Abstract
Background: Our group previously developed an upper extremity repositioning (Sup-ER) protocol for brachial plexus birth injuries (BPBIs) that may improve supination and external rotation (ER) at 2 years of age. Questions were raised about the potential for the protocol to cause internal rotation (IR) deficits. The goal of this study was to explore the longer-term outcomes of the Sup-ER protocol and investigate IR/ER function. Methods: This prospective cross-sectional cohort study examined 16 children older than 4 years of age with significant enough BPBI to be treated with the Sup-ER protocol. Total shoulder and elbow function were assessed, including passive and active ranges of motion and strength of IR and ER. Results: Range of motion (ROM) for most active movements was decreased in the affected compared to unaffected arm. Notably, IR passive ROM was similar in the affected (78.7°) and unaffected arm (82.8°). External rotation strength of the affected arm was weaker (42.8 N) compared to the unaffected arm (57.9 N). IR strength had a greater deficit in the affected (43.2 N) arm compared to the unaffected arm (72.2 N), but both ER and IR showed less deficit than described in the literature. Conclusions: Despite differences in ranges of motion between the affected and unaffected arms, ROMs for the affected arm were comparable to the functional limits as reported in the literature. The Sup-ER protocol shows potential to optimize long-term shoulder rotation function in children with BPBI without compromising IR.
Keywords: shoulder, anatomy, brachial plexus, nerve, diagnosis, pediatric, outcomes, research & health outcomes, treatment
Introduction
Shoulder dystocia may result in injury to the brachial plexus ranging from reversible neurapraxia to complete nerve root avulsion. These brachial plexus birth injuries (BPBIs) occur at a rate of 1.24 per 1000 live births in Canada. 1 Up to 88% of BPBIs reportedly result in very good recovery; however, more severe forms of BPBI will present with persistent functional deficits.2-4 Most centers employ a multidisciplinary treatment approach incorporating: physiotherapy, peripheral nerve surgery, and the use of orthoses. 5 Consensus regarding the optimal treatment of BPBI has yet to be achieved,5-15 and use of early positioning and splinting protocols is not universal.
Our center prioritizes early optimization of shoulder function. Currently accepted therapies include focused passive stretching and, if indicated, surgery. Early surgeries are focused on nerve repair and nerve transfers, and where required, shoulder relocation, whereas secondary surgeries are solely musculoskeletal in nature. Latissimus dorsi and teres major tendon transfers which promote the strengthening of external rotation (ER), may, however, result in internal rotation (IR) deficits.7,16
Growing bones and joints adapt to their load and range. Persistent muscle imbalance and weakness associated with BPBI may result in glenohumeral deformity and subluxation.17,18 To optimize normal anatomic growth and promote glenohumeral congruity during nerve recovery, our group previously developed an upper extremity repositioning program. In addition to physiotherapy, the program introduces early use of an orthosis that stabilizes the affected arm in forearm supination (Sup) and shoulder ER (Sup-ER). 14 The protocol algorithm outlines indications for the adjunctive use of orthoses, brachial plexus exploration and grafting, botulinum toxin injection, nerve transfers, tendon transfers, and osteotomies. Briefly, the key points of the Sup-ER protocol are summarized below:
If ER and/or supination Active Movement Scale 19 (AMS) scores are ≤ 2 at 4 to 8 weeks of age→ start Sup-ER orthosis at 6 to 8 weeks, in conjunction with physiotherapy. The group of patients with these measurements represent our most severe cases and include those with root avulsions and/or significantly injured trunks. Only 15% of our clinic population falls into the category where Sup-ER is recommended.
If at 1-month intervals, the shoulder remains reduced and AMS scores improve→ continue Sup-ER orthosis and physiotherapy until approximately 12 months of age as tolerated by the patient.
Brachial plexus exploration and grafting at 3 to 4 months of age where required for global or root avulsion injuries.
If ER passive range of motion (ROM) is limited and/or the shoulder shows signs of subluxation as early as 4 months→ Botulinum toxin and cast, or surgical reduction of the shoulder and cast, followed by Sup-ER splint over a longer time period is undertaken. More currently, we may also first use an elbow constraint band to try to encourage active external rotation and decrease the elbow forward posture, but most of the patients in this earlier cohort were not treated this way.
