Abstract
Objective
Physical activity (PA) and sleep are leading health indicators for individuals of all ages. Monitoring young children’s PA and sleep using psychometrically sound instruments could help facilitate timely interventions to promote healthy development. This article describes the development of the PROMIS® Early Childhood (EC) Parent Report Physical Activity (PA) and Sleep Problems (SP) measures for children aged 1–5 years.
Methods
Item pools were generated by interviewing parents, input from content experts, and literature review. Data from a U.S. general population sample were used to determine factor structures of item pools via factor analytic approaches, estimate item parameters via item response theory (IRT) models, and establish norms. Pearson correlations were used to evaluate across-domain associations. Analysis of variance was used and known-groups’ validity of PA and SP by comparing their scores to PROMIS EC Parent Report Global Health: child’s physical, emotional, and mental conditions.
Results
Initial item pools consisted of 19 and 26 items for PA and SP, respectively. Factor analyses’ results supported unidimensionality of 5 and 16 items measuring PA and SP, respectively, which were then calibrated using IRT. Norms were established by centering to a probability-based U.S. general population. Computerized adaptive testing algorithms were established. Some analyses supported initial measure validity.
Conclusions
The PROMIS EC PA calibrated scale and SP item banks are user-friendly and brief, yet produce precise scores. Both measures enable psychometrically sound assessment of PA behavior and sleep problems. Future studies to comprehensively evaluate the validity of these two measures are warranted.
Keywords: health behavior, infancy and early childhood, measure validation, preschool children, quality of life, sleep
Introduction
Physical activity (PA), sedentary behavior, and sleep collectively constitute a movement behavior continuum across a child’s typical week. All components of the continuum are associated with overall health (Chaput et al., 2014). PA is recognized as a leading health indicator (Healthy People 2020, 2016) and can mitigate the early onset and burden of chronic disease (Lai et al., 2014), as well as improve motor skills, cognitive development, and skeletal health (Carson et al., 2017; Timmons et al., 2012). Sleep, a multidimensional construct including duration, timing, quality, sleepiness/wakefulness, and satisfaction with sleep (Buysse, 2014), is integral to developmental outcomes and is associated with multiple aspects of physical and emotional health (Felzer-Kim & Hauck, 2020; Hosker et al., 2019; Matricciani et al., 2019). Recent findings also show positive associations between moderate to vigorous PA and sleep among young children (Armstrong et al., 2019; Felzer-Kim & Hauck, 2020).
Recognizing the importance of PA and sleep in early childhood, the World Health Organization (Chomistek et al., 2012; World Health Organization, 2019) published guidelines for children under 5. For PA, guidelines are 30 min of daily activity for 0–1 year; 180 min daily for 1–2 years; and 180 min daily for 3–4 years, of which 60 min is moderate (3–<6 metabolic equivalents [METS]) to vigorous (≥6 METS). For sleep, guidelines are 12–16 hr daily for 0–1 year, 11–14 hr daily for 1–2 years, and 10–13 hr daily for 3–4 years (World Health Organization, 2019).
Despite the importance of activity and sleep in childhood (Carson et al., 2017; Hosker et al., 2019), relatively little research has addressed them in young children and few studies evaluate the relationship between PA and mental health outcomes in young children (Rodriguez-Ayllon et al., 2019); while a larger body of work exists on sleep and early childhood mental health, few extend beyond measures of individual sleep problem symptoms (e.g., difficulty falling asleep, night waking) to a holistic assessment that better aligns with clinical criteria for such conditions as insomnia disorders outlined in the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013). A major barrier is a lack of developmentally sensitive measures of PA and sleep problems that are user-friendly and inexpensive to implement. Though objective measures (e.g., accelerometers) are becoming increasingly prevalent, they only capture motion related to energy expenditure and sleep timing and duration. They cannot capture children’s lived experience, which is a critical component of patient-centered care (Institute of Medicine, 2001) and foundational to pediatric psychology (Anderson et al., 2020). Alternatively, most patient-reported outcome (PRO) measures for younger children are based on those used in older children; these are often inadequate for infants and preschoolers. For example, young children play and move “functionally” rather than for “exercise” and tend to move in short bursts of higher activity. Bipedal locomotion (walking, running), commonly used in PA measures, is less relevant given the youngest children are not necessarily walking yet. For young children, items that include actions of environmental exploration (e.g., reaching repeatedly outside the base of support, playing at low tables with frequent weight shifts) provide a more nuanced perspective on the stages of movement development. PRO measures of PA and sleep for this age group are thus critical to better understand these health behaviors in younger children. To fill this need, we developed the PROMIS® Early Childhood (EC) Parent Report Physical Activity (PA) and Sleep Problems (SP) measures for children aged 1–5 years. This article reports the development and psychometric evaluation of these two new instruments.
Methods
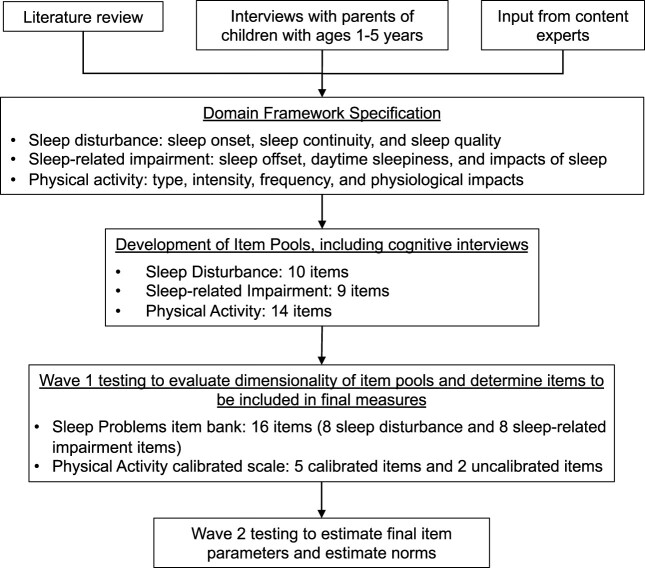
We applied the PROMIS methodology standards (PROMIS Cooperative Group, 2013), which are reviewed in depth in Cella et al. (this issue; qualitative methods) and Lai et al. (this issue; quantitative methods). Here, we focus on the PROMIS EC Physical Activity and Sleep Problems measures, with an overview of the steps used to develop these instruments provided in Figure 1. Data are available upon request.
Figure 1.
Steps to develop sleep problems item bank and Physical Activity calibrated scale. Note. A calibrated measure with 10 or more items is called an “item bank” while a measure with less than 10 items is called a “calibrated scale.” During Wave 1 testing, Sleep Problems and Physical Activity items were administered in Form A.
Concept Specification
In consultation with content experts via a series of conference calls and face-to-face meetings, we reviewed the existing PROMIS Pediatric Physical Activity (Tucker et al., 2014) and Sleep domain frameworks (Bevans et al., 2019) to determine whether existing facets were developmentally appropriate for early childhood and that items reflected expert knowledge of these domains as they pertain specifically to young children. In PROMIS, sleep is divided into two unidimensional constructs and associated item banks for individuals aged 8 years and older: Sleep Disturbance (trouble with sleep onset and maintenance) and Sleep-related Impairment (daytime function affected by poor sleep). We therefore started with these two separate sleep domains to be consistent with the PROMIS Pediatric sleep measures. Experts included developers of these original instruments, a pediatric physical therapist, a pediatric occupational therapist, a pediatric sleep specialist, developmental methodologists, and psychometricians. We also conducted concept elicitation interviews with 14 parents of children aged 1–5 years to understand parents’ perceptions of their child’s physical activity and sleep experiences. See Cella et al. (this issue) and accompanying supplementary materials for expert and participant details, interview guides, and qualitative data analysis procedures.
