Abstract
Objective
Assessing general (“global”) health is important to clinicians caring for patients, researchers studying patient subgroups, and epidemiologists tracking population trends. The Patient-Reported Outcomes Measurement Information System® (PROMIS®) introduced an adult self-report Global Health measure (ages 18+) in 2009 and pediatric versions (ages 5–17 years) in 2014. Our aim was to extend global health assessment to 1–5-year olds.
Methods
We used the PROMIS mixed-methods approach to develop PROMIS Early Childhood (EC) Global Health, emphasizing qualitative measure development guidance utilizing input from experts and parents. Quantitatively, we conducted two data collection waves with parents of 1–5-year olds and applied state-of-the-science measure development methods, including exploratory, confirmatory, and bi-factor analytics, particularly regarding potentially multi-dimensional Global Health item content. We conducted a series of hypothesis-based across-domain association analyses, which were more exploratory in nature, and known-groups validity analyses.
Results
Experts emphasized the physical, mental, and social facets of global health, and parents described the broader, overarching construct. Using Waves 1 (N = 1,400) and 2 (N = 1,057) data, we retained six items directly sourced from the age 5–17 version and two new items. The resulting 8-item PROMIS EC Global Health was sufficiently unidimensional, so we fit item responses to the graded response model for parameter estimation. This produced an 8-item scale with one total score. Across-domain associations and known-groups validity analyses largely supported our hypotheses.
Conclusions
We achieved our aim to extend global health assessment to 1–5-year olds and to thereby expand the range of PROMIS life course global health assessment from children aged 1–17 years, to adults of all ages.
Keywords: health promotion and prevention, infancy and early childhood, measure validation, preschool children, quality of life
Introduction
The concept of global health, that is, general or overall health, is so familiar that it can defy description. Simple greetings shared between neighbors and colleagues—“Hello! How are you doing?”—illustrate this concept’s ubiquity, its assumed comprehension, and its importance. The formal assessment of global health status is also of considerable significance: to clinicians in their care of individual patients, to researchers in their widely diverse range of studies and study settings, including patient subgroups and treatment regimens, and to epidemiologists in their describing and tracking of population trends.
In 2009, in its first step toward providing a life course assessment of global health status, the Patient-Reported Outcomes Measurement Information System® (PROMIS®) initiative introduced a 10-item self-report Global Health measure for adults ages 18 years and older (Hays et al., 2009, 2017). Its item content covers the three dimensions of the PROMIS conceptual framework for health, adopted from the World Health Organization (WHO) tri-dimensional conceptualization of human health (i.e., physical, mental, and social health), which now facilitates the mapping of PROMIS measures onto the WHO International Classification of Functioning, Disability, and Health (Cella et al., 2007; Tucker et al., 2014; World Health Organization, 1948). PROMIS Global Health provides 4-item evaluations of Physical and Mental Health, respectively, as well as single-item scores for overall health and pain intensity. In 2014, PROMIS introduced two 7-item pediatric Global Health measures, one self-report (for children ages 8–17 years) and one parent-proxy-report (for children ages 5–17 years; Forrest et al., 2014, 2016). As with the adult Global Health items, the pediatric items also include content covering physical, mental, and social health; they yield a total Global Health score. Items measuring pain and fatigue can optionally be added to the 7-item version, producing “Global Health 7 + 2” versions, with the same total Global Health score and single-item scores for fatigue and pain.
In this study, our aim was to extend global health assessment to 1–5-year olds, thereby expanding the reach of PROMIS life course global health assessment. We strove to maintain consistency with both the adult and pediatric Global Health measures while ensuring the developmental appropriateness of extant items and adequate coverage of developmentally meaningful facets that may not be covered in the version for older children and youth. Conceptually, this meant including existing health dimensions or “facets” from the adult and pediatric measures (physical, mental, social health). Practically, it meant ensuring a more uniform assessment of Global Health for children across the ages of 1–17 by retaining, to the extent possible, pediatric Global Health measure-specific item content, item framing, and item response option sets. Unlike pediatric Global Health, with both self-report and parent-proxy-report versions, PROMIS Early Childhood (EC) Global Health is a parent-report measure only.
To achieve our aim, we used the PROMIS mixed-methods approach (Cella et al., 2007, 2010; Forrest et al., 2012) to develop PROMIS EC Global Health. We placed considerable emphasis on qualitative guidance, utilizing input from experts and especially from parents, the eventual responders to PROMIS EC Global Health. Quantitatively, we applied psychometric state-of-the-science measure development methods (e.g., bifactor analysis for confirming essential unidimensionality), particularly for addressing the question of whether there are multiple, distinct dimensions versus multiple related facets (i.e., conceptual aspects within a dimension) in Global Health item content. Finally, we conducted a series of exploratory hypothesis-based across-domain association analyses and a specific set of known-groups validity analyses.
Methods
For detailed methods used across the PROMIS EC measures, see Cella et al. (qualitative methods, this issue) and Lai et al. (quantitative methods, this issue). Data available upon request.
Concept Specification
To develop a shared conceptualization of global health in early childhood, we hosted a half-day meeting with 17 transdisciplinary experts, who reviewed the existing PROMIS pediatric Global Health instrument content and domain framework (Forrest et al., 2014, 2016). They discussed its applicability to younger children, including item modifications and whether additional content/facets were required to make it developmentally appropriate for 1–5-year olds. For additional details about participating experts, see supplementary materials in Cella et al. (this issue). We then conducted semi-structured interviews with 13 parents to understand their definitions of early childhood global health and how they perceive their own 1–5-year-old child’s global health. We considered the qualitative guidance derived from parental input as particularly weighty, as it is parents who will respond to PROMIS EC Global Health. Therefore, we made the a priori decision to defer to a parental conceptual perspective, should an unresolvable discrepancy arise between parents versus expert thinking. See Cella et al. (this issue) and associated supplementary materials for additional details regarding parent concept elicitation interviews, including participant demographics, interview protocols, and coding procedures.
