OBJECTIVES:
Major postintensive care sequelae affect up to one in three adult survivors of critical illness. Large cohorts on educational outcomes after pediatric intensive care are lacking. We assessed primary school educational outcomes in a statewide cohort of children who survived PICU during childhood.
DESIGN:
Multicenter population-based study on children less than 5 years admitted to PICU. Using the National Assessment Program—Literacy and Numeracy database, the primary outcome was educational achievement below the National Minimum Standard (NMS) in year 3 of primary school. Cases were compared with controls matched for calendar year, grade, birth cohort, sex, socioeconomic status, Aboriginal and Torres Strait Islander status, and school. Multivariable logistic regression models to predict educational outcomes were derived.
SETTING:
Tertiary PICUs and mixed ICUs in Queensland, Australia.
PATIENTS:
Children less than 5 years admitted to PICU between 1998 and 2016.
INTERVENTIONS:
Not applicable.
MEASUREMENTS AND MAIN RESULTS:
Year 3 primary school data were available for 5,017 PICU survivors (median age, 8.0 mo at first PICU admission; interquartile range, 1.9–25.2). PICU survivors scored significantly lower than controls across each domain (p < 0.001); 14.03% of PICU survivors did not meet the NMS compared with 8.96% of matched controls (p < 0.001). In multivariate analyses, socioeconomic status (odds ratio, 2.14; 95% CI, 1.67–2.74), weight (0.94; 0.90–0.97), logit of Pediatric Index of Mortality-2 score (1.11; 1.03–1.19), presence of a syndrome (11.58; 8.87–15.11), prematurity (1.54; 1.09–2.19), chronic neurologic conditions (4.38; 3.27–5.87), chronic respiratory conditions (1.65; 1.24–2.19), and continuous renal replacement therapy (4.20; 1.40–12.55) were independently associated with a higher risk of not meeting the NMS.
CONCLUSIONS:
In this population-based study of childhood PICU survivors, 14.03% did not meet NMSs in the standardized primary school assessment. Socioeconomic status, underlying diseases, and severity on presentation allow risk-stratification to identify children most likely to benefit from individual follow-up and support.
Keywords: child, critical care, education, mortality, neurodevelopment, school achievement
In high-income countries, each year between 1.43 and 2.12 per 1,000 children requires PICU admission for treatment or monitoring due to life-threatening illness or surgery (1, 2). Mortality remains the primary measure to assess PICU outcomes, and standardized mortality rates represent the most widely used benchmarks for evaluating the performance of PICUs (3). Over the past decades, survival for critically ill children has continuously improved with current mortality rates as low as 2.18% (1, 4–6).
An emerging body of literature in critically ill adults has brought the extensive psychologic and cognitive impact of critical illness on patients and their families to attention (7, 8). Sequelae ranging from posttraumatic stress disorder or mental health problems, physical disabilities, to long-term cognitive impairment as a result of brain injury affect up to one in three adult survivors of critical illness. In critically ill children, 28–31% of patients with severe sepsis (9, 10) and up to 38% of infants undergoing surgery for congenital heart disease (11) suffer from substantial disability following PICU discharge (12). Long-term morbidity after critical illness directly affects quality of life in survivors and represents a patient-centered outcome of great relevance to families (13, 14).
To date, pediatric long-term outcome literature has been primarily based on cohort studies with a follow-up duration of less than 24-month post-PICU stay using tests of gross function or quality of life (15, 16). Although persisting functional and cognitive impairments can be more reliably assessed once school age is reached, such follow-up, where available, has been largely restricted to highly selected subgroups such as children with congenital heart disease or extremely low birth weight infants (17, 18). Access to robust long-term outcome data will position us to better understand the long-term cost of disease, provide parents with more accurate prognostic estimates, and allow measuring the long-term impact of different interventions (19).
The aim of this study was to assess educational outcomes at school age in children who had required ICU admission before 5 years old. We analyzed performance during primary school using a standardized national school assessment in a population-based cohort of critically ill children and identified predictors of poor educational outcomes.
PATIENTS AND METHODS
This is a multicenter statewide data linkage study based on the Australian and New Zealand Paediatric Intensive Care (ANZPIC) Registry. The study was approved by the Human Research and Ethics Committee (Children’s Health Queensland, Brisbane, Australia; number HREC/16/QRCH/255), including waiver of consent. Children less than 5 years requiring ICU admission in Queensland, Australia, between January 1, 1998, and December 31, 2016, were eligible. During this time, the population of Queensland increased from 3,401,232 to 4,883,739 (Australian Bureau of Statistics). We linked the ANZPIC Registry data with the Registrar General deaths registry and with educational data provided by the Queensland Curriculum and Assessment Authority (QCAA). A combination of deterministic and probabilistic matching was performed by the Statistical Services Branch, Queensland Health, depending on the available identifying information in each data source: using sex, date of birth, post code, facility, date of admission, and name.
The ANZPIC Registry (3, 20) prospectively records data fields among children less than 16 years admitted to ICU, including patient characteristics, diagnoses, severity markers, and physiologic variables, with regular data validation and auditing. The QCAA data cover the National Assessment Program—Literacy and Numeracy (NAPLAN, https://www.nap.edu.au/), a nationwide standardized assessment for all students in school years 3, 5, 7, and 9, and have been administered annually since 2008 across Australian public and private schools (Supplemental Methods, http://links.lww.com/CCM/G987). NAPLAN test domains include: 1) reading, 2) writing, 3) spelling, 4) grammar and punctuation, and 5) numeracy.