Draft Item Pool Development
We reviewed existing items from the PROMIS Pediatric Physical Activity, Sleep Disturbance, and Sleep-related Impairment item banks and measures recommended by content experts and those identified via comprehensive literature reviews, such as the Colorado Childhood Temperament Inventory (Rowe & Plomin, 1977), Infant Behavior Questionnaire (Bosquet Enlow et al., 2016), Observational System for Recording Physical Activity in Children—Preschool Version (Brown et al., 2006), Activity Scale for Kids (Young et al., 2000), Sleep Disturbance Scale for Children (Bruni et al., 1996), Children’s Sleep-Wake Scale (LeBourgeois & Harsh, 2016), and Children’s Sleep Habits Questionnaire (Goodlin-Jones et al., 2008). Description of concept specification experts are shown in Supplementary Material A in Cella et al. (this issue). We wrote new items or modified existing items to capture concepts not covered by existing PROMIS measures but raised by experts and/or interviewees. All newly developed or modified items were reviewed by at least five parents of young children to ensure content appropriateness and item readability. During these cognitive interviews, parents were also asked general questions about the appropriateness of the recall timeframe (past seven days) and response options. Any items with major revisions underwent additional review with five more parents. See Cella et al. (this issue, Table 3) for cognitive interview participant details. Final items underwent a Lexile reading-level analysis (Lennon & Burdick, 2004) and were retained if they were at or below a sixth grade reading level per PROMIS standards (PROMIS Cooperative Group, 2013).
Table III.
Planned Comparisons of Physical Activity Calibrated Scale and Sleep Problems Item Bank
| Variable | Physical activity |
Sleep problems |
||||
|---|---|---|---|---|---|---|
| All sample | 1–2 years | 3–5 years | All sample | 1–2 years | 3–5 years | |
| Physical activity | ||||||
| All sample | r a = 1 | |||||
| 1–2 years | r = 1 | |||||
| 3–5 years | r = 1 | |||||
| Sleep problems | ||||||
| All sample | r = 0.19*** | r = 1 | ||||
| 1–2 years | r = 0.23*** | r = 1 | ||||
| 3–5 years | r = 0.16*** | r = 1 | ||||
| Global health | ||||||
| All sample | r = 0.03 | r = −0.36*** | ||||
| 1–2 years | r = 0.05 | r = −0.35*** | ||||
| 3–5 years | r = 0.01 | r = −0.38*** | ||||
| Physical condition (0 vs. 1+) | ns | ns | ns | t = 9.81*** | t = 7.35*** | t = 7.09*** |
| Emotional/behavioral condition (0 vs. 1+) | t b = 3.0** | ns | t = 2.62** | t = 12.18*** | t = 7.64*** | t = 10.14*** |
| Vigorous activities frequency | c = 0.32*** | = 0.39*** | = 0.27*** | |||
Note. Vigorous activity frequency: “In the past 7 days, how many days did your child do vigorous physical activities for 30 min or more?” (no days; 1 day; 2–3 days; 4–5 days; 6–7 days); ANOVA = analysis of variance; ns = not significant at p < .05; *p < .05; **p < .01; ***p < .001.
Pearson correlation coefficient.
t-Value from t-test.
Spearman’s rho.
Item Bank Development and Psychometric Evaluation
Item pool psychometric properties were evaluated on data collected from two waves of testing: Wave 1 (Form A; n = 700) and Wave 2 (n = 1,057). See Lai et al. (this issue) for sample characteristics, data collection procedures, and analytic approaches. We used data from Wave 1 Form A to confirm the hypothesized factor structures of the Physical Activity and Sleep Problems item pools using confirmatory factor analysis (CFA) and/or a bi-factor analysis. We evaluated whether items fit Samejima’s (1997) graded response model (GRM), estimated initial item parameters, and evaluated measurement stability between ages (1–2 vs. 3–5 years), child sex (female vs. male), and parent sex (female vs. male) using differential item functioning (DIF). Using combined data from Wave 1 Form A and Wave 2, we estimated final item parameters using multi-group GRM analyses. The final parameters were centered on the Wave 2 sample because it was a probability-based sample, and data were weighted to match the U.S. Census Bureau’s March 2018 Current Population Survey. We evaluated score precision by estimating information function at the item and measure levels; the former was used to select items included in short forms, while the latter was used to describe characteristics of the measures, which were then transformed into item response theory (IRT)-based reliabilities. Scores were reported using the PROMIS T-score metric (mean = 50; standard deviation [SD] = 10). We simulated computerized adaptive testing (CAT) administration for item banks with >8 items and evaluated the mean and median number of items administered and Pearson r correlation between CAT score and full bank score.
Across-Domain Associations and Known-Groups Validity
We calculated Pearson correlation coefficients between Physical Activity and Sleep Problems and PROMIS EC Global Health. We hypothesized positive correlations among Physical Activity and Global Health, negative correlations between Physical Activity and Sleep Problems, and negative correlations between Sleep Problems and Global Health. Strength of associations was evaluated using standard criteria: r = 0, no correlation; r = below ±0.10, low; r = ±0.30, moderate; r ±0.50, large; r = 1, perfect correlation (Cohen, 1988). We evaluated known-groups differences using analysis of variance and hypothesized that: (a) children with (vs. without) physical health conditions will have lower levels of Physical Activity and worse Sleep Problems scores; (b) children with (vs. without) an emotional or behavioral condition or developmental delay/disorder (EBD; e.g., anxiety, conduct problems, autism spectrum disorder) will have worse Sleep Problems but no/negligible differences on Physical Activity; and (c) children with a higher frequency of weekly vigorous physical activity will have higher Physical Activity scores, as measured by the item, “In the past 7 days, how many days did your child do vigorous physical activities for 30 minutes or more?” (no days; 1 day; 2–3 days; 4–5 days; 6–7 days). Analyses were conducted across all participants as well as by child age (1–2 years, 3–5 years).
Results
Concept Specification
Physical Activity
Parents described five facets for their children’s PA behaviors that aligned with the existing PROMIS Pediatric PA domain framework: activity types (structured, unstructured), intensity, frequency, duration, and physiological impacts. First, all parents (n = 14) discussed a range of unstructured activity types (e.g., running around, walking, playing on the playground), and half (n = 6) discussed structured activity types (e.g., swim lessons, sports), all of whom had children 2 years and older. Some (n = 3) parents viewed such activities as pretend cleaning (e.g., using a toy sweeper) or pushing a toy shopping cart as PA in early childhood. Second, all 14 parents commented on the intensity of their children’s PA and used terms such as “really” or “very” active; “tons of” or “so much” energy; “non-stop” physically active; “more active” than other children; and “always on the go.” Third, parents reported a wide range of PA frequency and duration. When asked how many hours their child engaged in PA per day, parents said anywhere from 2 hr every other day to 10 hr per day. Parents who reported lower frequencies also said that their children were “very active,” indicating perceptions of “activity” levels varied. Finally, six parents reported physiological impacts of PA, most notably discussing how their children were more tired if they did more physical activities and less tired if they were less active.