Draft Item Pool Development
Our initial goal was to develop an item pool reflecting children’s overall health, as perceived by parents. An attempt was made to conceptually align this item pool with the existing PROMIS Parent Proxy Scale v1.0—Global Health 7 + 2 measure for 5–17-year olds (Forrest et al., 2014, 2015), understanding that some modifications might be necessary for assessing younger children. We evaluated each of the nine existing items for developmental appropriateness in the context of expert meeting notes and parent interview results. All draft items underwent a Spanish translatability review (Devine et al., 2018), followed by cognitive interviews with five parents per item, with each item reviewed by at least one set of non-white parents and one parent with less than a 12th grade education. For additional details about cognitive interview participant recruitment, see Cella et al. (this issue, Table III). Lexile reading-level analysis (Lennon & Burdick, 2004) was conducted on final items, which were retained if they were at or below a 6th grade reading level per PROMIS standards (PROMIS Cooperative Group, 2013).
Table III.
PROMIS EC Global Health Wave 2 Known-Groups Validity Evidence: Mean T-Score Differences
| Known-groups factor | Group | N | Global Health |
p-Value | 2g | |
|---|---|---|---|---|---|---|
| Mean | SD | |||||
| Physical conditiona | No | 830 | 50.8 | 8.85 | ||
| Yes | 214 | 47.0 | 9.21 | <.001 | 0.03 | |
| EBD conditionb | No | 927 | 51.1 | 8.53 | ||
| Yes | 110 | 41.9 | 9.35 | <.001 | 0.10 | |
| Any conditionc | No | 770 | 51.5 | 8.46 | ||
| Yes | 285 | 46.2 | 9.44 | <.001 | 0.07 | |
| Traumatic eventd | No | 857 | 50.7 | 8.77 | ||
| Yes | 200 | 47.2 | 9.57 | <.001 | 0.02 | |
| Income insecuritye | No | 946 | 50.6 | 8.83 | ||
| Yes | 109 | 45.1 | 9.29 | <.001 | 0.03 | |
| Unsafe environmentf | No | 658 | 50.6 | 8.90 | ||
| Yes | 398 | 49.1 | 9.17 | .008 | 0.01 | |
For example, allergies, asthma, obesity.
For example, anxiety, conduct problems, speech disorder.
Any physical or EBD condition.
For example, parent divorced, parent served jail time, child a victim of violence.
That is, hard to cover basics (food, housing) on family income.
For example, extent of problems with: heavy traffic, stranger danger, limited public transportation.
2 = eta2.
Item Bank Development and Psychometric Evaluation
We conducted two large-scale field tests to evaluate PROMIS EC Global Health items (see Lai et al., this issue, for details). All Wave 1 parents, both those randomized to Form A and to Form B questionnaires, completed all items of the PROMIS EC Global Health draft item pool; all Wave 2 parents completed items retained from Wave 1 analyses. For additional sample details, including demographic characteristics, see Table I in Lai et al. (this issue).
Table I.
PROMIS EC Global Health Item Descriptive Statistics
| Item ID | Item source ID | Item | Wave 1 |
Wave 2 |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | SD | Mean | Median | SD | ||||
| GH1 | Global01_PXR1 | In general, would you say your child’s health is: | 4.4 | 5 | 0.82 | 4.5 | 5 | 0.64 | |
| GH2 | Global02_PXR1 | In general, would you say your child’s quality of life is: | 4.5 | 5 | 0.78 | 4.6 | 5 | 0.61 | |
| GH3 | Global03_PXR1 | In general, how would you rate your child’s physical health? | 4.4 | 5 | 0.8 | 4.6 | 5 | 0.62 | |
| GH4 | Global04_PXR1a | In general, how would you rate your child’s mental health? | 4.4 | 5 | 0.87 | 4.6 | 5 | 0.66 | |
| GH5 | Global04_PXR1b | How would you rate your child’s mood? | 4.1 | 4 | 0.9 | 4.3 | 4 | 0.76 | |
| GH6 | glo_ec3r1 | How would you rate your child’s social skills? | 4 | 4 | 1.02 | 4.1 | 4 | 0.88 | |
| GH7 | Global04_PXR1c | How would you rate your child’s ability to think? | 4.3 | 5 | 0.84 | 4.5 | 5 | 0.69 | |
| GH8 | glo_ec1 | How well is your child meeting developmental milestones? | 4.2 | 5 | 0.99 | 4.4 | 5 | 0.81 | |
Note. SD = standard deviation. Source IDs are used across PROMIS instruments and can be used to compare exact item content across PROMIS EC and pediatric Global Health versions. Item response option set: excellent (5), very good (4), good (3), fair (2), and poor (1).
We conducted Wave 1 dimensionality analyses following established item bank/measure development standards (Reeve et al., 2007), employing classical test theory (CTT), exploratory and categorical confirmatory factor analysis (EFA, CCFA), and confirmatory bifactor analysis (CBFA). First, using CCT, we conducted item and scale analyses, obtaining distributional characteristics (e.g., means, medians, standard deviations [SDs], minimum/maximum observed scores). We conducted item-to-scale internal validity analyses (item-rest score correlations) to identify items poorly related (r < 0.4) to global health. Second, using EFA, we obtained a quantitative sense of PROMIS EC Global Health’s dimensionality, using the eigenvalue 1-to-2 ratio (>4.0) and percent of variance accounted for by eigenvalue 1 (>40%) as unidimensionality guidance criteria (Hu & Bentler, 1999; Kline, 2008; Lai et al., 2006, 2011b). Third, we used CCFA with inter-item polychoric correlations and a weighted least square mean- and variance-adjusted estimator (Muthen et al., 1997) to estimate a single-factor model for PROMIS EC Global Health and, at the item level, examined factor loadings for item-to-construct internal validity (loadings ≥ 0.50) and residual correlations for item local independence (r ≤ 0.20). At the measure level, we summarized CCFA results via standard overall model fit index criteria: confirmatory fit index (CFI) ≥ 0.90, Tucker–Lewis Index (TLI) ≥ 0.90, and root mean square error of approximation (RMSEA) < 0.10 (Hu & Bentler, 1999; Lai et al., 2011a, 2014). When a CCFA model suggested possible multi-dimensionality, we conducted a CBFA to diagnose its potential impact (Lai et al., 2006; McDonald, 1999). We determined if (a) analyzed items were essentially unidimensional (general factor omega-H > 0.80), and (b) the model’s general factor had a majority of reliable variance attributable to it (omega-H-to-omega ratio > 0.50), supporting use of a PROMIS EC Global Health total score (Reise et al., 2007, 2013). We combined evidence from CCFA and CBFA modeling to establish PROMIS EC Global Health’s essential unidimensionality, a requirement for item response theory (IRT) analyses. We confirmed Wave 1 dimensionality analyses by conducting corresponding Wave 1 (final item set) and Wave 2 analyses.
