Abstract
Background: Trapeziometacarpal arthroplasties are designed to restore an adequate level of mobility, stability, and grip strength. In this article, pain and functional and radiographic outcome of Ivory arthroplasty in male patients are investigated. Methods: Between 2005 and 2012, the Ivory arthroplasty was inserted in 21 male patients with degenerative trapeziometacarpal osteoarthritis, of which 14 patients were found eligible for inclusion. Mobility, grip strength, patient self-assessment (pain; Quick Disabilities of the Arm, Shoulder, and Hand [QuickDASH]), and radiographic outcome were measured. Twenty-two female patients who received an Ivory arthroplasty between 2005 and 2007 were included and underwent the same evaluation. Age at primary surgery, survival rate of the implant, and clinical outcome were compared between the 2 groups. Results: In both groups, QuickDASH score and mean pain sensation improved significantly. The improvement in mobility obtained significance in the female group. In the male group, 7 arthroplasties failed (mean follow-up of 65 months). In the female group, 3 of the 24 arthroplasties failed (mean follow-up of 123 months). Kaplan-Meier survival analysis demonstrated a significant lower implant survival in the male group. Conclusions: Decrease in muscle mass and decline in grip strength that postmenopausal women tend to experience might explain the significant difference in implant survival between sexes. In 4 of the 7 failed arthroplasties in the male group, no surgical revision was required. Trapeziometacarpal arthroplasty, even after radiographic failure, still served as a spacer, avoiding collapse of the thumb base. Nevertheless, the failure rate of the Ivory arthroplasty in male patients is high, and an alternative treatment should be considered.
Keywords: arthroplasty, arthritis, diagnosis, CMC, osteoarthritis, biomechanics, basic science, thumb, anatomy, ivory prosthesis, ball-and-socket arthroplasty
Introduction
Background
Trapeziometacarpal joint is a biconcave saddle joint that allows a wide range of movements. The downside of this great mobility is limited stability; and as a result, degenerative trapeziometacarpal joint osteoarthritis frequently develops over time. 1 In case of failure of a conservative treatment, several surgical options—arthroplasty, trapeziectomy, or arthrodesis—can be adopted. Procedures such as excision of the trapezium, ligament reconstruction, or tendon interposition can result in loss of thumb length and hence pinch strength. Trapeziometacarpal joint fusion typically causes loss of mobility and overcharging of the neighboring joints. 2 Trapeziometacarpal arthroplasties are designed to restore normal thumb length and to obtain an adequate level of mobility, stability, and grip strength. Dislocation and loosening of the arthroplasty with secondary wear are possible complications. 3 Many types of uncemented ball-and-socket arthroplasties exist: the Arpe, Roseland, Elektra, Moje, Maïa, and Ivory are examples.3-8 At our center, Ivory arthroplasty (Stryker Oratiereeks, Kalamazoo, MI, USA) is most frequently used. The double-coned shape of the cup of the Ivory enhances stability. The Ivory arthroplasty has a rotational arc of 90°, which approximates 75° of a normal trapeziometacarpal joint. Different types of ball-and-socket prostheses have a mobility range up to 120° (eg, Arpe; Zimmer Biomet, Warsaw, IN, USA), rendering the arthroplasty more prone to dislocation.
Purpose of This Study
The first objective of this study was to evaluate whether in men the Ivory arthroplasty is a reliable surgical option for advanced trapeziometacarpal joint osteoarthritis when conservative treatment has failed. This was performed by studying the clinical and radiographic outcomes of the arthroplasty in a male group. A second objective was to compare these outcomes and implant survival with a female group, subjected to an analog evaluation. This comparison was considered a quick win, as we had the disposal of a historical cohort of female patients undergoing the same surgical intervention by the same surgeon in the same center, was at our disposal.
Materials and Methods
Study Design
In this retrospective study, male patients who received an Ivory arthroplasty for trapeziometacarpal joint osteoarthritis were evaluated for clinical outcome, overall function, radiographic outcome, and qualitative outcome.