Control Groups
Averaged NAPLAN test results for all Queensland students participating in a Year 3 NAPLAN test during 2008 to 2017 were used as overall controls. In addition, 1:1 matched controls were extracted from QCAA (Supplementary Methods, http://links.lww.com/CCM/G987) based on the following criteria by order of priority: 1) calendar year of the NAPLAN test, 2) year level (grade), 3) year of birth, 4) sex, 5) socioeconomic status (SES), 6) Aboriginal and Torres Strait Islander status, and 7) school.
Definitions and Outcomes
We extracted critical care variables based on the principal, underlying, and associated diagnoses captured in ANZPIC Registry (4, 20), admission characteristics, and treatment and severity factors such as Pediatric Index of Mortality-2 (21, 22) (PIM-2). SES was constructed using information on maternal and paternal highest education and profession in the QCAA dataset and was classified into low, middle, and high SES (23, 24). The data captured through the standardized NAPLAN testing performed at year 3 of primary school (children are usually 8 ± 1 years of biological age when sitting this test) were used to construct the outcomes. For each of the five NAPLAN measurement domains, we considered their score and whether a student had been exempt. As per the NAPLAN standards, exempt students are those with significant disability or coexisting conditions that severely limit their capacity to participate in the tests. Exemptions are recorded along with other reasons for missing tests, including being absent on the test day, or having been withdrawn from testing by their parents. A threshold defined as the National Minimum Standard (NMS) exists for each domain, capturing the minimum acceptable standard of knowledge and skills without which a student will have difficulty making sufficient progress at school. Band 2 (lower threshold score of 270) is the minimum standard for Year 3 NAPLAN testing. Children who are exempt are automatically classified as below NMS. Of the five NAPLAN domains, reading and numeracy are considered most important due to their impact on long-term academic achievement (25). Numeracy and reading correlate highly with the other NAPLAN domains, and previous studies demonstrated their utility and stability over time (26). We therefore defined the primary outcome as children classified below the NMS on both NAPLAN numeracy and reading domains in year 3. Secondary outcomes included children classified below the NMS on Numeracy or Reading domains, classified below the NMS on all five NAPLAN domains, and classified below the NMS on at least one of the five NAPLAN domains.
Statistical Analyses
Data are presented as percentages and numbers or medians with interquartile range (IQR). T tests were used to compare normally distributed data, and proportion tests were used to compare subgroups. Outcome prediction models were developed using a stepwise logistic regression approach considering patient characteristics, physiologic and severity values at admission, diagnostic codes characterizing main disease and comorbidities, treatment interventions, number of ICU admissions, and SES. We used a backward stepwise elimination procedure to eliminate nonsignificant predictors based on p > 0.05, keeping test year in the model. The main multivariable model was based on data available during the first PICU admission before a child’s fifth birthday. Sensitivity analyses were conducted including information from all PICU admissions occurring before the fifth birthday in the model. All analyses were conducted using Stata (Version 14.0, Stata Corp, College Station, TX). p values of less than 0.05 were considered statistically significant.
RESULTS
Cohort Overview
A total of 6,948 patients were admitted to ICU in Queensland before their fifth birthday between 1998 and 2016 and were eligible for NAPLAN testing based on their age and birth cohort (Supplementary Fig. 1, http://links.lww.com/CCM/G987). n = 414 (6.0%) had died before the NAPLAN test date including deaths in ICU and deaths postdischarge. A total of 5,017 out of 6,534 eligible children (76.8%) with a median age at first admission to ICU of 8.0 months (IQR, 1.9–25.2) had ICU data successfully linked to Year 3 NAPLAN outcome data and comprised the final study cohort (Table 1). Children who were not successfully linked were significantly younger, had a higher proportion of syndromes, had higher predicted mortality, and required more intensive care support in comparison with the children included in the study (p < 0.05; Supplementary Table 1, http://links.lww.com/CCM/G987).