We conducted Wave 1 IRT-based analyses, again following established item bank/measure development standards (Reeve et al., 2007), employing IRT modeling, item misfit analysis, and differential item functioning (DIF) investigations. We modeled responses to PROMIS EC Global Health items using the graded response model (Samejima, 1997) and defined misfit as an item fit test ratio of chi-squared-to-degrees-of-freedom >3.0 (Crişan et al., 2017; Stark et al., 2006). We evaluated items for potential DIF based on child age (1–2 vs. 3–5 years) and sex (female vs. male). We confirmed Wave 1 IRT-based analyses by conducting corresponding Wave 2 analyses.
Centering and Calibration
We conducted multi-group item calibration analyses using Wave 2 response data as our centering (normative) sample while incorporating Wave 1 responses. We conducted scaled score analyses and obtained Waves 1 and 2 distributional characteristics (e.g., means, medians, SDs, minimum/maximum observed scores, skewness, excess kurtosis). We considered >15% of respondents receiving the minimum or maximum possible score as suggesting possible floor or ceiling effects (Terwee et al., 2007; Wamper et al., 2010). For skewness and excess kurtosis, we interpreted values between –1.0 and +1.0 as indicating distributional normality (Hair et al., 2017). Following centering and calibration, we conducted Waves 1 and 2 reliability analyses, obtaining Cronbach’s alpha internal consistency estimates and IRT-based estimates at the overall scale level (i.e., distribution-informed estimates, derived from observed T-scores and SEs) and the individual score level (i.e., unique for each T-score along the PROMIS EC Global Health measurement continuum; Pilkonis et al., 2014).
Across-Domain Associations and Known-Groups Validity
We examined Wave 2 normative sample associations between PROMIS EC Global Health scores and other PROMIS EC measure scores (e.g., see Blackwell et al., Sherlock et al., Lai et al., this issue, for descriptions of these other PROMIS EC measures) using Pearson r correlations. We used Cohen’s (1988) standard criteria to assess strength of associations: r = 0, no correlation; r = below ±0.10, low; r = ±0.30, moderate; r ±0.50, large; r = 1, perfect correlation. We hypothesized correlations between PROMIS EC Global Health and other PROMIS EC domains that are both reflective of and impacted by one’s general health status. Specifically, we hypothesized positive correlations with the positively-valenced measures—PROMIS EC Engagement—Curiosity, Engagement—Persistence, Self-Regulation—Flexibility, Self-Regulation—Frustration Tolerance, Physical Activity, Positive Affect, and Social Relationships—and negative correlations with the negatively-valenced measures—PROMIS EC Anxiety, Depressive Symptoms, Anger/Irritability, and Sleep Problems.
We also established known groups based on parent-reported (a) physical condition (e.g., allergies, asthma, obesity; yes vs. no); (b) emotional/behavioral/developmental (EBD) condition (e.g., anxiety, conduct problems, speech disorder; yes vs. no); (c) any condition (i.e., any physical or EBD condition; yes vs. no); (d) child experienced at least one adverse life event (e.g., parent divorced, parent served jail time, child a victim of violence; yes vs. no; Ghandour et al., 2018); (e) income insecurity (i.e., hard to cover basics such as food and housing; yes vs. no; Ghandour et al., 2018); and (f) parent-perceived neighborhood environment stressors (e.g., problems with heavy traffic, stranger danger; yes vs. no; Timperio et al., 2004, 2005, 2006). We hypothesized each known group with a reported physical and/or EBD condition, traumatic life event, income insecurity, or parent-perceived “unsafe” neighborhood environment would have relatively worse PROMIS EC Global Health mean scores. We investigated groups as to their PROMIS EC Global Health mean score differences using one-way analysis of variance. We used as our effect size measure with the following interpretations: “small” = 0.01–0.05; “medium” = 0.06–0.14; “large” = >0.14 (Cohen, 1988).
Results
Concept Specification
Experts agreed that the concept of global health was relevant for young children and considered it well-represented by the current PROMIS facets (physical, mental, social). Experts’ review of the PROMIS Parent Proxy Scale v1.0—Global Health 7 + 2 items led to three primary considerations: (a) divide the mental health item (“In general, how would you rate your child’s mental health, including mood and ability to think?”) into two items to capture its emotional (“mood”) and cognitive (“ability to think”) components separately; (b) add an item about meeting general developmental milestones; and (c) examine parents’ understanding and interpretation of “quality of life” for young children.
Parents, somewhat distinctly from our expert panel, had a holistic view of children’s global health. While they often highlighted physical health (e.g., “Health means no illnesses”), they expanded upon this narrow definition by explaining general health as an overarching construct. As one parent noted, “When I think about health, it’s kind of been a total package thing, so it’s not just the food. It’s also activity, social. How does he interact with other kids his age? And then emotional as well.” Parents also confirmed the need for separate mental health items. Three parents described mental health as cognitive abilities, while others described mental health in terms of their children’s mood and emotional state (e.g., happy, mad). They also noted the importance of meeting developmental milestones as a core component of young children’s health, with one parent explaining, “Is he making any kind of advancement on the growth chart? How is [sic] his language skills for his age? Is he hitting his milestones?” Another parent said, “I think they (health, developmental milestones) are in the same category because you want your children to meet those milestones and if they don’t, you’re kind of like, something’s not right.” Parents similarly discussed quality of life as part of health but noted its dependence on the child’s broader social context, noting that it depends on access to quality food and education, having stimulating experiences and opportunities to explore the environment, and having quality relationships. Finally, all but one parent expressed the importance of children’s social health, in addition to general physical and mental health. Parents primarily described social health as interacting well with others.