Female patients who were treated with an Ivory arthroplasty in the same center were submitted to an analog evaluation. When found eligible for inclusion, outcome data on the female patients were partially (eg, 21 of 22 patients) retrieved from a previous study, described in Vissers et al. 8 This historical cohort of patients provided an excellent basis for comparison because of a systematic clinical and radiographic follow-up and long-term registration. All surgical interventions (male and female patients) were performed by 2 consultant hand surgeons of our orthopedic unit. Surgical approach, as well as technique, did not change over time. Age at primary surgery, survival rate, and clinical outcome (opposition and retropulsion, as described by Kapandji in 1990) 9 were compared between the 2 groups.
Patients
Male patients who were treated with an Ivory arthroplasty between 2005 and 2012 were evaluated. The Ivory arthroplasty was inserted in 21 patients with trapeziometacarpal osteoarthritis. They all had primary degenerative osteoarthritis. Inclusion criteria were based on severe pain at rest and during activity that did not respond to conservative treatment for more than 3 months. Conservative treatment included night splinting, nonsteroidal anti-inflammatory drugs, and/or intra-articular corticosteroid infiltration. On a radiological classification, Dell stages II and III were considered to be good candidates for the Ivory Arthroplasty. 10 Preoperatively, every patient was offered the choice of trapeziectomy as an alternative to the Ivory arthroplasty. Patients with a high demand for thumb grip and strength were advised to consider the Ivory arthroplasty over trapeziectomy. In a vast majority of patients with degenerative trapeziometacarpal arthritis—high and low demand—an Ivory arthroplasty was the chosen surgical treatment.
Twenty-two female patients who received an Ivory arthroplasty between 2005 and 2007 were included based on the same criteria and were submitted to the same evaluation with a minimum of 5 years of follow-up.
Ivory Arthroplasty
The Ivory arthroplasty is modular: the individual components are an anatomical hydroxyapatite-covered metal stem, a neck with or without offset, a hydroxyapatite-covered cup, and an ultra-high-molecular-weight polyethylene insert. The cup is tapered in a coronal and sagittal plane (double-tapered): this ensures a stable press fit in the trapezium. The noncemented anatomical stem matches the specific anatomy of the thumb metacarpal, which facilitates incorporation and diminishes the loosening possibility subsequently. Different neck heights (eg, short, medium, and long) can be inserted. Furthermore, the neck can be placed on the stem in different rotations (eg, −30°, 0°, and +30°). In this way, a well-balanced tension can be obtained, and impingement is avoided. In our series, the amount of rotation was determined during surgery to ensure optimal stability in both retropulsion and opposition. The neutral rotation (0°) was selected in most of the patients.
A detailed description of the surgical procedure can be found in literature and is not included in this article.3,8,11
Assessment
All patients were assessed preoperatively and postoperatively. The consultant hand surgeon performed the preoperative assessment and immediate postoperative follow-up. For each patient, clinical outcome (mobility and strength) and overall function (including pain score) were objectified. Every patient visited the outpatient clinic the first postoperative day. A radiographic evaluation was performed, and a thumb spica cast was applied for 3 weeks. Cast removal and initiation of mobilization occurred after 3 weeks. The first full clinical and radiographic assessment took place after 6 weeks and was repeated after 12 weeks. From the fourth postoperative month, patients were allowed to increase grip power and to exert force against resistance. From then on, the same full assessments were intended on a yearly basis. Final assessment was carried out by a hand surgeon who was not present during the preoperative assessment or the operation. The assessment of the mobility of the thumb occurred by grading opposition and retropulsion. 9
A calibrated hydraulic pinch gauge and a calibrated hydraulic dynamometer (Baseline Fabrication Enterprises Inc., Irvington, NY, USA) were used to measure key pinch, precision pinch, and grip strength, respectively, and assessment of the mobility of the thumb occurred by grading opposition and retropulsion. 9
The Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) score was obtained to determine overall function. Pain was objectified by a Visual Analog Scale (VAS), where a score of 0 indicated no pain and a score of 10 the worst pain imaginable by the patient.