TABLE 1.
Descriptive Statistics of 5,017 Children Surviving PICU Admission Based on First and All PICU Admissions Before the Fifth Birthday
| Variables | First Admission (n = 5,017) | All Admissions (n = 5,017) | All Readmissions (n = 5,017) |
|---|---|---|---|
| Demographics | |||
| Sex (male) | 2,954 (58.9%) | ||
| Aboriginal and Torres Strait Islander | 552 (11.0%) | ||
| Socioeconomic status | |||
| No information | 699 (13.9%) | ||
| Low SES | 1,377 (27.4%) | ||
| Medium SES | 1,513 (30.2%) | ||
| High SES | 1,428 (28.5%) | ||
| Age, d, median (IQR) | 239 (56–757) | 319.50 (80–825) | 445 (151–957) |
| Weight, kg, median (IQR) | 7.94 (4.00–12.00) | 8.66 (4.60–12.50) | 4.50 (3.30–7.90) |
| No. of PICU admissions before the fifth birthday | |||
| 1 | 3,885 (77.4%) | ||
| 2 | 651 (13.0%) | ||
| ≥ 3 | 481 (9.6%) | ||
| Main disease groups | |||
| Asthma | 174 (3.5%) | 185 (3.7%) | 19 (0.8%) |
| Bronchiolitis | 510 (10.2%) | 559 (11.1%) | 176 (7.5%) |
| Invasive infections | 312 (6.2%) | 379 (7.6%) | 96 (4.1%) |
| Congenital heart disease | 1,036 (20.6%) | 1,086 (21.6%) | 908 (38.8%) |
| Oncologic conditions | 114 (2.3%) | 123 (2.5%) | |
| Chronic respiratory conditions | 506 (10.1%) | 612 (12.2%) | 320 (13.7%) |
| Chronic neurologic conditions | 277 (5.5%) | 349 (7.0%) | 242 (10.3%) |
| Prematurity | 294 (5.9%) | 294 (5.9%) | 219 (9.4%) |
| Trauma | 440 (8.8%) | 462 (9.2%) | 42 (1.8%) |
| Congenital syndrome | 314 (6.3%) | 371 (7.4%) | 346 (14.8%) |
| Admission characteristics | |||
| PIM-2 risk of death, mean (sd) | 2.29% (5.1%) | 2.65% (5.6%) | 3.1% (5.9%) |
| PIM-2 risk of death, median (IQR) | 0.90% (0.2–2.5%) | 1.02% (0.2–3.0%) | 1.3% (0.4–3.2%) |
| Interhospital transfer | 1,191 (23.7%) | 1,280 (25.5%) | 479 (20.5%) |
| Elective admission | 2,337 (46.6%) | 2,625 (52.3%) | 1,279 (54.6%) |
| Recovery from surgery | 2,405 (47.9%) | 2,754 (54.9%) | 1,124 (48.0%) |
| Severity and treatment | |||
| Intubation, d, median (IQR) | 0 (0.00–0.93) | 0 (0.00–1.59) | 1.0 (0.06–3.63) |
| PICU length of stay, d, median (IQR) | 1.04 (0.72–2.67) | 1.43 (0.78–3.85) | 1.61 (0.76–4.32) |
| Hospital length of stay, d, median (IQR) | 6.95 (3.31–12.04) | 4.36 (0.00–11.16) | 13.15 (6.65–29.75) |
| Respiratory support, d, median (IQR) | 0.54 (0.17–1.42) | 0.00 (0.00–0.00) | 0.74 (0.52–2.50) |
| Extracorporeal membrane oxygenation | 2 (< 0.1%) | 5 (0.1%) | 10 (0.4%) |
| Inhaled nitric oxide | 34 (0.7%) | 70 (1.4%) | 43 (1.8%) |
| Continuous renal replacement | 16 (0.3%) | 24 (0.5%) | 40 (1.7%) |
| High-frequency oscillatory ventilation | 36 (0.7%) | 59 (1.2%) | 27 (1.2%) |
IQR = interquartile range, PIM-2 = Pediatric Index of Mortality-2, SES = socioeconomic status.
Description of Educational Outcomes in ICU Survivors
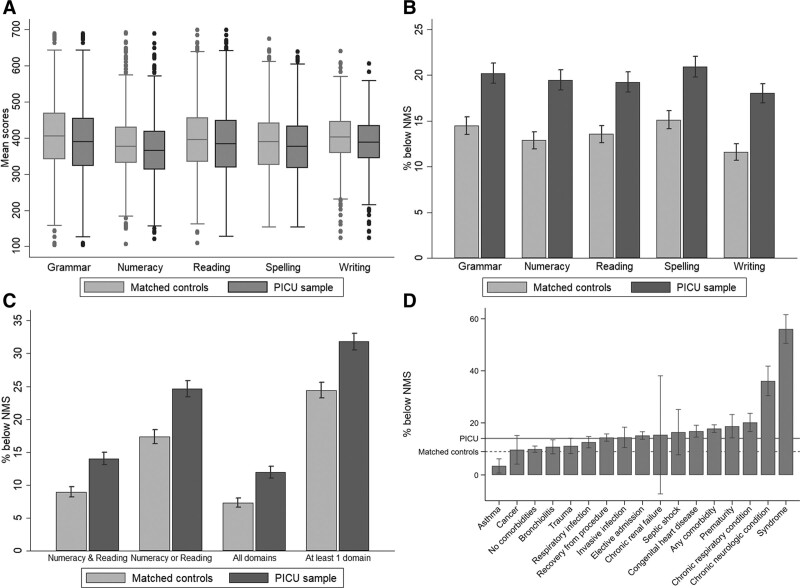
We compared the rates of participation and average scores in the NAPLAN tests between the ICU sample, the average Queensland student population, and matched controls (Supplementary Tables 2–6, http://links.lww.com/CCM/G987). ICU cases had lower rates of participation in NAPLAN and significantly higher rates of being exempt from NAPLAN testing, compared with the Queensland student population (p < 0.001), and to matched controls (both p < 0.001) in each of the five domains. On average, 79.0% (n = 3,964) of the ICU survivors were able to participate in Year 3 NAPLAN across the five domains, compared with 93.2% in the Queensland student population, and 87.0% (mean n = 4,357) in the matched control sample (p < 0.001). On average, 11.7% (mean n = 588) of the PICU group were exempt from the five NAPLAN domains, compared with 1.6% in the Queensland student population (p < 0.001) and 7.3% (mean n = 363) in the matched controls group (p < 0.001). In addition, rates of withdrawal due to parental decisions were significantly higher in ICU survivors compared with both control groups across NAPLAN domains (p < 0.001). When comparing the average Year 3 NAPLAN scores for those who were able to participate in the tests, ICU survivors consistently scored lower compared with the average Queensland student population and compared with the matched control sample across all NAPLAN domains (Supplementary Table 7, http://links.lww.com/CCM/G987; and Fig. 1A). On average, the ICU sample scored 20 points lower than the Queensland population (ICU = 379; Queensland population = 399; p < 0.001) and 13 points (ICU = 379; Controls = 392; p < 0.001) lower than the matched control sample.