Sleep Problems
For Sleep Disturbance, parents identified all three of the existing facets (sleep onset, continuity, and quality). The majority of parents (n = 10) discussed their children’s sleep onset, including five mentioning difficulties falling asleep. Parents also reported their children purposely resisted bedtime, engaging in such behaviors as crying, fussing. All parents (n = 14) reported that sleeping through the night (i.e., sleep continuity) was the prime indicator of sleep quality. Alternatively, poor sleep quality was described as waking up frequently in the middle of the night, tossing and turning, nightmares, and parasomnias. When asked about sufficient hours of sleep, parents reported 8–12 hr was “enough” sleep for their children. One parent noted, “It’s not just quantity of hours, it’s quality of sleep also,” suggesting the need to move beyond measuring hours of sleep to understanding how well the child slept.
For Sleep-related Impairment, parents described all five facets (sleep offset, daytime sleepiness, impact: cognitive, impact: affect and behavior, impact: activities). First, most parents (n = 11) discussed sleep offset, describing their children’s wakefulness as an indicator of whether the child had good sleep. Parents used phrases such as “rested and waking up on their own,” “being alert and ready to go,” and “looking well-rested” as specific sleep offset behaviors that indicated good sleep. Alternatively, parents reported “groggy and slow moving,” “waking up in a bad mood, cranky, or upset,” and “looking tired” as specific sleep offset indicators of poor sleep. Four parents discussed daytime sleepiness and used behavioral (e.g., yawning) and verbal indicators (e.g., child saying he/she was tired). All parents (n = 14) described the impact of sleep on their children’s daily lives: 14 discussed impact on affect and behavior (e.g., more temper-tantrums, cranky, fussy); 9 discussed impact on daily activities (e.g., not wanting to go to afterschool activities); and only 2 discussed cognitive impact (e.g., decreased attention).
Draft Item Pool Development
Based on parent concept elicitation interviews, input from content experts, and review of the existing PROMIS domain frameworks, we identified three facets within sleep disturbance, three facets within sleep-related impairment, and five facets within physical activity. For Sleep Disturbance, we retained the original three facets of sleep onset (difficulty falling asleep, intentional bedtime resistance), sleep continuity (staying asleep), and sleep quality (satisfaction with sleep). For Sleep-related Impairment, we retained two of the original facets—sleep offset (wakefulness) and daytime sleepiness (being tired during the day)—and merged the remaining three regarding impacts into a single facet called “impacts of sleep” that included impact of sleep quality on cognition, daily activities, and mood. For Physical Activity, we retained the original PROMIS Pediatric PA emphasis on children’s lived PA experience—a broader perspective of PA than the METS minutes based approach—and included facets of activity type (what physical activity the child engages in), intensity (physical exertion), frequency (how often child engages in physical activity), duration (length an activity lasts), and physiological impacts (bodily impact of physical activity, e.g., feeling more tired or needing more sleep, sweating, or breathing hard).
For Sleep and Physical Activity item pools, we compared PROMIS Pediatric Physical Activity (Tucker et al., 2014), Sleep Disturbance, and Sleep-related Impairment (Forrest et al., 2018) items to our identified facets to ensure conceptual alignment across ages. Content experts provided feedback on candidate items and identified potential content gaps via conference calls and face-to-face meetings. For Physical Activity, 288 items from 11 measures were reviewed. For the Sleep domains 392 items from 14 measures were reviewed. We excluded items that were not appropriate for younger children, such as items measuring exercise (e.g., “How many days did your child play or exercise so hard that his/her muscles burned?”), structured activities (e.g., “On a typical day, how often your child play team sports?”), and cognitive impacts from poor sleep (e.g., “My child had a hard time concentrating because he/she was sleepy.”). We also excluded items with similar content. For example, among 11 items measuring physical activity physiological symptoms, we retained three items assessing breathing, sweating and fatigue/tiredness. Items that did not have hierarchical orders and therefore could not be calibrated, such as locations (e.g., parks, home) and time of the day (e.g., morning, before bed), were also excluded. When possible, we used exact or similar wording to existing items when deemed developmentally appropriate for 1–5 years.
The resulting Physical Activity item pool included 19 items, including existing (n = 2) or modified (n = 6) PROMIS items and 11 new items. The 17 modified and new items were tested with parents via cognitive interviews, and 8 items were retained, 4 were revised, and 5 were dropped primarily due to redundancy. This resulted in 14 items: 7 physiological symptom items (e.g., breathing and sweating); 3 duration items asking numbers of days the child was physically active for 10, 30, or 60 min; 3 duration and intensity items asking the numbers of days child’s vigorous physical activities for 10, 30, or 60 min; and 1 overall item (“On a usual day, how physically active was your child?”). All items used the same frequency-based rating scale (no days, 1 day, 2–3 days, 4–5 days, and 6–7 days) except for the overall item, which used an intensity-based rating scale (not at all, a little bit, somewhat, quite a bit, and very much).
The Sleep Problems item pool included 14 sleep disturbance and 12 sleep-related impairment items, including 10 existing PROMIS items. The 16 new items were tested with parents via cognitive interviews: 9 items were retained without revisions and 7 were removed due to age-inappropriateness, redundancy, and lack of comprehensibility. This resulted in 19 Sleep Problems items (10 sleep disturbance, 9 for sleep-related impairment) with a frequency-based rating scale (never, almost always, sometimes, almost always, and always). All items were at or below a fifth grade reading level and thus retained. Information regarding items dropped, modified, or retained is shown in Supplementary Materials A and B.
Item Bank Development and Psychometric Evaluation
Physical Activity
Initial CFA showed unacceptable fit indices: comparative fit index (CFI) = 0.815, root mean square error of approximation (RMSEA) = 0.263, and four items had R-square < 0.3. After discussing with content experts, we explored a bi-factor model with two local factors: (a) physiological symptom items and (b) intensity/duration items. Due to the redundant nature among the intensity/duration items, (e.g., a child who is physically active for more than 60 min is also active for 10+ and 30+ min), a bi-factor model did not work. These findings were similar to our work developing the PROMIS Pediatric Physical Activity item bank. We therefore worked on models that focused on physiological symptoms with additional “physically active” and/or “vigorous physical activities” items and one overall item. A series of CFAs led to five physiological symptom items and one overall item with acceptable fit indices: CFI = 0.99, RMSEA = 0.08, R-square > 0.3 (except the overall item) and residual correlations < 0.15. The item, “On a usual day, how physically active was your child?” had a very low R-square of 0.02. Without this overall item, a borderline RMSEA (0.11) was obtained, and all other fit indices met criteria. The study team decided to include this overall item in GRM analysis but it had a very low slope (0.24) parameter, suggesting that it did not provide meaningful information in the Physical Activity measure and was therefore excluded from the subsequent analyses. GRM results indicated that the remaining five items fit the model with a chi-square to degree of freedom ratio <3. The final Physical Activity calibrated scale consisted of five IRT-calibrated and two non-calibrated items (“On a usual day, how physically active was your child?” and “How many days did your child do vigorous physical activities for 30 minutes or more?”). These two non-calibrated items were included because of their important content. Cronbach’s alpha of these 5 calibrated items was 0.82 (see Table I for descriptive statistics).
Table I.
