blinding of the outcome assessor. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Comment: the trial authors did not report the dropout rate. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the trial authors did not report the method of analysis (ITT versus per protocol). |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "The study included 30 patients with stage 1 and 2 CRPS Type I in the upper extremities". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "Only short‐term follow‐up results were evaluated with assessments performed at baseline and after treatment. No long‐term results were available". Comment: the trial authors did not measure outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Bϋyϋkturan 2018.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, single‐blind RCT Setting: Ahi Evran University Training and Research Hospital (Turkey; from September 2014 to February 2016) Interventions: electromagnetic field therapy (EMFT) plus physiotherapy or placebo EMFT plus physiotherapy Sample size calculation: assuming a large effect size, with a statistical significance level of 5% (P = 0.05), statistical power of 80%, and an effect size of 0.8, a minimum of 21 participants were required per group |
|
| Participants |
Number of participants: 42 (21 in each group) Type of noxious initiating event: mixed (fractured elbow (n = 11), fractured distal radius (n = 10), fractured ulnar styloid process (n = 3), tendon injury (n = 9), hand contusion (n = 5), fractured shaft of humerus (n = 3, fractured index finger (n = 1)) (upper limb) Diagnostic criteria:Harden 2007 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in both groups were i) permitted to take non‐steroidal anti‐inflammatory drugs and/or analgesics and ii) received physiotherapy including passive (weeks 1 and 2), active‐assistive (weeks 3 and 4), and active (weeks 5 and 6) daily range of motion (ROM) exercises for the wrist (flexion, extension, radial and ulnar deviation) and fingers (flexion and extension) (3 sets of 10 repetitions, 5 times per week for 6 weeks; total 30 sessions). Participants were also given 'instructions' and 'informative explanations' (details not reported). EMFT (n = 21) Components of intervention: treatment was administered using a MG WAVE Magnetotherapy (Via Canapa, Italy) device. Participants were positioned in supine lying with their affected extremity placed within a “sliding coil” electrode. Dosage: 100 Gauss intensity and 50 Hz frequency for 60 minutes Frequency of administration: once a day, 5 times a week, for 6 weeks (total of 30 sessions) Provider: physiotherapist Placebo EMFT (n = 21) Components of intervention: participants affected extremities were placed in the same device without it being switched on |
|
| Outcomes | Outcomes assessed at baseline and on completion of the intervention period
|
|
| Notes |
Source of funding: no funding was provided Statement regarding declarations of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "This study was a randomized, singleblinded and placebo‐controlled trial". Quote: "Randomization was carried out using the sealed envelope system. Each participant picked up one of the 46 prepared envelopes that contained a card in a specific color". Comment: the trial authors used a non‐random sequence generation process. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization was carried out using the sealed envelope system. Each participant picked up one of the 46 prepared envelopes that contained a card in a specific color. They were placed in either EMFT or p‐EMFT group depending on the color of the card inside their envelope". Comment: the trial authors did not adequately report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "So, everything was the same as the EMFT application, except for the fact that the device did not supply current". Comment: participants were likely to have been adequately blinded but the trial authors did not explicitly report the extent to which the placebo intervention controls for the auditory and sensory characteristics of the intervention. Comment: the trial authors did not adequately report the procedure for blinding of care providers. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Quote: "In p‐EMFT application; the very same position of the patients and electrodes were used. However, the device was switched off. So, everything was the same as the EMFT application, except for the fact that the device did not supply current". Comment: the participants who completed self‐reported outcome measures were probably blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Quote: "Assessments and evaluations, however, were done both at baseline and at the end of the training by same researcher". Comment: the trial authors did not provide a statement of procedures regarding blinding of the outcome assessor. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "All patients successfully completed the whole treatment program". Comment: all randomly assigned participants appear to have completed the study. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the trial authors did not report the method of analysis (ITT versus per protocol). |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "Forty‐two individuals were randomly assigned into either EMFT (N=21) or placebo EMFT (p‐EMFT) (N=21) groups". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "Assessments and evaluations, however, were done both at baseline and at the end of the training by same researcher". Comment: the trial authors did not measure outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Cacchio 2009a.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, single‐blind RCT Setting: inpatient and outpatient rehabilitation centre (Italy; October 2000 to December 2006) Interventions: mirror therapy or placebo control (covered mirror) Sample size calculation: 24 participants per group required to detect a 2 cm reduction in pain on a 10 cm VAS (SD 1.5) with 0 cm labelled as "no pain" and 10 cm as "worst pain I have ever had" at 1 week after treatment at 1% level of statistical significance with 90% power, including a 30% rate of loss at follow‐up |
|
| Participants |
Number of participants: 48 (24 per group) Type of noxious initiating event: stroke (upper limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in both groups received 4 weeks of conventional stroke rehabilitation comprising neuro‐rehabilitation techniques, occupational therapy (OT) and speech therapy (if required), consisting of 5 x 1‐hour sessions per week. Conventional stroke rehabilitation plus mirror therapy (n = 24) Components of intervention: mirror therapy programme: whilst seated with a mirror board positioned between the upper limbs, perpendicular to the midline and with the unaffected limb facing the reflective surface and with their affected upper limb hidden from view, participants observed the reflection of their unaffected upper limb while performing flexion and extension at the shoulder, elbow and wrist and pronation and supination of the forearm. Dosage: 30 minutes per session (for the first 2 weeks), 1 hour per session (for the second 2 weeks) Frequency of administration: 5 times per week for 4 weeks (20 sessions) Provider: physiotherapist Conventional stroke rehabilitation plus placebo control (n = 24) Components of intervention: participants performed the same exercises, according to the same dosage and frequency, with the reflective mirror surface covered |
|
| Outcomes | Outcomes assessed at baseline and at 1 week and 6 months post‐treatment Primary outcomes:
Secondary outcomes:
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...we undertook a randomized placebo‐controlled study in which stroke patients with CRPSt I were randomly allocated..." Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "All the patients were examined 3 times by an investigator who was blinded to the nature of treatment performed". Comment: the outcome assessor was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Quote: "Two patients (8%) in the mirror group and 7 patients (29%) in the control group dropped out of the study". Quote: "One of the 2 patients in the mirror group dropped out because he moved to another city, while the other decided to perform corticosteroid injection therapy in another center. Three of the 7 patients in the control group refused to complete the study, while 4 decided to perform corticosteroid injection therapy in another center". Comment: the extent to which an overall dropout rate of 19% and an unequal dropout rate between groups may have introduced biased estimates of treatment effect is uncertain. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Quote: "Both the primary and secondary outcome analyses were performed according to the intention‐to‐treat (ITT) principle. In this study, subjects that provided baseline and at least 1 post‐treatment measurement constituted the ITT population, whereas those who completed all tests from baseline to the 6‐month follow‐up constituted the per protocol population." Comment: the trial authors reported analyses according to the ITT principle. |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "48 patients with CRPSt1 of the affected upper limb were enrolled". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Low risk | Quote: "The decision to set the follow‐up at 6 months is based on the hypothesis that pain improves spontaneously over a long period of time". Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Cacchio 2009b.
| Study characteristics | ||
| Methods |
Design: parallel‐group, single‐blind, 3‐arm, sham‐controlled RCT. (Whilst the trial authors reported that a number of participants from the 2 comparator groups crossed over into the experimental group, this was not undertaken in a randomised way and therefore we deemed that this trial did not employ a true cross‐over design. We analysed it as a 3‐arm parallel‐group trial up to the endpoint just prior to cross‐over). Setting: not reported (Italy, dates not reported) Interventions: mirror therapy or placebo control (covered mirror) or mental imagery Sample size calculation: not reported |
|
| Participants |
Number of participants: 24 (8 per group) Type of noxious initiating event: stroke (upper limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics: not adequately reported Inclusion criteria: not explicitly reported Exclusion criteria: not reported |
|
| Interventions |
Mirror therapy (n = 8) Components of intervention: whilst viewing a reflected image of the unaffected arm in a mirror, participants performed all of the cardinal (proximal to distal) movements of the affected arm (reported as the 'affected' arm but assumed to be the 'unaffected' arm) Dosage: 30 minutes per session Frequency of administration: daily for 4 weeks (28 sessions) Provider: not reported Placebo control (n = 8) Components of intervention: participants performed the same movements, according to the same dosage and frequency, with the reflective mirror surface covered Provider: not reported Mental imagery (n = 8) Components of intervention: not reported Dosage: not reported Frequency of administration: not reported Provider: not reported |
|
| Outcomes | The trial authors assessed outcomes at baseline and on completion of the intervention period (4 weeks post recruitment) Primary outcomes:
Secondary outcomes:
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We conducted a randomised, sham‐controlled study involving 24 patients with stroke". Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "We randomly assigned the 24 patients to one of three groups". Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "The investigators were unaware of the study‐group assignments". Comment: outcome assessors were blinded to participants group allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "In the active‐mirror group, seven of eight patients (88%) reported reduced pain". Quote: "In the covered‐mirror group, only one of eight patients (12%) reported reduced pain". Quote: "In the mental‐imagery group, two of eight patients (25%) reported reduced pain". Comment: there were no apparent dropouts. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Comment: the trial authors analysed participants in the group to which they were allocated but did not report the method of analysis (ITT versus per protocol). |
| Selective reporting (reporting bias) | High risk | Quote: "After 4 weeks of active mirror therapy, the pain intensity decreased (Fig. 1), and motor function, brush‐induced allodynia, and edema improved (data not shown)". Comment: the trial authors presented mean values for the primary outcome of pain severity in graphical format only; they did not report raw data in numerical form with measures of variation. Comment: the trial authors did not report any outcome data for the three secondary outcome measures (motor function, brush‐induced allodynia, oedema). |
| Sample size | High risk | Quote: "We conducted a randomised, sham‐controlled study involving 24 patients..." Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "The primary end point was the score for the severity of pain after 4 weeks of therapy". Comment: the trial authors re‐measured outcomes on completion of the intervention period only and did not measure them over a clinically relevant length of time. |
| Other bias | Unclear risk | Comment: the trial was reported and published as a 'Letter to the Editor'. Full trial methodology and results have not been published elsewhere (Cacchio, personal communication). Comment: the trial authors presented limited group‐specific baseline data. Comment: the trial authors did not report any inclusion/exclusion data. |
den Hollander 2016.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT Setting: Department of Rehabilitation at Maastricht University Medical Center (The Netherlands; from January 2009 to June 2013) Interventions: exposure in vivo (EXP) or pain‐contingent treatment as usual (TAU) Sample size calculation: "The square root from this partial eta‐squared was used as effect estimator in the software program nQuery Advision 5.0 with alpha 0.05, 2‐tailed, and statistical power of 0.80, resulting in 39 participants per condition. Taking into account the duration of the trial, required effort from participants, and dropout rates from previous studies (EXP 33% and TAU 23%), 55 participants per condition was aimed for". |
|
| Participants |
Number of participants: 46 (23 in each group) Type of noxious initiating event: aetiology not reported (upper or lower limb) Diagnostic criteria:Merskey 1994 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Exposure in vivo (n = 23) Components of intervention: EXP is characterised by repeated exposure to feared movements, activities, and/or sensations to create expectancy violations, resulting in a lowered threat value of these stimuli
Dosage: 1 hour per session Frequency of administration: weeks 1 to 4, 2 sessions per week; weeks 5 to 19, 1 session per week; weeks 10 to 17, 1 session every other week (total 17 hours over 17 sessions) Provider: psychologist and physical or occupational therapist Pain‐contingent treatment as usual (n = 23) Components of intervention: a standardised physical therapy treatment aimed at increasing control over pain, and optimising coping with CRPS I
Dosage: 30 minutes per session Frequency of administration: weeks 1 to 4, 3 sessions per week; weeks 5 to 13, 2 sessions per week; weeks 14 to 17, 1 session per week (total 17 hours over 34 sessions) Provider: physical therapist |
|
| Outcomes | Outcomes assessed at baseline, at the end of the treatment period and 6 months post‐treatment Primary outcomes:
Secondary outcomes:
|
|
| Notes |
Source of funding: the trial was supported by a grant from Profileringsfonds azM and governmental funding for Maastricht University, Faculty of Psychology. J. W. S. Vlaeyen was also supported by the Odysseus Grant G090208N “The Psychology of Pain and Disability Research Program” funded by the Research Foundation Flanders (FWO Vlaanderen), Belgium, as well as the “Asthenes” long‐term structural funding–Methusalem grant by the Flemish Government, Belgium. Funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript. Statement regarding declarations of interest: the authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computerized “adaptive biased urn randomization” was used to generate a randomization schedule". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Low risk | Quote: "This schedule was generated by an independent statistician and was only accessible to 1 researcher who was not involved in the selection, treatment, and measurement." Comment: the trial authors probably used an acceptable method to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "Participants knew that they would receive 1 of the 2 possible treatments. The content of allocated treatment was revealed in the first treatment session, the content of the other treatment remained unaddressed". Quote: "Research assistants were not informed about treatment assignment. Their coordinating role in receiving data (audiotapes, planning of measurements) made it practically impossible to keep them fully blinded". Quote: "EXP therapists rated EXP a more credible treatment than TAU therapists rated TAU. Although patients rated both treatments equally credible, and our fidelity check confirmed that treatments were delivered according to the protocolized manuals, we do not know if the differential treatment credibility influenced overall quality of treatment delivery, possibly favoring EXP". Comment: given the nature of the intervention, participants and some personnel were not blinded to treatment allocation but the extent to which the lack of blinding may have introduced bias is uncertain. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Quote: "Participants knew that they would receive 1 of the 2 possible treatments. The content of allocated treatment was revealed in the first treatment session, the content of the other treatment remained unaddressed". Quote: "...patients rated both treatments equally credible, and our fidelity check confirmed that treatments were delivered according to the protocolized manuals." Comment: the participants were not blinded to treatment allocation and self‐reported some outcomes but lack of blinding unlikely to have biased the results given that participants received interventions judged to have been of relatively equal credibility. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | High risk | Quote: "Three participants did not have any treatment contact (1 EXP, 2 TAU). Eight participants (3 EXP, 5 TAU) did not complete treatment protocol; they were requested to complete further measurements, but only 3 (all TAU) continued testing, resulting in 38 postmeasurements (19 EXP, 19 TAU). At 6‐month follow‐up, 35 participants (18 EXP, 17 TAU) completed the measurements. Comment: a total dropout rate of 24% (at 6‐month follow‐up) may have introduced bias in the estimates of treatment effect. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Quote: "Data were analyzed using an intention‐to‐treat approach; no participants were excluded from data analyses". Comment: the trial authors reported analyses according to the ITT principle. |
| Selective reporting (reporting bias) | High risk | Quote: "Posttreatment assessments were completed within 2 weeks after treatment, at 6‐month, and 12‐month follow‐up. The current report includes posttreatment and 6‐month followup data". Comment: data not reported for all time points. Comment: the authors supplied 12‐month outcome data for outcomes specified in the trial report on request. Quote: "Physical measures including physical activity in daily life and body function will be reported elsewhere". Comment: the trial authors have not fully reported outcome data for all outcomes. Comment: a number of secondary outcomes outlined, but not fully specified, in the trial registration have not been reported. Comment: measurement of pain intensity using the Neuropathic Pain Scale was reported in the trial report but not the trial registration. |
| Sample size | High risk | Quote: "We conducted a randomized controlled trial (N = 46) Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Low risk | Quote: "Pretreatment to posttreatment and pretreatment to 6‐month follow‐up change scores were tested". Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Devrimsel 2015.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT Setting: not reported (Turkey; dates not reported) Interventions: whirlpool bath plus under underwater ultrasound and exercise therapy or neuromuscular electrical stimulation (NMES) plus under underwater ultrasound and exercise therapy Sample size calculation: not reported |
|
| Participants |
Number of participants: 60 (30 in each group) Type of noxious initiating event: mixed (fracture distal radius n = 33, fracture metacarpal n = 9, tendon injury n = 18) (upper limb) Diagnostic criteria:Harden 2010 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in both groups received i) underwater ultrasound therapy (performed by placing the ultrasound probe 1 to 2.5 cm away from the hand and wrist underwater; treatment intensity was 1.5 W/cm2, and the probe was slowly moved parallel to the treatment area for 5 minutes; ii) exercise therapy (joint range of motion and stretching up to each patient’s pain threshold, further details not reported); each for 5 days per week for 3 weeks), and iii) were allowed to take paracetamol (500 mg, 3 times per day) Whirlpool bath (n = 30) Components of intervention: treatment was administered using a Chiron extremity caldron device (Chirana Progress, Slovakia). The water temperature was set at 40 °C and monitored with a thermometer. Hands and wrists were positioned in the most comfortable resting position that would not impede perfusion and placed in the water tank. Dosage: 30 minutes Frequency of administration: 5 days per week for 3 weeks (total 15 sessions) Provider: not reported NMES (n = 30) Components of intervention: treatment was administered using a Cefar device (Cefar, European Union) Dosage: symmetrical biphasic current pulses were applied at a 30 Hz frequency for 300 ms. Each muscle group (flexor and extensor muscle groups) was treated for 20 minutes Frequency of administration: 5 days per week for 3 weeks (total 15 sessions) Provider: not reported |
|
| Outcomes | Outcomes assessed at baseline and on completion of the intervention period.
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients were randomized into two 30‐patient groups". Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Comment: participants were not blinded to treatment allocation but a lack of blinding is unlikely to have biased the results given that participants received interventions judged to have been of relatively equal credibility. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Comment: participants were not blinded to treatment allocation but a lack of blinding is unlikely to have biased the results given that participants received interventions judged to have been of relatively equal credibility. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Comment: the trial authors did not give a statement of procedures regarding blinding of the outcome assessor. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Comment: the dropout rate was not reported. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the method of analysis (ITT versus per protocol) was not reported. |
| Selective reporting (reporting bias) | Low risk | Comment: outcome data were adequately reported for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "Sixty outpatients (30 per group) with complex regional pain syndrome participated". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "All parameters were measured at baseline (week 0) and at the trial end (week 3)". Comment: the trial authors did not measure outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Dimitrijevic 2014.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, single‐blind RCT Setting: outpatient clinic (Serbia; December 2004 to January 2007) Interventions: low‐level laser therapy and kinesitherapy or interferential current therapy and kinesitherapy Sample size calculation: not reported |
|
| Participants |
Number of participants: 50 (25 per group) Type of noxious initiating event: trauma (no further details reported) (upper and lower limb) Diagnostic criteria:Harden 2005 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants were instructed not to take any specific CRPS medication (corticosteroids, bisphosphonates, calcitonin, nifedipine, antiepileptic drugs, etc.) or analgesic medication. Participants in both groups received individual kinesitherapy (active and active assisted exercises, strictly dosed up to pain threshold) for 30 minutes, twice a day. Low‐level laser therapy and kinesitherapy (n = 20) Components of intervention: using a GaAs laser diode, 8 points along the joint line and painful points in the affected area were treated using the following parameters: a low power of 70 mW, 810 nm wavelength, and 70 Hz, 640 Hz and 5000 Hz frequency, depending on the dominant findings Dosage: 1.5 J/cm2 Frequency of administration: 5 days a week for 2 weeks (10 sessions), and then every other day (10 sessions) (20 sessions) Provider: not reported Interferential current therapy and kinesitherapy (n = 25) Components of intervention: bipolar IFC therapy was applied with electrodes positioned locally on the painful and swollen part using the following parameters: 90 Hz frequency Dosage: 15 minutes Frequency of administration: 5 days a week for 2 weeks (10 sessions), and then every other day (10 sessions) (20 sessions) Provider: not reported |
|
| Outcomes | The trial authors did not explicitly specify the time points at which outcomes were measured in the trial report. Outcomes assessed at baseline and on completion of the intervention period (6 weeks post recruitment) (Dimitrijevic, personal communication). The trial authors did not state any primary outcome.
|
|
| Notes |
Source of funding: the trial authors declared that this study received no financial support Statement regarding declarations of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...patients were randomly selected and classified into two groups using sequentially numbered, closed, opaque envelopes that had been prepared earlier using a computer‐generated list of random numbers, and balanced to ensure equal numbers in each group". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Low risk | Quote: "...patients were randomly selected and classified into two groups, using sequentially numbered, closed, opaque envelopes that had been prepared earlier". Comment: the trial authors used an acceptable method to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Comment: the participants were not blinded to treatment allocation but lack of blinding unlikely to have biased the results given that participants received interventions judged to have been of relatively equal credibility. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Comment: the participants were not blinded to treatment allocation and self‐reported some outcomes but lack of blinding unlikely to have biased the results given that participants received interventions judged to have been of relatively equal credibility. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Comment: the trial authors did not provide a statement of procedures regarding blinding of the outcome assessor. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Quote: "During the study, 5 out of 50 patients dropped out. A total of 45 patients completed the study". Comment: all 5 dropouts came from the laser therapy group (lost to follow‐up, n = 2; discontinued intervention, n = 3). Whilst the overall dropout rate was 10%, the extent to which an unequal dropout rate between groups may have biased the results is uncertain. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Comment: the trial authors excluded 3 participants from the laser therapy group from the analysis because they discontinued the intervention, in violation of the ITT principle. |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "The prospective randomized study included 50 patients with unilateral post‐traumatic CRPS I". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "All patients underwent evaluation of each separate parameter before treatment and after applying 20 therapeutic procedures". Comment: outcomes were re‐measured on completion of the intervention period only and were not measured over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Duman 2009.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT Setting: not reported (Turkey; dates not reported) Interventions: conventional care plus manual lymphatic drainage (MLD) or conventional care Sample size calculation: not reported |
|
| Participants |
Number of participants: 34 (experimental group n = 18, control group n = 16) Type of noxious initiating event: mixed (fracture n = 23, soft tissue trauma n = 7, incisive injury n = 3, non‐traumatic n = 1) (upper limb) Diagnostic criteria:Bruehl 1999 (RSD i.e. CRPS I) Baseline characteristics: Total sample (separate intervention and control group data not reported but no statistically significant between‐group differences). Mean (±) age = 20.6 (0.8) years; female:male = not reported Mean (±) duration of reflex sympathetic dystrophy (RSD) 5.1 (1.3) months Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in both groups received conventional care including non‐steroidal anti‐inflammatory drugs (NSAIDs) (type, dosage, frequency of administration not reported) and physical therapy (once per day, 5 days per week for 3 weeks), comprising therapeutic ultrasound of the affected limb and stellate ganglions (treatment parameters not reported) and therapeutic exercises for all joints of the affected limb (10 repetitions, twice per day; type of exercises performed not reported) followed by a 2‐month programme of home maintenance therapeutic exercises. MLD (n = 18) Components of intervention: MLD. Light massage for superficial abdominal, axillary and upper limb lymphatic stimulation of the affected upper limb followed by light upper limb massage in a distal to proximal direction up to the axillary region. Dosage: 1 session per day for approximately 45 minutes administered by a therapist plus 1 session per day of participant self‐administered MLD (duration not reported). Frequency of administration: 5 times per week for 3 weeks (15 sessions), followed by a home maintenance programme of self‐administered MLD for 2 months Provider: not reported Conventional care (n = 16) |
|
| Outcomes | Outcomes assessed at baseline, at the end of the 3‐week treatment period and 2 months post‐treatment. The trial authors did not state any primary outcome.