Across all the NAPLAN domains, the proportion of students who were below the NMS in PICU survivors was higher than the matched control group (p < 0.001) (Table 2 and Fig. 1, B and C). The proportion of PICU survivors who did not meet the NMS for numeracy and reading varied severalfold between different patient diagnostic groups (Fig. 1D). Overall, 14.0% of PICU survivors did not meet the NMS for numeracy and reading, in comparison with 9.0% of matched controls (absolute difference 5.1%, p < 0.001). Similar differences were found for the secondary outcomes.
TABLE 2.
Incidence of Main and Secondary Outcomes in 5,017 Children Who Survived PICU Admission Before Their Fifth Birthday
| Outcome | PICU Sample | Matched Controls | Difference |
|---|---|---|---|
| Main outcome | |||
| % below NMS on both numeracy and reading | 14.03 | 8.96 | 5.07% (z = 7.96)a |
| Secondary outcomes | |||
| % below NMS on numeracy or reading | 24.64 | 17.38 | 7.25% (z = 8.92)a |
| % below NMS on all NAPLAN domains | 11.94 | 7.32 | 4.62% (z = 7.83)a |
| % below NMS on at least one NAPLAN domain | 31.81 | 24.41 | 7.40% (z = 8.25)a |
NAPLAN = National Assessment Program—Literacy and Numeracy, NMS = National Minimal Standard.
p < 0.001,
The proportions of students failing to meet NMS (defined as a score below 270 or being exempt from testing) during the NAPLAN are compared between PICU survivors and matched controls. Data are based on pooled results of NAPLAN testing between 2008 and 2017. Z-statistics from proportions test are shown. Italics indicate significance (p < 0.001).
Figure 1.
Educational outcomes assessed through the Year 3 National Assessment Program—Literacy and Numeracy (NAPLAN) in 5,017 children who survived PICU admission before their fifth birthday are shown comparing PICU survivors and matched controls. A, Box-whisker plots comparing Year 3 NAPLAN scores between PICU survivors and controls for each of the five NAPLAN domains. B, Proportion of students failing to meet the National Minimal Standard (NMS) during Year 3 NAPLAN testing between cases and controls for each of the five NAPLAN domains. C, Proportion of students failing to meet the NMS during Year 3 NAPLAN testing between cases and controls for both reading and numeracy, either reading and numeracy, all NAPLAN domains, or at least one NAPLAN domain. D, Proportion of students failing to meet the NMS during Year 3 NAPLAN is shown in ascending order for different diagnostic groups in comparing with the average outcomes of PICU survivors (straight horizontal line) and in relation to matched controls (dashed horizontal line). Error bars represent 95% CIs.
Prediction of Poor Educational Outcomes Using Variables Available at Time of PICU Discharge
We built logistic regression models using data available at the time of PICU discharge to predict poor educational outcomes (Table 3), adjusted for SES, age, sex, weight, and Aboriginal and/or Torres Strait Islander status. Low SES was significantly associated with the primary outcome with an odds ratio (OR) of 2.14 (95% CI, 1.67–2.74; p < 0.001) compared with high SES. In addition, there was weak evidence for Aboriginal and Torres Strait Islander patients to be at increased risk of not meeting NMS (p = 0.051). Higher weight at PICU admission was associated with lower odds of not meeting the NMS (OR, 0.94; 95% CI, 0.90–0.97; p = 0.001). In the adjusted models, several clinical variables were independently associated with a higher risk of not meeting the NMS: severity at admission as measured by the probability of death (logit of PIM-2 1.11; 1.03–1.19; p = 0.006), presence of a syndrome (11.58; 8.87–15.11; p < 0.001), prematurity (1.54; 1.09–2.19; p = 0.015), chronic neurologic conditions (4.38; 3.27–5.87; p < 0.001), chronic respiratory conditions (1.65; 1.24–2.19; p = 0.001), and need for continuous renal replacement therapy (4.20; 1.40–12.55; p = 0.010). A diagnosis of asthma was protective (0.39; 0.17–0.92; p = 0.032). Additional multivariable analysis showed that the absence of comorbidities was not significantly associated with failure to meet NMS (1.08; 0.82–1.41; p = 0.590).
TABLE 3.