Item Descriptive Information—Physical Activity Calibrated Scale
| Item stem | Wave 1 (N = 700) |
Wave 2 (N = 1057) |
||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Floor (%)a | Ceiling (%)a | Mean | SD | Floor (%)a | Ceiling (%)a | |
| How many days was your child so physically active that he/she sweated? | 2.83 | 1.28 | 21.00 | 10.71 | 3.39 | 1.22 | 11.64 | 19.58 |
| How many days did your child play so hard that he/she got physically exhausted? | 2.54 | 1.21 | 26.86 | 5.43 | 2.83 | 1.20 | 19.96 | 7.38 |
| How many days did your child play so hard that he/she fell asleep early? | 2.75 | 1.10 | 15.00 | 6.00 | 2.27 | 1.11 | 33.11 | 2.65 |
| How many days did your child play so hard that he/she needed an extra or longer nap? | 2.56 | 1.16 | 23.29 | 5.43 | 1.98 | 1.05 | 45.51 | 1.61 |
| How many days did your child play so hard that he/she felt tired? | 2.98 | 1.06 | 9.43 | 8.00 | 2.85 | 1.13 | 14.66 | 8.33 |
| How many days did your child do vigorous physical activities for 30 min or more?b | 3.16 | 1.36 | 16.43 | 21.71 | 3.00 | 1.32 | 20.34 | 13.91 |
| On a usual day, how physically active was your child?b | 4.22 | 0.84 | 0.86 | 42.86 | 3.88 | 0.84 | 1.23 | 22.80 |
Note. IRT = item response theory; SD = standard deviation.
Rating scale used: 1 = no days, 2 = 1 day, 3 = 2–3 days, 4 = 4–5 days, 5 = 6–7 days. “Floor” referred to percentage of participants who endorsed “no days”; “ceiling” referred to percentage of participants who endorsed “6–7 days.”
Items were not calibrated together with the rest of items using IRT, but they were included in the Physical Activity calibrated scale.
Sleep Problems
Initial CFA results on the Sleep Disturbance item pool showed acceptable CFI (0.96) and R-squares (all items >0.3) but a non-acceptable RMSEA (0.19). A residual correlation of 0.28 was found between the only two positively worded items. We removed these items as their concepts were covered by other negatively worded items in the item pool. For the remaining eight items, CFI = 0.98, R-square = 0.51–0.84, RMSEA = 0.18, residual correlations <0.15. For Sleep-related Impairment, one item specific to children ages 3–5 years (“When my child didn’t sleep well, he/she had a hard time focusing”) was removed so that the resulting item pool was applicable across ages 1–5 years. Of the remaining items, CFI = 0.96, R-square = 0.53–0.84, and RMSEA = 0.20. Residual correlations were between 0.15 and 0.20 on two item-pairs.
We then evaluated unidimensionality of Sleep Problems using a bi-factor model, with a general factor of Sleep Problems and two local factors (Sleep Disturbance and Sleep-related Impairment). Content experts noted the original two domains may not be distinct in early childhood, suggesting a broader construct reflecting sleep problems may be more appropriate if the core facets were still represented. Psychometrically, a simulation study comparing fit indices under various lengths of survey and data distributions concluded that CFA fit values are sensitive to influence other than dimensionality of the data and recommended bi-factor analysis as an adequate and informative approach for developing an item bank (Cook et al., 2009). Results of our bi-factor analysis showed acceptable fit indices: CFI = 0.98, R-square = 0.53–0.69, RMSEA = 0.010, all residual correlations <0.1. All items had high loadings to the general factor (0.58–0.86). The majority (85%) of model variance was explained by the general factor, supporting sufficient unidimensionality; we concluded that a single Sleep Problems item bank was appropriate.
All 16 items fit the GRM model with chi-square/df <3. Slope parameters ranged from 1.76 to 3.2, and threshold parameters ranged from −1.42 to 2.77. No items exhibited DIF on child’s sex, parent’s sex, and child’s age groups. Thus, the final Sleep Problems item bank consisted of eight Sleep Disturbance items and eight Sleep-related Impairment items. Cronbach’s alpha for the full item bank was 0.95 (see Table II for item descriptive statistics).
Table II.
Item Descriptive Information—Sleep Problems Item Bank
| Item stem | Wave 1 (N = 700) |
Wave 2 (N = 1,057) |
||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Floor (%)a | Ceiling (%)a | Mean | SD | Floor (%)a | Ceiling (%)a | |
| It took my child a long time to fall asleep. | 2.55 | 1.07 | 17.43 | 4.86 | 2.12 | 0.97 | 31.69 | 1.32 |
| My child woke up too early and could not fall back asleep. | 2.35 | 1.03 | 22.86 | 4.00 | 1.88 | 0.91 | 42.57 | 0.28 |
| My child slept poorly. | 2.17 | 1.04 | 30.86 | 3.43 | 1.79 | 0.84 | 44.28 | 0.47 |
| My child resisted bedtime. | 2.62 | 1.12 | 19.86 | 5.00 | 2.35 | 1.06 | 26.77 | 2.27 |
| My child had difficulty falling asleep.b | 2.47 | 1.09 | 21.43 | 4.71 | 2.04 | 0.94 | 34.34 | 1.14 |
| My child woke up at night and had trouble falling back to sleep.b | 2.21 | 1.02 | 28.43 | 2.71 | 1.71 | 0.84 | 50.14 | 0.47 |
| My child tossed and turned at night.b | 2.55 | 1.08 | 19.14 | 4.43 | 1.98 | 0.96 | 39.83 | 0.57 |
| My child had trouble sleeping.b | 2.22 | 1.05 | 30.00 | 2.86 | 1.75 | 0.84 | 46.64 | 0.66 |
| When my child didn't sleep well, he/she got mad easily. | 2.85 | 1.11 | 14.00 | 7.86 | 2.29 | 1.02 | 28.86 | 1.23 |
| When my child didn't sleep well, he/she had more temper tantrums than usual. | 2.91 | 1.14 | 14.43 | 8.71 | 2.36 | 1.05 | 27.44 | 1.61 |
| My child seemed sleepy when he/she woke up. | 2.56 | 1.03 | 17.14 | 4.00 | 2.26 | 0.94 | 24.88 | 1.42 |
| My child could not keep his/her eyes open during the day. | 2.05 | 1.05 | 37.71 | 2.86 | 1.51 | 0.71 | 59.41 | 0.19 |
| When my child didn't sleep well, it was hard for him/her to play.b | 2.50 | 1.11 | 21.71 | 5.43 | 1.95 | 0.92 | 39.45 | 0.95 |
| When my child didn't sleep well, he/she was in a bad mood.b | 2.85 | 1.10 | 14.43 | 7.14 | 2.31 | 0.99 | 27.34 | 1.23 |
| When my child didn't get enough sleep, he/she became frustrated easily.b | 2.83 | 1.10 | 14.43 | 6.29 | 2.44 | 1.04 | 25.07 | 1.61 |
| My child's daytime activities or routines were disturbed by poor sleep.b | 2.36 | 1.09 | 25.43 | 3.86 | 1.71 | 0.78 | 47.68 | 0.09 |
Rating scale used: 1 = never, 2 = almost never, 3 = sometimes, 4 = almost always, 5 = always. “Floor” referred to percentage of participants who endorsed “never”; “ceiling” referred to percentage of participants who endorsed “always.”
Items included in the 8-item short form.