An arthroplasty was considered to be a failure whenever failing of 1 or more of the individual components occurred. Dislocation of the cup, fracture of the neck, chronic luxation, and polyethylene wear were all considered to be a failure. An early postoperative luxation of the neck, in which case a closed reduction was performed, was not considered to be a failure. Radiographic evaluation included the trapeziometacarpal joint assessment as described by Kapandji and Kapandji, 12 a frontal view of the scaphotrapezial joint (Bett’s view), 13 and Eaton views. 12
Statistical Analysis
Statistical analyses were performed to assess the relationship of dependent variables (opposition, retropulsion, opening of the first web, metacarpophalangeal flexion and extension, grip strength, key pinch, and precision pinch) over time (from the preoperative findings until the final evaluation). Analyses also allowed us to model the relationship between the operated hand and the contralateral hand at final evaluation. For each paired comparison, we only kept observations having no missing values for the preoperation and postoperation. We took the difference between the parameter measured before and after operation and assessed whether the difference was normally distributed using the Kolmogorov-Smirnov test. When this difference had proven to be normally distributed, we performed a paired t test and reported mean ± SD, and if this was not the case, we performed a paired Wilcoxon test and reported medians and interquartile ranges.
Age at primary surgery and clinical outcome (mean difference in opposition and retropulsion between preoperative and postoperative value) were compared between the male and female subgroups, using a nonpaired Student t test. Similar tests were performed for pain sensation (VAS) and overall function (QuickDASH). A survival analysis of the arthroplasty in the male and female group was compared using Kaplan-Meier χ2 analyses.
Results
Patients
In the male group, 17 Ivory arthroplasties were evaluated. Of the 21 patients who were originally treated with the Ivory arthroplasty, 14 patients were eligible for inclusion, including 3 patients with bilateral arthroplasties. Four patients were deceased, and 3 others were lost to follow-up. There was a mean follow-up period of 65 (range, 3-119) months postoperatively.
In the female group, 29 patients were treated with the Ivory arthroplasty, of which 22 were eligible for inclusion. Two patients were deceased, and 5 were lost to follow-up. Bilateral arthroplasties were found in 2 of the remaining patients. For implant survival, the mean follow-up period was 123 (range, 46-142) months postoperatively.
Outcomes Over Time
The preoperative and postoperative outcomes in the male group are shown in Table 1. The QuickDASH score decreased from 30.60 to 19.40, which is a significant improvement (P = .0083). Mean pain sensation according to the VAS decreased from 65 to 10 (P = 0.0001). No statistically significant changes occurred in other preoperative and postoperative outcomes.
Table 1.
Clinical Outcomes and Overall Function Preoperatively and Postoperatively in the Male Group of Patients.
| Variable | No. of subjects | Mean preoperatively | Mean at follow-up | P value |
|---|---|---|---|---|
| Oppostion a | 9 | 8.83 ± 0.79 | 8.56 ± 1.57 | .6419 |
| Retropulsion a | 9 | 2.39 ± 0.74 | 2.56 ± 0.73 | .6364 |
| Key pinch, kg | 11 | 6.50 ± 3.52 | 7.54 ± 2.35 | .4224 |
| Precision pinch, kg | 11 | 4.46 ± 2.19 | 5.045 ± 1.88 | .5040 |
| Grip strength, kg | 10 | 30.00 ± 10.20 | 30.70 ± 14.97 | .9041 |
| QuickDASH score | 10 | 30.60 ± 7.15 | 19.40 ± 7.93 | .0038 |
| VAS | 10 | 65.30 ± 18.23 | 10.20 ± 9.34 | .0001 |
Note. QuickDASH = Quick Disabilities of the Arm, Shoulder, and Hand; VAS = Visual Analog Scale.