If ROM issues or shoulder joint malposition persist for several months despite these modalities, the patients are considered for more invasive interventions including nerve and tendon transfers. Generally, tendon transfer timing is considered less ideal before the age of 2 years, but decisions are made on an individual basis.
Findings of a pilot study demonstrated improved supination and ER of 12 patients who used the Sup-ER protocol, compared to controls at 2 years of age. 8 Concerns were recognized about the potential for a reduction of IR in patients using the protocol. The goal of this study was to measure shoulder ER and IR ROM and strength in the affected arm compared to the unaffected side in patients who had used the protocol.
Methods
This prospective cross-sectional cohort study was approved by the University of British Columbia Children’s and Women’s Health Centre of British Columbia Research Ethics Board (study ID: H18-01006). All parents provided written informed consent and all children over the age of 7 provided written informed assent.
Study Participants
Study participants were identified from the British Columbia Children’s Hospital (BCCH) Brachial Plexus Clinic database, which included all patients that have been evaluated by the Brachial Plexus Clinic team. BPBI patients who used the Sup-ER protocol and were at least 4 years of age at the time of the study were invited to participate. Four years was determined as the minimum appropriate age for compliance with functional scales used in the study visit. Patients lost to follow-up, no longer living in the province, or those unable to complete the study assessment due to lack of cooperation (eg, severe developmental delay) were excluded.
Study Assessments
Patients who consented to participate had their chart reviewed and attended a single 1-hour study visit. Past medical history, specific procedures, and details of Sup-ER orthosis use including complications and documented compliance where available, were obtained from each participant’s clinical chart. Based on the Sup-ER splint time period and post-Botox casting duration, the Sup-ER Protocol for each participant was recorded as shorter than regular (splint started after 20 weeks of age, or used for 4 or less months and/or cast < 3 weeks), regular (splint started by 20 weeks of age and used for 5-10 months and/or cast 3-5 weeks), longer than regular (splint started by 20 weeks of age and used for >10 months and/or cast >5 weeks), or not followed (splint started after 12 months of age).
The study visit assessed (in order): ABC Loops, modified Mallet scale, active and passive ROM for IR and ER, strength of IR and ER at mid-range, then the passive and active ranges of motion of supination, pronation, elbow flexion and elbow extension.20,21 The IR and ER results are discussed in this article.
Individual assessments were always first performed on the unaffected arm. Using a standardized script, each motion was introduced to the participant by verbal and visual demonstration, then if needed, positive reinforcement (by asking the participant to reach for a prize), and lastly, physical guidance through a brief (10°-15°) range before asking the patient to perform it independently. If the participant was unable to perform the movement following these steps the outcome of the test was recorded as a failure. All measurements were performed by the same physiotherapist (D.B.) and trained clinical evaluator (L.S.Y.) for all participants.
ROM
Measuring objective rotation at the shoulder is difficult because of 3-dimensional compensation involving elbow extension and trunk positioning, and difficulty defining the point of rotation. To decrease this effect, we created a stable tabletop base securing the elbow to a rotating disk in an attempt to isolate testing to true rotational movement and allow a more objective comparison to the control arm (Supplementary Figures 3 and 4).
Shoulder IR and ER movements were performed elbow down (vs. shoulder abducted to 90°) to represent more common functional movements (eg, buttoning a blouse) requiring no assumptions of normal abduction function. 22 All measurements were taken with the participant standing in the cut-out of the tabletop. The trunk was stabilized by an assistant to minimize compensatory movements. The elbow was flexed to 90°, and the shoulder abducted just enough that the thenar eminence would align with the participant’s umbilicus at maximum available IR with elbow flexed. The elbow was secured into position on the rotating disk with the support of a Velcro sensitive neoprene arm cuff. A goniometer was used to measure ROM with the vertex at the center of the disk and the zero line representing forearm pointing forward (Supplementary Figures 3 and 4). Compensatory movements were minimized by evaluators.
