Abstract
Background:
Intramedullary mature teratomas (IMMTs) are rare. This is particularly true in the adult population.
Case Description:
A 49-year-old female developed progressive paraparesis due to a T6 intramedullary mature teratoma with an exophytic component. She was successfully managed, utilizing a laminectomy with microsurgical tumor removal. The literature review documented 57 similar cases.
Conclusion:
Here, we presented a 49-year-old female with a T6 intramedullary mature teratoma accompanied by an exophytic component who underwent total tumor resection with an incomplete recovery.
Keywords: Adult, Intramedullary epidermoid, Intramedullary teratoma spinal cord, Thoracic spine

INTRODUCTION
Spinal teratomas account for approximately 0.1–0.5% of all spinal tumors.[1-6,9,10] They display a mixture of tissues derived from three primitive germ layers and are classified as mature, immature, or malignant.[1-6,9,10] Intramedullary mature teratomas (IMMTs) are the least common subtype found in adults.[1-6,9,10] Here, we present a 49-year-old female with a T6 IMMT who underwent surgical extirpation of the lesion with a resolution of the right lower extremity weakness, but residual left leg paresis. The literature review revealed 57 similar cases.[1-6,9,10]
CASE DESCRIPTION
A 49-year-old female presented with progressive weakness of both lower extremities of 2 years duration (i.e., bed-ridden). She was originally misdiagnosed with multiple sclerosis (MS). On examination, she exhibited a severe spastic paraparesis with hyperactive reflexes/bilateral Babinski signs. The thoracic MRI demonstrated a focal intramedullary lesion with an exophytic component at the T6 level with a mixed T2 signal intensity [Figure 1]. Utilizing an operating microscope, the patient underwent a laminectomy and midline myelotomy resulting in gross- total tumor excision [Figure 2]. The lesion proved to be a mature teratoma [Figure 3]. On the 10-day postoperative, MRI confirmed complete tumor resection [Figure 4]. Ten months later, her right lower extremity strength had dramatically improved, but left lower paresis remained unchanged.
Figure 1:
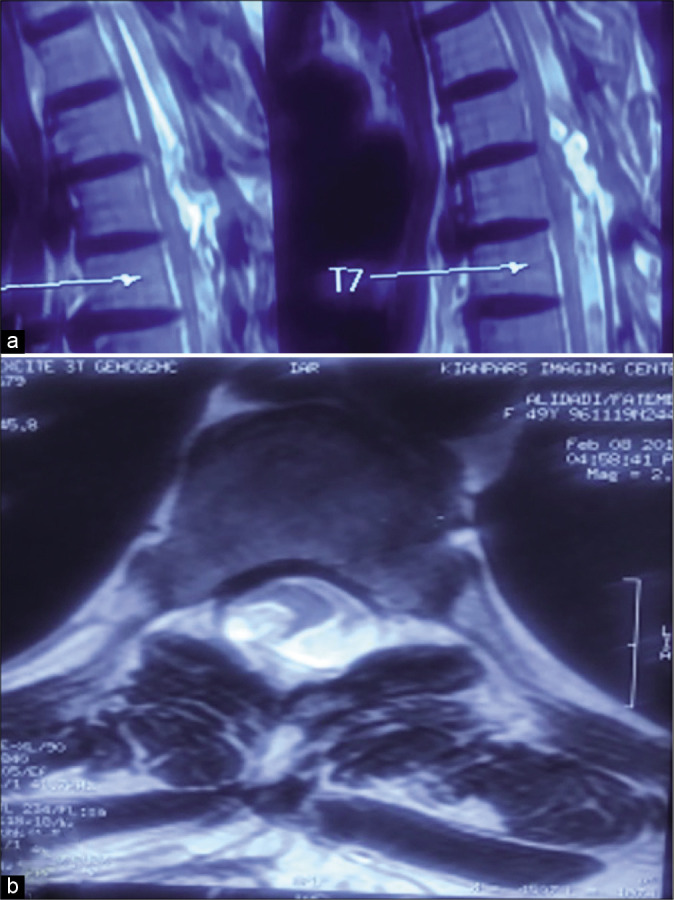
T2-weighted magnetic resonance imaging of the thoracic spine: (a) sagittal image showing a heterogeneous mass with an exophytic component at T6 level and (b) axial image.