As defined by Kapandji and Kapandji. 12
Failure occurred in 7 of the 17 arthroplasties. Three patients experienced a cup dislocation due to collapse of the trapezial bone. One was converted to a trapeziectomy. In a second patient, an augmentation of the cup was performed with an autologous iliac crest bone block graft. A third patient had little discomfort and did not undergo surgical revision. Two other arthroplasties had neck fractures. One of them underwent surgical revision, although the last radiographic checkup showed a new neck fracture. Both neck fractures were well tolerated by the patient. The decision to change the first broken neck was more a suggestion of the surgeon than a request by the patient. In the 2 remaining patients, extreme polyetylene wear was diagnosed. One of them underwent a conversion to a trapeziectomy. The other one experienced little to no discomfort and was treated by a close follow-up in our outpatient clinic.
In the female group, a significant improvement was found in opposition and retropulsion. The QuickDASH score and mean pain sensation significantly improved when compared with the preoperative condition. At a minimum follow-up period of 10 years, 3 failures were encountered. Two patients experienced a cup dislocation. One of them was submitted to surgical revision in which the dislocated cup was replaced by a larger sized cup. In the other patient, the arthroplasty was converted to a trapeziectomy. The third patient had a chronic subluxation of the arthroplasty. Results are shown in Table 2. An overview of the individual failures is displayed in Table 3. Time points for these failures are included as well.
Table 2.
Clinical Outcomes in the Operated Hand and the Contralateral Hand at Follow-up.
| Variable | No. of objects | Mean at follow-up | Mean contralateral at follow-up | P value |
|---|---|---|---|---|
| Opening first web, deg | 10 | 50.2 ± 14.59 | 46.9 ± 12.63 | .2185 |
| Oppostion a | 11 | 8.82 ± 0.98 | 8.55 ± 1.37 | .4316 |
| Retropulsion a | 11 | 2.14 ± 0.64 | 2.23 ± 1.03 | .7787 |
| MP flexion, deg | 10 | 53.1 ± 20.25 | 43.7 ± 24.26 | .0901 |
| MP extension, deg | 10 | 14.7 ± 8.26 | 12.9 ± 10.28 | .6642 |
| Key pinch, kg | 11 | 7.09 ± 2.15 | 7.68 ± 2.23 | .2051 |
| Precision pinch, kg | 11 | 5.05 ± 1.85 | 5.18 ± 2.32 | .7643 |
| Grip strength, | 11 | 29.91 ± 15.01 | 31.82 ± 9.31 | .5291 |
Note. MP = metacarpophalangeal.
As defined by Kapandji and Kapandji. 12
Table 3.
Failures of the Ivory Arthroplasty.
| Patient number | Sex | Age | Cause of failure | Treatment | Time point of failure (months postoperatively) |
|---|---|---|---|---|---|
| 1 | M | 51 | Cup dislocation | Trapeziectomy | 97 |
| 2 | M | 68 | Cup dislocation | Cup augmentation | 68 |
| 3 | M | 58 | Cup dislocation | No surgical treatment | 43 |
| 4 | M | 59 | Neck fracture | No surgical treatment | 97 |
| 5 | M | 67 | Neck fracture | Replacement neck | 88 |
| 6 | M | 58 | Polyethylene wear | No surgical treatment | 70 |
| 7 | M | 69 | Polyethylene wear | Trapeziectomy | 55 |
| 8 | F | 64 | Cup dislocation | Replacement cup | 46 |
| 9 | F | 63 | Cup dislocation | Trapeziectomy | 114 |
| 10 | F | 70 | Chronic subluxation | Replacement polyethylene | 48 |
M = male; F = female.