Strength
Upper extremity strength was evaluated 1 minute after the ER/IR ROM assessment. While maintaining the elbow in the cuff, a “neutral rotation point” was defined for that patient as the midpoint between the previously determined IR and ER maximal range. Strength was measured at this position using a make test with a hand-held dynamometer (Commander™ Muscle Tester) and reported in Newtons. The dynamometer pad was placed 4 cm proximal to the thenar eminence for IR, and 4 cm proximal to the ulnar styloid for ER. The participants were given an opportunity to perform a sub-maximal effort test to familiarize them with the movement and scripted instructions as previously described. The participants were given 3 trials to perform the test with maximal effort, with 5 seconds of rest between each repetition. The greatest value measured was used for analyses.
Statistical Analysis
The data were analyzed descriptively. The Wilcoxon signed-rank test was used to assess the differences in the population means between the strength and ROM of the participants’ affected and unaffected sides. The level of significance was set at P < .05. The R statistical language (version 3.5.1) with ggplot2 graphics package (version 3.0.0), and MATLAB® (MATLAB version 9.3.0 [R2017b]. Natick, Massachusetts: The MathWorks Inc.) were used for statistical analysis and figure production.
Results
This study invited 32 children (4-11 years old) treated with the Sup-ER protocol to join the study. Seventeen children participated, yielding a 53% recruitment rate. One child with autism later withdrew due to severe cooperation issues during the assessment. The final cohort included 16 participants, 13 females, and 3 males. The mean age of the participants was 7.0 years of age (range: 4.5-11.6 years). Past medical history revealed that 12 of the 16 participants had undergone at least one additional procedure in addition to physiotherapy and the Sup-ER protocol (Table 1).
Table 1.
Patient Characteristics.
| Characteristic | No. (%) ‡ |
|---|---|
| N | 16 |
| Age, mean (SD) | 6.4 (2.2) |
| Sex | |
| F | 13 (81.2) |
| M | 3 (18.8) |
| Affected side | |
| L | 7 (43.8) |
| R | 9 (56.2) |
| Handedness | |
| L | 5 (31.2) |
| R | 11 (68.8) |
| Procedures | |
| Brachial plexus exploration and grafting | 5 (31.2) |
| Botulinum toxin injection | 7 (43.8) |
| Nerve transfers | 5 (31.2) |
| Tendon transfers | 6 (37.5) |
| Osteotomies | 1 (6.2) |
F = female; M = male; L = left; R = right.
Unless otherwise indicated.
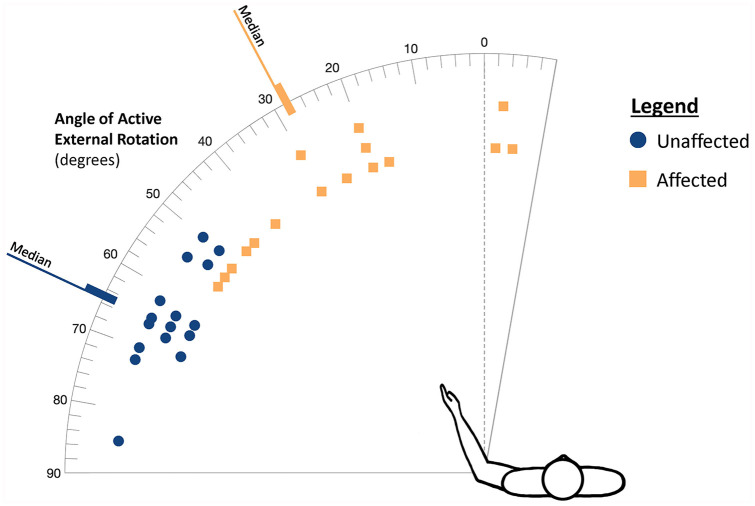
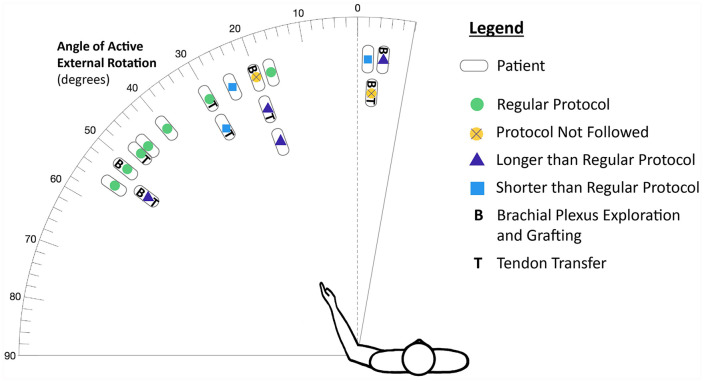
The greatest statistically significant difference between the affected and unaffected side ROM was in ER, both active (P < .001) and passive (P = .003). The median active ER ROM was 27.5° (range: -5°-55°) in the affected arm and 65.0° (range: 50°-85°) in the unaffected arm. The median passive ER ROM was 46.0° (range: 22°-83°) in the affected arm and 67.0° (range: 53°-85°) in the unaffected arm (Figures 1-2 and Supplementary Figure 1).
