Abstract
Background: The treatment of rhizarthritis involves several surgical techniques; among them, bioabsorbable scaffolds have begun to be proposed to avoid the use of other biological tissues or artificial permanent devices. Methods: In this study, we evaluated the long-term outcomes of poly-ld-lactic acid scaffold in interposition arthroplasty in a series of patients treated in our department. Results: Strength, range of motion, and pain improved after the intervention and lasted over the years; nonetheless, most of the radiographs showed a progressive collapse of the first metacarpal. Conclusions: Despite radiological findings, we believe that poly-ld-lactic acid scaffold can be considered a good alternative to traditional trapeziectomy with tendon interposition and suspensionplasty, with long-lasting satisfactory clinical results.
Keywords: biomaterials, interposition arthroplasty, joint scaffold, poly-ld-lactic acid, rhizarthritis
Introduction
Arthritis of the trapeziometacarpal joint is one of the most common causes of hand pain and dysfunction. It mainly affects middle-aged women and manual workers, causing problems and difficulties in working and daily activities. Various etiological theories have been proposed, including age, hormonal factors, ligamentous laxity with consequent instability, and early cartilage wear.1,2
Usually, nonoperative treatment with splints, physiotherapy, and intra-articular injections is used in the initial phases of trapeziometacarpal arthritis, whereas surgery is considered in advanced stages when the conservative approach has been ineffective.3,4 Several surgical techniques ranging from trapeziectomy to the more recent prosthetic implants have been reported in the literature.5-9
During the last decades, many new materials have been developed to act as structural support in the initial phases and then be resorbed in a later period. The use of these biological spacers was thought to preserve other biological tissues like tendons for interposition-suspensionplasty and avoid the implant of permanent artificial devices to decrease comorbidity.10-12 They consist of cylinders of different sizes, made of poly-ld-lactic acid (PLDLA) multifilaments. Variable short- and medium-term results for the treatment of trapeziometacarpal joint with PLDLA scaffold have been reported in the literature,13-16 but until now, to our knowledge, no studies have investigated the long-term results of this biological spacer.
The aim of our study was to reevaluate at a long-term follow-up clinical and radiological results in a group of patients undergoing carpometacarpal (CMC) arthroplasty with a PLDLA scaffold (RegJoint) in the Department of Hand and Microsurgery of the University Hospital Policlinico of Modena to confirm the maintenance over the years of the positive results showed in a previous short-term investigation.
Materials and Methods
From November 2004 to June 2006, 25 patients with trapeziometacarpal arthritis were treated with the PLDLA scaffold in our department by a single surgeon with the same surgical technique. These patients were already subjected to a short-term evaluation in 2006 by the same authors.
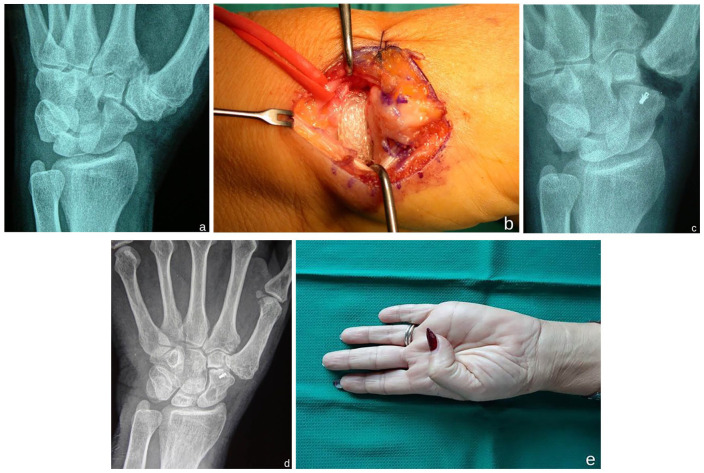
Figure 1.
(a) Preoperative radiograph, (b) positioning of the scaffold after trapeziectomy, (c) immediate postoperative radiograph, (d) radiograph at final follow-up, and (e) clinical recovery.
The patients were contacted by phone and invited to undergo a clinical and radiological check. Some patients (6) were unreachable, and others (9) refused to return to control because of the distance and difficulty to travel due to elderly age. For this reason, a relevant number of patients were lost to follow-up (15 of 25). For this study, we were then finally able to review 10 of the 25 patients of the initial case series, with a mean follow-up of 13.6 (range = 12-15) years. All the patients reviewed were middle-aged women at the time of surgery, with a mean age of 51.5 (range = 40-63) years.