Comparing Outcomes of the Male and Female Groups
Male and female observations were collected at a mean follow-up of 65 months. When comparing the male and female groups, men are significantly younger at primary surgery than women (P = .0011). When comparing the change in QuickDASH between the preoperative and postoperative assessment, no significant difference could be found between the male and female groups. Similar analysis showed no significance for the change in retropulsion. The mean differences in pain sensation (VAS) and opposition were significantly larger in the female group than in the male group. All results are displayed in Table 4. Kaplan-Meier survival analysis—women: n = 24; men: n = 17, χ2(1)=5.26; P < .05—demonstrated a significantly lower implant survival in the male group. The survival curves are displayed in Figure 1.
Table 4.
Comparison of the Change in Clinical Outcomes and Overall Function Between the Male and Female Groups.
| Variable | Male group | Female group | P value |
|---|---|---|---|
| Age, y | 71.33 ± 7.16 | 62.94 ± 7.42 | .0129 |
| Change in opposition a | −0.28 ± 1.00 | 0.70 ± 1.14 | .0356 |
| Change in retropulsion a | 0.17 ± 1.09 | 0.53 ± 0.86 | .3495 |
| Change in VAS | 11.33 ± 9.15 | 58.75 ± 23.91 | .0001 |
| Change in QuickDASH score | 10.56 ± 10.94 | 24.86 ± 26.94 | .1439 |
Note. QuickDASH = Quick Disabilities of the Arm, Shoulder, and Hand; VAS = visual analogue scale.
All values are represented as mean +/– SD.
As defined by Kapandji Kapandji. 12
Figure 1.
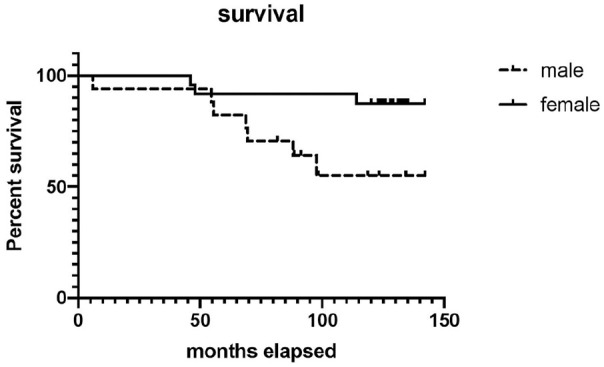
Kaplan-Meier survival analysis—women: n = 24; men: n = 17, χ2(1)=5.26; P < .05—demonstrated a significant lower implant survival in the male group.
Discussion
Overall function of the Ivory arthroplasty in the male group ameliorated when compared with the preoperative situation. This is mainly due to the improvement in QuickDASH score and the reduction in pain according to the VAS. Similar improvements were described in earlier analyses of the same arthroplasty.3,8,11
The survival rate of the Ivory arthroplasty in male patients in our series is 65% after a mean follow-up of 65 months. No more than 3 studies in literature incorporated more than 10 male patients. None of these studies described differences in outcome between men and women, and in neither one, the Ivory arthroplasty was used. In 1 series considering the Elektra arthroplasty, 15 of 100 patients were men. 14 Nineteen arthroplasties failed after a mean follow-up of 53 months. In another series reporting outcome of the Guepar II arthroplasty, 13 of the 68 patients were men, and only 1 failure was encountered after 50 months of follow-up. 15 In a third series, studying the Maïa arthroplasty, a 5% failure rate was described after 72 months of follow-up. 16 In this series, 11 of the 80 patients were men. Nevertheless, because of the abovementioned reasons, a comparison with the male group of patients in our series is of limited value.