Figure 1.
Active external rotation: Unaffected vs. affected arm.
Figure 2.
Active external rotation of the affected arm.
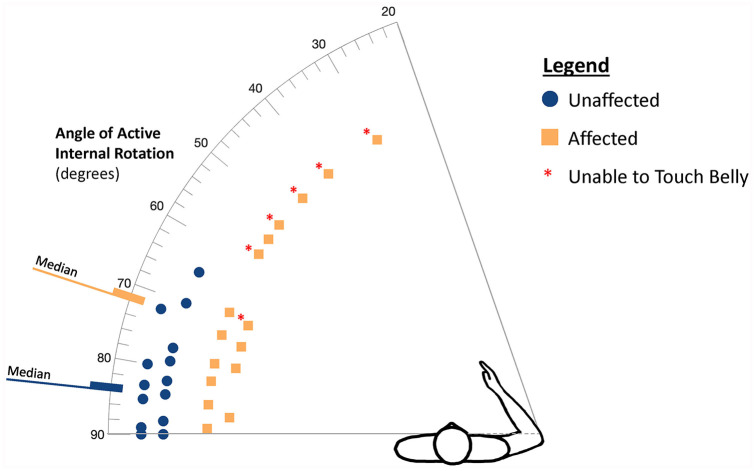
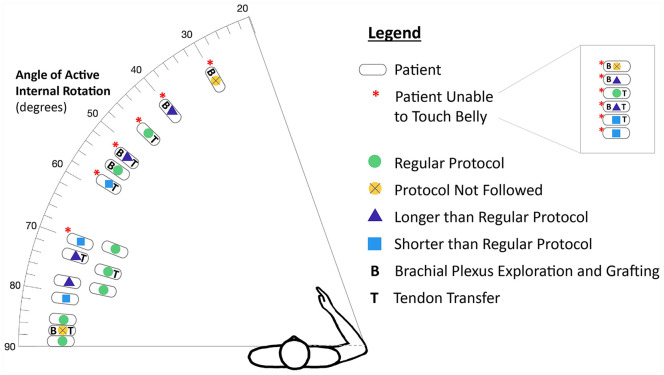
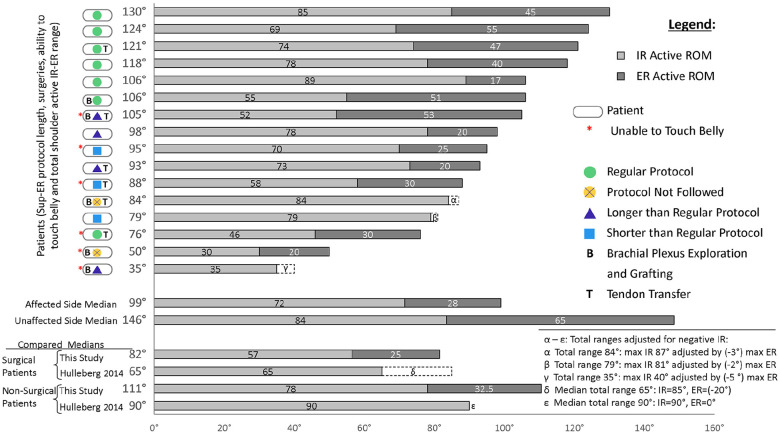
The affected arm had a median passive IR ROM of 80.0° (range: 65°-89°) vs. 84.5° (range: 65°-92°) in the unaffected arm, which was not statistically significant (P = .055). The median active IR ROM was 71.5° (range 30°-89°) in the affected arm and 83.5° (range: 65°-92°) in the unaffected arm, which was statistically different (P = .004). Six participants could not touch their belly when the affected elbow was stabilized in the standardized position on the Velcro disk. Factors or treatments that could possibly impact passive or active IR function were also plotted (Figures 3-4 and Supplementary Figure 2). It should be noted that 3 of the unaffected arm maximum IR active range measurements were equal to or less than the median affected range, demonstrating the degree of constraint of the measurement device.