Grip strength and pinch strength were evaluated with the Jamar and pinch tests. Grip strength was measured using the Jamar grip dynamometer (Lafayette Instrument Co, Lafayette, Indiana). Pinch strength was measured using the hydraulic pinch gauge (Lafayette Instrument Co). The range of motion of the thumb was graded according to the Kapandji test. 17 Subjective perception of pain was assessed using the visual analog scale (VAS) with no intermediate marking.
The radiological evolution of surgical procedure was evaluated by measuring the residual space between the base of the first metacarpal and the distal pole of the scaphoid on standard radiographs. We compared these evaluations with preoperative values obtained from hospital records to verify whether the long-term outcomes confirmed the clinical improvement achieved after surgery. We did not per-form a comparative statistical analysis with other surgical techniques, but only a comparison between early and final results of the use of PLDLA scaffold for the treatment of trapeziometacarpal arthritis.
Figure 2.
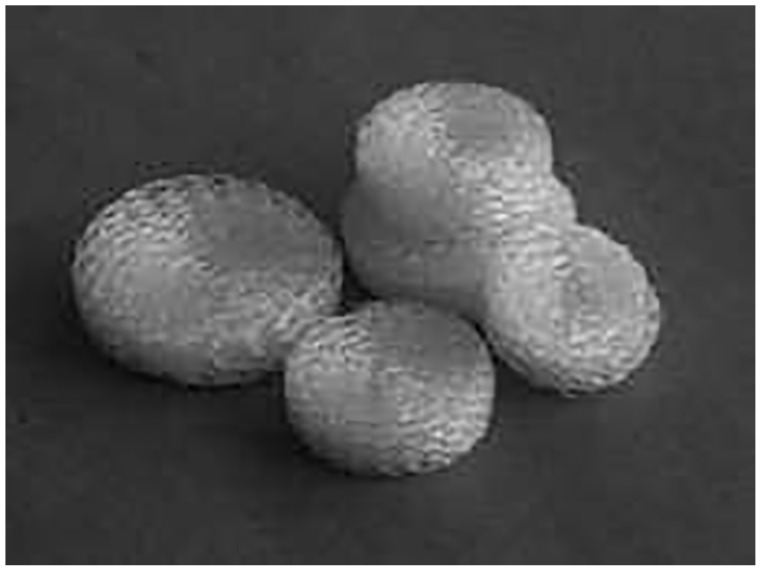
Poly-ld-lactic acid copolymer scaffold.
Results
A relevant improvement of the grip strength measured with the Jamar dynamometer was observed at the late visit. The average value was 16.8 kg at the preoperative evaluation, passing to 24 kg at the long-term follow-up (increase of 42.8%). Similarly, the key pinch passed from 4.2 to 5.42 kg (increase of 29%) and the tip pinch from 2.8 to 3.2 kg (increase of 14.2%) at the final visit.
The opposition of the thumb values with the Kapandji test improved from 7 to 8. The most positive results were observed for pain relief. Subjective perception of pain passed from 7.5 to 2.3 at the VAS scale, with important and lasting pain relief in these patients.
Despite this, the radiological findings were somewhat disappointing. The measurement of the articular space between the base of the first metacarpal and the distal pole of the scaphoid showed an average loss of height of 81.4%, passing from a mean value of 5.4 mm in the immediate postoperative visit to less than 1 mm at the final follow-up, with a complete collapse in 50% of the cases (Table 1). None of the patients included in this study underwent revision surgery.
Table 1.
Clinical and Radiological Findings (Mean) of Patients Evaluated at a Long-term Follow-up.
| Preoperatively | Immediate postoperatively | Final follow-up | Variation % | |
|---|---|---|---|---|
| Jamar, kg | 16.8 | 24 | +42.8 | |
| Key, kg | 4.2 | 5.42 | +29 | |
| Tip, kg | 2.8 | 3.2 | +14.2 | |
| Kapandji | 7.6 | 8.2 | +7.8 | |
| Visual analog scale | 7.5 | 2.3 | −69.3 | |
| Articular space, mm | 5.4 | 1 | −81.4 |
Discussion
In this article, we reevaluated at long-term follow-up a clinical series of patients operated on in our department to verify clinical and radiological evolution of PLDLA scaffolds (RegJoint) implanted for trapeziometacarpal arthritis. In a previous study performed by the same authors with short-term follow-up, clinical results had been very encouraging, with a significant increase in grip and pinch strength in the scaffold group, compared with controls, and a global improvement in pain and hand function. 18 At this long-term follow-up evaluation, we noticed that these results had been satisfactory over the time. Mobility, strength, and global function of the hand were satisfactory, and the pain relief was remarkable with a settlement of the VAS score to the lowest values.