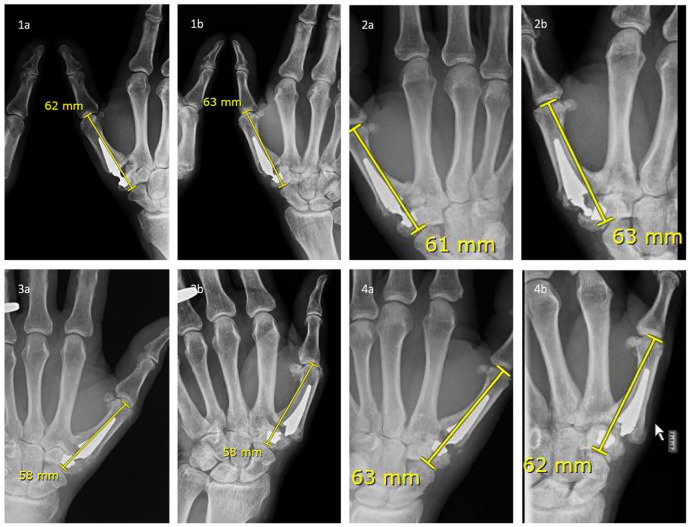
Radiographic analysis of the 17 arthroplasties in the male group described in this article demonstrated failure in 7 of them. In 4 patients, revisionary surgery was performed. In 1 of these patients, a change of the neck of the arthroplasty resulted in a new neck fracture over time. In this patient and in the 3 remaining arthroplasties, radiographs at the follow-up consultation demonstrated substantial osteophytes over time, and the complications resulted in little or no shortening of the thumb (Figure 2). This states the impression that trapeziometacarpal arthroplasty, even after radiographic failure, still served as a spacer, avoiding collapse of the thumb base. These patients were pleased with their overall function, had acceptable discomfort, and did not seek invasive treatment of their arthroplasty. In this way, these anomalous arthroplasties can be compared with the patients who develop a nonunion of their attempted trapeziometacarpal arthrodesis. These patients typically regard their procedure as successful once the stabilizing material has been removed. This observation stimulated some authors to take it 1 step further and to create a trapeziometacarpal narrow pseudarthrosis, with a significant improvement in QuickDASH score, mobility, and pain sensation. 17 Technically, the patients with a failed prosthesis, failed arthrodesis, and controlled pseudarthrosis have in common that the degenerated cartilage and eburnated subchondral bone were removed. Mechanical stability is provided to the previously unstable joint, and a fair degree of mobility of the thumb is restored.
Figure 2.
Radiographic evaluation of the trapeziometacarpal joint as described by Kapandji and Kapandji. 12
Note. Patient 1: polyethylene wear; patient 2: cup dislocation and subsequent chronic luxation; patients 3, 4: neck fractures. “a” represents the situation before and “b” the situation after the complication. No collapse or radiographic shortening of the thumb occurred in these patients following the complication. None of these patients required explantation.
The overall survival in the female subgroup, described in this article, is significantly higher compared with the male subgroup, with 3 failures out of the 24 arthroplasties after a mean follow-up of 123 months. A plausible explanation can be the fact that postmenopausal women tend to experience progressive decline in muscle mass. 18 The consequential decrease in muscular strength might increase the difference in, for instance, grip strength between men and women with aging. We must not forget that in a key pinch maneuver, the cantilever bending loads produce a dorsoradial force at the thumb metacarpal base that is over 12 times the force applied at the fingertip. 19 The pressure applied on a trapeziometacarpal prosthesis is consequently larger in men. This can explain the high radiographic failure rate in men and renders the use of the Ivory arthroplasty in a male population debatable. Because of this high radiographic complication rate (7 of 17 arthroplasties), an alternative treatment should be considered in the male patient. Several studies have conducted a long-term comparison of outcome between a trapeziometacarpal prosthesis and a trapeziectomy with ligament reconstruction and tendon interposition (LRTI). Robles-Molina et al 20 compared trapeziectomy with LRTI and the Arpe prosthesis and demonstrated similar pain relief and functional improvement between the 2 groups. Pinch strength and range of motion were superior in the Arpe group. Cebrian-Gomez et al 21 conducted an analog comparison with the Ivory prosthesis. In their series, prosthetic replacement provided significantly better thumb abduction, adduction, pinch strength, QuickDASH, pain relief, satisfaction, and a faster return to work. Ulrich-Vinther et al 22 compared the Elektra prosthesis with trapeziectomy with LRTI and reported significantly faster pain relief, stronger grip function, and improved range of motion in the prosthesis group. Vandenberghe et al 23 could not find any difference in long-term impairment, pain reduction, patient satisfaction, and disability between trapeziectomy with LRTI, and de la Caffinière or Roseland arthroplasty. In these comparative studies, no differences in outcome between the sexes are mentioned, although the relative percentage of men included in the individual study is low and only exceeds 10% in the study by Ulrich-Vinther et al. 22
Acknowledgments
The authors wish to thank Gino Vissers for his work in data collection processing. They also wish to thank Jean François Fils, Ars Statistica S.P.R.L., Nivelles, Belgium, for his assistance with the statistical analyses in this article. Furthermore, they wish to thank their secretaries and nurses of the hospital for their organizational support.