Item Calibration, Scale Information, and Reliability
All 7 (5 IRT-calibrated and 2 uncalibrated) Physical Activity items and 16 Sleep Problems items were included in wave 2 testing. The information function curves of the Physical Activity calibrated scale and Sleep Problems item bank are depicted in Figure 2. An IRT-based reliability of 0.9 and 0.7 occurred when the information function value equaled 10 and 3.3, respectively. For Physical Activity, IRT-based reliabilities ≥0.7 were found when T-scores were ≤54, suggesting that 66% of participants were measured precisely with an IRT-based reliability >0.7. For Sleep Problems, an IRT-based reliability ≥0.7 when T-scores were ≥31.6, indicating that 95% of participants were measured precisely with an IRT-based reliability ≥0.7.
Figure 2.
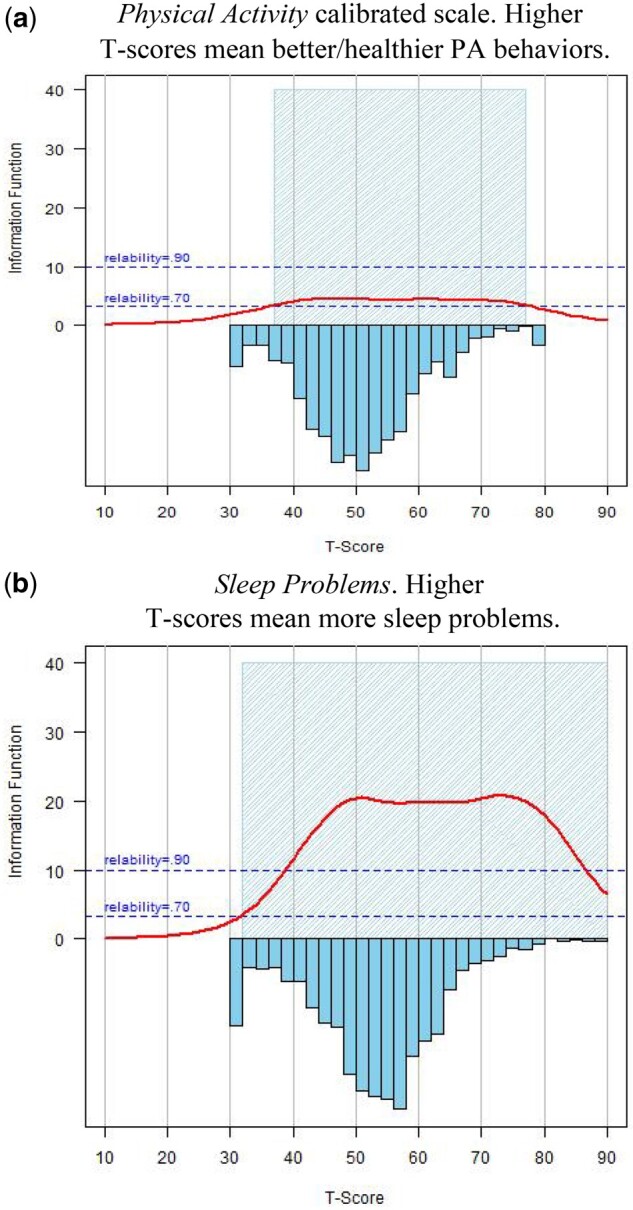
Comparisons of measure precision levels across the measurement continuum and the score distributions of both wave 1 and wave participants. (a) Physical Activity calibrated scale. Higher T-scores mean better/healthier PA behaviors. (b) Sleep Problems. Higher T-scores mean more sleep problems.Note. Y-axis represents information function. An information function value of 10 and 3.3 is corresponding to an IRT-based reliability of 0.90 and 0.70, respectively. X-axis represents T-scores, in which T = 50 is the mean of the U.S. general population. PA = Physical activity; IRT = item response theory.
CAT simulation of the Sleep Problems item bank showed that mean and median numbers of items administered were 4.69 (SD = 1.3) and 4, respectively. High correlation (r = 0.96) between scores obtained using CAT and the full-length item bank was found. We developed a 4- and 8-item short form (see Table II) with considerations of item content and better precision across the measurement continuum. We also developed sub-domain-specific short forms for those who wish to only evaluate sleep disturbance or sleep-related impairment. No CAT simulation was conducted for Physical Activity since it only consisted of five calibrated items.
Across-Domain Associations and Known-Groups Validity
The full correlation matrix across all domains is shown in Lai et al. (this issue, Table 4). Table III summarizes results that are related to Physical Health domains. Contrary to our hypothesis, Physical Activity scores were not significantly correlated with Global Health (r = 0.03, p = .251), and there were no differences in PA scores for children with versus without chronic physical health conditions (t(1742) = 1.08, p = .279). Children with EBD conditions had significantly higher Physical Activity scores than those who did not have EBD conditions (t(1735) = 3.00, p = .003). Physical Activity scores were significantly correlated with frequency of vigorous PA (r = 0.32, p < .001), which was consistent with our hypothesis. We further explored differences between age groups and found for children aged 3–5 years, children with EBD conditions had significantly higher Physical Activity scores than those who did not (t(1016) = 2.62, p = .009); yet we did not find significant differences on children aged 1–2 years (t(717) = 1.74, p = .082). No significant differences by age were found for physical health conditions.
Sleep Problems scores were significantly negatively correlated with Global Health (r = −0.36, p < .001). Children with physical health conditions and EBD conditions had worse parent-reported Sleep Problems than those without physical health conditions (physical health conditions: t(1742) = 9.81, p < .001; EBD: t(1735) = 12.18, p < .001). These results were consistent with our hypotheses. However, Sleep Problems scores were positively correlated with Physical Activity (r = 0.19, p < .001), which was contrary to our hypothesis that children with more sleep problems would have lower levels of physical activity compared to children with fewer sleep problems. Similar results were found when we analyzed by age group.
Discussion
We report the development and psychometric properties of the PROMIS EC Parent Report Physical Activity calibrated scale and Sleep Problems item bank for 1–5 years. These measures were developed to extend PROMIS to younger children to enable assessing PA and sleep problems in a psychometrically sound and developmentally sensitive manner. To enhance continuity across the lifespan within the PROMIS system from both conceptual and psychometric perspectives, we retained some PROMIS Pediatric items to allow for linking the early childhood versions to pediatric versions, enabling monitoring children’s PA behavior and sleep problems throughout the lifespan. Overall, both measures met the PROMIS standards with acceptable psychometric properties and were calibrated by using IRT, allowing for CAT or short form administrations. Both measures are reported using a T-score scoring system (mean = 50; SD = 10) and are referenced to parents with 1–5 years of the U.S. general population.
Known associations between childhood PA behaviors and sleep problems with health outcomes later in life (Cappuccio et al., 2008; Chaddock et al., 2012; Liese et al., 2013; Smaldone et al., 2007; Williamson et al., 2020) emphasize the importance of evaluating such constructs in early childhood. However, research on PA in young children is limited, due to the assumption that this age group is fairly active (Tremblay et al., 2012) and difficulties in accurately assessing what is often sporadic and short bouts of activity (Loprinzi & Cardinal, 2011). While children, on average, engage in significantly more physical activities than adults, their overall levels of PA still fall short of international health guidelines (Hnatiuk et al., 2014; Vanderloo et al., 2014, 2015). Similarly, various studies show 25–40% of healthy children and adolescents experience sleep problems (Erwin & Bashore, 2017; Meltzer & Mindell, 2008; Owens, 2007). In our study, 12.2% had sleep scores 1 SD worse than the norm. Such findings indicate that more is needed to improve younger children’s PA behavior and sleep.