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were allocated randomly into two groups". Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Quote: "All of the parameters were obtained before the treatment (baseline), after treatment and 2 months after treatment (follow‐up) by a different physician". Comment: the trial authors did not report a statement of procedures regarding blinding of the outcome assessor. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "After 2 months, all of the patients were re‐evaluated". Comment: there were no apparent dropouts. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Quote: "After 2 months, all of the patients were re‐evaluated". Comment: trial authors analysed participants analysed in the group to which they were allocated but did not report the method of analysis (ITT versus per protocol). |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "A total of 34 patients who fulfilled the modified International Association for the Study of Pain (IASP) criteria and diagnosed as RSD were enrolled". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Low risk | Quote: "After 2 months, all of the patients were re‐evaluated". Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Durmus 2004.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, double‐blind, placebo‐controlled RCT Setting: out‐patient rehabilitation clinic (Turkey; 1999 to 2001) Interventions: usual care plus pulsed electromagnetic field treatment or usual care plus placebo pulsed electromagnetic field treatment Sample size calculation: not reported |
|
| Participants |
Number of participants: 40 (number of participants per group not reported) Type of noxious initiating event: Colles fracture (upper limb) Diagnostic criteria:Merskey 1994 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in both groups received 100 units of calcitonin via intramuscular injection for 6 weeks; once per day for the first 3 weeks then once every other day for the second 3 weeks, and performed active and active assisted range of motion exercises and a stretching programme for 30 minutes, 3 times per day. Electromagnetic field treatment (n = not reported) Components of intervention: pulsed electric magnetic field treatment. Treatment was administered using a Magnetic‐Therapy Mg Port Cosgamma® device. The trial authors did not report participant and equipment positioning. Dosage: 100 Gauss intensity and 50 Hz frequency for 60 minutes per session Frequency of administration: 5 times per week for 6 weeks (30 sessions) Provider: not reported Placebo (n = not reported) Components of intervention: participants were placed in the same device without it being switched on |
|
| Outcomes | The trial authors assessed outcomes at baseline and on completion of the intervention period (6 weeks post recruitment). The trial authors did not state any primary outcome.
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were divided into two groups with the random numbers table". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "In this randomized double‐blind, placebo‐controlled study". Quote: "the second group of patients received placebo treatment by being placed in the same device without it being switched on". Comment: participants were likely to have been adequately blinded but the trial authors did not explicitly report the extent to which the placebo intervention controls for the auditory and sensory characteristics of the intervention. Comment: the trial authors did not report the procedure for blinding of care providers. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Quote: "the second group of patients received placebo treatment by being placed in the same device without it being switched on". Comment: the participants who completed self‐reported outcome measures were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "The patients were assessed at the beginning of a 6 week course of treatment and on the final week of treatment by a physician who did not know which group received the applied magnetic field treatment". Comment: the outcome assessor was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "There were no refusals or drop‐outs from the study". Comment: all randomly assigned participants completed the study. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Quote: "There were no refusals or drop‐outs from the study". Comment: the trial authors did not report the method of analysis (ITT versus per protocol). |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors fully reported outcome data for the 2 main pain outcomes but did not report any outcome data for the 4‐point verbal pain scale or any other outcomes (pain on palpation, ratings of stiffness and change of colour, range of motion and 3‐phase bone scintigraphy), as reported in the methods section of the publication. |
| Sample size | High risk | Quote: "Forty patients diagnosed as having Type I CRPS subsequent to trauma (Colles Fracture), who consulted the Physical Medicine and Rehabilitation Department of Istanbul University, Istanbul Medical Faculty between 1999 and 2001 were included in the study". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "Patients were assessed at the beginning of a 6 week course of treatment and on the final week of treatment". Comment: the trial authors re‐evaluated participants at the end of the treatment period only. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Halicka 2021.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, double‐blind RCT Setting: university clinics and patients' homes (United Kingdom; March 2017 to July 2019) Interventions: prism adaptation treatment or sham prism adaptation treatment Sample size calculation: 21 participants per treatment group required to provide 90% power to detect a minimal clinically significant reduction of 2 on the primary outcome of pain intensity (0 to 10 NRS), with a SD of 1.98, and a 2‐tailed alpha of 0.05 |
|
| Participants |
Number of participants: 52 (26 per group) (N.B. 3 participants dropped out after randomisation and during the baseline assessment process. The following data are for n = 49). Type of noxious initiating event: mixed (hand surgery n = 3, hand soft tissue injury n= 3, finger fracture n = 3, arm fracture n = 3, wrist sprain n = 5, finger soft tissue injury n = 4, wrist fracture n = 8, elbow fracture n = 2, wrist surgery n = 2, shoulder whiplash injury n = 2, arm soft tissue injury n = 2, shoulder surgery n = 1, breast surgery n = 1, elbow soft tissue injury n = 1, heart surgery n = 1, hand surgery n = 1, arm fracture n = 1, shoulder dislocation n = 2, none n = 4) (upper limb). (N.B. multiple inciting events were reported for many participants. 'Initiating events' have been categorised according to the first event in the list for simplicity). Diagnostic criteria: 'Budapest criteria' Harden 2010 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in both groups were instructed to continue any usual treatments (including medications) but were asked not to change their treatment regimens throughout the duration of the trial if possible. Prism adaptation treatment (n = 23) Participants used welding goggles fitted with 35‐diopter Fresnel lenses that induced approximately 19° optical deviation away from the CRPS‐affected side. Participants were seated approximately 50 cm from a wall and an A4 sheet was positioned on the wall in landscape orientation at eye‐level and aligned with their body midline. There were 2 targets (2 cm‐diameter red circles) on the sheet, located 12.5 cm to the left and 12.5 cm to the right of the participant's body midline. While wearing the prism goggles, participants used their CRPS‐affected arm to perform 50 pointing movements, as fast as possible, alternating between the left and right target. The welding goggles occluded the first half of the arm movement and participants were encouraged to point as quickly as possible. Participants were instructed to perform self‐guided treatment sessions at home. Dosage: (duration of each session) not reported Frequency of administration: 2 times per day for 2 weeks (29 sessions) Provider: research psychologists Sham prism adaptation treatment (n = 26) Participants carried out exactly the same procedure as the active group, except the welding goggles used were fitted with neutral lenses that did not induce any lateral shift. The neutral lenses distorted the acuity and clarity of vision to a similar extent as prism lenses. Dosage: not reported Frequency of administration: 2 times per day for 2 weeks (29 sessions) Provider: research psychologists |
|
| Outcomes | Outcomes assessed over 2 baseline sessions (3 to 4 weeks before randomisation and 1 to 5 days before the commencement of treatment), on completion of the treatment period (primary endpoint), and then 4 weeks, 3 months and 6 months post‐treatment. Primary outcomes:
Secondary outcomes:
N.B. trial authors assessed a range of additional measures of sensory function (quantitative sensory testing, two‐point discrimination thresholds), autonomic and motor function (temperature difference, oedema, grip strength,delta finger‐to‐palm distance) and neuropsychological functions (visuospatial attention in near space (Temporal Order Judgement, Landmark, and Greyscales tasks), mental representation of space (Mental Number Line Bisection task), spatially defined motor function, and body representation (Hand Laterality Recognition task)) not further detailed here. |
|
| Notes |
Source of funding: The study was supported by a grant from the Reflex Sympathetic Dystrophy Syndrome Association (RSDSA) awarded to JHB and MJP. The RSDSA approved the design of the study. The funders had no role in data collection and analysis, decision to publish, or preparation of the manuscript. Statement regarding declarations of interest: "MH and ADV were supported by studentships from the University of Bath and the GW4 BioMed Medical Research Council Doctoral Training Partnership (ref. 1793344), respectively". 2 authors have received support from the Pain Relief Foundation, Liverpool, 3 authors are committee members of the CRPS UK Research Network, and 1 author is a committee member of the Physiotherapy Pain Association and the British Pain Society. The authors have no other competing interests to declare. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomly assigned to either PA or sham treatment group with equal allocation ratio, using MINIM software". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The researcher responsible for enrolment and all data collection remained blinded to participants’ treatment allocation". Comment: the trial authors did not adequately report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The participants were blinded to their treatment allocations throughout the entire duration of the trial". Quote: "The only researchers who were aware of individual treatment allocations were those who randomised the participants and/or trained them in carrying out PA or sham treatments and provided them with prism or neutral goggles". Comment: the participants and personnel were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Quote: "The participants were blinded to their treatment allocations throughout the entire duration of the trial". Quote: "Only 12% of participants in each group correctly guessed their treatment allocation, therefore participant blinding was successful". Comment: the participants who completed self‐reported outcome measures were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "The researcher responsible for enrolment and all data collection remained blinded to participants’ treatment allocation". Comment: the outcome assessor was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | High risk | Quote: "Eight participants (16%) withdrew from the study following treatment allocation". Comment: The trial's CONSORT diagram shows i) an additional 4 participants (2 in each group) were lost secondary to 'loss of contact, giving an overall dropout rate of 24%, and ii) the dropout rate was uneven between groups (n = 4 in the prism adaptation group, n = 8 in the sham prism adaptation group). Comment: a total dropout rate of 24% (at 6‐month follow‐up) may have introduced bias in the estimates of treatment effect. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Quote: "Our primary analysis involved the intention‐to‐treat population, that is, participants who received their allocated intervention (i.e. received in‐person training immediately after RS2), regardless of their treatment adherence or completion of the outcome assessments (PA treatment = 23, sham treatment = 26). Note that the trial protocol defined this population as all participants allocated to treatment, which did not account for the possibility that they could withdraw before being trained in how to carry out their allocated intervention. This was the case for three participants who were not included in the intention‐to‐treat sample as per an updated definition". Comment: the trial authors violated the ITT principle. |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors reported incomplete outcome data (no measures of variance) for all outcomes reported in the methods section of the manuscript. Comment: the authors supplied these missing data for our outcomes of interest on request. |
| Sample size | High risk | Quote: "Forty‐nine eligible adults with CRPS were randomized to undergo two‐weeks of twice‐daily home‐based prism adaptation treatment (n = 23) or sham treatment (n = 26)". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Low risk | Quote: "Long‐term postal follow‐ups were conducted three and six months after treatment". Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Hazneci 2005.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT Setting: Department of Physical Medicine and Rehabilitation Clinic, Gulhane Military Medical Academy (Turkey; 2001 to 2002) Interventions: transcutaneous electrical nerve stimulation (TENS) or pulsed ultrasound of the stellate ganglion Sample size calculation: not reported |
|
| Participants |
Number of participants: 30 (TENS N = 16; pulsed ultrasound N = 14) Type of noxious initiating event: mixed (trauma n = 20, sports injury n = 5, post finger amputation n = 1, post injection n = 1, idiopathic n = 3) (upper limb) Diagnostic criteria:Kozin 1992 (stage I and II) (reflex sympathetic dystrophy syndrome) Baseline characteristics
Inclusion criteria: CRPS I Exclusion criteria: not reported |
|
| Interventions | Participants in both groups received contrast bathing (the upper extremity was put in hot water for 4 minutes and then in cold water for 1 minute and this procedure was repeated for 20 minutes) and an exercise programme (undertaken with the assistance of a physiotherapist and comprising active, assisted active and passive exercise within the pain limits; including extension, flexion, ulnar and radial deviation for the wrist, abduction and flexion for the thumb, flexion and extension for the metacarpophalangeal, proximal and distal interphalangeal joints). TENS (n = 16) Components of intervention: TENS was applied, using a Myomed 932 Enraf model, to the painful area of the involved upper extremity Dosage: frequency 100 Hz, mono‐rec wave module Frequency of administration: once per day, for 20 minutes, for 3 weeks (total number of sessions not reported) Provider: not reported Pulsed ultrasound of the stellate ganglion (n = 14) Components of intervention: using a BTL 07p model ultrasound device pulsed ultrasound was applied with a 1 cm² probe to the stellate ganglion on the involved side of the upper extremity Dosage: 3 watt/cm² (pulsed) Frequency of administration: once per day, for 5 minutes, for 3 weeks (total number of sessions not reported) Provider: not reported |
|
| Outcomes | The trial authors assessed outcomes at baseline and on completion of the intervention period (3 weeks post recruitment):
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were divided into two groups randomly". Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Comment: the participants appear not to have been blinded to treatment allocation but lack of blinding is unlikely to have biased the results given that participants received interventions judged to have been of relatively equal credibility. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Comment: participants appear not to have been blinded to treatment allocation and self‐reported some outcomes, but lack of blinding is unlikely to have biased the results given that participants received interventions judged to have been of relatively equal credibility. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Comment: the trial authors did not give a statement of procedures regarding blinding of the outcome assessor. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Comment: the trial authors did not report the dropout rate. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the trial authors did not report the method of analysis (ITT versus per protocol). |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "30 patients diagnosed with Reflex Sympathetic Dystrophy Syndrome at the upper extremities were included into the study". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "All patients evaluated before treatment and 3rd week following the treatment" Comment: the trial authors re‐measured outcomes on completion of the intervention period only and they were not measured over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Hwang 2014.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 3‐arm RCT Setting: tertiary pain management centre in Seoul (South Korea; dates not reported) Interventions: ‘virtual body swapping with mental rehearsal’ (VBS) or ‘watching movement only’ (WM) or ‘mental rehearsal only' (MR) Sample size calculation: not reported |
|
| Participants |
Number of participants: 39 (13 in each group) Type of noxious initiating event: not reported (upper and lower limb) Diagnostic criteria:Bruehl 1999 (CRPS I and II) Baseline characteristics:
Inclusion criteria:
Exclusion criteria: not reported |
|
| Interventions |
VBS (n = 13) Components of intervention: in a semi‐reclined position and wearing a VR 2000 3D Visor Head‐Mounted Display (HMD) (League City, Texas, USA), participants watched a video clip consisting of 4 actions (‘making the fists and opening up the fingers’, ‘bending and unbending the elbows’, ‘bending the ankles forward and backward’, and ‘bending and unbending the legs'). Participants were asked to mentally synchronise their own movements with the movements displayed on the HMD. Dosage: participants watched the video clip twice with a 1‐minute break between sessions (not exceeding 10 minutes) Frequency of administration: single session Provider: not reported WM (n = 13) Components of intervention: in a semi‐reclined position and wearing a VR 2000 3D Visor Head‐Mounted Display (HMD) (League City, Texas, USA), participants watched a video clip consisting of 4 actions (‘making the fists and opening up the fingers’, ‘bending and unbending the elbows’, ‘bending the ankles forward and backward’, and ‘bending and unbending the legs'). Participants were asked to simply watch the video clip on the HMD, which was the same video used in the VBS group. Dosage: participants watched the video clip twice with a 1‐minute break between sessions (not exceeding 10 minutes) Frequency of administration: single session Provider: not reported MR (n =13) Components of intervention: in a semi‐reclined position participants listened to a voice recording consisting of 4 imaginary actions: ‘making the fists and opening up the fingers’, ‘bending and unbending the elbows’, ‘bending the ankles forward and backward’, and ‘bending and unbending the legs’. Dosage: participants listened to the voice recording twice with a 1‐minute break between sessions (not exceeding 10 minutes) Frequency of administration: single session Provider: not reported |
|
| Outcomes | Outcomes assessed at baseline and on completion of the intervention period
|
|
| Notes |
Source of funding: the trial was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2012R1A1A2008624) Statement regarding declarations of interest: the authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All participants were assigned randomly to one of the three experimental groups". Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: given the nature of the intervention, participants were not blinded to treatment allocation but the extent to which the lack of blinding may have introduced bias is uncertain. Comment: the trial authors did not give a statement of procedures regarding blinding of personnel and the extent to which the lack of blinding may have introduced bias is uncertain. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Unclear risk | Comment: given the nature of the intervention, participants were not blinded to treatment allocation but the extent to which the lack of blinding may have introduced bias is uncertain. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Comment: the trial authors did not explicitly report the dropout rate. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the method of analysis (ITT versus per protocol) was not reported. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors did not fully report outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: "The participants were 39 patients with CRPS". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "Pretreatment pain intensity and BPD were compared with post‐treatment perceptions". Comment: the trial authors re‐evaluated participants at the end of the treatment period only. |
| Other bias | Unclear risk | Comment: some baseline imbalances between groups with respect to gender and duration of pain. |
Jeon 2014.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, placebo‐controlled pilot RCT Setting: tertiary university pain centre (South Korea; dates not reported) Interventions: virtual body swapping with mental rehearsal or virtual body swapping alone Sample size calculation: pilot RCT with bootstrapping method to increase the robustness of small‐sample analyses |
|
| Participants |
Number of participants: 10 (number per group not reported) Type of noxious initiating event: not reported (upper limb only n = 1, lower limb only n = 1, multiple limbs n = 4, and whole body n = 4) Diagnostic criteria:Harden 2007 (CRPS I) Baseline characteristics: Total sample (separate intervention and control group data not reported but no statistically significant between‐group differences) Mean (SD) age: 39.30 (10.99) years; female:male = 0:10 Median (range) duration of CRPS I: 52 (33 to 120) months Inclusion criteria: CRPS I Exclusion criteria: not reported |
|
| Interventions | The trial authors did not report any co‐interventions. Virtual body swapping with mental rehearsal (n = not reported) Components of intervention:
Dosage: 1 training session Frequency of administration: the experimental video clip was played twice with a 1‐minute break given between viewings Provider: 1 specialist in pain and 2 assistants (trained graduate students); professional discipline not reported Virtual body swapping alone (n = not reported) Components of intervention: participants watched the same video but did not perform mental rehearsal of the 4 physical movements Dosage: 1 training session Frequency of administration: the experimental video clip was played twice with a 1‐minute break given between viewings Provider: 1 specialist in pain and 2 assistants (trained graduate students); professional discipline not reported |
|
| Outcomes | The trial authors did not explicitly specify the time points at which they measured outcomes in the trial report. The outcomes were assessed immediately pre‐intervention and postintervention. The trial authors did not state any primary outcome.