The radiological findings, however, were disappointing, with an almost complete collapse of the metacarpal base on the distal pole of the scaphoid in more than 80% of the patients. Then the hypothetical substitution of the scaffold with fibrous tissue did not allow the formation of a permanent scar tissue able to support the first metacarpal after scaffold resorption. However, these results did not correspond with clinical outcomes that were very satisfactory in our long-term experience.
In the literature, we found contrasting results about the use of PLDLA scaffolds (RegJoint) for trapeziometacarpal arthritis. Two studies conducted by Mattila et al at a short- and medium-term follow-up reported some adverse tissue reactions related to the degradation process of the implant.14,15 The authors reported some degree of osteolysis in most of the patients, cases of foreign body reactions in about one-third, and need for surgical revision in 3 patients.
In contrast, a recent study by Kennedy et al 13 reported very good clinical results at a medium-term follow-up (mean, 36 months) in a group of 16 patients with 19 (RegJoint) implants for thumb metacarpophalangeal joint arthritis. Notably, they did not observe soft tissue reaction and bone erosion. As observed in our experience, they reported very good clinical outcomes in grip and pinch strength, in Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) score with similar range of motion compared with contralateral side. The authors also showed that there was no correlation between the QuickDASH and VAS score with residual joint space, CMC subluxation ratio, and postoperative bone erosion. As in our case series, no patients underwent surgical revision. This is an encouraging data because despite the limited number of patients included in our long-term follow-up series, they confirmed the safety and effectiveness of surgical procedure.
A recent critical literature review published by Gottschalk et al 19 investigated current treatment options for basilar thumb arthritis. According to the authors, trapeziectomy, trapeziectomy with distraction arthroplasty, and trapeziectomy with ligament tendon reconstruction interposition (LTRI) are the surgical techniques supported by good evidence (level I studies with consistent findings) for recommending intervention. On the contrary, long-term results of implant arthroplasty continue to demonstrate a high complication rate. Poly-ld-lactic acid scaffold (RegJoint) in CMC arthroplasty is a temporary porous support positioned in resected joint space that promotes scar tissue ingrowth and dense fibrous pseudoarthrosis acting like a spacer. The scaffold is implanted without ligament tendon suspensionplasty, and this technique may be considered similar to trapeziectomy and trapeziectomy with distraction arthroplasty that are also supported by good evidence (level I studies with consistent findings) for recommending intervention.
Our studies had several limitations. The number of patients included in this series was limited, and most of the initial cases were lost to follow-up. Statistical analysis on such a small number of patients would have had limited value. Moreover, we could not compare our data with other common and reliable surgical techniques for CMC thumb arthritis like trapeziectomy and trapeziectomy with LTRI supported by literature review.