Footnotes
Ethical Approval: This trial has been approved by the Leading Ethics Committee of AZ Sint-Jan Hospital in Bruges on November 29, 2016, with trial number 2069.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: All patients enrolled in this study gave informed consent to participate, and no identifying factors were used.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Bert Vanmierlo  https://orcid.org/0000-0002-0157-3316
https://orcid.org/0000-0002-0157-3316
Kjell Van Royen  https://orcid.org/0000-0002-1861-601X
https://orcid.org/0000-0002-1861-601X
References
- 1. Baker RHJ, Al-Shukri J, Davis TRC. Evidence-based medicine: thumb basal joint arthritis. Plast Reconstr Surg. 2017;139(1):256e-266e. [DOI] [PubMed] [Google Scholar]
- 2. Cootjans K, Vanhaecke J, Dezillie M, et al. Joint survival analysis and clinical outcome of total joint arthroplasties with the ARPE implant in the treatment of trapeziometacarpal osteoarthritis with a minimal follow-up of 5 years. J Hand Surg Am. 2017;42(8):630-638. [DOI] [PubMed] [Google Scholar]
- 3. Goubau JF, Goorens CK, Van Hoonacker P, et al. Clinical and radiological outcomes of the Ivory arthroplasty for trapeziometacarpal joint osteoarthritis with a minimum of 5 years of follow-up: a prospective single-centre cohort study. J Hand Surg Eur Vol. 2013;38(8):866-874. [DOI] [PubMed] [Google Scholar]
- 4. Apard T, Saint-Cast Y. Results of a 5 years follow-up of Arpe prosthesis for the basal thumb osteoarthritis [in French]. Chir Main. 2007;26:88-94. [DOI] [PubMed] [Google Scholar]
- 5. Guardia C, Moutet F, Corcella D, et al. Roseland® prosthesis: quality of life’s studies about 68 patients with a mean followed-up of 43.8 months [in French]. Chir Main. 2010;29:301-306. [DOI] [PubMed] [Google Scholar]
- 6. Jager T, Barbary S, Dap F, et al. Evaluation of postoperative pain and early functional results in the treatment of carpometacarpal joint arthritis. Comparative prospective study of trapeziectomy vs. MAIA® prosthesis in 74 female patients [in French]. Chir Main. 2013;32:55-62. [DOI] [PubMed] [Google Scholar]
- 7. Klahn A, Nygaard M, Gvozdenovic R, et al. Elektra prosthesis for trapeziometacarpal osteoarthritis: a follow-up of 39 consecutive cases. J Hand Surg Eur Vol. 2012;37(7):605-609. [DOI] [PubMed] [Google Scholar]
- 8. Vissers G, Goorens CK, Vanmierlo B, et al. Ivory arthroplasty for trapeziometacarpal osteoarthritis: 10-year follow-up. J Hand Surg Eur Vol. 2019;44(2):138-145. [DOI] [PubMed] [Google Scholar]
- 9. Kapandji A. Bioméchanique des articulations trapézo-métacarpienne et scapho-trapézienne. In: Saffar P. ed. La rhizarthrose, monographies du groupe d’études de la main. Paris, France: Expansion Scientifique Française; 1990:30. [Google Scholar]