Draft Item Pool Development
We developed the PROMIS EC Global Health domain framework based on the existing PROMIS pediatric domain framework, with modifications derived from expert input and parent interviews. We confirmed the need for three primary facets (physical, mental, and social health) as well as the inclusion of more global concepts of developmental milestones and quality of life.
An important goal in developing the new PROMIS EC Global Health parent-report measure was to maintain consistency, to the extent possible, with the existing PROMIS pediatric parent-proxy Global Health measure, both in item wording and concepts. Therefore, we retained all nine existing items from the PROMIS Parent Proxy Scale v1.0—Global Health 7 + 2 instrument and developed an additional nine items to test in cognitive debriefing (N = 18 total items). Specifically, we separated the existing mental health item into three items, adding two age-appropriate items for the mental health domain; added developmental milestones and social health items; and modified three existing items. For consistency, we used the primary 5-point Likert-type response option set utilized by existing PROMIS Global Health instruments for the 11 “how would you rate” items (i.e., excellent, very good, good, fair, poor); for the 7 “how often” items, we used two frequency-oriented response option sets (i.e., never, rarely, sometimes, often, always; and never, almost never, sometimes, often, almost always).
All new items were tested via cognitive interviews with at least five parents of 1–5-year olds, except for “How often does your child seem really sad?”; the change to this item was minor, and a similar item (“My child seemed sad”) was tested as part of the depressive symptoms measure development (see Sherlock et al., this issue). We also tested the existing item, “My child had pain,” to determine whether parents felt it was relevant for their children. Of the 10 items included in cognitive interviews, six were retained without revisions; two were revised, retested, and subsequently retained; and two were removed (see Supplementary Material A for details on the item retention and revision process). The PROMIS EC Global Health draft item pool contained 16 items: seven original and seven modified pediatric parent-proxy Global Health items and two new items. Lexile reading analysis showed all items were at the beginning reader level (i.e., BR100L-0L) and thus retained.
Item Bank Development and Psychometric Evaluation
Using Wave 1 data, we evaluated the PROMIS EC Global Health item pool dimensionality, determined items to be included for Wave 2 testing, and estimated initial item parameters. A series of EFAs led to removing five items (four original and one modified item), due to: (a) content redundancy (N = 1; “In general, how would you rate your child’s mental health, including mood and ability to think?” [response options: “poor” to “excellent”]); (b) developmental inappropriateness (N = 1; “How often does your child feel that you listen to his or her ideas?” [response options: “never” to “always”]); and (c) low relevance for most children (i.e., item-rest correlation <0.40; N = 3; “My child got tired easily;” “My child had pain;” and “My child had trouble sleeping when he/she had pain” [response options: “never” to “almost always”]). For the remaining 11 items, the eigenvalue 1-to-2 ratio was 5.44, and the percent of variance accounted for by eigenvalue 1 was 61.6; both guidance values supported item set unidimensionality. Of note, though, was eigenvalue 2 accounting for 11.3% of variance beyond eigenvalue 1, providing a caution about possible secondary multi-dimensionality.
In a single-factor CCFA model, three item factor loadings were <0.30. For overall model fit of the single-factor model, fit indices were as follows: CFI = 0.93, TLI = 0.92, RMSEA = 0.16. The relatively high RMSEA value may have been due to multidimensionality among the 11 retained items. We therefore pursued CBFA based on EFA promax rotation findings with two local factors. Results supported excellent overall model fit (CFI = 0.99, TLI = 0.98, RMSEA = 0.07). All items had higher factor loadings on the general factor than on local factors. Given these results, we concluded these 11 items were sufficiently unidimensional for IRT modeling.
In GRM analyses, three items had very low slope parameter estimates (i.e., 0.65, 0.93, and 1.08); these poorly discriminating items (“How often does your child have fun with other children?,” “How often does your child come to you or other parent for help if he/she needs it?,” and “How often does your child seem really sad?” [response options: “never” to “always”]) were therefore removed. The eight remaining items all fit our IRT model (i.e., all χ2/df ratios were <3). No items were flagged for DIF based on child age and sex, resulting in a final 8-item instrument (see Table I).
We conducted a final 8-item CCFA and obtained the following overall model fit indices: CFI = 0.94, TLI = 0.92, RMSEA = 0.21. We then confirmed the Wave 1 data-based PROMIS EC Global Health 8-item set as essentially unidimensional using CBFA: general factor omega-H = 0.85; omega-H-to-omega ratio = 0.88, that is, the general factor had 88% of reliable variance attributable to it. Therefore, CBFA modeling with Wave 1 data established PROMIS EC Global Health items as essentially unidimensional.
We conducted confirming analyses with Wave 2 data. EFA results showed the eigenvalue 1-to-2 ratio was 6.46, and the percent of variance accounted for by eigenvalue 1 was 69.64, supporting essential unidimensionality. CCFA resulted in all factor loadings ≥0.50, and all residual correlations were ≤0.20; thus, items met validity and independence criteria. The overall model fit indices were as follows: CFI = 0.96, TLI = 0.94, RMSEA = 0.20. We confirmed the conclusion made with Wave 1 data that PROMIS EC Global Health items were essentially unidimensional using CBFA: general factor omega-H = 0.89; omega-H-to-omega ratio = 0.92, that is, the general factor had 92% of reliable variance attributable to it. Therefore, combined evidence from CCFA and CBFA modeling across Wave 1 and Wave 2 established PROMIS EC Global Health items as essentially unidimensional. In Wave 2 IRT analysis, all items fit the GRM model, and no items showed DIF for child age or child sex.