|
|
| Notes |
Source of funding: Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2012R1A1A2008624) and the Chung‐Ang University Excellent Student Scholarship in 2014 Statement regarding declarations of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Ten patients who met the diagnostic criterion for CRPS type 1 were randomly assigned to either the treatment or control group". Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: given the nature of the intervention, participants were not blinded to treatment allocation but the extent to which the lack of blinding may have introduced bias is uncertain. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Unclear risk | Comment: given the nature of the intervention, participants were not blinded to treatment allocation but the extent to which the lack of blinding may have introduced bias is uncertain. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Comment: the trial authors did not report the dropout rate but, given the intervention comprised a single session with post‐intervention follow‐up only it is likely there were no dropouts. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Comment: the trial authors did not report the method of analysis but, given the methodology, it is likely that they analysed all participants in the group to which they were allocated. |
| Selective reporting (reporting bias) | High risk | Quote: "There was no significant difference between the groups in pain intensity, F(1, 7) = 0.05, p = 0.81". Comment: the trial authors did not report any pre‐intervention or postintervention outcome data for self‐reported pain intensity. |
| Sample size | High risk | "Ten patients with CRPS type 1 were recruited from a tertiary university pain center in Seoul, Korea". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "The experimental video clip was played twice with a 1‐minute break given between viewing's. The participants were then asked to respond to the pain intensity question...and to complete the BPDQ". Comment: the trial authors re‐measured outcomes on immediate completion of the intervention period only and did not measure them over a clinically relevant length of time. |
| Other bias | Unclear risk | Comment: the trial authors did not report baseline pain data. |
Lewis 2021.
| Study characteristics | ||
| Methods |
Design: parallel, 2‐arm RCT Setting: clinics a the Royal National Hospital for Rheumatic Diseases, Royal United Hospitals Bath NHS Foundation Trust, Bath and The Walton Centre NHS Foundation Trust, Liverpool (United Kingdom, dates not reported) Interventions: mediated virtual reality or sham mediated virtual reality Sample size calculation: a total sample size of 88 participants (44 per group) was calculated as sufficient for a mean (SD) reduction on the 11‐point numerical pain rating scale of 1.733 (2.89) points, with 80% power and a 0.05 two‐sided significance |
|
| Participants |
Number of participants: 45 (experimental group n = 23; control group n = 22) Type of noxious initiating event: not reported (upper limb) Diagnostic criteria: 'Budapest criteria' Harden 2010 (CRPS type not reported) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Mediated virtual reality (n = 23) Components of intervention:
Dosage: up to 5 sessions of 30 minutes duration each Frequency of administration: not reported Provider: not reported Sham mediated virtual reality (n = 22) Components of the intervention: the procedure and duration were identical to the experimental group with the exception that the image of the participant's hand was not visually altered, though the participant believed it to have been. A satisfaction rating of <+1 was not required to proceed with the intervention. Dosage: up to 5 sessions of 30 minutes duration each Frequency of administration: not reported Provider: not reported |
|
| Outcomes | Outcomes were assessed pre‐intervention and post‐intervention, and a subgroup was followed up 2 weeks post‐intervention. Primary outcomes: 1. Body perception of the affected limb using the Bath Body Perception Disturbance (BPD) scale, with higher scores indicating a greater degree of disturbance (score range not reported) 2. Self‐rated current pain using an 11‐point Numerical Rating Scale (NRS), anchored with 0 "no pain" and 10 "worst pain imaginable" 3. Subjective perceptual changes associated with the affected hand by providing perceptual statement ratings to two statements on a 7‐point Likert scale ranging from ‐3 "strongly disagree" to + 3 "strongly agree" Secondary outcomes: 1. Self‐reported severity of neuropathic pain using the Neuropathic Pain Symptom Inventory (NPSI), different neuropathic symptoms are rated on an 11‐point numerical rating scale and a total score is created by summing the 5 categories; higher scores denote greater intensity (score range not reported) |
|
| Notes |
Source of funding: one researcher's salary and the costs of the project were funded by a National Institute for Health Research Post‐Doctoral Fellowship (grant number CAT‐CL‐03‐2012‐019) Statement regarding declarations of interest: no conflicts of interests were declared for any author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a person independent of data collection used a computer generated random sequence to produce information regarding group allocation". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Low risk | Quote: "in advance of testing, a person independent of data collection used a computer generated random sequence to produce information regarding group allocation that was placed in sealed and numbered envelopes". Comment: the trial authors used an acceptable method to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "to minimise performance and detection bias, the clinical assessor and participants were blinded to group allocation. Participants were not informed of the study hypothesis to minimise responder bias". Comment: the participants were blinded to treatment allocation. Comment: care provider not blinded but we judge that both intervention arms reflect active interventions of relatively equal credibility delivered with equal enthusiasm such that outcomes were unlikely to be influenced by a lack of blinding. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Quote: "to minimise performance and detection bias, the clinical assessor and participants were blinded to group allocation. Participants were not informed of the study hypothesis to minimise responder bias." Comment: the participants who completed self‐reported outcome measures were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "the clinical assessor and participants were blinded to group allocation" Comment: outcome assessors were blinded to participants group allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Quote: "Analysis of data was conducted in 45 participants for single exposure and in 39 participants for repeated exposure and follow up". Comment: there were no dropouts for the primary outcome but there was an unequal dropout rate between groups at follow‐up (E = 9%, C = 18%). Reasons for dropout were given. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the authors did not provide a statement detailing whether the participants were analysed in the group to which they were randomised. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors fully reported outcome data graphically for all outcomes; but did not report raw data in numerical form with measures of variation. |
| Sample size | High risk | Quote: "Forty‐five participants were randomised". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "BPD and pain were measured pre and post‐intervention". Comment: the trial authors did not measure outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Li 2012.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT Setting: hospital (China; July 2008 to July 2010) Interventions: acupuncture and massage or rehabilitation therapy Sample size calculation: not reported |
|
| Participants |
Number of participants: 120 (60 per group) Type of noxious initiating event: stroke (upper limb) Diagnostic criteria:Steinbrocker 1948 (stage 1) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Acupuncture and massage (n = 60) Components of intervention:
Dosage: acupuncture = 25 minutes, massage = 25 minutes Frequency of administration: once per day for 6 therapeutic courses; each course comprised 5 sessions, with a 2‐day interval between courses (30 sessions) Provider: doctors Rehabilitation therapy (n = 60) Components of intervention: active‐assisted scapular movements; Bobath exercises to clench the fist, functional transfers (e.g. changing position from prone to sitting, sitting to standing); proprioceptive neuromuscular facilitation (PNF) Dosage: active‐assisted scapular movements = 15 minutes, Bobath exercises and functional transfers = 15 minutes, PNF = 10 minutes Frequency of administration: once per day for 6 therapeutic courses; each course comprised 5 sessions, with a 2‐day interval between courses (30 sessions) Provider: doctors |
|
| Outcomes | The trial authors assessed outcomes at baseline, at the end of the 6‐week treatment period and at 12 weeks post‐treatment Primary outcomes:
Secondary outcomes
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A random encoding plan was designed using SPSS software". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Low risk | Quote: "A random encoding plan was designed using SPSS software and concealed in an envelope Comment: the trial authors used an adequate method to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants who may have had different expectations about the benefits of the intervention they received self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Comment: the trial authors did not give a statement of procedures regarding blinding of the outcome assessor. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "All patients finished the treatment and had a follow‐up visit". Comment: all randomly assigned participants completed the study. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Quote: "All patients finished the treatment and had a follow‐up visit". Comment: the trial authors did not report the method of analysis (ITT versus per protocol). |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for all outcomes reported in the methods section of the publication. |
| Sample size | Unclear risk | Quote: "The 120 subjects in this series...were selected from 202 stroke patients...They were randomly divided into an acupuncture‐massage group and a rehabilitation group, with 60 cases in each". Comment: the extent to which the small to moderate sample size may have introduced bias into estimates of treatment effect is uncertain. |
| Duration of follow‐up | Low risk | Quote: "Each of the above indices was recorded before treatment, at the end of the 6‐week treatment period and at the 12th‐week follow‐up visit". Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Moseley 2004.
| Study characteristics | ||
| Methods |
Design: single‐blind, 2‐arm RCT. (The trial author reported that participants in the control group crossed over into the experimental group. However, we deemed that this trial had not employed a true cross‐over design and we analysed it as a 2‐arm parallel‐group trial up to the endpoint just prior to cross‐over). Setting: hospital physiotherapy department (Australia; dates not reported) Interventions: graded motor imagery (GMI) or ongoing medical management Sample size calculation: not reported |
|
| Participants |
Number of participants: 13 (experimental group n = 7; control group n = 6) Type of noxious initiating event: wrist fracture (upper limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics:
Inclusion criteria: > 6 months post non‐complicated wrist fracture Exclusion criteria:
|
|
| Interventions |
GMI (n = 7) Components of intervention:
Dosage: hand laterality and imagined movements tasks ‐ 3 times; mirror therapy task ‐ 10 times Frequency of administration: each waking hour, daily for 2 weeks (6 weeks in total) Provider: not reported Ongoing medical management (n = 6) Components of intervention:
|
|
| Outcomes | Trial authors assessed outcomes at baseline, at 2 and 4 weeks after commencement of treatment, at the end of the 6‐week treatment period (week 6) and 6 weeks post‐treatment (week 12). The trial authors did not state a primary outcome.
|
|
| Notes |
Source of funding: Clinical Research Fellowship from the National Health and Medical Research Council of Australia ID 210348 Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised by an independent investigator to the 6‐week MIP treatment group or to ongoing medical management (control) using a random number table". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. NPS). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "All assessments were made by a separate investigator who was blind to experimental group and measurement occasion". Comment: the outcome assessor of objective outcomes was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Comment: all randomly assigned participants completed the study (as displayed in the published report's 'Experimental plan'). |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Comment: the trial authors analysed participants in the group to which they were allocated. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors fully reported outcome data graphically for all outcomes, but did not report raw data in numerical form with measures of variation. |
| Sample size | High risk | Quote: "Written informed consent was obtained from the remaining 13 subjects". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Unclear risk | Quote: "Post hoc analyses showed...a significant reduction in all three variables during the MIP with the effect maintained for at least 6 weeks after the completion of treatment". Comment: the clinical relevance of a 6‐week follow‐up of outcomes is uncertain. |
| Other bias | Unclear risk | Comment: we did not identify any other sources of bias. |
Moseley 2005.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 3‐arm, single‐blind RCT Setting: not reported (Australia; dates not reported) Interventions: hand laterality recognition followed by imagined movements followed by mirror movements (RecImMir, MIP) or imagined movements followed by laterality recognition followed by imagined movements (ImRecIm) or laterality recognition followed by mirror movements followed by recognition (RecMirRec) Sample size calculation: not reported |
|
| Participants |
Number of participants: 20 (RecImMir, MIP group (1) n = 7; ImRecIm group (2) n = 6; RecMirRec group (3) n = 7) Type of noxious initiating event: wrist fracture (upper limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics:
Inclusion criteria: onset of CRPS I post non‐complicated wrist fracture > 6 months prior to enrolment Exclusion criteria:
|
|
| Interventions | Participants were advised to avoid changing medication or seeking alternative treatment during the course of the trial up to and including the 12‐week follow‐up. Participants were permitted to attend physiotherapy during the 12‐week follow‐up, but no criteria about physiotherapy were set. RecImMir, group 1 (n = 7) Components of intervention:
Dosage: hand laterality task ‐ 3 times, imagined movements task ‐ twice; mirror therapy task ‐ 5 times Frequency of administration: each waking hour, daily for 2 weeks (6 weeks in total) Provider: not reported ImRecIm, group 2 (n = 6) Components of intervention: 2 weeks imagined movements, 2 weeks hand laterality recognition, 2 weeks imagined movements (components described above) Dosage and frequency of administration: as described above RecMirRec, group 3 (n = 7) Components of intervention: 2 weeks hand laterality recognition, 2 weeks mirror therapy, 2 weeks hand laterality recognition (components described above) Dosage and frequency of administration: as described above |
|
| Outcomes | The trial authors assessed outcomes at baseline, at 2 and 4 weeks after commencement of treatment, at the end of the 6‐week treatment period (week 6) and 12 weeks post‐treatment (week 18). The trial authors did not state a primary outcome.
|
|
| Notes |
Source of funding: Australian Clinical Research Fellowship from the National Health and Medical Research Council of Australia ID 210348 Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using a random numbers table, an independent investigator allocated consenting patients into one of three treatment groups". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Comment: participants were not blinded to treatment allocation but a lack of blinding is unlikely to have biased the results given that participants received interventions judged to have been of relatively equal credibility. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Low risk | Comment: participants were not blinded to treatment allocation and self‐reported their outcomes but lack of blinding unlikely to have biased the results given that participants received interventions judged to have been of relatively equal credibility. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Not applicable. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Comment: all but one randomly assigned participant completed the study, and the one participant appeared to have dropped out from group 3 (as displayed in the published report's 'Treatment plan'). |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Comment: the trial authors did not report the method of analysis (ITT versus per protocol). The trial authors appear to have excluded one participant from group 3 from the analysis in an apparent violation of the principle of ITT. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors fully reported outcome data graphically for all outcomes; but did not report raw data in numerical form with measures of variation. |
| Sample size | High risk | Quote: "Twenty subjects with chronic CRPS1 initiated by wrist fracture and who satisfied stringent inclusion criteria, were randomly allocated to one of three groups". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Low risk | Quote: "Single blind randomised trial with 12‐week follow‐up". Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | Unclear risk | Comment: we did not identify any other sources of bias. |
Moseley 2006.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, single‐blind RCT. NB: this trial recruited participants with CRPS I and phantom limb pain. However, we only included information and data from participants with CRPS for the purpose of this systematic review. Setting: not reported (Australia; dates not reported) Interventions: GMI or physiotherapy and ongoing medical care Sample size calculation: a total sample size of 51 participants would detect an effect size of 0.80 (equivalent to a reduction in pain of 29 mm on a 100 mm VAS), with a probability of 80%, assuming an alpha level of 0.05 |
|
| Participants |
Number of participants: 37 (experimental group n = 17; control group n = 20) Type of noxious initiating event: mixed (fractures n = 14, soft‐tissue injury n = 15, post carpal tunnel release n = 2, venepuncture site n = 2, post finger/toe amputation n = 2, carpal tunnel syndrome n = 1, nail infection n = 1) (upper and lower limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics:
Inclusion criteria: CRPS I of an upper or lower limb Exclusion criteria:
|
|
| Interventions |
GMI (n = 17) Components of intervention:
Dosage: participants were prescribed a training protocol of gradually increased training load according to task difficulty during each of the 3 GMI phases, as detailed by the trial authors Frequency of administration: hourly training (further details not reported) Provider: physiotherapist Physiotherapy and ongoing medical care (n = 20) Components of intervention: not reported Dosage: not reported Frequency of administration: minimum of once per week together with an hourly home programme Provider: physiotherapists |
|
| Outcomes | Outcomes assessed at baseline, at the end of the 6‐week treatment period and 6 months post‐treatment Primary outcomes:
|
|
| Notes | Original trial publication reported data for participants with CRPS I and phantom limb pain (N = 51). Details reported above refer to only those participants with CRPS I (N = 37). Source of funding: not reported Statement regarding declarations of interest: the authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomized via random number generation by an independent investigator...using a random numbers table". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "One female subject in the control group withdrew from the study because she sustained an unrelated injury. There were no other dropouts or withdrawals". Comment: the minimal dropout rate (5% from 1 trial arm) is unlikely to have biased the results. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Comment: the trial authors performed an available case analysis and there was only 1 loss to follow‐up. |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors fully reported outcome data for self‐reported function and pain severity outcomes for participants with CRPS and phantom limb pain combined as conceived in the original trial design. They presented outcome data for participants with CRPS graphically only. |
| Sample size | High risk | Quote: "Fifty‐one patients [37 with CRPS] with phantom limb pain or CRPS1 were randomly allocated". Comment: the small sample size may have introduced bias in the estimates of treatment effect. (We acknowledge that our judgement regarding the risk of bias linked to sample size for this study is based on the purposeful exclusion of a number of participants with phantom limb pain (N = 14) that the original design did not intend). |
| Duration of follow‐up | Low risk | Quote: "All assessments were undertaken at prerandomization and at 6 weeks (completion of the treatment period). Pain VAS and function NRS were also undertaken at 6 months follow‐up". Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | Unclear risk | Comment: we did not identify any other sources of bias. |
Moseley 2009.
| Study characteristics | ||
| Methods |
Design: within‐subject randomised cross‐over design Setting: not reported (Australia; dates not reported) Interventions: tactile discrimination training (TDT) under 4 separate conditions Sample size calculation: not reported |
|
| Participants |
Number of participants: 10 Type of noxious initiating event: mixed (fractures of the hand or wrist n = 4, sprains n = 2, carpal tunnel syndrome n = 2, post hand cannulation n = 1, thumb dislocation n = 1) (upper limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics:
Inclusion criteria: CRPS of 1 wrist of hand Exclusion criteria: not reported |
|
| Interventions |
TDT (n = 10) Components of intervention:
Dosage: 3 x 6‐minute blocks of 24 stimuli were undertaken with a 3‐minute rest period between blocks. Each treatment session involved 72 stimuli and lasted for 24 minutes. Frequency of administration: each participant received 4 sessions of each experimental condition in varying order (total of 16 sessions), with 3 to 4 days between sessions Provider: not reported |
|
| Outcomes | The trial authors assessed outcomes at baseline, immediately and 2 days post‐treatment Primary outcomes: 2‐point discrimination threshold, measured in mm, using a mechanical calliper Secondary outcomes: self‐rated current pain (at rest) severity using a 100 mm VAS anchored with "no pain" and "worst possible pain" |
|
| Notes |
Source of funding: Nuffield Oxford Medical Fellowship, NHMRC Senior Research Fellowship, Templeton Foundation Statement regarding declarations of interest: the authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The conditions were randomised and counterbalanced so that each participant had four sessions of each condition, but in varying order". Comment: the trial authors did not report the method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Comment: this was not applicable (when cross‐over design employed). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: given the nature of the intervention, participants were not blinded to treatment allocation but the extent to which the lack of blinding may have introduced bias is uncertain. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | Unclear risk | Comment: unblinded participants self‐reported some outcomes (e.g. pain intensity) but the extent to which the lack of blinding may have introduced bias is uncertain. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Comment: we do not known whether or not the outcome assessors were blinded to the treatment condition. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Comment: the trial authors did not report any dropouts; they presented results based on the total number of included participants. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Comment: not applicable (when cross‐over design employed). |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors fully reported outcome data graphically for all outcomes; they did not report raw data in numerical form with measures of variation. |
| Sample size | High risk | Quote: "Ten patients with chronic CRPS of one hand or wrist (diagnosed according to Bruehl et al.) were recruited". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "The TPD for the three sites was averaged to provide a measure at pre‐training, post‐training and 2 days later". Comment: the trial authors did not measure outcomes over a clinically relevant length of time. |
| Other bias | Unclear risk | Quote: "...there were 1–2 days between the follow‐up assessment and the next training session. Participants were advised not to undertake tactile training in between sessions". Comment: the extent to which an interval of 1 to 2 days between outcome assessment and training sessions represented an adequate wash‐out period, and therefore the extent to which a carry‐over effect may have introduced bias in the estimates of treatment effect, is not known. |
Mucha 1992.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT. (The trial authors reported that participants in the control group crossed over into the experimental group. However, we deemed that this trial did not employ a true cross‐over design and we analysed it as a 2‐arm, parallel‐group trial up to the endpoint just prior to cross‐over). Setting: not reported (Germany; dates not reported) Interventions: CO2 baths plus exercise therapy or exercise therapy alone Sample size calculation: not reported |
|
| Participants |
Number of participants: 40 (20 per group) Type of noxious initiating event: post‐trauma (no further details reported) (upper limb) Diagnostic criteria: acute algodystrophy of the hand (diagnostic criteria not reported) Baseline characteristics: Total sample (separate intervention and control group data not reported) Age range 47 to 56 years (group data not reported) Duration of CRPS (range) 2 to 6 weeks (group data not reported)
Inclusion criteria:
Exclusion criteria: more than 6 weeks duration of symptoms |
|
| Interventions | Those participants on medication prior to the trial were instructed to cease their medication at the start of the trial CO2 baths plus exercise (n = 20) Components of intervention
Dosage: 12 minute CO2 bath with water temperature of 32 °C to 33 °C and a CO2 concentration of 800 mg/L to 1000 mg/L Frequency of administration: 5 times a week for 4 weeks (20 sessions) Provider: not reported Exercise (n = 20) Components of intervention: progressive exercise therapy. The intensity was dependent on pain level and symptom behaviour. Dosage: not reported Frequency of administration: 5 times a week for 4 weeks (20 sessions) Provider: not reported |
|
| Outcomes | The trial authors assessed outcomes at baseline and twice weekly until completion of the intervention period (4 weeks post recruitment). The trial authors did not state any primary outcomes.