Previous research on PA and sleep among young children was primarily conducted using complimentary methods of direct observation, sleep diaries, and devices such as actigraphy/accelerometers (Erwin & Bashore, 2017; Sylvia et al., 2014). Though such assessments are reliable and valid, they are impractical for large-scale epidemiological research and clinical practice due to the high cost and excessive administrative burden. PROs offer complementary assessments that evaluate children’s lived experience perceived by parents. While objective measures can provide important metrics on the timing and duration of PA and sleep as well as physiological indicators (e.g., heartrate, oxygen uptake, pulse oximetry), they cannot provide information on an individual’s PA experiences, perception of sleep quality, or the impact of sleep on daily functioning. While objective monitoring devices are commonly used to assess energy expenditure via absolute motion performed by the individual during specified time periods, PROMIS EC Physical Activity assesses a child’s performance of activities that require physical actions reflecting bodily movement levels ranging from simple static behaviors with minimal muscle activity to more complex activities involving dynamic or sustained muscle activity and greater movement of the body. Similarly, actigraphy may capture timing and duration of sleep, but PROMIS EC Sleep Problems capture sleep quality and impact. As suggested by prior research comparing scores between parent-report surveys and actigraphy on PA (Sarker et al., 2015) and sleep (Mazza et al., 2020), PROs may be valid complementary indicators of these constructs.
A major barrier to understanding PA in younger children is a reliance on the prototypical definitions of “activity” that are based on older children but may not always be applicable to the activity of toddlers and preschoolers. During concept elicitation interviews, parents described activities such as going up and down the stairs and used broad terms (e.g., “very active”) to describe their child’s PA behavior, and concepts such as exercise are not necessarily developmentally appropriate for 1–5 years. It was therefore not surprising that the early childhood version retained only the PROMIS Pediatric PA-related physiological symptom items verbatim. We thus included two un-calibrated items measuring children’s overall PA and frequencies of vigorous activity to maintain conceptual continuity. Responses on these two items do not contribute to the IRT-based PA T-scores but can be used to understand the degree to which children comply with the national and international PA guidelines. Similar to Physical Activity, different psychometric structures of sleep were found between young children and children 5 years and older. While Sleep-related Impairment and Sleep Disturbance are considered two separate constructs for older children, the early childhood version modeled them as two sub-domains under the same construct—Sleep Problems—and thus only one item bank was developed. If investigators are interested in only sleep disturbance or sleep-related impairment, we have created facet-specific short forms and scores from short forms are comparable to those from the full-length item banks (Lai et al., 2011).
Our results did not show a significant correlation between physical activity levels and general health, as measured by PROMIS EC Global Health, nor were there significant differences in PA scores for children with versus without chronic physical health conditions. One possible explanation for the lack of association found here is that while parents of young children with physical health conditions may be apprehensive for their children to engage in strenuous PA or certain PA activities, they also recognize the importance of PA to their children’s overall health and well-being; therefore, they may act no differently than parents of children without such conditions and, thus, their children have similar levels of general health.
Alternatively, the PROMIS EC Global Health instrument covers the broad domains of physical, mental, social, and overall health as stated by Kallen et al. (this issue), of which PA is only a small and more distal component. The physiological symptoms measured by PROMIS EC Physical Activity are part of one’s PA behavior, which is a component of the larger construct of physical functioning embedded in the broad domain of physical health. In addition, for young children, movement development includes physical exploration within their environment (e.g., reaching repeatedly outside the base of support, playing at low tables with frequent weight shifts). Thus, parents may perceive young children’s physical activities differently compared to older children and adults. Given the dearth of high-quality studies exploring the relationships between PA and physical health in young children (Carson et al., 2017), future studies are warranted to examine these hypotheses.
Our results showed that children with a higher level of physical activity had more sleep problems. This finding did not support our initial hypothesis. Extant literature presents inconsistent findings regarding the relationship between PA and sleep in early childhood. Our findings replicate those in a large-scale study of 3-year olds where more physical activity was associated with excessive sleep duration (Wang et al., 2016). However, Williams et al. (2014) found that 3–7-year olds who spent more time in light physical activities had lower total sleep time, with no significant relationships between moderate to vigorous physical activity and sleep. Such findings reflect those of Duraccio and Jensen (2017), where no associations were found between the number of days young children engaged in 20 min or more of physical activity and sufficient sleep. Alternatively, Zhang et al. (2019) found 12–28-month olds who engaged in less physical activity were more likely to have longer nighttime sleep durations, which is in direct contrast to work by Hager et al. (2016) who found 12–32-month olds who engaged in more moderate to vigorous physical activity had longer nighttime sleep durations. One primary limitation of these extant studies is the focus on sleep duration, rather than sleep quality, which is the focus of the PROMIS EC Sleep Problems instrument. Thus, future studies on the movement behavior continuum are needed, particularly to investigate the relationship between early childhood physical activity and sleep, as well as establish the optimal amount of moderate to vigorous physical activities, on which the PROMIS EC Physical Activity items focus.
Limitations and Future Directions
The primary aim of this study was to describe the creation of developmentally appropriate PROMIS early childhood measures for sleep and physical activity and to provide initial evidence for their unidimensionality and performance using IRT modeling consistent with PROMIS standards. The broad discussion of the strength and limitations of the methodologies used are available Cella et al. (this issue, qualitative approaches) and the Lai et al. (this issue, quantitative methods). Specific to this article, with consideration of respondent burden, this study did not include contextual information on additional PA or sleep moderators or legacy measures typically used to assess PA and sleep (e.g., accelerometry, existing surveys). We also did not collect information on parents, such as attitude toward child’s PA and their own PA, which was a strong predictor of child’s PA in prior work with older children (Tandon et al., 2014). Future studies should be conducted to comprehensively evaluate convergent and divergent validity with external criteria. There are multiple means to measure PA behaviors and sleep problems, yet no single comprehensive measure of choice. We chose a T-score metric system centering on the U.S. general population for interpretation consistent with the PROMIS system. This approach allows us to evaluate children who are not yet locomoting within normal developmental limits, and future studies can evaluate the performance of these measures in populations with significant impairments that result in their being non-ambulatory. In addition, we did not include sedentary behavior as part of the Physical Activity instrument because it is a separate domain in PROMIS. Future work to evaluate relationships between the PROMIS EC Physical Activity calibrated scale and measures of sedentary behavior and how that impacts sleep health can provide further insight into discriminant validity. Finally, given our focus on measurement development, we were limited in our ability to examine longitudinal predictive validity. However, we designed the measures to align conceptually with the PROMIS Pediatric versions for 5–17-year olds. Having the ability for continuous assessment while maintaining developmental specificity within life stages is a prime strength of the PROMIS Early Childhood Parent Report Physical Activity and Sleep Problems instruments. Importantly, taking advantages of IRT-based measures, clinicians and researchers now have a brief yet precise and psychometrically sound way to evaluate these understudied constructs in early childhood.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Funding
Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) program, Office of The Director, National Institutes of Health, under Award Number U24OD023319 with co-funding from the Office of Behavioral and Social Sciences Research (OBSSR; Person Reported Outcomes Core).