Figure 2:
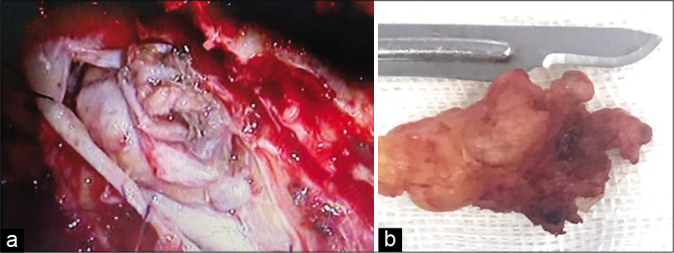
Intraoperative photographs (a) during the excision of a creamy yellow tumor which is fungating from the cord; (b) an irregularly shaped solid-soft tumor mass measuring 3 × 1.5 × 1 cm tumor after total removal.
Figure 3:
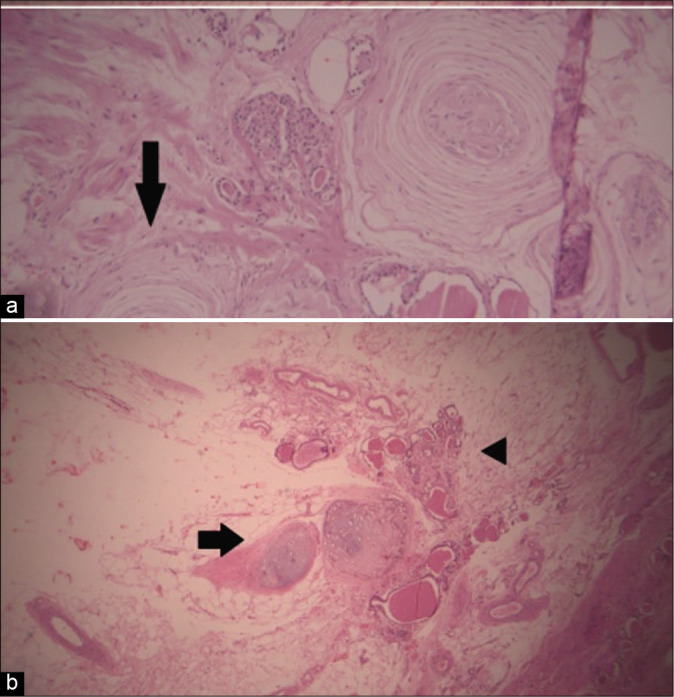
Pathology of the tumor, (a) presence of different components including thyroid like glands along with organoid corpuscle like nerve bundles (arrow) and (b) abundant adipose tissue along with focal mature cartilage (arrow) and some glandular structures (arrowhead).
Figure 4:
Postoperative T2-weighted sagittal magnetic resonance imaging of the thoracic spine shows total removal of the teratoma.
DISCUSSION
Etiology
Teratomas originate from pluripotent stem cells which are derived from all three germ cell layers. In IMMTs, all three embryonic layers are misplaced within the dorsal aspect of the spinal cord (e.g., in the midline during their normal migration from the primitive yolk sac during neural tube closure).[1-6,9,10] Associated congenital anomalies include spina bifida, split cord malformation (SCM), meningomyelocele, and Klippel-Feil syndromes.
Incidence
IMMs are very rare in adults; there are 57 similar cases reported in the literature [Table 1]. In those studies, patients averaged 39.9 years of age and included 31 males and 26 females [Table 2].
Table 1:
Approximately 57 reported cases of IMM in adults within medical literature; IMMs in adults are very rare.