Uni- and Multivariate Regression Analyses of Risk Factors for Not Reaching the National Minimum Standard on Year 3 National Assessment Program—Literacy and Numeracy Reading and Numeracy in 5,017 Children Who Survived PICU Admission Before Their Fifth Birthday
| Variables | Bivariate Regressions | Multivariate Regressions (First Admission) | Multivariate Regressions (All Admissions) | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | P | |
| Demographics | ||||||
| Female | 1.02 (0.87–1.20) | 0.835 | 0.96 (0.80–1.15) | 0.644 | 0.92 (0.77–1.11) | 0.396 |
| Aboriginal and Torres Strait Islander | 1.41 (1.18–1.69) | < 0.001 | 1.29 (1.00–1.67) | 0.051 | 1.33 (1.03–1.73) | 0.032 |
| Socioeconomic status (reference: high SES) | ||||||
| No information | 2.27 (1.87–2.75) | < 0.001 | 2.28 (1.71–3.03) | < 0.001 | 2.19 (1.63–2.93) | < 0.001 |
| Low SES | 1.85 (1.56–2.19) | < 0.001 | 2.14 (1.67–2.74) | < 0.001 | 2.22 (1.73–2.86) | < 0.001 |
| Medium SES | 1.19 (0.99–1.42) | 0.061 | 1.28 (1.00–1.65) | 0.054 | 1.27 (0.98–1.64) | 0.069 |
| Age, d | 1.00 (1.00–1.00) | 0.563 | 1.00 (1.00–1.00) | 0.007 | 1.00 (1.00–1.00) | 0.022 |
| Weight, kg | 0.98 (0.96–0.99) | 0.007 | 0.94 (0.90–0.97) | 0.001 | 0.96 (0.93–0.99) | 0.025 |
| No. of PICU admissions | – | – | – | – | 1.06 (0.99–1.13) | 0.082 |
| Main disease groups and comorbidities | ||||||
| Asthma | 0.21 (0.09–0.48) | < 0.001 | 0.39 (0.17–0.92) | 0.032 | 0.66 (0.33–1.34) | 0.251 |
| Bronchiolitis | 0.72 (0.54–0.96) | 0.026 | 0.79 (0.56–1.12) | 0.183 | NA | – |
| Invasive infections | 1.03 (0.75–1.43) | 0.837 | NA | – | NA | – |
| Oncologic conditions | 0.65 (0.35–1.21) | 0.176 | NA | – | NA | – |
| Trauma | 0.75 (0.55–1.02) | 0.068 | NA | – | NA | – |
| Chronic neurologic condition | 3.87 (2.98–5.02) | < 0.001 | 4.38 (3.27–5.87) | < 0.001 | 5.08 (3.88–6.64) | < 0.001 |
| Prematurity | 1.44 (1.07–1.96) | 0.018 | 1.54 (1.09–2.19) | 0.015 | 1.55 (1.09–2.19) | 0.014 |
| Congenital syndrome | 10.08 (7.93–12.83) | < 0.001 | 11.58 (8.87–15.11) | < 0.001 | 10.27 (7.98 –13.21) | < 0.001 |
| Chronic respiratory condition | 1.64 (1.30–2.07) | < 0.001 | 1.65 (1.24–2.19) | 0.001 | 1.90 (1.46–2.47) | < 0.001 |
| Congenital heart disease | 1.31 (1.09–1.58) | 0.004 | 1.21 (0.93–1.57) | 0.155 | NA | – |
| Chronic renal failure | 1.11 (0.25–5.04) | 0.888 | NA | – | NA | – |
| Admission characteristics | ||||||
| Pediatric Index of Mortality-2 risk of death (logit) | 1.10 (1.04–1.16) | < 0.001 | 1.11 (1.03–1.19) | 0.006 | 1.20 (1.13–1.28) | < 0.001 |
| Interhospital transfer | 1.08 (0.90–1.30) | 0.397 | NA | – | NA | – |
| Elective admission | 1.19 (1.01–1.39) | 0.034 | 0.84 (0.66–1.07) | 0.150 | NA | – |
| Severity and treatment | ||||||
| Intubation, d | 1.01 (1.00–1.03) | 0.022 | 0.98 (0.96–1.01) | 0.269 | NA | – |
| PICU length of stay, d | 1.02 (1.01–1.03) | 0.003 | 1.02 (1.00–1.05) | 0.102 | NA | – |
| Hospital length of stay, d | 1.01 (1.00–1.01) | 0.005 | NA | – | NA | – |
| Respiratory support, d | 1.07 (0.98–1.16) | 0.125 | NA | – | NA | – |
| Invasive ventilation, d | 1.06 (0.98–1.15) | 0.167 | NA | – | NA | – |
| Extracorporeal membrane oxygenation | 6.13 (0.38–98.18) | 0.200 | NA | – | NA | – |
| Inhaled nitric oxide | 1.32 (0.54–3.19) | 0.544 | NA | – | NA | – |
| Continuous renal replacement | 4.80 (1.78–12.94) | 0.002 | 4.20 (1.40–12.55) | 0.010 | 2.31 (0.88–6.04) | 0.088 |
| High-frequency oscillatory ventilation | 1.23 (0.51–2.96) | 0.648 | NA | – | NA | – |
NA = not applicable, OR = odds ratio, SES = socioeconomic status.
Multivariate regression models were built using information from the first PICU admission (main analyses) and using information from all PICU admissions that occurred before the fifth birthday (sensitivity analyses). All analyses are adjusted for year of test (not shown).
Sensitivity analyses adding variables on cumulative exposure in children who had greater than one PICU admission before their fifth birthday (Table 3) confirmed the main analyses, except that asthma and renal replacement were no longer significantly associated with the outcome. Multivariable logistic regression on the secondary outcomes (Supplementary Table 8, http://links.lww.com/CCM/G987) identified the same independent predictors as the main model. In addition, length of ICU stay emerged as a significant predictor (p < 0.05). Sensitivity analyses restricted to children after nonelective admission (Supplementary Table 9, http://links.lww.com/CCM/G987) did not confirm the association of weight, prematurity, and chronic respiratory conditions with outcomes, whereas length of intubation and length of ICU stay were significant predictors.
DISCUSSION
In this statewide population-based study assessing educational outcomes in the third year of primary school in 5,017 children who had been admitted to PICU before their fifth birthday, 14% failed to achieve the national minimum standard requirements without which a student will have difficulty making sufficient progress at school. The findings were consistent when comparing PICU survivors with statewide controls and matched controls, with comparable effect sizes observed across each of the five domains of educational assessment. SES emerged as a strong nondisease-related predictor of long-term outcomes, highlighting the importance of supporting children from socially disadvantaged families. Disease severity as assessed by PIM-2 and major chronic conditions were identified as key risk factors. Although some of the effects may be caused by underlying, that is, preexisting conditions rather than reflecting solely the sequelae of critical illness, the findings from this large cohort serve to inform parents, clinicians, and policy makers about the long-term outcomes of childhood PICU survivors.