Our clinical experience showed that the PLDLA scaffold in the treatment of the rhizarthritis may represent a good surgical option in long-term follow-up. Nevertheless, long-term studies on larger case series and comparative investigations with higher level of evidence should be conducted to clearly ascertain the appropriateness and effectiveness of this implant.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Giulia Colzani  https://orcid.org/0000-0002-3885-3178
https://orcid.org/0000-0002-3885-3178
References
- 1. Armstrong AL, Hunter JB, Davis TR. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg Br. 1994;19(3):340-341. [DOI] [PubMed] [Google Scholar]
- 2. Edmunds JO. Current concepts of the anatomy of the thumb trapeziometacarpal joint. J Hand Surg Am. 2011;36(1):170-182. [DOI] [PubMed] [Google Scholar]
- 3. Spaans AJ, van Minnen LP, Kon M, et al. Conservative treatment of thumb base osteoarthritis: a systematic review. J Hand Surg Am. 2015;40:16-21. [DOI] [PubMed] [Google Scholar]
- 4. Berggren M, Joost-Davidsson A, Lindstrand J, et al. Reduction in the need for operation after conservative treatment of osteoarthritis of the first carpometacarpal joint: a seven year prospective study. Scand J Plast Reconstr Surg Hand Surg. 2001;35(4):415-417. [DOI] [PubMed] [Google Scholar]
- 5. Vermeulen GM, Slijper H, Feitz R, et al. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011;36(1):157-169. [DOI] [PubMed] [Google Scholar]
- 6. Barron OA, Catalano LW. Thumb basal joint arthritis. In: Wolfe SW, Hotchkiss RN, Pederson WC, et al., eds. Green’s Operative Hand Surgery. 6th ed. New York, NY: Churchill-Livingstone; 2011:405-426. [Google Scholar]
- 7. Li YK, White C, Ignacy TA, et al. Comparison of trapeziectomy and trapeziectomy with ligament reconstruction and tendon interposition: a systematic literature review. Plast Reconstr Surg. 2011;128(1):199-207. [DOI] [PubMed] [Google Scholar]
- 8. Ferrière S, Mansat P, Rongières M, et al. Trapézectomie totale avec tendinoplastie de suspension et d’interposition dans le traitement de la rhizarthrose: résultats à 6.5 ans de recul moyen. Chir Main. 2010;29:16-22. [DOI] [PubMed] [Google Scholar]
- 9. Moineau G, Richou J, Liot M, et al. Prognostic factors for the recovery of hand function following trapeziectomy with ligamentoplasty stabilization. Orthop Traumatol Surg Res. 2009;95:352-358. [DOI] [PubMed] [Google Scholar]
- 10. Honkanen PB, Kellomäki M, Lehtimäki MY, et al. Bioreconstructive joint scaffold implant arthroplasty in metacarpophalangeal joints: short-term results of a new treatment concept in rheumatoid arthritis patients. Tissue Eng. 2003;9(5):957-965. [DOI] [PubMed] [Google Scholar]
- 11. Honkanen PB, Kellomäki M, Konttinen YT, et al. A midterm follow-up study of bioreconstructive polylactide scaffold implants in metacarpophalangeal joint arthroplasty in rheumatoid arthritis patients. J Hand Surg Eur Vol. 2009;34(2):179-185. [DOI] [PubMed] [Google Scholar]
- 12. Ikävalko M, Skyttä ET, Belt EA. One-year results of use of poly-L/D-lactic acid joint scaffolds and bone packing in revision metacarpophalangeal arthroplasty. J Hand Surg Eur Vol. 2007;32(4):427-433. [DOI] [PubMed] [Google Scholar]
- 13. Kennedy AM, Barker J, Estfan E, et al. The use of the RegJoint™ implant for base of thumb osteoarthritis: results with a minimum follow-up of 2 years. Hand Surg Rehabil. 2020;39(1):53-58. [DOI] [PubMed] [Google Scholar]
- 14. Mattila S, Waris E. Unfavorable short-term outcomes of a poly-L/D-lactide scaffold for thumb trapeziometacarpal arthroplasty. J Hand Surg Eur. 2016;41:328-334. [DOI] [PubMed] [Google Scholar]
- 15. Mattila S, Ainola M, Waris E. Bioabsorbable poly-L/D-lactide (96/4) scaffold arthroplasty (RegJointTM) for trapeziometacarpal osteoarthritis: a 3-year follow-up study. J Hand Surg Eur. 2018;43:413-419. [DOI] [PubMed] [Google Scholar]
- 16. Van Royen K, Kestens B, Van Laere S, et al. Short-term results after total trapeziectomy with a poly-L/D-lactide spacer. J Wrist Surg. 2018;7(5):394-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kapandji A. Clinical test of apposition and counter-apposition of the thumb. Ann Chir Main. 1986;5(1):67-73. [DOI] [PubMed] [Google Scholar]
- 18. Leti Acciaro A, Marcuzzi A, Della Rosa N, et al. Progetto europeo “Joint Scaffold”: sviluppo e valutazione clinica dell’impiego di innovativi impianti biosostituibili nel trattamento della rizoartrosi mediante artroplastica di interposizione. Riv Chir Mano. 2006;43:355-359. [Google Scholar]
- 19. Gottschalk MB, Patel NN, Boden AL, et al. Treatment of basilar thumb arthritis: a critical analysis review. JBJS Rev. 2018;6(7):e4. doi: 10.2106/JBJS.RVW.17.00156. [DOI] [PubMed] [Google Scholar]