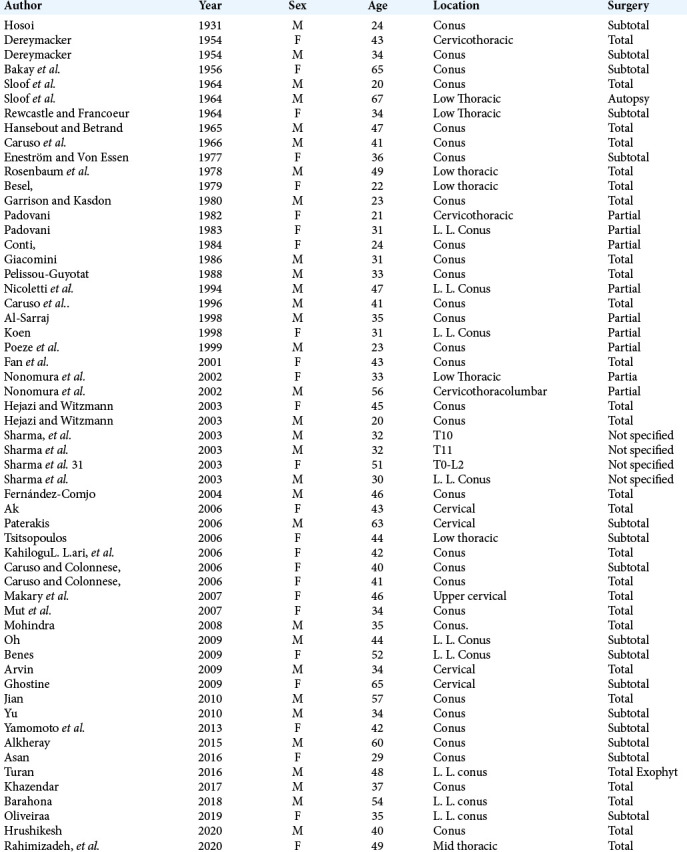
Table 2:
The sex frequency and percentage of 57 adult cases with IMMT.
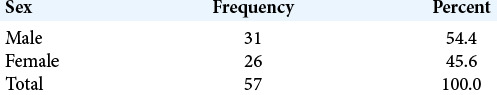
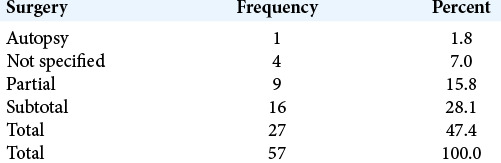
Table 3:
Management of 57 patients with IMMT with frequency and percentage.
The majority of lesions (39 cases) involved the terminal portion of the spinal cord/conus followed by the lower thoracic region (eight cases), cervical spine (five cases), cervicothoracic junction (three cases), and mid thoracic level (one case) (i.e., decreasing frequency).
Clinical picture
The clinical features of IMMTs reflect their locations. Those with conus lesions typically present with over-flow incontinence and progressive lower extremity paraparesis. More cephalad cervical tumors may result in quadriparesis, while upper thoracic lesions will be associated with higher- level paraparesis.
Imaging with CT/MR
MR scans are the studies of choice, as they readily demonstrate intramedullary heterogeneous cystic and/ or solid masses with/without an exophytic component (latter seven patients in the literature). CT may document attendant bony abnormalities (i.e., a variable tumor density or calcification within the tumor).
Histopathology
As they originate from pluripotent stem cells, teratomas can incorporate a wide range of tissues including; skin, muscle, bone, cartilage, intestinal mucosa, fat, teeth, and even hair.[1-6,9,10] The distinction between epidermoid cysts and juxtamedullary lipomas with IMMTs may prove difficult.[7,8]
Treatment
The best treatment for IMMTs is gross total surgical excision (e.g., found in 27 cases from the literature). Intimate adherence of tumor to the spinal cord parenchyma may preclude total removal (e.g., showing in 25 cases). Notably, 4 out of 57 cases in the literature did not specify what operative approaches were utilized [Table 3]. Postoperative neurological recovery may vary, long-lasting urinary incontinence and/or other long-term permanent deficits may not improve or resolve, and there is always the risk of worsening.[1-6,9,10]
CONCLUSION
The occurrence of an IMMT in an adult is rare. Timely diagnosis and surgical management (e.g., gross total if feasible) of these lesions remain critical in achieving the best postoperative outcomes.