Figure 3.
Active internal rotation: Unaffected vs. affected arm.
Figure 4.
Active internal rotation of the affected arm.
Mean strength in IR was 43.2 N (±15.1 N) in the affected arm and 72.2 N (±22.8 N) in the unaffected arm, a difference which was statistically significant (P < .001). Mean strength in ER was 42.8 N (±20.9 N) in the affected, and 57.9 N (±19.0 N) in the unaffected arm (P = .007) (Table 2).
Table 2.
Internal and external rotation strength outcomes.
| Unaffected arm mean strength (N) (SD) | Affected arm mean strength (N) (SD) | Mean relative strength of affected arm (%) (95% CI) | P-value | |
|---|---|---|---|---|
| Internal Rotation | 72.2 (22.8) | 43.2 (15.1) | 62.0 (54.4-69.6) | <.001 |
| External Rotation | 57.9 (19.0) | 42.8 (20.9) | 73.8 (59.0-88.6) | .007 |
Median strength in IR was 35.2 N in the affected arm and 70.4 N in the unaffected arm. Median strength in ER was 39.6 N in the affected, and 58.3 N in the unaffected arm (Table 2).
Discussion
By study criteria, our population included only our most severe BPBI patients; we anticipated and found that affected arms had reduced ROM and strength compared to unaffected arms. Normative literature published by Gates et al, 23 suggests there is an ability for young adults to undertake activities of daily living at a normal level with ER of 55°, and IR of 79°. That study measured rotation in free space with motion capture, and without specifically constraining compensatory rotation of the trunk.
In affected arms in our group, the median active ER (28°) and IR (72°) were below these thresholds, although the amount of disparity may be exaggerated by our more strictly constrained measurement of rotation. Even in healthy arms in our study, the median active ER was 65° and IR was 84° where we would have previously expected these would approach 90° in this age group. Therefore, our ER/IR ranges may not be completely comparable to published literature. As we aimed to measure pure rotation with comparisons to self, if anything, our measurements may underreport any improvements.
In the most comparable BPBI article we identified, Hulleberg et al 24 describe median active IR of 85° in operated patients and 90° in un-operated patients between 10 and 20 years of age, which was greater than our findings of 57° and 78°.
However, the median active ER in our treatment population was 28°, objectively more than the -20° and 0° found in Hulleberg’s patients, and again, device constraint may be underestimating the disparity of this comparison. No patient in their study population achieved active ER > 15°, whereas in our group, 13/16 achieved 17° or greater, with the maximum active ER recorded being 55°.
Additionally, the median active total IR to ER range of patients in our study was greater than that of Hulleberg, (Figure 5). Our constrained IR mean and median values measured only slightly less but our ER improvement was notably better, in both operated and nonoperated patients.
Figure 5.
Active total internal rotation and external rotation ROM.