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: " Patients were randomised into two groups". Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Comment: the trial authors did not report the statement of procedures regarding blinding of the outcome assessor. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Comment: there were no apparent dropouts. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Comment: the trial authors analysed participants in the group to which they were allocated but did not explicitly report the method of analysis (ITT versus per protocol). |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors fully reported outcome data graphically for all outcomes; but did not report raw data in numerical form with measures of variation. |
| Sample size | High risk | Quote: "20 participants per group". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Comment: comparison was only possible immediately at the end of the 4‐week therapy session as the control group crossed over to the treatment arm at this point. |
| Other bias | Low risk | Quote: "Statistical testing showed homogeneity across both groups". Comment: there were no apparent baseline differences between groups. Comment: we did not identify any other sources of bias. |
Oerlemans 1999.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 3‐arm, single‐blind RCT Setting: outpatient clinics of 2 university hospitals (The Netherlands; June 1994 to February 1998) Interventions: physical therapy (PT) plus medical treatment or occupational therapy (OT) plus medical treatment or minimal care plus medical treatment (control) Sample size calculation: the study planned to recruit 150 participants (50 per group) in order to be able to detect between‐group differences of 6 to 7 points in the impairment level sum score (ISS) with 80% power |
|
| Participants |
Number of participants: 135 (physical therapy group n = 44; OT group n = 44; SW (control) group n = 47) Type of noxious initiating event: mixed (fracture (53%), spontaneous onset (13%), contusion (11%), mallet finger, carpal tunnel syndrome, postoperative interventions, sprains (proportions not reported) (upper limb) Diagnostic criteria:Veldman 1993 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | All participants received medical treatment according to a fixed pre‐established protocol, consisting of free‐radical scavengers (dimethylsulfoxide (DMSO) 50% applied locally 5 times a day at the affected location or if DMSO‐intolerant, N‐acetylcysteine (600 mg 3 times a day), peripheral vasodilators in the case of primarily cold CRPS I (calcium entry blocker verapamil, sustained‐release 240 mg once per day or ketanserine 20 mg twice per day eventually increased to 40 mg or pentoxifylline 400 mg twice per day) and treatment of trigger points. Participants also received general information regarding CRPS I; including advice to rest the extremity and not provoke pain. PT (n = 44) Components of intervention:
Dosage: 30 minutes per session (details for individual components not reported) Frequency of administration: adjusted to the needs of each individual participant (details not reported) Provider: physical therapists OT (n = 44) Components of intervention:
Dosage: 30 minutes per session (details for individual components not reported) Frequency of administration: adjusted to the needs of each individual participant (details not reported) Provider: occupational therapists Minimal care (n = 47) Components of intervention:
Dosage: 45 minutes per session Frequency of administration: adjusted to needs of each individual participant (details not reported) Provider: social workers |
|
| Outcomes | Outcomes, as reported across trial reports, variously assessed at baseline and at 6 weeks, 3 months, 6 months and 12 months post recruitment. The primary endpoint was the difference in impairment level sum score between baseline and 12 months post recruitment.
|
|
| Notes |
Source of funding: research grant from the National Health Insurance Board (Ziekenfondsraad), The Netherlands Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly assigned to one of three groups". Quote: "Randomisation was restricted to blocks of six". Quote: "Assignment to groups was performed according to allocation lists established by the Department of Medical Statistics of the University of Nijmegen". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Assignment to groups was performed according to allocation lists established by the Department of Medical Statistics of the University of Nijmegen". Comment: the trial authors did not adequately report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Comment: we do not know if outcome assessors were blinded to treatment allocation when measuring percentage loss of joint mobility, impairment ratings, impairment level sum score and disability‐based measures. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Quote: "After inclusion in the study, 44 patients were assigned to PT, 44 patients to OT and 47 patients to CT. In the course of the 1‐year study period, seven, four and four patients abandoned the trial, respectively". Comment: whilst the overall dropout rate was acceptable (11%), there was an unequal dropout rate between groups (PT: 16%, OT: 9%, CT: 9%) and the trial authors did not report the reasons for dropping out. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Low risk | Quote: "Two analyses were done: an intention‐to‐treat analysis (ITT) and a per‐protocol analysis (PP). In the ITT analysis, outcomes of all the participants were used for the group they were originally assigned to. In the PP analysis, outcomes of protocol violators were ignored". Quote: "Three patients from the PT group could not complete the treatment protocol (so were protocol violators) but had test continuity". Comment: the trial authors presented limited data from both ITT and per protocol analyses for selected outcomes. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors reported limited and incomplete outcome data across 4 separate trial reports for self‐reported pain and disability outcomes and for investigator‐administered outcomes. Comment: no numerical data presented for 3 out of the 4 measures of self‐rated pain intensity or percentage of reduced normal mobility outcomes. Comment: no numerical data reported for impairment rating. Comment: limited numerical data presented for ISS. Comment: no numerical data presented for the Radboud Skills Questionnaire, modified Greentest or Radboud Dexterity Test. |
| Sample size | High risk | Quote: "After inclusion in the study, 44 patients were assigned to PT, 44 patients to OT and 47 patients to CT". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Low risk | Quote: "Re‐assessment was performed 6 weeks (t1), 3 months (t2), 6 months (t3) and 12 months (t4) after inclusion in the study". Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | High risk | Quote: "If, during the period of the trial, the patient explicitly indicated that he or she wanted to switch to another adjuvant therapy, this was allowed. Using a coin, with heads or tails it was decided which adjuvant therapy was next". Quote: "Fourteen patients switched therapies: 12 from CT to PT (nine patients) or OT (three patients) and two from OT to PT". Comment: violations of the random sequence generation were permitted. |
Ozcan 2019.
| Study characteristics | ||
| Methods |
Design: parallel, 2‐arm single‐blind RCT Setting: inpatient rehabilitation centre (Turkey; recruitment between April 2014 to March 2015) Interventions: conventional stroke rehabilitation programme plus fluidotherapy or conventional stroke rehabilitation programme alone Sample size calculation: a total sample size of 28 participants were necessary to detect a between‐group difference of at least 2 painDETECT units with 0.80 power and 0.05 error |
|
| Participants |
Number of participants: 32 (experimental group n = 16, control group n = 16) Type of noxious initiating event: hemiplegia following stroke (upper limb) Diagnostic criteria:Harden 2010 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | All participants received a conventional stroke rehabilitation including neurophysiological treatment approaches, occupational therapy, physiotherapy (positioning, ROM, stretching, strengthening exercises, postural control, weight‐shifting, gait training, endurance training, orthosis (if required) and education), and speech therapy (if required). Both groups also received conventional TENS (Everyway branded, EV‐603M) to the hemiplegic upper extremity at a frequency of 100 hertz with 10 mA to 30 mA and 50 ms to 100 ms pulse duration. Stroke rehabilitation plus fluidotherapy (n = 16) Components of the intervention:
Dosage: 2 to 4 hours of rehabilitation plus 20 minutes of fluidotherapy Frequency of administration: 5 days a week for 3 weeks (total 15 sessions) Provider: not reported Stroke rehabilitation programme (n = 16) Dosage: 2 to 4 hours a day Frequency of administration: 5 days a week for 3 weeks (total 15 sessions) Provider: not reported |
|
| Outcomes | The trial authors assessed outcomes at baseline and on completion of the intervention period.
|
|
| Notes |
Source of funding: no funding was reported Statement regarding declarations of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated randomization program was used to randomly assign the patients to the control group or experimental group." Comment: it is likely that the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. VAS). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "Same investigator (U.H.T) who was blinded to group allocation performed the pre and post‐treatment evaluations". Comment: the outcome assessor of objective outcomes was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Quote: "During the rehabilitation program 1 patient from each group had to remove from the study because of the new onset unstable medical conditions. At last 15 patients in control group and 15 patients in experimental group completed the rehabilitation program and were included the final analysis". Comment: the minimal dropout rate (1 participant from each trial arm) is unlikely to have biased the results. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Comment: the trial authors excluded 2 participants (1 from the fluidotherapy group and 1 from the control group) from the analysis because of the onset of unstable medical conditions, in violation of the ITT principle. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors did not provide a study protocol and outcome measures are reported as median and range without measures of variance. |
| Sample size | High risk | Quote: "Considered the inclusion and exclusion criteria only 32 patients were eligible for study and they were randomly assigned to control and experimental group". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "We evaluated the patients before and after a 3‐week rehabilitation program". Comment: the trial authors did not measure outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Ryan 2017.
| Study characteristics | ||
| Methods |
Design: parallel‐group, placebo‐controlled, 2‐arm pilot RCT Setting: NHS Hospital (United Kingdom, dates not reported) Interventions: usual care physiotherapy plus transcutaneous electrical nerve stimulation (TENS) or placebo TENS Sample size calculation: since this was a feasibility study a sample size calculation was not undertaken |
|
| Participants |
Number of participants: 8 (experimental group n = 6, control group n = 2) Type of noxious initiating event: not reported (upper limb) Diagnostic criteria: 'Budapest criteria' Harden 2010 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | All participants received usual care physiotherapy including, but not limited to, advice, education, exercise, cognitive behavioural therapy, motor imagery, hand laterality recognition training, desensitising and hydrotherapy TENS (n = 6) Components of the intervention: patient self‐administered, pulsed, synchronised dual channel TENS using a two‐channel TENS unit (Elpha II 3000 muscle and pain stimulator, Danmeter) was applied to the upper arm proximal to the affected site Dosage: 20 pulses, delivered over a 1‐second period (20 Hz stimulation frequency) with a non‐stimulation interval of 5 seconds Frequency of administration: 90 minutes daily for 3 weeks (total number of sessions completed not reported) Provider: usual care physiotherapy was provided by a single physiotherapist and TENS was self‐administered Placebo TENS (n = 2) Components of the intervention: the placebo group received TENS in an identical manner to the active intervention except that no electrical current was delivered. The power light flashed pulsatingly to indicate the device was switched on. Provider: usual care physiotherapy was provided by a single physiotherapist and placebo TENS was self‐administered |
|
| Outcomes | The trial authors assessed outcomes at baseline, on the completion of the intervention period (3 weeks) and at 3 months:
|
|
| Notes |
Source of funding: this study was supported by a research grant from the British Association of Hand Therapists Statement regarding declarations of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible participants provided informed consent and were randomly allocated to TENS or placebo TENS using a random number generator". Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Low risk | Quote: "Eligible participants provided informed consent and were randomly allocated to TENS or placebo TENS using a random number generator and pre‐filled concealed envelopes by a team member uninvolved in participant contact." Comment: the trial authors used an acceptable method to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The placebo group received TENS in an identical manner to the active intervention except that no electrical current was delivered, although the power light flashed pulsatingly indicating that the device was switched on. It was impossible to blind participants to receiving a strong non‐painful TENS sensation." Quote: "Blinding the therapist was not possible". Comment: given the nature of the intervention, participants may not have been blinded to treatment and may have had different expectations about the benefits of each intervention. Personnel were not blinded and may have inferred different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Quote: "It was impossible to blind participants to receiving a strong non‐painful TENS sensation." Comment: the sham intervention did not control for the sensory characteristics of the real intervention and as such participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. Quote: "At the three‐month follow‐up, all three of the participants from the TENS group who completed these questions were certain that their TENS unit was working correctly, while the one participant from the placebo group thought that the TENS unit was working correctly but was not certain". Comment: while trialists attempted to investigate patients' expectations and the validity of their single‐blinding procedures, the dropout rate of 50% means they were not able to do this thoroughly. |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | High risk | Quote: "There was a 50% dropout rate with only four participants providing data at the three‐month follow‐up point". Comment: the high dropout rate may have introduced bias in the estimates of treatment effect. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Comment: the method of analysis (ITT versus per protocol) was not reported. Comment: 2 out of 8 participants did not receive their allocated intervention. |
| Selective reporting (reporting bias) | Low risk | Comment: reported data were either presented graphically or incomplete. Comment: the authors supplied the missing data for our outcomes of interest on request. |
| Sample size | High risk | Quote: "Thirteen individuals initially showed interest in participating of whom eight consented and were randomised". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Low risk | Quote: "VAS data were collected at baseline, post‐treatment and at three‐month follow‐up" Comment: the trial authors measured outcomes over a clinically relevant length of time. |
| Other bias | High risk | Quote: "The imbalance in the randomisation was also an issue. The randomisation had been undertaken to ensure an equal number of 15 participants would be randomised to each group; however, by chance, the random sequence initially was loaded towards assigning more to the intervention group rather than the placebo group." Quote: "In addition, monitoring the number of usual care physiotherapy sessions was an important step with respect to monitoring co‐interventions. The number of sessions varied quite considerably between participants". Comment: the trial groups were imbalanced and engagement with physiotherapy treatment differed between groups, which may have introduced bias in the estimates of treatment effects. Quote: "Those who once fulfilled the criteria, no longer did, but had ongoing pain were classed as CRPS‐NOS (not otherwise specified) and were also included". Comment: including patients who no longer satisfied the trial's diagnostic criteria may have compromised the external validity of the findings. |
Saha 2021.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT Setting: out‐patient rehabilitation centre (India, dates not reported) Interventions: mirror therapy plus stroke rehabilitation or stroke rehabilitation Sample size calculation: “In this study, expected effect size d was considered as 0.4. Sample size estimation yielded a sample size of 42, with significance level α = 0.05 and a power of study 80%” |
|
| Participants |
Number of participants: 38 (19 in each group) Type of noxious initiating event: stroke (upper limb) Diagnostic criteria: shoulder‐hand syndrome (i.e. post‐stroke complex regional pain syndrome), (diagnostic criteria not reported) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants in both groups received 4 weeks of conventional stroke rehabilitation comprising supervised neurodevelopmental facilitation techniques, range of motion exercises, stretching for elbow, wrist, fingers and task training of the upper extremity; 30 minutes a day, 5 days a week for 4 weeks Stroke rehabilitation plus mirror therapy (n = 19) Components of intervention: patients were seated on a chair or stool close to a mirror (55 cm x55 cm) positioned vertically between the patient's upper limbs. The unaffected limb was placed in front of the mirror, whereas the affected limb was placed in the opposite side of the mirror, which made it invisible. Whilst performing the same exercises as those in the ‘Stroke rehabilitation’ group (as detailed below) patients observed the mirror image of their unaffected limb as if it was their affected limb. All patients were instructed to attempt to perform the exercises bilaterally. Dosage: 30 minutes a day Frequency of administration: 5 days a week for 4 weeks (total of 20 sessions) Provider: physiotherapist Stroke rehabilitation (n = 19) Components of intervention: bilateral rhythmical flexion and extension of the shoulder and elbow, forearm supination and pronation, wrist flexion and extension, finger flexion and extension, fanning out the hand, finger and thumb abduction, making a fist and release, lateral prehension, pad to pad, pad to side grip, grasping objects, single finger movement and thumb opposition; stretching of shoulder retractors, elbow flexors, forearm pronators, wrist flexors and finger flexors through weight bearing on affected hand, and touching the opposite shoulder and head by affected hand. Instruction was given to the patients to keep the affected limb elevated during night as much as possible. Patients performed all the exercises of stroke rehabilitation programme, while directly visualising their both affected and unaffected limbs. Dosage: 30 minutes a day Frequency of administration: 5 days a week for 4 weeks (total of 20 sessions) Provider: physiotherapist |
|
| Outcomes | Outcomes assessed at baseline, after treatment and 2 weeks post‐treatment. The trial authors did not state any primary outcome.
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Patients (n = 38) were randomly allocated by sealed, numbered envelopes with the randomization sequence, into two equal groups, Group A (control group) and Group B (experimental group)”. Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Low risk | Quote: “Patients (n = 38) were randomly allocated by sealed, numbered envelopes with the randomization sequence, into two equal groups, Group A (control group) and Group B (experimental group)”. Comment: the trial authors probably used an acceptable method to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | High risk | Quote: “All the evaluations were carried out by the same physiotherapist, who have supervised the therapy, so there was no blinding to group allocation”. Comment: outcome assessors were unblinded to participant group allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | High risk | Quote: “Initial sample of 38 patients witnessed five dropouts along the course of the study. Thirty‐three patients (Group A [n = 17], Group B [n = 16]) completed the 4‐week supervised stroke rehabilitation program and participated in postintervention evaluation. Three patients were lost to follow‐up and hence 30 patients (Group A [n = 15] and Group B [n = 15]) were included for the statistical analyses" Quote: “A plausible limitation of this study is the dropouts due to inability to continue intervention and also missed follow‐up by a considerable number of patients”. Comment: an overall dropout rate of 21% may have introduced bias in the estimates of treatment effect. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Quote: “As reasons for dropout were nonclinical, so a per‐protocol analysis instead of an intention‐to‐treat analysis, was used during the statistical analysis to see the effect of interventions if patients were fully compliant”. Comment: violation of the principle of ITT analysis may have introduced bias in the estimates of treatment effect. |
| Selective reporting (reporting bias) | Low risk | Comment: outcome data were adequately reported for all outcomes reported in the methods section of the publication. |
| Sample size | High risk | Quote: “…hence 30 patients (Group A [n = 15] and Group B [n = 15]) were included for the statistical analyses”. Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Unclear risk | Quote: “Evaluations were done at baseline, immediately after 4‐week intervention and during follow‐up after 2‐week postintervention”. Comment: the clinical relevance of a 2‐week follow‐up of outcomes is uncertain. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Sarkar 2017.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 3‐arm, single‐blind RCT Setting: urban pain referral centre (India; recruitment from January 2016 to June 2016) Interventions: anti‐neuropathic medicine and contrast baths or anti‐neuropathic medicine and exercise or anti‐neuropathic medicine and mirror therapy Sample size calculation: not reported |
|
| Participants |
Number of participants: 30 (10 in each group) Type of noxious initiating event: aetiology not reported (upper and lower limb) Diagnostic criteria: 'Budapest criteria' Harden 2007 (CRPS type not reported) Baseline characteristics: not reported Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | All participants received anti‐neuropathic medicines (gabapentin 900 mg daily in 3 divided doses and amitriptyline 10 mg daily) Contrast baths (n = 10) Components of the intervention: patients were asked to immerse the affected body part (hand/foot) in cold and hot water (tolerable) alternatively for 3 minutes and 1 minute, respectively. Procedures started and ended with cold water immersion. Dosage: 15 minutes per session Frequency of administration: details not reported Provider: not reported Exercise (n = 10) Components of the intervention: patients were seated comfortably keeping a nonreflecting board or curtain perpendicular to his or her midline with the unaffected limb facing the non‐reflective surface and affected limb hidden. Patients were asked to do exercises of the unaffected limb attending to the non‐reflective surface, which was followed by their painful limb (if possible). The following movements were practised:
Dosage: 2 minutes of exercise followed by 2 minutes of rest, for 20 minutes Frequency of administration: twice per day (duration of intervention period not explicitly reported) Provider: not reported Mirror therapy (n = 10) Components of the intervention: patients were asked to sit comfortably keeping a mirror perpendicular to the midline with the unaffected side in front of the reflecting surface of mirror and the affected side hidden behind the mirror. The affected limb was relaxed and rested on a support surface behind the mirror throughout. Patients were asked to look at the mirror and assume that the mirror image of unaffected side was the affected body part. Patients performed exercises (not fully reported) of the unaffected body part in a full and pain free range in all directions front of the mirror. By seeing the mirror image patients imagined the affected limb was moving in pain‐free manner. Dosage: 2 minutes of exercise followed by 2 minutes of rest, for 20 minutes Frequency of administration: twice per day (duration of intervention period not explicitly reported) Provider: not reported |
|
| Outcomes | Outcomes assessed at baseline, and at 1, 2 and 4 weeks within the intervention period. No follow‐up post intervention.