- 10. Dell PC, Brushart TM, Smith RJ. Treatment of trapeziometacarpal arthritis: results of resection arthroplasty. J Hand Surg Am. 1978;3(3):243-249. [DOI] [PubMed] [Google Scholar]
- 11. Spaans A, van Minnen LP, Weijns ME, et al. Retrospective study of a series of 20 ivory prostheses in the treatment of trapeziometacarpal osteoarthritis. J Wrist Surg. 2016;5(2):131-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kapandji TG, Kapandji AI. New radiologic data on the trapezo-metacarpal joint. The results of 330 cases. Ann Chir Main Memb Super. 1993;12(4):263-274. [DOI] [PubMed] [Google Scholar]
- 13. Taleisnik J. The Wrist. New York, NY: Churchill Livingstone, 1985. [Google Scholar]
- 14. Regnard P-J. Electra trapezio metacarpal prosthesis: results of the first 100 cases. J Hand Surg Br. 2006;31(6):621-628. [DOI] [PubMed] [Google Scholar]
- 15. Lemoine S, Wavreille G, Alnot JY, et al. Second generation GUEPAR total arthroplasty of the thumb basal joint: 50 months follow-up in 84 cases. Orthop Traumatol Surg Res. 2009;95(1):63-69. [DOI] [PubMed] [Google Scholar]
- 16. Toffoli A, Teissier J. MAÏA trapeziometacarpal joint arthroplasty: clinical and radiological outcomes of 80 patients with more than 6 years of follow-up. J Hand Surg Am. 2017;42:838.e1-838.e8. [DOI] [PubMed] [Google Scholar]
- 17. Rubino M, Civani A, Pagani D, et al. Trapeziometacarpal narrow pseudarthrosis: a new surgical technique to treat thumb carpometacarpal joint arthritis. J Hand Surg Eur Vol. 2013;38(8):844-850. [DOI] [PubMed] [Google Scholar]
- 18. Armstrong AL, Oborne J, Coupland CA, et al. Effects of hormone replacement therapy on muscle performance and balance in post-menopausal women. Clin Sci (Lond). 1996;91(6):685-690. [DOI] [PubMed] [Google Scholar]
- 19. Cooney WP, 3rd, Chao EY. Biomechanical analysis of static forces in the thumb during hand function. J Bone Joint Surg Am. 1977;59(1):27-36. [PubMed] [Google Scholar]
- 20. Robles-Molina MJ, Lopez-Caba F, Gomez-Sanchez RC, et al. Trapeziectomy with ligament reconstruction and tendon interposition versus a trapeziometacarpal prosthesis for the treatment of thumb basal joint osteoarthritis. Orthopedics. 2017;40(4):e681-e686. [DOI] [PubMed] [Google Scholar]
- 21. Cebrian-Gomez R, Lizaur-Utrilla A, Sebastia-Forcada E, et al. Outcomes of cementless joint prosthesis versus tendon interposition for trapeziometacarpal osteoarthritis: a prospective study. J Hand Surg Eur Vol. 2019;44:151-158. [DOI] [PubMed] [Google Scholar]
- 22. Ulrich-Vinther M, Puggaard H, Lange B. Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J Hand Surg Am. 2008;33(8):1369-1377. [DOI] [PubMed] [Google Scholar]
- 23. Vandenberghe L, Degreef I, Didden K, et al. Long term outcome of trapeziectomy with ligament reconstruction/tendon interposition versus thumb basal joint prosthesis. J Hand Surg Eur Vol. 2013;38(8):839-843. [DOI] [PubMed] [Google Scholar]