When we looked for more granular details related to active IR, we could not identify any pattern of treatment that was common to the patients who could not touch their belly, or was different to those who could. Three of them had undergone tendon transfers (identical to the number of tendon transfers in the group who could touch their belly), 3 had brachial plexus exploration (nearly identical to the group who could touch their belly), 2 had shorter than regular Sup-ER protocol, 2 had longer than regular protocol, and 1 did not start the protocol before 1 year of age. All 6 patients had different overall treatment combinations. However, of the 7 patients who followed the regular Sup-ER protocol, only one could not touch their belly, and that patient also had tendon transfers. Although the majority of participants who could touch their belly had followed a regular Sup-ER protocol (6 out of 10), and the majority of the participants who could not touch their belly had not followed a regular Sup-ER protocol (5 of 6), it would require a much larger data set to assign any statistical or conclusive significance to any of the individual factors or to the Sup-ER program itself.
IR Strength
We have previously documented decreased strength of IR in the majority of our recovered patients, even in the presence of IR contractures. 25 This is consistent with the literature.24,26
Our current study found reduced strength outcomes comparable to those previously reported in the literature.24,26 Median IR in affected arms was 38% weaker than unaffected arms (Table 2), better than Brochard et al, who found a 49% median decrease, and comparable to the Hulleberg study which showed 39% median strength reduction in operated patients and 17% reduction in nonoperated patients.24,26
Even when participants maintained the IR ROM required to touch their abdomen, their overall strength was diminished. This is very important to note when considering secondary shoulder rebalancing procedures. Prior to shoulder tendon transfers, formal measurement of IR strength is recommended to avoid potentially unbalanced outcomes.
ER Strength
Our ER strength deficits are dramatically less than those reported in the literature. In our study cohort, the median ER strength in the affected arm was 20% weaker than the unaffected, compared to Brochard’s 73% weakness, and 45% and 73% weakness in Hulleberg’s nonoperated and operated patients with permanent lesions.24,26 We cannot rule out that the greater strength deficit found by Brochard et al 26 and Hulleberg et al 24 may be due to deconditioning or age-related factors, as the average age of the children from the aforementioned studies was 11.2 years and 14, respectively, whereas the mean age in our study cohort was 6.4 years.
Study limitations
One of the limitations of our study is its small sample size, which makes it difficult to assign statistical significance. This cross-sectional cohort study recruited study participants by invitation, which increases the likelihood of a self-selection sampling bias. Therefore, our sample may not be representative of the entire population. By study design, we cannot include patients who did not consent to participate, but we scanned the nonparticipant global scores in our database, and found no major outliers, or reason to suspect that “worse” patients were hidden in that group. In fact, none of them had undergone surgery, and one third of them had not a single AMS score below 6 on their most recent evaluation.
The Sup-ER protocol notably continued to evolve and develop during the time period the study participants were treated. Individualized application of the protocol and heterogeneity of the already limited population may also serve as confounding factors in our study.
Accurate measurement of IR and ER in children can be challenging. We designed a measurement table in an attempt to assess IR and ER ROM and strength in an objective and standardized manner (Supplementary Figures 3 and 4). Of note, even unaffected side measurements were less than usual expectations, thus this technique may underrepresent our study’s positive findings. Additionally, while this measurement technique has not been validated, inconsistency in techniques described in current literature makes comparisons difficult.
Conclusion
In this study, participants treated with the Sup-ER protocol were shown to have affected-arm reduction in rotational ROM and rotational strength compared to their unaffected arm, as expected for the severity of their injury. Compared to the literature, participants who used the Sup-ER protocol were shown to have much improved ER strength and ROM. Even with measurements potentially reduced by the constraints of our tool, total IR to ER range was greater than values reported in the literature, where less standardized measurement techniques may have been used. A subset of participants could not touch their belly in our ROM assessment. This subset population was disparate. No causative treatment variation or pattern could be identified, including use of the Sup-ER protocol. In study participants, IR strength of the affected side was diminished compared to the unaffected side, as expected, but comparable to or greater than the IR strength in children with BPBIs reported in the literature. The best outcomes in total shoulder rotation range were achieved in participants who undertook the “normal” regular Sup-ER protocol length of treatment.
This pilot study supports the efficacy of the Sup-ER protocol without compromising shoulder IR ROM or strength. The need for consistent documentation of both shoulder and elbow ROM and strength is emphasized to guide therapeutic initiatives and support research endeavors.