Conflicts of interest: None declared.
Supplementary Material
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th edn). American Psychiatric Association. [Google Scholar]
- Anderson L. M., Papadakis J. L., Vesco A. T., Shapiro J. B., Feldman M. A., Evans M. A., Weissberg-Benchell J. (2020). Patient-reported and parent proxy-reported outcomes in pediatric medical specialty clinical settings: A systematic review of implementation. Journal of Pediatric Psychology, 45(3), 247–265. [DOI] [PubMed] [Google Scholar]
- Armstrong B., Covington L. B., Hager E. R., Black M. M. (2019). Objective sleep and physical activity using 24-hour ankle-worn accelerometry among toddlers from low-income families. Sleep Health, 5(5), 459–465. 10.1016/j.sleh.2019.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevans K. B., Meltzer L. J., De La Motte A., Kratchman A., Viél D., Forrest C. B. (2019). Qualitative development and content validation of the PROMIS Pediatric Sleep Health items. Behavioral Sleep Medicine, 17(5), 657–671. [DOI] [PubMed] [Google Scholar]
- Bosquet Enlow M., White M. T., Hails K., Cabrera I., Wright R. J. (2016). The Infant Behavior Questionnaire-Revised: Factor structure in a culturally and sociodemographically diverse sample in the United States. Infant Behavior and Development, 43, 24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown W. H., Pfeiffer K. A., Mclver K. L., Dowda M., Almeida M. J. C. A., Pate R. R. (2006). Assessing preschool children's physical activity: The Observational System for Recording Physical Activity in children-preschool version. Research Quarterly for Exercise and Sport, 77(2), 167–176. [DOI] [PubMed] [Google Scholar]
- Bruni O., Ottaviano S., Guidetti V., Romoli M., Innocenzi M., Cortesi F., Giannotti F. (1996). The Sleep Disturbance Scale for Children (SDSC) Construct ion and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. Journal of Sleep Research, 54(4), 251–261. [DOI] [PubMed] [Google Scholar]
- Buysse D. J. (2014). Sleep health: Can we define it? Does it matter? Sleep, 37(1), 9–17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3902880/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio F. P., Taggart F. M., Kandala N.-B., Currie A., Peile E., Stranges S., Miller M. A. (2008). Meta-analysis of short sleep duration and obesity in children and adults. Sleep, 31(5), 619–626. 10.1093/sleep/31.5.619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson V., Lee E.-Y., Hewitt L., Jennings C., Hunter S., Kuzik N., Stearns J. A., Unrau S. P., Poitras V. J., Gray C., Adamo K. B., Janssen I., Okely A. D., Spence J. C., Timmons B. W., Sampson M., Tremblay M. S. (2017). Systematic review of the relationships between physical activity and health indicators in the early years (0-4 years). BMC Public Health, 17(S5), 33–63. 10.1186/s12889-017-4860-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaddock L., Erickson K. I., Prakash R. S., Voss M. W., VanPatter M., Pontifex M. B., Hillman C. H., Kramer A. F. (2012). A functional MRI investigation of the association between childhood aerobic fitness and neurocognitive control. Biological Psychology, 89(1), 260–268. 10.1016/j.biopsycho.2011.10.017 [DOI] [PubMed] [Google Scholar]
- Chaput J. P., Carson V., Gray C. E., Tremblay M. S. (2014). Importance of all movement behaviors in a 24 hour period for overall health. International Journal of Environmental Research and Public Health, 11(12), 12575–12581. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4276632/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. (1988). Statistical power analysis for the behavioral sciences. Routledge Academic. [Google Scholar]
- Chomistek A. K., Cook N. R., Flint A. J., Rimm E. B. (2012). Vigorous-intensity leisure-time physical activity and risk of major chronic disease in men. Medicine & Science in Sports & Exercise, 44(10), 1898–1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook K. F., Kallen M. A., Amtmann D. (2009). Having a fit: Impact of number of items and distribution of data on traditional criteria for assessing IRT's unidimensionality assumption. Quality of Life Research, 18(4), 447–460. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2746381/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duraccio K. M., Jensen C. D. (2017). Associations between physical and sedentary activity regularity and sleep in preschoolers and kindergartners. Sleep Health, 3(4), 263–268. [DOI] [PubMed] [Google Scholar]
- Erwin A. M., Bashore L. (2017). Subjective sleep measures in children: Self-report. Frontiers in Pediatrics, 5, 22–22. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5303893/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felzer-Kim I. T., Hauck J. L. (2020). Sleep duration associates with moderate-to-vigorous intensity physical activity and body fat in 1- to 3-year-old children. Infant Behavior & Development, 58, 101392. 10.1016/j.infbeh.2019.101392 [DOI] [PubMed] [Google Scholar]
- Forrest C. B., Meltzer L. J., Marcus C. L., De La Motte A., Kratchman A., Buysse D. J., Pilkonis P. A., Becker B. D., Bevans K. B. (2018). Development and validation of the PROMIS Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep, 41(6). [DOI] [PubMed] [Google Scholar]
- Goodlin-Jones B. L., Sitnick S. L., Tang K., Liu J., Anders T. F. (2008). The Children's Sleep Habits Questionnaire in toddlers and preschool children. Journal of Developmental & Behavioral Pediatrics, 29(2), 82–88. [DOI] [PubMed] [Google Scholar]
- Hager E. R., Calamaro C. J., Bentley L. M., Hurley K. M., Wang Y., Black M. M. (2016). Nighttime sleep duration and sleep behaviors among toddlers from low-income families: Associations with obesogenic behaviors and obesity and the role of parenting. Childhood Obesity (Print), 12(5), 392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthy People 2020. (2016). Nutrition, physical activity, and obesity. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Nutrition-Physical-Activity-and-Obesity. Retrieved 1 March 2022. [Google Scholar]
- Hnatiuk J. A., Salmon J., Hinkley T., Okely A. D., Trost S. (2014). A review of preschool children’s physical activity and sedentary time using objective measures. American Journal of Preventive Medicine, 47(4), 487–497. 10.1016/j.amepre.2014.05.042 [DOI] [PubMed] [Google Scholar]
- Hosker D. K., Elkins R. M., Potter M. P. (2019). Promoting mental health and wellness in youth through physical activity, nutrition, and sleep. Child and Adolescent Psychiatric Clinics of North America, 28(2), 171–193. 10.1016/j.chc.2018.11.010 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press. [PubMed]
- Lai J.-S., Butt Z., Zelko F., Cella D., Krull K., Kieran M., Goldman S. (2011). Development of a parent-report cognitive function item bank using item response theory and exploration of its clinical utility in computerized adaptive testing. Journal of Pediatric Psychology, 36(7), 766–779. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3146757/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai S. K., Costigan S. A., Morgan P. J., Lubans D. R., Stodden D. F., Salmon J., Barnett L. M. (2014). Do school-based interventions focusing on physical activity, fitness, or fundamental movement skill competency produce a sustained impact in these outcomes in children and adolescents? A systematic review of follow-up studies. Sports Medicine (Auckland, N.Z.), 44(1), 67–79. [DOI] [PubMed] [Google Scholar]
- LeBourgeois M. K., Harsh J. R. (2016). Development and psychometric evaluation of the Children's Sleep-Wake Scale. Sleep Health, 2(3), 198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennon C., Burdick H. (2004). Lexile frameworkas an approach for reading measurement and success. Lexile Framework for Reading. http://cdn.lexile.com/m/resources/materials/Lennon__Burdick_2004.pdf. Retrieved 1 March 2022.