Over the past decade, research on postintensive care syndrome has highlighted the consequences many survivors experience after critical care, affecting emotional, mental, psychomotor, and cognitive functions of well-being (19). Many studies have applied standardized tests such as the Pediatric Quality of Life Inventory or the Functional Status Scale to children around 12-month post-PICU discharge (15, 16). Studies in extremely preterm infants revealed that early testing both over- and underpredicted a substantial proportion of children who manifested long-lasting impairments evident during assessment at school age (18). Hence, reliable assessment of neurodevelopmental outcomes requires comprehensive assessment at school age, as demonstrated in our study where the median follow-up duration was over 7-year post-ICU stay. Using a standardized national program that has been annually assessing student performance across five domains in all Australian private and public schools since 2008, we were able to analyze long-term educational outcomes of a large cohort of PICU survivors. In contrast to previous studies restricted to specific high-risk groups (27, 28), our findings cover the entire range of causes leading to PICU admission. Major comorbidities known to affect brain development, such as syndromes and chronic neurologic conditions, were associated adverse long-term outcomes. In addition, prematurity and chronic respiratory conditions showed independent associations with educational outcomes. Interestingly, PIM-2 was observed to be the most important severity variable contributing independently to poor educational outcomes. We hypothesize that higher PIM-2 values characterize children exposed to both increased disease-related (such as shock with cerebral hypoperfusion) and treatment-related risks (such as sedation-related neurotoxicity) who, despite a high risk of mortality, survive thanks to modern intensive care.
Importantly, low SES conferred a greater risk of poor educational outcomes than disease features such as prematurity or chronic respiratory conditions. Social disadvantage may expose children to inequities resulting in poor prevention, higher prevalence of infections, delayed recognition of deterioration, restricted access to healthcare, and less support for their well-being and development post-PICU (29, 30). Of note, the matched controls systematically performed worse than the average statewide controls in our cohort, illustrating the importance of thorough matching to avoid bias due to gender, age, geography, school type, and SES. In this context, recent reports of deteriorating indicators of child and adolescent health in high-income countries are of great concern (31, 32) and indicate an urgent need to design post-PICU support measures for vulnerable populations.
The majority of children admitted to PICU are below 5 years old and, in principle, have a life expectancy of 80 years ahead if not limited by congenital conditions or the disease process. Consequently, adverse outcomes related to critical illness will exert an impact on the surviving child, its parents, siblings, and future offspring for many decades to come and translate into professional achievement, economic productivity, and dependency on others, including social welfare. At present, although guidelines recommend structured follow-up for specific patient groups such as high-risk congenital heart disease or extreme prematurity, most countries have no follow-up systems to assess long-term outcomes in critically ill children (19, 33, 34). Considering the resourcing implications to establish structured PICU follow-up programs (14), our study provides a framework to stratify children according to their risk of poor long-term educational outcomes. Children more likely to suffer from adverse long-term outcomes should be prioritized for targeted follow-up such as questionnaires by proxy and face-to-face assessments. Importantly, such strategies may enable research on early developmental interventions by general practitioners, hospital specialists, and early school support (35).
Several limitations of the study design need to be considered that affect the generalizability of results. First, although the outcome assessment was based on a standardized national school assessment that has been performed annually since 2008 in Australian schools, NAPLAN testing has not been internationally normalized. Second, a large proportion of the difference in the primary outcome between PICU survivors and controls was caused by a higher proportion of PICU survivors being exempt from NAPLAN testing. Although the Australian Curriculum Assessment and Reporting Authority rules state that teachers can only issue an exemption if students are affected by factors that severely limit their capacity to participate in the tests, including suffering from substantial disabilities, the exact disability was not documented in the dataset. Third, causality related to PICU exposure cannot be claimed, given the dataset did not contain neurocognitive assessment pre- and post-PICU admissions—which is an inherent limitation of PICU long-term outcome studies given that the majority of children require PICU preschool age, often for congenital conditions. The multivariable analyses show that both preexisting patient factors such as syndromes as well as severity on presentation and treatments affect long-term outcomes. Fourth, linked school outcome data were not available for 23% of the eligible cohort, representing interstate mobility, families moving overseas, home schooling, and true linkage failures. As the PICU admission characteristics of children not included in the linkage revealed slightly higher severity, complexity, and younger age, it is possible that our measures of long-term outcomes underestimate the true burden. Finally, the majority of students included in this follow-up experienced ICU care over a decade ago in Australia, and the practices and patient population may not be representative of contemporary PICU populations and their care.
In conclusion, we demonstrate and quantify for the first time the long-term educational impacts of pediatric critical illness. In this population-based study of children requiring PICU during early childhood, one in seven survivors did not meet NMSs in the school assessment performed during year 3 of primary school. Failing to meet minimal academic requirement carries a high likelihood of derailing educational and occupational trajectories well into adulthood, affecting both survivors and the society. Our findings indicate a substantial long-term cognitive burden related to critical illness, warranting research on rehabilitation and school support for survivors of critical illness.
ACKNOWLEDGMENTS
We thank the Queensland Curriculum and Assessment Authority and Queensland Department of Education for their support in accessing and interpreting the data. In particular, we thank Michelle Nesic and Roland Simons. The authors acknowledge the data linkage team of the Statistical Services Branch, Queensland Health, for linking the datasets used for this project. We thank Jan Alexander and the Australian and New Zealand Paediatric Intensive Care (ANZPIC) Registry for providing Queensland data. We also thank the intensivists, data managers, and other staff in the participating ICUs for their data contributions. The ANZPIC Registry is one of four registries managed by the Australian and New Zealand Intensive Care Society’s Centre for Outcome and Resource Evaluation (ANZICS CORE). ANZICS CORE is supported by the Ministry of Health (New Zealand) and State and Territory Health Departments (Australia). We thank the Paediatric Study Group of the Australian and New Zealand Intensive Care Society for supporting this study.