|
|
| Notes |
Source of funding: no funding was provided Statement regarding declarations of interest: the authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The patients were asked to draw a chit from a jar containing 30 chits (10 chits for each group), and they were randomly allocated into following three groups containing ten patients in each group". Comment: the trial authors used a non‐random sequence generation process. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not adequately report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "The progression and outcome of each subject were recorded by an independent investigator (single‐blinded study– blinded at the level of investigator)". Comment: outcome assessors were blinded to participants' group allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Comment: not reported. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the method of analysis (ITT versus per protocol) was not reported. |
| Selective reporting (reporting bias) | Low risk | Comment: the trial authors reported outcome data for all outcomes reported in the methods section of the publication but reported the standard error of the mean rather than the standard deviation. Comment: the authors supplied the missing data for our outcomes of interest on request. |
| Sample size | High risk | Quote: "A total 30 patients were selected". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Unclear risk | Comment: not adequately reported. |
| Other bias | Unclear risk | Comment: baseline sample demographics and characteristics not reported. |
Schreuders 2014.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm, single‐blind RCT Setting: not reported (The Netherlands; dates not reported) Interventions: GMI programme plus conventional treatment or conventional treatment alone Sample size calculation: not reported |
|
| Participants |
Number of participants: 18 (experimental group n = 11, control group n = 7) Type of noxious initiating event: not reported (upper limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria: not reported |
|
| Interventions | All participants received conventional treatment including a 6‐week OT and physiotherapy programme, including training of grip function, muscle strengthening and joint mobility interventions, writing exercises and advice to reduce the use of splints. Participants were asked not to participate in other treatment programmes during the 12‐week period and not to change the type or dosage medication of their medication unless instructed to do so by their physician. GMI programme (n = 11) Components of intervention:
Dosage: 10 minutes Frequency of administration: every hour (3 times per day minimum) for a total of 6 weeks Provider: therapists (distinction between physio‐ and occupational therapist not reported) Standard care (n = 7) Components of intervention:
Dosage: 60 minutes per week (over 1 or 2 sessions) Frequency of administration: 1 or 2 sessions per week, for 6 weeks Provider: physical therapists and occupational therapists |
|
| Outcomes | Outcomes were assessed at baseline and after 3, 6 (immediately post‐treatment) and 12 weeks (6 weeks post‐treatment) post enrolment Primary outcomes:
Secondary outcomes: fine hand co‐ordination of both hands by using the Nine Hole Peg Test (recorded in seconds) |
|
| Notes |
Source of funding: ErasmusMC Mrace Project Zorg 2004‐20, grant number 2004‐20 Statement regarding declarations of interest: the trial authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Based on a computerized random schedule..." Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Low risk | Quote: "Based on a computerized random schedule, a researcher not involved in the execution of the trial, made a sequence of numbered opaque envelopes. These envelopes were prepared with equality being achieved after every ten subjects (block size 10)". Quote: "Envelopes were given in sequence of entry to the patient and were opened by the patient". Comment: the trial authors used an acceptable method to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Patients were not blinded to the treatment as they were aware of the treatment content". Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "The assessor was blinded for the allocation to the experimental or control group". Quote: "The measurements were performed by trained blinded assessors". Comment: the trial authors blinded outcome assessors to participant group allocation |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | High risk | Comment: the trial authors did not adequately report the dropout rate in the 'Results' section of the manuscript. Comment: according to 'Figure 2' of the manuscript, 1 participant was lost to follow‐up and 2 discontinued the intervention from the experimental group, 1 participant withdrew after randomisation, 1 participant was lost to follow‐up and 3 discontinued the intervention from the conventional treatment group, giving dropout rates of 27% and 71% respectively, and an overall dropout rate of 44%. Comment: the high dropout rate may have introduced bias in the estimates of treatment effect. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Comment: the trial authors reported analysis as ITT in Figure 2 of the unpublished manuscript. Quote: "Three patients (one in the experimental group, two in the control group) could not be included in the analysis due to insufficient compliance in filling out the VAS and RASQ questionnaires or because of immediate withdrawal from the control therapy because the participants only wanted the graded MIP". Comment: violation of the principle of ITT analysis may have introduced bias in the estimates of treatment effect. Quote: "From seven of the remaining fifteen patients (five in the experimental group and two in the control group) there were missing end‐tests" (i.e. at 12 weeks post enrolment/6 weeks postintervention). Quote: "Differences in changes in both groups over times were tested using a generalized estimating equations (GEE) approach. Under the assumption that missing data were random and not due to group allocation or treatment effect, this model estimates missing data values, thereby allowing the use of data from all participants, irrespective of whether they were measured at all time points". Comment: use of GEE may have introduced bias in the estimates of treatment effect. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors reported outcome data graphically for all self‐reported pain outcomes and did not report raw data in numerical form with measures of variation. The trial authors presented effect sizes with measures of variation for the Radboud Skills Questionnaire and Nine Hole Peg Test and did not report numerical data with measures of variation. |
| Sample size | High risk | Quote: "For this trial eighteen patients were included". Quote: "For this study only 18 patients were assessed for eligibility and only 15 of them could be included in the analysis. The number of patients in the study was therefore too small to detect possible effects with the intended power for which 52 patients were needed". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | Unclear risk | Quote: "Outcome was assessed at baseline, after 3, 6 and 12 [i.e. 6 weeks post‐treatment] weeks". Comment: the clinical relevance of a 6‐week follow‐up of outcomes is uncertain. |
| Other bias | High risk | Comment: baseline data for 3 participants excluded from the analysis not reported. Comment: likely highly significant baseline imbalance in duration of symptoms between groups. |
Strauss 2021.
| Study characteristics | ||
| Methods |
Design: cross‐over group, 2‐arm RCT Setting: University Medical Centre; recruitment via support groups (Germany; from 2019 to 2020) Interventions: graded motor imagery or wait‐list control Sample size calculation: “Statistical power calculations were based on the outcome parameter “pain” from the study of Moseley, 2006. Here, the GMI training showed an improvement of 23.4 mm (range: 16.2−30.4 mm) on a 100mm VAS whereas the control group (physiotherapy without GMI) showed only an improvement of 10.5 mm (range: 1.9−19.2 mm). A resulting effect size of 1.29 (G*power) with alpha 0.05 and power 0.95 (one‐tailed) resulted in 9 participants per treatment group. In addition a 15% dropout rate for longitudinal studies had to be added. Because the results of Moseley, 2006 were considered rather optimistic, the group size of the current study was planned for about 25 participants for inclusion in the study and about 22 participants for final analysis of treatment effect.” |
|
| Participants |
Number of participants: 22 (numbers randomised to each phase not reported; baseline data for only 20 of 22 participants reported) Type of noxious initiating event: mixed (carpal tunnel surgical intervention (25%), ‘cervical spine’ (10%), ‘other surgery’ (40%), wrist fracture (20%), not reported (5%)) (upper limb) Diagnostic criteria: unilateral CRPS type II (diagnostic criteria not reported) Baseline characteristics: Total sample (separate data by treatment phase not reported):
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Graded motor imagery Components of intervention: 3 sequential treatment stages (left/right judgements, imagined movements, mirror therapy) each lasting 2 weeks. The first 2 stages were performed with the ‘Recognise Hand’ app (Neuro Orthopaedic Institute, Australia). The mirror therapy stage was performed with a foldable mirror and a set of cars with images of hands in different positions. For left/right judgements, patients were asked to classify whether images showed a left or right hand. For imagined movements, patients were asked to mentally match the exact hand posture shown in the picture. For mirror therapy, patients were asked to perform movements displayed on the cards with their non‐affected hand first while observing it in the mirror, and then increasing the intensity of the tasks by using objects and coactivating the affected hand that remained in the mirror box. Dosage: at least 10 minutes every waking hour Frequency of administration: 7 days a week for 6 weeks Provider: not reported 6‐week waiting period Components of intervention: not reported |
|
| Outcomes | Outcomes were assessed at baseline, after treatment phase 1 at 6 weeks, and after treatment phase 2 at 12 weeks. The trial authors did not state any primary outcome.
|
|
| Notes |
Source of funding: "ML was supported by the National Institute for Health & Collaborative Research Australia for travel to Adelaide (Memorise Grand) and the DFG (LO 795/28‐1). NN received local funding from the exchange program of the University of Greifswald (International Office). SS was awarded a Gerhard‐Domagk fellowship for undertaking this study; he also received a grant by the Else Kroner Fresenius‐Stiftung 2019‐A24, which enabled to support JH and SB during their doctoral thesis." Statement regarding declarations of interest: "ML receives financial reimbursement for editing a Neuroscience journal by the Thieme Verlag. GLM has received support from: ConnectHealth UK, Seqirus, Kaiser Permanente, Workers’ Compensation Boards in Australia, Europe and North America, AIA Australia, the International Olympic Committee, Port Adelaide Football Club, Arsenal Football Club. Professional and scientific bodies have reimbursed him for travel costs related to presentation of research on pain at scientific conferences/symposia. He has received speaker fees for lectures on pain and rehabilitation. He receives book royalties from NOIgroup publications, Dancing Giraffe Press & OPTP for books on pain and rehabilitation. The funding organizations did not have an impact on the design of the study and the results reported here." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “participants were randomly allocated to one of 2 groups; random group 1 started with the 6‐week training period after the baseline parameters had been collected. After 6 weeks of GMI therapy in random group 1, a 6 week waiting period followed. Random group 2 started with a 6‐ week waiting period and continued with the 6‐week GMI therapy.” Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Quote: “participants were randomly allocated to one of 2 groups; random group 1 started with the 6‐week training period after the baseline parameters had been collected. After 6 weeks of GMI therapy in random group 1, a 6 week waiting period followed. Random group 2 started with a 6‐ week waiting period and continued with the 6‐week GMI therapy.” Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Quote: “Effects (behavioural measures and fMRI) over groups were evaluated by an evaluator blinded for the GMI or waiting period.” Comment: it is unclear whether the authors considered the CRPS Severity Score a ‘behavioural’ measure’ and as such it is unclear whether the outcome assessor for this outcome was blinded. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Unclear risk | Quote: “Twenty‐six CRPS patients were included for the intervention study. Twenty‐two finished measurements as planned but 2 of these could not come to the post MRI assessment after GMI intervention, because of the onset of SARS‐CoV‐2 (corona virus) pandemic in March 2020.“ Comment: the extent to which an overall dropout rate of 15% may have introduced biased estimates of treatment effect is uncertain. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Quote: “Twenty‐six CRPS patients were included for the intervention study. Twenty‐two finished measurements as planned, but 2 of these could not come to the post MRI assessment after GMI intervention, because of the onset of SARS‐CoV‐2 (corona virus) pandemic in March 2020. Therefore, in the final group analysis we included 20 patients diagnosed with CRPS”. Comment: the method of analysis was not reported for clinical outcomes. The trial authors excluded 6 participants in violation of the ITT principle. |
| Selective reporting (reporting bias) | Low risk | Comment: outcome data for pain intensity and CRPS Severity Score were inadequately reported after treatment phases and DASH was only reported at baseline. Comment: the authors supplied the missing data for our outcomes of interest on request. |
| Sample size | High risk | Quote: “Twenty‐six CRPS patients were included for the intervention study. Twenty‐two finished measurements as planned“. Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: “participants were randomly allocated to one of 2 groups; random group 1 started with the 6‐week training period after the baseline parameters had been collected. After 6 weeks of GMI therapy in random group 1, a 6 week waiting period followed. Random group 2 started with a 6‐ week waiting period and continued with the 6‐week GMI therapy. After each time period, clinical and neurophysiological parameters were assessed”. Comment: the trial authors did not measure outcomes over a clinically relevant length of time. |
| Other bias | High risk | Quote: “…we investigated 20 CRPS patients in a wait‐list crossover design with 3 evaluation time points. Patients underwent a 6 week GMI treatment and a 6 week waiting period in a randomized group assignment…” Comment: in the trial registry the study is variously described as ‘non‐interventional’, ‘observational’ and a ‘non‐randomised controlled trial’ (https://drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00017214). Comment: in the trial report the trial authors did not state any primary outcome. In the trial registry the primary outcome is specified as ‘Pain intensity (visual analogue scale, after the 6 weeks training period)’. Comment: differences in descriptions of the trial design and specification of a primary outcome measure between the trial registration and the published trial report may have introduced bias. Comment: the absence of a washout period between treatment periods allows for potential differential carryover effects that may have biased estimates of treatment effect. |
Topcuoglu 2015.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT Setting: Ankara Physical Medicine and Rehabilitation Education and Research Hospital (Turkey; recruitment between March 2009 to September 2009) Interventions: physiotherapy plus upper extremity aerobic exercise or physiotherapy alone Sample size calculation: not reported |
|
| Participants |
Number of participants: 40 (20 in each group) Type of noxious initiating event: hemiplegia following stroke (upper limb) Diagnostic criteria:Bruehl 1999 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | All participants received medical treatment and physiotherapy programmes for CRPS and stroke rehabilitation. The CRPS physiotherapy programme included TENS (shoulder‐hand region encompassing the painful region (100 Hz frequency, 20 min per day)), cold pack (20 minutes per day), retrograde massage and contrast baths, The comprehensive stroke physiotherapy programme included therapeutic exercises, neurophysiological exercises, postural exercises, balance and co‐ordination exercises and exercises of activities of daily living. The medical treatment included diclofenac Na (twice per day) and paracetamol (4 times per day) (doses not reported). Physiotherapy plus upper extremity aerobic exercise (n = 20) Components of the intervention: arm crank ergonometry using a 35 cm‐diameter upper arm ergonometer with adjustable resistance (MONARK, Riverside, CA, USA) Dosage: upper extremity aerobic exercise was performed at 5 watts per minute for 30 minutes Frequency of administration: physiotherapy frequency not reported; upper extremity aerobic exercise was performed 5 days a week for 4 weeks Provider: doctor in cardiopulmonary rehabilitation Physiotherapy (n = 20) Dosage and frequency of administration: not reported |
|
| Outcomes | The trial authors assessed outcomes at baseline and on completion of the intervention period. Primary outcomes:
Secondary outcomes:
|
|
| Notes |
Source of funding: no funding received Statement regarding declarations of interest: the authors declared no conflicts of interest |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed using computer‐generated numbers and the treatment group was assigned by the system." Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. VAS). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Unclear risk | Quote: "Four weeks later after the treatment ended, the assessments were repeated by the same assessor physician, who was unaware of the patient’s group assignment." Comment: the outcome assessor of investigator‐administered outcomes was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Comment: the trial authors did not report any information regarding the presence or absence of dropouts or a study participant flowchart but all randomised participants were accounted for in the analyses. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the method of analysis (ITT versus per protocol) was not reported. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors did not provide a study protocol and reported incomplete outcome data for measures of pain. Only one of the continuous outcome measures was reported using point estimates and measures of variance. |
| Sample size | High risk | Quote: "The study included 40 patients with CRPS I after stroke". Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "These assessments were performed at baseline week 0 and after the end of the program week 4.". Comment: outcomes were not measured over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Uher 2000.
| Study characteristics | ||
| Methods |
Design: parallel‐group, 2‐arm RCT Setting: not reported (Germany, dates not reported) Interventions: manual lymph drainage (MLD) plus exercise or exercise alone Sample size calculation: not reported |
|
| Participants |
Number of participants: 40 (15 in the manual lymph drainage group, 25 in the exercise alone group) Type of noxious initiating event: mixed (postfracture n = 27, post dislocation n = 9, postsurgery n = 4) (lower limb) Diagnostic criteria: CRPS I (diagnostic criteria not reported) Baseline characteristics: Total sample: female:male 31:4
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants were given a brochure providing general advice (details not reported), no analgesic or anti‐inflammatory medication prescribed, participants were asked to inform the clinician if they took analgesia or anti‐inflammatory medication for more than 3 days. Manual lymph drainage plus exercise (n = 15) Components of intervention:
Dosage: 30 minutes Frequency of administration: 3 times per week for 6 weeks (18 sessions) Provider: physiotherapists Exercise (n = 25) Components of intervention:
Dosage: 30 minutes Frequency of administration: 3 times per week for 6 weeks (18 sessions) Provider: physiotherapists |
|
| Outcomes | Outcomes assessed at baseline and immediately on completion of the intervention period (6 weeks post recruitment). The trial authors did not state any primary outcome.
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the trial authors did not report the method of sequence generation. |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomisation was done using the sealed envelope method, by a doctor not involved in the study". Comment: the trial authors used an acceptable method to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. pain intensity). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "Tested by a doctor who did not know group assignment". Comment: the outcome assessor was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Comment: an overall, and balanced, dropout rate of 12% is unlikely to have biased the results. |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | High risk | Comment: the trial authors excluded three participants (2 from the MLD group and 1 from the exercise group) from the analysis because they did not regularly attend for therapy, in violation of the ITT principle. Two participants from the exercise group were excluded after randomisation secondary to wrongful inclusion despite fulfilment of exclusion criteria. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors did not report outcome data for pain intensity. |
| Sample size | High risk | Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "Assessment after six weeks of therapy". Comment: outcomes were re‐measured on immediate completion of the intervention period only and were not measured over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Vural 2016.
| Study characteristics | ||
| Methods |
Design: parallel, 2‐arm, single‐blind RCT Setting: training and research hospital (Turkey; recruitment between November 2011 to September 2012) Interventions: conventional stroke rehabilitation programme plus mirror therapy or conventional stroke rehabilitation programme alone Sample size calculation: calculated with an assumed difference in post‐treatment VAS score of 1.2 between groups. A total sample size of 28 (14 study participants and 14 controls) was necessary for a 2‐sided test with statistical power of 0.90 and an alpha level of 0.05. |
|
| Participants |
Number of participants: 30 (15 in each group) Type of noxious initiating event: hemiplegia following stroke (upper limb) Diagnostic criteria:Veldman 1993 (CRPS I) Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | All participants received a patient‐specific conventional stroke rehabilitation programme consisting of neurodevelopmental facilitation techniques, occupational therapy, physiotherapy and speech therapy (if required). Mirror therapy (n = 15) Components of the intervention:
Dosage: 2 to 4 hours of rehabilitation plus 30 minutes of mirror therapy Frequency of administration: 5 days a week for 4 weeks (total 20 sessions) Provider: not reported Stroke rehabilitation programme (n = 15) Dosage: 2 to 4 hours a day Frequency of administration: 5 days a week for 4 weeks (total 20 sessions) Provider: not reported |
|
| Outcomes | The trial authors assessed outcomes at baseline and on completion of the intervention period.
|
|
| Notes |
Source of funding: not reported Statement regarding declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly assigned to the mirror therapy group or the control group using computer‐generated random numbers" Comment: the trial authors used an acceptable method to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the trial authors did not report the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: given the nature of the intervention, participants were not blinded to treatment and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) Self‐reported outcomes | High risk | Comment: unblinded participants, who may have had different expectations about the benefits of the intervention they received, self‐reported some outcomes (e.g. VAS). |
| Blinding of outcome assessment (detection bias) Investigator‐administered outcomes | Low risk | Quote: "The assessments were performed by the same investigator (S.P.V.), who was blinded to group allocation." Comment: the outcome assessor of investigator‐administered outcomes was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) Dropout rate described and acceptable | Low risk | Comment: all randomly assigned participants completed the study (as displayed in the published report's 'Flow diagram'). |
| Incomplete outcome data (attrition bias) Participants analysed in the group to which they were allocated | Unclear risk | Comment: the method of analysis (ITT versus per protocol) was not reported. |
| Selective reporting (reporting bias) | High risk | Comment: the trial authors did not provide a study protocol and outcome measures are reported as median and range without measures of variation. |
| Sample size | High risk | Quote: "According to these criteria, 30 patients were eligible for the study." Comment: the small sample size may have introduced bias in the estimates of treatment effect. |
| Duration of follow‐up | High risk | Quote: "We evaluated the clinical outcome scales only twice, before and 4 weeks after the therapy, and did not include follow‐up evaluation". Comment: the trial authors did not measure outcomes over a clinically relevant length of time. |
| Other bias | Low risk | Comment: we did not identify any other sources of bias. |
Abbreviations: CRPS I: complex regional pain syndrome type 1; CT: control therapy; GMI: graded motor imagery; IFC: interferential current; ITT: intention to treat; MIP: motor imagery programme; MLD: manual lymphatic drainage; NPS: neuropathic pain scale; NRS: numerical rating scale; OT: occupational therapy; PT: physiotherapy/physical therapy; RCT: randomised controlled trial; RSD: reflex sympathetic dystrophy; SD: standard deviation; SGB: stellate ganglion block; SPSS: Statistical Package for the Social Sciences; SW: social work; TDT: tactile discrimination training; TENS: transcutaneous electrical nerve stimulation; TPD: two‐point discrimination; US: ultrasound; VAS: visual analogue scale.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bolel 2006 | This study only evaluated the outcome measure of 'sympathetic skin response' and fell outside the inclusion criteria of this review |
| David 2015 | Not a RCT Previously registered as a RCT (NCT 01915329) in the original review ('Characteristics of ongoing studies' table) (Smart 2016) |
| den Hollander 2020 | Not a RCT |
| Dimitrijevic 2018 | The study authors evaluated 'infrared thermography' and 'hand oedema' as outcome measures, which fell outside the inclusion criteria of this review |
| Fialka 1992 | Not a RCT |
| Fialka 1996 | Autogenic training does not fall within the scope of practice of physiotherapy |
| Field 1993 | Not a RCT |
| Gromo 1974 | Not a RCT |
| Jasmina 2012 | Not a RCT |
| JPRN‐UMIN000027348 | Not a RCT (cross‐over, non‐randomised); originally identified in a trial registry Trial terminated early secondary to the transfer of a researcher (personal communication: Prof. Naoki Aizu, 8 August 2020) |
| Karabegović 2009 | Not a RCT |
| Kocić 2010 | The study authors evaluated 'infrared thermovision' as the only outcome measure, which fell outside the inclusion criteria of this review |
| Kotiuk 2019 | The study authors evaluated 'body perception disturbance' as the only outcome measure, which fell outside the inclusion criteria of this review |
| Liao 2006 | Acupuncture does not fall within the scope of practice of physiotherapy as defined in our protocol (Smart 2013) |
| Marianne 2015 | Not a RCT Previously registered as a RCT (NCT01915329) in the original review ('Characteristics of ongoing studies' table) (Smart 2016) |
| NCT02667717 | Originally identified in a trial registry. Trial terminated early secondary to difficulties recruiting patients and an apparent lack of effect from the experimental intervention (intermediate analysis). Observations reported by the primary investigator included: 1) 27 from a target of 88 participants had been recruited at the point of early termination, 2) after an intermediate statistical analysis it was found that there was a significant pain improvement in both groups but without any differences between groups and that the clinical improvement was maintained after 16 weeks in both groups, 3) there were no serious adverse events, 4) patients and practitioners found the experimental intervention interesting but too time consuming (personal communication: Dr Christelle Créac'h, 6 August 2020). |
| Perrigot 1982 | Not a RCT |
| Solcà 2018 | Not a RCT |
| Toth 2014 | The trial included participants (N = 54) with mixed aetiologies but only 2 participants with complex regional pain syndrome (CRPS) with 1 randomised to each trial arm. We could not make any meaningful comparison. |
| Tulgar 1991 | Not a RCT |
| Wu 1999 | Qigong does not fall within the scope of practice of physiotherapy |
| Zyluk 1994 | Not a RCT |
Abbreviations: RCT: randomised controlled trial.