For Waves 1 and 2, all item response option categories were utilized by parents with 8-item PROMIS EC Global Health. Item descriptive statistics by Wave are presented in Table I. Item means were somewhat high and ranged from 4.0 to 4.5 for Wave 1 and 4.1 to 4.6 for Wave 2. The summed score distribution for Wave 1 had a mean = 34.3, median = 36.0, and SD = 5.44 and for Wave 2 had a mean = 35.6, median = 37.0, SD = 4.33; minimum/maximum observed summed scores were 8 and 40, respectively (Wave 1) and 12 and 40, respectively (Wave 2). The lowest possible summed score (8) was observed once in Wave 1 (N = 1; 0.1%) and not at all in Wave 2. Approximately a fifth in each Wave (Wave 1: N = 249, 17.8%; Wave 2: N = 253, 23.9%) had the highest possible summed score (40), suggestive of a possible ceiling effect; this effect was investigated more thoroughly with PROMIS EC Global Health scaled scores. Inter-item correlations ranged from 0.48 to 0.88 for Wave 1 and from 0.49 to 0.93 for Wave 2 (see Table II). No item had an item-rest score correlation (item-to-scale internal validity) below criterion in either Wave; thus, all items appeared sufficiently related to the PROMIS EC Global Health construct (minimum/maximum r = 0.66/0.77).
Table II.
PROMIS EC Global Health Inter-Item Correlations by Data Collection Wave
| GH1 | GH2 | GH3 | GH4 | GH5 | GH6 | GH7 | |
|---|---|---|---|---|---|---|---|
| Wave 1 | |||||||
| GH2 | 0.80 | ||||||
| GH3 | 0.88 | 0.81 | |||||
| GH4 | 0.59 | 0.65 | 0.61 | ||||
| GH5 | 0.51 | 0.52 | 0.53 | 0.76 | |||
| GH6 | 0.48 | 0.49 | 0.48 | 0.71 | 0.67 | ||
| GH7 | 0.57 | 0.58 | 0.58 | 0.79 | 0.69 | 0.69 | |
| GH8 | 0.59 | 0.56 | 0.57 | 0.75 | 0.64 | 0.71 | 0.77 |
| Wave 2 | |||||||
| GH2 | 0.72 | ||||||
| GH3 | 0.93 | 0.75 | |||||
| GH4 | 0.73 | 0.77 | 0.75 | ||||
| GH5 | 0.61 | 0.64 | 0.65 | 0.80 | |||
| GH6 | 0.50 | 0.51 | 0.49 | 0.66 | 0.68 | ||
| GH7 | 0.56 | 0.54 | 0.55 | 0.67 | 0.58 | 0.65 | |
| GH8 | 0.62 | 0.58 | 0.61 | 0.67 | 0.58 | 0.70 | 0.77 |
Centering and Calibration
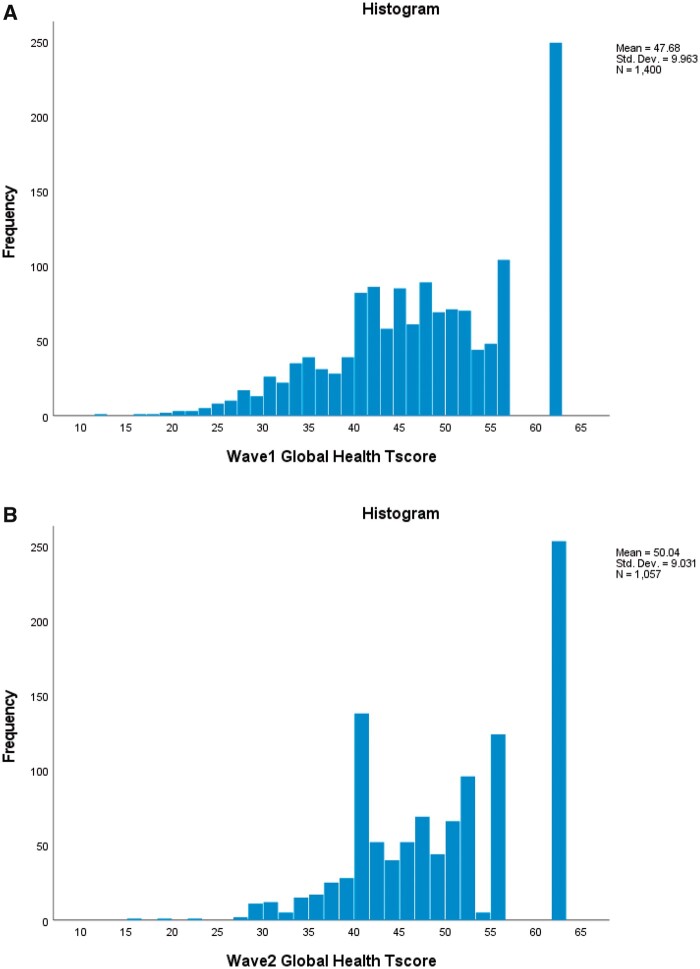
We used Wave 2 as the representative sample for PROMIS EC Global Health measure centering, incorporated Wave 1 into our analyses, and successfully conducted multi-group item calibration analyses for the 8-item PROMIS EC Global Health measure. The T-score distribution of PROMIS EC Global Health had a mean = 47.7, median = 47.8, and SD = 9.96 for Wave 1 (mean = 50.0, median = 50.2, SD = 9.03 for Wave 2); minimum/maximum observed T-scores were 11.6 and 61.9, respectively for Wave 1 (15.4 and 61.9, respectively for Wave 2). An N of 1 (0.1%) of Wave 1 [N = 0 (0.0%) of Wave 2] had the lowest possible T-score, while N = 249 (17.8%) of Wave 1 [N = 253 (23.9%) of Wave 2] had the highest possible T-score, indicative of a ceiling effect. Skewness was –0.32, and excess kurtosis was –0.43 for Wave 1 (skewness = –0.25, excess kurtosis = –0.67 for Wave 2). Thus, PROMIS EC Global Health T-scores from Wave 1 and Wave 2 appeared normally distributed but with an observed ceiling effect (see Figure 1A and B).
Figure 1.
PROMIS EC Global Health T-score distributions. (A) Wave 1 T-score distributions. (B) Wave 2 T-score distribution.
Cronbach’s alpha was 0.90 for Wave 1 (0.89 for Wave 2), indicating very good (≥0.80) to excellent (≥0.90) CTT-based overall internal consistency reliability. Similarly, IRT-based reliability at the overall scale level was 0.90 for Wave 1 (0.88 for Wave 2), also indicating very good-to-excellent IRT-based overall internal consistency reliability. IRT-based score-level reliability was excellent for individual T-scores ranging from 10 to 51 (see Figure 2).