Footnotes
How to cite this article: Rahimizadeh A, Malekmohammadi Z, Samie S, Williamson WL, Amirzadeh M. Intramedullary mature teratoma with an exophytic component in an adult: Report of a case and literature review. Surg Neurol Int 2020;11:187.
Contributor Information
Abolfazl Rahimizadeh, Email: a_rahimizadeh@hotmail.com.
Zahed Malekmohammadi, Email: dr.malekmohammadi@gmail.com.
Saed Samie, Email: ssamie@parsgeneralhospital.com.
Walter L. Williamson, Email: wlw83@hotmail.com.
Mahan Amirzadeh, Email: mahan.amirzade@gmail.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alkherayf F, Arab AF, Tsai E. Conus medullaris teratoma with utilization of fiber tractography: Case report. J Neurol Surg Rep. 2015;76:e183–7. doi: 10.1055/s-0035-1555134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beneš V, Barsa P, Mikuláštík J, Suchomel P. Exophytic intramedullary mature teratoma of the conus medullaris: Case report and review of the literature. Cent Eur Neurosurg. 2009;70:154–60. doi: 10.1055/s-0028-1082062. [DOI] [PubMed] [Google Scholar]
- 3.Ghostine S, Perry E, Vaynman S, Raghavan R, Tong KA, Samudrala S, et al. The rare case of an intramedullary cervical spinal cord teratoma in an elderly adult: Case report and literature review. Spine. 2009;34:E973–8. doi: 10.1097/BRS.0b013e3181ba0fe5. [DOI] [PubMed] [Google Scholar]
- 4.Jian W, Ying W, Chao Y. Intramedullary spinal teratoma of the conus medullaris: Report of two cases. Acta Neurochir (Wien) 2010;152:553–4. doi: 10.1007/s00701-009-0466-3. [DOI] [PubMed] [Google Scholar]
- 5.Jinlu Y, Ye L, Huang H. Coexistence of spinal teratoma of the conus medullaris and arteriovenous malformation in an adult: A case report. Turk Neurosurg. 2012;22:510–4. doi: 10.5137/1019-5149.JTN.3961-10.1. [DOI] [PubMed] [Google Scholar]
- 6.Mut M, Shaffrey ME, Bourne TD, Jagannathan J, Shaffrey CI. Unusual presentation of an adult intramedullary spinal teratoma with diplomyelia. Surg Neurol. 2007;67:190–4. doi: 10.1016/j.surneu.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Rahimizadeh A, Sharifi G. Spinal intramedullary epidermoid cysts: Three case presentations and literature review. Surg Neurol Int. 2020;11:17. doi: 10.25259/SNI_540_2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahimizadeh A, Soufiani H. Upper cervical intermedullary lipoma with extension into the cistern magna in an elderly: Report of a case and review of the literature. World Spinal Column J. 2011;2:114–8. [Google Scholar]
- 9.Turgut M. Spinal intramedullary teratoma with exophytic components. Neurosurg Rev. 2004;27:137–8. doi: 10.1007/s10143-003-0314-5. [DOI] [PubMed] [Google Scholar]
- 10.Yamamoto J, Takahashi M, Nakano Y, Saito T, Kitagawa T, Ueta K, et al. Intratumoral hemorrhage because of primary spinal mixed germ cell tumor presenting with atypical radiological features in an adult. Spine J. 2013;13:e31–8. doi: 10.1016/j.spinee.2013.05.055. [DOI] [PubMed] [Google Scholar]