Characteristics of studies awaiting classification [ordered by study ID]
Dimitrijevic 2019.
| Methods | Not yet assessed |
| Participants | Not yet assessed |
| Interventions | Not yet assessed |
| Outcomes | Not yet assessed |
| Notes | The findings from this trial are currently only available as a conference abstract |
Dimitrijevic 2020.
| Methods | Not yet assessed |
| Participants | Not yet assessed |
| Interventions | Not yet assessed |
| Outcomes | Not yet assessed |
| Notes | The findings from this trial are currently only available as a conference abstract |
ISRCTN39729827.
| Methods | Not yet assessed |
| Participants | Not yet assessed |
| Interventions | Not yet assessed |
| Outcomes | Not yet assessed |
| Notes | As of 18 August 2020 we were unable to make contact with the author for an update of this trial's progress |
ISRCTN97144266.
| Methods | Not yet assessed |
| Participants | Not yet assessed |
| Interventions | Not yet assessed |
| Outcomes | Not yet assessed |
| Notes | As of 30July 2020 we were unable to make contact (email delivery failure) with the author for an update of this trial's progress. We note that this trial was registered in 2005 and now assume that it is unlikely ever to be published. |
Mallikarjunaiah 2015.
| Methods | Not yet assessed |
| Participants | Not yet assessed |
| Interventions | Not yet assessed |
| Outcomes | Not yet assessed |
| Notes | The findings from this trial are currently only available as a conference abstract |
NCT01944150.
| Methods | Not yet assessed |
| Participants | Not yet assessed |
| Interventions | Not yet assessed |
| Outcomes | Not yet assessed |
| Notes | Originally identified in a trial registry and included as a trial in the 'Classification of ongoing studies' table in the original review (Smart 2016). As of 30 July 2020 we were unable to make contact (email delivery failure) with the author for an update of this trial's progress. We note that this trial was registered in 2013 and now assume it is unlikely ever to be published. |
Patru 2017.
| Methods | Not yet assessed |
| Participants | Not yet assessed |
| Interventions | Not yet assessed |
| Outcomes | Not yet assessed |
| Notes | The findings from this trial are currently only available as a conference abstract |
UKCRN ID 12602.
| Methods | Parallel‐group, 2‐arm RCT (UK) |
| Participants |
Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Experimental group: ESDT and de‐sensitisation tasks Active comparator group: routine care, including de‐sensitisation tasks |
| Outcomes |
|
| Notes | As of 30 July 2020, the author updated us via email that this trial is delayed |
CRPS: complex regional pain syndrome; ESDT: electrical sensory discrimination therapies; RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
ChiCTR1900020835.
| Study name | Manual lymphatic drainage combined with transcranial magnetic stimulation for post‐stroke type I complex regional pain syndrome: an exploratory clinical study |
| Methods | Parallel‐group, 2‐arm RCT (China) |
| Participants |
Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Experimental group: routine rehabilitation and MLD and rTMS Active comparator group: routine rehabilitation |
| Outcomes |
Primary outcome measures:
|
| Starting date | January 2019 |
| Contact information | Dr Bai Yulong, dr_baiyl@fudan.cn; Qiu Xiao, qiuxiaoabc@126.com |
| Notes | As of 17 August 2020 we were unable to make contact with the author for an update of this trial's progress |
CTRI/2019/01/017272.
| Study name | Efficacy of an integrated approach encompassing pregabalin and mirror therapy in management of complex regional pain syndrome type 1‐a pilot study |
| Methods | Parallel‐group, 2‐arm RCT (India) |
| Participants |
Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Experimental group: cap pregabalin 75 mg BD (twice per day), scrub descrub therapy and mirror therapy Active comparator group: cap pregabalin 75 mg BD and scrub descrub therapy |
| Outcomes |
Primary outcome measures:
Secondary outcome measures:
|
| Starting date | January 2019 |
| Contact information | Anish Malik, anishmalik14@yahoo.com |
| Notes | As of 17 August 2020 we were unable to make contact with the author for an update of this trial's progress |
JPRN‐UMIN000029801.
| Study name | The effectiveness of graded mirror therapy based on the assessment of mirrored limb perception to the patients with complex regional pain syndrome |
| Methods | Parallel‐group, 2‐arm RCT (Japan) |
| Participants |
Inclusion criteria: (not specified) Exclusion criteria:
|
| Interventions |
Experimental group: graded mirror therapy Active comparator group: conventional mirror therapy |
| Outcomes |
Primary outcome measures:
Secondary outcome measures: (not specified) |
| Starting date | June 2019 |
| Contact information | Akira Mibu, a_mibu@konan‐wu.ac.jp |
| Notes | As of 18 August 2020 the author updated us via email that this trial is ongoing and delayed secondary to the spread of COVID‐19 infection |
NCT02395211.
| Study name | Effects of proprioceptive stimulation under visual feedback in patient with CRPS: an exploratory study |
| Methods | Parallel‐group, 2‐arm RCT (Italy) |
| Participants |
Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Experimental group: Gloreha device Active comparator group: usual physiotherapy |
| Outcomes |
Primary outcome measures:
Secondary outcome measures:
|
| Starting date | January 2015 |
| Contact information | Dr Sofia Straudi, sofia.straudi@gmail.com |
| Notes | As of 30 July 2020 the author updated us via email that this trial is ongoing |
NCT02753335.
| Study name | A randomized trial of patients with complex regional pain syndrome comparing graded motor imagery and desensitization versus simple desensitization and changes in resting‐state connectivity of cerebral networks before and after treatment |
| Methods | Randomised cross‐over design |
| Participants |
Inclusion criteria:
Exclusion criteria:
For patients who participate in the MRI related analyses:
|
| Interventions |
Experimental group: graded motor imagery and desensitisation Active comparator group: desensitisation |
| Outcomes |
Primary outcome measures:
Secondary outcome measures:
|
| Starting date | April 2016 |
| Contact information | Lena Danielsson, lena.danielsson@unn.no |
| Notes | As of 24 August 2020, the author updated us via email that this trial is ongoing |
NCT03377504.
| Study name | Clinical evaluation of the effects of mirror therapy in patients with complex regional pain syndrome (CRPS) type 1: prospective randomized single blind controlled study |
| Methods | Parallel‐group, 2‐arm RCT (Turkey) |
| Participants |
Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Experimental group: mirror therapy and routine physical therapy Active comparator group: routine physical therapy |
| Outcomes |
Primary outcome measures:
Secondary outcome measures:
|
| Starting date | March 2017 |
| Contact information | Dr Ayşe Adile Küçükdeveci, ayse.kucukdeveci@gmail.com. Ankara University. Faculty of Medicine, İbn‐i Sina Research and Application Hospital, Ankara, Turkey, 06030). |
| Notes | As of 6 August 2020, the author updated us via email that this trial is completed and being analysed |
NCT03887962.
| Study name | Trial of virtual reality biofeedback in patients with motor neglect from chronic pain or cerebrovascular disease |
| Methods | Parallel‐group, 2‐arm RCT (UK) |
| Participants |
inclusion criteria:
Exclusion criteria:
|
| Interventions |
Experimental group: virtual environment feedback Active comparator group: control intervention |
| Outcomes |
Primary outcome measures:
Secondary outcome measures:
|
| Starting date | May 2017 |
| Contact information | Dr Nicholas Shenker |
| Notes | As of 30 July 2020 the author updated us via email that this trial is completed and being analysed |
Abbreviations: ESDT: electrical sensory discrimination therapies; PGIC: patient global impression of change; RCT: randomised controlled trial; RSS: repetitive electrical sensory discrimination; TENS: transcutaneous electrical nerve stimulation; UK: United Kingdom; VAS: visual analogue scale.
Differences between protocol and review
2016 Review
We did not search the reference lists of key physiotherapy textbooks. With respect to Types of interventions, after the publication of Smart 2013 we decided to exclude studies that evaluated non‐physiotherapy based interventions (e.g. pharmacological) in which all study arms received the same physiotherapy intervention (differing only in the application of the non‐physiotherapy component) as they are unlikely to offer any insight into the value of physiotherapy management. In Smart 2013 we stated our intention to search the SciVerse SCOPUS electronic database. However, we did not search this database as the primary review author (KMS) did not have institutional access. The Information Specialist of the Cochrane PaPaS group advised that its omission was unlikely to adversely influence our search results. We have described, in additional detail, our operational definitions upon which we based our risk of bias judgements (see the Assessment of risk of bias in included studies section). In the original Cochrane Review we specified the criteria upon which we based our GRADE judgements for rating the quality of evidence (see the Data synthesis section).
2021 Update
In a change to our original protocol (Smart 2013) and systematic review (Smart 2016) we extended our interpretation of changes in outcomes to include between‐group differences based on the recommendations of the OMERACT 12 group, as detailed in the Primary outcomes section. In a further change we also excluded studies that did not measure any of the primary or secondary outcomes of interest. Our GRADE judgements now rate the 'certainty' rather then the 'quality' of evidence (see 'Summary of findings and assessment of the certainty of the evidence' section). We have explained and justified our presentation of a limited number of summary of findings tables in the summary of findings table section.
Contributions of authors
KMS conceived and designed the protocol, implemented the search strategy, applied eligibility criteria, assessed studies, extracted and analysed data, and led the write‐up of the review.
MCF applied eligibility criteria, assessed studies, extracted and analysed data, and assisted with the write‐up of the updated review.
BMW informed the protocol design, applied eligibility criteria, assessed studies, extracted and analysed data (in the original review), and assisted with the write‐up of the review.
NOC informed the protocol design, acted as the third review author, oversaw data synthesis and assisted with the write‐up of the review.
KMS will be responsible for updating this Cochrane Review.
Sources of support
Internal sources
No sources of support provided
External sources
-
National Institute for Health Research (NIHR), UK
Cochrane Infrastructure funding to the Cochrane Pain, Palliative and Supportive Care Review Group (PaPaS)
Declarations of interest
KMS: none known. KMS maintains a small clinical caseload as a clinical specialist physiotherapist and manages patients with CRPS.
MCF: none known.
BMW: none known.
NOC: none known. NOC is an author as well as PaPaS Co‐ordinating Editor but had no input into the editorial decisions or processes for this review.
KMS, BMW and NOC are qualified physiotherapists, and MCF is a health scientist, although none currently practice in private health care or for a 'for profit' organisation.
Since NOC is an author and PaPaS Co‐ordinating Editor, we acknowledge the input of Christopher Eccleston, who acted as Sign‐off Editor for this review. NOC had no input into the editorial decisions or processes for this review.
Edited (no change to conclusions)
References
References to studies included in this review
Askin 2014 {published data only}
- Askin A, Savas S, Koyuncuoglu HR, Baloglu HH, Inci MF. Low dose high frequency ultrasound therapy for stellate ganglion blockade in complex regional pain syndrome type I: a randomised placebo controlled trial. International Journal of Clinical and Experimental Medicine 2014;7(12):5603-11. [PMC free article] [PubMed] [Google Scholar]
Aydemir 2006 {published data only}
- Aydemir K, Taşkaynatan MA, Yaziicioğlu K, Özgül A. The effects of stellate ganglion block with lidocaine and ultrasound in complex regional pain syndrome: a randomized, double blind, placebo controlled study [Kompleks bölgesel ağri sendromunda Lydokane ultrason ile yapilan stellat ganglyon blokajinin etkinliği: çift kör randomize plasebo kontrollü çalişma]. Journal of Rheumatology and Medical Rehabilitation 2006;17(3):193-200. [Google Scholar]
Barnhoorn 2015 {published data only}
- Barnhoorn K, Staal JB, Dongen RT, Frölke JPM, Klomp FP, de Meent H, et al. Pain exposure physical therapy versus conventional treatment in complex regional pain syndrome type 1—a cost-effectiveness analysis alongside a randomized controlled trial. Clinical Rehabilitation 2018;32(6):790-8. [DOI: 10.1177/0269215518757050] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnhoorn KJ, Oostendorp RAB, Dongen RTM, Klomp FP, Samwel H, Wilt GJ, et al. The effectiveness and cost evaluation of pain exposure physical therapy and conventional therapy in patients with complex regional pain syndrome type 1. Rationale and design of a randomized controlled trial. BMC Musculoskeletal Disorders 2012;13:58. [DOI: 10.1186/1471-2474-13-58] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnhoorn KJ, Staal JB, Dongen RTM, Frölke JPM, Klomp FP, de Meent H, et al. Are pain-related fears mediators for reducing disability and pain in patients with complex regional pain syndrome type 1? An explorative analysis on pain exposure physical therapy. PLOS One 2015;10(4):e0123008. [DOI: 10.1371/journal.pone.0123008] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnhoorn KJ, de Meent H, Dongen RTM, Klomp FP, Groenewoud H, Samwel H, et al. Pain exposure physical therapy (PEPT) compared to conventional treatment in complex regional pain syndrome type 1: a randomised controlled trial. BMJ Open 2015;5:e008283. [DOI] [PMC free article] [PubMed] [Google Scholar]
Benedetti 2018 {published data only}
- Benedetti MG, Cavazzuti L, Mosca M, Fusaro I, Zati A. Bio-electro-magnetic-energy-regulation (BEMER) for the treatment of type I complex regional pain syndrome: a pilot study. Physiotherapy Theory and Practice 2018;36(4):498-506. [DOI] [PubMed] [Google Scholar]
Bilgili 2016 {published data only}
- Bilgili A, Çakır T, Dogan SK, Erçalık T, Filiz MB, Toraman F. The effectiveness of transcutaneous electrical nerve stimulation in the management of patients with complex regional pain syndrome: a randomized, double-blinded, placebo-controlled prospective study. Journal of Back and Musculoskeletal Rehabilitation 2016;29:661-71. [DOI] [PubMed] [Google Scholar]
Bϋyϋkturan 2018 {published data only}
- Bϋyϋkturan O, Bϋyϋkturan B, Kurt EE. Effectiveness of electromagnetic field therapy in upper extremity complex regional pain syndrome type I: a randomized controlled study. Journal of Exercise Therapy and Rehabilitation 2018;5(1):9-18. [Google Scholar]
Cacchio 2009a {published data only}
- Cacchio A, De Blasis E, De Blasis V, Santilli V, Spacca G. Mirror therapy in complex regional pain syndrome type 1 of the upper limb in stroke patients. Neurorehabilitation and Neural Repair 2009;23(8):792-9. [DOI] [PubMed] [Google Scholar]
Cacchio 2009b {published data only}
- Cacchio A, De Blasis E, Necozione S, di Orio F, Santilli V. Mirror therapy for chronic complex regional pain syndrome type 1 and stroke. New England Journal of Medicine 2009;361(6):634-6. [DOI] [PubMed] [Google Scholar]
den Hollander 2016 {published data only}
- den Hollander M, Goossens M, Jong J, Ruijgrok J, Oosterhof J, Onghena P, et al. Expose or protect? A randomized controlled trial of exposure in vivo vs pain-contingent treatment as usual in patients with complex regional pain syndrome type 1. Pain 2016;157(10):2318-29. [DOI] [PubMed] [Google Scholar]
- den Hollander M, Heijnders N, Jong JR, Vlaeyen JWS, Smeets RJEM, Goossens MEJB. Exposure in vivo versus pain-contingent physical therapy in complex regional pain syndrome type I: a cost-effectiveness analysis. International Journal of Technology Assessment in Health Care 2018;34(4):400-9. [DOI: 10.1017/S0266462318000429] [DOI] [PubMed] [Google Scholar]
Devrimsel 2015 {published data only}
- Devrimsel G, Turkyilmaz AK, Yildirim M, Beyazal MS. The effects of whirlpool bath and neuromuscular electrical stimulation on complex regional pain syndrome. Journal of Physical Therapy Science 2015;27:27-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dimitrijevic 2014 {published data only}
- Dimitrijevic IM, Lazovic MP, Kocic MN, Dimitrijevic LR, Mancic DD, Stankovic AM. Effects of low-level laser therapy and interferential current therapy in the treatment of complex regional pain syndrome. Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi [Turkish Journal of Physical Medicine and Rehabilitation] 2014;60(2):98-105. [Google Scholar]
Duman 2009 {published data only}
- Duman I, Ozdemir A, Kenan Tan A, Dincer K. The efficacy of manual lymphatic drainage therapy in the management of limb edema secondary to reflex sympathetic dystrophy. Rheumatology International 2009;29(7):759-63. [DOI] [PubMed] [Google Scholar]
Durmus 2004 {published data only}
- Durmus A, Cakmak A, Disci R, Muslumanoglu L. The efficiency of electromagnetic field treatment in complex regional pain syndrome type 1. Disability and Rehabilitation 2004;26(9):537-45. [DOI] [PubMed] [Google Scholar]
Halicka 2021 {published data only}
- Halicka M, Vittersø AD, McCullough H, Goebel A, Heelas L, Proulx MJ, et al. Prism adaptation treatment for upper-limb complex regional pain syndrome: a double-blind randomized controlled trial. Pain 2021;62(2):471-89. [DOI: 10.1097/j.pain.0000000000002053] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hazneci 2005 {published data only}
- Hazneci B, Tan AK, Özdem T, Dinçer K, Kalyon TA. The effects of transcutaneous electroneurostimulation and ultrasound in the treatment of reflex sympathetic dystrophy syndrome [Refleks sempatik distrofi sendromu tedavisinde transkutanöz elektronörostimülasyon ve ultrasonun etkileri]. Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi [Turkish Journal of Physical Medicine and Rehabilitation] 2005;51(3):83-9. [Google Scholar]
Hwang 2014 {published data only}
- Hwang H, Cho S, Lee J-H. The effect of virtual body swapping with mental rehearsal on pain intensity and body perception disturbance in complex regional pain syndrome. International Journal of Rehabilitation Research 2014;37:167-72. [DOI] [PubMed] [Google Scholar]
Jeon 2014 {published data only}
- Jeon B, Cho S, Lee J-H. Application of virtual body swapping to patients with complex regional pain syndrome: a pilot study. Cyberpsychology, Behavior and Social Networking 2014;17(6):366-70. [DOI] [PubMed] [Google Scholar]
Lewis 2021 {published and unpublished data}
Li 2012 {published data only}
- Li N, Tian F, Wang C, Yu P, Zhou X, Wen Q, et al. Therapeutic effect of acupuncture and massage for shoulder hand syndrome in hemiplegia patients: a clinical two-centre randomized controlled trial. Journal of Traditional Chinese Medicine 2012;32(3):343-9. [DOI] [PubMed] [Google Scholar]
Moseley 2004 {published data only}
- Moseley GL. Graded motor imagery is effective for long-standing complex regional pain syndrome: a randomised controlled trial. Pain 2004;108(1-2):192-8. [DOI] [PubMed] [Google Scholar]
Moseley 2005 {published data only}
- Moseley GL. Is successful rehabilitation of complex regional pain syndrome due to sustained attention to the affected limb? A randomised clinical trial. Pain 2005;114(1-2):54-61. [DOI] [PubMed] [Google Scholar]
Moseley 2006 {published data only}
- Moseley GL. Graded motor imager for pathologic pain: a randomised controlled trial. Neurology 2006;67(12):2129-34. [DOI] [PubMed] [Google Scholar]
Moseley 2009 {published data only}
- Moseley GL, Wiech K. The effect of tactile discrimination training is enhanced when patients watch the reflected image of their unaffected limb during training. Pain 2009;144(3):314-9. [DOI] [PubMed] [Google Scholar]
Mucha 1992 {published data only}
- Mucha C. Effects of CO2-baths in the combined concept of the early functional therapy in cases of algodystrophy [Einflub von CO 2 -Badern im fruhfunktionellen Therapiekonzept der Algodystrophie]. Physikalische Medizin und Kur Medizin 1992;2:173-8. [Google Scholar]
Oerlemans 1999 {published data only}
- Oerlemans HM, Goris RJA, Boo T, Oostendorp RAB. Do physical therapy and occupational therapy reduce the impairment percentage in reflex sympathetic dystrophy? American Journal of Physical Medicine and Rehabilitation 1999;78(6):533-9. [DOI] [PubMed] [Google Scholar]
- Oerlemans HM, Oostendorp RAB, Boo T, Goris RJA. Pain and reduced mobility in complex regional pain syndrome I: outcome of a prospective randomised controlled trial of adjuvant physical therapy versus occupational therapy. Pain 1999;83(1):77-83. [DOI] [PubMed] [Google Scholar]
- Oerlemans HM, Oostendorp RAB, Boo T, Laan L, Severens JL, Goris RJA. Adjuvant physical therapy versus occupational therapy in patients with reflex sympathetic dystrophy/complex regional pain syndrome type I. Archives of Physical Medicine and Rehabilitation 2000;81(1):49-56. [PubMed] [Google Scholar]
- Severens JL, Oerlemans HM, Weegels JPG, 't Hof MA, Oostendorp RAB, Goris RJA. Cost-effectiveness analysis of adjuvant physical therapy or occupational therapy for patients with reflex sympathetic dystrophy. Archives of Physical Medicine and Rehabilitation 1999;80(9):1038-43. [DOI] [PubMed] [Google Scholar]
Ozcan 2019 {published data only}
- Ozcan DS, Tatli HU, Polat CS, Oken O, Koseoglu BF. The effectiveness of fluidotherapy in poststroke complex regional pain syndrome: a randomized controlled study. Journal of Stroke and Cerebrovascular Diseases 2019;28(6):1578-85. [DOI] [PubMed] [Google Scholar]
Ryan 2017 {published data only}
- Ryan CG, King R, Robinson V, Punt TD, Dinse HR, Grunenberg C, et al. Transcutaneous electrical nerve stimulation using an LTP-like repetitive stimulation protocol for patients with upper limb complex regional pain syndrome: a feasibility study. Hand Therapy 2017;22(2):52-63. [Google Scholar]
Saha 2021 {published data only}
- Saha S, Sur M, Chaudhuri GR, Agarwal S. Effects of mirror therapy on oedema, pain and functional activities in patients with poststroke shoulder-hand syndrome: a randomized controlled trial. Physiotherapy Research International 2021;26(3):e1902. [DOI] [PubMed] [Google Scholar]
Sarkar 2017 {published data only}
- Sarkar B, Goswami S, Mukherjee D, Basu S. Efficacy of motor imagery through mirror visual feedback therapy in complex regional pain syndrome: a comparative study. Indian Journal of Pain 2017;31:164-9. [Google Scholar]
Schreuders 2014 {unpublished data only}
- Schreuders TAR, Tichelaar R, Huygen FJPM, Hitters MWMGC, Stam HJ, Selles RW. Effects of a graded motor imagery program in patients with longstanding complex regional pain syndrome I (as supplied 29 May 2014). Data on file.