Figure 2.
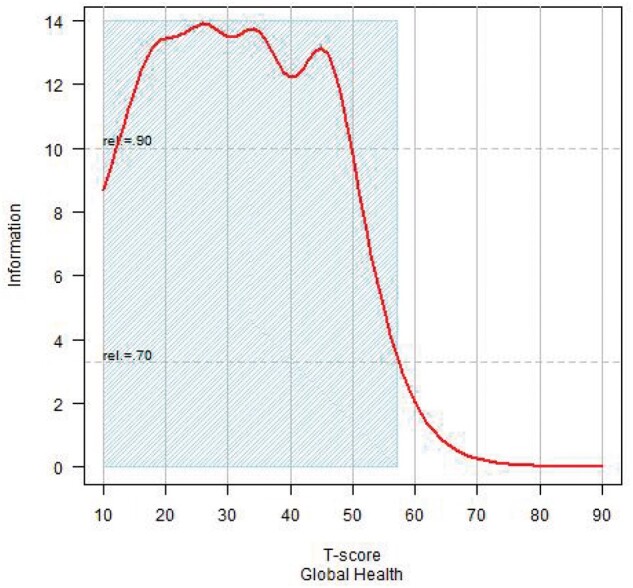
PROMIS EC Global Health test information, reliability, and combined Wave 1/Wave 2 T-score distribution. Note. Shading indicates the range of T-scores where reliability ≥0.70. The abbreviation “rel.” stands for “reliability.” Statistical “information” is related to score standard error (SE) and reliability. For example, when information = 10, SE = 3.16, and reliability = 0.90.
Across-Domain Associations and Known-Groups Validity
Wave 2 associations between PROMIS EC Global Health and the PROMIS EC well-being domains of Engagement—Curiosity, Engagement—Persistence, Self-Regulation—Flexibility, Self-Regulation—Frustration Tolerance, Positive Affect, and Social Relationships were all positive and of moderate magnitude (0.37–0.46); the associations between PROMIS EC Global Health and PROMIS EC negative health domains, that is, Depressive Symptoms, Anger/Irritability, Anxiety, and Sleep Problems, were negative and of or approaching moderate magnitude (–0.27 to –0.36). Conversely, the association between PROMIS EC Global Health and PROMIS EC Physical Activity was significantly lower in magnitude (0.08). This may, in part, be due to PROMIS EC Global Health having a general, overall health status assessment objective and an unspecified time context, while PROMIS EC Physical Activity has a distinctly different targeted, number of days-related frequency of play and physical activity assessment objective and an “In the last 7 days” time context. See Table IV in Lai et al. (this issue) for the full correlation matrix.
All known-groups analyses based on reported physical condition, EBD condition, any condition (physical and/or EBD), traumatic life event, income insecurity, and parent-perceived neighborhood “unsafe” environment were statistically significant (p < .05). The EBD condition and any condition analyses had medium effect sizes; the physical condition, traumatic life event, and income insecurity analyses had small effect sizes; and the “unsafe” environment analysis had a trivial effect size. Each “negative condition present” group had lower mean PROMIS EC Global Health scores (see Table III).
Discussion
A primary aim of the current measurement development initiative was to maintain conceptual consistency with established adult and pediatric PROMIS Global Health measures, incorporating their assessed facets of physical, mental, and social health into PROMIS EC Global Health, while ensuring a developmentally-appropriate assessment of global health for youth in early childhood. To ensure children ages 1–17 years can be assessed for global health status as uniformly as possible, we also maintained a practical level of consistency with pediatric Global Health. First, we retained item content from the existing pediatric instrument, with six of the PROMIS EC Global Health’s eight items directly sourced from the pediatric version. Second, we retained item framing, employing the “In general” frame where it had been employed by pediatric Global Health and then used no framing for other item content, as had been done for the pediatric version. Finally, we retained the main item response option sets from the pediatric Global Health measure. Unlike the pediatric version, with self-report and parent proxy versions, PROMIS EC Global Health was developed as a parent report measure only due to its targeting children aged 1–5 years, for whom self-report measure completion is unrealistic.
From our qualitative work, both experts and parents recommended distinct items be included to assess “mental health,” “mood,” and “ability to think.” Both experts and parents also recommended including an item assessing “meeting developmental milestones.” We consider this item a reading of global parental perceptions of milestones, and we justify its use based on its reported performance. Future research can help evaluate its relevance to formal objective measures of developmental milestones, as well as its status within the conceptualization of global health as a unique dimension or intrinsically linked to physical, mental, and social health.
Parents described subtle distinctions between “health” and “quality of life,” with “health” being a more basic, fundamental state and “quality of life” referring to the degree to which one can thrive, have stimulating experiences, and lead a joyful life. Experts deferred to parents’ understanding and interpretation of “quality of life.” Parents recommended asking about social health. Both expert and parent recommendations were incorporated in the development of the draft item pool; the soundness of those recommendations is evident in the final version of PROMIS EC Global Health, which retains items reflecting those recommendations.
Experts and parents differed in a nuanced but meaningful way in terms of defining the construct of global health. Experts emphasized the multi-component nature of global health, comprised of physical, mental, and social dimensions. Parents held a more holistic view, acknowledging the presence of physical, mental, and social facets but considered global health to be a singular, unified, overarching construct. Ultimately, our quantitative analyses supported both perspectives as we found PROMIS EC Global Health to be essentially unidimensional but comprised of the three primary dimensions of physical, mental, and social health.
Limitations and Future Directions
With the successful development of PROMIS EC Global Health, we achieved our aim of extending global health assessment to 1–5-year olds; simultaneously, we achieved a larger goal of expanding the range of PROMIS life course global health assessment, now from children aged 1–17 years to adults of all ages. For the field of pediatric psychology, this creates new assessment opportunities, single-point-in-time and longitudinal, regarding individual children and cohorts, for enhanced general health status monitoring, the supporting of clinical decision making, and the larger goal of improving outcomes. Using this instrument to more readily obtain a marker or signal of underlying health status may also help facilitate efforts to better understand child health psychology, particularly children with chronic conditions.