- Liese A. D., Ma X., Maahs D. M., Trilk J. L. (2013). Physical activity, sedentary behaviors, physical fitness, and their relation to health outcomes in youth with type 1 and type 2 diabetes: A review of the epidemiologic literature. Journal of Sport and Health Science, 2(1), 21–38. [Google Scholar]
- Loprinzi P. D., Cardinal B. J. (2011). Measuring children's physical activity and sedentary behaviors. Journal of Exercise Science & Fitness, 9(1), 15–23. [Google Scholar]
- Matricciani L., Paquet C., Galland B., Short M., Olds T. (2019). Children's sleep and health: A meta-review. Sleep Medicine Reviews, 46, 136–150. 10.1016/j.smrv.2019.04.011 [DOI] [PubMed] [Google Scholar]
- Mazza S., Bastuji H., Rey A. E. (2020). Objective and subjective assessments of sleep in children: Comparison of actigraphy, sleep diary completed by children and parents' estimation. Frontiers in Psychiatry, 11, 495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer L. J., Mindell J. A. (2008). Behavioral sleep disorders in children and adolescents. Sleep Medicine Clinics, 3(2), 269–279. 10.1016/j.jsmc.2008.01.004 [DOI] [Google Scholar]
- Owens J. (2007). Classification and epidemiology of childhood sleep disorders. Sleep Medicine Clinics, 2(3), 353–361. 10.1016/j.jsmc.2007.05.009 [DOI] [Google Scholar]
- PROMIS Cooperative Group. (2013). PROMIS® Instrument Development and Validation Scientific Standards Version 2.0. https://www.healthmeasures.net/images/PROMIS/PROMISStandards_Vers2.0_Final.pdf. Retrieved 1 March 2022.
- Rodriguez-Ayllon M., Cadenas-Sánchez C., Estévez-López F., Muñoz N. E., Mora-Gonzalez J., Migueles J. H., Molina-García P., Henriksson H., Mena-Molina A., Martínez-Vizcaíno V., Catena A., Löf M., Erickson K. I., Lubans D. R., Ortega F. B., Esteban-Cornejo I. (2019). Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: A systematic review and meta-analysis. Sports Medicine, 49(9), 1383–1410. [DOI] [PubMed] [Google Scholar]
- Rowe D. C., Plomin R. (1977). Temperament in early childhood. Journal of Personality Assessment, 41(2), 150–156. [DOI] [PubMed] [Google Scholar]
- Samejima F. (1997). The graded response model. In van der Linden W. J., Hambleton R. (Eds.), Handbook of modern item response theory (pp. 85–100). Springer-Verlag. [Google Scholar]
- Sarker H., Anderson L. N., Borkhoff C. M., Abreo K., Tremblay M. S., Lebovic G., Maguire J. L., Parkin P. C., Birken C. S; TARGet Kids Collaboration (2015). Validation of parent-reported physical activity and sedentary time by accelerometry in young children. BMC Research Notes, 8(1), 735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smaldone A., Honig J. C., Byrne M. W. (2007). Sleepless in America: Inadequate sleep and relationships to health and well-being of our nation’s children. Pediatrics, 119(Supplement_1), S29–S37. 10.1542/peds.2006-2089F [DOI] [PubMed] [Google Scholar]
- Sylvia L. G., Bernstein E. E., Hubbard J. L., Keating L., Anderson E. J. (2014). Practical guide to measuring physical activity. Journal of the Academy of Nutrition and Dietetics, 114(2), 199–208. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3915355/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon P., Grow H. M., Couch S., Glanz K., Sallis J. F., Frank L. D., Saelens B. E. (2014). Physical and social home environment in relation to children's overall and home-based physical activity and sedentary time. Preventive Medicine, 66, 39–44. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4125450/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmons B. W., Leblanc A. G., Carson V., Connor Gorber S., Dillman C., Janssen I., Kho M. E., Spence J. C., Stearns J. A., Tremblay M. S. (2012). Systematic review of physical activity and health in the early years (aged 0-4 years). Applied Physiology, Nutrition, and Metabolism, 37(4), 773–792. 10.1139/h2012-070 [DOI] [PubMed] [Google Scholar]
- Tremblay M. S., LeBlanc A. G., Carson V., Choquette L., Connor Gorber S., Dillman C., Duggan M., Gordon M. J., Hicks A., Janssen I., Kho M. E., Latimer-Cheung A. E., LeBlanc C., Murumets K., Okely A. D., Reilly J. J., Spence J. C., Stearns J. A., Timmons B. W. (2012). Canadian physical activity guidelines for the early years (aged 0–4 years). Applied Physiology, Nutrition, and Metabolism, 37(2), 345–356. 10.1139/h2012-018 [DOI] [PubMed] [Google Scholar]
- Tucker C. A., Bevans K. B., Teneralli R. E., Smith A. W., Bowles H. R., Forrest C. B. (2014). Self-reported pediatric measures of physical activity, sedentary behavior, and strength impact for PROMIS: Item development. Pediatric Physical Therapy, 26(4), 385–392. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4176727/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderloo L. M., Tucker P., Johnson A. M., Burke S. M., Irwin J. D. (2015). Environmental influences on Preschoolers' physical activity levels in various early-learning facilities. Research Quarterly for Exercise and Sport, 86(4), 360–370. 10.1080/02701367.2015.1053105 [DOI] [PubMed] [Google Scholar]
- Vanderloo L. M., Tucker P., Johnson A. M., van Zandvoort M. M., Burke S. M., Irwin J. D. (2014). The influence of centre-based childcare on preschoolers’ physical activity levels: A cross-sectional study. International Journal of Environmental Research and Public Health, 11(2), 1794–1802. 10.3390/ijerph110201794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F., Liu H., Wan Y., Li J., Chen Y., Zheng J., Huang T., Li D. (2016). Sleep duration and overweight/obesity in preschool-aged children: A prospective study of up to 48,922 children of the Jiaxing birth cohort. Sleep, 39(11), 2013–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams S. M., Farmer V. L., Taylor B. J., Taylor R. W. (2014). Do more active children sleep more? A repeated cross-sectional analysis using accelerometry. PLoS One, 9(4), e93117. 10.1371/journal.pone.0093117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson A. A., Mindell J. A., Hiscock H., Quach J. (2020). Longitudinal sleep problem trajectories are associated with multiple impairments in child well-being. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 61(10), 1092–1103. 10.1111/jcpp.13303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2019). Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. World Health Organization. https://apps.who.int/iris/handle/10665/311664. Retrieved 1 March 2022. [PubMed] [Google Scholar]
- Young N. L., Williams J. I., Yoshida K. K., Wright J. G. (2000). Measurement properties of the activities scale for kids. Journal of Clinical Epidemiology, 53(2), 125–137. [DOI] [PubMed] [Google Scholar]
- Zhang Z., Sousa-Sá E., Pereira J., Chaput J. P., Okely A., Feng X., Santos R. (2019). Correlates of nocturnal sleep duration, nocturnal sleep variability, and nocturnal sleep problems in toddlers: Results from the GET UP! study. Sleep Medicine, 53, 124–132. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.