Supplemental Material
Supplemental material, Supplementary_Figure_1 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_Figure_2 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_Figure_3 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_Figure_4 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_figure_and_table_legends for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_material for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_Table_1 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Acknowledgments
The authors would like to acknowledge Iris Liu for her work on the graphic designs of the figures.
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (UBC C&W Research Ethics Board) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients and their parents for being included in the study.
Statement of Informed Consent: This study included pediatric population. Informed consent was obtained from all individual participants’ parents and assent was obtained from all children over the age of 7.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by a UBC Plastic Surgery Academic grant. L.S.Y. received a UBC Summer Student Research Program grant. R.C. and M.B. declare that they are working full time as clinical research coordinators for UBC. As part of their employment, they worked on this study and received pay from UBC, but do not declare conflict of interest. D.B., K.D., S.H., and C.V. received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Leeor S. Yefet  https://orcid.org/0000-0003-1504-1772
https://orcid.org/0000-0003-1504-1772
Cynthia Verchere  https://orcid.org/0000-0002-8284-1975
https://orcid.org/0000-0002-8284-1975
References
- 1. Coroneos CJ, Voineskos SH, Coroneos MK, et al. Obstetrical brachial plexus injury: burden in a publicly funded, universal healthcare system. J Neurosurg Pediatr. 2016;17(2):222-229. doi: 10.3171/2015.6.PEDS14703. [DOI] [PubMed] [Google Scholar]
- 2. Chauhan SP, Rose CH, Gherman RB, et al. Brachial plexus injury: a 23-year experience from a tertiary center. Am J Obstetr Gynecol. 2005;192(6):1795-1800. doi: 10.1016/j.ajog.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 3. Lagerkvist A-L, Johansson U, Johansson A, et al. Obstetric brachial plexus palsy: a prospective, population-based study of incidence, recovery, and residual impairment at 18 months of age. Develop Med Child Neurol. 2010;52(6):529-534. doi: 10.1111/j.1469-8749.2009.03479.x. [DOI] [PubMed] [Google Scholar]
- 4. Hoeksma AF, Wolf H, Oei SL. Obstetrical brachial plexus injuries: incidence, natural course and shoulder contracture. Clin Rehabil. 2000;14(5):523-526. doi: 10.1191/0269215500cr341oa. [DOI] [PubMed] [Google Scholar]
- 5. Coroneos CJ, Voineskos SH, Christakis MK, et al. Obstetrical brachial plexus injury (OBPI): Canada’s national clinical practice guideline. BMJ Open. 2017;7(1):e014141. doi: 10.1136/bmjopen-2016-014141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Raducha JE, Cohen B, Blood T, et al. A review of brachial plexus birth palsy: injury and rehabilitation. Rhode Island Med. 2017;100(11):17-21. [PubMed] [Google Scholar]
- 7. Erel S, Şimşek İE, Ayhan Bek ÇN, et al. An adjustable shoulder abduction orthosis for the post-operative management of tendon transfers: a preliminary study. Prosthet Ortho Int. 2008;32(2):129-135. doi: 10.1080/03093640802015755. [DOI] [PubMed] [Google Scholar]
- 8. Verchere C, Durlacher K, Bellows D, et al. An early shoulder repositioning program in birth-related brachial plexus injury: a pilot study of the sup-ER protocol. HAND. 2014;9(2):187-195. doi: 10.1007/s11552-014-9625-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vuillermin C, Bauer AS. Boston Children’s Hospital approach to brachial plexus birth palsy. J Pediatr Orthop. 2016;25(4):296-304. doi: 10.1097/BPB.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 10. Abid A. Brachial plexus birth palsy: management during the first year of life. Orthop Traumatol Surg Res. 2016;102(1):S125-S132. doi: 10.1016/j.otsr.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 11. Torode I, Donnan L. Posterior dislocation of the humeral head in association with obstetric paralysis. J Pediatr Orthop. 1998;18(5):611-615. [DOI] [PubMed] [Google Scholar]