Supplementary Material
Footnotes
*See also p. 1010.
The Australian and New Zealand Intensive Care Society Paediatric Study Group (ANZICS PSG) are as follows: Anusha Ganeshalingam, Claire Sherring, Starship Children’s Hospital, Auckland, New Zealand; Simon Erickson, Samantha Barr, Perth Children`s Hospital, Perth, Australia; Sainath Raman, Debbie Long, Luregn Schlapbach (Chair), Breanna Pellegrini (Australian and New Zealand Paediatric Intensive Care [ANZPIC] registry), Queensland Children’s Hospital, Brisbane, Australia; Shane George, Gold Coast University Hospital; Gary Williams, Vicky Smith, Sydney Children’s Hospital, Randwick, Australia; Warwick Butt, Carmel Delzoppo, Johnny Millar (ANZPIC registry lead), Ben Gelbart (Vice Chair), Royal Children’s Hospital, Melbourne, Australia; Felix Oberender, Monash Children`s Hospital, Melbourne, Australia; Subodh Ganu, Georgia Letton, Women’s and Children’s Hospital, Adelaide, Australia; and Gail Harper, Marino Festa (Past Chair), Westmead Children’s Hospital, Sydney, Australia.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http:/journals.lww.com/ccmjournal).
Dr. Schlapbach designed the study and supervised all aspects of study conduct and analyses, and wrote the first draft of the article. Drs. Tomaszewski and Straney contributed to study design, reviewed analyses, and contributed to article drafting. Dr. Ablaza performed the main analyses and contributed to article drafting. Ms. Taylor contributed to study design, performed the data linkage, and contributed to article drafting. Dr. Millar contributed to study design and article drafting. All authors have reviewed and approved the final article.
Dr. Tomaszewski’s institution received funding from the Queensland Department of Education; he disclosed that data linkage was provided free of charge by the Queensland Department of Health. This manuscript provides research findings and does not represent the views of the Department of Education. Dr. Schlapbach received support for article research from grants from the Intensive Care Foundation Australia, an Education Horizon grant from the Queensland Department of Education, and Children’s Hospital Foundation Australia, and the National Health and Medical Research Council Practitioner Fellowship. The remaining authors have disclosed that they do not have any potential conflicts of interest.
The study was approved by the Human Research and Ethics Committee (Children`s Health Queensland, Brisbane, Australia; number HREC/16/QRCH/255), including waiver of consent.
The data are owned by the Australian and New Zealand Intensive Care Registry. The authors can be contacted for data inquiries.
The work was performed at The University of Queensland, Brisbane, Australia.
REFERENCES
- 1.ANZICS Centre for Outcome and Resource Evaluation (CORE): Australian and New Zealand Paediatric Intensive Care Registry Activity Report 2018. 2020. Available at: https://www.anzics.com.au/wp-content/uploads/2020/02/Australian-and-New-Zealand-Paediatric-Intensive-Care-Registry-Activity-Report-2018.pdf. Accessed October 25, 2020
- 2.PICA Network: Paediatric Intensive Care Audit Network Annual Report 2019. Available at: https://www.picanet.org.uk/wp-content/uploads/sites/25/2019/12/PICANet-2019-Annual-Report-Summary_v1.0.pdf. Accessed November 1, 2021
- 3.Straney L, Clements A, Parslow RC, et al. ; ANZICS Paediatric Study Group and the Paediatric Intensive Care Audit Network: Paediatric index of mortality 3: An updated model for predicting mortality in pediatric intensive care*. Pediatr Crit Care Med 2013; 14:673–681 [DOI] [PubMed] [Google Scholar]
- 4.Moynihan KM, Alexander PMA, Schlapbach LJ, et al. ; Australian and New Zealand Intensive Care Society Pediatric Study Group (ANZICS PSG) and the ANZICS Centre for Outcome and Resource Evaluation (ANZICS CORE): Epidemiology of childhood death in Australian and New Zealand intensive care units. Intensive Care Med 2019; 45:1262–1271 [DOI] [PubMed] [Google Scholar]
- 5.Butt W, Shann F, Tibballs J, et al. : Long-term outcome of children after intensive care. Crit Care Med 1990; 18:961–965 [DOI] [PubMed] [Google Scholar]
- 6.Namachivayam P, Shann F, Shekerdemian L, et al. : Three decades of pediatric intensive care: Who was admitted, what happened in intensive care, and what happened afterward. Pediatr Crit Care Med 2010; 11:549–555 [DOI] [PubMed] [Google Scholar]
- 7.Prescott HC, Iwashyna TJ, Blackwood B, et al. : Understanding and enhancing sepsis survivorship. Priorities for research and practice. Am J Respir Crit Care Med 2019; 200:972–981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iwashyna TJ, Ely EW, Smith DM, et al. : Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 2010; 304:1787–1794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss SL, Fitzgerald JC, Pappachan J, et al. ; Sepsis Prevalence, Outcomes, and Therapies (SPROUT) Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network: Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med 2015; 191:1147–1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boeddha NP, Schlapbach LJ, Driessen GJ, et al. ; EUCLIDS consortium: Mortality and morbidity in community-acquired sepsis in European pediatric intensive care units: a prospective cohort study from the European Childhood Life-threatening Infectious Disease Study (EUCLIDS). Crit Care 2018; 22:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walker K, Badawi N, Halliday R, et al. : Early developmental outcomes following major noncardiac and cardiac surgery in term infants: A population-based study. J Pediatr 2012; 161:748–752.e1 [DOI] [PubMed] [Google Scholar]