Strauss 2021 {published data only}
- Strauss S, Barby S, Härtner, Neumann N, Moseley GL, Lotze M. Modifications in fMRI representation of mental rotation following a 6 week graded motor imagery training in chronic CRPS patients. Journal of Pain 2021;22(6):680-91. [DOI] [PubMed] [Google Scholar]
Topcuoglu 2015 {published data only}
- Topcuoglu A, Gokkaya NKO, Ucan H, Karakuş D. The effect of upper-extremity aerobic exercise on complex regional pain syndrome type I: a randomized controlled study on subacute stroke. Topics in Stroke Rehabilitation 2015;22(4):253-61. [DOI] [PubMed] [Google Scholar]
Uher 2000 {published data only}
- Uher EM, Vacariu G, Schneider B, Fialka V. Comparison of manual lymph drainage with physical therapy in the complex regional pain syndrome I. A comparative randomised controlled therapy study [Manuelle Lymphdrainage im Vergleich zur Physiotherapie bei Complex Regional Pain Syndrom Typ I. Randomisierte kontrollierte Therapievergleichsstudie]. Wiener Klinische Wochenschrift 2000;112(3):133-7. [PubMed] [Google Scholar]
Vural 2016 {published data only}
- Vural SP, Yuzer GFN, Ozcan DS, Ozbudak SD, Ozgirgin N. Effects of mirror therapy in stroke patients with complex regional pain syndrome type 1: a randomized controlled study. Archives of Physical Medicine and Rehabilitation 2016;97(4):575-81. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bolel 2006 {published data only}
- Bolel K, Hizmetli S, Akyüz A. Sympathetic skin responses in reflex sympathetic dystrophy. Rheumatology International 2006;26(9):788-91. [DOI] [PubMed] [Google Scholar]
David 2015 {published data only}
- David M, Dinse HR, Mainka T, Tegenthoff M, Maier C. High-frequency repetitive sensory stimulation as intervention to improve sensory loss in patients with complex regional pain syndrome I. Frontiers in Neurology 2015;6:242. [DOI: 10.3389/fneur.2015.00242] [DOI] [PMC free article] [PubMed] [Google Scholar]
den Hollander 2020 {published data only}
- den Hollander M, Jong J, Onghena P, Vlaeyen JWS. Generalization of exposure in vivo in complex regional pain syndrome type I. Behaviour Research and Therapy 2020;124:103511. [DOI] [PubMed] [Google Scholar]
Dimitrijevic 2018 {published data only}
- Dimitrijevic I, Kocic M, Lazovic M, Mancic D, Filipov R. Evaluation of interferential currents in the treatment of complex regional pain syndrome after distal radius fracture. Osteoporosis International 2018;29(Suppl 1):S149-565 (P958). [Google Scholar]
Fialka 1992 {published data only}
- Fialka VV, Wickenhauser J, Engel A, Schneider B. Sympathetic reflex dystrophy. Effectiveness of physical therapy treatment of Sudek's syndrome [Sympathische Reflexdystrophie. Wirksamkeit physiotherapeutischer Behandlungsmaßnahmen des Sudeksyndrom]. Fortschritte der Medzin 1992;110(9):146-8. [PubMed] [Google Scholar]
Fialka 1996 {published data only}
- Fialka V, Korpan M, Saradeth T, Paternostro-Slugo T, Hexel O, Frischenschlager O, et al. Autogenic training for reflex sympathetic dystrophy: a pilot study. Complementary Therapies in Medicine 1996;4(2):103-5. [Google Scholar]
Field 1993 {published data only}
- Field J, Atkins RM. Effect of guanethidine on the natural history of post-traumatic algodystrophy. Annals of the Rheumatic Diseases 1993;52(6):467-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gromo 1974 {published data only}
- Gromo G, Ceroni P, Sosso A. Iontophoresis with a diffuser enzyme (Thiomucase) associated with diadynamic currents in the physiokinetictherapy management of post-traumatic algodystrophic edematous syndromes of the limbs [La ionoforesi con enzima diffusore (Thiomucase) associata alle correnti diadinamiche nel trattamento fisiokinesiterapico delle sindromi edematose algodistrofiche post-traumatiche degli arti]. Minerva Medica 1974;65(77):4015-25. [PubMed] [Google Scholar]
Jasmina 2012 {published data only}
- Jasmina T, Genchev G, Savova A, Dantchev N, Petrova G. Cost-effectiveness and activities of daily living in patients with complex regional pain syndrome type I. International Journal of Pharmaceutical Sciences Review and Research 2012;17(1):16-21. [Google Scholar]
JPRN‐UMIN000027348 {unpublished data only}
- JPRN-UMIN000027348. Understanding changes of body-specific attention and spatial attention in patients with complex regional pain syndrome. http://www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000027348.
Karabegović 2009 {published data only}
- Karabegović A, Kapidžić-Duraković S, Ljuca F. Laser therapy of painful shoulder and shoulder-hand syndrome in treatment of patients after the stroke. Bosnian Journal of Basic Medical Sciences 2009;9(1):59-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kocić 2010 {published data only}
- Kocić M, Lazović M, Dimitrijević I, Mančić D, Stanković A. Evaluation of low level laser and interferential current in the therapy of complex regional pain syndrome by infrared thermographic camera [Procena terapijskog efekta lasera male snage i interferenthih struja kod bolesnika sa kompleksnim regionalnim bolnim sindromom primenom infracrvene termovizijske kamere]. Vojnosanitetski Pregled 2010;67(9):755-60. [DOI] [PubMed] [Google Scholar]
Kotiuk 2019 {published data only}
- Kotiuk V, Burianov O, Kostrub O, Khimion L, Zasadnyuk I. The impact of mirror therapy on body schema perception in patients with complex regional pain syndrome after distal radius fractures. British Journal of Pain 2019;13(1):35-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liao 2006 {published data only}
- Liao HW. Clinical observations on the efficacy of occupational therapy plus acupuncture for treating reflex sympathetic dystrophy [作业疗法合针灸治疗肩手综合征45例疗效观察]. Shanghai Journal of Acupuncture and Moxibustion (上海针灸杂志) 2006;3:9-10. [Google Scholar]
Marianne 2015 {published data only}
- Marianne D, Dinse HR, Mainka T, Tegenthoff M, Maier C. High-frequency repetitive sensory stimulation as intervention to improve sensory loss in patients with complex regional pain syndrome I. Frontiers in Neurology 2015;6:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02667717 {unpublished data only}
- NCT02667717. Efficacy and safety of a learning program of self-rehabilitation exercises by mirror therapy in the complex regional pain syndrome of the upper limb: a multicentric randomized open study. https://clinicaltrials.gov/ct2/show/NCT02667717 (first received 29 January 2016).
Perrigot 1982 {published data only}
- Perrigot M, Bergego C, Hocini A, Pierrot-Deseilligny E. Algodystrophic syndrome in hemiplegia. Clinical and therapeutic study [Le syndrome algodystrophique chez l'hémiplégique. Étude clinique et thérapeutique]. Annales de Médecine Interne 1982;133(8):544-8. [PubMed] [Google Scholar]
Solcà 2018 {published data only}
- Solcà M, Ronchi R, Bello-Ruiz J, Schmidlin T, Herbelin B, Luthi F, et al. Heartbeat-enhanced immersive virtual reality to treat complex regional pain syndrome. Neurology 2018;91(5):e479-89. [DOI] [PubMed] [Google Scholar]
Toth 2014 {published data only}
- Toth C, Brady S, Gagnon F, Wigglesworth K. A randomized, single-blind, controlled, parallel assignment study of exercise versus education as adjuvant in the treatment of peripheral neuropathic pain. Clinical Journal of Pain 2014;30(2):111-8. [DOI] [PubMed] [Google Scholar]
Tulgar 1991 {published data only}
- Tulgar M, McGlone F, Bowsher D, Miles JB. Comparative effectiveness of different stimulation modes in relieving pain. Part I. A pilot study. Pain 1991;47(2):151-5. [DOI] [PubMed] [Google Scholar]
Wu 1999 {published data only}
- Wu W, Bandilla E, Ciccone DS, Yang J, Cheng SC, Carner N, et al. Effects of Qigong on late-stage complex regional pain syndrome. Alternative Therapies in Health and Medicine 1999;5(1):45-54. [PubMed] [Google Scholar]
Zyluk 1994 {published data only}
- Zyluk A. Clinical estimation of late treatment results in posttraumatic Sudeck's dystrophy treated with mannitol, calcitonin and exercise therapy [Kliniczna ocena odległych wynikow leczenia pourazowej dystrofii sudecka za pomocą mannitolu, kalcytoniny I terapii ruchowej]. Annales Academiae Medicae Stetinensis 1994;40:133-44. [PubMed] [Google Scholar]
References to studies awaiting assessment
Dimitrijevic 2019 {unpublished data only}
- Dimitrijevic I, Kocic M, Lazovic M, Mancic D, Filipov R. Evaluation of low level laser therapy in the treatment of complex regional pain syndrome after ankle fracture. Osteoporosis International 2019;30(Suppl 2):S253-773 (P933). [Google Scholar]
Dimitrijevic 2020 {published data only}
- Dimitrijevic I, Kocic M, Lazovic M, Mancic D, Filipov R. Evaluation of the therapeutic effect of physical agents in complex regional pain syndrome by infrared thermography. Osteoporosis International 2020;31(Suppl 1):S133-621. [Google Scholar]
ISRCTN39729827 {published data only}39729827
- ISRCTN39729827. Investigation of the effectiveness of biofeedback therapy on complex regional pain syndrome (CRPS) of the upper limb. http://www.isrctn.com/ISRCTN39729827 (first received 25 October 2007).
ISRCTN97144266 {unpublished data only}ISRCTN97144266
- ISRCTN97144266. Treatment of complex regional pain syndrome (CPRS) type I with mirror therapy. http://www.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN97144266.
Mallikarjunaiah 2015 {published data only}
- Mallikarjunaiah HS. Efficacy of iontophoresis on shoulder pain and its function in stroke survivors having type II complex regional pain syndrome. Physiotherapy 2015;101(Suppl 1):eS833–1237 (eS943). [Google Scholar]
NCT01944150 {unpublished data only}
- NCT01944150. Interest of the association of two complementary techniques, hypnosis and transcutaneous electrical nerve stimulation in the treatment of chronic non-cancer pain, nociceptive and/or neuropathic pain: randomized trial. https://clinicaltrials.gov/ct2/show/NCT01944150 (first received 17 September 2013).
Patru 2017 {unpublished data only}
- Patru S, Marcu IR, Matei D, Bumbea AM, Bighea AC. Mirror visual feedback therapy improves clinical outcomes and the activity of daily living to patients with hand complex regional pain syndrome. Annals of the Rheumatic Diseases 2017;76(Suppl 2):478. [Google Scholar]
UKCRN ID 12602 {published data only}
- UKCRN ID 12602. Development of an electrical sensory discrimination therapies device (ESDT) for the relief of chronic pain in complex regional pain syndrome. A proof of concept study. Identified in our previous review (Smart 2016); database no longer functional. Accessed 8 February 2014.
References to ongoing studies
ChiCTR1900020835 {unpublished data only}
- ChiCTR1900020835. Manual lymphatic drainage combined with transcranial magnetic stimulation for post-stroke type I complex regional pain syndrome: an exploratory clinical study. http://www.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR1900020835.
CTRI/2019/01/017272 {unpublished data only}
- CTRI/2019/01/017272. Efficacy of an integrated approach encompassing pregabalin and mirror therapy in management of complex regional pain syndrome type 1-a pilot study. http://www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2019/01/017272.
JPRN‐UMIN000029801 {unpublished data only}
- JPRN-UMIN000029801. The effectiveness of graded mirror therapy based on the assessment of mirrored limb perception to the patients with complex regional pain syndrome. http://www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000029801.
NCT02395211 {unpublished data only}
- NCT02395211. Effects of proprioceptive stimulation under visual feedback in patient with CRPS: an exploratory study. https://clinicaltrials.gov/ct2/show/NCT02395211 (first received 23 March 2015).
NCT02753335 {unpublished data only}
- NCT02753335. A randomized trial of patients with complex regional pain syndrome comparing graded motor imagery and desensitization versus simple desensitization and changes in resting-state connectivity of cerebral networks before and after treatment. https://clinicaltrials.gov/ct2/show/NCT02753335 (first received 27 April 2016).
NCT03377504 {unpublished data only}
- NCT03377504. Clinical evaluation of the effects of mirror therapy in patients with complex regional pain syndrome (CRPS) type 1: prospective randomized single blind controlled study. https://clinicaltrials.gov/ct2/show/NCT03377504 (first received 19 December 2017).
NCT03887962 {unpublished data only}
- NCT03887962. Trial of virtual reality biofeedback in patients with motor neglect from chronic pain or cerebrovascular disease. https://clinicaltrials.gov/ct2/show/NCT03887962 (first received 25 March 2019).