- 12. Safoury YA, Eldesoky MT, Abutaleb EE, et al. Postoperative physical therapy program for latissimus dorsi and teres major tendons transfer to rotator cuff in children with obstetrical brachial plexus injury. Euro J Phys Rehabil Med. 2017;53(2):277-285. doi: 10.23736/S1973-9087.16.03910-1. [DOI] [PubMed] [Google Scholar]
- 13. Ramos LE, Zell JP. Rehabilitation program for children with brachial plexus and peripheral nerve injury. Sem Pediatr Neurol. 2000;7(1):52-57. doi: 10.1016/S1071-9091(00)80010-8. [DOI] [PubMed] [Google Scholar]
- 14. Durlacher KM, Bellows D, Verchere C. Sup-ER orthosis: an innovative treatment for infants with birth related brachial plexus injury. J Hand Therapy. 2014;27(4):335-340. doi: 10.1016/j.jht.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 15. Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop. 2005;25(1):116-126. [DOI] [PubMed] [Google Scholar]
- 16. Pearl ML, Edgerton BW, Kazimiroff PA, et al. Arthroscopic release and latissimus dorsi transfer for shoulder internal rotation contractures and glenohumeral deformity secondary to brachial plexus birth palsy. J Bone Joint Surg-Am Vol. 2006;88(3):564-574. [DOI] [PubMed] [Google Scholar]
- 17. Gharbaoui IS, Gogola GR, Aaron DH, et al. Perspectives on glenohumeral joint contractures and shoulder dysfunction in children with perinatal brachial plexus palsy. J Hand Therapy. 2015;28(2):176-184. doi: 10.1016/j.jht.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 18. Waters PM, Smith GR, Jaramillo D. Glenohumeral deformity secondary to brachial plexus birth palsy. J Bone Joint Surg. 1998;80(5):668-677. doi: 10.2106/00004623-199805000-00007. [DOI] [PubMed] [Google Scholar]
- 19. Curtis C, Stephens D, Clarke HM, et al. The active movement scale: an evaluative tool for infants with obstetrical brachial plexus palsy. The Journal of Hand Surgery. 2002;27(3):470-471. doi: 10.1053/jhsu.2002.32965. [DOI] [PubMed] [Google Scholar]
- 20. Mallet J. [Obstetrical paralysis of the brachial plexus. II. Therapeutics. Treatment of sequelae. Priority for the treatment of the shoulder. Method for the expression of results]. Rev Chir Orthop Reparatrice Appar Mot. 1972;58(Suppl. 1):166-168. [PubMed] [Google Scholar]
- 21. Pearl ML, van de Bunt F, Pearl M, et al. Assessing shoulder motion in children: age limitations to mallet and ABC loops. Clin Orthop Relat Res. 2014;472(2):740-748. doi: 10.1007/s11999-013-3324-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Blaauw G, Muhlig RS. Measurement of external rotation of the shoulder in patients with obstetric brachial plexus palsy. J Brachial Plex Peripher Nerve Inj. 2012;7:8. doi: 10.1186/1749-7221-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gates DH, Walters LS, Cowley J, et al. Range of motion requirements for upper-limb activities of daily living. Am J Occup Ther. 2016;70(1):7001350010. doi: 10.5014/ajot.2016.015487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hulleberg G, Elvrum A-KG, Brandal M, Vik T. Outcome in adolescence of brachial plexus birth palsy. Acta Orthopaedica. 2014;85(6):633-640. doi: 10.3109/17453674.2014.964614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bellows D, Bucevska M, Verchere C. Coordination and balance in children with birth-related brachial plexus injury: a preliminary study. Physiother Can. 2015;67(2):105-112. doi: 10.3138/ptc.2013-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brochard S, Alter K, Damiano D. Shoulder strength profiles in children with and without brachial plexus palsy. Muscle Nerve. 2014;50(1):60-66. doi: 10.1002/mus.24099. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_Figure_1 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_Figure_2 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_Figure_3 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_Figure_4 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_figure_and_table_legends for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_material for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND
Supplemental material, Supplementary_Table_1 for Shoulder Rotation Function following the Sup-ER Protocol in Children with Brachial Plexus Injuries by Leeor S. Yefet, Doria Bellows, Marija Bucevska, Rebecca Courtemanche, Kim Durlacher, Sally Hynes and Cynthia Verchere in HAND