Because we found PROMIS EC Global Health to be essentially unidimensional, global health status can be reported using an overall score. For clinicians and investigators in pediatric psychology who are interested in specific global health facets (i.e., physical, mental, social health), individual item responses to PROMIS EC Global Health can be reviewed. Thus, for clinicians caring for individual patients, researchers studying patient subgroups, and epidemiologists tracking population trends, PROMIS EC Global Health offers brief yet robust status assessment for monitoring as well as investigative purposes.
For a broader perspective and discussion of our study’s qualitative and quantitative limitations, please see Cella et al. (qualitative methods, this issue) and Lai et al. (quantitative methods, this issue). For PROMIS EC Global Health, future work collecting time-separated data and longitudinal data can help establish test–retest reliability and responsiveness to change. Furthermore, we were limited in our ability to collect additional parent-report and non-parent report measures of general health; thus, future work evaluating PROMIS EC Global Health together with other reporting sources, such as objective measures (physical, mental health diagnoses), second parent/caregiver, educator (daycare, preschool teacher), and medical provider reports can further establish instrument validity. Studies to establish norms and cut-off scores for identifying at-risk children would be beneficial, as would a comprehensive, within and across national borders, cross-cultural validation effort. For PROMIS EC Global Health to be an international “go to” measure of global health status, it must establish evidence of its multi-cultural validity.
A “version 2” alternative for the PROMIS EC Global Health item “How well is your child meeting developmental milestones?” might be as follows: “In general, please rate how well your child is meeting developmental milestones.” Response options for both item versions would remain the same (i.e., excellent, very good, good, fair, poor). The new item version could then be qualitatively and psychometrically evaluated in the context of a rigorous future study.
PROMIS EC Global Health offers a brief and convenient means of obtaining a measurement of early childhood global health status. Used for single-point-in-time or longitudinal assessment, the measurements it provides function as easily obtained markers or signals of underlying health status. As such, when those measurements indicate, for example, excellent or poor health status, or when change in measurements across time suggests important shifts in a child’s health status, those measurements themselves might now be employed as “flags” or “triggers” prompting further investigation into the inter-connections between child health status and child health psychology.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Funding
Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) program, Office of The Director, National Institutes of Health, under Award Number U24OD023319, with co-funding from the Office of Behavioral and Social Sciences Research (OBSSR; Person Reported Outcomes Core).
Conflicts of interest: None declared.
Supplementary Material
References
- Cella D., Riley W., Stone A., Rothrock N., Reeve B., Yount S., Amtmann D., Bode R., Buysse D. J., Choi S., Cook K., Devellis R., Dewalt D., Fries J. F., Gershon R., Hahn E. A., Pilkonis P., Revicki D., Rose M., Lai J.-S; PROMIS Cooperative Group. (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2965562/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D., Yount S., Rothrock N., Gershon R., Cook K., Reeve B., Ader D., Fries J. F., Bruce B., Rose M.; PROMIS Cooperative Group. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH roadmap cooperative group during its first two years. Medical Care, 45(5 Suppl 1), S3–S11. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2829758/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. (1988). Statistical power analysis for the behavioral sciences. Routledge Academic. [Google Scholar]
- Crişan D. R., Tendeiro J. N., Meijer R. R. (2017). Investigating the practical consequences of model misfit in unidimensional IRT models. Applied Psychological Measurement, 41(6), 439–455. 10.1177/0146621617695522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine J., Klasen F., Moon J., Herdman M., Hurtado M. P., Castillo G., Haller A. C., Correia H., Forrest C. B., Ravens-Sieberer U. (2018). Translation and cross-cultural adaptation of eight pediatric PROMIS® item banks into Spanish and German. Quality of Life Research, 27(9), 2415–2430. https://www.ncbi.nlm.nih.gov/pubmed/29766439 [DOI] [PubMed] [Google Scholar]
- Forrest C., Tucker C., Ravens-Sieberer U., Pratiwadi R., Moon J., Teneralli R., Becker B., Bevans K. (2016). Concurrent validity of the PROMIS® pediatric global health measure. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 25(3), 739–751. 10.1007/s11136-015-1111-7 [DOI] [PubMed] [Google Scholar]
- Forrest C. B., Bevans K. B., Pratiwadi R., Moon J., Teneralli R. E., Minton J. M., Tucker C. A. (2014). Development of the PROMIS® pediatric global health (PGH-7) measure. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 23(4), 1221–1231. 10.1007/s11136-013-0581-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest C. B., Bevans K. B., Tucker C., Riley A. W., Ravens-Sieberer U., Gardner W., Pajer K. (2012). Commentary: The Patient-Reported Outcome Measurement Information System (PROMIS®) for children and youth: application to pediatric psychology. Journal of Pediatric Psychology, 37(6), 614–621. 10.1093/jpepsy/jss038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghandour R. M., Jones J. R., Lebrun-Harris L. A., Minnaert J., Blumberg S. J., Fields J., Bethell C. D., Kogan M. D. (2018). The design and implementation of the 2016 National Survey of Children’s. Maternal and Child Health Journal, 22(8), 1093–1102. 10.1007/s10995-018-2526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair J., Hult G., Ringle C., Sarstedt M. (2017). A primer on partial least squares structural equation modeling (PLS-SEM) (2nd edn). Sage. [Google Scholar]