Additional references
Anderson 2002
- Anderson DM. Mosby's Medical, Nursing & Allied Health Dictionary. 6th edition. St. Louis: Mosby, 2002. [Google Scholar]
Atamaz 2012
- Atamaz FC, Durmaz B, Baydar M, Demircioglu OY, Iyiyapici A, Kuran B, et al. Comparison of the efficacy of transcutaneous electrical nerve stimulation, interferential currents, and shortwave diathermy in knee osteoarthritis: a double-blind, randomized, controlled, multicenter study. Archives of Physical Medicine and Rehabilitation 2012;93(5):748-56. [DOI] [PubMed] [Google Scholar]
Atkins 2010
- Atkins RM. Principles of complex regional pain syndrome. In: Buscholz RW, Heckman JD, Court-Brown CM, Tornetta P, editors(s). Rockwood and Green's Fractures in Adults. 7th edition. Vol. 1. Philadelphia: Lippincott Williams & Wilkins, 2010:602-14. [Google Scholar]
Bafeta 2012
- Bafeta A, Dechartres A, Trinquart L, Yavchitz A, Boutron I, Ravaud P. Impact of single centre status on estimates of intervention effects in trials with continuous outcomes: meta-epidemiological study. BMJ 2012;344:e813. [DOI: 10.1136/bmj.e813] [DOI] [PMC free article] [PubMed] [Google Scholar]
Balshem 2011
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401-6. [DOI] [PubMed] [Google Scholar]
Bean 2015
- Bean DJ, Johnson MH, Heiss-Dunlop W, Lee AC, Kydd RR. Do psychological factors influence recovery from complex regional pain syndrome type 1? A prospective study. Pain 2015;156:2310-8. [DOI] [PubMed] [Google Scholar]
Beerthuizen 2009
- Beerthuizen A, 't Spijker A, Huygen FJPM, Klein J, Wit R. Is there an association between psychological factors and the complex regional pain syndrome type 1 (CRPS1) in adults? A systematic review. Pain 2009;145(1-2):52-9. [DOI] [PubMed] [Google Scholar]
Beerthuizen 2012
- Beerthuizen A, Stronks DL, Van't Spijker A, Yaksh A, Hanraets BM, Klein J, et al. Demographic and medical parameters in the development of complex regional pain syndrome type 1 (CRPS1): prospective study on 596 patients with a fracture. Pain 2012;153(6):1187-92. [DOI] [PubMed] [Google Scholar]
Bialosky 2018
- Bialosky JE, Beneciuk JM, Bishop MD, Coronado RA, Penza CW, Simon CB, et al. Unraveling the mechanisms of manual therapy: modeling an approach. Journal of Orthopaedic & Sports Physical Therapy 2018;48(1):8-20. [DOI] [PubMed] [Google Scholar]
Birklein 2017
- Birklein F, Dimova V. Complex regional pain syndrome – up-to-date. Pain Reports 2017;2(6):e624. [DOI: 10.1097/PR9.0000000000000624] [DOI] [PMC free article] [PubMed] [Google Scholar]
Borchers 2014
- Borchers AT, Gershwin ME. Complex regional pain syndrome: a comprehensive and critical review. Autoimmunity Reviews 2014;13:242-65. [DOI] [PubMed] [Google Scholar]
Bowering 2013
- Bowering KJ, O'Connell NE, Tabor A, Catley MJ, Leake HB, Moseley GL, et al. The effects of graded motor imagery and its components on chronic pain: a systematic review and meta-analysis. Journal of Pain 2013;14(1):3-13. [DOI] [PubMed] [Google Scholar]
Bruehl 1999
- Bruehl S, Harden RN, Galer BS, Saltz S, Bertram M, Backonja M, et al. External validation of IASP diagnostic criteria for complex regional pain syndrome and proposed research diagnostic criteria. International Association for the Study of Pain. Pain 1999;81(1-2):147-54. [DOI] [PubMed] [Google Scholar]
Bruehl 2010
- Bruehl S. An update on the pathophysiology of complex regional pain syndrome. Anesthesiology 2010;113(3):713-25. [DOI] [PubMed] [Google Scholar]
Bruehl 2015
- Bruehl S. Complex regional pain syndrome. BMJ 2015;350:h2730. [DOI: 10.1136/bmj.h.2730] [DOI] [PubMed] [Google Scholar]
Brunner 2010
- Brunner F, Gymesi A, Kissling R, Bachmann LM. Patients' disease-related knowledge of complex regional pain syndrome: a pilot study. Journal of Rehabilitation Medicine 2010;42:458-62. [DOI] [PubMed] [Google Scholar]
Busse 2015
Button 2013
- Button KS, Ioanidis JPA, Mokrysz C, Nosek BA, Flint J, Robinson ESJ, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nature Reviews Neuroscience 2013;14(5):365-76. [DOI] [PubMed] [Google Scholar]
Chan 2013
- Chan A-W, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 Statement: Defining standard protocol items for clinical trials. Annals of Internal Medicine 2013;158(3):200-7. [DOI: DOI: 10.7326/0003-4819-158-3-201302050-00583] [DOI] [PMC free article] [PubMed] [Google Scholar]
Coderre 2011
- Coderre TJ. Complex regional pain syndrome: what's in a name? Journal of Pain 2011;12(1):2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cossins 2013
- Cossins L, Okell RW, Cameron H, Simpson B, Poole HM, Goebel A. Treatment of complex regional pain in adults: a systematic review of randomized controlled trials published from June 2000 to February 2012. European Journal of Pain 2013;17(2):158-73. [DOI] [PubMed] [Google Scholar]
Daly 2009
- Daly AE, Bialocerkowski AE. Does evidence support physiotherapy management of adult complex regional pain syndrome type one? A systematic review. European Journal of Pain 2009;13(4):339-53. [DOI] [PubMed] [Google Scholar]
Dechartres 2013
- Dechartres A, Trinquart L, Boutron I, Ravaud P. Influence of trial sample size on treatment effect estimates: meta-epidemiological study. BMJ 2013;346:f2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
de Mos 2009
- Mos M, Huygen FJ, Hoeven-Borgman M, Dieleman JP, Ch Stricker BH, Sturkenboom MCJM. Outcome of the complex regional pain syndrome. Clinical Journal of Pain 2009;25(7):590-7. [DOI] [PubMed] [Google Scholar]
de Rooij 2009
- Rooij AM, Mos M, Sturkenboom MC, Marinus J, den Maagdenberg AM, Hilten JJ. Familial occurrence of complex regional pain syndrome. European Journal of Pain 2009;13(2):171-7. [DOI] [PubMed] [Google Scholar]
Deschartes 2011
- Deschartes A, Boutron I, Trinquart L, Charles P, Ravaud P. Single-center trials show larger treatment effects than multicenter trials: evidence from a meta-epidemiologic study. Annals of Internal Medicine 2011;155:39-51. [DOI: 10.7326/0003-4819-155-1-201107050-00006] [DOI] [PubMed] [Google Scholar]
Dimova 2020
- Dimova V, Herrnberger M, Escolano-Lozano F, Rittner H, Vlckova E, Sommer C, et al. Clinical phenotypes and classification algorithm for complex regional pain syndrome. Neurology 2020;94:1-11. [DOI] [PubMed] [Google Scholar]
Duong 2018
- Duong S, Bravo D, Todd KJ, Finlayson RJ, MD, Tran DQ. Treatment of complex regional pain syndrome: an updated systematic review and narrative synthesis. Canadian Journal of Anaesthesia 2018;65(6):658-84. [DOI: 10.1007/s12630-018-1091-5] [DOI] [PubMed] [Google Scholar]
Dworkin 2008
- Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. Journal of Pain 2008;9(2):105-21. [DOI] [PubMed] [Google Scholar]
Dworkin 2009
- Dworkin RH, Turk DC, McDermott MP, Peirce-Sandner S, Burke LB, Cowan P, et al. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain 2009;146(3):238-44. [DOI] [PubMed] [Google Scholar]
Dworkin 2010
- Dworkin RH, Turk DC, Peirce-Sandner S, Baron R, Bellamy N, Burke LB, et al. Research design considerations for confirmatory chronic pain clinical trials: IMMPACT recommendations. Pain 2010;149(2):177-93. [DOI] [PubMed] [Google Scholar]
Elsharydah 2017
- Elsharydah A, Loo NH, Minhajuddin A, Kandil ES. Complex regional pain syndrome type 1 predictors — Epidemiological perspective from a national database analysis. Journal of Clinical Anesthesia 2017;39:34-7. [DOI] [PubMed] [Google Scholar]
Galer 2000
- Galer BS, Henderson J, Perander J, Jensen MP. Course of symptoms and quality of life measurement in complex regional pain syndrome: a pilot survey. Journal of Pain and Symptom Management 2000;20(4):286-92. [DOI] [PubMed] [Google Scholar]
Geertzen 1998
- Geertzen JHB, Dijkstra PU, Sonderen ELP, Groothoff JW, ten Duis HJ, Eisma WH. Relationship between impairments, disability and handicap in reflex sympathetic dystrophy patients: a long-term follow-up study. Clinical Rehabilitation 1998;12(5):402-12. [DOI] [PubMed] [Google Scholar]
Goebel 2011
- Goebel A. Complex regional pain syndrome in adults. Rheumatology 2011;50(10):1739-50. [DOI] [PubMed] [Google Scholar]
Goebel 2018
- Goebel A, Barker CH, Turner-Stokes L. Complex Regional Pain Syndrome in Adults: UK Guidelines for Diagnosis, Referral and Management in Primary and Secondary Care. 2nd edition. London: Royal College of Physicians, 2018. [Available from: https://www.rcplondon.ac.uk/guidelines-policy/complex-regional-pain-syndrome-adults] [Google Scholar]
Grieve 2016a
- Grieve S, Adams J, McCabe C. ‘What I really needed was the truth’. Exploring the information needs of people with complex regional pain syndrome. Musculoskeletal Care 2016;14:15-25. [DOI] [PubMed] [Google Scholar]
Grieve 2016b
- Grieve S, Jones L, Walsh N, McCabe C. What outcome measures are commonly used for complex regional pain syndrome clinical trials? A systematic review of the literature. European Journal of Pain 2016;20:331-40. [DOI: 10.1002/ejp.733] [DOI] [PubMed] [Google Scholar]
Grieve 2017
- Grieve S, Perez RSGM, Birklein F, Brunner F, Bruehl S, Harden N, et al. Recommendations for a first core outcome measurement set for complex regional pain syndrome clinical studies (COMPACT). Pain 2017;158(6):1083-90. [DOI: 10.1097/j.pain.0000000000000866] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grieve 2019
- Grieve S, Llewellyn A, Jones L, Manns S, Glanville V, McCabe CS. Complex regional pain syndrome: an international survey of clinical practice. European Journal of Pain 2019;23:1890-903. [DOI] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction - GRADE evidence profiles and summary of findings table. Clinical Journal of Clinical Epidemiology 2011a;64(4):383-94. [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). Journal of Clinical Epidemiology 2011;64(4):407-15. [DOI] [PubMed] [Google Scholar]
Harden 2005
- Harden RN, Bruehl SP. Diagnostic criteria: the statistical derivation of the four criterion factors. In: Wilson P, Stanton-Hicks M, Harden RN, editors(s). CRPS: Current Diagnosis and Therapy. Progress in Pain Research and Management. Vol. 32. Seattle: IASP Press, 2005:45-58. [Google Scholar]
Harden 2007
- Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Medicine 2007;8(4):326-31. [DOI] [PubMed] [Google Scholar]
Harden 2010
- Harden RN, Bruehl S, Perez RSGM, Birklein F, Marinus J, Maihofner C, et al. Validation of proposed diagnostic criteria (the "Budapest criteria") for complex regional pain syndrome. Pain 2010;150(2):268-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harden 2013
- Harden RN, Oaklander AL, Burton AW, Perez RSGM, Richardson K, Swan M, et al. Complex regional pain syndrome: practical diagnostic and treatment guidelines, 4th edition. Pain Medicine 2013;14(2):180-229. [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG. Chapter 16: Special topics in statistics. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Hoffman 2014
- Hoffmann T, Glasziou P, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI: 10.1136/bmj.g1687] [DOI] [PubMed] [Google Scholar]
Hoogeboom 2020
- Hoogeboom TJ, Kousemaker MC, Meeteren NLU, Howe T, Bo K, Tugwell P et al. i-CONTENT tool for assessing therapeutic quality of exercise programs employed in randomised clinical trials. British Journal of Sports Medicine 2020 Nov 3 [Epub ahead of print]. [DOI: 10.1136/bjsports-2019-101630] [DOI] [PMC free article] [PubMed]
ICMJE 2019
- International Committee of Medical Journal Editors. Up-dated ICMJE Recommendations (December 2019). http://www.icmje.org/news-and-editorials/updated_recommendations_dec2019.html 2019.
Johnston‐Devin 2018
- Johnston-Devin C, Oprescu F, Gay M. Living with complex regional pain syndrome: understanding the battle. In: Rysewyk S, editors(s). Meanings of Pain. Volume 2: Common Types of Pain and Language. Springer, 2018:163-83. [ISBN 978-3-030-24153-7 ] [Google Scholar]
Kemler 2000
- Kemler MA, Vet HC. Health-related quality of life in chronic refractory reflex sympathetic dystrophy (complex regional pain syndrome type I). Journal of Pain and Symptom Management 2000;20(1):68-76. [DOI] [PubMed] [Google Scholar]
Kisner 2002
- Kisner C, Colby LA. Therapeutic Exercise: Foundations and Techniques. 4th edition. Philadelphia: F.A. Davis Company, 2002. [Google Scholar]
Knudsen 2019
- Knudsen LF, Terkelsen AJ, Drummond PD, Birklein F. Complex regional pain syndrome: a focus on the autonomic nervous system. Clinical Autonomic Research 2019;29:457-67. [DOI] [PubMed] [Google Scholar]
Kozin 1992
- Kozin F. Reflex sympathetic dystrophy syndrome: a review. Clinical and Experimental Rheumatology 1992;10(4):401-9. [PubMed] [Google Scholar]
Logan 2017
- Logan CA, Asnis PD, Provencher MT. The role of therapeutic modalities in surgical and nonsurgical management of orthopaedic injuries. Journal of the American Academy of Orthopedic Surgeons 2017;25(8):556-68. [DOI] [PubMed] [Google Scholar]
Lohnberg 2013
- Lohnberg JA, Altmaier EM. A review of psychosocial factors in complex regional pain syndrome. Journal of Clinical Psychology in Medical Settings 2013;20(2):247-54. [DOI] [PubMed] [Google Scholar]
Marinus 2011
- Marinus J, Moseley GL, Birklein F, Baron R, Maihöfner C, Kingery WS, et al. Clinical features and pathophysiology of complex regional pain syndrome. Lancet Neurology 2011;10(7):637-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Merskey 1994
- Merskey H, Bogduk N. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. 2nd edition. Seattle: IASP Press, 1994. [Google Scholar]
Miller 2017
- Miller C, Williams M, Heine P, Williamson E, O’Connell N. Current practice in the rehabilitation of complex regional pain syndrome: a survey of practitioners. Disability and Rehabilitation 2017;41(7):847-53. [DOI] [PubMed] [Google Scholar]
Miller 2019
- Miller C, Williams M, Heine P, Williamson E, O'Connell N. Current practice in the rehabilitation of complex regional pain syndrome: a survey of practitioners. Disability and Rehabilitation 2019;41(7):847-53. [DOI: 10.1080/09638288.2017.1407968] [DOI] [PubMed] [Google Scholar]
Möhler 2015
- Möhler R, Köpke S, Meyer G. Criteria for reporting the development and evaluation of complex interventions in healthcare: revised guideline (CReDECI 2). Trials 2015;16:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 2008
- Moore RA, Barden J, Derry S, McQuay HJ. Managing potential publication bias. In: McQuay HJ, Kalso E, Moore RA, editors(s). Systematic Reviews in Pain Research: Methodology Refined. Seattle: IASP Press, 2008:15-23. [Google Scholar]
Moore 2010
- Moore RA, Eccleston C, Derry S, Wiffen P, Bell RF, Straube S, et al. "Evidence" in chronic pain--establishing best practice in the reporting of systematic reviews. Pain 2010;150(3):386-9. [DOI] [PubMed] [Google Scholar]
Moore 2012
- Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for neuropathic pain and fibromyalgia in adults. Cochrane Database of Systematic Reviews 2012, Issue 12. Art. No: CD008242. [DOI: 10.1002/14651858.CD008242.pub2] [DOI] [PubMed] [Google Scholar]
Moseley 2012
- Moseley GL, Flor H. Targeting cortical representations in the treatment of chronic pain: a review. Neurorehabilitation and Neural Repair 2012;26(6):646-52. [DOI] [PubMed] [Google Scholar]
Moseley 2015
- Moseley GL, Butler DS. 15 years of explaining pain: the past, present and future. Journal of Pain 2015;16(9):807-13. [DOI] [PubMed] [Google Scholar]
Nijs 2012
- Nijs J, Kosek E, Van Oosterwijck J, Meeus M. Dysfunctional endogenous analgesia during exercise in patients with chronic pain: to exercise or not to exercise? Pain Physician 2012;15(3 Suppl):ES205-13. [PubMed] [Google Scholar]
Nüesch 2010
- Nüesch E, Trelle S, Reichenbach S, Rutjes AWS, Tschannen B, Altman DG, et al. Small study effects in meta-analyses of osteoarthritis trials: meta-epidemiological study. BMJ 2010;341:c3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Connell 2013
- O’Connell NE, Wand BM, McAuley J, Marston L, Moseley GL. Interventions for treating pain and disability in adults with complex regional pain syndrome- an overview of systematic reviews. Cochrane Database of Systematic Reviews 2013, Issue 4. Art. No: CD009416. [DOI: 10.1002/14651858.CD009416.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Packham 2018
- Packham T, Holly J. Mechanism-specific rehabilitation management of complex regional pain syndrome: proposed recommendations from evidence synthesis. Journal of Hand Therapy 2018;31:238-49. [DOI] [PubMed] [Google Scholar]
Packham 2020
- Packham TL, Wainio K, Wong M-K. Persons with complex regional pain syndrome renegotiate social roles and intimacy: a qualitative study. Pain Medicine 2020;21(2):239-46. [DOI] [PubMed] [Google Scholar]
Parkitny 2013
- Parkitny L, McAuley JH, Di Pietro F, Stanton TR, O'Connell NE, Marinus J, et al. Inflammation in complex regional pain syndrome: a systematic review and meta-analysis. Neurology 2013;80(1):106-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perez 2010
- Perez RS, Zollinger PE, Dijkstra PU, Thomassen-Hilgersom IL, Zuurmond WW, Rosenbrand KCL, et al. Evidence based guidelines for complex regional pain syndrome type 1. BMC Neurology 2010;10:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reinders 2002
- Reinders MF, Geertzen JHB, Dijkstra PU. Complex regional pain syndrome type I: use of the International Association for the Study of Pain diagnostic criteria defined in 1994. Clinical Journal of Pain 2002;18(4):207-15. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Review Manager. Version 5.3. Copenhagen: The Nordic Cochrane Centre; The Cochrane Collaboration, 2014.
Robertson 2006
- Robertson V, Ward A, Low J, Reed A. Electrotherapy Explained. Principles and Practice. 4th edition. London: Butterworth-Heinemann, 2006. [Google Scholar]
Sandroni 2003
- Sandroni P, Benrud-Larson LM, McClelland RL, Low PA. Complex regional pain syndrome type I: incidence and prevalence in Olmsted county, a population-based study. Pain 2003;103(1-2):199-207. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Sharma 2009
- Sharma A, Agarwal S, Broatch J, Raja SN. A web-based cross-sectional epidemiological survey of complex regional pain syndrome. Regional Anesthesia and Pain Medicine 2009;34(2):110-5. [DOI] [PubMed] [Google Scholar]
Shea 2017
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. [doi: 10.1136/bmj.j4008.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shepherd 2018
- Shepherd M, Louw A, Podolak J. The clinical application of pain neuroscience, graded motor imagery, and graded activity with complex regional pain syndrome—a case report. Physiotherapy Theory and Practice 2018;36(9):1043-55. [DOI: 10.1080/09593985.2018.1548047] [DOI] [PubMed] [Google Scholar]
Shim 2019
- Shim H, Rose J, Halle S, Shekane P. Complex regional pain syndrome: a narrative review for the practising clinician. British Journal of Anaesthesia 2019;123(2):e424-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shipton 2009
- Shipton EA. Complex regional pain syndrome - mechanisms, diagnosis, and management. Current Anaesthesia & Critical Care 2009;20(5-6):209-14. [Google Scholar]
Smith 2005
- Smith TO. How effective is physiotherapy in the treatment of complex regional pain syndrome type I? A review of the literature. Musculoskeletal Care 2005;3(4):181-200. [DOI] [PubMed] [Google Scholar]
Smith 2015
- Smith SM, Hunsinger M, McKeown A, Parkhurst M, Allen R, Kopko S, et al. Quality of pain intensity assessment reporting: ACTTION systematic review and recommendations. Journal of Pain 2015;16(4):299-305. [DOI] [PubMed] [Google Scholar]
Smith 2019
- Smith BE, Hendrick P, Bateman M, Holden S, Littlewood C, Smith TO, et al. Musculoskeletal pain and exercise - challenging existing paradigms and introducing new. British Journal of Sports Medicine 2019;53(14):907-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stanton‐Hicks 2002
- Stanton-Hicks MD, Burton AW, Bruehl SP, Carr DB, Harden RN, Hassenbusch SJ, et al. An updated interdisciplinary clinical pathway for CRPS: report of an expert panel. Pain Practice 2002;2(1):1-16. [DOI] [PubMed] [Google Scholar]
Steinbrocker 1948
- Steinbrocker O, Spitzer N, Friedman HH. The shoulder-hand syndrome in reflex dystrophy of the upper extremity. Annals of Internal Medicine 1948;29(1):22-52. [DOI] [PubMed] [Google Scholar]
Todorova 2013
- Todorova J, Dantchev N, Petrova G. Complex regional pain syndrome acceptance and the alternative denominations in the medical literature. Medical Principles and Practice 2013;22(3):295-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Turk 2008a
- Turk DC, Dworkin RH, McDermott MP, Bellamy N, Burke LB, Chandler JM, et al. Analyzing multiple endpoints in clinical trials of pain treatments: IMMPACT recommendations. Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials. Pain 2008;139(3):485-93. [DOI] [PubMed] [Google Scholar]
Turk 2008b
- Turk DC, Dworkin RH, Revicki D, Harding G, Burke LB, Cella D, et al. Identifying important outcome domains for chronic pain clinical trials: an IMMPACT survey of people with pain. Pain 2008;137(2):276-85. [DOI] [PubMed] [Google Scholar]
Unverzagt 2013
- Unverzagta S, Prondzinskyb R, Peinemann F. Single-center trials tend to provide larger treatment effects than multicenter trials: a systematic review. Journal of Clinical Epidemiology 2013;66:1271-80. [DOI: 10.1016/j.jclinepi.2013.05.016] [DOI] [PubMed] [Google Scholar]
Vaneker 2006
- Vaneker M, Wilder-Smith OH, Schrombges P, Oerlemans HM. Impairments as measured by ISS do not greatly change between one and eight years after CRPS 1 diagnosis. European Journal of Pain 2006;10(7):639-44. [DOI] [PubMed] [Google Scholar]
van Rijn 2011
- Rijn MA, Marinus J, Putter H, Bosselaar SRJ, Moseley GL, Hilten JJ. Spreading of complex regional pain syndrome: not a random process. Journal of Neural Transmission 2011;118(9):1301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Velzen 2019
- Velzen GAJ, Huygen FJPM, Kleef M, Eijs FV, Marinus J, Hilten JJ. Sex matters in complex regional pain syndrome. European Journal of Pain 2019;23:1108-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Veldman 1993
- Veldman PH, Reynen HM, Arntz IE, Goris RJ. Signs and symptoms in reflex sympathetic dystrophy: prospective study of 829 patients. Lancet 1993;342(8878):1012-6. [DOI] [PubMed] [Google Scholar]
Viergever 2014
- Viergever RF, Karam G, Reis A, Ghersi D. The quality of registration of clinical trials: still a problem. PLOS One 2014;9(1):e84727. [DOI: 10.1371/journal.pone.0084727] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wertli 2013
- Wertli M, Bachmann LM, Schecter Weiner S, Brunner F. Prognostic factors in complex regional pain syndrome 1: a systematic review. Journal of Rehabilitation Medicine 2013;45:225-31. [DOI] [PubMed] [Google Scholar]
Williams 2020
- Williams AC de C, Fisher E, Hearn L, Eccleston C. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database of Systematic Reviews 2020, Issue 8. Art. No: CD007407. [DOI: 10.1002/14651858.CD007407.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zyluk 1998
- Zyluk A. The natural history of post-traumatic reflex sympathetic dystrophy. Journal of Hand Surgery 1998;23(1):20-3. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Smart 2013
- Smart KM, Wand BM, O'Connell NE. Physiotherapy for pain and disability in adults with complex regional pain syndrome (CRPS) types I and II. Cochrane Database of Systematic Reviews 2013, Issue 11. Art. No: CD010853. [DOI: 10.1002/14651858.CD010853] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smart 2016
- Smart KM, Wand BM, O'Connell NE. Physiotherapy for pain and disability in adults with complex regional pain syndrome (CRPS) types I and II. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No: CD010853. [DOI: 10.1002/14651858.CD010853.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