- 12.Gaynor JW, Stopp C, Wypij D, et al. ; International Cardiac Collaborative on Neurodevelopment (ICCON) Investigators: Neurodevelopmental outcomes after cardiac surgery in infancy. Pediatrics 2015; 135:816–825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woolfall K, O’Hara C, Deja E, et al. ; PERUKI (Paediatric Emergency Research in the UK and Ireland) and PICS (Paediatric Intensive Care Society): Parents’ prioritised outcomes for trials investigating treatments for paediatric severe infection: A qualitative synthesis. Arch Dis Child 2019; 104:1077–1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fink EL, Maddux AB, Pinto N, et al. ; Pediatric Outcomes STudies after PICU (POST-PICU) Investigators of the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network and the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN): A core outcome set for pediatric critical care. Crit Care Med 2020; 48:1819–1828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zimmerman JJ, Banks R, Berg RA, et al. ; Life After Pediatric Sepsis Evaluation (LAPSE) Investigators: Critical illness factors associated with long-term mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit Care Med 2020; 48:319–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zimmerman JJ, Banks R, Berg RA, et al. ; Life After Pediatric Sepsis Evaluation (LAPSE) Investigators: Trajectory of mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit Care Med 2020; 48:329–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schlapbach LJ, Adams M, Proietti E, et al. ; Swiss Neonatal Network & Follow-up Group: Outcome at two years of age in a Swiss national cohort of extremely preterm infants born between 2000 and 2008. BMC Pediatr 2012; 12:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marlow N, Wolke D, Bracewell MA, et al. ; EPICure Study Group: Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med 2005; 352:9–19 [DOI] [PubMed] [Google Scholar]
- 19.Watson RS, Choong K, Colville G, et al. : Life after critical illness in children-toward an understanding of pediatric post-intensive care syndrome. J Pediatr 2018; 198:16–24 [DOI] [PubMed] [Google Scholar]
- 20.Schlapbach LJ, Straney L, Alexander J, et al. ; ANZICS Paediatric Study Group: Mortality related to invasive infections, sepsis, and septic shock in critically ill children in Australia and New Zealand, 2002-13: A multicentre retrospective cohort study. Lancet Infect Dis 2015; 15:46–54 [DOI] [PubMed] [Google Scholar]
- 21.Slater A, Shann F, Pearson G; Paediatric Index of Mortality (PIM) Study Group: PIM2: A revised version of the paediatric index of mortality. Intensive Care Med 2003; 29:278–285 [DOI] [PubMed] [Google Scholar]
- 22.Shann F, Pearson G, Slater A, et al. : Paediatric index of mortality (PIM): A mortality prediction model for children in intensive care. Intensive Care Med 1997; 23:201–207 [DOI] [PubMed] [Google Scholar]
- 23.Werner H, Latal B, Valsangiacomo Buechel E, et al. : Health-related quality of life after open-heart surgery. J Pediatr 2014; 164:254–258.e1 [DOI] [PubMed] [Google Scholar]
- 24.Landolt MA, Vollrath M, Laimbacher J, et al. : Prospective study of posttraumatic stress disorder in parents of children with newly diagnosed type 1 diabetes. J Am Acad Child Adolesc Psychiatry 2005; 44:682–689 [DOI] [PubMed] [Google Scholar]
- 25.Duncan GJ, Dowsett CJ, Claessens A, et al. : School readiness and later achievement. Dev Psychol 2007; 43:1428–1446 [DOI] [PubMed] [Google Scholar]
- 26.Lain SJ, Bentley JP, Wiley V, et al. : Association between borderline neonatal thyroid-stimulating hormone concentrations and educational and developmental outcomes: A population-based record-linkage study. Lancet Diabetes Endocrinol 2016; 4:756–765 [DOI] [PubMed] [Google Scholar]
- 27.Buysse CM, Raat H, Hazelzet JA, et al. : Long-term health status in childhood survivors of meningococcal septic shock. Arch Pediatr Adolesc Med 2008; 162:1036–1041 [DOI] [PubMed] [Google Scholar]
- 28.Naef N, Liamlahi R, Beck I, et al. : Neurodevelopmental profiles of children with congenital heart disease at school age. J Pediatr 2017; 188:75–81 [DOI] [PubMed] [Google Scholar]
- 29.Marmot M: The health gap: The challenge of an unequal world. Lancet 2015; 386:2442–2444 [DOI] [PubMed] [Google Scholar]
- 30.Ostrowski JA, MacLaren G, Alexander J, et al. : The burden of invasive infections in critically ill Indigenous children in Australia. Med J Aust 2017; 206:78–84 [DOI] [PubMed] [Google Scholar]
- 31.The LANCET: The health inequalities and ill-health of children in the UK. Lancet 2017; 389:477. [DOI] [PubMed] [Google Scholar]
- 32.The L: Taking urgent action on health inequities. Lancet 2020; 395:659. [DOI] [PubMed] [Google Scholar]
- 33.Heneghan JA, Pollack MM: Morbidity: Changing the outcome paradigm for pediatric critical care. Pediatr Clin North Am 2017; 64:1147–1165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fink EL, Jarvis JM, Maddux AB, et al. ; Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Long-term Outcomes Subgroup Investigators, and; Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN): Development of a core outcome set for pediatric critical care outcomes research. Contemp Clin Trials 2020; 91:105968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spittle A, Orton J, Anderson PJ, et al. : Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst Rev 2015; 2015:CD005495. [DOI] [PMC free article] [PubMed] [Google Scholar]