- Hays R. D., Bjorner J., Revicki R. A., Spritzer K. L., Cella D. (2009). Development of physical and mental health summary scores from the Patient Reported Outcomes Measurement Information System (PROMIS) global items. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 18(7), 873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays R. D., Schalet B. D., Spritzer K. L., Cella D. (2017). Two‐item PROMIS® global physical and mental health scales. Journal of Patient-Reported Outcomes, 1(1), 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L. T., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Kline R. B. (2008). Principles and practice of structural equation modeling (2nd edn). Guilford Press. [Google Scholar]
- Lai J.-S., Cella D., Choi S., Junghaenel D. U., Christodoulou C., Gershon R., Stone A. (2011). How item banks and their application can influence measurement practice in rehabilitation medicine: A PROMIS fatigue item bank example. Archives of Physical Medicine and Rehabilitation, 92(10 Suppl), S20–S27. 10.1016/j.apmr.2010.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J.-S., Crane P. K., Cella D. (2006). Factor analysis techniques for assessing sufficient unidimensionality of cancer related fatigue. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 15(7), 1179–1190. 10.1007/s11136-006-0060-6 [DOI] [PubMed] [Google Scholar]
- Lai J.-S., Zelko F., Butt Z., Cella D., Kieran M. W., Krull K. R., Magasi S., Goldman S. (2011). Parent-perceived child cognitive function: results from a sample drawn from the US general population. Child's Nervous System: ChNs: Official Journal of the International Society for Pediatric Neurosurgery, 27(2), 285–293. http://www.ncbi.nlm.nih.gov/pubmed/20652814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J.-S., Zelko F., Krull K., Cella D., Nowinski C., Manley P., Goldman S. (2014). Parent-reported cognition of children with cancer and its potential clinical usefulness. Quality of Life Research, 23(4), 1049–1058. 10.1007/s11136-013-0548-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennon C., Burdick H. (2004). Lexile frameworkas an approach for reading measurement and success. Lexile Framework for Reading. http://cdn.lexile.com/m/resources/materials/Lennon__Burdick_2004.pdf. Retrieved 1 March 2022. [Google Scholar]
- McDonald R. P. (1999). Test theory: A unified treatment. Lawrence Earlbaum Associates, Inc. [Google Scholar]
- Muthen B. O., Du Toit S. H. C., Spisic D. (1997). Robust inference using weighted least squares and quadratic estimating equations in latent variable modeling with categorical and continuous outcomes. Unpublished technical report. https://www.statmodel.com/download/Article_075.pdf. Retrieved 1 March 2022. [Google Scholar]
- Pilkonis P. A., Yu L., Dodds N. E., Johnston K. L., Maihoefer C. C., Lawrence S. M. (2014). Validation of the depression item bank from the Patient-Reported Outcomes Measurement Information System (PROMIS) in a three-month observational study. Journal of Psychiatric Research, 56, 112–119. 10.1016/j.jpsychires.2014.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- PROMIS Cooperative Group (2013). PROMIS® instrument development and validation scientific standards (Version 2.0). https://www.healthmeasures.net/images/PROMIS/PROMISStandards_Vers2.0_Final.pdf. Retrieved 1 March 2022.
- Reeve B. B., Hays R. D., Bjorner J. B., Cook K. F., Crane P. K., Teresi J. A., Thissen D., Revicki D. A., Weiss D. J., Hambleton R. K., Liu H., Gershon R., Reise S. P., Lai J. S., Cella D.; PROMIS Cooperative Group. (2007). Psychometric evaluation and calibration of health-related quality of life item banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Medical Care, 45(5 Suppl 1), S22–S31. 10.1097/01.mlr.0000250483.85507.04 [DOI] [PubMed] [Google Scholar]
- Reise S. P., Morizot J., Hays R. D. (2007). The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Quality of Life Research, 16 Suppl 1, 19–31. PM:17479357. [DOI] [PubMed] [Google Scholar]
- Reise S. P., Scheines R., Widaman K. F., Haviland M. G. (2013). Multidimensionality and structural coefficient bias in structural equation modeling a bifactor perspective. Educational and Psychological Measurement, 73(1), 5–26. [Google Scholar]
- Samejima F. (1997). The graded response model. In van der Linden W. J.,Hambleton R. (Eds.), Handbook of modern item response theory (pp. 85–100). Springer-Verlag. [Google Scholar]
- Stark S., Chernyshenko O. S., Drasgow F., Williams B. A. (2006). Examining assumptions about item responding in personality assessment: Should ideal point methods be considered for scale development and scoring? The Journal of Applied Psychology, 91(1), 25–39. 10.1037/0021-9010.91.1.25 [DOI] [PubMed] [Google Scholar]
- Terwee C. B., Bot S. D., de Boer M. R., van der Windt D. A., Knol D. L., Dekker J., Bouter L. M., de Vet H. C. (2007, Jan). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology, 60(1), 34–42. https://doi.org/S0895-4356(06)00174-0 [pii] [DOI] [PubMed] [Google Scholar]
- Timperio A., Ball K., Salmon J., Roberts R., Giles-Corti B., Simmons D., Baur L. A., Crawford D. (2006). Personal, family, social, and environmental correlates of active commuting to school. American Journal of Preventive Medicine, 30(1), 45–51. 10.1016/j.amepre.2005.08.047 [DOI] [PubMed] [Google Scholar]
- Timperio A., Crawford D., Telford A., Salmon J. (2004). Perceptions about the local neighborhood and walking and cycling among children. Preventive Medicine, 38(1), 39–47. 10.1016/j.ypmed.2003.09.026 [DOI] [PubMed] [Google Scholar]
- Timperio A., Salmon J., Telford A., Crawford D. (2005). Perceptions of local neighbourhood environments and their relationship to childhood overweight and obesity. International Journal of Obesity (2005), 29(2), 170–175. 10.1038/sj.ijo.0802865 [DOI] [PubMed] [Google Scholar]
- Tucker C. A., Cieza A., Riley A. W., Stucki G., Lai J. S., Ustun T. B., Kostanjsek N., Riley W., Cella D., Forrest C. B. (2014). Concept analysis of the patient reported outcomes measurement information system (PROMIS®) and the international classification of functioning, disability and health (ICF). Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 23(6), 1677–1686. [DOI] [PubMed] [Google Scholar]
- Wamper K. E., Sierevelt I. N., Poolman R. W., Bhandari M., Haverkamp D. (2010). The Harris hip score: Do ceiling effects limit its usefulness in orthopedics? Acta Orthopaedica, 81(6), 703–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (1948). Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference. New York, 19 June–22 July 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the WHO, no. 2, p. 100) and entered into force on April 7, 1948. World Health Organization, Geneva, Switzerland.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.